Abstract
Background
The glenoid labrum can be torn in 1 or more locations. It is undetermined if the location of the labral tear alters patient outcomes after repair.
Methods
A total of 252 labral repair cases were retrospectively reviewed using prospectively collected patient-ranked outcomes and examiner-determined assessments preoperatively, at 1 week, 6 weeks, 24 weeks, and at a minimum of 2 years after surgery.
Results
Preoperatively, patients who underwent a superior labral repair reported worse pain at night and during activity than patients who subsequently underwent an isolated anterior labral repair or a combined anterior and superior labral repair (P < .05). After surgery, patients who underwent an isolated superior labral repair reported more severe pain at night and during activity, increased stiffness, and less satisfaction with their shoulder than patients who had an isolated anterior (P < .05) or a combined anterior and superior labral repair (P < .05).
Conclusions
Patients with isolated superior labral repairs have more pain both before and after repair than patients who undergo anterior or anterior and superior labral repairs.
Keywords: Glenoid, labrum, tear, repair, SLAP, instability
The glenoid labrum is a fibrocartilaginous structure that runs circumferentially around the rim of the glenoid fossa.1,16 It provides stability to the glenohumeral joint by contributing approximately 50% of the depth of the glenoid and is an attachment site for the glenohumeral ligaments anteriorly and the long head of the biceps tendon superiorly.11 Tears can occur in the anterior labrum, superior labrum, posterior labrum, or any combination of the three.
Anterior labral lesions are the most common, involving the detachment of the anterior labrum from the underlying glenoid rim with variable involvement of the glenohumeral ligaments after traumatic anterior shoulder dislocations. Patients with anterior glenoid labral lesions typically complain of shoulder instability and pain, especially in the provocative position of humeral abduction and external rotation.5 Superior labral tears, often referred to as superior labrum from anterior to posterior lesions, involve the detachment of the superior labrum from the underlying glenoid rim with or without involvement of the long head of the biceps tendon.
Combined anterior and superior labral tears have also been observed during shoulder arthroscopies and are usually secondary to 1 or more traumatic anterior dislocations.4,8
Labral repair is a common management option for labral tears. It involves the reattachment of the labrum to the glenoid rim via bioabsorbable suture tacks, transosseous sutures, and/or suture anchors.2 Studies have examined the outcomes of a labral repair in patients who have undergone an isolated superior labral repair, an isolated anterior labral repair, or a combined anterior and superior labral repair and reported improvements in pain-related scores and global shoulder scores from preoperatively to postoperatively.3,6,8,9,19,20
Previous studies on labral repairs have only compared functional outcomes of isolated anterior labral repairs with combined anterior and superior labral repairs and have found no difference in patient-reported outcomes between the lesions both preoperatively and postoperatively.4,8,10 Several authors have reported that patients with combined anterior and superior lesions have exhibited decreased range of shoulder motion after surgery compared with patients who had an isolated anterior labral repair.7,10
Nashikkar et al14 compared patients who underwent an isolated superior labral repair with those who had a combined anterior and superior labral repair, finding that patients with isolated superior labral tears were 7 times more likely to have signs of a retorn labrum on computed tomography arthrography than patients who underwent a combined anterior and superior labral repair. However, they found no difference in global shoulder outcomes between isolated superior labral repair patients and combined anterior and superior labral repair patients, nor between patients who had radiographic signs of labral healing and those that were retorn. However, their sample size was small, consisting of 28 patients in the isolated superior labral repair group and 15 in the combined anterior and superior labral repair group. Patient range of shoulder motion was not analyzed.14
To our knowledge, no studies have examined if the location of a labral lesion (anterior, superior, or combined anterior and superior) affects patient outcomes after repair. The purpose of this study therefore was to determine if the location of a labral repair (anterior, superior, or combined anterior and superior) affects patient outcomes after repair, specifically the patient's overall shoulder satisfaction at more than 2 years after repair.
Materials and methods
Study design
A retrospective cohort study was performed using prospectively collected data.
Inclusion and exclusion criteria
Patients were included in this study if they underwent an arthroscopic repair of a superior labral lesion and/or an anterior labral tear between January 2007 and May 2017. Patients were excluded if the surgery was a revision labral surgery or they had never answered the shoulder function assessment questionnaire; glenohumeral arthritis (of grade II or greater as per Outerbridge classification)17; concurrent fracture of the humerus, scapula, or clavicle; biceps tenodesis; calcific débridement; or rotator cuff repair. Patients who met the inclusion criteria were contacted via letter and telephone and asked to complete an assessment either at the clinic or via telephone if they were unable to attend a clinic appointment. Post hoc patients were then allocated to groups according to whether they had an isolated superior labral repair, an isolated anterior labral repair, or a combined anterior and superior labral repair. Anterior labral tears were defined as detachment of the glenoid labrum from the glenoid rim anywhere between 3 and 5 o'clock on a superimposed clockface.
Patient assessment
At presentation, each patient completed a questionnaire asking when the problem began, whether it was related to a specific injury, and whether it was work related.
Shoulder function
Preoperatively and at 1 week, 6 weeks, 6 months, and more than 2 years postoperatively, patients answered a standardized questionnaire that was based on the L'Insalata Shoulder Rating Questionnaire using a 5-point Likert scale.13 The questions appraised frequency of shoulder pain, level of shoulder pain, level of shoulder stiffness, difficulty with reaching the back, difficulty with overhead activities, and overall shoulder satisfaction.
Range of motion
Examiners measured passive shoulder range of motion preoperatively and at 6 weeks, 6 months, and more than 2 years postoperatively. The ranges of external rotation, forward flexion, abduction, and internal rotation were determined visually, according to a previously validated protocol.18
Operative procedure and rehabilitation
All operations were performed by the senior author (G.A.C.M.). Surgeries were performed with the patient in the beach chair position under general anesthesia and local interscalene nerve block. A standard posterior viewing portal was established followed by a routine diagnostic examination of the joint.
Labral lesions were repaired via the transrotator cuff technique described by O'Brien et al.15 An anterior superior portal and a transrotator cuff portal were established under direct visualization with the use of a spinal needle (outside-in technique). After skin incision, a 5.5-mm disposable cannula was inserted. The superior anterior portal was created anterior to the long head of the biceps in the rotator cuff interval. The transrotator cuff portal was created posterior from the biceps tendon, medial from the rotator cuff ligament. Next, a stab incision was made longitudinal to the supraspinatus tendon and the trocar was introduced.
A probe was used to determine the amount of labrum detachment and documented clockwise. Scar tissue was detached and the outer edge of the glenoid rim was roughened using an arthroscopic rasp. A Spectrum suture passer was used to pass a nylon 3.0 suture through the labrum. An arthroscopic grabber was used to pick up the wire through the second portal. Next, a FiberWire, 38″ blue (Arthrex) was tied to the nylon suture and shuttled through the labrum. An arthroscopic drill guide was inserted (Arthrex, Naples, FL, USA) and positioned on the edge of the glenoid at a 30°-45° angle anterior of the posterior border of the labral lesion. A hole was drilled using a 2.9-mm PushLock drill. The FiberWire, 38″ blue was connected to the suture anchor followed by insertion of the anchor according to the manufacturer's manual. As many suture anchors as necessary were used to create a stable labrum and biceps anchor. The number of suture anchors used was noted as well as their positions in regard to the glenoid. After fixation of the labrum, the cannulas were removed.
Postoperative management
All patients with a labral repair underwent a standardized rehabilitation program. The patients were asked to wear a sling for 6 weeks. On day 1, the patients started with pendulum exercises of the arm and scapular strengthening. In the second week, patients were allowed to passively flex the shoulder. This was followed by passive horizontal flexion stretching and shoulder extension from 3 to 6 weeks postoperatively. At 6 weeks postoperatively, the patients were assessed and instructed by a physical therapist for phase II of our rehabilitation protocol from 6 weeks to 3 months postoperatively. In phase II, actively supported external rotation was initiated together with isometric strengthening exercises. At 3 months postoperatively, the patients were seen by a physical therapist and were instructed to start phase III exercises until 6 months postoperatively. Phase III consisted of active theraband exercises consisting of rowing, external rotation, internal rotation, adduction, and shoulder extension as well as straight arm lifts. The rehabilitation protocol concluded at 6 months after surgery.
Statistical analysis
All statistical analyses were performed on an intent-to-treat basis. Comparisons were made between isolated superior labral repair, isolated anterior labral repair, and combined anterior and superior labral repair cohorts at each time point using a 1-way analysis of variance for parametric data and the Kruskal-Wallis test for nonparametric data with post hoc analysis.
Multiple regression analysis was used to determine the contribution of preoperative and intraoperative variables to overall shoulder satisfaction at more than 2 years after surgery. For this analysis, overall shoulder satisfaction was the dependent variable, and all demographic and preoperative patient-ranked outcomes, examiner-assessed range of motion, and intraoperative data were included as potential independent variables. The level of significance was set at P < .05 for all statistical analyses.
Results
Study group
Between January 2007 and May 2017, 348 labral repairs were performed by a single surgeon. Of these, 45 were excluded for being labral repair revisions, 5 for the presence of glenohumeral arthritis that was grade II or greater, 30 for concurrent rotator cuff repair, and 2 for concurrent calcific débridement. A total of 14 patients failed to answer the shoulder function questionnaire. This left 252 shoulders (250 patients) (Fig. 1). These patients formed the study cohort. In this cohort, 65 had an isolated superior labral repair, 129 an isolated anterior labral repair, and 58 a combined anterior and superior labral repair.
Figure 1.
Patient selection flowchart.
Cohort demographics
The demographics of the 3 groups are outlined in Table I. Patients who underwent an isolated superior labral repair were older and more likely to report a work-related injury than the isolated anterior labral repair and combined anterior and superior labral repair patients (P < .05). There were no other differences between the 3 groups with respect to gender, time from symptom onset to surgery, affected shoulder, or time from surgery to final follow-up.
Table I.
Demographic characteristics of superior labral repair, anterior labral repair, and combined anterior and superior labral repair
| Superior repair group | Anterior repair group | Combined repair group | P value | |
|---|---|---|---|---|
| Sex (n), male:female | 58:7 | 106:25 | 52:6 | .1 |
| Age at surgery, mean (range) | 37 (18-57) | 26 (12-55) | 30 (18-52) | <.05∗ |
| Time from symptom onset to surgery (mo), mean ± SEM (range) | 27 ± 6 (1-259) | 43 ± 5 (0-354) | 40 ± 7 (0-299) | .2 |
| Affected shoulder left:right (n) | 25:40 | 68:61 | 23:35 | .1 |
| Follow-up (yr), mean ± SEM (range) | 4 ± 0.3 (2-11) | 4 ± 0.2 (2-11) | 4 ± 0.3 (2-7) | .97 |
| Work related (%) | 48 | 14 | 26 | <.05† |
SEM, standard error of the mean.
Patient age was statistically different between each group (P < .05).
Isolated superior labral repair patients were more likely to have work-related injuries than anterior labral repair or combined anterior and superior labral repair patients (P < .05).
Intraoperative group data are illustrated in Table II. On average, 2 anchors were used in isolated superior labral repairs, 3 in anterior labral repairs, and 4 in combined anterior and superior labral repairs (P < .05). Patients who had a combined anterior and superior labral repair had longer operations than the anterior labral repair and superior labral repair patients (39 vs. 28 and 27 minutes, respectively, P < .05).
Table II.
Operative data of superior labral repair, anterior labral repair, and combined anterior and superior labral repair groups
| Superior repair group | Anterior repair group | Combined repair group | P value | |
|---|---|---|---|---|
| Number of anchors used, mean (range) | 2 (1-5) | 3 (1-4) | 4 (2-6) | <.0001∗ |
| Operation time (min), mean ± SEM (range) | 28 ± 2 (9-70) | 28 ± 1 (7-60) | 39 ± 2 (18-120) | <.0001† |
SEM, standard error of the mean.
All groups' numbers of anchors used were significantly different from each other (P < .0001).
Combined anterior and superior labral repair cases had significantly longer operation times than superior and anterior labral repair groups (P < .0001).
Functional outcomes
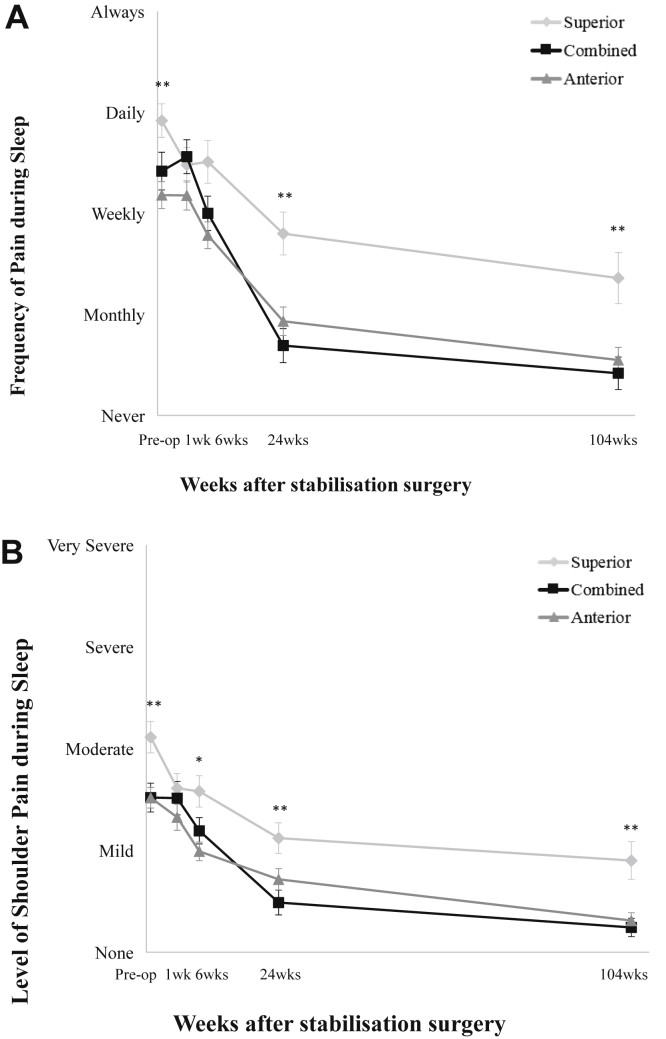
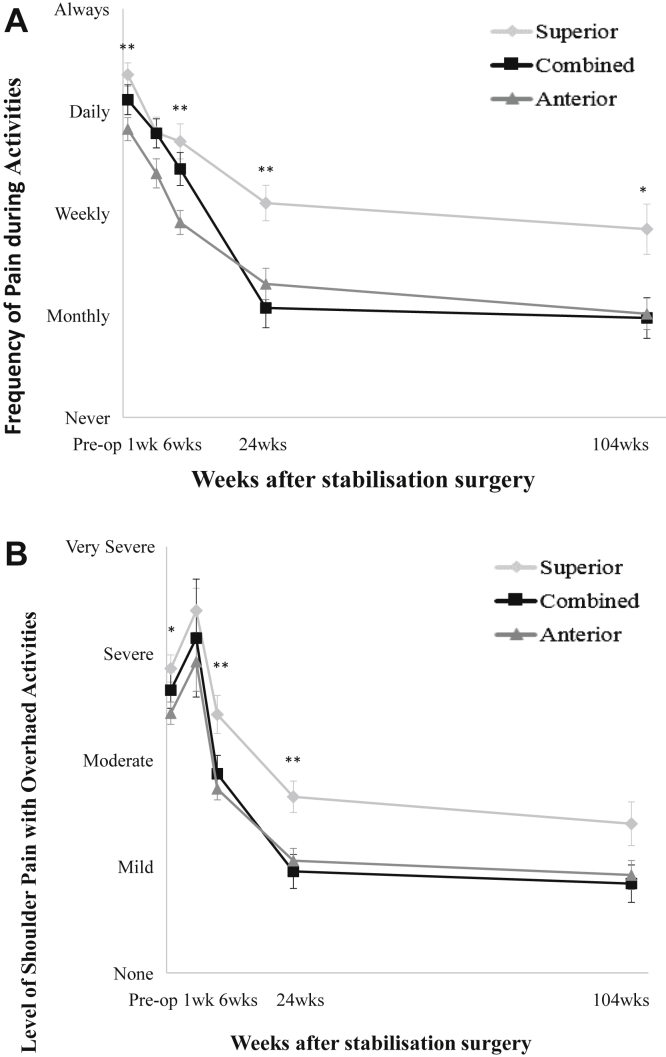
Preoperatively, patients who had an isolated superior labral repair reported more frequent and severe night pain and pain with activities than patients who underwent an isolated anterior labral repair (Figs. 2 and 3).
Figure 2.
(A) Frequency and (B) level of shoulder pain during sleep in patients who underwent anterior stabilization, superior labral repair, or combined anterior and superior labral repair. ∗P < .05; ∗∗P < .01. Comparisons were made using 1-way analysis of variance with post hoc analysis.
Figure 3.
(A) Frequency and (B) level of pain during activities in patients who underwent anterior labral repair, superior labral repair, or combined anterior and superior labral repair. ∗P < .05; ∗∗P < .01. Comparisons were made using 1-way analysis of variance with post hoc analysis.
At 6 weeks, 6 months, and more than 2 years after surgery, patients who had an isolated superior labral repair also reported more frequent and more severe pain at night and with activities than patients who had an isolated anterior labral repair or who had a combined anterior and superior labral repair (Figs. 2 and 3).
Stiffness and range of motion
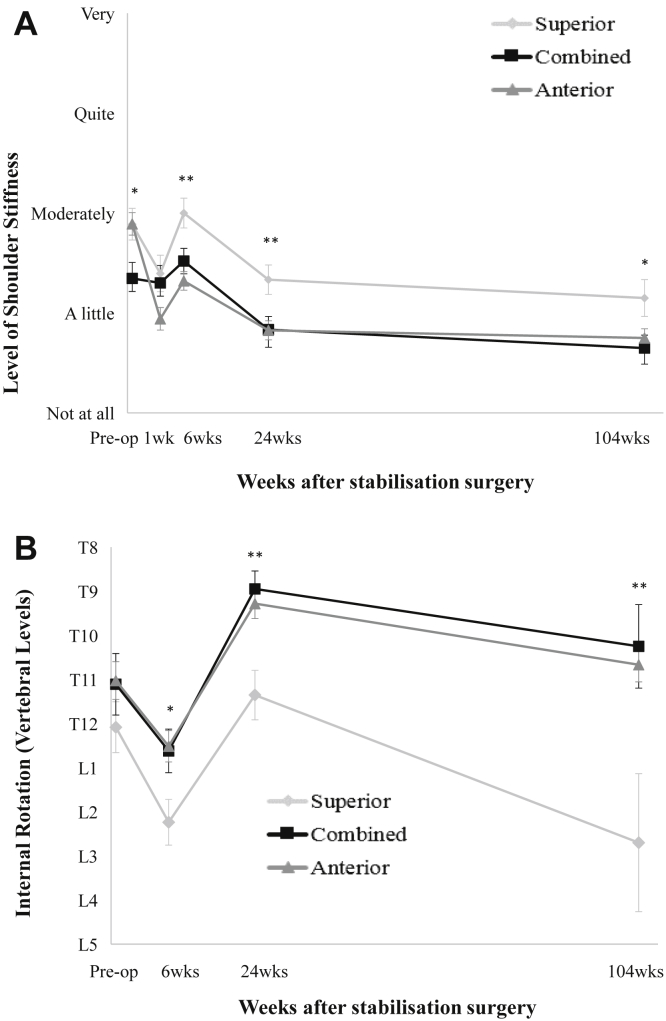
Patients who underwent a combined anterior and superior labral repair before surgery reported less stiffness than patients who had an isolated superior labral repair (P = .045) or an isolated anterior labral repair (P = .02).
Patients who underwent an isolated superior labral repair reported more stiffness at 6 weeks, 6 months, and more than 2 years after surgery than patients who had an isolated anterior labral repair or who had a combined anterior and superior labral repair (Fig. 4, A).
Figure 4.
(A) Level of shoulder stiffness and (B) internal rotation range of shoulder motion in patients who underwent anterior labral repair, superior labral repair, or combined anterior and superior labral repair. ∗P < .05; ∗∗P < .01. Comparisons were made using the Kruskal-Wallis test for nonparametric data and 1-way analysis of variance for parametric data with post hoc analysis.
After the labral repair, there was a transient loss of shoulder motion at 6 weeks that was restored by 6 months. Patients who underwent an isolated superior labral repair demonstrated reduced range of shoulder motion in internal rotation at 6 weeks, 6 months, and more than 2 years postoperatively compared with patients who underwent an isolated anterior labral repair or had a combined anterior and superior labral repair (Fig. 4, B).
At more than 2 years postoperatively, the isolated superior labral repair group had less forward flexion shoulder range of motion than the anterior labral repair and combined anterior and superior labral groups (P < .05).
There were no significant differences in range of shoulder motion between anterior labral repair and combined anterior and superior labral repair patients.
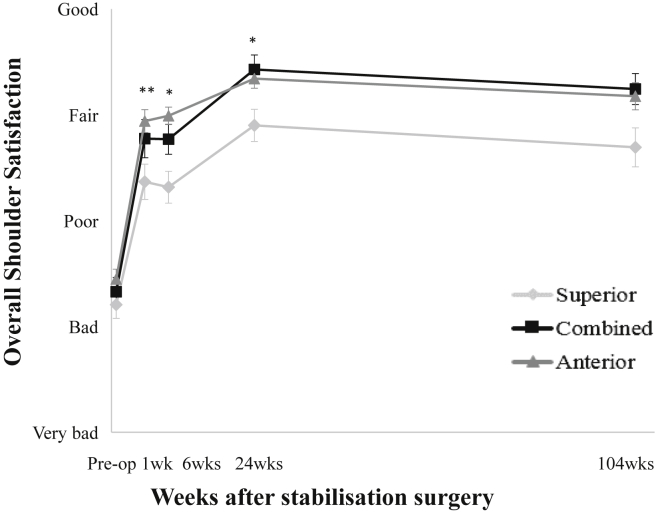
Overall shoulder satisfaction
Preoperatively, there was no difference in overall shoulder satisfaction between groups (P > .05).
Beginning at 1 week and continuing at 6 weeks and 6 months after surgery, patients who had an isolated superior labral repair reported less satisfaction with their shoulders than patients who had undergone an isolated anterior labral repair or who had a combined anterior and superior labral repair (Fig. 5).
Figure 5.
Overall shoulder satisfaction of patients who underwent anterior labral repair, superior labral repair, or combined anterior and superior labral repair. ∗P < .05; ∗∗P < .01. Comparisons were made using 1-way analysis of variance with post hoc analysis.
Regression analysis
Multiple regression analysis was used to determine which preoperative and intraoperative factors were predictive of overall shoulder satisfaction at more than 2 years after repair. Patients who preoperatively experienced less pain with overhead activity, had more frequent extreme pain and pain at rest, and were less satisfied with their shoulder were more likely to have less satisfaction with their shoulders at more than 2 years postoperatively (P < .05). Patient demographics, time from symptom onset to surgery, nature of injury, whether it was work related, operative time, number of anchors, and range of shoulder motion were not predictive of isolated superior labral repair patients' overall shoulder satisfaction at more than 2 years postoperatively.
Discussion
The study showed that patients with isolated superior labral lesions had more shoulder pain before surgery than patients with anterior labral lesions, or those who had combined anterior and superior labral lesions. After surgery, patients who underwent an isolated superior labral repair had more pain, shoulder stiffness, and were less satisfied with their shoulders than patients who had undergone an isolated anterior labral repair or who had a combined anterior and superior labral repair.
Before and after repair, patients with superior labral repairs reported more severe pain with activities and during sleep than patients who had undergone an isolated anterior labral repair or a combined anterior and superior labral repair. Several studies have compared isolated anterior labral repairs with combined anterior and superior labral repairs, generally finding no difference between the 2 lesions in regard to patient-reported outcomes.4,7,8,10 We also found no difference between patients who underwent an isolated anterior labral repair and those who had a combined anterior and superior repair, with the only difference being that combined anterior and superior labral repairs had less shoulder stiffness preoperatively.
Only one other study, Nashikkar et al,14 directly compared isolated superior labral lesions with combined anterior and superior labral lesions. Unlike our study, they found no difference between the 2 labral lesions in patient-reported outcomes, measured using a Constant score and pain visual analog scale, though their surgical technique of using bioabsorbable suture anchors and not placing anchors anterior to the biceps tendon in superior labral repairs differed to that used in our study, where anchors were placed as needed and non-bioabsorbable anchors were used. Nashikkar et al14 did also find that isolated superior labral repairs were 7 times more likely than combined anterior and superior labral repairs to have signs on computed tomography arthrography of failed healing at minimum 1 year after repair. In a study comparing an isolated superior labral repair with a superior labral repair with concomitant pathology in a military population, Waterman et al21 found that the presence of concomitant injury including anterior labral tears was associated with a decreased risk of revision surgery (P = .01).
We hypothesize that combined anterior and superior labral lesions are essentially large anterior labral tears. Both anterior and combined anterior and superior labral tears are predominantly secondary to a traumatic anterior dislocation. The pathogenesis of superior labral tears and the surgical outcomes are different.
In our study, patients who had a combined anterior and superior labral repair had similar range of shoulder motion as or better range of shoulder motion than patients who underwent an isolated anterior or superior labral repair. In a retrospective study examining 15 anterior labral lesions and 15 combined anterior and superior labral lesions, Cho et al7 found that combined lesions had a restricted range of shoulder motion in forward flexion and external rotation compared with the isolated anterior lesions at 6 and 9 weeks postoperatively (P < .05). By 12 weeks after surgery, there was no difference.7 We found no difference in any shoulder range of motion between the anterior labral or combined anterior and superior labral lesions. The difference in our study's results regarding shoulder range of motion between anterior and combined anterior and superior labral repairs compared with Cho et al may be due to differing surgical techniques and anchor placement. However, we did find that patients who underwent a superior labral repair exhibited increased loss of internal rotation shoulder range of motion postoperatively when compared with patients who underwent an isolated anterior labral repair or a combined anterior and superior labral repair. Although isolated superior labral repair patients regained their preoperative internal rotation range of motion by 6 months, they still exhibited less range of internal rotation than anterior or combined anterior and superior labral repairs.
Our results that combined anterior and superior labral lesions did not have worse patient outcomes than either isolated anterior or isolated superior labral lesions concur with the current literature that larger labral lesions are not associated with poor outcomes. In a 2013 study, Kim et al12 examined patients who underwent an anterior labral repair, patients who underwent a combined anterior and superior labral repair, and patients who underwent a circumferential-labral repair and found no difference in functional outcomes between lesions. Studies analyzing functional outcomes based on the size of the lesion using a clockface measurement may help confirm that lesion size does not affect patient-reported outcomes.
The strengths of this study were its high internal validity, with all labral tears being diagnosed and repaired using the same technique and anchors by the same surgeon. Furthermore, almost all patient data were collected prospectively.
There were several potential limitations of this study that should be considered. There was a significantly higher rate of work-associated injuries, which are often associated with worse outcomes, in the superior labral repair group than the other labral repair groups, which may have contributed to the worse outcomes in the superior labral repair group, although logistic regression analyses did not show injury work status to be an independent predictor of overall shoulder satisfaction. Similarly, patients who underwent a superior labral repair were generally older than other labral repair patients, which may have contributed to the worse outcomes. We also cannot comment on patients who did not come to surgery.
Conclusions
Patients who underwent an isolated superior labral repair had more pain than patients with other labral repairs both before and after repair and more stiffness and less satisfaction in the early postoperative period (<6 months), suggesting that the superior labrum might be a particularly sensitive area.
Acknowledgments
The authors would like to thank Linda Dodd and Marina Zimmerman for their help with communication, organization, and assistance with the project.
Disclaimer
George A.C. Murrell is on the editorial or governing boards of Journal of Shoulder and Elbow Surgery, Shoulder and Elbow, and Techniques in Shoulder and Elbow Surgery; and is a paid consultant and receives research support from Smith & Nephew.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was received from the South Eastern Sydney Local Health District ethical committee (number 09/STG/85).
References
- 1.Alashkham A., Alraddadi A., Felts P., Soames R. Histology, vascularity and innervation of the glenoid labrum. J Orthop Surg (Hong Kong) 2018;26:1–7. doi: 10.1177/2309499018770900. [DOI] [PubMed] [Google Scholar]
- 2.Alpert J.M., Wuerz T.H., O'Donnell T.F., Carroll K.M., Brucker N.N., Gill T.J. The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med. 2010;38:2299–2303. doi: 10.1177/0363546510377741. [DOI] [PubMed] [Google Scholar]
- 3.Arroyo W., Misenhimer J., Cotter E.J., Wang K.C., Heida K., Pallis M.P. Effect of anterior anchor on clinical outcomes of type II SLAP repairs in an active population. Orthopedics. 2019;42:e32–e38. doi: 10.3928/01477447-20181102-04. [DOI] [PubMed] [Google Scholar]
- 4.Aydin N., Unal M.B., Asansu M., Tok O. Concomitant SLAP repair does not influence the surgical outcome for arthroscopic Bankart repair of traumatic shoulder dislocations. J Orthop Surg (Hong Kong) 2017;25 doi: 10.1177/2309499017718952. 2309499017718952. [DOI] [PubMed] [Google Scholar]
- 5.Bankart A.S. Recurrent or habitual dislocation of the shoulder-joint. Br Med J. 1923;2:1132–1133. doi: 10.1136/bmj.2.3285.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brockmeier S.F., Voos J.E., Williams R.J., III, Altchek D.W., Cordasco F.A., Allen A.A. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91:1595–1603. doi: 10.2106/jbjs.h.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho H.L., Lee C.K., Hwang T.H., Suh K.T., Park J.W. Arthroscopic repair of combined Bankart and SLAP lesions: operative techniques and clinical results. Clin Orthop Surg. 2010;2:39–46. doi: 10.4055/cios.2010.2.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Durban C.M., Kim J.K., Kim S.H., Oh J.H. Anterior shoulder instability with concomitant Superior Labrum from Anterior to Posterior (SLAP) lesion compared to anterior instability without SLAP lesion. Clin Orthop Surg. 2016;8:168–174. doi: 10.4055/cios.2016.8.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friel N.A., Karas V., Slabaugh M.A., Cole B.J. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19:859–867. doi: 10.1016/j.jse.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hantes M.E., Venouziou A.I., Liantsis A.K., Dailiana Z.H., Malizos K.N. Arthroscopic repair for chronic anterior shoulder instability: a comparative study between patients with Bankart lesions and patients with combined Bankart and superior labral anterior posterior lesions. Am J Sports Med. 2009;37:1093–1098. doi: 10.1177/0363546508331139. [DOI] [PubMed] [Google Scholar]
- 11.Howell S.M., Galinat B.J. The glenoid-labral socket. A constrained articular surface. Clin Orthop Relat Res. 1989:122–125. [PubMed] [Google Scholar]
- 12.Kim D.S., Yi C.H., Kwon K.Y., Oh J.R. Relationship between the extent of labral lesions and the frequency of glenohumeral dislocation in shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2013;21:430–437. doi: 10.1007/s00167-012-2045-z. [DOI] [PubMed] [Google Scholar]
- 13.L'Insalata J.C., Warren R.F., Cohen S.B., Altchek D.W., Peterson M.G. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79:738–748. [PubMed] [Google Scholar]
- 14.Nashikkar P.S., Rhee S.M., Desai C.V., Oh J.H. Is anatomical healing essential for better clinical outcome in type II SLAP repair? Clinico-radiological outcome after type II SLAP repair. Clin Orthop Surg. 2018;10:358–367. doi: 10.4055/cios.2018.10.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Brien S.J., Allen A.A., Coleman S.H., Drakos M.C. The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372–377. doi: 10.1053/jars.2002.30646. [DOI] [PubMed] [Google Scholar]
- 16.Ockert B., Braunstein V., Sprecher C.M., Shinohara Y., Milz S. Fibrocartilage in various regions of the human glenoid labrum. An immunohistochemical study on human cadavers. Knee Surg Sports Traumatol Arthrosc. 2012;20:1036–1041. doi: 10.1007/s00167-011-1686-7. [DOI] [PubMed] [Google Scholar]
- 17.Outerbridge R.E. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 18.Ronquillo J.C., Szomor Z., Murrell G.A.C. Examination of the shoulder. Tech Should Surg. 2011;12:116–125. doi: 10.1097/BTE.0b013e31823a10c6. [DOI] [Google Scholar]
- 19.Saper M.G., Milchteim C., Zondervan R.L., Andrews J.R., Ostrander R.V., III Outcomes after arthroscopic Bankart repair in adolescent athletes participating in collision and contact sports. Orthop J Sports Med. 2017;5:1–8. doi: 10.1177/2325967117697950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroder C.P., Skare O., Gjengedal E., Uppheim G., Reikeras O., Brox J.I. Long-term results after SLAP repair: a 5-year follow-up study of 107 patients with comparison of patients aged over and under 40 years. Arthroscopy. 2012;28:1601–1607. doi: 10.1016/j.arthro.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Waterman B.R., Arroyo W., Heida K., Burks R., Pallis M. SLAP repairs with combined procedures have lower failure rate than isolated repairs in a military population: surgical outcomes with minimum 2-year follow-up. Orthop J Sports Med. 2015;3:1–7. doi: 10.1177/2325967115599154. [DOI] [PMC free article] [PubMed] [Google Scholar]