Abstract
BACKGROUND
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion.
CASE SUMMARY
We present a patient with obstructive jaundice who was diagnosed with IPNB using cholangioscopy during endoscopic retrograde cholangio-pancreatography. Using the SpyGlass DS II technology, we were able to define tumor extension and obtain targeted Spy-byte biopsies. After multidisciplinary evaluation, the patient was scheduled for surgical resection of the tumor, which was radically removed.
CONCLUSION
Cholangioscopy appears to be crucial for the rapid and clear diagnosis of lesions in the bile duct to achieve radical surgical resection.
Keywords: Intraductal papillary neoplasm, Cholangioscopy, Bile duct, Surgical resection, SpyGlass, Case report
Core Tip: Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion. We present a patient with obstructive jaundice who was diagnosed with IPNB using cholangioscopy during endoscopic retrograde cholangio-pancreatography. Using the SpyGlass DS II technology we were able to define tumor extension and to obtain targeted Spy-byte biopsies. The patient underwent successful surgical rsection of the tumor.
INTRODUCTION
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare variant of bile duct tumors, characterized by an exophytic growth exhibiting a papillary mass within the bile duct lumen and it can be localized anywhere along the biliary tree, with morphological variations and occasional invasion. IPNB can be classified into extra-hepatic IPNB and intra-hepatic IPNB. Surgical resection is the first-line treatment and the prognosis of this tumor is better than that of cholangiocarcinoma[1,2].
CASE PRESENTATION
Chief complaints
A 72-year-old male patient was admitted to our hospital due to obstructive jaundice and abdominal pain.
History of present illness
He was a pacemaker carrier and had a history of significant cardiovascular comorbidities.
History of past illness
No significant past illnesses, apart from cardiovascular disorders.
Personal and family history
No family history of gastrointestinal tumors.
Physical examination
On physical examination there was tenderness in the right upper quadrant of the abdomen. Temperature was normal and blood pressure was 100/60 mmHg.
Laboratory examinations
Blood tests showed high direct bilirubin levels (6.5 mg/dL) and altered liver function tests.
Imaging examinations
Computed tomography scan revealed a 3 cm hyperdense mass within the common hepatic duct (CHD). Cholangiography during endoscopic retrograde cholangio-pancreatography (ERCP) confirmed the presence of segmental CHD dilation without clear filling defects in the distal tract (Figure 1).
Figure 1.
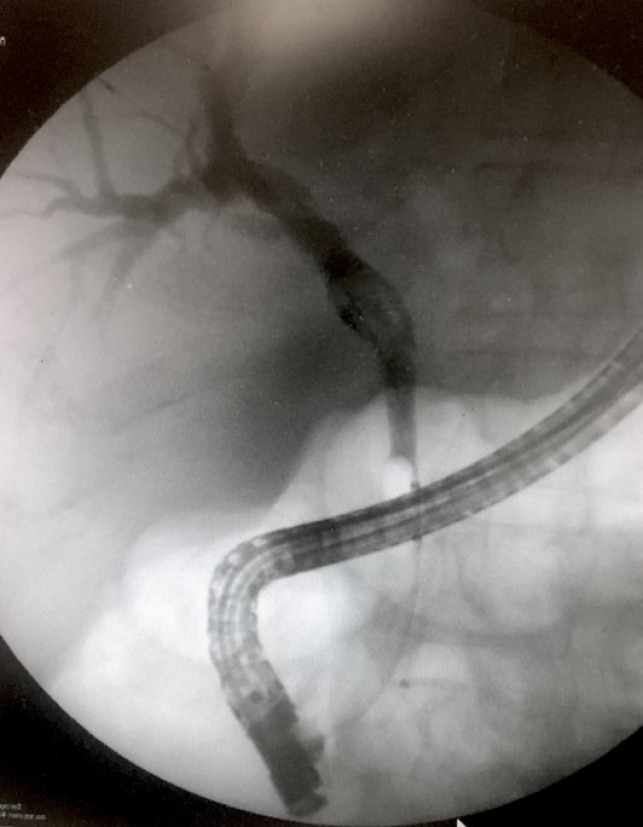
Cholangiography findings during endoscopic retrograde cholangio-pancreatography of the intraductal papillary neoplasm of the bile duct.
FINAL DIAGNOSIS
Peroral cholangioscopy (POC), using the SpyGlass DS II technology (Boston Scientific Ltd., Ireland) was performed. After extensive irrigation due to the presence of secretions, an intraductal papillary mass, characterized by papillary projections with fine vascular cores protruding into the lumen was visualized (Figure 2). The mass involved the CHD and was 1 cm from the hilar bifurcation (Klatskin Tumor type I), extending 1 cm up to the cystic insertion in the CHD. Targeted Spy-byte biopsies were obtained, and the results of pathologic examination were consistent with IPNB.
Figure 2.
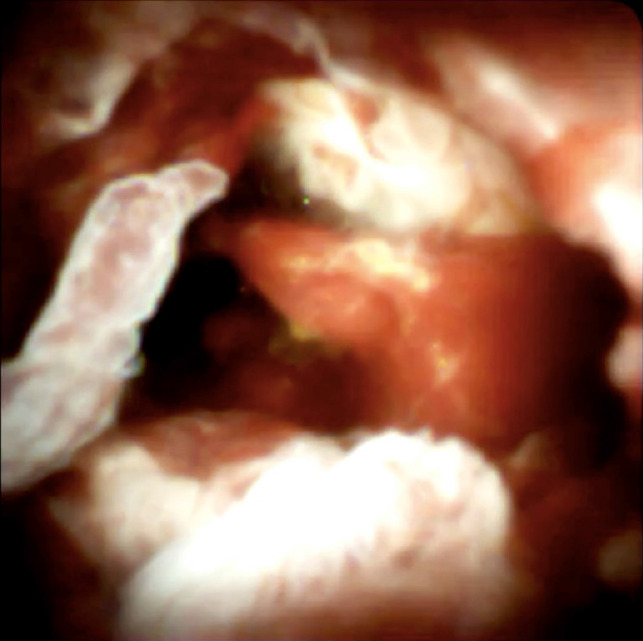
Image of the intraductal papillary neoplasm of the bile duct visualized using the SpyGlass DS II technology.
TREATMENT
After multidisciplinary evaluation, the patient was scheduled for CHD surgical resection, cholecystectomy and hepatico-jejunostomy.
OUTCOME AND FOLLOW-UP
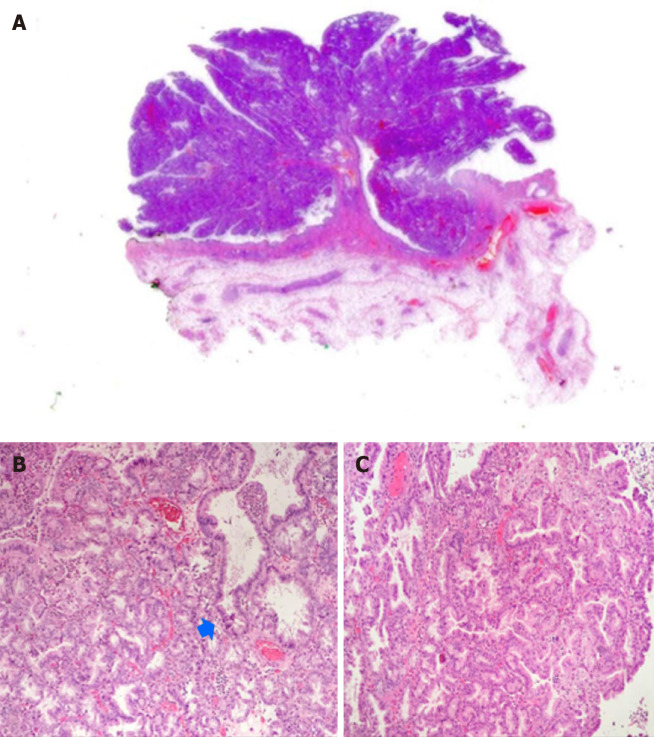
Final pathology showed IPNB within different grades of dysplasia and invasive cancer involving 3% of the lesion, which was radically resected (R0 margins) (Figure 3). The post-operative course was uneventful and a good prognosis is expected at this stage.
Figure 3.
Hematoxylin and eosin staining results. A: Whole section of the intraductal papillary neoplasm of the bile duct with villous silhouette and pseudo-infiltration of the stroma - arrow (1.25 ×); B and C: Foci of marked cytological atypia in papillomatous background architecture (20 ×).
DISCUSSION
POC is an essential tool in the diagnosis and management of undetermined biliary strictures or filling defects, and the accuracy of the direct visual impression during cholangioscopy seems to be greater than that with ERCP. Moreover, POC allows exact localization of the tumor, which is crucial for surgical planning in order to perform a radical resection[3-6].
CONCLUSION
The SpyGlass technology appears to be crucial for the rapid diagnosis and a clear evaluation of the extension of lesions such as IPNB, which can easily be misdiagnosed due to their mucin production and flat appearance.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement: The authors have read the CARE Checklist, and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: August 18, 2020
First decision: September 18, 2020
Article in press: November 4, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Rerknimitr R S-Editor: Chen XF L-Editor: Webster JR P-Editor: Liu JH
Contributor Information
Silvia Cocca, Endoscopy Unit, Azienda Ospedaliero-Universitaria di Modena, Modena 41121, MO, Italy. cocca.silvia@aou.mo.it.
Giuseppe Grande, Endoscopy Unit, Azienda Ospedaliero-Universitaria di Modena, Modena 41121, MO, Italy.
Luca Reggiani Bonetti, Department of Pathologic Anatomy, University of Modena and Reggio Emilia, Modena 41124, MO, Italy.
Paolo Magistri, Hepato-pancreato-biliary Surgery and Liver Transplantation Unit, University of Modena and Reggio Emilia, Modena 41124, MO, Italy.
Stefano Di Sandro, Hepato-pancreato-biliary Surgery and Liver Transplantation Unit, University of Modena and Reggio Emilia, Modena 41124, MO, Italy.
Fabrizio Di Benedetto, Hepato-pancreato-biliary Surgery and Liver Transplantation Unit, University of Modena and Reggio Emilia, Modena 41124, MO, Italy.
Rita Conigliaro, Endoscopy Unit, Azienda Ospedaliero-Universitaria di Modena, Modena 41121, MO, Italy.
Helga Bertani, Endoscopy Unit, Azienda Ospedaliero-Universitaria di Modena, Modena 41121, MO, Italy.
References
- 1.Nakanuma Y, Kakuda Y, Uesaka K. Characterization of Intraductal Papillary Neoplasm of the Bile Duct with Respect to the Histopathologic Similarities to Pancreatic Intraductal Papillary Mucinous Neoplasm. Gut Liver. 2019;13:617–627. doi: 10.5009/gnl18476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lendvai G, Szekerczés T, Illyés I, Dóra R, Kontsek E, Gógl A, Kiss A, Werling K, Kovalszky I, Schaff Z, Borka K. Cholangiocarcinoma: Classification, Histopathology and Molecular Carcinogenesis. Pathol Oncol Res. 2020;26:3–15. doi: 10.1007/s12253-018-0491-8. [DOI] [PubMed] [Google Scholar]
- 3.Bill JG, Chaterjee D, Mullady DK. Using peroral cholangioscopy to diagnose an intraductal papillary neoplasm of the bile duct. VideoGIE. 2020;5:68–71. doi: 10.1016/j.vgie.2019.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korrapati P, Ciolino J, Wani S, Shah J, Watson R, Muthusamy VR, Klapman J, Komanduri S. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E263–E275. doi: 10.1055/s-0042-100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nanashima A, Imamura N, Hiyoshi M, Hamada T, Yano K, Wada T, Kawakami H, Ban T, Kubota Y, Sato Y, Harada K. Planned limited resection of the extrahepatic bile duct in a case of intraductal papillary neoplasm of the bile duct based on preoperative examinations. Clin J Gastroenterol. 2020;13:233–239. doi: 10.1007/s12328-019-01049-8. [DOI] [PubMed] [Google Scholar]
- 6.Ogawa T, Ito K, Koshita S, Kanno Y, Masu K, Kusunose H, Sakai T, Murabayashi T, Hasegawa S, Noda Y. Usefulness of cholangioscopic-guided mapping biopsy using SpyGlass DS for preoperative evaluation of extrahepatic cholangiocarcinoma: a pilot study. Endosc Int Open. 2018;6:E199–E204. doi: 10.1055/s-0043-117949. [DOI] [PMC free article] [PubMed] [Google Scholar]