Abstract
Background
Reverse shoulder arthroplasty is gaining popularity owing to its proven longevity and good outcome scores. Scapular notching remains a concern. This study aimed to assess the safety of larger polyethylene glenospheres with increased eccentricity in comparison with the more conventional metal bearings. The secondary effects on scapular notching, clinical outcomes, range of movement, and complications were also analyzed.
Methods
We conducted a 10-year retrospective review of 145 SMR reverse shoulder arthroplasties (LimaCorporate, Udine, Italy) in 132 patients with radiographs at a minimum of 2 years postoperatively. The primary outcome measure was the survivorship of the larger polyethylene glenospheres. Secondary outcomes were the presence and size of notching, subjective satisfaction score, American Shoulder and Elbow Surgeons score, Oxford Shoulder Score, range of motion, and shoulder-related complications.
Results
No failures of the polyethylene glenospheres were noted in the 10-year period. At a minimum of 2 years’ follow-up, notching was noted in 16 (25%) of the metal glenospheres vs. 9 (11.1%) of the polyethylene glenospheres (P = .028). The mean Oxford Shoulder Score was lower for the metal glenospheres (P = .005). Range of motion, complications, and overall satisfaction were similar in both groups.
Conclusion
The inverted bearing configuration demonstrated no failures at a minimum of 2 years’ follow-up. A larger study is required to determine whether the decreased incidence and size of early notching are related to the bearing size or material.
Keywords: Reverse shoulder arthroplasty, polyethylene glenosphere, scapular notching, rotator cuff arthropathy, shoulder, SMR
Reverse shoulder arthroplasty (RSA) is becoming increasingly more common as its indications expand and confidence in its longevity increases. Scapular notching is unique to RSA, with its presence being associated with inferior outcomes. It can progress over time, lead to early glenoid prosthesis loosening, and reduce glenoid bone stock for potential revision arthroplasty.18,23,26 Multiple design changes have been made in an effort to decrease the incidence of notching. These include larger glenospheres, glenosphere eccentricity, a decrease in the neck-shaft angle from 155° to 135°, and the ability to lateralize the glenosphere.1,2,7,10,12,19,27,29 The outcomes of such changes remain unclear.
The SMR RSA (LimaCorporate, Udine, Italy) is the prosthesis of choice in our institution. It has an inlay design with a neck-shaft angle of 150° and 3 glenosphere sizes (36, 40, and 44 mm). The 36- and 44-mm glenospheres have a 4-mm eccentric option (Fig. 1). The 36-mm glenosphere is only manufactured in metal. The system is unique in that the 40- and 44-mm glenospheres are only manufactured with an inverted material bearing. These larger glenospheres are composed of polyethylene coupled with a metal central peg, whereas the humeral cup liners are composed of cobalt chrome. This articulation is proposed to prevent the generation of polyethylene debris from mechanical impingement of the humeral cup liner against the scapula that occurs in the traditional bearing configuration. In our study, the size and bearing configuration of each RSA were determined intraoperatively by the surgeon on the basis of clinical findings such as stability and soft-tissue tension.
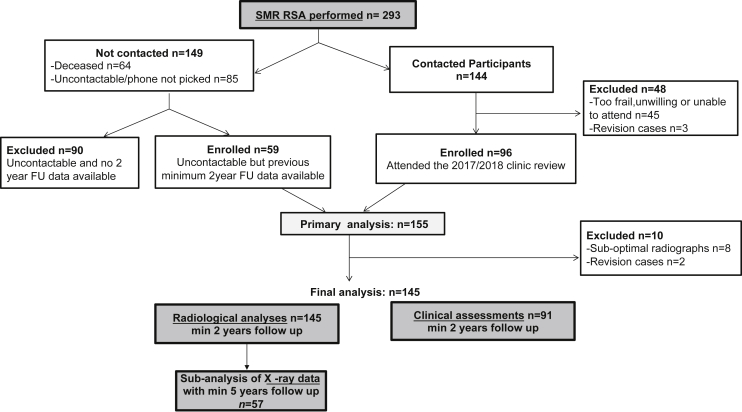
Figure 1.
The SMR reverse shoulder arthroplasty glenosphere is available in 3 sizes (36, 40, and 44 mm). The smallest and largest sizes also have the option of +4 mm eccentricity. The 40- and 44-mm versions are composed of polyethylene.
Our primary aim was to report on the safety of larger polyethylene glenospheres in comparison with their metallic counterparts. The secondary aims were to determine whether these larger glenospheres with the inverted material coupling reduced scapular notching and to determine the impact on clinical outcomes, range of motion (ROM), and complications.
Materials and methods
We conducted a retrospective review of 293 patients who underwent an SMR RSA performed at North Shore Hospital, Takapuna, Auckland, New Zealand. Patients underwent surgery between June 2005 and December 2015 under the care of 3 subspecialized shoulder surgeons, all of whom exclusively used the SMR RSA. The review process formed part of normal RSA hospital follow-up practice. The auditing of outcomes was carried out between July 2017 and September 2018.
All patients who had shoulder radiographs obtained at a minimum of 2 years postoperatively were included in the study and were invited to undergo a clinical review. Patients who had undergone previous shoulder surgery were excluded, as were those with suboptimal radiographs.
A total of 293 SMR RSAs were performed in a 10-year period. Almost half of these patients (n = 149) were either deceased (n = 64) or unable to be contacted for the invitation to be reviewed in the clinic (n = 85). Of the 144 patients whom we were able to contact, 96 completed the clinical review and were enrolled in this study. By use of data available from previous clinical reviews, an additional 59 RSAs were enrolled from the list of patients who were unable to be contacted, giving a total of 155 RSAs to be included for primary analysis (Fig. 2). A further 10 patients were excluded because they either had suboptimal radiographs or were revision cases. This left 145 RSAs (132 patients [13 bilateral]) for final analysis (Table I). Of the patients, 102 (70.3%) were women and 43 (29.7%) were men; the mean age was 75.2 years (range, 53-89 years). The mean body mass index was similar in both the metal and polyethylene glenosphere groups. The mean follow-up period was 4 years (range, 2-12 years), with mean follow-up periods of 5 years and 4 years for the metal and polyethylene glenosphere groups, respectively. The most common diagnosis was rotator cuff arthropathy (51%), followed by osteoarthritis (31%) and fracture (13.8%). Of the 145 RSAs implanted, 81 had polyethylene glenospheres. There was a propensity for the 36-mm metal bearing to be implanted in female patients (55 women vs. 9 men). Eccentric glenospheres were used 67.2% of the time in the 36-mm metal glenosphere group vs. 32.1% of the time in the larger polyethylene glenosphere group.
Figure 2.
Patient enrollment flow diagram. RSA, reverse shoulder arthroplasty; FU, follow-up; min, minimum.
Table I.
Demographic and surgical data
| Metal glenosphere (n = 64) | Larger polyethylene glenosphere (n = 81) | Total (n = 145) | P value | |
|---|---|---|---|---|
| Sex | <.001∗ | |||
| Female | 55 (85.9) | 47 (58.0) | 102 (70.3) | |
| Male | 9 (14.1) | 34 (42.0) | 43 (29.7) | |
| Age at procedure, yr | .830 | |||
| Mean ± SD | 75.8 ± 6.6 | 74.8 ± 6.5 | 75.2 ± 6.5 | |
| Range | 54-87 | 53-89 | 53-89 | |
| BMI† | .186 | |||
| Mean ± SD | 28.1 ± 5.9 | 29.7 ± 6.4 | 29.1 ± 6.2 | |
| Range | 19-45 | 15-53 | 15-53 | |
| Affected side | .933 | |||
| Right | 36 (56.3) | 45 (55.6) | 81 (55.9) | |
| Left | 28 (43.7) | 36 (44.4) | 64 (44.1) | |
| Diagnosis | .012∗ | |||
| Rotator cuff arthropathy | 36 (56.3) | 38 (46.9) | 74 (51.0) | |
| Osteoarthritis | 15 (23.4) | 30 (37.0) | 45 (31.0) | |
| Fracture | 7 (10.9) | 13 (16.0) | 20 (13.8) | |
| Rheumatoid arthritis | 6 (9.4) | 0 (0.0) | 6 (4.1) | |
| Glenosphere used | <.001∗ | |||
| Concentric | 21 (32.8) | 55 (67.9) | 76 (52.4) | |
| Eccentric | 43 (67.2) | 26 (32.1) | 69 (47.6) | |
| Follow-up duration, mean (range), yr | 5 (2-12) | 4 (2-10) | 4 (2-12) | .029∗ |
SD, standard deviation; BMI, body mass index.
Data are presented as number (percentage) unless otherwise indicated. Percentages are rounded to 1 decimal point.
Statistically significant difference (P < .05).
BMI values were missing in 29 cases.
The primary outcome assessed was survivorship. Secondary outcomes were the presence and size of any inferior scapular notching, humeral osteolysis, subjective satisfaction rating of the patient, American Shoulder and Elbow Surgeons (ASES) score,22 Oxford Shoulder Score (OSS),9 ROM, and shoulder-related complications. Patient-related outcome measures were recorded at the time of the clinical review. OSS values at 6 months and 5 years, as well as dislocation and infection rates, were requested from the New Zealand Joint Registry for comparison. Patients who were unable to attend a clinical review completed a postal questionnaire and were also contacted telephonically by the department’s research assistant (I.C.).
Patient satisfaction was recorded as very dissatisfied, dissatisfied, neutral, satisfied, or very satisfied. Shoulder movements of forward flexion, abduction, and external rotation at 90° of abduction (or as best able) were recorded using the mobile phone application Clinometer (Plaincode Software Solutions, Gunzenhausen, Germany).30 External rotation in adduction was recorded using a goniometer, whereas internal rotation was recorded based on where the patient was able to place his or her thumb in terms of the hip, sacroiliac joint, mid-lumbar spine, thoracolumbar junction, or mid-thoracic spine.
The radiographs (anteroposterior glenoid views) of each patient were reviewed independently by 2 experienced shoulder fellows (C.W.J. and M.B.). Interobserver reliability was assessed, with an intraclass correlation coefficient of 0.86. The radiographs were assessed for the presence and size of inferior scapular notching, implant failure, areas of radiolucency, and osteolysis of the glenoid and proximal humerus. The radiographs of patients who underwent RSA for fracture were not assessed for humeral osteolysis. Notching was measured by drawing a line continuous with the inferior scapular neck; a second line was then drawn perpendicular to this, aiming for the apex or maximal part of the notch (Figs. 3 and 4). Notching was measured in millimeters. The Nerot grading system for notching was not used as the SMR metaglene uses variable-angle screws rather than fixed-angle screws.
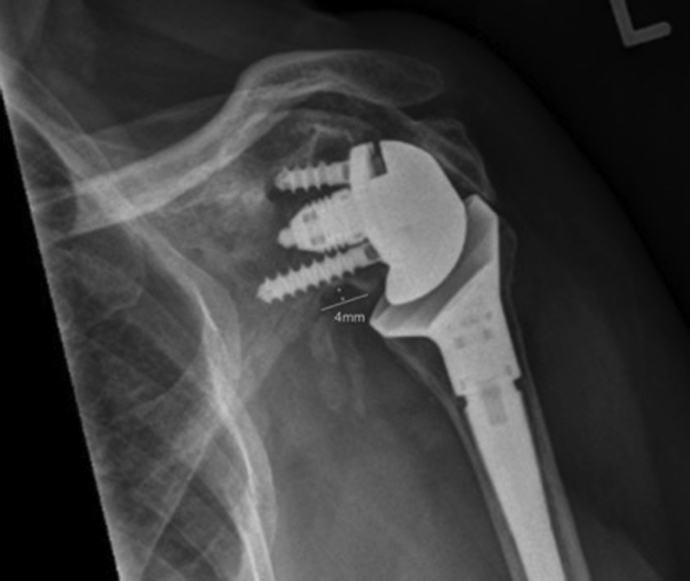
Figure 3.
The notch size (X) was measured by drawing a line from the apex of the notch perpendicular to a line drawn along the inferior glenoid neck.
Figure 4.
A radiograph demonstrating our measurement of scapular notching. The Nerot grading system was not used as the SMR RSA uses variable angle screws.
Osteolysis of the glenoid was assessed and graded as follows: grade 0, no osteolysis; grade 1, minor osteolysis, defined as osteolysis up to and involving the inferior screw; grade 2, major osteolysis, defined as osteolysis extending past the inferior screw, but no loosening; or grade 3, loosening and osteolysis around the baseplate. Osteolysis of the humerus was assessed and graded as follows: grade 0, no osteolysis; grade 1, <50% resorption of the greater tuberosity; grade 2, >50% resorption of the greater tuberosity; grade 3, complete resorption of the greater tuberosity; or grade 4, complete resorption of the greater tuberosity plus the lateral humerus.
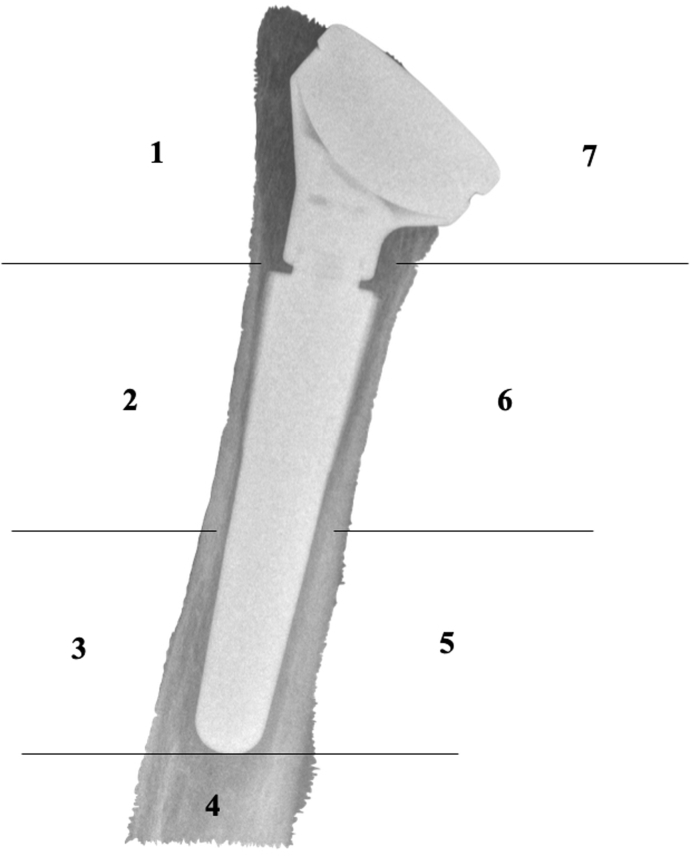
Additionally, calcar osteolysis was recorded. Areas of radiolucency around the humeral stem were recorded from zone 1 laterally to zone 7 medially, with zone 4 being around the tip of the stem (Fig. 5). Finally, any evidence of humeral subsidence was recorded.
Figure 5.
Zones of humeral osteolysis.
Statistical analysis
Demographic, surgical, radiographic, and clinical outcome data were compared between the 2 glenosphere groups (metal vs. larger polyethylene). Continuous data were assessed for normality using the Shapiro-Wilk test and an evaluation of normality plots. The differences between groups were assessed using the Student t test or, if data were non-normally distributed, the Mann-Whitney test. Differences between categorical variables were evaluated using the Pearson χ2 or Fisher exact test for observed cell counts < 5. Finally, with adjustment for the demographic and surgical factors that were statistically different between the metal and polyethylene glenosphere groups, a multiple logistic regression model was performed to investigate the adjusted association between the glenosphere used and the notching rate. For notching and osteolysis rates, an additional subanalysis including 57 participants who had attained 5 years of follow-up was conducted. Assessments for osteolysis excluded fracture cases. All statistical analyses were completed using SPSS software (version 24; IBM, Armonk, NY, USA). Results were considered significant at P < .05.
Results
No failures of the polyethylene glenospheres were noted at any time over the 10-year period. At a minimum of 2 years’ follow-up, notching was noted in 16 (25%) of the metal glenospheres vs. 9 (11.1%) of the polyethylene glenospheres (P = .028) (Table II). The mean notch size was 5 mm (range, 3-13 mm) in the metal glenosphere group and 4 mm (range, 3-5 mm) in the polyethylene glenosphere group. After adjustment for the confounding factors—namely, sex, diagnosis, glenosphere eccentricity, and follow-up duration—the data demonstrated that notching was less likely to occur among patients who had polyethylene glenospheres when compared with the metal glenosphere group, with an odds ratio of 0.28 (95% confidence interval, 0.09-0.86) (P = .03). Similarly, among participants who had attained a minimum of 5 years’ follow-up, there was a tendency toward a higher prevalence of notching with the smaller metal bearing, but this was not statistically significant (P = .170). The presence of osteolysis affecting the humerus and/or glenoid was comparable in both groups at a minimum of 2 and 5 years’ follow-up (P > .500) (Table II). Because of the small number of patients with osteolysis, further analysis of the humeral or glenoid zones involved was not performed.
Table II.
Glenosphere associations with radiologic outcomes and postoperative complications
| Metal glenosphere | Larger polyethylene glenosphere | Total | P value | |
|---|---|---|---|---|
| Notching at ≥2-yr FU | .028∗ | |||
| No | 48 (75.0) | 72 (88.9) | 120 (82.8) | |
| Yes | 16 (25.0) | 9 (11.1) | 25 (17.2) | |
| Osteolysis at ≥2-yr FU† | .530 | |||
| No | 46 (82.5) | 53 (77.9) | 100 (80.0) | |
| Yes | 10 (17.5) | 15 (22.1) | 25 (20.0) | |
| Notching at ≥5-yr FU | .166 | |||
| No | 25 (75.8) | 22 (91.7) | 47 (82.5) | |
| Yes | 8 (24.2) | 2 (8.3) | 10 (17.5) | |
| Osteolysis at ≥5-yr FU† | .527 | |||
| No | 25 (83.3) | 16 (76.2) | 41 (80.4) | |
| Yes | 5 (16.7) | 5 (23.8) | 10 (19.6) | |
| Postoperative complications | .040∗ | |||
| No | 52 (81.3) | 75 (92.6) | 127 (87.6) | |
| Yes | 12 (18.8) | 6 (7.4) | 18 (12.4) | |
| Revision,n/total | 1/64 | 0/84 | 1/145 | — |
FU, follow-up.
Data are presented as number (percentage) unless otherwise indicated. Percentages are rounded to 1 decimal point.
Statistically significant difference (P < .05).
Fracture cases (n = 20) were excluded from osteolysis assessment.
The mean OSS in the metal glenosphere group was significantly lower than that in the polyethylene glenosphere group: 38 (range, 14-47) vs. 42 (range, 25-48) (P = .005) (Table III). The mean ASES score was 72 (range, 17-95) and 79 (range, 38-100) in the metal and polyethylene glenosphere groups, respectively, but the mean difference did not reach statistical significance (P = .160). Similar ranges of movement were recorded for both groups. Overall, in 85.7% of cases across the 2 groups, patients were satisfied or very satisfied with the outcome of their RSA. We recorded 12 complications (18.8%) in the metal glenosphere group vs. 6 (7.4%) in the polyethylene glenosphere group (P = .040) (Table IV). The difference in complication rates was not significant in the regression model (P = .198). None of the complications required reoperations.
Table III.
Clinical and functional outcomes
| Metal glenosphere (n = 27) | Polyethylene glenosphere (n = 64) | Total (n = 91) | P value | |
|---|---|---|---|---|
| Pain rating, mean (range) | 2.1 (0-7) | 1.8 (0-9) | 1.9 (0-9) | .971 |
| OSS, mean (range) | 38 (14-47) | 42 (25-48) | 41 (14-48) | .005∗ |
| ASES score, mean (range) | 72 (17-95) | 79 (38-100) | 77 (17-100) | .157 |
| ROM | ||||
| Forward flexion, ° | ||||
| Mean ± SD | 115 ± 27 | 117 ± 20 | 116 ± 22 | .796 |
| Range | 60-180 | 55-150 | 55-180 | |
| Abduction while erect, ° | ||||
| Mean ± SD | 107 ± 23 | 108 ± 25 | 107 ± 24 | .843 |
| Range | 60-161 | 40-150 | 40-161 | |
| ER in abduction, ° | ||||
| Mean ± SD | 33 ± 17 | 32 ± 14 | 33 ± 15 | .865 |
| Range | 8-80 | 10-70 | 8-80 | |
| ER abduction while supine, ° | ||||
| Mean ± SD | 45 ± 19 | 49 ± 20 | 48 ± 19 | .364 |
| IR while erect† | .256 | |||
| Hip | 6 (24.0) | 9 (17.3) | 15 (19.5) | |
| Sacroiliac joint | 5 (20.0) | 18 (34.6) | 23 (29.9) | |
| Mid-lumbar spine | 9 (36.0) | 9 (17.3) | 18 (23.4) | |
| Thoracolumbar junction | 1 (4.0) | 7 (13.5) | 8 (10.4) | |
| Mid-thoracic spine | 4 (16.0) | 9 (17.3) | 13 (16.9) | |
| Satisfaction score | .291 | |||
| Very dissatisfied | 0 (0) | 1 (1.6) | 1 (1.1) | |
| Dissatisfied | 0 (0) | 1 (1.6) | 1 (1.1) | |
| Neutral | 4 (14.8) | 7 (10.9) | 11 (12.1) | |
| Satisfied | 6 (22.2) | 27 (42.2) | 33 (36.3) | |
| Very satisfied | 17 (63.0) | 28 (43.8) | 45 (49.5) |
OSS, Oxford Shoulder Score; ASES, American Shoulder and Elbow Surgeons; ROM, range of motion; SD, standard deviation; ER, external rotation; IR, internal rotation.
Data are presented as number (percentage) unless otherwise indicated. Percentages are rounded to 1 decimal place.
Statistically significant difference (P < .05).
Data for IR while erect were missing in 14 cases.
Table IV.
Complications by glenosphere size
| Metal | Polyethylene |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C, concentric; GT, greater tuberosity; E, eccentric; DVT, deep vein thrombosis; ROM, range of motion.
Discussion
A biomechanical concern with the use of a larger glenosphere composed of polyethylene is that a stress riser occurs at the interface between the central metallic peg and the polyethylene glenosphere. This theoretically could lead to glenosphere breakage, especially given the semiconstrained nature of a reverse total shoulder joint replacement. Because of these concerns, the smaller 36-mm glenosphere is only manufactured in metal. Our series showed no adverse effects, breakages, or catastrophic failures in relation to the polyethylene glenosphere. Our study suggests that inversing the material in the articulation of the reverse shoulder prosthesis has a safety profile comparable to that of conventional metal glenospheres.
Scapular notching is a phenomenon unique to the reverse total shoulder arthroplasty, with some studies in the literature reporting rates as high as 50%-96%.3,5,21,28,31 Its clinical significance remains unclear, but its presence has been linked to lower functional scores and higher complication rates.18,23,26 To minimize scapular notching, the design of reverse total shoulder implants has evolved to include larger-diameter glenospheres as well as the option of glenosphere eccentricity. In addition, the larger SMR glenospheres are composed of polyethylene and are coupled with metal humeral liners. This design using a metal humeral liner decreases the polyethylene debris generated from the liner of the humeral cup when it impinges against the scapular neck.4
It is well documented that inferior scapular notching can extend beyond the inferior screw and progressively enlarge over time postoperatively, supporting the theory that although notching is initially mechanical in nature, its late progression may be biological.4 It is, in part, a result of osteolysis due to polyethylene debris generated from the mechanical impingement of the polyethylene humeral cup against the glenoid neck. When the larger SMR polyethylene glenospheres are used, the reciprocal humeral liner is metal. This configuration does not generate polyethylene debris when it impinges; this, in turn, may reduce osteolysis. In our cohort of patients who underwent radiographic analysis, we noted a decreased incidence of notching in the group with larger polyethylene glenospheres compared with the group with smaller metallic glenospheres at a minimum of 2 years’ follow-up. There was a similar trend in the cohort of patients who underwent radiographic follow-up at ≥5 years, but this did not reach statistical significance. This is likely a result of the small number of patients with longer follow-up in this cohort. The larger polyethylene glenosphere group also demonstrated a smaller mean notch size (3.7 mm vs. 5.0 mm). Multiple logistic regression analysis indicated that notching was less likely to occur among patients with polyethylene glenospheres when compared with the smaller metal glenosphere group (P = .026). This finding is in keeping with the work performed by Bloch et al1 using the same SMR implant system, although their study only compared the smallest 36-mm concentric and eccentric metal glenospheres with the largest 44-mm polyethylene glenosphere. Although some studies have found inferior outcomes and decreased ROM in the presence of notching, our analysis demonstrated no significant difference in the notched vs. un-notched groups.13, 14, 15 We acknowledge that this study was unable to determine whether, in fact, the glenosphere size or material, or a combination thereof, had the most significant effect on the incidence of notching. It was not possible to add glenosphere material and size in the same regression model owing to multicollinearity.
The relationship between glenosphere size and range of movement has been a subject of interest in the recent literature.15 Some authors have noted that eccentricity improved deltoid efficiency independent of glenosphere size while lowering joint reaction forces.24 In a previous biomechanical study, Chou et al7 demonstrated that larger glenospheres and eccentricity (2 mm) allowed a greater range of movement, with eccentricity having a greater effect on adduction. At the time of their study, the 44-mm glenospheres had an eccentricity of 2 mm, which was increased to 4 mm in late 2009. Our study, which included the glenospheres with higher eccentricity, showed no difference in the ROM or overall satisfaction rates. These results echo the findings of Müller et al17 in their retrospective analysis of 68 RSAs using the same SMR system. No difference was found between the 36- and 44-mm groups in terms of flexion, abduction, and internal or external rotation at 90° of abduction. They did, however, demonstrate better external rotation in adduction, as well as better abduction strength, in the group of patients with the larger-diameter glenosphere.
In addition to range of movement, we analyzed functional outcomes using the ASES score and OSS.9,22 Our results demonstrated better OSS values for the larger polyethylene glenosphere compared with the smaller metal glenosphere group at a minimum of 2 years’ follow-up. Although the difference in scores (ie, 2 points) was statistically significant, future research is necessary to ascertain what margin of difference in the OSS bears clinical significance.8 Regarding the ASES score, there was no significant difference between the 2 groups. Similarly, by use of the New Zealand national registry data, the OSS values of the 2 groups at 6 months and 5 years were compared and showed no significant difference (0.233 and 0.361, respectively).20 The overall satisfaction rates between the 2 bearing types were similar.
Rates of reported complications following RSA remain relatively high, with some studies citing rates between 19% and 75%.6,25,28 These complications include infection, instability, fracture, and neurologic injury. Infection rates have been reported to be between 1% and 10%, with Trappey et al28 reporting a 3% infection rate in a large, 280-patient single-surgeon cohort study. There was no significant difference in the complication rates between the 2 groups in our study, which could be attributed to the low rate of complications overall. Proven or suspected infection was only noted in the metal glenosphere cohort and represented 2 of the 12 shoulder-related complications. There were also 3 acromial stress fractures in this group. Greater tuberosity fracture or avulsion (n = 2) was the most common complication in the larger glenosphere group, which had no confirmed infections, although there were 2 patients with chronic stiffness. The low rate of infection in RSA patients makes it difficult to identify risk factors. Morris et al16 found that younger patient age and revision arthroplasty were associated with higher infection rates after bivariate and multivariable logistic regression analyses of 301 patients undergoing RSA. Smoking, obesity, rheumatoid arthritis, and diabetes did not prove to be risk factors in their series. The 40- and 44-mm glenospheres are composed of polyethylene and are solid, whereas the metal 36-mm glenosphere has a hollow backside. We postulated that the reduction in dead space may potentially lead to a reduction in infection. The rate of proven infection in our series was too small (n = 2) to adequately assess for statistical significance between the 2 types of glenospheres. The New Zealand national joint registry data recorded no revisions for deep infection in either glenosphere group. Although the literature has reported dislocation rates between 2% and 31% for RSA, we recorded no dislocations in our series of patients. Analysis of the New Zealand national joint registry data revealed 2 revisions for dislocation in the smaller metal glenosphere group, but this was not statistically significant. Most patients in our series underwent repair of the subscapularis tendon, which has been shown to halve the number of dislocations after RSA.11
The main weaknesses of this study are its retrospective nature and the substantial number of patients lost to follow-up. As mentioned earlier, the study is unable to separately analyze the effects of the bearing size and material on notching. The study’s strengths include representing data from a single center, using only 1 type of prosthesis, controlling for implant and surgical technique variables. This report also demonstrates the safety and clinical results of an inverted-material RSA. Currently, there is a paucity of publications on inverted material in RSA in the literature.
Conclusion
Our study has shown that larger polyethylene glenospheres are a safe option with no recorded glenosphere implant failures in 145 patients with a minimum of 2 years’ radiographic follow-up. The larger polyethylene glenospheres decreased the incidence and size of early notching when compared with the smaller metal glenospheres. They were also associated with a statistically significant improvement in OSS values. A larger study with a longer duration of follow-up is necessary to assess the individual effects of bearing size and material on notching rates as well as functional scores.
Disclaimer
Support in the form of funding for data analysis was provided by LimaCorporate. Although LimaCorporate provided funding for auditing of the 10-year data in this study, all data collection and manuscript preparation were conducted independently.
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors thank Mustafa Saffi and Yee Sing for their contribution to the initial data capture for this study.
Footnotes
North Shore Hospital institutional approval was granted (no. RM14048). North Shore Hospital’s Ethical Committee was consulted regarding the need for ethical approval: As this study used data from the standard clinic follow-up of patients after reverse shoulder arthroplasty, the committee classified this study as an audit and consequently advised that no ethical approval was necessary. A similar decision was made by the Health and Disability Ethics Committee of New Zealand. The data reported in this study were just a small part of a much larger database that formed part of our auditing process to ensure good clinical practice. Patients are not required to complete any consent for use of their unidentified data.
References
- 1.Bloch H., Budassi P., Bischof A., Agneskirchner J., Domenghini C., Frattini M. Influence of glenosphere design and material on clinical outcomes of reverse total shoulder arthroplasty. Shoulder Elbow. 2014;6:156–164. doi: 10.1177/1758573214535574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P., Moineau G., Roussanne Y., O’Shea K. Bony increased-offset reversed shoulder arthroplasty minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011;469:2558–2567. doi: 10.1007/s11999-011-1775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boileau P., Watkinson D., Hatzidakis A., Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:S147–S161. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P., Watkinson D., Hatzidakis M., Hovorka I. The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Boulahia A., Edwards T., Walch G., Baratta R. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2000;25:129–133. doi: 10.3928/0147-7447-20020201-16. [DOI] [PubMed] [Google Scholar]
- 6.Cheung E., Willis M., Walker M., Clark R., Frankel M. Complications in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2011;19:439–449. [PubMed] [Google Scholar]
- 7.Chou J., Malak S., Anderson I., Astley T., Poon P. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: range of motion and risk of scapular notching. J Shoulder Elbow Surg. 2009;18:354–359. doi: 10.1016/j.jse.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Christiansen D., Frost P., Falla D., Haahr J., Frich L., Svendsen W. Responsiveness and minimal clinically important change: a comparison between 2 shoulder outcome measures. J Orthop Sports Phys Ther. 2009;45:620–625. doi: 10.2519/jospt.2015.5760. [DOI] [PubMed] [Google Scholar]
- 9.Dawson J., Fitzpatrick R., Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br. 2009;78-B:593–600. doi: 10.1302/0301-620X.78B4.0780593. [DOI] [PubMed] [Google Scholar]
- 10.De Wilde L., Poncet D., Middernacht B., Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop. 2010;81:719–726. doi: 10.3109/17453674.2010.538354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards T., Williams M., Labriola J., Elkousy H., Gartsman G., O’Connor D. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:892–896. doi: 10.1016/j.jse.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Helmkamp J., Bullock G., Amilo N., Guerrero E., Ledbetter L., Sell T. The clinical and radiographic impact of centre of rotation lateralization in reverse shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018;27:2099–2107. doi: 10.1016/j.jse.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Lévigne C., Garret J., Boileau P., Alami G., Favard L., Walch G. Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res. 2011;469:2512–2520. doi: 10.1007/s11999-010-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mollon B., Mahure S., Roche C., Zuckerman J. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg. 2017;26:1253–1261. doi: 10.1016/j.jse.2016.11.043. [DOI] [PubMed] [Google Scholar]
- 15.Mollon B., Mahure S., Roche C., Zuckerman J. Impact of glenosphere size on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 297 shoulders. J Shoulder Elbow Surg. 2016;25:763–771. doi: 10.1016/j.jse.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 16.Morris B., O’Connor D., Torres D., Elkousy H., Gartsman G., Edwards T. Risk factors for periprosthetic infection after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24:161–166. doi: 10.1016/j.jse.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 17.Müller A., Born M., Jung C., Flury M., Kolling C., Schwyzer H. Glenosphere size in reverse shoulder arthroplasty: is larger better for external rotation and abduction strength? J Shoulder Elbow Surg. 2018;27:44–52. doi: 10.1016/j.jse.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Nam D., Kepler C., Nho S., Craig E., Warren R., Wright T. Observations on retrieved humeral polyethylene components from reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:1003–1012. doi: 10.1016/j.jse.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Nelson R., Lowe J., Lawler S., Fitzgerald M., Mantell M., Jawa A. Lateralized centre of rotation and lower neck-shaft angle are associated with lower rates of scapular notching and heterotopic ossification and improved pain for reverse shoulder arthroplasty at 1 year. Orthopedics. 2018;41:230–236. doi: 10.3928/01477447-20180613-01. [DOI] [PubMed] [Google Scholar]
- 20.New Zealand Joint Registry The New Zealand Joint Registry: nineteen year report—January 1999 to December 2017. https://nzoa.org.nz/system/files/DH8152_NZJR_2018_Report_v6_4Decv18.pdf
- 21.Nyffeler R., Werner C., Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–528. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Richards R., An K., Bigliani L., Friedman R., Gartsman G., Gristina A. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 23.Roche C., Marczuk Y., Wright T., Flurin P., Grey S., Jones R. Scapular notching and osteophyte formation after reverse shoulder replacement. Bone Joint J. 2013;95-B:530–535. doi: 10.1302/0301-620X.95B4.30442. [DOI] [PubMed] [Google Scholar]
- 24.Scalise J., Jaczynski A., Jacofsky M. The effect of glenosphere diameter and eccentricity on deltoid power in reverse shoulder arthroplasty. Bone Joint J. 2016;98-B:218–223. doi: 10.1302/0301-620X.98B2.35912. [DOI] [PubMed] [Google Scholar]
- 25.Scarlat M.M. Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop. 2013;37:843–851. doi: 10.1007/s00264-013-1832-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simovitch R., Zumstein M., Lohri E., Helmy N., Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 27.Torrens C., Miquel J., Martínez R., Santana F. Can small glenospheres with eccentricity reduce scapular notching as effectively as large glenospheres without eccentricity? A prospective randomized study. J Shoulder Elbow Surg. 2020;29:217–224. doi: 10.1016/j.jse.2019.09.030. [DOI] [PubMed] [Google Scholar]
- 28.Trappey G., O’Connor D., Edwards T. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469:2505–2511. doi: 10.1007/s11999-010-1686-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Valenti P., Sauzières P., Katz D., Kalouche I., Kilinc A. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res. 2011;469:2550–2557. doi: 10.1007/s11999-011-1844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werner B., Holzgrefe R., Griffin J., Lyons M., Cosgrove C., Hart J. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23:e275–e282. doi: 10.1016/j.jse.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 31.Werner C., Steinmann P., Gilbart M., Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]