Abstract
Background
Various surgical strategies have been used for the treatment of sternoclavicular joint instability with variable results. The purpose of this study was to report the clinical results of patients who underwent single-loop allograft reconstruction for sternoclavicular joint instability.
Methods
A total of 10 patients underwent single-loop allograft reconstruction for sternoclavicular joint instability from June 2012 to August 2014 by a single surgeon. All patients had a history of instability of the sternoclavicular joint with persistent chronic subluxation of the joint, magnetic resonance imaging disruption of the sternoclavicular ligaments, and persistent symptoms of pain and instability. Regarding the surgical technique, a single 5.5 mm drill hole was placed in the sternum and a second was placed in the medial aspect of the clavicle. A semitendinosus hamstring allograft was looped between the 2 holes and then tied in a square knot anteriorly. A #5 high-strength suture was used as cerclage as well. Nine of 10 patients (90% follow-up) were available at an average of 3.3 ± 0.84 years postoperatively. The average age of patients at the time of surgery was 42 years (range, 20-73 years). Patients were evaluated postoperatively with outcome scores (visual analog scale pain, American Shoulder and Elbow Surgeons, Simple Shoulder Test), a question regarding tenderness at the sternoclavicular joint, and a question regarding residual instability and overall patient satisfaction (yes/no).
Results
The average functional outcome scores for the Simple Shoulder Test, visual analog scale pain, and American Shoulder and Elbow Surgeons score were 11.8, 0.9, and 94.8, respectively. Three of 9 patients reported some residual tenderness located to the sternoclavicular joint. No patients reported any residual instability of the sternoclavicular joint. Eight of 9 patients reported that they were satisfied with the procedure. No patients required reoperation, and there were no complications.
Conclusion
Single-loop allograft reconstruction of the sternoclavicular joint provides reliable pain relief, functional improvement, and joint stability for patients with chronic sternoclavicular joint instability. The simplicity of the procedure eliminates the need for small, multiple drill holes that may lead to fracture between tunnels or the use of a small, thin graft.
Keywords: Allograft, sternoclavicular joint instability, functional outcomes, reconstruction, clavicle, loop
Sternoclavicular joint (SCJ) dislocations are uncommon and account for only 2%-3% of all dislocations of the shoulder girdle.2 Most dislocations occur anteriorly, whereas only 5%-27% occur in a posterior direction.5 Anterior dislocations often do not require any acute treatment, whereas posterior dislocations will require either closed reduction or surgical stabilization due to the proximity of vital structures posterior to the sternum.3 A thoracic surgeon should be available during the reduction if attempted. In the setting of persistent anterior or posterior sternoclavicular instability, a variety of methods have been described for reconstruction including local soft tissue repair or augmentation with synthetic material, ligament reconstruction with an autograft or allograft, or tendon transfer.5 A majority of ligament reconstruction techniques report the use of an autograft tendon and a modification of a figure-of-eight construct.4,6,7,10 There are few prior reports of the results of allograft reconstructions or constructs using a simpler reconstruction pattern like a simple loop.7, 8, 9
A variety of ligament reconstruction techniques have been described, but a strong emphasis has been placed on using a figure-of-eight construct because of its biomechanical properties.1,6,9,11 Spencer et al11 compared a figure-of-eight reconstruction technique using a tendon graft with both an intramedullary ligament reconstruction and a subclavius tendon transfer in a cadaveric model. The figure-of-eight fashion was found to be superior to both intramedullary ligament reconstruction and subclavius tendon reconstruction with significantly greater load to failure (anteroposterior) in the figure-of-eight reconstruction compared with the other techniques. No other ligament reconstruction techniques were reported. Long-term clinical outcomes of this surgical technique using an autograft have been reported with 90% survivorship at 5 years with excellent return to sport and a low complication rate.6 Limitations of this technique include the requirement for 4 smaller drill holes (2 in the clavicle and 2 in the sternum) that may be challenging especially in smaller patients or with compromised bone stock. Also, an autograft requires a separate incision and potentially increased morbidity. A simple loop reconstruction using an allograft may be an easier, less morbid technique especially in cases of smaller patients or limited bone stock.
The purpose of this study was to retrospectively review a series of patients who underwent single-loop allograft reconstruction for sternoclavicular instability treated by a single surgeon. Functional outcomes, symptoms of residual instability, complications, and reoperations were collected. Our hypothesis was that single-loop allograft reconstruction would result in excellent outcomes and a low complication rate.
Methods
The operative logs of the senior surgeon (R.Z.T.) were reviewed for all patients who underwent an SCJ reconstruction over a 5-year period from June 2012 to June 2017. Inclusion criteria included any primary SCJ reconstruction using a single-loop technique between the medial clavicle and the sternum using an allograft tendon. Exclusion criteria included any patient who underwent a revision procedure, if the reconstruction extended to the first rib, if an autograft was used, or if the patients had less than a minimum of 2-year follow-up. Overall, there were 2 patients who had a reconstruction extending to the first rib due to extreme hypermobility of the medial clavicle. One patient underwent a revision of a prior sternoclavicular reconstruction, and a hamstring autograft was used in this case.
The included patients were initially contacted by mail and then followed up by a phone call 2 weeks later for recruitment. Patients completed questionnaires online using REDCap questionnaires (Vanderbilt University—[8UL1TR000105 (formerly UL1RR025764) NCATS/NIH]). REDCap is a secure, internationally implemented research collection electronic data capture program created by Vanderbilt University and used extensively in postsurgical studies at the University of Utah. Questionnaires included the Simple Shoulder Test, the American Shoulder and Elbow Surgeons (ASES) score, and a visual analog scale for pain. Patients were asked a yes/no question if they were satisfied with the surgery along with a yes/no question if they had any tenderness at the SCJ. Patients were also asked to complete an online assessment of their range of motion (abduction, forward flexion, external rotation in abduction, external rotation at the side, internal rotation at the side) that has been previously published for assessment of range of motion after shoulder arthroplasty.12 Only patients with greater than a minimum of 2-year follow-up were included.
Surgical technique
The loop allograft reconstruction used 1 tunnel in the clavicle and 1 tunnel in the sternum with an allograft hamstring tendon graft and suture cerclage (Fig. 1). All surgical reconstructions were performed in the supine position under general anesthesia. A thoracic surgeon was present for the entire procedure and assisted throughout the procedures especially with exposure posterior to the clavicle and sternum. A hockey stick incision is made over the SCJ approximately 6 cm in length (Fig. 2). The subcutaneous tissues are dissected down to the joint. The sternal head of the sternocleidomastoid was protected and not released. The clavicular attachment of the sternocleidomastoid along with the pectoralis and the anterior and posterior sternoclavicular ligaments were circumferentially dissected from the medial clavicle. Care was taken to not extend the dissection laterally more than 2 cm to avoid disruption of the costoclavicular ligaments if still intact. The intra-articular disc was removed, and the exposure of the anterior and posterior aspects of the medial clavicle and the sternum was performed. A single 5.5 mm drill hole was then placed 1.5 cm from the joint on both the sternal and clavicular side going through both the anterior and posterior cortexes protecting vital structures posteriorly during drilling (Fig. 3). During drilling of the sternum, the thoracic surgeon placed an army-navy retractor under the sternum displacing the vascular structures posteriorly allowing drilling into the retractor. A 6 mm semitendinosus hamstring allograft tendon was then passed from anterior to posterior through the sternal tunnel and then back up from posterior to anterior through the clavicular tunnel (Figs. 4 and 5). Two #5 high-strength sutures (Fiberwire; Arthrex, Naples, FL, USA) were also passed with the graft separately, which would be used as an internal brace during graft healing. The clavicle was then reduced to the sternum, and the high-strength sutures were tied and then the graft was tied in a square knot (Figs. 6 and 7). No. 2 high-strength figure-of-eight stitches were passed in each throw of the square knot to improve the strength of the construct. The muscular flaps were then closed over the construct using a #2 high-strength suture. Patients were treated with an abduction sling for 6 weeks during which no shoulder therapy was performed. At 6 weeks postoperatively, 10 pounds of lifting was allowed with no active elevation above shoulder height. At 3 months postoperatively, formalized physical therapy was initiated allowing range of motion active and passive in all directions; strengthening of the rotator cuff, deltoid, and scapular stabilizers; and 13.5 kg (30 lbs) of lifting. At 4.5 months postoperatively, up to 22.5 kg (50 lbs) of lifting was allowed. At 6 months postoperatively, patients were allowed to return to all activities without restriction.
Figure 1.
Sternoclavicular joint reconstruction using one 5.5 mm tunnel in the sternum and one tunnel in the medial clavicle with #5 Fiberwire (Arthrex) cerclage.
Figure 2.

Hockey stick incision over the sternoclavicular joint.
Figure 3.
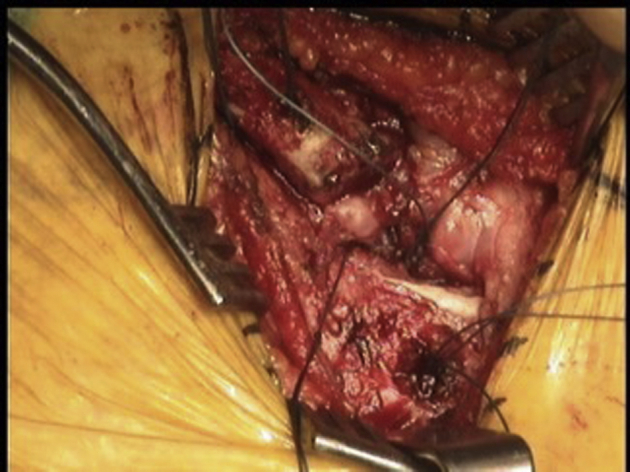
Two 5.5 mm tunnels created for loop reconstruction (1 in the sternum and 1 in the medial clavicle) with shuttling sutures placed.
Figure 4.
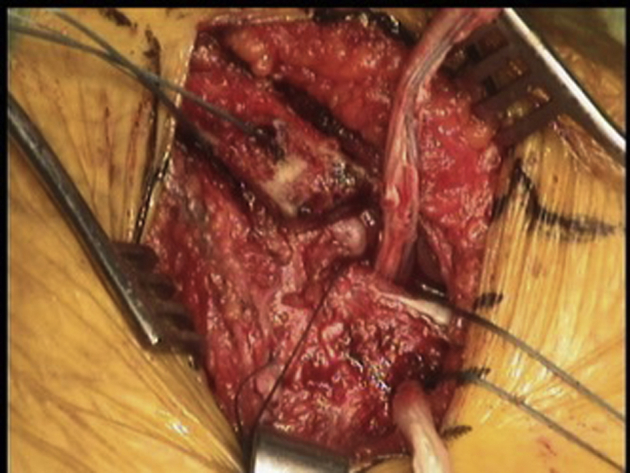
Semitendinosus hamstring allograft passed from anterior to posterior through the sternal tunnel.
Figure 5.

Posterior to anterior passage of the graft through the clavicular tunnel.
Figure 6.

Tying of the high-strength suture cerclages between the sternal and clavicular tunnels.
Figure 7.
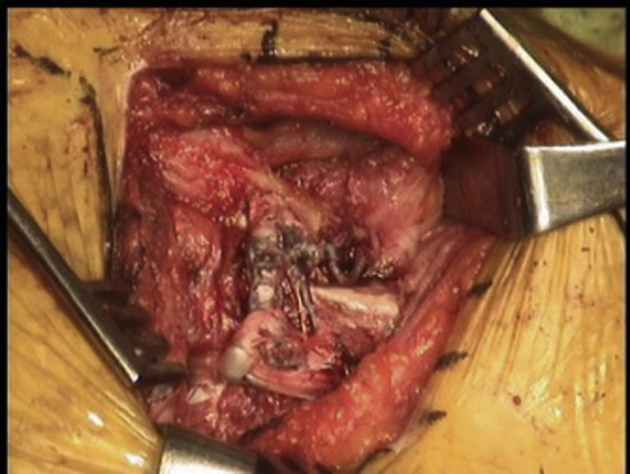
Final reconstruction after the graft tied in a square knot.
Results
Ten patients underwent single-loop allograft reconstruction during the study period, and 9 of 10 (90%) were available for a minimum of 2-year postoperative follow-up. Five of 10 patients had traumatic posterior instability that was closed reduced but had persistent symptoms of instability after reduction. Five of 10 patients had traumatic anterior instability with persistent symptoms of instability after nonoperative treatment. No patient had evidence of osteoarthritis of the SCJ on preoperative computed tomography scans of the chest. The average age of patients at the time of surgery was 42 years (range, 20-73 years). Outcomes were collected at an average of 3.3 ± 0.84 years postoperatively (range, 2.4-4.9 years). Surgeries were performed at an average of 41 ± 20 months (range, 21-74 months) from injury. There were 6 males and 3 females.
The average final postoperative functional outcome scores for the Simple Shoulder Test, visual analog scale pain, and ASES score were 11.8 ± 0.7, 0.9 ± 1.2, and 94.8 ± 6.9, respectively. Three of 9 patients reported some residual tenderness located to the SCJ. No patients reported any residual instability of the SCJ. Eight of 9 patients reported that they were satisfied with the procedure. No patients required reoperation, and there were no complications.
In terms of self-reported range of motion and strength, the average shoulder abduction, forward elevation, external rotation in 90° of abduction, and external rotation in adduction were 167° ± 16°, 163° ± 24°, 81° ± 15°, and 71° ± 11°, respectively. Four patients reported that they could internally rotate to their low back, 4 patients reported that they could internally rotate to their mid back, and 1 patient reported that he or she could internally rotate to his or her upper back. All patients stated that they could raise a quart of water to shoulder height in both abduction and forward flexion.
Discussion
SCJ reconstruction using a single-loop hamstring allograft reliably restores stability with a low complication rate. Functional outcomes based on shoulder-specific measures were extremely high and pain levels very low at mid-term follow-up. A minority of patients reported some tenderness, and there was a very high satisfaction rate with the procedure. Range of motion and weight bearing were comparable with normal shoulder function at final follow-up. The ASES score and visual analog scale pain scores are comparable with prior reports for autograft figure-of-eight reconstructions reported in the literature supporting single-loop allograft reconstruction is a reasonable alternative.6,7
Several authors have reported the clinical outcomes of sternoclavicular reconstruction using a graft. Singer et al10, 11 reported on 6 patients after autograft figure-of-eight reconstruction using the technique described by Spencer et al.10, 11 The authors reported on 6 patients and reported significant improvements in disabilities of the arm, shoulder and hand scores with all patients returning to activity and sport without restriction.10 Guan et al4 reported on a modification of the technique where only the anterior cortex of the clavicle and sternum were drilled and reported excellent results in 6 patients using autograft hamstring with an average disabilities of the arm, shoulder and hand score of 4.3. Petri et al7 reported on 19 patients who underwent reconstruction, with 16 of them having the figure-of-eight autograft technique. They did report that 3 patients had insufficient bone stock available for 2 holes in the clavicle; therefore, a single-loop autograft technique was used. The authors reported an average final ASES score of 82 and noted significantly worse ASES scores in patients who were not satisfied with the surgery (4 of 19 patients) although these 4 had other concomitant preoperative injuries as well.7 The same group followed up on a similar cohort of patients with a minimum of 5 years of follow-up and noted final ASES scores of 91 with low complication rates and high return to sport.6 Allograft reconstruction has been reported using a figure-of-eight construct in 1 series and reported comparable final ASES scores of 84 in 10 patients with no reconstruction failures.8 Comparing the current data using an allograft, the results are very similar to those reported in the literature for an autograft and similar to the Sabatini et al8 series using an allograft. Also, the single-loop construct did not appear to negatively impact the stability or functionality of the construct at final follow-up.
A single-loop reconstruction has multiple advantages over a figure-of-eight reconstruction. First, fewer holes must be drilled, and thus the risk for iatrogenic fracture is lower. Second, because fewer holes must be drilled, the risk of insufficient osseous space available for these holes is lower. Third, because fewer holes must be drilled, the neurovascular risk is lower. Fourth, if a revision is required, more native bone stock remains, allowing additional flexibility. Fifth, a larger caliber graft can be used. Sixth, a shorter graft can be used, which allows a wider variety of grafts to be used. Seventh, because the graft must make fewer turns, graft passage is easier and there is less opportunity for the graft to be abraded and compromised. As a result of all the advantages listed, the senior authors' preference is to use this technique in all cases instead of in just smaller patients although a smaller graft could be considered with smaller tunnels in these patients using a 4-tunnel technique as well. Potential disadvantages of the current technique are drill holes exiting the posterior sternal cortex placing vascular structures at risk, the need for a thoracic surgeon intraoperatively, a graft knot that may be bulky although does smooth out over time, and no biomechanical data supporting equivalence or superiority to a 4-tunnel technique.
There are several limitations to this study including a small sample size, no comparison cohort of patients, and no consistent preoperative functional outcome measures. Nevertheless, final outcomes and range of motion were reported using self-assessed questionnaires, and the outcomes are comparable with prior reports of constructs in the literature.
Conclusion
Single-loop allograft reconstruction of the SCJ provides reliable pain relief, functional improvement, and joint stability for patients with chronic SCJ instability. The simplicity of the procedure eliminates the need for small, multiple drill holes that may lead to fracture between tunnels or the use of a small, thin graft.
Disclaimer
Robert Z. Tashjian is a paid consultant for Zimmer/Biomet, Wright Medical, and Mitek; has stock in Conextions, INTRAFUSE, Genesis, and KATOR; receives intellectual property royalties from Wright Medical, Shoulder Innovations, and Zimmer/Biomet; receives publishing royalties from the Journal of Bone and Joint Surgery and Springer; and serves on the editorial board for the Journal of American Association of Orthopaedic Surgeons and Shoulder & Elbow.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was obtained from the University of Utah School of Medicine before initiating this study (IRB# 101394).
References
- 1.Bak K., Fogh K. Reconstruction of the chronic anterior unstable sternoclavicular joint using a tendon autograft: medium-term to long-term follow-up results. J Shoulder Elbow Surg. 2014;23:245–250. doi: 10.1016/j.jse.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Dennis M.G., Kummer F.J., Zuckerman J.D. Dislocations of the sternoclavicular joint. Bull Hosp Jt Dis. 2000;59:153–157. [PubMed] [Google Scholar]
- 3.Groh G.I., Wirth M.A., Rockwood C.A., Jr. Treatment of traumatic posterior sternoclavicular dislocations. J Shoulder Elbow Surg. 2011;20:107–113. doi: 10.1016/j.jse.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Guan J.J., Wolf B.R. Reconstruction for anterior sternoclavicular joint dislocation and instability. J Shoulder Elbow Surg. 2013;22:775–781. doi: 10.1016/j.jse.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Kendal J.K., Thomas K., Lo I.K.Y., Bois A.J. Clinical outcomes and complications following surgical management of traumatic posterior sternoclavicular joint dislocations: a systematic review. JBJS Rev. 2018;6:e2. doi: 10.2106/JBJS.RVW.17.00157. [DOI] [PubMed] [Google Scholar]
- 6.Lacheta L., Dekker T.J., Goldenberg B.T., Horan M.P., Rosenberg S.I., Pogorzelski J. Minimum 5-year clinical outcomes, survivorship, and return to sports after hamstring tendon autograft reconstruction for sternoclavicularjoint instability. Am J Sports Med. 2020;48:939–946. doi: 10.1177/0363546519900896. [DOI] [PubMed] [Google Scholar]
- 7.Petri M., Greenspoon J.A., Horan M.P., Martetschläger F., Warth R.J., Millett P.J. Clinical outcomes after autograft reconstruction for sternoclavicular joint instability. J Shoulder Elbow Surg. 2016;25:435–441. doi: 10.1016/j.jse.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Sabatini J.B., Shung J.R., Clay T.B., Oladeji L.O., Minnich D.J., Ponce B.A. Outcomes of augmented allograft figure-of-eight sternoclavicular joint reconstruction. J Shoulder Elbow Surg. 2015;24:902–907. doi: 10.1016/j.jse.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Sanchez-Sotelo J., Baghdadi Y., Nguyen N.T.V. Sternoclavicular joint allograft reconstruction using the sternal docking technique. JSES Open Access. 2018;2:190–193. doi: 10.1016/j.jses.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singer G., Ferlic P., Kraus T., Eberl R. Reconstruction of the sternoclavicular joint in active patients with the figure-of-eight technique using hamstrings. J Shoulder Elbow Surg. 2013;22:64–69. doi: 10.1016/j.jse.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Spencer E.E., Jr., Kuhn J.E. Biomechanical analysis of reconstructions for sternoclavicular joint instability. J Bone Joint Surg Am. 2004;86:98–105. doi: 10.2106/00004623-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Yang J.S., Keener J.D., Yamaguchi K., Chen J., Stobbs-Cucchi G., Patton R. Reliability of patient self-assessment of shoulder range of motion and strength after shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:1–10. doi: 10.1016/j.jse.2014.08.025. [DOI] [PubMed] [Google Scholar]



