Abstract
Purpose:
This article describes the Health Access Initiative (HAI), an intervention to improve the general and sexual health care experiences of sexual and gender minority youth (SGMY) by providing training and technical assistance to providers and staff. The training consisted of an online and in-person training, followed by site-specific technical assistance. We present the findings of a pilot evaluation of the program with 10 diverse clinics in Michigan.
Methods:
This program was developed using community-based participatory research principles. Based on a framework of cultural humility, program activities are guided by the Situated Information—Motivation—Behavioral Skills Model. The mixed method program evaluation used training feedback surveys assessing program feasibility, acceptability, and effectiveness; pre/post surveys assessing knowledge, attitudes, and practices toward SGMY; and in-depth interviews with site liaisons assessing technical assistance and structural change.
Results:
The HAI is a highly feasible and acceptable intervention for providers and staff at a variety of health care sites serving adolescents and emerging adults. The results from 10 clinics that participated in the HAI indicate strong intervention efficacy, with significant and meaningful improvements seen in the knowledge of, attitudes toward, and practices with SGMY reported by providers and staff at 6-month follow-up compared with baseline, as well as in qualitative interviews with site liaisons.
Conclusions:
The HAI is a promising intervention to improve the quality of primary and sexual health care provided to SGMY. Expanded implementation with continued evaluation is recommended. The HAI may also be adapted to address specific health needs of SGMY beyond sexual health.
Keywords: Program evaluation, LGBT youth, Sexual and gender minority, Health care providers, Cultural humility, Sexual health
Lesbian, gay, bisexual, transgender (In this article, we are using “transgender” as an umbrella term that is inclusive of transgender, non-binary, and other gender identities that differ from one’s sex assigned at birth.), queer/questioning, and other sexual and gender minority adolescents and emerging adults (“LGBTQ+ youth”) face discrimination and oppression alongside systematic health inequities, which have intersecting and compounding effects [1]. Although variations exist between subpopulations, sexual and gender minority youth (SGMY) experience disproportionate rates of health-related concerns, including sexually transmitted infections (STIs) and HIV; anxiety, depression, and suicide; substance use and misuse; and violence [2—5]. SGMY also experience more housing instability, unemployment, poverty, and incarceration than their heterosexual and cisgender peers [5—9]. These structural and health inequities are worse among transgender youth and SGMY of color [10—12].
SGMY have less access to health care, frequently encounter discriminatory or disrespectful interactions with providers, and have trouble finding providers adept in addressing their specific health needs [13—15], underscoring their need for high-quality health care services [16,17]. These inequities may be amplified when SGMY encounter providers and staff who are not knowledgeable about the unique challenges faced by SGMY and/or are stigmatizing [18]. At present, health care providers (e.g., physicians and nurses) typically receive minimal, if any, training specific to SGM patients, whereas health care staff (e.g., front desk staff and medical assistants) typically receive no training on these topics [19,20]. Thus, efforts focused on training health care providers, and staff on culturally and developmentally appropriate care for SGMY remain a priority [21].
Although there has been a push to increase training on topics related to LGBTQ+ health and SGM patients [14,22], many existing programs have a pre-professional focus (i.e., training for medical and nursing students) or exclude nonclinical staff, although they are often the first people with whom SGMY interact, setting the tone for subsequent health care experiences (c.f., [23,24]). To address these needs, we developed the Health Access Initiative (HAI), a manualized systems-level intervention [25] that includes training and technical assistance (TA) for all providers and staff in health care settings serving adolescents and emerging adults. The HAI was developed by the Michigan Forward in Enhancing Research & Community Equity (MFierce) coalition using community-based participatory research (CBPR) methods [26] and is grounded in a framework of cultural humility [27]. The HAI aims to improve the quality of care provided to SGMY by increasing participants’ knowledge of LGBTQ+ identities, terminology, and unique concerns; improve participants’ attitudes toward working with SGMY; increase affirming practices with SGMY; and implement clinic-level changes to improve the health care experiences of SGMY.
Methods
Intervention development
The MFierce coalition used a process grounded in CBPR principles to develop and implement a structural-level intervention to reduce the burden of STIs on young gay and bisexual men and transgender youth. Although the overarching goal of the coalition was to reduce STI disparities among SGMY most at risk for HIV/STIs (i.e., young gay and bisexual men and transgender youth), there was community demand for inclusive LGBTQ+ content in the training. Therefore, HAI content was designed to be inclusive of SGMY populations (e.g., sexual minority women), although the STI-specific sessions had a greater focus on gay/bisexual young men and transgender youth.
Our coalition included academic partners from public health and psychology disciplines, a Steering Committee of representatives from community-based organizations focused on sexual health and/or SGM populations, and a Youth Advisory Board (YAB) of local LGBTQ+ adolescents and emerging adults. Through community dialogs and participatory decision-making processes, we prioritized SGMY’s lack of access to culturally and developmentally appropriate, high-quality health care, including sexual health care, as the structural factor influencing STI disparities on which we would focus [28], and created the HAI to address this gap. Development of the HAI was led by the academic partners in close collaboration with the YAB and Steering Committee, relying on community and medical provider input throughout the process.
The HAI is grounded in the concept of cultural humility [27] and uses the Situated Information—Motivation—Behavioral Skills model [29] as a theory of behavior change. A cultural competence framework often emphasizes the learner’s mastery of facts about and typical experiences of marginalized populations. As such, cultural competence can place an undue burden on providers to be “competent” in every culture and can result in stereotyping rather than improving interactions and health outcomes. Cultural humility, however, emphasizes that learners engage in a lifelong process of self-reflection and self-critique, challenge power dynamics, commit to understanding and respecting different points of view, and engage with others authentically and from a place of learning [27,30]. To structure intervention activities, we relied on the Situated Information—Motivation—Behavioral Skills model [29], which posits that to change behavior, one must have the correct relevant information, be personally and/or socially motivated to change this behavior, and be equipped with the tools/resources needed to do the behavior within that social-environmental context.
Intervention curriculum
The HAI consists of a 1-hour online training and 2-hour in-person training, followed by 3 months of site-specific TA to improve clinic- and structural-level issues related to LGBTQ+ care (Figure 1). The online training (Access the Health Access Initiative online training free of charge at mfierce.org.) focuses on LGBTQ+ terminology and cultural humility, featuring testimonials from YAB members and health care providers. The in-person training (Supplemental File 1: Health Access Initiative Manual) includes didactic learning methods and group activities on challenging biases and stereotypes, considerations for providing patient-centered care, cultural humility practices, taking a comprehensive and affirming sexual health history, patient-centered STI prevention counseling, and best practices for referrals and resource provision with SGMY. A medical doctor and health educator—both with extensive experience working with SGMY—cofacilitated the in-person trainings. Many but not all trainings (80%) also included a YAB member as a cofacilitator. The TA was unstructured and tailored to each site. HAI staff met with a site liaison before and after the training to identify and address the site’s most pressing needs related to serving SGMY, such as resources, referrals, and reviews of clinic forms and policies.
Figure 1.
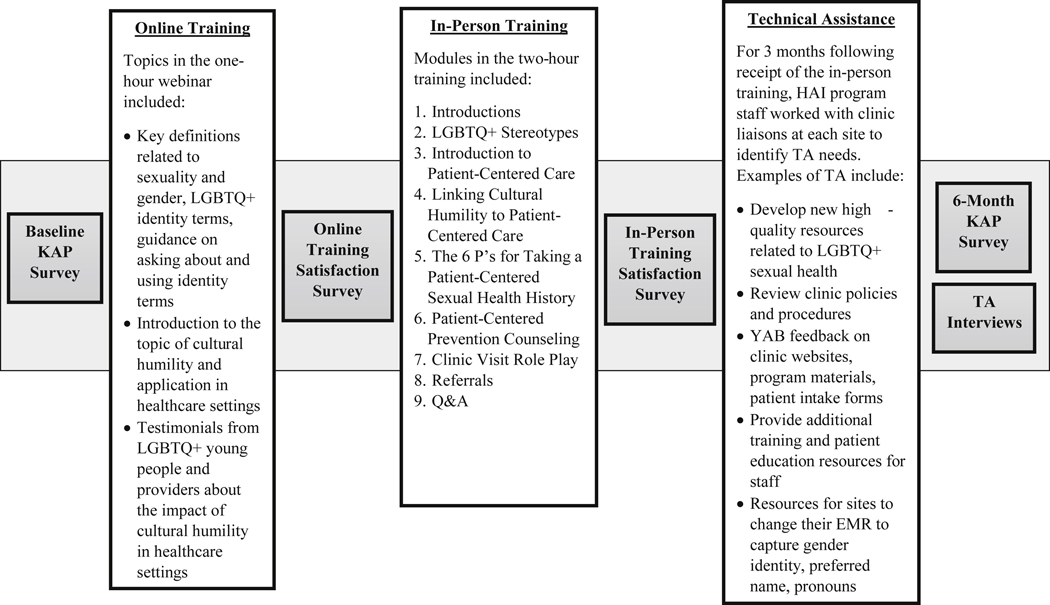
Health access initiative intervention and evaluation components, HAI intervention components, and a summary of their content are included in white boxes below; evaluation activities are included in gray boxes.
Intervention implementation
The HAI was implemented at 10 sites in Southeast Michigan, including three health departments, a school-based health clinic, two community health centers, two youth-specific health centers, a pediatric clinic, and an HIV prevention and treatment clinic. Sites were located in the Detroit Metro Area (n = 5), Flint Metro Area (n = 1), and Ann Arbor-Ypsilanti Area (n = 4). Sites’ main patient populations varied widely in terms of age (n = 1; pediatric clinic, n = 3 exclusively serving adolescents and young adults, and n = 6 serving all ages), socioeconomic status, and racial/ethnic identities. A liaison at each site provided contextual information about the clinic, including their experience with and level of comfort serving SGMY, and coordinated their site’s training and TA. Between these sites, 101 providers and staff completed the online training, and 153 providers and staff completed the in-person training on LGBTQ+ cultural humility practices and sexual health. We provided nursing, social work, and health education continuing education credits for the training free of cost. Following the training, program staff and YAB members provided TA to all 10 sites for approximately 3 months.
Evaluation design
A mixed methods evaluation was used to understand the intervention’s influence on individual and organizational behaviors and the clinic environment. This included a quantitative pre/post survey assessing changes in knowledge, attitudes, and practices (KAP); feedback on training sessions; and in-depth interviews with site liaisons (Figure 1 ).
Training feedback surveys.
Participating providers and staff completed feedback surveys immediately after online and onsite trainings. Surveys assessed the training’s relevance and applicability, the degree to which the content improved participants’ ability to interact with SGMY, participants’ intentions to apply what they learned, and participants’ evaluation of intervention facilitation. In addition, youth and adult members of the coalition conducted semistructured observations of the in-person sessions and provided direct feedback to facilitators.
KAP surveys.
Pre/post surveys assessed changes in participants’ knowledge and attitudes (adapted from the studies by Kelley et al., Maher, and Strong and Folse [24,31,32]), changes in clinic-level practices, individual practices with SGM patients, and perceptions of the clinic environment. Knowledge was assessed with 12 items (e.g., “Sexual orientation identity labels: 1 = are always an accurate reflection of an individual’s sexual behaviors; 2 = are not limited to lesbian, gay, bisexual, queer, questioning, and straight; 3 = are limited to lesbian, gay, bisexual, queer, questioning, and straight; and 4 = cannot change over time”). We computed a sum score based on the tally of correct answers. We used 14 items to measure individual attitudes toward SGMY (e.g., “I would be able to talk with LGBQ+ youth in a sensitive manner”) using a 4-point scale (1 = strongly disagree and 4 = strongly agree). A mean attitude score was estimated (Cronbach’s alpha = .92 at baseline; Cronbach’s alpha = .91 at 6-month follow-up). Clinic practices related to SGMY (13 items; e.g., “Our clinic has educational materials specifically tailored for gay or bisexual young men”) could be answered as yes, no, or do not know. For our analyses, we collapsed answers into a dichotomous variable (0 = no/do not know and 1 = yes) and summed these into a total score. We used four items to examine changes in the frequency of participants’ individual practices with SGM patients (e.g., “use their preferred name”) using a 5-point scale (1 = never and 5 = always). Finally, we examined perceived changes to the clinical environment (e.g., “I am willing to work with my co-workers to create a more affirming clinic for transgender and gender nonconforming youth”) across 4 items that could be answered as yes, no, or do not know. For our analyses, we collapsed these answers into dichotomous variables (0 = no/do not know and 1 = yes).
Limited demographic data related to the site of participation, professional role, age, gender identity, and sexual orientation were collected at the end of the KAP survey. To ensure participants felt comfortable completing a survey with questions related to their performance at work, surveys were completed anonymously and can only be aggregated by the site where the training took place. As such, single participant data cannot be compared across time.
TA interviews.
To measure the provision and impact of TA for providers and staff, TA activities were documented, and in-depth interviews were conducted with site liaisons after the provision of TA. An assistant not involved in program implementation conducted phone interviews.
Analytic methods
A total of 101 providers and staff completed the feedback survey for the online training, and 153 completed the feedback survey for the onsite training. To examine the overall acceptability and satisfaction of participants with the online and onsite trainings, we used descriptive statistics to calculate the mean response and standard deviation (SD) across items, as well as the percentage of the sample that responded “agree” or “strongly agree.”
A total of 153 providers and staff completed the baseline KAP survey, and 80 completed the 6-month follow-up KAP survey. Subsequent analyses are presented as site-aggregated scores to reflect changes at the agency-level rather than individual-level changes. To measure changes in KAP over time, we first aggregated participant responses into the site where the training occurred, given the anonymous nature of the baseline and follow-up surveys. Using these site-aggregated scores, we used paired-samples t tests to examine the differences from pretest to post-test in our outcomes and estimated Cohen’s d as our indicator of effect size [33]. We used the corrected Cohen’s d formula for correlated comparisons in a one-sample design proposed by Rosenthal [34]. Given the relatively small number of sites (n = 10) and overall participants (n = 153) in this pilot intervention, we present findings that are significant at both the p < .05 and p < .10 levels. Effect sizes [35] are interpreted using Cohen’s original thresholds: trivial (d < .20), small (.20 ≤ d < .50), moderate (.50 ≤ d ≤ .80), and large (d > .80).
In-depth interviews with site liaisons to assess TA were analyzed using a Rapid Content Analysis [36] approach. Members of the research team took extensive notes while listening to the interviews and categorized arising themes related to participants’ experiences with the HAI and receiving TA and recommendations for future improvements.
Results
Participant characteristics
Demographic data on participants collected during the baseline KAP surveys are presented in Table 1. HAI participants were diverse in terms of the type of health care setting in which they worked, their professional role, age, and sexual orientation.
Table 1.
Health access initiative participant characteristics
| Onsite training participants (n = 153) | N | Percentage of total sample |
|---|---|---|
| Healthcare setting (n = 153) | ||
| Community health center (two sites) | 31 | 20.2% |
| Adolescent health clinic (two sites) | 24 | 15.7% |
| Health department (three sites) | 40 | 26.1% |
| Adolescent HIV clinic (one site) | 30 | 19.6% |
| Pediatric clinic (one site) | 15 | 9.8% |
| School-based health clinic (one site) | 13 | 8.5% |
| Professional role (n = 153)a | ||
| Medical doctor, physician’s assistant | 12 | 7.8% |
| Nurse practitioner, nurse | 48 | 31.4% |
| Medical assistant, certified nursing assistant | 4 | 2.6% |
| Social worker | 16 | 10.4% |
| Psychologist, counselor | 14 | 9.2% |
| Administrator, medical office clerk | 26 | 17.0% |
| Health educator, HIV test counselor | 26 | 17.0% |
| Community health worker/peer support/outreach | 7 | 4.6% |
| CEO/executive director | 2 | 1.3% |
| Age (n = 151) | ||
| 20–29 | 33 | 21.9% |
| 30–39 | 34 | 22.5% |
| 40–49 | 37 | 24.5% |
| 50–59 | 34 | 22.5% |
| 60+ | 13 | 8.6% |
| Gender (n = 151) | ||
| Cisgender women | 126 | 83.4% |
| Cisgender men | 23 | 15.2% |
| Transgender/genderqueer/gender nonconformingb | 2 | 1.3% |
| Sexual orientation (n = 149) | ||
| LGBTQ+ | 29 | 19.4% |
| Straight/heterosexual | 120 | 80.5% |
LGBTQ = acronym for lesbian, gay, bisexual, transgender and queer.
Percentages total >100% as many participants reported filling multiple roles.
These categories have been collapsed together due to small sample size.
Training feedback
Post-training feedback data were collected after the online training (n = 101) and onsite trainings (n = 153) across the 10 sites. Overall, participants were highly satisfied with the online and onsite trainings (with >90% agreeing or strongly agreeing with satisfaction items). Participants also found the trainings useful (with >90% agreeing or strongly agreeing with usefulness items) and impactful (with 78%—97% agreeing or strongly agreeing to impact items; Table 2). In response to open-ended questions, participants commented on the high relevance of and high usefulness of many aspects of the training, including understanding cultural humility, learning LGBTQ+ terminology, especially related to gender identity and expression; the role-play demonstration; interactive discussions that included an LGBTQ+ young adult and medical provider; learning techniques for taking an inclusive sexual health history; and learning STI screening guidelines. Training participants commonly reported the desire for additional in-depth training on some of the topics highlighted in the training (e.g., use of pre-exposure prophylaxis to prevent HIV, working with parents and families, and policy change to support LGBTQ+ people), and recommendations to expand the cultural humility-grounded program to include trainings focused on additional health topics (e.g., mental health services) and/or additional identities (e.g., immigrant populations and religious minorities). Write-in responses were overwhelmingly but not universally positive. One participant did not find the training highly useful because they already knew most of the content; another participant shared their disagreement with the statement made in the training that “sexuality is a spectrum, and heterosexuality should not be assumed as a default.” Some participants expressed a desire for the in-person training to be longer or to have additional sessions.
Table 2.
Satisfaction with online and on-site training
| Mean (SD) | Percentage agree/strongly agree | |
|---|---|---|
| Webinar | ||
| Satisfaction with webinar | ||
| Overall, I was satisfied with this webinar. (range: 1–5) | 4.40 (.76) | 93.07% |
| The webinar narrator was an effective presenter. (range: 1–5) | 4.38 (.76) | 95.05% |
| The information was presented in ways I could clearly understand. (range: 1–5) | 4.34 (.86) | 90.10% |
| Usefulness of webinar | ||
| The training content was of interest to me professionally. (range: 1–5) | 4.51 (.66) | 95.96% |
| The training content is relevant to my day-to-day work life. (range: 1–5) | 4.43 (.72) | 91.84% |
| Impact of webinar | ||
| My understanding of the subject matter has improved as a result of having participated in this training. (range: 1–5) | 4.33 (.66) | 94.79% |
| My interest in developing/conducting activities aimed at LGBTQ+ cultural humility practices has increased as a result of having participated in this training. (range: 1–5) | 4.21 (.82) | 80.21% |
| My ability to develop/conduct activities aimed at LGBTQ+ cultural humility practices has increased as a result of having participated in this training. (range: 1–5) | 4.19 (.80) | 81.25% |
| I intend to apply what I learned in this training to my work. (range: 1–5) | 4.52 (.65) | 96.88% |
| I have identified actions I will take to apply information I learned from this training in my work. (range: 1–5) | 4.38 (.74) | 89.58% |
| Onsite training | ||
| Satisfaction with onsite training | ||
| Overall, I was satisfied with this training. (range: 2–5) | 4.68 (.58) | 94.70% |
| The facilitators engaged the participants. (range: 3–5) | 4.75 (.50) | 96.03% |
| The information was presented in ways I could clearly understand. (range: 3–5) | 4.81 (.41) | 99.34% |
| Usefulness of onsite training | ||
| The training content was of interest to me professionally. (range: 3–5) | 4.68 (.57) | 94.70% |
| The training content is relevant to my day-to-day work life. (range: 2–5) | 4.54 (.68) | 90.73% |
| Impact of onsite training | ||
| My understanding of the subject matter has improved as a result of having participated in this training. (range: 2–5) | 4.47 (.70) | 90.79% |
| My interest in developing/conducting activities aimed at LGBTQ+ cultural humility practices has increased as a result of having participated in this training. (range: 2–5) | 4.32 (.82) | 82.78% |
| My ability to develop/conduct activities aimed at LGBTQ+ cultural humility practices has increased as a result of having participated in this training. (range: 2–5) | 4.34 (.74) | 86.67% |
| I intend to apply what I learned in this training to my work. (range: 3–5) | 4.68 (.54) | 96.05% |
| I have identified actions I will take to apply information I learned from this training in my work. (range: 1–5) | 4.30 (.93) | 78.95% |
Response options: 1, strongly disagree; 2, disagree; 3, neutral; 4, agree; 5, strongly agree.
Changes in KAP
Correct knowledge items significantly increased from baseline (mean = 7.22, SD = .71) to the 6-month follow-up (mean = 7.82, SD = .80; t(9) = 3.30; p = .009). We also observed significant positive changes in attitudes from baseline (mean = 3.40, SD = .22) to the 6-month follow-up (mean = 3.61, SD = .17; t(9) = 4.17; p = .002), as well as clinic practices from baseline (mean = 7.22, SD = 1.64) to the 6-month follow-up (mean = 9.95, SD = 1.43; t(9) = 7.43, p ≤ .001).
We noted a decrease in participants’ reported assumptions regarding patients’ heterosexuality from baseline (mean = 2.67, SD = .55) to the 6-month follow-up (mean = 1.93, SD = .35; t(9) = 3.94; p = .003) as well as reported assumptions regarding patients’ gender identity from baseline (mean = 3.26, SD = .55) to the 6-month follow-up (mean = 2.27, SD = .47; t(9) = 6.31; p ≤ .001). We did not observe significant changes in participants’ reported use of SGMY’s preferred names or pronouns (Table 2). We found improved changes in sites’ endorsement of environmental changes, including their perception that their clinical environment is a safe space for gay and bisexual youth (baseline: mean = .90, SD = .10; 6-month follow-up: mean = 1.00; SD = 0; t(9) = 3.14; p = .001) as well as transgender and gender nonconforming youth (baseline: mean = .87, SD = .13; 6-month follow-up: mean = .99; SD = .02; t(9) = 3.44; p = .007). We observed ceiling effects on sites’ willingness to create more affirming spaces for LGBTQ+ youth (Table 3).
Table 3.
Changes in knowledge, attitudes, and practices
| Indicator | Baseline, mean (SD) | 6 months, mean (SD) | t test | p value | Effect size, Cohen’s d |
|---|---|---|---|---|---|
| Knowledge total score (range: 0–12) | 7.22 (.71) | 7.82 (.80) | 3.30 | .009a | 1.04 |
| Attitudes total score (range: 1–4) | 3.45 (.20) | 3.64 (.17) | 4.03 | .003a | 1.26 |
| Clinic practices total score (range: 0–13) | 7.22 (1.64) | 9.95 (1.43) | 7.43 | .001a | 2.35 |
| Individual practices (range: 1–5) | |||||
| Use their preferred name. | 4.72 (.23) | 4.76 (.34) | .46 | .657 | .15 |
| Use their preferred pronouns. | 4.51 (.25) | 4.55 (.34) | .45 | .661 | .14 |
| Assume they are heterosexual unless they tell me otherwise. | 2.67 (.55) | 1.93 (.35) | −3.94 | .003a | 1.25 |
| Assume they identify with their sex assigned at birth unless they tell me otherwise. | 3.26 (.55) | 2.27 (.47) | −6.31 | .001a | 2.00 |
| Perceived environment (range: 0–1) | |||||
| Overall, I think our clinic is a safe space for gay and bisexual young men. | .90 (.10) | 1.00 (0) | 3.14 | .012a | .99 |
| Overall, I think our clinic is a safe space for transgender and gender nonconforming youth. | .87 (.13) | .99 (.02) | 3.44 | .007a | 1.09 |
| I am willing to work with my co-workers to create a more affirming clinic for transgender and gender nonconforming youth. | .98 (.04) | 1.00 (0) | 1.96 | .082b | .62 |
| I am willing to work with my co-workers to create a more affirming clinic for gay and bisexual young men. | .98 (.04) | 1.00 (0) | 1.96 | .082b | .62 |
Significant at p < .05.
Significant at p < .10.
Technical assistance
All sites requested materials related to LGBTQ+ sexual health, including resources on creating inclusive environments, sexual health handouts, additional training resources for staff, posters, and resources in other languages. Some sites asked for specific feedback on various programs or materials such as program recruitment advertisements and patient-intake forms. Others requested connections with specific people and organizations, which intervention staff helped initiate. Although existing materials were sometimes used, we worked collaboratively with YAB members to create 24 high-quality printed and digital resources for sites. In total, each site received an average of 209 resources or referrals.
Interviews (n = 11 interviews at 10 sites) with site liaisons revealed that the TA led to modifications in language and practices, increased awareness among staff, and greater dialog on how staff can support SGM people. Other changes included increased access to educational materials tailored to their clients’ needs and connections to organizations around Southeastern Michigan. As a result of the TA, 8 of the 10 sites were making changes to their electronic medical record or intake forms to collect patients’ gender identity, pronouns, preferred name, and sexual orientation identity according to best practices. All sites reported an increase in the number of posters inclusive of SGM people, which were mailed to all sites along with other printed resources. There was a tension between the expressed desire of site liaisons and some training participants for a longer in-person training and more in-depth information across all topics while simultaneously maintaining that 2 hours was the maximum amount of clinic time possible that could be devoted to the training. Site liaisons said staff overall were satisfied with the TA provided and desired training on additional topics, as well as a booster training on general LGBTQ+ issues.
Discussion
The HAI was successfully implemented as a systems-level intervention, with both individual and structural changes observed postintervention. Training feedback surveys and interviews with site liaisons indicate that the HAI intervention is highly feasible and acceptable for a wide range of health care settings that serve adolescents and emerging adults with varying levels of experience working with SGMY. Preliminary effectiveness data from the KAP surveys indicated participating in the HAI was associated with meaningful improvements in providers’ and staff’s knowledge and attitudes, clinic practices, individual practices, and perceived environment with regard to SGMY. Statistically significant improvements were seen across all dimensions assessed. The only two indicators where significant improvement was not seen were the frequencies with which participants reported using patients’ preferred name and using patients’ preferred pronouns, likely because of the high frequency with which participants reported doing this already at baseline. Changes across these indicators is highly promising. Analysis of in-depth interviews revealed that, overall, sites were satisfied with the TA provided through the HAI, and that it enabled their site to implement a number of environmental and policy changes to create a more welcoming and affirming environment for SGMY.
These findings are of note, especially for sites with limited experience or expertise with LGBTQ+ health. Through initial meetings with sites’ clinic liaisons and information gained by facilitators during the in-person training, we learned that clinics’ perceived levels of experience with sexual and gender minority health varied widely. For example, some sites had a long history of working with transgender youth, whereas other sites were lacking in awareness and affirming practices. The in-person training session was structured but allowed room for facilitators to adjust the amount of time spent in different areas and to tailor discussions to a more introductory or advanced level. This fact, combined with the provision of TA tailored to each site’s needs, meant that the HAI could be implemented in a way that was consistent with the principles of cultural humility, asking about and then responding to the unique needs of each site. Although the same overall topics were covered with each clinic, some sites needed a more detailed introduction, whereas others were ready for deeper conversations. Because of this, site liaisons were extremely important. They were necessary for the coordination of onsite trainings and TA, and they were useful as a champion at their site, encouraging their colleagues to participate in trainings and complete evaluations as well as working with leadership to implement structural changes. Collectively, this suggests that the intervention holds promise for addressing the needs of diverse clinics. Findings from feedback surveys allowed the intervention staff to make training facilitation and content adjustments along the way and indicate the need for slight modifications to the final curriculum to structure opportunities for participants to identify specific actions they will take to apply the information learned to their work.
Strengths, limitations, and implications
The current analysis focuses on individual- and clinic-level changes after participation in the HAI. Although intended as a structural-level intervention, the project funding period limited the extent to which we could examine these systemic changes; a study by Kazaleh Sirdenis et al. provides more details on the MFierce coalition and initial HAI structural level changes [37]. We recognize that we would require a longer follow-up period to monitor and evaluate how HAI created improvements in health outcomes (i.e., greater screening and treatment of STIs). Although we asked sites to provide HIV and STI testing and treatment data before and after participation in the HAI, our ability to capture these data in a consistent way across agencies was not possible, given the absence of a harmonized STI reporting tool. Future research examining the impact of HAI on STIs might benefit from a longer study period to capture changes in STI testing over time, as well as allow for the systematic collection of data across diverse types of agencies (e.g., electronic medical records). Additional research examining the long-term effects of the HAI on clinic and health outcomes is warranted.
We allowed HAI participants to take the pre/post surveys anonymously to protect their confidentiality and in hope that they would answer more honestly about workplace attitudes and performance. This meant we were unable to follow up with individual participants who had not completed the 6-month follow-up survey. Nevertheless, given the HAI’s focus on system-level changes, our site-level aggregated outcomes and analyses attenuate retention-related concerns. We were unable to tell if there were group differences between the participants who completed the evaluation at baseline and at 6 months. To increase follow-up completion rates and to allow assessment of changes within individual participants, future iterations should track respondents with a unique identifier. Because the overarching coalition goal was to reduce STI disparities among SGMY most at risk of HIV, some evaluation items (perceived environment) were specific to young gay and bisexual men and transgender youth; in the future, items should be added specific to young lesbian and bisexual women as well. Finally, responses to the survey items that ask about clinic-level practices reflect participants’ awareness of these factors but do not necessarily evaluate staff’s adoption of these changes. In future iterations, a more structured pre/post interview with site liaisons including a quality assurance component could assess these changes.
Using CBPR methods to identify the type of intervention and receive iterative feedback throughout the development and implementation of the HAI contributed to the success of this pilot by increasing community buy-in and drawing on the diverse experiences and expertise of community and coalition members. Collaborative facilitation was another strength; the online training included testimonials from SGMY about their own health care experiences as well as experienced health care providers, and the onsite trainings were facilitated by a team that included a medical doctor, a health educator, and (often) a YAB member.
Ultimately, the HAI shows promise as a training intervention for both providers and staff in health care settings to improve knowledge and attitudes toward SGMY, particularly regarding sexual health. Although several other trainings aiming to improve health outcomes for SGM people have similarly reported significant improvements in training participants’ knowledge and attitudes [21,38—40], several aspects of the HAI intervention and evaluation extend this work by offering valuable contributions. Not only was the training received in a variety of health care settings but also the intervention resulted in meaningful improvements in KAP while providing TA to providers and staff across health sectors, specialties, and focus populations. Given these promising results, the HAI should be implemented and evaluated with a larger sample with individual-level data for pre/post-tests to more comprehensively examine the efficacy of the HAI. Multilevel models examining how systems-level changes also contribute to improvements in individual-level staff outcomes, as well as in patients’ health outcomes, are needed.
Although the MFierce coalition sought to reduce STI inequities specifically among young gay and bisexual men and transgender youth, the core of the curriculum consisted of a cultural humility framework alongside contextual information about the lives of SGMY and health care barriers they may face. This framework and contextual information were used when providing examples of how providers and staff can effectively take a sexual history or discuss prevention options with SGMY patients. Thus, the emphasis on culturally sensitive care for SGMY that served as a backbone for the training intervention could be used for health issues outside of sexual health. The authors are currently adapting the HAI curriculum to focus on mental health and substance use among SGMY in addition to cultural humility practices. Given the positive results of the HAI across 10 clinics, adapting the curriculum and expanding implementation across a greater number of sites holds promise in further addressing the various health inequities faced by SGMY.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
The Health Access Initiative, a cultural humility-based manualized training and technical assistance program to improve general and sexual health care services for SGMY, is a highly feasible and acceptable intervention. Across settings, significant and meaningful improvements were seen in providers’ and staff’s knowledge, attitudes, and practices with SGMY.
Acknowledgments
The authors would like to thank the following individuals, groups, and entities for their contributions to this study: This project was supported by the Centers for Disease Control and Prevention’s Community Approaches to Reducing Sexually Transmitted Diseases (STD) Initiative (U22 PS004520–01). The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. Government. The authors thank the MFierce Advocacy Collective and the organizations that participated in the MFierce Steering Committee, including UNIFIED—HIV Health and Beyond, Wellness Services, Inc., the Detroit Health Department STD/HIV [17 Prevention, Michigan Department of Health & Human Services (Division of HIV & STD Programs), and LGBT Detroit. The authors thank the many community partners, investigators, staff, and [18 students who, over many years, contributed to the partnerships that led to this program. The authors thank Dr Maureen Connelly and Dr Kathy Fessler for their cofacilitation of the program and for their invaluable input on the curriculum content and delivery. Finally, the authors thank the clinics, providers, and staff that participated in the Health Access Initiative.
The role of the study sponsor—the Centers for Disease Control and Prevention’s Community Approaches to Reducing STDs Initiative—is described in the following statements. (1) The study sponsor required the reporting of certain variables in the evaluation. (2) The study sponsor was not involved in the collection, analysis, or interpretation of the data. (3) The study sponsor was not involved in the writing of this manuscript. (4) The study sponsor was not involved in the decision to submit this manuscript for publication. The first draft of the manuscript was written by L.J.-C., J.C., and J.B. No honorarium, grant, or other form of payment was given to anyone to produce this manuscript.
Footnotes
Supplementary Data
Supplementary data related to this article can be found at http://doi.org/10.1016/jjadohealth.2020.01.013.
Conflicts of interest: No conflicts of interest have been identified.
References
- [1].Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: Research evidence and clinical implications. Pediatr Clin North Am 2016; 63:985–97. [DOI] [PubMed] [Google Scholar]
- [2].Wood SM, Salas-Humara C, Dowshen NL. Human immunodeficiency virus, other sexually transmitted infections, and sexual and reproductive health in lesbian, gay, bisexual, transgender youth. Pediatr Clin North Am 2016; 63:1027–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Connolly MD, Zervos MJ, Barone CJ 2nd, et al. The mental health of transgender youth: Advances in understanding. J Adolesc Health 2016;59: 489–95. [DOI] [PubMed] [Google Scholar]
- [4].Ploderl M, Tremblay P. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry 2015;27:367–85. [DOI] [PubMed] [Google Scholar]
- [5].James SE, Herman JL, Rankin S, et al. The report of the 2015 U.S. Transgender survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- [6].Keuroghlian AS, Shtasel D, Bassuk EL. Out on the street: A public health and policy agenda for lesbian, gay, bisexual, and transgender youth who are homeless. Am J Orthopsychiatry 2014;84:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Krause KD, Kapadia F, Ompad DC, et al. Early life psychosocial stressors and housing instability among young sexual minority men: The P18 cohort study. J Urban Health 2016;93:511–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Raiford JL, Hall GJ, Taylor RD, et al. The role of structural barriers in risky sexual behavior, victimization and readiness to change HIV/STI-related risk behavior among transgender women. AIDS Behav 2016;20:2212–21. [DOI] [PubMed] [Google Scholar]
- [9].Wilson BDM, Jordan SP, Meyer IH, et al. Disproportionality and disparities among sexual minority youth in custody. J Youth Adolesc 2017;46: 1547–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bowleg L “Once You’ve Blended the Cake, You Can’t Take the Parts Back to the Main Ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles 2013;68:754–67. [Google Scholar]
- [11].Reed SJ, Miller RL. Thriving and adapting: Resilience, sense of community, and syndemics among young black gay and bisexual men. Am J Community Psychol 2016;57:129–43. [DOI] [PubMed] [Google Scholar]
- [12].Wilson BDM, Harper GW. Race and ethnicity in lesbian, gay, and bisexual communities In: Patterson CJ, D’Augelli AR, eds. Handbook of psychology and sexual orientation. New York, NY: Oxford University Press; 2013:281–96. [Google Scholar]
- [13].Macapagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health 2016;3:434–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gridley SJ, Crouch JM, Evans Y, et al. Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. J Adolesc Health 2016;59:254–61. [DOI] [PubMed] [Google Scholar]
- [15].Snyder BK, Burack GD, Petrova A. LGBTQ youth’s perceptions of primary care. Clin Pediatr 2017;56:443–50. [DOI] [PubMed] [Google Scholar]
- [16].Meanley S, Gale A, Harmell C, et al. The role of provider interactions on comprehensive sexual healthcare among young men who have sex with men. AIDS Educ Prev 2015;27:15–26. [DOI] [PubMed] [Google Scholar]
- [17].Bauermeister JA, Pingel ES, Jadwin-Cakmak L, et al. The use of mystery shopping for quality assurance evaluations of HIV/STI testing sites offering services to young gay and bisexual men. AIDS Behav 2015;19: 1919–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Eaton LA, Earnshaw VA, Maksut JL, et al. Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. J Behav Med 2018;41:458e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 2011;306:971–7. [DOI] [PubMed] [Google Scholar]
- [20].Bonvicini KA. LGBT healthcare disparities: What progress have we made? Patient Educ Couns 2017;100:2357–61. [DOI] [PubMed] [Google Scholar]
- [21].Sekoni AO, Gale NK, Manga-Atangana B, et al. The effects of educational curricula and training on LGBT-specific health issues for healthcare students and professionals: A mixed-method systematic review. J Int AIDS Soc 2017;20:21624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Cohen R Medical students push for more LGBT health training to address disparities. Available at: https://www.npr.org/sections/health-shots/2019/01/20/683216767/medical-students-push-for-more-lgbt-health-training-to-address-disparities. Accessed January 28, 2019.
- [23].Braun HM, Garcia-Grossman IR, Quinones-Rivera A, et al. Outcome and impact evaluation of a transgender health course for health profession students. LGBT Health 2017;4:55–61. [DOI] [PubMed] [Google Scholar]
- [24].Kelley L, Chou CL, Dibble SL, et al. A critical intervention in lesbian, gay, bisexual, and transgender health: Knowledge and attitude outcomes among second-year medical students. Teach Learn Med 2008;20:248–53. [DOI] [PubMed] [Google Scholar]
- [25].Bauermeister JA, Tross S, Ehrhardt AA. A review of HIV/AIDS system-level interventions. AIDS Behav 2009;13:430–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Publ Health 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- [27].Tervalon M, Murray-García J. Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved 1998;9:117–25. [DOI] [PubMed] [Google Scholar]
- [28].Bauermeister JA, Pingel ES, Sirdenis TK, et al. Ensuring community participation during program planning: Lessons learned during the development of a HIV/STI program for young sexual and gender minorities. Am J Community Psychol 2017;60:215–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Amico KR. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): An IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol 2011;16:1071–81. [DOI] [PubMed] [Google Scholar]
- [30].Hook JN, Davis DE, Owen J, et al. Cultural humility: Measuring openness to culturally diverse clients. J Couns Psychol 2013;60:353–66. [DOI] [PubMed] [Google Scholar]
- [31].Maher A Transgender health for nurses: Evaluation of nursing students’ knowledge and beliefs before and after transgender curriculum integration. Chicago, IL: APHA Annual Meeting and Exposition; 2015. [Google Scholar]
- [32].Strong KL, Folse VN. Assessing undergraduate nursing students’ knowledge, attitudes, and cultural competence in caring for lesbian, gay, bisexual, and transgender patients. J Nurs Educ 2015;54:45–9. [DOI] [PubMed] [Google Scholar]
- [33].Calculating Lakens D. and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front Psychol 2013;4: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rosenthal R Meta-analytic procedures for social research. Newbury Park, CA: SAGE Publications Incorporated; 1991. [Google Scholar]
- [35].Hemphill JF. Interpreting the magnitudes of correlation coefficients. Am Psychol 2003;58:78–9. [DOI] [PubMed] [Google Scholar]
- [36].Krippendorff K Content analysis: An introduction to its methodology. 3rd edition Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- [37].Kazaleh Sirdenis T, Harper GW, Carrillo M, et al. Toward sexual health equity for gay, bisexual and transgender youth: An inter-generational collaborative multi-sector partnerships approach to structural change. Health Educ Behav 2019;46(1_suppl):88Se99S. [DOI] [PubMed] [Google Scholar]
- [38].Bristol S, Kostelec T, MacDonald R. Improving emergency health care workers’ knowledge, competency, and attitudes toward lesbian, gay, bisexual, and transgender patients through interdisciplinary cultural competency training. J Emerg Nurs 2018;44:632–9. [DOI] [PubMed] [Google Scholar]
- [39].Lelutiu-Weinberger C, Pollard-Thomas P, Pagano W, et al. Implementation and evaluation of a pilot training to improve transgender competency among medical staff in an urban clinic. Transgend Health 2016;1:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Radix A, Maingi S. LGBT cultural competence and interventions to help oncology nurses and other health care providers. Semin Oncol Nurs 2018; 34:80–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


