Abstract
Background
Contemporary studies note sustained clinical benefit and decreasing complications after reverse total shoulder arthroplasty (RTSA), which warrant a comparison with the standard anatomic total shoulder arthroplasty (ATSA). The purpose of this study is to evaluate and compare differences in midterm survivorship between ATSA and RTSA patients treated with a single platform shoulder prosthesis. Secondary objectives include a comparison of the clinical outcomes and complication profile for each procedure.
Methods
A prospective analysis of all primary ATSA and RTSA performed by 3 surgeons between 2007 and 2012 was conducted. Selection of the ATSA or RTSA implant configuration was determined by the surgeons per their clinical understanding of each individual patient's glenoid morphology, rotator cuff, and patient expectations. All 778 procedures were performed using a single platform shoulder system.
Results
Survivorship for ATSA was similar to that for RTSA at all time points; ATSA at 2 and 8 years was 98.5% and 96.0%, whereas RTSA at 2 and 8 years was 98.7% and 96.0%, respectively ( P= .392). All postoperative range of motion scores for ATSA patients were greater than those for RTSA patients. The overall rate of complications between the ATSA and RTSA groups was similar (6.3% vs. 4.9%, P= .414).
Conclusions
On the basis of this cohort comparison, both ATSA and RTSA demonstrated similar survivorship at 8 years after surgery with multiple surgeons practicing in different countries. Our results demonstrate that the RTSA and ATSA implants have comparable results and can be expected to provide similar implant longevity over the midterm with excellent functional outcomes.
Keywords: Shoulder arthroplasty, anatomic shoulder arthroplasty, reverse shoulder arthroplasty, shoulder arthroplasty survivorship, shoulder arthroplasty performance scores, shoulder arthroplasty complications
Modern studies demonstrate a sustained clinical benefit and decreasing complication rate after reverse total shoulder arthroplasty (RTSA), prompting a comparison with the standard anatomic total shoulder arthroplasty (ATSA).23,28,37,38,40 In the setting of rotator cuff compromise or significant glenoid deformity, the benefits of RTSA are apparent.11,23,34 However, as the indications for RTSA have widened, patients may be considered candidates for either RTSA or ATSA based on age, preoperative function, glenoid bone loss, retroversion, and rotator cuff disease without full thickness rotator cuff tears.16,22,37,
Given the option of 2 different shoulder arthroplasty surgical procedures (RTSA and ATSA) for overlapping patient indications, the orthopedic surgeon must consider the differences in postoperative outcomes in relation to each patient's individual goals and requirements. Differences in postoperative range of motion (ROM) and complication rates have been previously reported between ATSA and RTSA. Because of the unconstrained design of the ATSA and an intact rotator cuff, it is reported to have a greater ROM than RTSA.2,35
Historically, RTSA complication and revision rates have exceeded the rates for ATSA causing some surgeons trepidation regarding the procedure.23 However, with modern implant designs, RTSA complications and revision rates have decreased4 such that these rates are similar to those of ATSA.8,18,33,39 The most frequent complications for ATSA remain aseptic glenoid loosening and rotator cuff tears,10,12,13,15,24 which lead to an increased rate of revision surgery at midterm follow-up.29 The most frequent complication for RTSA is scapula notching, but this rarely results in the need for revision. Other complications after RTSA are glenoid component failure and instability both of which typically result in the need for revision surgery.6 With modern implants and techniques, it is important to continually re-evaluate the survivorship curves of ATSA and RTSA as differences may exist. Previous reports have evaluated revision rates of ATSA and RTSA at midterm or longer follow-up, but these have failed to evaluate the survivorship over time using more traditional survivorship analyses.8,18,19,37 The primary purpose of this study is to evaluate and compare differences in midterm survivorship between ATSA and RTSA patients treated with a single platform shoulder prosthesis. Secondary objectives include a comparison of the clinical outcomes and complication profile for each procedure.
Methods
A retrospective analysis of all primary ATSA and RTSA performed on prospectively collected data by 3 fellowship-trained high-volume surgeons between 2007 and 2012 was conducted. Data were collected through a multinational shoulder arthroplasty registry operated by the sponsor (WIRB approved #20091701), using standardized data collection forms. Patients were excluded if they had a preoperative diagnosis of infection, revision arthroplasty, humeral fracture, neuromuscular disorders, brachial plexopathy, and alcohol/substance abuse.
Selection of the ATSA or RTSA implant configuration was determined by the surgeons per their clinical understanding of each individual patient's glenoid morphology, rotator cuff, and patient expectations. Seven hundred seventy-eight shoulders (286 ATSA [M = 125/F = 160/1 unknown] and 492 RTSA [M = 156/F = 336]) were evaluated in this study. All patients were included for survivorship analysis. However, only patients with a minimum 2-year follow-up (253 ATSA, 382 RTSA) were included in clinical outcomes analysis. ATSA patients had a mean follow-up of 64.0 ± 32.0 months, and RTSA patients had a mean follow-up of 56.4 ± 23.8 months. All ATSA were performed with a hybrid (biologic central cage and 3 peripheral titanium cemented pegs) (n = 144) or keel (n = 142) cemented glenoid component. RTSA surgeries were performed using the same platform stem with nonaugmented glenoid baseplates.
Patients were evaluated preoperatively, through the immediate postoperative period (2-24 weeks), and annually thereafter. At each visit, the surgeons and/or their surrogate evaluated the patient assessing ROM and obtained multiple different patient-reported outcome scores. ROM was measured using a goniometer during active shoulder movements including abduction, forward elevation, and external rotation. Internal rotation was assessed using an 8-point scale ranging from no internal rotation (hip) = 0 to full internal rotation (T7 or higher) = 7.14 Strength in forward elevation was measured in pounds. Patient outcomes were quantified using the global shoulder function score (0-10), patient satisfaction rating (assessment of their shoulder condition presurgery to postsurgery, with possible responses being worse, unchanged, better, or much better), visual analog scale pain score (0-10), Simple Shoulder Test (SST), Constant-Murley score (CONSTANT), American Shoulder and Elbow Surgeons assessment (ASES), University of California Los Angeles Shoulder Score (UCLA), and the Shoulder Pain and Disability Index (SPADI).3,7,21,26,27 At each postoperative visit, radiographs were evaluated for humeral radiolucent lines according to Sanchez et al, radiolucent glenoid lines according to Lazarus et al (ATSA only), and scapular notching according to Sirveaux et al (RTSA only).20,28,32 Postoperative complications and reoperations were also recorded at each visit.
A survivorship analysis was performed using the Kaplan-Meier method. The survivorship analysis (Kaplan-Meier, complication rates, and revision rates) included all patients (N = 778). Patients undergoing any operation requiring explant of any component were classified as revised or failed.
Statistical analysis
Statistical analyses compared outcome measures between ATSA and RTSA patients. Numeric outcome measure comparisons were performed using a Student's t-test. Gender, diagnosis, patient satisfaction ratings, and complication rates were analyzed with the χ2 analysis. A comparison of the survivorship curves was performed with the log-rank test. Depending on the observed frequencies, the complication and revision rates were evaluated with the Fisher exact test or the χ2 test.
Results
The majority of patients had a diagnosis of osteoarthritis (ATSA = 93%, RTSA = 58%). RTSA patients were significantly older (74 vs. 68, P < .001) and more commonly female (68% vs. 56%, P < .001). See Table I for full demographic details.
Table I.
Patient demographics, indications for surgery, and duration of postoperative follow-up for each study group
| Study demographics | ATSA group | RTSA group | P value |
|---|---|---|---|
| Group size | 286 | 492 | – |
| Gender | |||
| Female | 160 (56%) | 336 (68%) | χ2 = 12 P < .001 |
| Male | 126 (44%) | 156 (32%) | |
| Age at surgery | |||
| Average ± SD | 67.8 ± 9.6 | 74.2 ± 7.4 | <.001 |
| Demographic characteristics | |||
| Height (cm) | 165.9 ± 12.4 | 157.7 ± 30.0 | <.001 |
| Weight (kg) | 79.4 ± 17.6 | 71.4 ± 21.0 | <.001 |
| BMI | 29.4 ± 15.0 | 28.1 ± 12.5 | .236 |
| Diagnosis | |||
| Osteoarthritis | 261 (91.3 %) | 138 (28.0%) | χ2 = 194 P < .001 |
| Osteoarthritis and rotator cuff insufficiency | 8 (2.8%) | 150 (30.5%) | |
| Rotator cuff insufficiency | 0 (0%) | 136 (27.6%) | |
| Other | 17∗ (5.9%) | 68† (13.8%) | |
SD, standard deviation; BMI, body mass index; ATSA, anatomic total shoulder arthroplasty; RTSA, reverse total shoulder arthroplasty.
Other diagnoses are post-traumatic arthritis (7), osteonecrosis (4), fracture (2), rheumatoid arthritis (1), psoriatic arthropathy (1), and not documented (2).
Other diagnoses are fracture (26), post-traumatic arthritis (8), rheumatoid arthritis (4), osteonecrosis (3), instability (3), pseudoparalysis (2), bicep synovectomy (2), neuropraxia (1), and not documented (19).
RTSA shoulders had similar preoperative active forward elevation and external rotation ROM scores to ATSA patients, as well as similar preoperative ASES and SPADI patient-reported outcome measures. RTSA shoulders did have greater internal rotation than ATSA patients (RTSA = 3.6, ATSA = 3.1, P = .003) but significantly less preoperative active abduction (RTSA = 77°, ATSA = 83°, P = .04). Furthermore, the RTSA preoperative scores SST, CONSTANT, and UCLA were lower than those for ATSA patients, and the preoperative RTSA max strength was much lower (RTSA = 1.0 kg, ATSA = 2.9 kg, P < .001).
All postoperative ROM scores for ATSA patients were greater than those for RTSA patients ([active abduction ATSA = 131, RTSA = 114, P < .001], [forward elevation ATSA = 150, RTSA = 141, P < .001], [external rotation ATSA = 48, RTSA = 36, P < .001], and [internal rotation ATSA = 5.2, RTSA = 4.7, P < .001]). Furthermore, the postoperative max strength for ATSA patients was significantly higher (ATSA = 4.1 kg, RTSA = 3.5 kg, P = .002) (Table II). ATSA patient–reported outcome measure (SST) was greater than RTSA (ATSA = 10.9, RTSA = 10.0, P = .022), whereas no differences were observed in the CONSTANT, ASES, UCLA, and SPADI postoperative scores between RTSA and ATSA patients.
Table II.
Average and standard deviation of the preoperative and postoperative performance metrics for each patient group
| Clinical metric | Time of measure | ATSA | RTSA | P value |
|---|---|---|---|---|
| Active abduction | Preop | 83 ± 30 | 77 ± 33 | .038 |
| Last postop | 131 ± 36 | 114 ± 32 | <.001 | |
| Delta | 53 ± 44 | 34 ± 43 | <.001 | |
| Active forward elevation | Preop | 107 ± 36 | 103 ± 43 | .215 |
| Last postop | 150 ± 34 | 141 ± 29 | <.001 | |
| Delta | 51 ± 44 | 39 ± 45 | .003 | |
| Active external rotation | Preop | 15 ± 23 | 16 ± 24 | .529 |
| Last postop | 48 ± 21 | 36 ± 20 | <.001 | |
| Delta | 35 ± 26 | 19 ± 27 | <.001 | |
| Active internal rotation | Preop | 3.1 ± 1.6 | 3.6 ± 1.9 | .003 |
| Last postop | 5.2 ± 1.4 | 4.7 ± 1.6 | <.001 | |
| Delta | 2.1 ± 1.9 | 1.2 ± 2.2 | <.001 | |
| Forward flexion max strength (kg) | Preop | 2.9 ± 2.8 | 1.0 ± 1.5 | <.001 |
| Last postop | 4.1 ± 2.6 | 3.5 ± 2.3 | .002 | |
| Delta | 1.3 ± 2.9 | 2.5 ± 2.2 | <.001 | |
| Shoulder function | Preop | 3.6 ± 1.7 | 2.9 ± 1.5 | <.001 |
| Last postop | 8.2 ± 2.0 | 7.9 ± 2.0 | .018 | |
| Delta | 4.6 ± 2.6 | 4.7 ± 2.3 | .650 | |
| VAS daily pain | Preop | 6.2 ± 1.9 | 6.1 ± 1.8 | .589 |
| Last postop | 1.3 ± 2.1 | 1.2 ± 2.1 | .526 | |
| Delta | −4.6 ± 3.1 | −4.8 ± 2.6 | .553 | |
| Patient satisfaction rating | Not recorded | 17 | 33 | χ2 = 6.8 P = .079 |
| Worse | 7 | 9 | ||
| Unchanged | 13 | 9 | ||
| Better | 43 | 94 | ||
| Much better | 206 | 347 | ||
| SST | Preop | 4.3 ± 3.0 | 3.6 ± 2.6 | .012 |
| Last postop | 10.9 ± 5.5 | 10.0 ± 2.5 | .022 | |
| Delta | 6.9 ± 7.5 | 7.0 ± 3.5 | .945 | |
| CONSTANT | Preop | 43 ± 16 | 38 ± 14 | .003 |
| Last postop | 74 ± 16 | 69 ± 15 | .445 | |
| Delta | 32 ± 19 | 31 ± 16 | .620 | |
| ASES | Preop | 37 ± 15 | 36 ± 14 | .581 |
| Last postop | 83 ± 20 | 82 ± 19 | .445 | |
| Delta | 46 ± 23 | 45 ± 22 | .507 | |
| UCLA | Preop | 14 ± 4 | 13 ± 4 | <.001 |
| Last postop | 30 ± 6 | 30 ± 5 | .594 | |
| Delta | 16 ± 7 | 17 ± 6 | .486 | |
| SPADI | Preop | 79 ± 21 | 82 ± 21 | .100 |
| Last postop | 19 ± 25 | 22 ± 24 | .154 | |
| Delta | −60 ± 29 | −59 ± 29 | .781 |
VAS, visual analog scale; SST, Simple Shoulder Test; CONSTANT, Constant-Murley score; ASES, American Shoulder and Elbow Surgeons assessment; UCLA, University of California Los Angeles Shoulder score; SPADI, Shoulder Pain and Disability Index; ATSA, anatomic total shoulder arthroplasty; RTSA, reverse total shoulder arthroplasty.
Last postop is the postoperative score collected at the last postoperative visit. Delta is the difference in the preoperative score to the last postoperative score.
The ATSA patients had significantly greater improvements in all ROM measurements over RTSA. Although the RTSA improvement of max shoulder strength was significantly greater than ATSA, the postoperative value was still smaller. No differences were noted in improvement for the patient-reported outcome measures (SST, CONSTANT, ASES, UCLA, and SPADI).
Although increased complications and associated revisions in the ATSA cohort at midterm follow-up resulted in a lower mean survivorship compared with RTSA, it was not statistically significant (ATSA = 96.0%, RTSA = 97.3%, P = .392). The overall rates of complication (excluding notching) between the ATSA and RTSA groups were similar (6.3% vs. 5.3%, P = .414). The most common complications for RTSA were acromial/scapula fractures and aseptic glenoid loosening, whereas the most common complications for ATSA were aseptic glenoid loosening and rotator cuff tear/subscapularis repair failure, as shown in Table III. When analyzing the rate of revision relative to orthopedic-related complications for both ATSA and RTSA, we identified that the odds ratio for revision for RTSA relative to ATSA is 0.367 (95% confidence interval [CI] = 0.10-1.28, P = .109). This implied that complications were more often revisions in the ATSA group, but the difference was not statistically significant.
Table III.
Postoperative complications, revisions, and survivorship
| Complications | Anatomic (ATSA), number (%) | Reverse (RTSA), number (%) | P value |
|---|---|---|---|
| Acromial/scapular fracture | 0 (0) | 6 (1.2) | .091 |
| Humeral fracture | 0 (0) | 3 (0.6) | .302 |
| Clavicle fracture | 0 (0) | 1 (0.2) | 1.000 |
| Aseptic glenoid loosening | 6 (2.1) | 5 (1.0) | .137 |
| Aseptic humeral loosening | 1 (0.3) | 0 (0) | .368 |
| Rotator cuff tear/subscapularis repair failure | 7 (2.4) | 0 (0) | .001 |
| Instability/dislocation | 2 (0.7) | 2 (0.4) | .628 |
| Total orthopedic-related complications | 18 (6.3)∗ | 26 (5.3)† | .557 |
| Scapular notching | NA | 27 (5.5) | NA |
| Revisions | 12 (4.2) | 11 (2.2) | .129 |
| Survivorship | |||
| 2 yr [95% CI] | 98.5% [97.0-100.0] | 98.7% [97.7-99.7] | .392 |
| 5 yr [95% CI] | 96.0% [93.3-98.6] | 97.3% [95.7-99.0] | |
| 8 yr [95% CI] | 96.0% [93.3-98.6] | 97.3% [95.7-99.0] | |
CI, confidence interval; ATSA, anatomic total shoulder arthroplasty; RTSA, reverse total shoulder arthroplasty.
Other ATSA complications include pain (2).
Other RTSA complications include pain (5), infection (2), stiffness (1), and hematoma (1).
Survivorship for ATSA was similar to that for RTSA at all time points (Fig. 1). At 2 years, survivorship for ATSA was 98.5% (95% CI = 97-100) compared with 98.7% (95% CI = 97.7-99.7) for RTSA. Survivorship remained similar at 8 years for both ATSA (96.0%, 95% CI = 93.3-98.6) and RTSA (97.3%, 95% CI = 95.7-99.0). When comparing the 3 participating surgeons individually, survivorship remained similar at all time points, as shown in Table IV, suggesting good generalizability of outcomes at each clinical site in the 3 different countries analyzed in this study.
Figure 1.
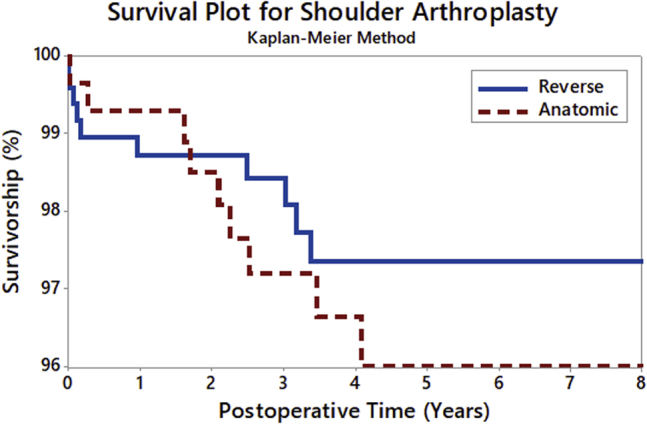
Kaplan-Meier survivorship curve for anatomic total shoulder arthroplasty and reverse total shoulder arthroplasty.
Table IV.
Survivorship calculations for each geographical area of sites
| Cohort | US site |
UK site |
EU site |
|||
|---|---|---|---|---|---|---|
| ATSA (N = 107) | RTSA (N = 161) | ATSA (N = 84) | RTSA (N = 77) | ATSA (N = 95) | RTSA (N = 254) | |
| Survivorship | ||||||
| Year 2 | 98.8 | 99.2 | 98.8 | 95.9 | 97.8 | 99.2 |
| Year 5 | 97.4 | 98.2 | 97.6 | 95.9 | 93.1 | 97.3 |
| Year 8 | 97.4 | 98.2 | 97.6 | 95.9 | 93.1 | 97.3 |
ATSA, anatomic total shoulder arthroplasty; RTSA, reverse total shoulder arthroplasty.
Discussion
As RTSA continues to gain popularity with an expansion of viable indications, it is important for surgeons to understand the performance and complication profile of the RTSA prosthesis relative to ATSA. On the basis of this cohort comparison, both ATSA and RTSA demonstrated similar survivorship at 8 years after surgery with multiple surgeons practicing in different countries. Both operations also performed similarly regarding patient-reported outcome measures, patient satisfaction ranking, complication, and revision rates. Considering the differences in indications, our results demonstrate that the RTSA and ATSA implants have comparable results with this platform shoulder system.
Although not significantly different, we observed that RTSA patients had a lower mean revision rate than ATSA patients at similar follow-up (RTSA = 2.2%, ATSA = 4.2%, P = .129). This finding is similar to the results reported by Wright et al,39 who compared 102 ATSA and 33 RTSA and reported a reoperation rate of 6.9% for ATSA compared with a 3.0% rate for RTSA patients. In addition, Kiet et al18 also found a slightly higher reoperation rate for ATSA patients (11%) than RTSA patients (9%) at 2-year follow-up. Smith et al33 asserted that with modern implants, the rate of complications and revisions for RTSA are now similar to those for ATSA. Continued follow-up is necessary to determine if differences in revision rate between ATSA and RTSA patients will be maintained in the long term, especially because rotator cuff disease likely progresses with age.17 Thus, long-term survivorship studies are needed to assess the effect of rotator cuff disease progression on ATSA.
Despite differences in the revision rate, both implant configurations performed similarly when assessed using a Kaplan-Meir survivorship analysis. The performance of both ATSA and RTSA was similar amongst study sites location, indicating that the results can be generalized across geographic locations and between surgeons. Although cultural and governmental differences exist between each of the sites, similar surgical techniques and study protocol were followed.
Clinically, ATSA demonstrated superior ROM compared with RTSA patients. Specifically, greater postoperative active abduction, active forward elevation, and active external rotation measures were observed after ATSA. When evaluating improvements in ROM from preoperatively to postoperatively, ATSA outperformed RTSA for all ROM measures in a statistically significant manner. This finding is consistent with other studies comparing ROM between RTSA and ATSA.35 However, the findings can be interpreted differently when analyzed according to whether or not the differences between ATSA and RTSA meet the thresholds for minimal clinically important difference (MCID) or substantial clinical benefit (SCB) as previously reported by Simovitch et al.30,31 The difference in improvement for active abduction between ATSA and RTSA exceeded MCID but did not meet the threshold for SCB. The difference in improvement for active forward elevation between ATSA and RTSA did not meet the threshold for MCID or SCB. The difference in improvement for active external rotation between ATSA and RTSA exceeded both MCID and SCB thresholds. In addition to ROM, our results demonstrated that ATSA patients were associated with greater max strength and shoulder function postoperatively than RTSA patients. The significant difference is likely secondary to the preoperative diagnosis of cuff tear arthropathy and patients treated with RTSA having significantly lower preoperative max strength and shoulder function. In addition, this significant difference might be an artifact of the demographic differences (gender and age) between the groups.
Our study has limitations, primarily related to the study design. Of particular note, this is an industry-funded study, including a sponsor-funded registry and results analyzed by sponsor statisticians. Although the sample size is large and the participating surgeons are highly experienced in using this shoulder implant, the ATSA study population remains different than the RTSA study population (Table I). We anticipate that the different patient populations are a major study limitation; although ATSA and RTSA are specific to different diagnoses, a more accurate comparison of ATSA and RTSA would be for patients only with osteoarthritis. These patient differences (age, gender ratios, height, weight, and preoperative diagnoses) could impact the postoperative measures. Specifically, the lower rate of revision for the RTSA patient cohort might be biased because of their older age as older patients may be less likely to choose to undergo revision surgery due to increased risks of doing so. Furthermore, the RTSA cohort has a much higher rate of rotator cuff insufficiency compared with the ATSA cohort, which might impact the ROM differences seen independent of implant type.5 A second limitation of the study is the lack of preoperative radiographic status, because the glenoid type could also impact postoperative outcomes. A third potential limitation of this study is that the comparison of the rate of revision may be biased because of the platform nature of the shoulder system used, which facilitates revision of an ATSA to an RTSA (most commonly) without humeral stem removal.1 Surgeons may have been more inclined to revise an ATSA due to ease in doing so because of the ability to retain the stem, whereas they may have been more disinclined to revise an RTSA as the outcomes of RTSA revisions are generally less predictable.1,25,36 This may be illustrated by our finding that 67% of ATSA patients with an orthopedic-related complication, as defined, underwent a revision, whereas only 42% of RTSA patients with an orthopedic-related complication, as defined, underwent a revision surgery. Therefore, surgeon-patient considerations and requirements that lead to ATSA revisions may be different than RTSA revisions.9
Conclusion
Our results indicate that both ATSA and RTSA can be expected to provide similar implant longevity over the midterm with excellent functional outcomes. ATSA patients can expect greater postoperative ROM and max strength compared with RTSA patients.
Based on these results, surgeons should feel confident indicating a patient for the appropriate polarity of shoulder arthroplasty based on their clinical judgment without concerns for survivorship at 8-year follow-up.
Acknowledgments
We would like to thank Eric Rohrs and Wen Fan, both contracted by the sponsor, for their assistance with the statistical analysis.
Disclaimer
This study was funded by Exactech.
Pierre Henri Flurin, Thomas Wright, and Joseph Zuckerman receive royalties on products discussed in this document. Pierre Henri Flurin, Ryan W. Simovitch, and Bradley S. Schoch Receives royalties from Exactech products not discussed in this article. Carl Tams and Christopher Roche are employees of Exactech.
Christopher Knudsen, his immediate family, and any research foundations with which he is affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Approval for this study was received from WIRB (#20091701).
References
- 1.Abdel M.P., Hattrup S.J., Sperling J.W., Cofield R.H., Kreofsky C.R., Sanchez-Sotelo J. Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J. 2013;95-B:668–672. doi: 10.1302/0301-620X.95B5.30964. [DOI] [PubMed] [Google Scholar]
- 2.Alta T.D., de Toledo J.M., Veeger H.E., Janssen T.W., Willems W.J. The active and passive kinematic difference between primary reverse and total shoulder prostheses. J Shoulder Elbow Surg. 2014;23:1395–1402. doi: 10.1016/j.jse.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz H.C., Sew Hoy A.L., Clarke I.C. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981:7–20. [PubMed] [Google Scholar]
- 4.Bohsali K.I., Bois A.J., Wirth M.A. Complications of shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:256–269. doi: 10.2106/JBJS.16.00935. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016;102:S33–S43. doi: 10.1016/j.otsr.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 6.Braun B.J., Holstein J., Fritz T., Veith N.T., Herath S., Mörsdorf P. Polytrauma in the elderly: a review. EFORT Open Rev. 2016;1:146–151. doi: 10.1302/2058-5241.1.160002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–164. [PubMed] [Google Scholar]
- 8.Cox R.M., Padegimas E.M., Abboud J.A., Getz C.L., Lazarus M.D., Ramsey M.L. Outcomes of an anatomic total shoulder arthroplasty with a contralateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:998–1003. doi: 10.1016/j.jse.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Crosby L.A., Wright T.W., Yu S., Zuckerman J.D. Conversion to reverse total shoulder arthroplasty with and without humeral stem retention: the role of a convertible-platform stem. J Bone Joint Surg Am. 2017;99:736–742. doi: 10.2106/JBJS.16.00683. [DOI] [PubMed] [Google Scholar]
- 10.Dillon M.T., Ake C.F., Burke M.F., Singh A., Yian E.H., Paxton E.W. The Kaiser Permanente shoulder arthroplasty registry: results from 6,336 primary shoulder arthroplasties. Acta Orthop. 2015;86:286–292. doi: 10.3109/17453674.2015.1024565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donohue K.W., Ricchetti E.T., Iannotti J.P. Surgical management of the biconcave (B2) glenoid. Curr Rev Musculoskelet Med. 2016;9:30–39. doi: 10.1007/s12178-016-9315-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fevang B.T., Lie S.A., Havelin L.I., Skredderstuen A., Furnes O. Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop. 2009;80:83–91. doi: 10.1080/17453670902805098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox T.J., Cil A., Sperling J.W., Sanchez-Sotelo J., Schleck C.D., Cofield R.H. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:859–863. doi: 10.1016/j.jse.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Flurin P.H., Marczuk Y., Janout M., Wright T.W., Zuckerman J., Roche C.P. Comparison of outcomes using anatomic and reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013) 2013;71(Suppl 2):101–107. [PubMed] [Google Scholar]
- 15.Gowd A.K., Garcia G.H., Liu J.N., Malaret M.R., Cabarcas B.C., Romeo A.A. Comparative analysis of work-related outcomes in hemiarthroplasty with concentric glenoid reaming and total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:244–251. doi: 10.1016/j.jse.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 16.Hartzler R.U., Steen B.M., Hussey M.M., Cusick M.C., Cottrell B.J., Clark R.E. Reverse shoulder arthroplasty for massive rotator cuff tear: risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24:1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 17.Keener J.D., Galatz L.M., Teefey S.A., Middleton W.D., Steger-May K., Stobbs-Cucchi G. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015;97:89. doi: 10.2106/JBJS.N.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiet T.K., Feeley B.T., Naimark M., Gajiu T., Hall S.L., Chung T.T. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:179–185. doi: 10.1016/j.jse.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 19.Latif V., Denard P.J., Young A.A., Liotard J.P., Walch G. Bilateral anatomic total shoulder arthroplasty versus reverse shoulder arthroplasty. Orthopedics. 2012;35:e479–e485. doi: 10.3928/01477447-20120327-25. [DOI] [PubMed] [Google Scholar]
- 20.Lazarus M.D., Jensen K.L., Southworth C., Matsen F.A., III The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84:1174–1182. doi: 10.2106/00004623-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Lippitt S.B., Harryman D.T., Matsen F.A. A practical tool for evaluating function: the Simple Shoulder Test. In: Matsen F.A., Fu F.H., Hawkins R.J., editors. The shoulder: a balance of mobility and stability. American Academy of Orthopaedic Surgeons; Rosemont, IL: 1992. pp. 501–518. [Google Scholar]
- 22.Mahony G.T., Werner B.C., Chang B., Grawe B.M., Taylor S.A., Craig E.V. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2018;27:968–975. doi: 10.1016/j.jse.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 23.Matsen F.A., III, Boileau P., Walch G., Gerber C., Bicknell R.T. The reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89:660–667. doi: 10.2106/00004623-200703000-00027. [DOI] [PubMed] [Google Scholar]
- 24.McLendon P.B., Schoch B.S., Sperling J.W., Sánchez-Sotelo J., Schleck C.D., Cofield R.H. Survival of the pegged glenoid component in shoulder arthroplasty: part II. J Shoulder Elbow Surg. 2017;26:1469–1476. doi: 10.1016/j.jse.2016.12.068. [DOI] [PubMed] [Google Scholar]
- 25.Melis B., Bonnevialle N., Neyton L., Lévigne C., Favard L., Walch G. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21:342–349. doi: 10.1016/j.jse.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 26.Richards R.R., An K.N., Bigliani L.U., Friedman R.J., Gartsman G.M., Gristina A.G. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 27.Roach K.E., Budiman-Mak E., Songsiridej N., Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4:143–149. [PubMed] [Google Scholar]
- 28.Sanchez-Sotelo J., O'Driscoll S.W., Torchia M.E., Cofield R.H., Rowland C.M. Radiographic assessment of cemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10:526–531. doi: 10.1067/mse.2001.118482. [DOI] [PubMed] [Google Scholar]
- 29.Schoch B., Werthel J.D., Schleck C.D., Harmsen W.S., Sperling J., Sánchez-Sotelo J. Optimizing follow-up after anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:997–1002. doi: 10.1016/j.jse.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 30.Simovitch R., Flurin P.H., Wright T., Zuckerman J.D., Roche C.P. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg. 2018;27:298–305. doi: 10.1016/j.jse.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 31.Simovitch R., Flurin P.H., Wright T., Zuckerman J.D., Roche C.P. Quantifying success after total shoulder arthroplasty: the substantial clinical benefit. J Shoulder Elbow Surg. 2018;27:903–911. doi: 10.1016/j.jse.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 32.Sirveaux F., Favard L., Oudet D., Huquet D., Walch G., Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 33.Smith C.D., Guyver P., Bunker T.D. Indications for reverse shoulder replacement: a systematic review. J Bone Joint Surg Br. 2012;94:577–583. doi: 10.1302/0301-620X.94B5.27596. [DOI] [PubMed] [Google Scholar]
- 34.Smithers C.J., Young A.A., Walch G. Reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2011;4:183. doi: 10.1007/s12178-011-9097-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Triplet J.J., Everding N.G., Levy J.C., Moor M.A. Functional internal rotation after shoulder arthroplasty: a comparison of anatomic and reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:867–874. doi: 10.1016/j.jse.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Wagner E.R., Hevesi M., Houdek M.T., Cofield R.H., Sperling J.W., Sanchez-Sotelo J. Can a reverse shoulder arthroplasty be used to revise a failed primary reverse shoulder arthroplasty? Revision reverse shoulder arthroplasty for failed reverse prosthesis. Bone Joint J. 2018;100:1493–1498. doi: 10.1302/0301-620X.100B11.BJJ-2018-0226.R2. [DOI] [PubMed] [Google Scholar]
- 37.Walch G., Young A.A., Boileau P., Loew M., Gazielly D., Molé D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94:145–150. doi: 10.2106/JBJS.J.00699. [DOI] [PubMed] [Google Scholar]
- 38.Wall B., Nové-Josserand L., O'Connor D.P., Edwards T.B., Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 39.Wright M.A., Keener J.D., Chamberlain A.M. Comparison of clinical outcomes after anatomic total shoulder arthroplasty and reverse shoulder arthroplasty in patients 70 years and older with glenohumeral osteoarthritis and an intact rotator cuff. J Am Acad Orthop Surg. 2020;28:e222–e229. doi: 10.5435/JAAOS-D-19-00166. [DOI] [PubMed] [Google Scholar]
- 40.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–147. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]


