Abstract
Background
Healthcare access has changed drastically during the COVID-19 pandemic. Elective medical procedures, including routine office visits, were restricted raising concerns regarding opioid and benzodiazepine provider and prescription availability.
Objective
To examine how the cancelation of elective medical procedures due to COVID-19 impacted the dispensing of opioid and benzodiazepine prescriptions in Texas.
Methods
Interrupted time series analyses were preformed to examine changes in prescription trends for opioids and benzodiazepines before and after the restriction on elective medical procedures. Samples of patients who filled an opioid or benzodiazepine prescription from January 5, 2020 to May 12, 2020 were identified from the Texas Prescription Monitoring Program. Elective medical procedures were restricted starting March 23, 2020 indicating the beginning of the intervention period.
Results
Restricting elective procedures was associated with a significant decrease in the number of patients (β = −6029, 95%CI = −8810.40, −3246.72) and prescribers (β = −2784, 95%CI = −3671.09, −1896.19) filling and writing opioid prescriptions, respectively. Also, the number of patients filling benzodiazepine prescriptions decreased significantly (β = −1982, 95%CI = −3712.43, −252.14) as did the number of prescribers (β = −708.62, 95%CI = −1190.54, −226.71).
Conclusion
Restricting elective procedures resulted in a large care gap for patients taking opioid or benzodiazepine prescriptions.
Introduction
Opioids and benzodiazepines are some of the most commonly dispensed controlled substance prescriptions (CSP) in the United States.1 However, in the last decade, opioid and benzodiazepine prescriptions have been declining in part due to increased awareness of the risks of opioids, systemic policy interventions such as pain clinic regulations, and the expansion of Prescription Drug Monitoring Programs (PMPs) that collect data regarding dispensed controlled substance prescriptions.1, 2, 3, 4, 5 In the US, PMPs are state-run all payer databases that collect data regarding dispensed CSPs. Information collected by PMPs include patient, prescriber, and pharmacy name and data regarding the prescription itself such as medication name, strength, quantity, and day's supply.5 , 6 Prescribers and dispensers of controlled substances can view important information regarding a patient's CSP history at the point of care in order to prevent patient harm, misuse, or diversion of controlled substances.7 Although prescriptions for opioids and benzodiazepines have been decreasing, they still remain an integral part of therapy for many patients.
During the COVID-19 pandemic declared by the World Health Organization (WHO) on March 11, 2020, many states, including Texas, have enacted changes to healthcare delivery systems in order to slow further transmission of the virus.8 , 9 Texas Governor Greg Abbott declared a state of disaster in Texas on March 13, 2020.10 Following the governor's declaration, policies to ease patient care were passed. Temporary waivers have been granted by Governor Abbott and the Texas Medical Board (TMB) allowing prescribers to authorize telephone refills of opioid prescriptions for established chronic pain patients.11 Additionally, existing barriers to the provision of healthcare services via video or telephone, also known as telehealth or telemedicine, have been relaxed by the United States Department of Health and Human Services. Telehealth allows patients to connect with their doctors from home in order to obtain prescriptions for medications including controlled substances such as opioids or benzodiazepines.12 , 13 On March 22, 2020 the Governor issued an Executive Order restricting elective medical procedures including many routine outpatient visits.14 The TMB passed emergency rules to enforce Governor Abbott's order on March 24, 2020.15
Although patients may still be able to connect with prescribers via telehealth, there remains concern regarding the availability and accessibility of providers of opioid and benzodiazepine prescriptions when elective procedures including office visits are restricted. Therefore, the objective of this study was to examine how the cancellation of elective medical procedures and routine office visits due to the COVID-19 pandemic affected the dispensing of opioid and benzodiazepine prescriptions in Texas.
Methods
This study used a daily time series design. Two autoregressive interrupted time series models with a term for the time trend in either opioid or benzodiazepine prescriptions and a binary indicator for the period before and after the executive order was used to measure the change in number of patients filling a prescription for the respective medication. Two samples of patients that filled prescriptions for either an opioid or a benzodiazepine product between January 5, 2020 through May 12, 2020 that were identified from the Texas PMP, a complete record of all controlled substances dispensed by community pharmacies in the state. Next, daily counts of the number of distinct patients and prescribers filling and prescribing a new opioid or benzodiazepine prescription on each weekday of the study period were derived. Refilled prescriptions were excluded. Prescriptions for opioids and benzodiazepines were identified with current and retired national drug codes (NDC) for hydrocodone, oxycodone, tramadol, codeine, fentanyl, morphine, oxymorphone, tapentadol, dihydrocodeine, alprazolam, diazepam, lorazepam, chlordiazepoxide, temazepam, clorazepate, clobazam, oxazepam, and prazepam from RxNav, a database from the National Library of Medicine that contains historical NDCs and is updated monthly.16
The intervention period for the auto-regressive models was defined based on the restriction on elective medical procedures. On March 22, Texas Governor Greg Abbott issued an Executive Order restricting elective medical procedures.14 The restriction was corroborated by the TMB and became enforceable on March 24. Observations between March 23, the first weekday of the intervention period, and March 30 were excluded from the model to account for latency between encounters before the restriction and the date a patient filled their prescription. Two similar models were used to examine the change in the number of distinct, daily opioid and benzodiazepine prescribers over the same study period.
Descriptive statistics including means and standard deviations were presented for the number of unique patients and prescribers for each drug of interest. For each model, the model parameter estimate with 95% confidence interval (95%CI) representing the effect of the intervention was also reported. The fitted values of the model were plotted along with the observed values for daily unique patients and prescribers for each medication.
Results
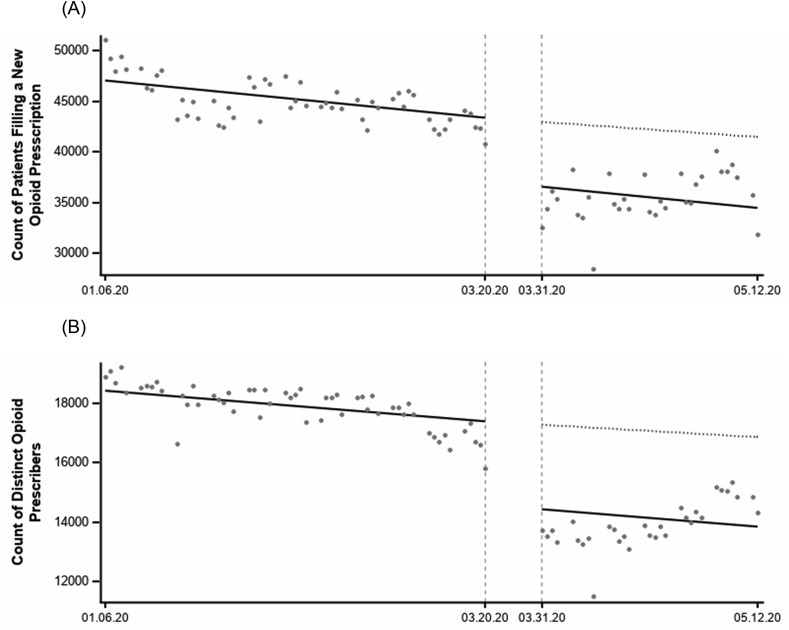
The average number of unique patients filling new opioid prescriptions each day was 45,044.49 (SD = 2190.86) before the intervention. The model demonstrated that the Executive Order restricting elective procedures was associated with a significant decrease in the number of patients who filled new opioid prescriptions (β = −6029, 95%CI = −8810.40, −3246.72). The average number of unique daily opioid prescribers was 17,921.53 (SD = 724.19) before the executive order. There was a significant decrease in the number of prescribers who issued new opioid prescriptions following the executive order (β = −2784, 95%CI = −3671.09, −1896.19) (Fig. 1 ).
Fig. 1.
Change in daily number of patients (A) and prescribers (B) for opioid prescriptions from 6 January 2020 through 12 May 2020 in Texas.
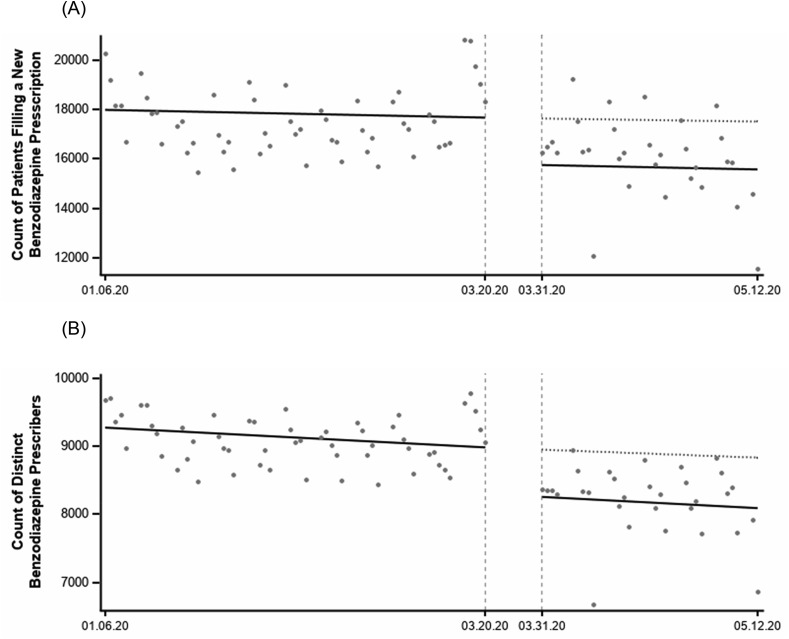
Prior to the intervention period, the average daily number of patients who filled new benzodiazepine prescriptions was 17,548.56 (SD = 1295.06). There was a significant decrease associated with the intervention (β = −1982, 95%CI = −3712.43, −252.14). A similar trend was observed with benzodiazepine prescribers. Before the executive order there were an average of 9,087.24 (SD = 356.26) unique daily prescribers of new benzodiazepine prescriptions. There was a significant decrease in benzodiazepine prescribers associated with the executive order (β = −708.62, 95%CI = −1190.54, −226.71) (Fig. 2 ).
Fig. 2.
Change in daily number of patients (A) and prescribers (B) for benzodiazepine prescriptions from 6 January 2020 through 12 May 2020 in Texas.
Discussion
Restricting elective medical procedures and routine office visits was associated with a significant decline in opioid and benzodiazepine patients and prescribers of their respective prescriptions. Following the executive order there was a significant reduction in the number of patients filling new opioid prescriptions per day and a significant reduction in the number of patients filling new benzodiazepine prescriptions per day through the end of the post intervention observation period. This indicates a significant gap in care for patients who are unable to obtain their prescriptions. Opioids and benzodiazepines play an integral role in the treatment of pain or anxiety and sleep disorders, respectively. Even during times of international crisis, patients still need their medications and most of those come from community pharmacies.3 , 17
Availability of prescribers via traditional office visits or telehealth services is an important factor of healthcare accessibility.18 During the COVID-19 pandemic existing telehealth services have been expanded to limit unnecessary direct patient contact and slow the spread of the virus; however, barriers such as poor computer literacy, lack of internet access, or privacy concerns may continue to prevent patients from using these services.19 , 20 Without an adequate number of available opioid or benzodiazepine prescribers, healthcare access for patients taking opioid or benzodiazepine prescriptions suffers resulting in a care gap. The consequences of untreated pain and anxiety disorders are well documented to include significant decrease in quality of life and significant cost burden to patients, healthcare systems, and economies.21 , 22
A portion of the reduction in patients filling opioid or benzodiazepine prescriptions may have been from elective surgical procedures requiring acute pain management that did not occur and would not be considered necessary in the post intervention time period. However, the need for opioid and benzodiazepine prescriptions for patients with chronic conditions persists in the midst of the COVID-19 pandemic and associated policy interventions. Patients with chronic conditions would be expected to return to the pre-intervention number of daily patients filling opioid and benzodiazepines.
This study is not without limitations. Although COVID-19 is a global pandemic, policy interventions vary widely, so the results may not be generalizable to locations outside of Texas. Additionally, including a week-long lag period and excluding weekends could alter the results of the study. In order to monitor CSP filling and patients’ access to care in times of crisis and rapid policy change, it is crucial that public health officials, in addition to regulatory agencies, have access to PMP data in real time.
Conclusion
The restriction of elective medical procedures, including routine office visits, due to the COVID-19 pandemic was associated with a significant decline in prescribers writing and patients filling opioid and benzodiazepine prescriptions indicating a large treatment gap.
Declaration of competing interest
The authors report no conflict of interest.
Acknowledgement of Funding
Dr. Thornton and Dr. Shen were partially supported by a grant from the National Institute of Health, National Institute on Drug Abuse (1R03DA047597-01). Data for this project were purchased by the Prescription Drug Misuse Education and Research (PREMIER) Center at the University of Houston College of Pharmacy.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sapharm.2020.06.003.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Bykov K., He M., Gagne J.J. Trends in utilization of prescribed controlled substances in US commercially insured adults, 2004-2019. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guy G.P., Jr., Zhang K., Bohm M.K. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. doi: 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strickler G.K., Kreiner P.W., Halpin J.F., Doyle E., Paulozzi L.J. Opioid prescribing behaviors - prescription behavior surveillance system, 11 states, 2010-2016. MMWR Surveill Summ. 2020;69(1):1–14. doi: 10.15585/mmwr.ss6901a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Champagne-Langabeer T., Madu R., Giri S., Stotts A.L., Langabeer J.R. Opioid prescribing patterns and overdose deaths in Texas. Subst Abuse. 2019:1–7. doi: 10.1080/08897077.2019.1675114. [DOI] [PubMed] [Google Scholar]
- 5.Yuanhong Lai A., Smith K.C., Vernick J.S., Davis C.S., Caleb Alexander G., Rutkow L. Perceived unintended consequences of prescription drug monitoring programs. Subst Use Misuse. 2019;54(2):345–349. doi: 10.1080/10826084.2018.1491052. [DOI] [PubMed] [Google Scholar]
- 6.Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33(5):319–328. doi: 10.3109/01612840.2011.654046. [DOI] [PubMed] [Google Scholar]
- 7.Doyle S., Leichtling G., Hildebran C., Reilly C. Research to support optimization of prescription drug monitoring programs. Pharmacoepidemiol Drug Saf. 2017;26(11):1425–1427. doi: 10.1002/pds.4300. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Timeline - Covid-19 World health organization. https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19 Updated 27 April 2020. Accessed 22 May, 2020.
- 9.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: community pharmacists' contribution during a public health crisis. Res Soc Adm Pharm. 2020 doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Governor Abbott Declares State of Disaster . Office of the Governor; Austin TX: March 13, 2020. (Texas Due to COVID-19). [Google Scholar]
- 11.Texas Medical Board Waiver for Chronic Pain Patients Granted by Governor Abbott. Texas Medical Board; March 19, 2020. press release. [Google Scholar]
- 12.Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html US Department of Health and Human Services, Updated March 30, 2020. Accessed May 23, 2020.
- 13.Shanthanna H., Strand N.H., Provenzano D.A. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia. 2020 doi: 10.1111/anae.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Texas GotSo Executive Order No. GA-09 relating to hospital capacity during the COVID-19 disaster. Secretary of State of Texas. https://gov.texas.gov/uploads/files/press/EO-GA_09_COVID-19_hospital_capacity_IMAGE_03-22-2020.pdf Published 2020. Accessed May 22, 2020.
- 15.Texas Medical Board Passes Emergency Rules to Enforce Gov. Abbott's Executive Order GA-09 [press release]. Texas Medical Board, March 24, 2020.
- 16.RxNorm frequently asked questions. National library of medicine. https://www.nlm.nih.gov/research/umls/rxnorm/faq.html Updated 31 March, 2020. Accessed 27 May, 2020.
- 17.Olfson M., King M., Schoenbaum M. Benzodiazepine use in the United States. JAMA Psychiatry. 2015;72(2):136–142. doi: 10.1001/jamapsychiatry.2014.1763. [DOI] [PubMed] [Google Scholar]
- 18.Levesque J.F., Harris M.F., Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 20.Kruse C.S., Karem P., Shifflett K., Vegi L., Ravi K., Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henschke N., Kamper S.J., Maher C.G. The epidemiology and economic consequences of pain. Mayo Clin Proc. 2015;90(1):139–147. doi: 10.1016/j.mayocp.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Stein D.J., Scott K.M., de Jonge P., Kessler R.C. Epidemiology of anxiety disorders: from surveys to nosology and back. Dialogues Clin Neurosci. 2017;19(2):127–136. doi: 10.31887/DCNS.2017.19.2/dstein. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.