Abstract
Objective
To determine how much future smoking-related mortality in the USA can be prevented, recognising that some of that future mortality results from past smoking.
Methods
Employing a dynamic population simulation model, we estimate smoking’s expected mortality burden in the USA, measured as life-years lost (LYL), in a status-quo scenario run from 2018 through 2100. We then estimate LYL attributable to past smoking assuming that all smoking ceases at the end of 2017. We calculate the potential avoidable LYL, which we call the maximum potential reduction in premature mortality (MPRPM), as the difference between the two. We use data from the US Census Bureau, National Vital Statistics Reports, the National Health Interview Survey and Cancer Prevention Study II.
Results
Under status-quo assumptions, smoking will claim 305 million LYL in the US from 2018 to 2100. If all smoking ceased at the end of 2017, past smoking would be responsible for 191.8 million LYL. Thus, avoidable LYL by 2100—the MPRPM—would be 113.2 million, 37% of the expected toll of smoking. A sensitivity analysis finds that were the annual smoking initiation rate 3% instead of 7.8%, the MPRPM would be 13–14% lower. Were the annual permanent smoking cessation rate twice our status-quo estimate of 4.35%, the MPRPM would be 38–39% lower.
Conclusions
Public health can address only the future toll of future smoking. Smoking’s MPRPM is the reduction in the mortality burden of smoking that tobacco control can strive to achieve.
INTRODUCTION
Public health has achieved great success in tobacco control in the USA over the past half century.1 Yet smoking still claims the lives of 480 000 Americans annually.2 Further, recent research has found that if current trends in smoking continue, smoking will cause tens of millions of premature deaths and hundreds of millions of lost life years in the USA by the end of the 21st century.3,4 Avoiding as much of this enormous toll as possible constitutes a major public health goal going forward.
But how much of smoking’s mortality burden can be avoided? Lost in discussions about smoking’s future toll is that much of it is already ‘baked in’ by virtue of smokers’ past cigarette consumption. Even if all smokers stopped smoking instantaneously, and no one started to smoke subsequently, smoking-related mortality would persist well into the future, reflecting the risks accrued by former smokers. That burden can be approximated by estimating future life-years lost (LYL) in the hypothetical situation in which all smoking ceased instantly and permanently. To determine avoidable future mortality, one can calculate total LYL due to smoking assuming continuation of current trends in smoking initiation and cessation, and then subtract the burden associated with former smoking. We estimate this avoidable smoking-produced mortality and compare it to the anticipated toll of smoking through the year 2100. We call the avoidable LYL the maximum potential reduction in premature mortality (MPRPM), the true feasible reduction in the mortality burden of smoking that tobacco control can strive to achieve.
METHODS
We employ a dynamic population simulation model used frequently in previous research,4 including two studies in which it accurately predicted US smoking prevalence.5,6 The model follows individuals from ages 0 to 110, distinguished by gender and smoking status. Census data provide birth cohort sizes.7 Age-specific and gender-specific death rates come from National Vital Statistics Reports.8 We use findings from Cancer Prevention Study II to produce age-specific and gender-specific death rates by smoking status (including years quit for former smokers).9 Initial age-specific and gender-specific smoking rates come from the National Health Interview Survey.10
At age 18, individuals are current or never smokers. Current smoking prevalence for 18–24 years old was 7.8% in 2018.11 We treat this as the smoking initiation rate, assuming no initiation at older ages. Individuals who begin smoking prior to 18 are included in the 18-year-olds’ prevalence (and hence in the initiation rate). The annual permanent smoking cessation rate, 4.35%, derives from a previous analysis using this model.12 The model assumes no smoking-related deaths before age 35.
After 18, current smokers in any given year equal the number of current smokers in the preceding year who survived to the current year and did not quit smoking. Former smokers are surviving former smokers from the previous year plus the previous year’s current smokers who quit smoking and did not die.
The model assumes that the smoking cessation rate does not vary with age. The effect of variation in this assumption is relatively small, as described in a working paper available here.
The model is calibrated to 2017 data. A complete description of the structure of the model is available in the online supplementary material.
We run the model under three different scenarios for the years 2018–2100:
The status-quo scenario maintains annual smoking initiation and cessation rates at 2018 levels through 2100. This scenario reflects what we expect to happen to the US population if nothing changes in terms of the future pattern of smoking initiation and cessation.
The no-future-smoking scenario assumes the age-specific and gender-specific distribution of smoking in 2017 but with all smokers quitting at the end of that year and no one starting thereafter. This scenario reflects solely the future burden of past smoking (prior to 2018).
The never-smoking scenario assumes that no one ever smoked and hence there is no smoking-related mortality. (All individuals in the model are subjected to never-smoker death rates.)
We estimate smoking’s mortality burden through 2100, measured as the number of LYL due to smoking, by subtracting, each year, the number of person years in the status-quo scenario from the number of person years in the never-smoking scenario. We then cumulate the individual years’ differences through 2100. Similarly, we estimate the LYL burden of former smoking by subtracting the number of person years in the no-future-smoking scenario from the number of person years in the never-smoking scenario. Finally, we calculate the avoidable LYL (the MPRPM) by subtracting the LYL under the no-future-smoking scenario from the LYL in the status-quo scenario. We also measure the MPRPM in relative terms by dividing MPRPM LYL by status quo LYL. In relative terms, the MPRPM thus is the percentage of the expected cumulative LYL due to smoking through a given year that can be avoided by preventing future smoking.
The smoking initiation rate has declined rapidly in the USA in recent years, from 20.1% in 201013 to 7.8% in 2018.11 The cessation rate has increased.12 Simply as a matter of existing trends, initiation might decline further and cessation increase more in the coming years; that is, such rate changes could result from previous tobacco control efforts and the trends in initiation and cessation they produced. To consider the impact of such changes on future LYL due to smoking and on the MPRPM, we perform a sensitivity analysis in which we examine the effects of assuming two lower initiation rates (3% and 5%, compared with the base-case assumption of 7.8%) and three larger cessation rates (increasing the base-case rate of 4.35% by 25%, 50% and 100%).
RESULTS
The red line in figure 1 shows cumulative LYL from 2018 to 2100 due to smoking under the status quo model assumption that the 2018 smoking initiation and cessation rates will continue through 2100. The blue line shows cumulative LYL through 2100 if all smokers had quit smoking at the end of 2017, with no smoking initiation thereafter. Smoking’s mortality toll in this scenario reflects the residual risk that former smokers carry throughout their lives. The difference between the two lines is the MPRPM (the green line), the LYL that could be avoided by additional effective tobacco control.
Figure 1.
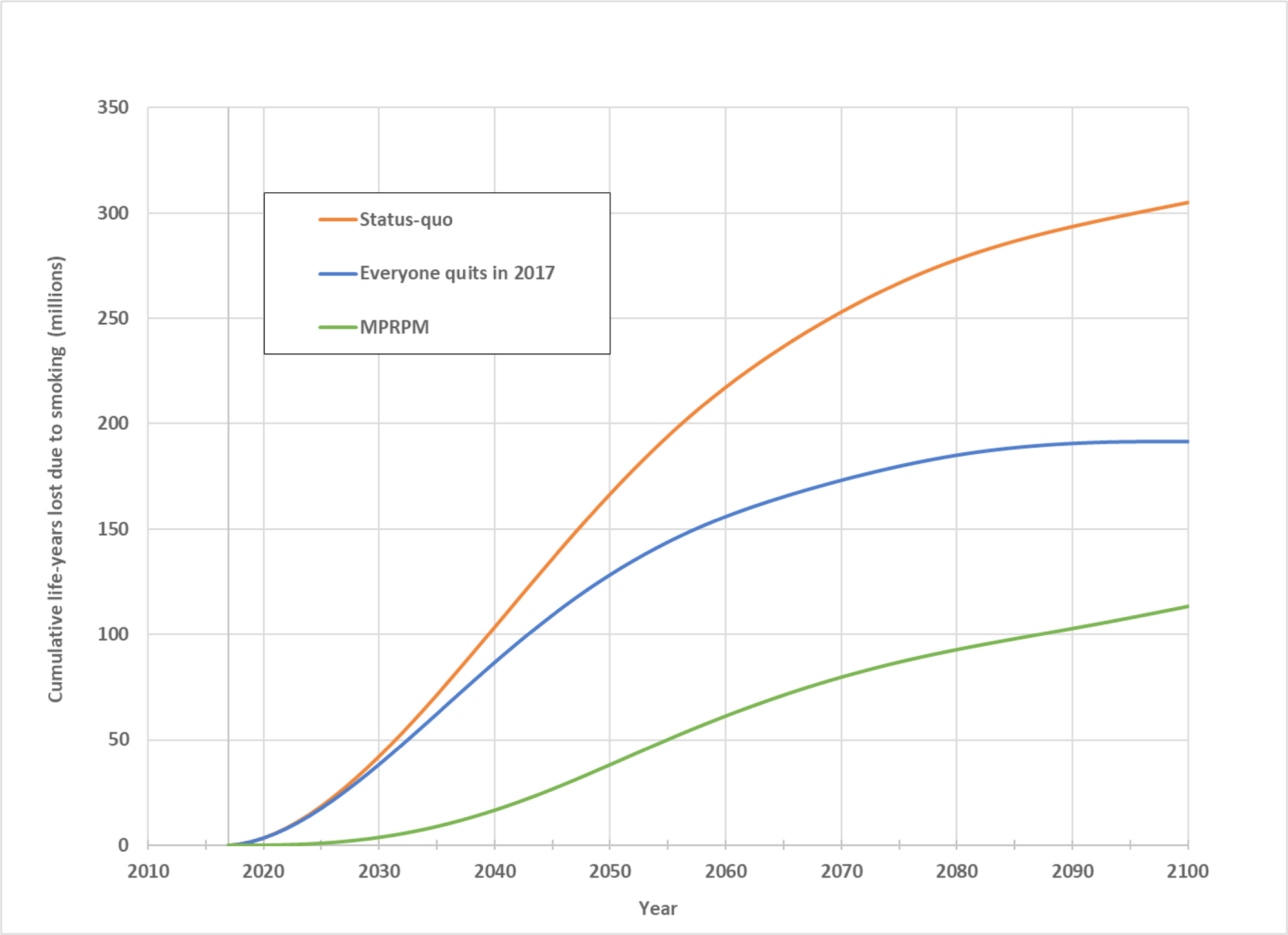
Cumulative life-years lost due to smoking, 2018–2100. MPRPM, maximum potential reduction in premature mortality.
Under status quo assumptions, we estimate that smoking will be responsible for 305 million LYL by 2100. If all smoking were to have ceased instantaneously by the end of 2017, 191.8 million life years would still be lost due to former smokers’ reservoir of smoking-related risk. Thus, avoidable LYL by 2100—the MPRPM—would be 113.2 million years, 37.1% of the toll of smoking. The MPRPM rises from 1.0 million years, and 5.4% of smoking’s toll, in 2025, to 38.2 million years and 22.9% in 2050, to 86.8 million years and 32.5% in 2075, to the year 2100 figures just noted. (The specific annual numerical results are available in online supplementary Table S-1.)
Figure 2 shows the results of the sensitivity analysis for the year 2100. The first 4 bars include the base case, with initiation and cessation rates effective in 2018 (7.8% and 4.35%, respectively (case 1)) and 3 subsequent cases in which, while initiation remains at 7.8%, the cessation rate increases by 25% (case 2), 50% (case 3) and 100% (case 4). In the second 4 bars, cases 5–8, the initiation rate is set at 5% and the cessation rate varies as for cases 1–4. In the final 4 bars, cases 9–12, the initiation rate is set at 3% and the cessation rate varies as for cases 1–4. The bars present MPRPM in millions of LYL. The line presents MPRPM as a percentage of the status quo LYL.
Figure 2.
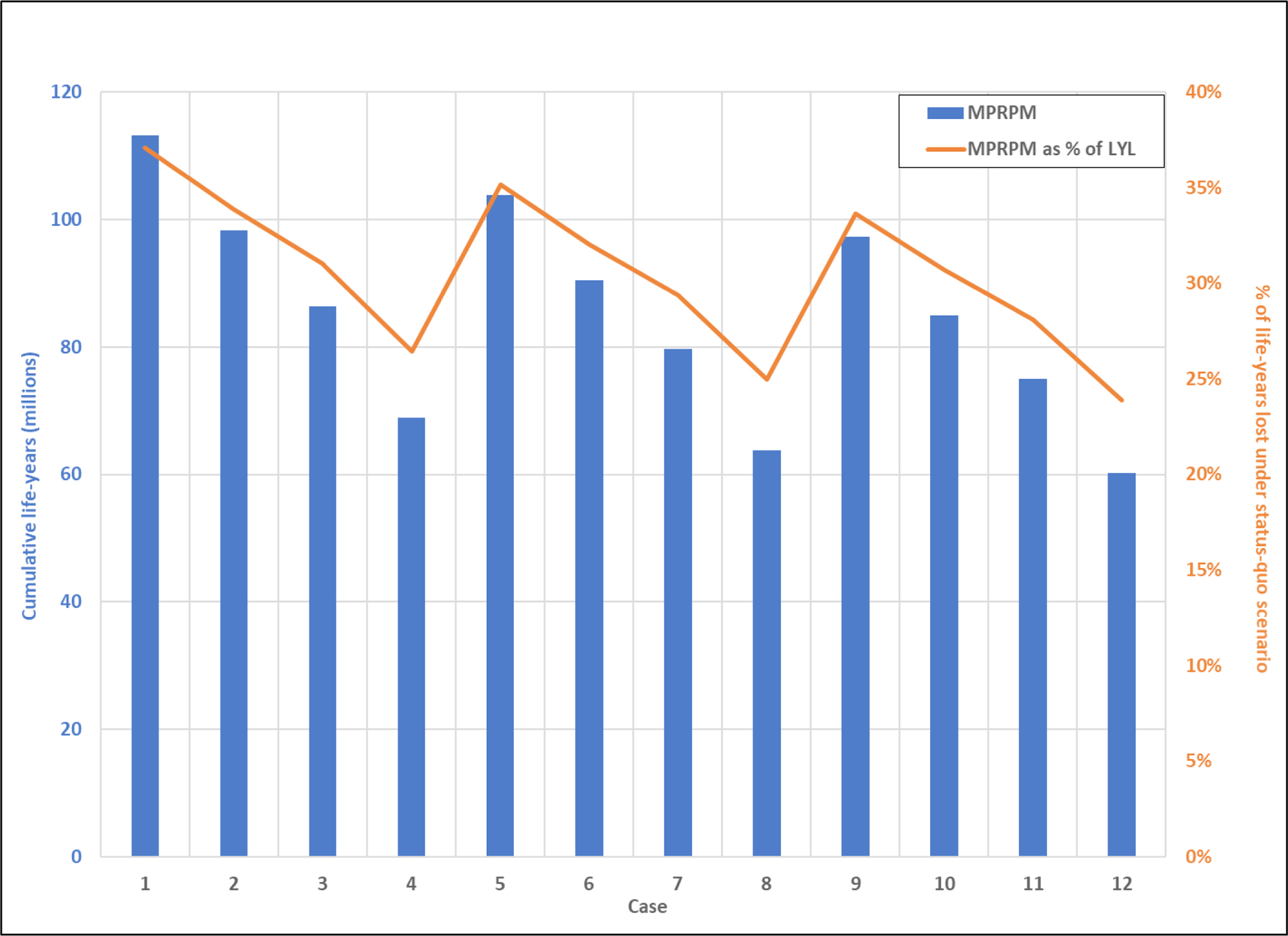
Maximum potential reduction in premature mortality (MPRPM) in 2100 under varied assumptions about smoking initiation and cessation rates. Case 1: 2018 initiation rate (7.8%) and cessation rate (4.35%). Cases 2–4: 2018 initiation rate (7.8%) and cessation rate increase of, respectively, 25% (to 5.44%), 50% (to 6.53%) and 100% (to 8.7%). Cases 5–8: initiation rate of 5% and cessation rates corresponding to those in cases 1–4. Cases 9–12: initiation rate of 3% and cessation rates corresponding to those in cases 1–4.
Case 1 results show the findings presented above for the base case (an MPRPM of 113.2 million LYL, constituting 37% of the toll of smoking). Holding the cessation rate constant, as the initiation rate declines from 7.8% (cases 1–4) to 3% (cases 9–12), MPRPM falls by 13–14% (eg, from 113.2 million to 97.3 million LYL in cases 1 and 9, respectively). Holding the initiation rate constant, as the cessation rate increases from 4.35% to 8.7% (ie, a 100% increase in the cessation rate), MPRPM falls by 38–39% (eg, from 113.2 million to 68.9 million in cases 1 and 4, respectively). MPRPM as a per cent of the status quo mortality burden of smoking follows a similar pattern, varying from a high of 37% in the base case (case 1) to a low of 24% in case 12. Case 12 represents the lowest initiation rate (3%) and the highest cessation rate (8.7%).
DISCUSSION
If smoking initiation and cessation rates in 2018 do not change, by 2100 smoking’s mortality toll will reach a breathtaking 305 million LYL. Perhaps more surprising, however, is that over 60% of that total results from former smokers’ continuing elevated risk of smoking-related premature mortality. Public health can address only the remainder, the future toll of future smoking. That remainder—smoking’s MPRPM—is the maximum reduction in the mortality burden of smoking that tobacco control can strive to achieve.
The sensitivity analysis demonstrates that the specific value of MPRPM (and of MPRPM as a per cent of status-quo LYL) is highly sensitive to the assumed smoking initiation and cessation rates, particularly the latter. For example, were the annual smoking cessation rate twice that of our base-case assumption, the MPRPM, measured as LYL, would fall by nearly 40%. This illustrates the dynamism of MPRPM: if either the smoking initiation rate or the cessation rate changes in the coming years as the result of past tobacco control interventions, estimates of MPRPM in the future will change substantially. See the online supplementary material for a detailed explanation.
The essential point, therefore, is not the specific year’s quantitative estimate of MPRPM. Rather it is the qualitative appreciation that our ability as a public health community to stem the future mortality toll of smoking is seriously constrained by the future burden associated with past smoking. This is not to suggest that persisting in aggressive tobacco control efforts is futile. Far from it. MPRPM may be a surprisingly small proportion of the projected toll of smoking. But its absolute value—in the present analysis, 113.2 million life years by 2100—is very large, reflecting the enormity of the anticipated future mortality burden of smoking. Reducing any significant portion of 113.2 million LYL would represent a major public health victory.
The concept of MPRPM applies to many public health problems. For example, were all alcohol abuse to cease entirely, we would continue to experience fatal cases of cirrhosis of the liver, cancer and heart disease reflecting past alcohol consumption. With regard to any public health problem, MPRPM allows us to understand the magnitude of mortality problems that can be addressed, and thereby to set more realistic goals as we aim for a healthier society.
Supplementary Material
What this paper adds.
Despite great tobacco control success, cigarette smoking still kills approximately 480 000 Americans every year.
What is not known, and indeed never previously considered, is what proportion of the future mortality toll of smoking can be prevented.
Some fraction of that future mortality toll is ‘baked in’ due to former smoking and thus cannot be avoided.
We estimate that smoking will be responsible for the loss of 305 million life years among Americans between 2018 and 2100 of which 191.8 million (63%) will result from smoking that occurred prior to 2018.
Only the future life years lost due to future smoking, which we call maximum potential reduction in premature mortality—113.2 million life years (37% of the expected total toll)—can be prevented by successful tobacco control.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health and Food and Drug Administration Centre for Tobacco Products (Award Number U54CA229974).
Footnotes
Publisher's Disclaimer: Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.U.S. Department of Health and Human Services. The health consequences of smoking: 50 years of progress. A report of the surgeon General Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. Printed with corrections, 2014. Available: https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf [Accessed 24 Nov 2019]. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Burden of cigarette smoking in the U.S. Centers for Disease Control and Prevention Available: https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html [Accessed 3 Mar 2020]. [Google Scholar]
- 3.Levy DT, Borland R, Lindblom EN, et al. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob Control 2018;27:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warner KE, Mendez D. E-Cigarettes: comparing the possible risks of increasing smoking initiation with the potential benefits of increasing smoking cessation. Nicotine Tob Res 2019;21:41–7. [DOI] [PubMed] [Google Scholar]
- 5.Mendez D, Warner KE. Adult cigarette smoking prevalence: declining as expected (not as desired). Am J Public Health 2004;94:251–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warner KE, Méndez D. Accuracy and importance of projections from a dynamic simulation model of smoking prevalence in the United States. Am J Public Health 2012;102:2045–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United States Census Bureau. Annual estimates of the resident population by single year of age and sex for the United States: April 1, 2010 to July 1, 2016 (NC-EST2016-AGESEX-RES). Available: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk [Accessed 4 Nov 2019].
- 8.United States. NCHS, National vital statistics system, mortality, 2017. Available: https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_07-508.pdf [Accessed 3 Mar 2020].
- 9.Warner KE, Mendez D, Smith DG. The financial implications of coverage of smoking cessation treatment by managed care organizations. Inquiry 2004;41:57–69. [DOI] [PubMed] [Google Scholar]
- 10.Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults - United States, 2017. MMWR Morb Mortal Wkly Rep 2018;67:1225–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68:1013–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Méndez D, Tam J, Giovino GA, et al. Has smoking cessation increased? an examination of the US adult smoking cessation rate 1990–2014. Nicotine Tob Res 2017;19:1418–24. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). Vital signs: current cigarette smoking among adults aged ≥18 years--United States, 2005–2010. MMWR Morb Mortal Wkly Rep 2011;60:1207–12. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


