Abstract
Background
The Latarjet and bone block procedures can be secured with screws or cortical buttons. The purpose of this biomechanical study was to compare quadruple buttons vs. double screws for fixation of anterior glenoid bone grafts.
Methods
Twelve cadaveric scapulae (6 pairs) were denuded, resected, and potted. Pairs were randomized to quadruple-button or double-screw fixation after creation of a 15% anterior glenoid defect. The specimens underwent cyclic uniaxial compressive glenoid loading between 50 and 200 N for 1000 cycles at 1 Hz. Testing was repeated for conjoint tendon loads of 0 N (simulating a bone block procedure), 10 N, and 20 N (simulating a Latarjet procedure). Peak resultant relative coracoid graft displacement was optically tracked at 3 points (superior, central, and inferior) on the edge of the coracoid.
Results
No significant differences were found between buttons and screws for bone block applications or with 10 N of conjoint tendon loading (P ≥ .095). At 20 N of conjoint tendon loading, however, the screws were significantly more stable than the buttons (P ≤ .023). During the initial 20-N conjoint load application, all 3 points displaced significantly more with the button reconstruction than with the screws (P ≤ .01). Overall, mean displacements did not exceed 1 mm at any position on the coracoid, regardless of testing condition.
Conclusions
The quadruple-button technique is comparable to screws when the coracoid is used as a bone block or when conjoint tendon loading is minimized. However, at higher conjoint tendon loads, the screws produced a more stable coracoid graft than the buttons.
Keywords: Latarjet, bone block, button, shoulder, coracoid, bone graft, EndoButton
The Latarjet procedure, first proposed by Michel Latarjet28 in 1954, has been commonly used to address shoulder instability, especially when associated with anterior glenoid bone loss.3,4,7,14,36,38,39,42,43 This procedure involves resection and transfer of the coracoid–conjoint tendon construct to the deficient anterior aspect of the glenoid. While joint stability is improved by reconstructing the anterior bone defect with the coracoid, further support is provided by the conjoint tendon, which creates a dynamic sling effect.19,28,34,43 The Latarjet procedure has generally been reported to have good outcomes, with high rates of patient satisfaction, low rates of recurrent instability, and high rates of return to preinjury sports performance levels.1,5,6,14,17,22,32,42
Recently, techniques have been developed to conduct the Latarjet procedure arthroscopically.9,12,13,26,27,33,40 However, Boileau et al10 (2016) have identified several drawbacks to arthroscopic procedures. The first is the technical challenge posed when attempting to surgically place screws parallel to the glenoid surface. Improper screw placement can lead to rapid-onset humeral head arthropathy from screw impingement32,38,42,46 or complications from graft malpositioning.22,32,42,46 Screw fixation issues1,32,42,44 can also present as coracoid fracture, screw pullout or loosening, resorption (3%-28%), and graft migration (4%-11%)1,2,42 and may be serious enough to warrant reoperation.13,15,39,46,47 Additionally, there is a risk of nerve injury owing to the proximity of drilling lines of action and screw insertion to the brachial plexus,11,12,18,46,47 as well as to the suprascapular nerve if screws protrude too medially on the posterior side.25,29,31 To avoid issues surrounding the aforementioned screw-related complications, a quadruple-button construct has been proposed as an alternative to screw-based fixation for the arthroscopic Latarjet procedure.10,21,40 The quadruple-button construct relies on a tensioned suture running between 2 bone-adjacent buttons to secure the coracoid graft to the glenoid (Fig. 1). In addition to Latarjet fixation, screws and cortical buttons can be used to secure bone block procedures such as iliac crest and distal clavicle autograft, as well as distal tibial allograft.
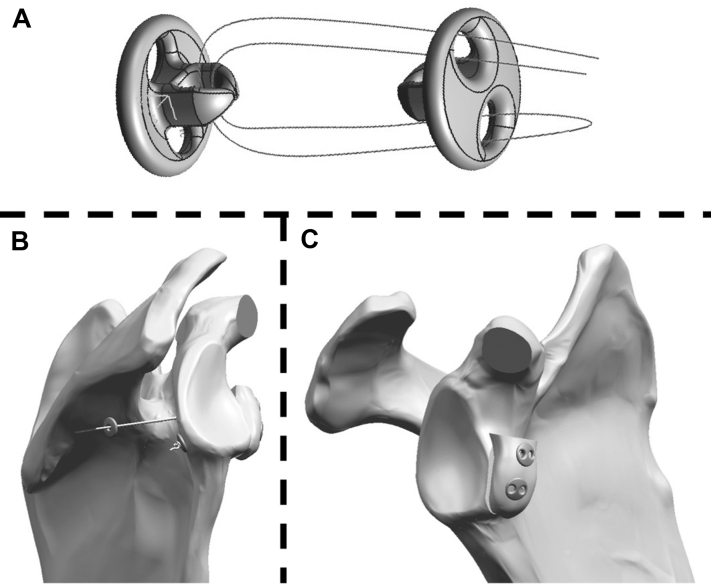
Figure 1.
Quadruple-button coracoid fixation construct (A), in which 2 cortical buttons are threaded together by a No. 3-4 suture, and posterior (B) and anterior (C) views of coracoid-scapula assembly.
The purpose of this in vitro biomechanical study was to compare the traditional double-screw technique with the quadruple-button fixation technique for simulated anterior glenoid bone block and Latarjet procedures in terms of graft displacement. It was hypothesized that coracoid graft displacement would not present as significantly different, regardless of which technique was used.
Methods
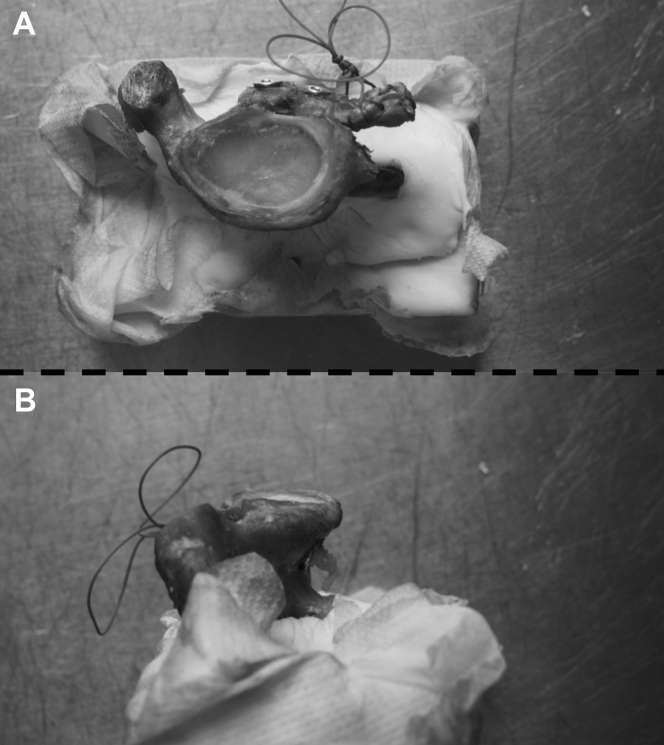
Twelve cadaveric shoulders (6 pairs; 5 men and 1 woman; age, 74 ± 3 years) were denuded, with the exception of the conjoint tendon origin on the coracoid. Each scapula was resected approximately 8 cm medial to the glenoid surface and was potted in bone cement with the glenoid articular surface parallel to the potting apparatus (ie, horizontal, as determined using a bubble level) (Fig. 2). A 15% anterior glenoid bone defect was then created. The 15% defect size was chosen to represent a clinically relevant injury size20,23,35 and was constructed in a repeatable manner as a percentage of the glenoid dish width. Right and left specimens were then randomized into groups: quadruple-button or double-screw reconstruction. The quadruple-button technique involved 2 suture fixation devices with No. 3-4 sutures tensioning cortical buttons, secured with a Nice knot,8 tensioned to 100 N using a commercially available tension device (Smith & Nephew, Andover, MA, USA). The initial knot was then backed up with 6 half-hitch knots after tensioning (Fig. 1). The traditional double-screw technique involved 2 bicortical 3.75-mm titanium cannulated screws (Arthrex, Naples, FL, USA).
Figure 2.
Top (A) and inferior (B) views of cadaveric glenoid potted in bone-cement rectangular prisms to enable rigid constraint during cyclic and static biomechanical testing.
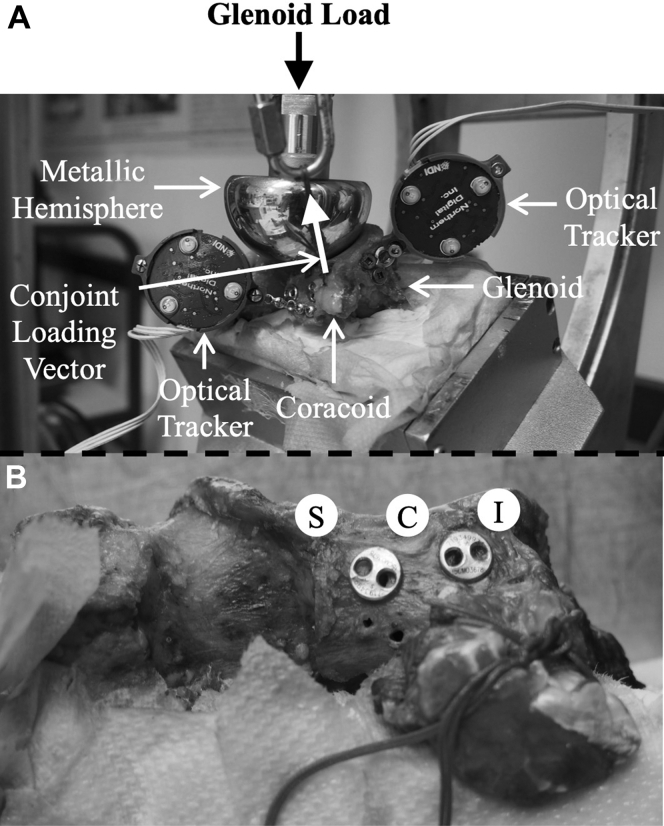
Each specimen was fixed in a custom rigid platform attached to a materials testing machine (Instron, Norwood, MA, USA) and was oriented in 30° of anteversion to represent glenohumeral loading just prior to shoulder dislocation.20 A uniaxial mechanical actuator loaded the coracoid-reconstructed glenoid dish via a 47-mm-diameter metallic hemisphere (Fig. 3). Cyclic compressive loading with an amplitude ranging between 50 and 200 N20 was applied to the glenoid at a rate of 1 Hz for 1000 cycles. Static conjoint tendon loading was applied via a suture24 attached to a weight, such that the line of action of the force ran from the inferior conjoint insertion and wrapped laterally around the metallic hemisphere. Testing was performed 3 times in a sequential (ie, stepwise) manner for static conjoint tendon loads of 0 N (simulating a bone block reconstruction), 10 N, and 20 N (simulating a Latarjet reconstruction).19 Although the exact magnitude of the load applied to the in vivo conjoint tendon was unknown, 10 N and 20 N were chosen to match and double, respectively, the conjoint forces that were suggested by Giles et al19 (2013). Each time that the conjoint tendon load was increased, a static load of 50 N was applied to the glenoid articular dish, and the conjoint force was applied.
Figure 3.
(A) Loading configuration, in which the coracoid-glenoid construct is positioned in 30° of anteversion. Optical tracking markers are affixed to the glenoid and coracoid, while a metallic hemisphere (47 mm in diameter) applies load to the glenoid articular surface. (B) Three points at the coracoid-glenoid boundary are digitized and tracked to quantify the relative displacement between the coracoid and glenoid: superior (S), central (C), and inferior (I).
To quantify the glenoid and coracoid positions, two 6-df Optotrak Certus optical tracking markers (NDI, Waterloo, ON, Canada) were fixed to the superior side of the anterior coracoid and approximately 10 mm below the inferior glenoid rim (Fig. 3). The positions of 3 points digitized on the inferior, central, and superior edges of the coracoid fragment were optically tracked with respect to a glenoid coordinate system throughout both cyclic testing and static testing to quantify coracoid displacement. Screw and button constructs were compared on the basis of maximum resultant displacement (d) at these 3 points (superior [dS], central [dC], and inferior [dI]). These displacements (ie, dS, dC, and dI) were quantified for both (1) the initial graft displacement when the static conjoint tendon load was applied with a constant glenoid dish load and (2) the ongoing graft displacement during glenoid dish cyclic loading. Statistical significance was assessed using a paired-samples t test (SPSS, version 23; IBM, Armonk, NY, USA), with the threshold of significance set at .05.
Results
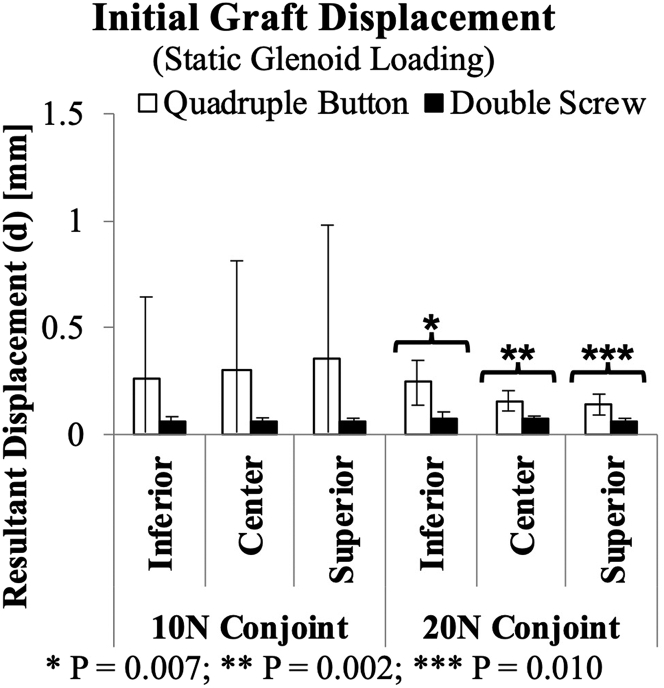
When the glenoid load was held constant at 50 N and the 10-N conjoint tendon load was initially applied, no significant differences (P ≥ .253) were found in graft displacement (dI, 0.26 ± 0.38 mm vs. 0.07 ± 0.02 mm; dC, 0.30 ± 0.51 mm vs. 0.06 ± 0.01 mm; and dS, 0.35 ± 0.63 mm vs. 0.06 ± 0.01 mm at 10 N) (Fig. 4). However, when the 20-N conjoint load was applied, the quadruple-button Latarjet reconstruction resulted in significantly larger graft displacement than the double screws for all 3 points (dI, 0.24 ± 0.10 mm vs. 0.07 ± 0.03 mm [P = .007, power = 0.979]; dC, 0.16 ± 0.05 mm vs. 0.07 ± 0.02 mm [P = .002, power = 0.999]; and dS, 0.14 ± 0.05 mm vs. 0.07 ± 0.01 mm [P = .010, power = 0.959] at 20 N).
Figure 4.
Mean peak resultant displacement (d) (± standard deviation) (in millimeters) of the coracoid relative to the glenoid at the superior, central, and inferior points along the coracoid-glenoid boundary during conjoint tendon load application. A static compressive load of 50 N was applied to the glenoid articular surface, while conjoint tendon loads of 10 and 20 N were applied prior to their respective 10 and 20-N cyclic tests.
When the glenoid dish was subsequently cyclically loaded without conjoint tendon loading, the quadruple-button and double-screw constructs did not produce significantly different (P ≥ .617) graft displacements (dI, 0.30 ± 0.43 mm vs. 0.20 ± 0.22 mm; dC, 0.36 ± 0.59 mm vs. 0.22 ± 0.25 mm; and dS, 0.44 ± 0.77 mm vs. 0.24 ± 0.29 mm at 0 N) (Fig. 5). Additionally, the quadruple-button construct was not found to differ significantly (P ≥ .095) from the double screws in terms of resultant coracoid displacement for any points when a 10-N load was applied to the conjoint tendon (dI, 0.30 ± 0.23 mm vs. 0.11 ± 0.03 mm; dC, 0.31 ± 0.34 mm vs. 0.11 ± 0.02 mm; and dS, 0.34 ± 0.45 mm vs. 0.11 ± 0.02 mm at 10 N). At 20 N of conjoint tendon loading, however, at the inferior and central points, the quadruple-button construct began to produce significantly larger displacements than the double screws during cyclic loading (dI, 0.39 ± 0.15 mm vs. 0.12 ± 0.02 mm [P = .004, power = 0.995]; and dC, 0.27 ± 0.12 mm vs. 0.12 ± 0.02 mm [P = .023, power = 0.968] at 20 N). It should be noted that the difference in superior point displacement did approach significance when the 20-N conjoint tendon load was applied (dS, 0.25 ± 0.13 mm vs. 0.12 ± 0.02 mm [P = .056, power = 0.686]).
Figure 5.
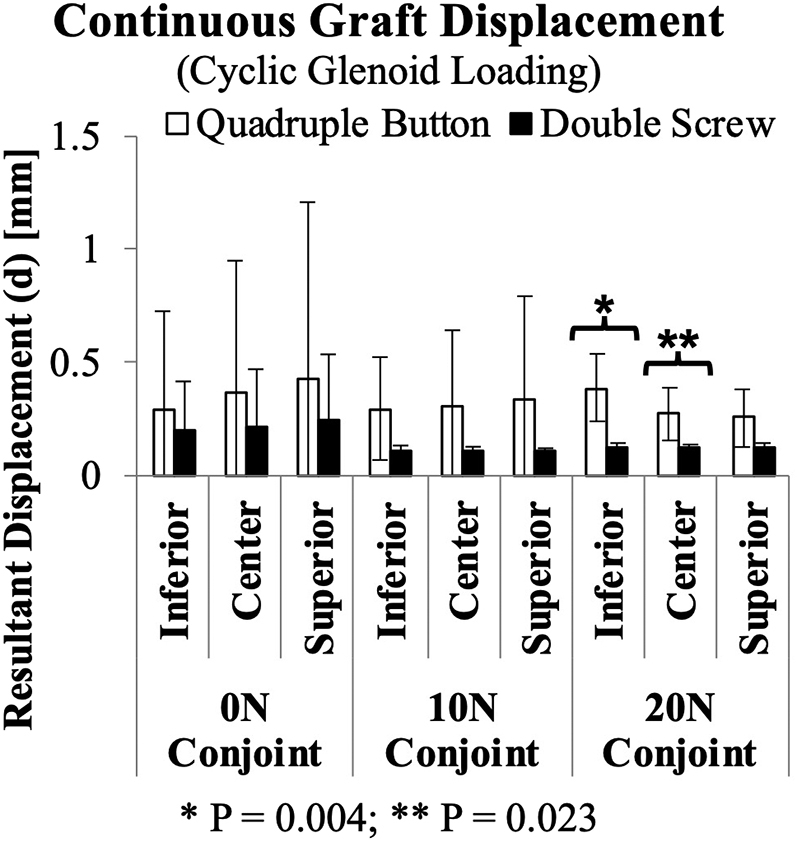
Mean peak resultant displacement (d) (± standard deviation) (in millimeters) of the coracoid relative to the glenoid at the superior, central, and inferior points along the coracoid-glenoid boundary during compressive cyclic glenoid loading. Compressive loading cycled between 50 and 200 N at a rate of 1 Hz for 1000 cycles. Testing was conducted for static conjoint tendon loads of 0, 10, and 20 N.
Discussion
This work constitutes an in vitro assessment of coracoid graft motion following quadruple-button fixation for anterior bone block and Latarjet procedures. The results indicate that when conjoint tendon loading was absent, which represents the clinical scenario of the coracoid being used as a bone block, the quadruple-button system is a suitable substitute for screw fixation. When conjoint tendon loading was applied to the coracoid graft, a rotational moment was generated at the inferior tendon insertion site, which resulted in some graft displacement. Owing to the small magnitude of resultant displacements when 10-N conjoint forces were applied, it is suggested that quadruple buttons may also act as a substitute for screws, provided that conjoint tendon loading is minimized during the postoperative graft-healing period. However, when loading the conjoint tendon to 20 N, significant differences in graft displacement between the screw and quadruple-button techniques occurred, which proves our initial hypothesis to be void. The results of the conjoint force application trials (ie, when conjoint load was first applied) suggest that 20 N of conjoint loading causes the coracoid graft to shift slightly (dI, 0.24 ± 0.10 mm; dC, 0.16 ± 0.05 mm; and dS, 0.14 ± 0.05 mm) on initial loading. This finding suggests that the quadruple-button reconstruction does not provide equivalent resistance to interface movement to that of bicortical screws under conjoint loads > 10 N. The increase in graft displacement at higher conjoint loads implies that further care must be taken to protect the graft in the early phases of healing, such as by conducting an associated labral repair, restricting heavy lifting, or ensuring shoulder immobilization with a sling.
Owing to the recent appearance of the quadruple-button fixation technique for the Latarjet procedure, little is known about its longer-term outcomes. However, our in vitro results support the in vivo results of Boileau et al10 (2016) that demonstrated the quadruple-button technique to be an effective alternative to screw fixation. Although their in vivo study used a single button set centered in the coracoid graft, graft healing was found in 91% of their subjects.10 This high prevalence of graft healing coupled with the present results suggests that graft displacement may remain within the acceptable range for ideal bone-on-bone healing noted by Claes et al16 (0.2-1 mm)41 regardless of which technique is used. This agrees well with the clinical finding of Metais et al30 (2016) that patient range of motion was similar between arthroscopic button and open or arthroscopic screw techniques at a mean of 27.7 months’ follow-up.
In this investigation, we chose to use 2 button sets (4 buttons) to further reduce graft rotation when the conjoint tendon was loaded, which is similar to the method presented by Valenti et al40 (2018), as well as the recent clinical cases reported by Hardy et al21 (2020). Although a direct assessment of graft migration was not performed, Hardy et al found that the dislocation rate was significantly higher for patients treated with cortical buttons (8.3%) than for those treated with screws (2.5%); however, they did find that reoperations were more common in the screw cohort (5.9%) than in the cortical button cohort (0%). These results agree well with the higher graft displacement noted for button reconstruction in our investigation and suggest a tradeoff between dislocation risk and hardware removal that requires further investigation.
In a biomechanical comparative study, Provencher et al37 compared screw vs. button fixation for the Latarjet procedure and found no substantial differences between techniques. Their finding of no difference may be attributed to the loading of the conjoint tendon, which peaked at 10 N. These findings are confirmed in our study, which also showed no differences when assessing fixation at values of conjoint tendon loading < 10 N. However, in our study, the difference between screws and buttons was only apparent at a 20-N load, which was not tested by Provencher et al. Williams et al45 also compared screws vs. buttons in their biomechanical study. However, they chose to test the coracoid without any load on the conjoint tendon. Our results indicate that loading of the conjoint tendon to varying degrees does have a significant effect on the fixation stability. In addition, Williams et al tested the coracoid graft fixation stability by applying a point load directly to the graft. Although this method of testing is able to effectively isolate the fixation of the graft to the glenoid, it may not re-create the clinical method of loading, which is via the humeral head. As such, a more clinically relevant assessment of graft stability may be conducted via loading through a simulated humeral head, as was performed in our study.
As with any in vitro investigation, there are inherent limitations that should be noted. The use of cadaveric specimens prevented the assessment of graft healing and limits the application of results to the immediate postoperative period. This period, prior to graft healing, represents the time during which each fixation technique would be most relied on and, accordingly, was a key time point for in vitro investigation. Because the primary purpose of both fixation techniques is to hold the coracoid graft in place until healing is achieved, the primary period of interest for comparing quadruple buttons vs. double screws should be prior to graft healing. Another limitation is that the cadaveric population was relatively old compared with a clinical population, as the Latarjet procedure is commonly performed to repair anterior glenoid defects arising from glenohumeral dislocations in a younger, athletic population. Hence, although the comparison of the 2 techniques is likely efficacious using these specimens, the absolute magnitude of displacement may be higher in an active population. All cadaveric subjects were screened for diseases that affect bone and were subjected to acquisition of computed tomography scans to ensure there were no traumatic injuries to the shoulder prior to testing. As such, the scapulae used in this investigation were of sufficient quality for an in vitro biomechanical investigation. Another limitation is that 1 generic metallic humeral head was used to load each specimen. This was done to maintain consistency between test specimens but is nonetheless a limitation.
Regarding conjoint tendon loading, Giles et al19 (2013) suggested that a force of 10 N is sufficient to simulate the encapsulating and/or buttressing effect of the conjoint tendon; however, the literature does not provide a direct measure of the in vivo loads to which this tendon is subjected. Accordingly, to avoid simulating an overly conservative conjoint tendon load, forces of 0, 10, and 20 N were applied independently in this investigation to ascertain the effect of conjoint loading on coracoid graft displacement. It should also be noted that the period of interest for graft healing is immediately after surgery, when the shoulder is likely in some degree of sling immobilization, with limited activity owing to postsurgical pain. Future in vivo work should seek to quantify any difference in coracoid graft healing, joint stability, and peri-screw or button bone resorption when the double-screw and quadruple-button techniques are used for the Latarjet procedure.
Conclusion
The quadruple-button technique has comparable fixation stability to double screws when the coracoid is used as a bone block or when conjoint tendon loading is minimized. However, at higher conjoint tendon loads, the double screws created a more stable construct than the quadruple buttons.
Disclaimer
Support for this study was provided by the National Science and Engineering Research Council of Canada (NSERC; grant no. R0598A01). In addition, Smith & Nephew provided the suture button constructs for testing.
George S. Athwal is a consultant for DePuy Synthes and Tornier. Additionally, he has received research support from Tornier, DePuy Synthes, and Exactech for research related to the subject of this article.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors would like to acknowledge support provided by The Bone and Joint Institute at the University of Western Ontario.
References
- 1.Allain J., Goutallier D., Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 2010;80:841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Athwal G.S., Meislin R., Getz C., Weinstein D., Favorito P. Short-term complications of the arthroscopic Latarjet procedure: a North American experience. Arthroscopy. 2016;32:1965–1970. doi: 10.1016/j.arthro.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 3.Balg F., Boileau P. The instability severity index score. J Bone Joint Surg Br. 2007;89-B:1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 4.Beran M.C., Donaldson C.T., Bishop J.Y. Treatment of chronic glenoid defects in the setting of recurrent anterior shoulder instability: a systematic review. J Shoulder Elbow Surg. 2010;19:769–780. doi: 10.1016/j.jse.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Bessière C., Trojani C., Carles M., Mehta S.S., Boileau P. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res. 2014;472:2345–2351. doi: 10.1007/s11999-014-3550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatia D.N., De Beer J.F., Du Toit D.F. Coracoid process anatomy: implications in radiographic imaging and surgery. Clin Anat. 2007;20:774–784. doi: 10.1002/ca.20525. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia S., Frank R.M., Ghodadra N.S., Hsu A.R., Romeo A.A., Bach B.R. The outcomes and surgical techniques of the Latarjet procedure. Arthroscopy. 2014;30:227–235. doi: 10.1016/j.arthro.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P., Alami G., Rumian A., Schwartz D.G., Trojani C., Seidl A.J. The doubled-suture Nice knot. Orthopedics. 2017;40:e382–e386. doi: 10.3928/01477447-20161202-05. [DOI] [PubMed] [Google Scholar]
- 9.Boileau P., Bicknell R.T., El Fegoun A.B., Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the “belt-and-suspenders” operative technique and preliminary results. Arthroscopy. 2007;23:593–601. doi: 10.1016/j.arthro.2007.03.096. [DOI] [PubMed] [Google Scholar]
- 10.Boileau P., Gendre P., Baba M., Thélu C.-É., Baring T., Gonzalez J.-F. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg. 2016;25:78–89. doi: 10.1016/j.jse.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Boileau P., Mercier N., Old J. Arthroscopic Bankart-Bristow-Latarjet (2B3) procedure: how to do it and tricks to make it easier and safe. Orthop Clin North Am. 2010;41:381–392. doi: 10.1016/j.ocl.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Boileau P., Mercier N., Roussanne Y., Thélu C.-E., Old J. Arthroscopic Bankart-Bristow-Latarjet procedure: the development and early results of a safe and reproducible technique. Arthroscopy. 2010;26:1434–1450. doi: 10.1016/j.arthro.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Boileau P., Thélu C.É., Mercier N., Ohl X., Houghton-Clemmey R., Carles M. Arthroscopic Bristow-Latarjet combined with Bankart repair restores shoulder stability in patients with glenoid bone loss. Clin Orthop Relat Res. 2014;472:2413–2424. doi: 10.1007/s11999-014-3691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burkhart S.S., De Beer J.F., Barth J.R.H., Criswell T., Roberts C., Richards D.P. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Butt U., Charalambous C.P. Complications associated with open coracoid transfer procedures for shoulder instability. J Shoulder Elbow Surg. 2012;21:1110–1119. doi: 10.1016/j.jse.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Claes L.E., Heigele C.A., Neidlinger-Wilke C., Kaspar D., Seidl W., Margevicius K.J. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998;355S(Suppl):S132–S147. doi: 10.1097/00003086-199810001-00015. [DOI] [PubMed] [Google Scholar]
- 17.Collin P., Rochcongar P., Thomazeau H. Résultat de la butée coracoïdienne type Latarjet pour instabilité antérieure chronique de l'épaule [Treatment of chronic anterior shoulder instability using a coracoid bone block (Latarjet procedure): 74 cases] Rev Chir Orthop Reparatrice Appar Mot. 2007;93:126–132. doi: 10.1016/s0035-1040(07)90215-9. [in French] [DOI] [PubMed] [Google Scholar]
- 18.Delaney R.A., Freehill M.T., Janfaza D.R., Vlassakov K.V., Higgins L.D., Warner J.J.P. 2014 Neer Award paper: neuromonitoring the Latarjet procedure. J Shoulder Elbow Surg. 2014;23:1473–1480. doi: 10.1016/j.jse.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Giles J.W., Boons H.W., Elkinson I., Faber K.J., Ferreira L.M., Johnson J.A. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22:821–827. doi: 10.1016/j.jse.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Giles J.W., Puskas G.J., Welsh M.F., Johnson J.A., Athwal G.S. Suture anchor fixation of bony Bankart fractures: comparison of single-point with double-point “suture bridge” technique. Am J Sports Med. 2013;41:2624–2631. doi: 10.1177/0363546513501795. [DOI] [PubMed] [Google Scholar]
- 21.Hardy A., Sabatier V., Schoch B., Vigan M., Werthel J.D., Nourissat G. Latarjet with cortical button fixation is associated with an increase of the risk of recurrent dislocation compared to screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020;28:2354–2360. doi: 10.1007/s00167-019-05815-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hovelius L., Sandström B., Olofsson A., Svensson O., Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012;21:647–660. doi: 10.1016/j.jse.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 23.Itoi E., Lee S.B., Berglund L.J., Berge L.L., An K.N. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Krackow K.A., Thomas S.C., Jones L.C. A new stitch for ligament-tendon fixation. Brief note. J Bone Joint Surg Am. 1986;68:764–766. [PubMed] [Google Scholar]
- 25.Lädermann A., Denard P.J., Burkhart S.S. Injury of the suprascapular nerve during Latarjet procedure: an anatomic study. Arthroscopy. 2012;28:316–321. doi: 10.1016/j.arthro.2011.08.307. [DOI] [PubMed] [Google Scholar]
- 26.Lafosse L., Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19(Suppl):2–12. doi: 10.1016/j.jse.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 27.Lafosse L., Lejeune E., Bouchard A., Kakuda C., Gobezie R., Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242.e1–1242.e5. doi: 10.1016/j.arthro.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Latarjet M. A propos du traitement des luxations récidivantes de l’épaule. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 29.Maquieira G.J., Gerber C., Schneeberger A.G. Suprascapular nerve palsy after the Latarjet procedure. J Shoulder Elbow Surg. 2007;16:e13–e15. doi: 10.1016/j.jse.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 30.Metais P., Clavert P., Barth J., Boileau P., Broszka R., Nourissat G. Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: prospective multicentre study of 390 cases. Orthop Traumatol Surg Res. 2016;102:S271–S276. doi: 10.1016/j.otsr.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 31.Meyer D.C., Moor B.K., Gerber C., Ek E.T.H. Accurate coracoid graft placement through use of a drill guide for the Latarjet procedure. J Shoulder Elbow Surg. 2013;22:701–708. doi: 10.1016/j.jse.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 32.Mizuno N., Denard P.J., Raiss P., Melis B., Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23:1691–1699. doi: 10.1016/j.jse.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Nourissat G., Nedellec G., O’Sullivan N.A., Debet-Mejean A., Dumontier C., Sautet A. Mini-open arthroscopically assisted Bristow-Latarjet procedure for the treatment of patients with anterior shoulder instability: a cadaver study. Arthroscopy. 2006;22:1113–1118. doi: 10.1016/j.arthro.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 34.Patte D., Bernageau J., Bancel P. The anteroinferior vulnerable point of the glenoid rim. In: Bateman J., Welsh R., editors. Surgery of the shoulder. Marcel Dekker; New York: 1985. pp. 94–99. [Google Scholar]
- 35.Piasecki D.P., Verma N.N., Romeo A.A., Levine W.N., Bach B.R., Provencher M.T. Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. J Am Acad Orthop Surg. 2009;17:482–493. doi: 10.5435/00124635-200908000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Provencher M.T., Bhatia S., Ghodadra N.S., Grumet R.C., Bach B.R., Dewing L.C.B. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92(Suppl 2):133–151. doi: 10.2106/JBJSJ.00906. [DOI] [PubMed] [Google Scholar]
- 37.Provencher M.T., Aman Z.S., LaPrade C.M., Bernhardson A.S., Moatshe G., Storaci H.W. Biomechanical comparison of screw fixation versus a cortical button and self-tensioning suture for the Latarjet procedure. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118777842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmid S.L., Farshad M., Catanzaro S., Gerber C. The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients. J Bone Joint Surg Am. 2012;94:e75. doi: 10.2106/JBJS.K.00380. [DOI] [PubMed] [Google Scholar]
- 39.Shah A.A., Butler R.B., Romanowski J., Goel D., Karadagli D., Warner J.J.P. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 40.Valenti P., Maroun C., Wagner E., Werthel J.D. Arthroscopic Latarjet procedure combined with Bankart repair: a technique using 2 cortical buttons and specific glenoid and coracoid guides. Arthrosc Tech. 2018;7:e313–e320. doi: 10.1016/j.eats.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vicenti G., Pesce V., Tartaglia N., Abate A., Mori C.M., Moretti B. Micromotion in the fracture healing of closed distal metaphyseal tibial fractures: a multicentre prospective study. Injury. 2014;45(Suppl 6):S27–S35. doi: 10.1016/j.injury.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 42.Walch G. La luxation recidivante anterieure d’epaule [Recurrent anterior shoulder instability] Rev Chir Orthop Reparatrice Appar Mot. 1991;77:177–191. [in French] [Google Scholar]
- 43.Walch G., Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000;4:256–261. [Google Scholar]
- 44.Weppe F., Magnussen R.A., Lustig S., Demey G., Neyret P., Servien E. A biomechanical evaluation of bicortical metal screw fixation versus absorbable interference screw fixation after coracoid transfer for anterior shoulder instability. Arthroscopy. 2011;27:1358–1363. doi: 10.1016/j.arthro.2011.03.074. [DOI] [PubMed] [Google Scholar]
- 45.Williams R.C., Morris R.P., El Beaino M., Maassen N.H. Cortical suture button fixation vs. bicortical screw fixation in the Latarjet procedure: a biomechanical comparison. J Shoulder Elbow Surg. 2020;29:1–9. doi: 10.1016/j.jse.2019.11.025. [DOI] [PubMed] [Google Scholar]
- 46.Young C.D., Rockwood C.A., Jr. Complications of a failed Bristow procedure and their management. J Bone Joint Surg Am. 1991;73:969–981. [PubMed] [Google Scholar]
- 47.Zuckerman J.D., Matsen F.A., III Complications about the glenohumeral joint related to the use of screws and staples. J Bone Joint Surg Am. 1984;66:175–180. [PubMed] [Google Scholar]