Abstract
Background
Podoconiosis, lymphatic filariasis (LF) and leprosy are neglected tropical diseases (NTDs) that cause lymphoedema. When left untreated, they lead to substantial disability. This study determined the quality of life (QOL) and depression associated with lymphoedema in patients with podoconiosis, LF and leprosy. The study was conducted in northwestern Ethiopia.
Methods
This baseline cross-sectional study, nested within an interventional, non-comparative, longitudinal study, included patients with lymphoedema. Depression and QOL were assessed using versions of the 9-item Patient Health Questionnaire and Dermatologic Life Quality Index (DLQI), respectively, that had been translated into Amharic and validated. Factors associated with depression and QOL were assessed using multivariate linear regression analysis.
Results
Of the 251 patients with lymphoedema included in the study, 119 (47.4%) had moderate to severe depression and overall QOL was poor (mean±standard deviation [SD] DLQI score: 11.4±4.2). Disability was significantly associated with depression (β=0.26 [95% confidence interval {CI} 0.19 to 0.33]). Currently receiving treatment (β=−3.05 [95% CI −5.25 to −0.85), disability (β=−0.08 [95% CI −0.15 to −0.01]) and social support (moderate support: β=−2.27 [95% CI −3.66 to −0.89] and strong support: β=−2.87 [95% CI −5.35 to −0.38]) were significantly associated with better QOL.
Conclusion
High levels of depression and low QOL were found among patients with lymphoedema due the three NTDs in Ethiopia.
Keywords: depression, leprosy, lymphatic filariasis (LF), lymphoedema, podoconiosis, quality of life
Introduction
Lymphoedema is a chronic condition that affects the lymphatic system and manifests as swelling of body tissues, most frequently the legs and arms. In the tropics, lymphoedema is principally caused by podoconiosis, lymphatic filariasis (LF) and leprosy, which are neglected tropical diseases (NTDs).1 NTDs are primarily diseases of rural and some urban poor communities where there is usually a lack of access to basic healthcare services.2
Podoconiosis mainly affects barefoot farmers in tropical Africa, but it is also endemic in parts of Latin America and India.3 Podoconiosis arises as a result of interaction between environmental factors and genetic predisposition.4 Mineral particles from red clay soil are thought to induce macrophage activation and fibrosis, leading to lymphostasis, lymphatic obstruction and then progressive lymphoedema.5 Recurrent adenolymphangitis (ADL) is both a consequence of lymphoedema and a risk factor for the progression of lymphoedema. In Ethiopia, podoconiosis is endemic in 345 of 775 surveyed districts and is estimated to affect 1.5 million people with 34.9 million people at risk of the disease.6
The main clinical manifestations of LF are chronic lymphoedema of the legs or arms and hydrocele.7 Similar to podoconiosis, recurrent ADL is a risk factor for lymphoedema in patients with LF. LF is reported throughout the tropics, with the highest prevalence in Brazil and India and including East/Southeast Asia, Oceania and other parts of Africa and South America. It is estimated that globally there are 67.88 million cases of LF, including 36.45 million microfilaria carriers, 19.43 million hydrocele cases and 16.68 million lymphoedema cases.8 In Ethiopia, LF is endemic in 70 districts, with >5.9 million people at risk of acquiring the disease.9
Leprosy mainly affects the limbs, skin, peripheral nerves and eyes.10 In 2018 there were 184 212 cases globally on multidrug therapy, with a registered prevalence of 0.24 per 10 000 population.11 In the same calendar year, 22 countries reported new cases and nearly 11 323 new leprosy cases presented with grade II disability at the time of diagnosis.11 Grade I indicates loss of sensation but no visible deformity, while grade II disability implies there is visible damage or deformity.
The majority of cases were from the Southeast Asia region and Latin America.11 In Ethiopia, in 2015, there were 3758 new leprosy cases, of which 12.8% were children. Moreover, 10.2% of new cases of leprosy had grade II disability at diagnosis.12
The objective of this study was to characterize the baseline depression and quality of life (QOL) of people with lymphoedema due to podoconiosis, LF or leprosy in Ethiopia prior to assessment of the impact of an integrated holistic physical, mental health and psychosocial care package. Specifically, the study aims were to determine the prevalence of depression among people with lymphoedema due to podoconiosis, LF or leprosy; measure the QOL among people with lymphoedema caused by podoconiosis, LF or leprosy; and determine the sociodemographic factors that contribute to depression and QOL in this population.
Methods
Study description
The ‘parent’ study from which the data were derived, the Excellence in Disability Prevention Integrated across NTDs (EnDPoINT) project, has three phases: in phase 1, a holistic care package involving physical, mental health and psychosocial care was developed; in phase 2 the care package was piloted in one subdistrict; then, based on the findings of phase 2, phase 3 will scale up the care package in three districts. The data analysed here originate from phase 2 of the parent study, which also corresponds to phase 2 of the framework on complex interventions of the United Kingdom's Medical Research Council (MRC).13 According to this MRC framework, phase 1 is development of the package, phase 2 is feasibility piloting, phase 3 is evaluation and phase 4 is implementation. The phase 2 study was conducted in Gusha Health Centre, in one cluster of Guagusa Shikudad District (Gusha cluster), in Awi Zone, Amhara Region, northwestern Ethiopia. In a cluster there are five kebeles (subdistricts) and one health centre serving approximately 25 000 people.
Study design
A longitudinal non-comparative study was conducted. After baseline data collection, the holistic package of physical, mental health and psychosocial care was implemented. Data were collected at the 3-month follow-up and we hope to collect data at 12 months. Here we report on the baseline depression and QOL data of lymphoedema cases due to the three NTDs of interest.
Ethical approval was obtained from the Research Governance and Ethics Committee (RGEC) of the Brighton & Sussex Medical School (reference number: ER/BSMS9D79/2) and the College of Health Sciences, Addis Ababa University Institutional Review Board (IRB) (reference number: 061/18/CDT). Written informed consent was obtained from study participants, who were informed that they were free to withdraw from the study at any stage.
Study area and population
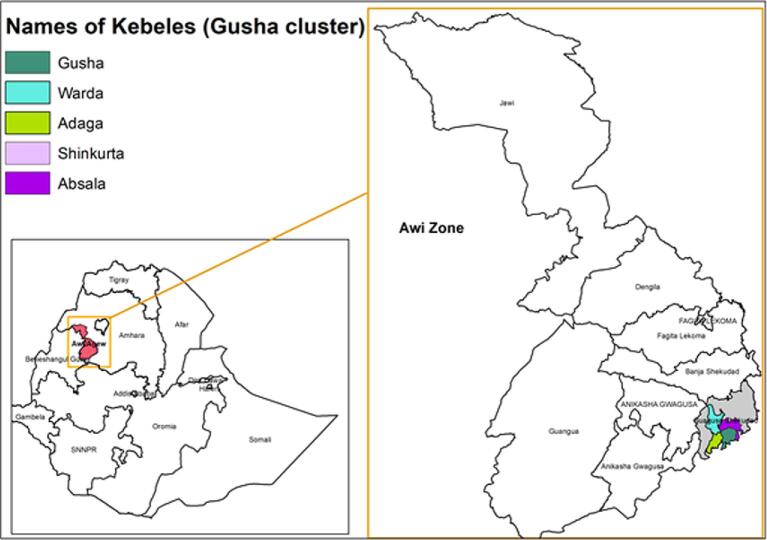
The study was conducted in the Gusha cluster of the Awi Zone, which is divided into seven districts and is one of 10 zones of the Amhara Region, northwestern Ethiopia (Figure 1). This zone was selected as it is co-endemic for the three NTDs of interest and, to date, few interventions addressing these diseases have been implemented there.
Figure 1.
Map of Ethiopia, Amhara Region, including Guagsa Shikudad District (Gusha cluster) in the Awi Zone.
Adults (≥18 y of age) with lower limb lymphoedema caused by LF, podoconiosis and/or leprosy were identified by community health extension workers during routine home visits and linked with Gusha Health Centre. Patients who gave their informed consent were eligible for inclusion in the study. Patients were excluded from the study if they expected to leave the study site during the study period, had nodular disease preventing the use of shoes (these individuals were referred for nodulectomy) or had complex wounds (these individuals were referred for specialist care in Injibara Hospital).
Data collection and management
Experienced data collectors were recruited and trained on how to use the study tools and how to extract information from both written and electronic health records. These trained community data collectors administered the validated questionnaires that had been translated into the local language of Amharic.
Regular supervision of the data collection process was carried out by the investigating team. Onsite supervision and feedback were given to the data collectors. All completed questionnaires and tools were checked for consistency, completeness, clarity and accuracy. Data were collected by smartphone using Open Data Kit, free software developed to allow data collection using Android mobile devices and data submission to an online server. After collection, data were transferred to an Excel (Microsoft, Redmond, WA, USA) data sheet for cleaning and verification, before being exported to Stata version 14 (StataCorp, College Station, TX, USA) for analysis.
Patient demographics (sex, age) and socio-economic characteristics (residence, education level, marital status, children, religion, employment status and relative income) were recorded at baseline using a pretested structured questionnaire.
The following physical and clinical characteristics were also measured using a validated questionnaire: history and frequency of acute attacks of lymphoedema and degree of disability. In addition, the following psychosocial outcomes were assessed: QOL, alcohol use disorder, social support and mental health condition of the participants, including depression, suicidal ideation and attempted suicide.
Assessment tools
We have read recent discussions about assessment tools of QOL in lymphoedema14,15 and have chosen the Dermatology Life Quality Index (DLQI) as suitable for our purpose.
QOL was assessed using the DLQI.16 It consists of 10 questions covering several dimensions of life quality, including pain, embarrassment, interference with activities of daily life and social and sexual relationships. Low DLQI scores suggest high QOL. DLQI has been used in patients with filarial lymphoedema in Guyana17 and India.18 It has been validated and translated into the official Ethiopian language, Amharic,19 and used to assess QOL in podoconiosis patients in southern Ethiopia.
Disability was measured using the World Health Organization Disability Assessment Schedule tool (the 12-item WHODAS version 2.0).20 The WHODAS was developed to measure disability and to assess the following: standing for long periods (e.g. 30 min), taking care of household responsibilities, learning a new task, joining community activities, effect of health problems on emotions, concentrating for 10 min, walking a long distance (1 km or equivalent), getting dressed, maintaining a friendship and maintaining day-to-day work. It has been translated into Amharic and used to assess disability due severe mental disorders in rural Ethiopia.21
Depression was assessed using the 9-item Patient Health Questionnaire (PHQ-9).22 It is a widely used depression screening scale for primary healthcare settings in high-income countries and has also been validated in low- and middle-income countries (LMICs).23 The nine items of the PHQ follow the Diagnostic and Statistical Manual (DSM) version IV diagnostic criteria for a depressive episode. Each question requires participants to rate the frequency of a depressive symptom experienced in the 2 weeks prior to evaluation. These items include little interest or pleasure in doing things, depressed mood, insomnia or hypersomnia, fatigue, appetite disturbances, guilt or worthlessness, diminished ability to concentrate, psychomotor agitation and suicidal thoughts. The total PHQ-9 score ranges from 0 to 27.22 In Ethiopia it has been translated into Amharic and used to detect depression in primary care settings.24,25
Alcohol use disorder was evaluated using the Fast Alcohol Screening Test (FAST).26 It is derived from the Alcohol Use Disorder Identification Test (AUDIT) and can be easily administered in 1 min. The items in FAST include: How often do you have eight or more drinks (six or more drinks for women) on one occasion? In the past year, how often have you been unable to remember what happened the night before because you had been drinking? Have you failed do what was normally expected of you because of drinking? Has a relative or friend, or a doctor or other health worker, been concerned about your drinking or suggested you cut down? The score ranges from 0 (never) to 4 (daily or almost daily). A score ≥3 out of 16 indicates hazardous alcohol use, a form of drinking that is related to increased risk of adverse psychological or physical consequences in the future.27,28 The FAST has also been translated into Amharic and used in assessing the burden of alcohol use disorder in rural Ethiopia.29 It has good psychometric properties, with sensitivity of 93% and specificity of 88%,27 which is comparable to the AUDIT.30 Local alcoholic beverages were converted into standard equivalent alcohol units when reported by the respondents using different containers such as flasks, cans and glasses.
Suicidal ideation and suicide attempts were measured using the Composite International Diagnostic Interview (CIDI) scale. There are four main questions: During the past 1 month: Did you think a lot about death?; Did you feel so low you thought a lot about committing suicide?; Did you make a plan as to how you might do it?; Did you attempt suicide?31 This CIDI has been used to measure suicidal ideation and suicide attempts among human immunodeficiency virus (HIV)-infected individuals.32 The CIDI was also used in studies in the community and primary health facilities in LMICs, including Ethiopia, with the study aim of determining the 12-month prevalence of suicidal ideation, plans and attempts, as well as associated risk factors.31
Social support was measured using the Oslo Social Support tool (Oslo-3),33 a very brief scale that assesses the number of close confidantes, perceived level of concern from others and perceived ease of getting help from neighbours. The total score ranges from 3 to 14 and higher scores represent better social support. The scores can be categorized in three levels: 3–8, poor social support; 9–11, moderate social support; and 12–14, strong social support.33 The internal consistency in a population based in Germany was 0.64, which was considered acceptable, as the scale is very brief with only three items.33 The Oslo-3 scale has been used in Ethiopia in a study that examined the prevalence of and factors associated with depression among patients with HIV/acquired immunodeficiency syndrome (AIDS),34 as well as a study addressing the prevalence and predictors of depression among pregnant women.35
Data analysis
Descriptive analysis was performed for sociodemographic factors, clinical and psychosocial explanatory factors and outcome variables.
Depression (measured using the PHQ-9) and QOL (measured using DLQI) were the primary outcome measures. There are four categories of depression, based on severity, using PHQ-9 cut-offs: <5, no depression; 5–9, mild depression; 10–14, moderate depression; 15–19, moderately severe depression; and 20–27, severe depression.22 For diagnosis of depression, PHQ-9 with a cut-off of 10 has shown good sensitivity and specificity, however, a cut-off of 5 had lower sensitivity and specificity.25 The best DLQI score is 0 and the worst score is 30.16
Linear regression analysis was used to examine the association between explanatory variables and depression measured by the PHQ-9 and QOL measured by DLQI. For both the PHQ-9 and DLQI, explanatory variables with an association of p < 0.2 in the bivariate analysis were included in the multivariate linear regression model. In the multivariate linear regression model, those explanatory variables with association at p<0.05 were considered statistically significant.
Results
Demographics and socio-economic characteristics at baseline
A total of 251 patients with lymphoedema associated with LF, podoconiosis or leprosy were included in the study. Their mean age was 51.9 y (range 18–88) (Table 1). Among the study participants, 52.6% were female, 99.6% lived in a rural area, 66.2% were illiterate, 67.7% were married, all were Orthodox Christians and 77.3% were farmers (Table 1).
Table 1.
Demographics and socio-economic characteristics of patients with lymphoedema participating in the study (N=251)
| Characteristics | Values |
|---|---|
| Sex, n (%) | |
| Female | 132 (52.6) |
| Male | 119 (47.4) |
| Residence, n (%) | |
| Urban | 1 (0.4) |
| Rural | 250 (99.6) |
| Age (years), mean (range) | 51.9 (18–88) |
| Age category (years), n (%) | |
| 18–24 | 10 (4.0) |
| 25–34 | 25 (10.0) |
| 35–44 | 40 (15.9) |
| 45–54 | 55 (21.9) |
| 55–64 | 57 (22.7) |
| ≥65 | 64 (25.5) |
| Education, n (%) | |
| Illiterate | 156 (62.2) |
| Literate | 95 (37.8) |
| Marital status, n (%) | |
| Never married | 25 (10.0) |
| Married | 170 (67.7) |
| Divorced | 27 (10.8) |
| Widowed | 29 (11.6) |
| Religion, Christian, n (%) | 251 (100) |
| Employment status, n (%) | |
| Salaried | 2 (0.8) |
| Self-employed | 2 (0.8) |
| Farming | 194 (77.3) |
| Housework | 47 (18.7) |
| Not working | 4 (1.6) |
| Othera | 2 (0.8) |
| Relative income, n (%) | |
| Very low | 40 (15.9) |
| Low | 106 (42.2) |
| Middle | 99 (39.4) |
| High | 6 (2.39) |
| Have children, n (%) | |
| Yes | 223 (88.8) |
| No | 28 (11.2) |
Percentages may not add up to 100 due to rounding.
One daily labourer and one unable work due to disability.
Clinical and psychosocial characteristics at baseline
Among the study population, 93.6% had a history of acute attack. The mean±standard deviation (SD) number of acute attacks in the month prior to the survey was 2.4 ± 2.6. Only 15.5% of participants had ever received treatment for their leg lymphoedema and only 8.4% of participants were currently receiving treatment or administering self-treatment at the time of enrolment (Table 2).
Table 2.
Clinical characteristics of patients with lymphoedema participating in the study (N=251)
| Variables | Values |
|---|---|
| Type of case with lymphoedema, n (%) | |
| Lymphatic filariasis/podoconiosis | 246 (98.0) |
| Leprosy | 5 (2.0) |
| Has your leg ever suddenly become hot, red and painful? (i.e. an acute attack), n (%) | |
| Yes | 235 (93.6) |
| No | 16 (6.4) |
| How often does your leg become hot, red and painful? (i.e. acute attack), n (%) (N=235) | |
| Every week | 62 (26.4) |
| Every 2 weeks | 58 (24.7) |
| Every month | 48 (20.4) |
| Every 3 months | 31 (13.2) |
| Every 6 months | 19 (8.1) |
| Every year | 11 (4.7) |
| ≥1 y | 6 (2.6) |
| Number of acute episodes in the month prior to the survey, mean±SD (range) | 2.4 ± 2.6 (0–20) |
| Have you ever received treatment for your leg lymphoedema?, n (%) | |
| Yes | 39 (15.5) |
| No | 212 (84.5) |
| Are you currently receiving treatment for, or self-treating your leg(s)?, n (%) | |
| Yes | 21 (8.4) |
| No | 230 (91.6) |
| Where did you receive/are you receiving treatment?, n (%) (N=39) | |
| Government clinic | 27 (69.2) |
| Non-government clinic | 6 (15.4) |
| Self-treatment | 4 (10.3) |
| Traditional healer | 1 (2.6) |
| Other | 1 (2.6) |
Percentages may not add up to 100 due to rounding.
The prevalence of depression with a PHQ-9 cut-off of 10 was 47.4% (119/251 participants). Considering the severity of depression, 39.0% of participants were classed as having mild depression, 29.9% moderate, 11.2% moderately severe and 6.4% severe depression (Table 3). The mean DLQI was 11.4 ± 4.2. Lymphoedema had a very large effect on the patient's QOL in 53.4% of cases and a moderate effect in 30.7% of cases (Table 3).
Table 3.
Mental health and psychosocial characteristics of patients with lymphoedema participating in the study (N=251)
| Variables | Values |
|---|---|
| Depressive symptoms (based on PHQ-9 score <5), n (%) | |
| Not depressed | 34 (13.5) |
| Depressed | 217 (86.5) |
| Level of depressive symptoms (based on PHQ-9 score), n (%) | |
| No depression (0–4) | 34 (13.5) |
| Mild (5–9) | 98 (39.0) |
| Moderate (10–14) | 75 (29.9) |
| Moderately severe (15–19) | 28 (11.2) |
| Severe (20–27) | 16 (6.4) |
| Alcohol use disorder (based on FAST), n (%) | |
| No alcohol use disorder | 159 (63.4) |
| Alcohol use disorder | 92 (36.7) |
| Social support (based on Oslo-3) | |
| Poor | 164 (65.3) |
| Moderate | 69 (27.5) |
| Strong | 18 (7.2) |
| Disability measure (based on WHODAS), mean±SD | |
| WHODAS score | 29.6 ± 8.8 (median 28.0) |
| How many days in the past 30 d have these difficulties been present? | 12.4 ± 6.2 |
| How many days in the past 30 d were you totally unable carry out your usual activities? | 6.3±4.7 |
| How many days in the past 30 d did you cut back or reduce your usual activities? | 3.7 ± 2.7 |
| Quality of life (DLQI score), mean±SD | 11.4±4.2 |
| DLQI effect on patients’ life, n (%) | |
| No effect (0–1) | 4 (1.6) |
| Small (2–5) | 27 (10.8) |
| Moderate (6–10) | 77 (30.7) |
| Very large (11–20) | 134 (53.4) |
| Extremely large (21–30) | 9 (3.6) |
| DLQI subscale, mean±SD | |
| Symptoms and feelingsa | 3.4 ± 1.4 |
| Daily activitiesa | 2.3 ± 1.7 |
| Leisurea | 1.8 ± 1.4 |
| Work and schoolb | 2.4 ± 1.1 |
| Personal relationshipsa | 1.1 ± 1.3 |
| Treatmentb | 0.7 ± 0.9 |
Percentages may not add up to 100 due to rounding.
Maximum value of subscale = 6.
Maximum value of subscale = 3.
Assessment of other psychosocial characteristics showed that 36.6% of participants displayed a hazardous drinking habit and 65.3% had poor social support (Table 3). The mean WHODAS score for disability was 29.6 ± 8.8, the mean number of days over the last 30 d where the person was unable do their usual activities or work was 6.3 ± 4.7 and the mean number of days where they cut back or reduced their usual activities was 3.7 ± 2.7 (Table 3).
Using the CIDI scale, 12.4% of 251 study participants had suicidal thoughts, 9.2% reported planning suicide and 7.6% reported a suicide attempt (Table 4). None of the participants with suicidal ideation had accessed any form of treatment for this (Table 4).
Table 4.
Suicidal ideation and suicide attempts, assessed using the CIDI, among patients with lymphoedema participating in the study (N=251)
| Variables | Values |
|---|---|
| Suicidal ideation in the last month, n (%) | |
| Yes | 31 (12.4) |
| No | 220 (87.6) |
| Suicide planning in the last month, n (%) | |
| Yes | 23 (9.2) |
| No | 228 (90.8) |
| Suicide attempts in the last month, n (%) | |
| Yes | 19 (7.6) |
| No | 232 (92.4) |
| Among those who attempted suicide (N=19), frequency of attempt, mean±SD (range) | 1.9 ± 0.9 (1–5) |
| Received any treatment for thinking about or attempting to take your own life?, n (%) | |
| Yes | 0 |
| No | 31 (100) |
Percentages may not add up to 100 due to rounding.
Factors associated with depression
In the bivariate linear regression analysis, sex, age, educational status, employment status, marital status, social support and relative income were significantly associated with depression (Table 5). However, in the multivariate linear regression analysis, none of these sociodemographic factors were significantly associated with depression. In the multivariate linear regression model, there was a positive, statistically significant, association between disability, as measured by the WHODAS, and depression, as measured by the PHQ-9 (β=0.26 [95% CI 0.19 to 0.33]) (Table 6).
Table 5.
Bivariate analysis using depression, assessed using the PHQ-9 scale, as a continuous outcome variable (N=251)
| Variable | PHQ-9 score, mean±SD | β (95% CI) | p-Valuea |
|---|---|---|---|
| Sex | |||
| Male | 9.2 ± 5.4 | −1.54 (−2.81 to −0.27) | 0.02 |
| Female (reference) | 10.7 ± 4.8 | 1.0 | |
| Age (continuous) | 10.0 ± 5.2 | 0.05 (0.01 to 0.08) | 0.03 |
| Education | |||
| Illiterate | 10.8 ± 5.4 | 2.32 (1.03 to 3.62) | <0.001 |
| Literate (reference) | 8.5 ± 4.4 | 1.0 | |
| Marital status | |||
| Currently married | 9.5 ± 5.2 | −1.44 (−2.81 to −0.08) | 0.04 |
| Currently not married (reference) | 10.9 ± 5.0 | 1.0 | |
| Employment | |||
| Employedb | 10.2 ± 5.5 | 0.90 (−0.71 to 2.42) | 0.28 |
| Not employed (reference) | 9.3 ± 3.20 | 1.0 | |
| Relative income | |||
| Very low and low (reference) | 11.3 ± 5.3 | 1.0 | <0.001 |
| Middle and high | 8.2 ± 4.4 | −3.11 (−4.35 to −1.87) | |
| Acute attack frequency (N=235) | |||
| Every week/2 weeks/month (reference) | 10.2 ± 5.1 | 1.0 | |
| ≥3 months | 9.3 ± 5.1 | −0.92 (−2.39 to 0.53) | 0.21 |
| Acute attack (continuous) | 10.0 ± 5.2 | 0.01 (−0.24 to 0.26) | 0.93 |
| Have you ever received treatment for your leg lymphoedema? | |||
| No (reference) | 9.8 ± 5.1 | 1.0 | 0.35 |
| Yes | 10.7 ± 5.6 | 0.84 (−0.93 to 2.61) | |
| Are you currently receiving treatment for, or self-treating your leg(s)? | |||
| No (reference) | 10.0 ± 5.1 | 1.0 | 0.82 |
| Yes | 9.7 ± 5.9 | −0.27 (−2.59 to 2.05) | |
| Hazardous drinking habit (FAST) | |||
| No (reference) | 9.7 ± 4.9 | 1.0 | 0.38 |
| Yes | 10.3 ± 5.5 | 0.60 (−0.74 to 1.93) | |
| Social support (based on Oslo-3) | |||
| Poor (reference) | 5.9 ± 5.2 | 1.0 | |
| Moderate | 9.0 ± 4.9 | −1.76 (−3.17 to −0.35) | 0.01 |
| Strong | 10.8 ± 3.5 | −4.85 (−7.29 to −2.41) | <0.001 |
| Disability assessment based on WHODAS (continuous) | 11.8 ± 5.1 | 0.31 (0.25 to 0.37) | <0.001 |
| DLQI (continuous) | 10.0 ± 5.2 | −0.04 (−0.17 to 0.09) | 0.52 |
Linear regression was used to examine the association between explanatory variables and depression measured by the PHQ-9. Explanatory variables with an association of p<0.2 in the bivariate analysis were included in the multivariate linear regression model.
Salaried, self-employed and farming.
Table 6.
Multivariate linear regression analysis using depression, assessed using the PHQ-9 scale, as a continuous outcome variable (N=251)
| Variables | PHQ-9, mean±SD | β (95% CI) | p-Valuea |
|---|---|---|---|
| Sex | |||
| Male | 9.2 ± 5.4 | 1.0 | |
| Female | 10.7 ± 4.8 | 0.39 (−1.02 to 1.80) | 0.59 |
| Age (continuous) | 10.0 ± 5.2 | ||
| Education | |||
| Illiterate | 10.8 ± 5.4 | 1.0 | |
| Literate | 8.5 ± 4.4 | 0.01 (−0.03 to 0.05) | 0.67 |
| Marital status | |||
| Currently married | 9.5 ± 5.2 | 1.0 | |
| Currently not married | 10.9 ± 5.0 | 0.07 (−1.30 to 1.43) | 0.92 |
| Relative income | |||
| Very low and low | 11.3 ± 5.3 | 1.0 | |
| Middle and high | 8.2 ± 4.4 | −1.17 (−2.42 to 0.09) | 0.07 |
| Social support (based on Oslo-3) | |||
| Poor (reference) | 5.9 ± 5.2 | 1.0 | |
| Moderate | 9.0 ± 4.9 | −0.83 (−2.09 to 0.41) | 0.19 |
| Strong | 10.8 ± 3.5 | −2.07 (−4.27 to 0.13) | 0.07 |
| Disability assessment based on WHODAS (continuous) | 11.8 ± 5.1 | 0.26 (0.19 to 0.33) | <0.001 |
Linear regression was used to examine the association between explanatory variables and depression measured by the PHQ-9. Explanatory variables with an association of p<0.2 in the bivariate analysis were included in the multivariate linear regression model. In the multivariate linear regression model, those explanatory variables with association at p<0.05 were considered statistically significant.
Factors associated with quality of life
In the bivariate linear regression analysis, none of the sociodemographic factors, history of acute attack or frequency of attack in the past month were associated with QOL as measured by the DLQI (Table 7). In the multivariate linear regression model, currently receiving treatment was significantly associated with improved QOL (β=−3.05 [95% CI −5.25 to −0.85]). Hazardous drinking habit was associated with poor QOL (β=1.31 [95% CI 0.02 to 2.59]). Social support was also significantly associated with improved QOL. Using poor social support as a reference, participants with moderate social support had β=−2.27 (95% CI −3.66 to −0.89) and those with strong social support had β=−2.87 (95% CI −5.35 to −0.38). In addition, disability was significantly associated with QOL (β=−0.08 [95% CI −0.15 to −0.01]) (Table 8).
Table 7.
Bivariate analysis using QOL, assessed using the DLQI as a continuous outcome variable (N=251)
| Variables | DLQI, mean ± SD | β (95% CI) | p-Valuea |
|---|---|---|---|
| Sex | |||
| Male | 12.4 ± 5.3 | 1.24 (−0.02 to 2.49) | 0.05 |
| Female (reference) | 11.2 ± 4.8 | 1.0 | |
| Age (continuous) | 11.8 ± 5.1 | −0.006 (−0.05 to 0.04) | 0.76 |
| Education | |||
| Illiterate | 11.3 ± 4.9 | −1.17 (−2.47 to 0.12) | 0.08 |
| Literate (reference) | 12.5 ± 5.4 | 1.0 | |
| Marital status | |||
| Currently married | 11.8 ± 5.2 | 0.06 (−1.29 to 1.41) | 0.93 |
| Currently not married (reference) | 11.7 ± 4.8 | 1.0 | |
| Employment | |||
| Employedb | 11.9 ± 5.1 | 0.82 (−0.72 to 2.37) | 0.24 |
| Not employed (reference) | 11.1 ± 5.0 | 1.0 | |
| Relative income | |||
| Very low and low (reference) | 11.8 ± 4.9 | 1.0 | |
| Middle and high | 11.6 ± 5.3 | −0.22 (−1.50 to 1.06) | 0.74 |
| Acute attack frequency (N=235) | |||
| Every week/2 weeks/month (reference) | 11.8 ± 5.1 | 1.0 | |
| ≥3 months | 11.8 ± 4.9 | −0.02 (−1.45 to 1.42) | 0.98 |
| Acute attack (continuous) | 11.8 ± 5.1 | 0.07 (−0.19 to 0.31) | 0.61 |
| Have you ever received treatment for your leg lymphoedema? | |||
| No (reference) | 11.9 ± 5.0 | 1.0 | |
| Yes | 11.0 ± 5.4 | −0.94 (−2.68 to 0.80) | 0.29 |
| Are you currently receiving treatment for, or self-treating your leg(s)? | |||
| No (reference) | 12.0 ± 5.1 | 1.0 | |
| Yes | 9.2 ± 4.2 | −2.74 (−4.99 to −0.48) | 0.02 |
| Hazardous drinking habit (FAST) | |||
| No (reference) | 11.3 ± 5.2 | 1.0 | |
| Yes | 12.5 ± 4.8 | 1.21(−0.09 to 2.51) | 0.07 |
| Social support (based on Oslo-3) | |||
| Poor (reference) | 12.4 ± 4.7 | 1.0 | |
| Moderate | 10.5 ± 5.2 | −1.93 (−3.35 to −0.52) | 0.008 |
| Strong | 10.7 ± 7.2 | −1.67 (−4.13 to 0.78) | 0.18 |
| Disability assessment based on WHODAS (continuous) | 11.8 ± 5.1 | −0.06 (−0.13 to 0.01) | 0.11 |
| PHQ-9 (continuous) | 11.8 ± 5.1 | −0.04 (−0.16 to 0.08) | 0.52 |
Linear regression was used to examine the association between explanatory variables and quality of life measured by DLQI. Explanatory variables with an association of p<0.2 in the bivariate analysis were included in the multivariate linear regression model.
Salaried, self-employed and farming.
Table 8.
Multivariate linear regression analysis using QOL assessed using the DLQI as a continuous outcome variable (N=251)
| Variables | DLQI, mean±SD | β (95% CI) | p-Valuea |
|---|---|---|---|
| Sex | |||
| Male | 12.4 ± 5.3 | −1.0 (−2.34 to 0.36) | 0.15 |
| Female (reference) | 11.2 ± 4.8 | 1.0 | |
| Education | |||
| Illiterate | 11.3 ± 4.9 | 0.75 (−0.64 to 2.14) | 0.29 |
| Literate (reference) | 12.5 ± 5.4 | 1.0 | |
| Are you currently receiving treatment for, or self-treating your leg(s)? | |||
| No (reference) | 12.0 ± 5.1 | 1.0 | |
| Yes | 9.2 ± 4.2 | −3.05 (−5.25 to −0.85) | 0.007 |
| Hazardous drinking habit (FAST) | |||
| No (reference) | 11.3 ± 5.2 | 1.0 | |
| Yes | 12.5 ± 4.8 | 1.31 (0.02 to 2.59) | 0.046 |
| Social support (based on Oslo-3) | |||
| Poor (reference) | 12.4 ± 4.7 | 1.0 | |
| Moderate | 10.5 ± 5.2 | −2.27 (−3.66 to −0.89) | 0.001 |
| Strong | 10.7 ± 7.2 | −2.87 (−5.35 to −0.38) | 0.024 |
| Disability assessment based on WHODAS (continuous) | 11.8 ± 5.1 | −0.08 (−0.15 to −0.01) | 0.035 |
Linear regression was used to examine the association between explanatory variables and quality of life measured by DLQI. Explanatory variables with an association of p<0.2 in the bivariate analysis were included in the multivariate linear regression model. In the multivariate linear regression model, those explanatory variables with association at p<0.05 were considered statistically significant.
Discussion
The present study demonstrated high levels of depression and low QOL among study participants with lymphoedema associated with LF, podoconiosis or leprosy. Disability, as assessed by the WHODAS, was the factor most significantly associated with depression in this population. A high proportion of patients (47.4%) reported moderate to severe depressive symptoms. QOL was significantly associated with current treatment, social support, alcohol use disorder and disability.
Among study participants, 12.4% had suicidal thoughts, 9.2% reported suicidal planning and 7.6% reported suicide attempts. This is lower than among HIV-positive individuals, among whom the lifetime prevalence of suicidal ideation was 26% and that of suicide attempt was 13%.32 Moreover, suicidal ideation was significantly associated with major depressive disorder.32 A similar prevalence of suicidal ideation (10.3%) and relatively lower rate of suicidal planning (2.2%) was reported previously in a study in five LMICs among community/healthcare-seeking populations presenting at primary care facilities.31
An association between depression and lymphoedema due to podoconiosis, LF or leprosy has also been reported by other researchers. A comparative cross-sectional study in northern Ethiopia showed a higher prevalence of depression, measured using the PHQ-9 scale, among patients with podoconiosis (12.6%) compared with their apparently healthy neighbours (0.7%).36 Another cross-sectional study among people living with LF in Nigeria, which used the PHQ-9 and CIDI to measure depression, found a higher prevalence of depression (20%) among LF-affected individuals than the reported ‘background’ prevalence among the general adult population in Nigeria (3.1–5.2%).37 A study in Cameroon used the PHQ-9 scale to demonstrate a high prevalence of depressive symptoms (38.5%) among individuals with lower limb lymphoedema (predominantly due to podoconiosis), although the majority had mild depression.38 Studies on individuals affected by leprosy have also reported a high burden of depression.39,40 For example, the prevalence of psychiatric morbidity among leprosy patients in Nigeria was found to be 58% and most cases had depression.39
Poor socio-economic status might contribute to the high burden of depression among the study participants. Only 2.4% of study participants belong to the high relative income group in our study. However, despite an association between relative income and depression, this was not statistically significant (p=0.07). It is possible that a lack of treatment for lymphoedema (as found in 85.5% of participants) led to disease progression, which itself may have led to depressive symptoms. Stigma and discrimination due to lymphoedema may also have contributed to the high prevalence of depressive symptoms.
QOL was moderately compromised in one-third of cases and severely compromised in about half of patients in the present study; the mean DLQI score was high at 11.4 ± 4.2. Similar results were reported in a previous intervention study from Guyana among people affected by LF lymphoedema, showing a baseline mean DLQI of 10.9.17 In contrast, a study from India among LF lymphoedema cases reported a relatively low mean DLQI value of 2.7 ± 4.4,18 indicating better QOL than was observed in the present study. Other studies have measured QOL using the World Health Organization Quality of Life Brief Version questionnaire (WHOQoL-BREF) and found that people with podoconiosis had significantly poorer QOL than controls.41 In a study in Bangladesh, the WHOQoL-BREF score was lower among people affected by leprosy than controls.42 A cross-sectional study in Brazil among leprosy-affected individuals also reported low WHOQoL-BREF scores.43 Here we demonstrated that patients currently on treatment had a better QOL than those who were not, implying that emphasis should be given to early diagnosis and management of cases.
The only factor significantly associated with depression among people with lymphoedema was higher disability score. Similarly, a study from northern Ethiopia among patients with podoconiosis showed that increased disability, as measured by the WHODAS, was associated with increased depression among patients with podoconiosis.36 A study conducted in Bangladesh on leprosy-affected individuals also showed a significant association between disability, as measured by the WHO disability grade, and depression as measured by the Centre for Epidemiologic Studies Depression Scale.40
Disability was inversely related to QOL, i.e. lower disability scores were associated with higher QOL. This suggests that prevention of disability due lymphoedema may also prevent depression and improve QOL. Hazardous alcohol consumption was positively associated with low QOL, while study participants with better social support had better QOL. Similar results have been reported in previous studies. A study in Iran among people living with HIV showed a significant association between QOL, as measured by the 36-item Short-Form Health Survey (SF-36), and social support.44 There was an association between QOL, as measured by the WHOQOL-BREF, and social support in a study on hospitalized schizophrenia patients in Malaysia,45 while disability was inversely related to QOL and improvement in disability was associated with improved QOL. Disability, measured using the WHODAS, was significantly associated with QOL, measured by the SF-36, in study participants with mental disorder46 and QOL, assessed by the WHOQOL-BREF, was significantly associated with disability among leprosy patients in northeastern Brazil.43
There were some limitations to the current study. First, the study design was cross-sectional in nature, making it difficult to determine a direction of association between presumed explanatory variables and depression or QOL. Second, although most of the tools, including the PHQ-9, DLQI and WHODAS, have been validated in Ethiopia, despite their use in studies in other parts of the world, the FAST and Oslo-3 have not been validated in Ethiopia. Third, we did not measure all factors that might be associated with depression e.g. family history of mental illness, wealth index or comorbidities or factors that might affect QOL, such as wealth index and comorbidities.
Conclusions
Our findings indicate a considerable burden of depression and poor QOL among study participants with lymphoedema due podoconiosis, LF or leprosy. Therefore a holistic package of care that addresses the physical, mental, social and psychological needs of people with lymphoedema is warranted. Interventions targeting morbidity management and disability prevention of these three NTDs should integrate best practices in addressing the mental, social and psychological aspects of these diseases.
Acknowledgements
The authors would like to acknowledge members of the EnDPoINT consortium for their input into the study. We also thank Clare Callow for National Institute for Health Research (NIHR) project management, through which EnDPoINT is funded, the Awi Zone health department and Guagsa Shikudad district health department staff, especially the NTD unit staff, the healthcare workers at Gusha Health Centre and CDT Africa field coordinator, Abdulkadir Ahmed. We are very grateful to all study participants. Catriona McKay, PhD provided help with editing of the manuscript.
Contributor Information
Oumer Ali, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT)-Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, 9086, Ethiopia; Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK.
Kebede Deribe, Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK; School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, 1176, Ethiopia.
Maya Semrau, Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK.
Asrat Mengiste, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT)-Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, 9086, Ethiopia.
Mersha Kinfe, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT)-Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, 9086, Ethiopia.
Abraham Tesfaye, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT)-Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, 9086, Ethiopia.
Stephen Bremner, Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK.
Gail Davey, Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK; School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, 1176, Ethiopia.
Abebaw Fekadu, Center for Innovative Drug Development and Therapeutic Trials for Africa (CDT)-Africa, College of Health Sciences, Addis Ababa University, Addis Ababa, 9086, Ethiopia; Centre for Global Health Research, Brighton and Sussex Medical School, University of Sussex, Falmer, Brighton BN1 9PX, UK.
Authors’ contributions
GD and AF are the principal investigators of the EnDPoINT study. OA, AT, AM and MK were responsible for implementation of the project. MS led the overall project activities. KD and SB led the statistical analysis. OA led the writing of the manuscript and prepared the first full draft. All authors contributed to the development of the manuscript and read and approved the final version.
Funding
This work was supported by the NIHR Global Health Research Unit on NTDs using Official Development Assistance (ODA) funding for Brighton and Sussex Medical School (award 16/136/29). The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. KD is supported by the Wellcome Trust (grant 201900/Z/16/Z) as part of his International Intermediate Fellowship.
Competing interests
None declared.
Ethical approval
Ethical approval for the study was obtained from Brighton and Sussex Medical School Research Governance and Ethics Committee, Brighton, UK (reference number ER/BSMS9D79/2) and the Institutional Review Board of the College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia (reference number 061/18/CDT).
Data availability
Data may be accessed up on request to data manager.
References
- 1. Liese B, Rosenberg M, Schratz A. Programmes, partnerships, and governance for elimination and control of neglected tropical diseases. Lancet North Am Ed. 2010;375(9708):67–76. [DOI] [PubMed] [Google Scholar]
- 2. Hotez PJ, Molyneux DH, Fenwick A et al. Control of neglected tropical diseases. N Engl J Med. 2007;357(10):1018–27. [DOI] [PubMed] [Google Scholar]
- 3. Deribe K, Simpson H, Cano J et al. Mapping the global distribution of podoconiosis: Applying an evidence consensus approach. PLoS Negl Trop Dis. 2019;13(12):e0007925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Davey G, GebreHanna E, Adeyemo A et al. Podoconiosis: a tropical model for gene–environment interactions? Trans R Soc Trop Med Hyg. 2007;101(1):91–6. [DOI] [PubMed] [Google Scholar]
- 5. Fyfe N, Price E. The effects of silica on lymph nodes and vessels—a possible mechanism in the pathogenesis of non-filarial endemic elephantiasis. Trans R Soc Trop Med Hyg. 1985;79(5):645–51. [DOI] [PubMed] [Google Scholar]
- 6. Deribe K, Cano J, Giorgi E et al. Estimating the number of cases of podoconiosis in Ethiopia using geostatistical methods. Wellcome Open Res. 2017;2:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Michael E, Bundy D, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology. 1996;112(4):409–28. [DOI] [PubMed] [Google Scholar]
- 8. Ramaiah K, Ottesen EA. Progress and impact of 13 years of the global programme to eliminate lymphatic filariasis on reducing the burden of filarial disease. PLoS Negl Trop Dis. 2014;8(11):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Belete Mengistu KD, Kebede F, Martindale S et al. The national programme to eliminate lymphatic filariasis from Ethiopia. Ethiop Med J. 2017;55(Suppl 1):45–54. [PMC free article] [PubMed] [Google Scholar]
- 10. Smith CS, Noordeen SK, Richardus JH et al. A strategy to halt leprosy transmission. Lancet Infect Dis. 2014;14(2):96–8. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization Global leprosy update, 2017: reducing the disease burden due to leprosy. Wkly Epidemiol Rec. 2018;93(35):445–56. [Google Scholar]
- 12. Federal Democratic Republic of Ethiopia Ministry of Health Guidelines for clinical and programmatic management of TB, leprosy and TB/HIV in Ethiopia. Addis Ababa: Federal Democratic Republic Of Ethiopia Ministry Of Health; 2016. [Google Scholar]
- 13. Baird J, Unit MLE, Petticrew M, White M. Developing and evaluating complex interventions. Swindon, UK: Medical Research Council; 2006. [Google Scholar]
- 14. Keeley V, Crooks S, Locke J et al. A quality of life measure for limb lymphoedema (LYMQOL). J Lymphoedema. 2010;5(1):26–37. [Google Scholar]
- 15. Caprioli T, Martindale S, Mengiste A et al. Quantifying the socio-economic impact of leg lymphoedema on patient caregivers in a lymphatic filariasis and podoconiosis co-endemic district of Ethiopia. PLoS Negl Trop Dis. 2020;14(3):e0008058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Finlay AY, Khan G. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–6. [DOI] [PubMed] [Google Scholar]
- 17. McPherson T. Impact on the quality of life of lymphoedema patients following introduction of a hygiene and skin care regimen in a Guyanese community endemic for lymphatic filariasis: a preliminary clinical intervention study. Filaria J. 2003;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Babu B, Nayak A, Rath K et al. Use of the Dermatology Life Quality Index in filarial lymphoedema patients. Trans R Soc Trop Med Hyg. 2006;100(3):258–63. [DOI] [PubMed] [Google Scholar]
- 19. Henok L, Davey G. Validation of the Dermatology Life Quality Index among patients with podoconiosis in southern Ethiopia. Br J Dermatol. 2008;159(4):903–6. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization WHO Disability Assessment Schedule 2.0 2018 [23 April 2020]. Available from: https://www.who.int/classifications/icf/whodasii/en/.
- 21. Habtamu K, Alem A, Medhin G et al. Validation of the World Health Organization disability assessment schedule in people with severe mental disorders in rural Ethiopia. Health Qual Life Outcomes. 2017;15(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gelaye B, Williams MA, Lemma S et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hanlon C, Medhin G, Selamu M et al. Validity of brief screening questionnaires to detect depression in primary care in Ethiopia. J Affect Disord. 2015;186:32–9. [DOI] [PubMed] [Google Scholar]
- 25. Fekadu A, Medhin G, Selamu M et al. Recognition of depression by primary care clinicians in rural Ethiopia. BMC Fam Pract. 2017;18(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hodgson R, Alwyn T, John B et al. The FAST alcohol screening test. Alcohol Alcoholism. 2002;37(1):61–6. [DOI] [PubMed] [Google Scholar]
- 27. Hodgson RJ, John B, Abbasi T et al. Fast screening for alcohol misuse. Addict Behav. 2003;28(8):1453–63. [DOI] [PubMed] [Google Scholar]
- 28. Health Development Agency, University of Wales College of Medicine . Manual for the Fast Alcohol Screening Test (FAST). London: Health Development Agency; 2002. [Google Scholar]
- 29. Teferra S, Medhin G, Selamu M et al. Hazardous alcohol use and associated factors in a rural Ethiopian district: a cross-sectional community survey. BMC Public Health. 2016;16(1):218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meneses-Gaya C, Crippa JAS, Zuardi AW et al. The Fast Alcohol Screening Test (FAST) is as good as the AUDIT to screen alcohol use disorders. Subst Use Misuse. 2010;45(10):1542–57. [DOI] [PubMed] [Google Scholar]
- 31. Jordans M, Rathod S, Fekadu A et al. Suicidal ideation and behaviour among community and health care seeking populations in five low-and middle-income countries: a cross-sectional study. Epidemiol Psychiatr Sci. 2018;27(4):393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Badiee J, Moore DJ, Atkinson JH et al. Lifetime suicidal ideation and attempt are common among HIV+ individuals. J Affect Disord. 2012;136(3):993–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kocalevent R-D, Berg L, Beutel ME et al. Social support in the general population: standardization of the Oslo Social Support Scale (OSSS-3). BMC Psychol. 2018;6:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Duko B, Geja E, Zewude M et al. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann Gen Psychiatry. 2018;17(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bisetegn TA, Mihretie G, Muche T. Prevalence and predictors of depression among pregnant women in Debretabor town, northwest Ethiopia. PLoS One. 2016;11(9):e0161108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bartlett J, Deribe K, Tamiru A et al. Depression and disability in people with podoconiosis: a comparative cross-sectional study in rural northern Ethiopia. Int Health. 2016;8(2):124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Obindo J, Abdulmalik J, Nwefoh E et al. Prevalence of depression and associated clinical and socio-demographic factors in people living with lymphatic filariasis in Plateau State, Nigeria. PLoS Negl Trop Dis. 2017;11(6):e0005567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Semrau M, Davey G, Beng AA et al. Depressive symptoms amongst people with podoconiosis and lower limb lymphoedema of other cause in Cameroon: a cross-sectional study. Trop Med Infect Dis. 2019;4(3):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Erinfolami AR, Adeyemi JD. A case control study of psychiatric morbidities among subjects with leprosy in Lagos, Nigeria. Int J Psychiatry Med. 2009;39(1):89–99. [DOI] [PubMed] [Google Scholar]
- 40. Tsutsumi A, Izutsu T, Akramul Islam MD et al. Depressive status of leprosy patients in Bangladesh: association with self-perception of stigma. Lepr Rev. 2004;75(1):57–66. [PubMed] [Google Scholar]
- 41. Mousley E, Deribe K, Tamiru A et al. The impact of podoconiosis on quality of life in northern Ethiopia. Health Qual Life Outcomes. 2013;11:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tsutsumi A, Izutsu T, Islam AM et al. The quality of life, mental health, and perceived stigma of leprosy patients in Bangladesh. Soc Sci Med. 2007;64(12):2443–53. [DOI] [PubMed] [Google Scholar]
- 43. Santos VS, Oliveira LS, Castro FD et al. Functional activity limitation and quality of life of leprosy cases in an endemic area in northeastern Brazil. PLoS Negl Trop Dis. 2015;9(7):e0003900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Charkhian A, Fekrazad H, Sajadi H et al. Relationship between health-related quality of life and social support in HIV-infected people in Tehran, Iran. Iran J Public Health. 2014;43(1):100–6. [PMC free article] [PubMed] [Google Scholar]
- 45. Munikanan T, Midin M, Daud TIM et al. Association of social support and quality of life among people with schizophrenia receiving community psychiatric service: a cross-sectional study. Compr Psychiatry. 2017;75:94–102. [DOI] [PubMed] [Google Scholar]
- 46. Al-Yahya AH, Raya Y, El-Tantawy A. Disability due to mental disorders and its relationship to severity of illness and quality of life. Int J Health Sci (Qassim). 2011;5(2 Suppl 1):33–4. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data may be accessed up on request to data manager.