Abstract
Patellofemoral pain (PFP) is among the most common injuries in recreational runners. Current evidence does not identify alignment, muscle weakness, and patellar maltracking or a combination of these as causes of PFP. Rather than solely investigating biomechanics, we suggest a holistic approach to address the causes of PFP. Both external loads, such as changes in training parameters and biomechanics, and internal loads, such as sleep and psychological stress, should be considered. As for the management of runners with PFP, recent research suggested that various interventions can be considered to help symptoms, even if these interventions target biomechanical factors that may not have caused the injury in the first place. In this Current Concepts article, we describe how the latest evidence on education about training modifications, strengthening exercises, gait and footwear modifications, and psychosocial factors can be applied when treating runners with PFP. The importance of maintaining relative homeostasis between load and capacity will be emphasized. Recommendations for temporary or longer-term interventions will be discussed. A holistic, evidence-based approach should consist of a graded exposure to load, including movement, exercise, and running, while considering the capacity of the individual, including sleep and psychosocial factors. Cost, accessibility, and the personal preferences of patients should also be considered.
Keywords: running, education, gait, exercise, psychosocial factors
Patellofemoral pain (PFP) is defined as pain around or behind the patella that is aggravated by at least 1 activity that loads the patellofemoral joint (PFJ) during weight bearing on a flexed knee.1 Patellofemoral pain is known as “runner's knee” for a reason. The knee is the most commonly injured body part in distance runners, and PFP represents as much as 13% to 30% of medical consultations for running-related injuries.2,3 These high percentages support the need to better understand risk factors for the condition and identify the most effective and clinically applicable treatment approaches based on current scientific evidence.
Historically, the main focus of PFP researchers has been on pathoanatomic and kinesiopathologic concepts, such as abnormal PFJ anatomy; impaired quadriceps function; altered foot, hip, and trunk kinematics; and muscle tightness.4 Concepts such as running kinematics and kinetics and muscle strength have dominated the field such that a biomechanical rationale for PFP is commonly accepted within the medical community.4 However, specific features that have been identified in runners with PFP compared with asymptomatic runners may sometimes be wrongfully interpreted as causes of the condition. The presence of a feature in symptomatic runners could simply be a consequence of pain and not its cause. When treating patients with PFP, clinicians must not lose sight of how muscle strength, kinetics, and kinematics interact with training loads and nonmechanical factors, such as the capacity of the body to recover or psychosocial aspects. Decreasing the load on an irritated PFJ via biomechanical interventions could be warranted, even though the load may not have caused the injury in the first place.
The same patient could potentially benefit from multiple treatment approaches, but both evidence and patient preferences should guide a proper shared decision-making approach.5 Rehabilitation professionals should also consider adapting their recommendations to the recent or persistent nature of PFP. Tailoring treatment to the stage of injury is advocated for several sport-related injuries, including ankle sprains,6 muscle injuries,7 tendon conditions,8 and overall injuries in elite athletes.9 Indeed, the recent onset of PFP may only require temporary interventions to decrease load on the irritated joint, whereas a prolonged symptom duration may call for interventions that shift the load away from the PFJ in the longer term, as well as a particular focus on psychosocial aspects.
In this Current Concepts article, we explore a contemporary approach to treating the runner with PFP that encompasses the whole person. Some widely accepted concepts are challenged. We focus on an approach that maximizes patient autonomy and cost effectiveness so that clinical recommendations can be applied to various populations, regardless of socioeconomic status or access to care.
WHY DOES IT HURT?
During running, the ground pushes back on the foot with forces of approximately 2.5 times body weight.10 That vertical ground reaction force is then transmitted up to the knee and the PFJ, resulting in the quadriceps compressing the patella in the femoral trochlea with forces of approximately 4 times body weight.11 Therefore, a runner taking 160 steps per minute loads the PFJ for a total of 320 body weights per minute, or 19 200 body weights per hour. A full marathon completed in the median time of 4 hours and 20 minutes applies a cumulative load beyond 80 000 times the body weight. This impressive amount of compression likely explains why the thickest articular cartilage in the body is found at the PFJ.12
The exact source of nociceptive input remains unclear and is likely to vary among individuals. Previous research13 has demonstrated that articular cartilage is not a source of nociception, which thereby casts doubt on chondromalacia as a significant source of pain. The subchondral bone, synovial membrane, fat pad, and retinacular tissues could all be responsible for nociceptive input.13 Individuals with persistent PFP may also present with pain sensitization, as outlined in a recent systematic review.14
Increased patellar intraosseous pressure could potentially contribute to pain. When compared with 10 asymptomatic female runners, a group of 10 female runners with retropatellar pain exhibited greater water content, or subchondral edema, in their patella.15 Although the cross-sectional nature of that study precluded conclusions about causation, a follow-up study16 linked fluctuations in water content after a 40-minute run with variations in the level of retropatellar pain. The total amount of load accumulated in the PFJ should be seen through the number of loading cycles (eg, 800 cycles per knee over 10 minutes, if running at 160 steps per minute) and the magnitude of that load.17 Considering the concept of cumulative load, it is plausible that running above the tissues' capacity for adaptation may explain persistent symptoms in runners with PFP or the onset of PFP in previously asymptomatic runners. Activities other than running (eg, plyometric workouts and stairs) should also be considered in the cumulative load.
EDUCATING PATIENTS ON THE BALANCE BETWEEN LOAD AND CAPACITY
A tissue homeostasis model was proposed by Dye18 in 1996. The model stipulates that to remain healthy, the PFJ requires loads to be applied within the envelope of function that correspond to the maximum capacity of the body to tolerate and recover from load. According to the model, exceeding the load threshold with too much magnitude or frequency or both represents supraphysiologic overload, which disrupts tissue homeostasis and, ultimately, contributes to symptoms. Although this concept seems logical from a clinical perspective, research supporting its role in the pathophysiology of PFP remains scarce.
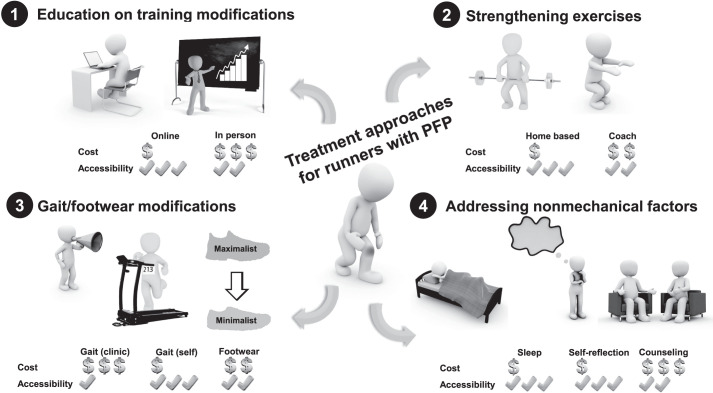
In runners, recent changes in training (eg, increasing distance, speed, and downhill) beyond the level of tissue adaptation are often believed to cause running injuries.19 To date, however, only 1 study20 suggested that novice runners who increased their weekly volume by more than 30% could be more prone to develop distance-based running injuries such as PFP than runners who changed their weekly running distance by less than 10%. This result may be due to the complexity of external load (influenced by, for example, speed,21 hills,22 foot-strike pattern,23 and cadence24) but may also be due to the difficulty of measuring maximum capacity, which may vary greatly among individuals and even among days in the same runner. As proposed by Wiese-Bjornstal,25 the sport injury risk consists of a combination of biological, physical, psychological, and sociocultural factors. Although changing loads on tissues beyond their tolerance must be considered in the pathophysiology of PFP, it is equally important to question patients about recent variations in nonmechanical factors, such as sleep, stress, or anxiety, as they may affect the body's capacity to recover from bouts of running that are usually well tolerated (Figure 1). A recent study in endurance athletes (including runners) outlined poor sleep quality as a significant contributor to injury risk,26 and general sports injuries in adolescents have been linked with a chronic lack of sleep.27 However, information on nonmechanical factors is rarely captured in prospective studies on running injuries. The interaction between variations in capacity related to physiological, psychological, and sociocultural factors and transient changes in training loads could possibly reveal important information for both the prevention and treatment of PFP and should be considered in future research.
Figure 1.
Factors involved in a potential imbalance between load and capacity. Abbreviation: PFP, patellofemoral pain.
Emerging evidence outlined the importance of patient education about activity modifications when treating individuals with PFP,28 even though more work is needed to provide clearer guidelines to clinicians.29 In a randomized clinical trial, Esculier et al30 assigned runners with PFP to 3 arms, all of which received an education component. Specifically, the participants were instructed to reduce their running distance and speed but to increase training frequency. They self-adjusted running training to maintain pain levels at a maximum of 2/10 on a numeric pain rating scale and increased training again based on symptoms. Runners in the second arm also received an exercise program targeting the quadriceps, hip, and trunk muscles. Runners in the third arm were instructed to modify their running pattern to decrease PFJ force (increase the step rate, run more softly, or use a forefoot-strike pattern). Interestingly, all 3 groups reported similar improvements in symptoms and function after the 8-week intervention, as well as at the 20-week follow-up.30 Although they did not discourage clinicians from prescribing exercises and recommending gait modifications, the authors emphasized that appropriate education on activity modification according to symptoms should be a primary component of rehabilitation in runners with PFP. In addition, Rathleff et al31 demonstrated impressive rates of clinical success using a multimodal intervention that combined activity modifications according to symptoms, an exercise program, and return-to-sport guidance in active adolescents with PFP. Participants were instructed to climb the activity ladder toward activities that applied greater loads on the PFJ but only if pain levels did not exceed 2/10. Immediately after their 12-week intervention, 86% of participants reported a successful treatment outcome, and success rates remained high at 6 months (77%) and 12 months (81%).31 According to a recent systematic review from de Oliveira Silva et al,28 education on load management for PFP alone, when delivered by health care professionals, can be as efficient as adding an exercise program to education and more efficient than education handouts.
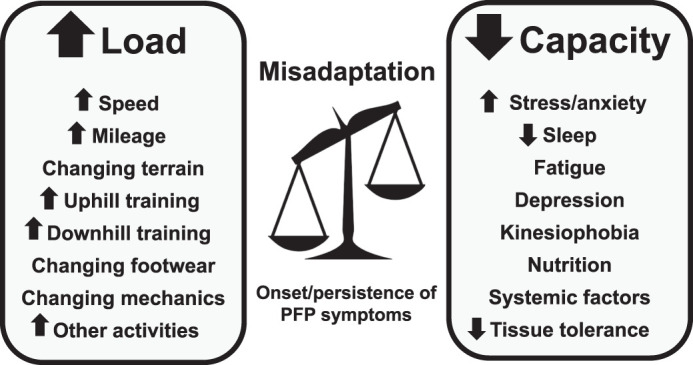
Based on these findings, we believe that education on load management, which can be included in a clinic-based intervention, shows great potential for empowering runners with PFP. Education provided through online tools represents an interesting approach that does not involve extensive time commitments, equipment, or financial resources (Figure 2).
Figure 2.
Components of a contemporary approach to patellofemoral pain (PFP) in runners that considers cost and accessibility.
DOES MUSCLE STRENGTH MATTER?
There is little doubt that individuals with PFP present with strength deficits, especially of the knee extensors and hip abductors, external rotators, and extensors.32–34 Decreased quadriceps strength has been identified as a potential risk factor for PFP in military populations,35 although it has yet to be demonstrated in runners. Decreased hip strength does not seem to be the cause of PFP but rather a consequence of pain. This concept was brought to the forefront by Rathleff et al33 in a systematic review. The authors drew a clear distinction between cross-sectional studies, which showed that individuals with PFP were weaker than their healthy counterparts, and prospective studies, which showed that hip strength was not a risk factor for the onset of PFP. This conclusion makes sense when we analyze the results from Finnoff et al.36 In their prospective cohort study, they provided evidence that, compared with baseline strength values when healthy, the 5 adolescent runners who developed PFP during a running program showed decreases in hip-abductor strength when tested in the presence of pain.
The absence of a cause-and-effect relationship between strength and PFP should not preclude clinicians from prescribing strengthening exercises. Systematic reviews37,38 and clinical guidelines34,39 were unequivocal about their benefits for rehabilitating individuals, including runners, with PFP. A strong level of evidence supports exercise therapy to reduce pain in the short, medium, and long term and improve function in the medium and long term. In particular, exercises targeting both the hip muscles and the quadriceps are recommended to optimize clinical outcomes.40 It must be noted, however, that the positive effects of strengthening are not explained by changes in hip kinematics during running41 and that the mechanisms underlying the benefits of exercise for PFP remain unclear. Optimal exercises and parameters have not yet been identified, due to a lack of reporting consistency among studies in which researchers investigated the effects of exercises on this condition.42
In summary, the current evidence justifies recommending strengthening of the quadriceps, hips, and trunk muscles in runners with PFP using a graded-exposure approach. Nonetheless, patients should be educated that strengthening may not address the main reason why they developed pain in the first place.
WHAT ABOUT “MALTRACKING”?
Anatomical factors previously thought to contribute to patellar maltracking, a concept that is still widely promoted, have been discredited by a large body of research. The quadriceps angle,35 patellar-tilt angle, sulcus angle, and trochlear inclination in those who eventually develop PFP are no different from those who do not, and healthy knees exhibit a high degree of variability.43 Using the maltracking rationale to prescribe exercises specifically to target the vastus medialis obliquus is erroneous in light of current evidence because a combination of hip and knee exercises, and even hip exercises alone,38 consistently yielded better clinical outcomes than quadriceps-only exercises.40 The absence of added benefits of exercises on top of education provided by health care professionals28 also speaks to the weakness of the maltracking theory. Similarly, patellar taping that was once believed to “correct patellar tracking” is now known to have no effects on patellar position.44 Taping is still advised as part of the treatment plan for runners with PFP because it has been shown to reduce symptoms,40 despite the uncertainty regarding the mechanisms by which it helps.
RUNNING MECHANICS: HOW IMPORTANT ARE THEY FOR PREVENTION AND TREATMENT?
Countless authors have tried to pinpoint the link between running kinetics and kinematics and PFP.4 However, through only very limited evidence have researchers established a causative link.45 Most studies that described biomechanical differences between runners with and those without PFP were cross-sectional in nature, thereby preventing any conclusions about a cause-and-effect association. Investigators46 in only 1 study identified proximal lower limb kinematics, namely greater peak hip adduction, as a potential risk factor for PFP in female runners. It must be noted that the runners who developed PFP showed only 4° of increased hip adduction during stance compared with those who did not develop PFP, and whether reducing the angle could help prevent PFP in female runners remains unknown. To date, the only intervention that yielded lower rates of PFP was reducing the vertical loading rate of impact by “running softer.”47 In a prospective randomized study, Chan et al47 reported only 4 cases of PFP in the year after the intervention group was trained to “run softer,” compared with 18 cases in the control group who did not change their running biomechanics. Although an expensive system was used to provide feedback to runners, previous research48 suggested that simple clinician feedback on “softer running,” or making less noise while running, was as effective in decreasing impact as feedback using expensive laboratory instruments.
Describing movement patterns as “faulty” or “abnormal” is potentially erroneous. Until the interaction between running mechanics and changes in training loads and nonmechanical factors is thoroughly studied, the importance of small kinematic differences in the development of PFP cannot be assumed. Cartilage and joints, just like bones and muscles,49 respond to loads applied up to their maximal capacity by increasing their tolerance.50 A runner with “atypical” running mechanics likely adapts to the pattern, and changing it could result in another injury secondary to forces being transferred to other tissues. For the same reasons, current evidence does not support transitioning an uninjured rearfoot-striking runner to a non-rearfoot pattern to prevent injuries.51 It is possible that, similar to muscle strength, kinematic patterns change after the onset of PFP, as a result of pain.52 Just as strengthening exercises target strength deficits (though they are not the cause) in individuals with PFP, gait modifications could be beneficial by decreasing forces at the PFJ45 and helping to restore tissue homeostasis. To address the recent onset of PFP in an experienced runner, a clinician could even consider gait modifications as a temporary intervention and gradually revert to the habitual running biomechanics once symptoms have improved. In a runner with persistent PFP, long-term gait modifications may be advised.
Running-gait modifications can be classified into 2 main approaches, both aimed at reducing PFJ stress during the stance phase, whether by decreasing compression forces in the joint or by distributing forces on a greater joint contact area. The first approach targets frontal- and transverse-plane kinematics and aims to reduce hip adduction, contralateral pelvic drop, and hip internal rotation. These movements are considered problematic by some, as they could increase PFJ stress (ie, the same amount of force on a reduced contact area).53 The benefits of this approach are thought to be an increased contact area for distributing PFJ contact force, which reduces joint stress. To date, in only 2 case series have researchers54,55 reported beneficial effects from reducing hip adduction during running by providing instructions such as “contract your gluteal muscles,” “run with your knees pointing straight ahead,” and “maintain a level pelvis.” Using either a 3-dimensional system54 or a mirror55 placed in front of a treadmill to provide live feedback during running, both studies demonstrated reductions in symptoms up to 3 months after the end of a 2-week intervention. Unfortunately, the applicability of this feedback method is limited to runners with PFP exhibiting “excessive hip adduction” (fewer than 12% of the 85 potential participants screened by Noehren et al54) and to those having access to a treadmill, a piece of equipment that is far from common in many regions of the world.
The second approach targets sagittal-plane kinematics to reduce PFJ loads. This could involve manipulating the foot-strike pattern or step rate (effectively decreasing the step length).56 Reductions in the vertical loading-rate of the ground reaction force and in PFJ contact force can be achieved by changing to a forefoot-strike pattern,57,58 although such a method could overload the distal structures (eg, the foot and Achilles tendon) if implemented too quickly. Unlike a switch in the foot-strike pattern, decreasing the step length by increasing the step rate (typically 7.5%–10%) does not increase the forces applied to the foot59 and could therefore represent the safest way to reduce PFJ kinetics. It can be practiced in the field using a watch,60 music, inexpensive wearable devices,61 or even a cheap metronome. It must be noted that increasing step rate has also been shown to reduce hip adduction and pelvic drop during the stance phase.62
To date, in most gait-retraining studies, researchers47,54–58 have used a time- and resource-consuming, laboratory-based faded-feedback schedule, which involves 8 training sessions over a 2-week period. Although such a schedule may improve the capacity of runners to learn a new motor pattern,63 it is potentially unrealistic for runners living in areas in which specialized professionals are not available or those who cannot afford, both in terms of time and financial resources, repeated visits during a short period of time. Fortunately, recent evidence62 indicated that 1 session of step-rate retraining was effective in increasing the step rate and improving the symptoms and function of runners with PFP. Importantly, the runners maintained the newly acquired running kinematics up to 3 months after the retraining session, thus challenging the need for an intensive, supervised retraining protocol.
In summary, experienced runners may have adapted to their running mechanics, which may not have caused PFP. Suggesting gait modifications could be useful for shifting forces away from the PFJ, especially in cases of persistent PFP. In those with a recent onset and no previous history of PFP, education on training loads may be sufficient to address the imbalance between load and capacity. Gait modifications could also be helpful as a temporary measure to adjust loading.
RUNNING FOOTWEAR: TO CHANGE OR NOT TO CHANGE?
Based on current evidence,64 footwear type does not seem to matter when it comes to preventing overall running injuries. Also, clinical trials assessing the effects of running footwear on the symptoms of injured runners are lacking. However, similar to studies on gait modifications, research comparing lower limb running biomechanics among footwear types could provide a logical framework for clinicians to use when treating runners with PFP.
It is beyond the scope of this paper to list all the authors who have evaluated the effects of minimalist shoes, defined as “footwear providing minimal interference with the natural movement of the foot due to its high flexibility, low heel to toe drop, weight and stack height, and the absence of motion control and stability devices,”65 on knee-joint loading. Yet readers must keep in mind that these investigators rather unanimously reported reductions in knee-joint moments and PFJ force when cushioning was removed. For example, Bonacci et al24 observed 17% less peak patellofemoral force when participants ran using FiveFingers (Vibram Corp, Brookline, MA) than when using traditional shoes. Bonacci et al24 proposed that the effects of gait modifications could potentially be supplemented by combining footwear with a greater degree of minimalism with cues to increase step rate by 10% resulted in 30% lower peak PFJ force. Using the Minimalist Index,65 both Esculier et al66 and Yang et al67 showed that greater levels of minimalism resulted in lower PFJ contact forces, without the need to use extremely minimalist shoes.66 On the flip side, although it may be seen as counterintuitive by many runners, maximalist footwear increased PFJ contact force by 20% per step and 10% per mile compared with traditional shoes.68
By no means should this information be considered an argument for every runner with PFP to transition to minimalist shoes, as no intervention studies showed benefits for symptoms and function. However, as with gait modifications, shifting force away from the PFJ can represent an interesting option for some runners, especially when they have been suffering from recurrent PFP. Even if more research is needed on footwear, the current state of research is similar to early findings on step-rate manipulation, demonstrating that PFJ contact force could be reduced while increasing the step rate.69–71 Yet the first trials demonstrating beneficial effects of this intervention in isolation on pain and function in runners with PFP were published in 201872 and 2019.56,62
When asked by injured runners about which type of footwear could be more efficient for decreasing PFJ force, clinicians can use their knowledge of biomechanical studies to guide their recommendations, similar to gait modifications. Minimalist footwear certainly represents one of the many options available in the treatment approach for runners with PFP, although a gradual transition period must be considered to allow for adaptation of the foot, the ankle and the calf muscle and the Achilles tendon unit.73
WHAT ABOUT NONMECHANICAL FACTORS?
Recently, authors investigating risk factors for running injuries have started to integrate psychosocial outcomes. In a 2-year prospective study of 300 runners, Messier et al74 identified lower mental health-related quality of life and more negative emotions as significant injury predictors. Their influence on injury risk was far from overwhelming, but both factors were more influential than several factors that were classically believed to cause PFP, such as flexibility, quadriceps angle, arch height, rearfoot motion, strength, and footwear. One strength of that study was that psychosocial outcomes were reassessed periodically, at 6 months and 12 months after starting the program as well as after injuries were diagnosed.74 Specifically in PFP, kinesiophobia may exert a greater influence on movement biomechanics than muscle strength.75 In fact, nonphysical constructs such as anxiety and catastrophization are increasingly regarded as important contributors to PFP and should be part of a global treatment approach in injured runners.76
Perfectionism has also recently been linked with a greater risk of sustaining running injuries.77 It is possible that such traits limit the ability of some runners to listen to their body when following their training program, thereby increasing the likelihood of surpassing the body's capacity to tolerate load. Acute physical fatigue leading to alterations in movement patterns has also been identified as a potential contributor to some injuries, including PFP.78 Similarly, overall fatigue could lead to a greater injury risk by affecting the body's capacity to recover. Decreased sleep quality is increasingly considered as a significant injury predictor,26 although the exact mechanisms by which it affects risk remain unclear. Psychological stress is also thought to modulate tissue capacity because higher stress levels have been associated with greater injury risks in triathletes79 and adolescents.80 Rehabilitation professionals can provide basic advice on nonmechanical factors or consider involving other health care professionals (eg, physician, counselor) if specialized advice on sleep or mental health is deemed necessary.
PUTTING IT ALL TOGETHER
As recommended in the latest consensus statement on PFP,40 the optimal treatment approach for runners with PFP likely combines several components, such as education, exercise, and running-specific interventions aimed at reducing PFJ force or modifying footwear. However, different individuals may have different preferences, along with limitations in terms of time, resources, and access to care. All of these factors should be taken into account when planning the treatment approach (Figure 2).
Considering the interaction between mechanical and nonmechanical factors, the concept of balance between load and capacity (Figure 1), and the envelope of function model of Dye,18 experienced runners may have fully adapted to running mechanics that could be perceived as atypical. For example, a runner may well have adapted to a greater vertical impact loading rate, greater peak hip adduction, and maximalist shoes over the previous 10 years but is now seeking help from a health care professional because of the recent onset of PFP. Although rehabilitation professionals may be tempted to address running mechanics in their treatment approach, it is erroneous to assume that any of these factors caused the injury in a well-adapted runner. Changes in factors influencing external load and internal capacity should be addressed to gain a better sense of potential contributors around the time of injury. A stressful family or workplace situation may be enough to affect the body's capacity to recover from training loads that were previously well tolerated. In this example, a clinician who addresses running biomechanics or footwear may miss the actual cause of the injury, or worse, trigger a new injury in a runner who was well adapted to his or her original biomechanics or footwear. Sometimes the best option may simply be to educate the runner on the concept of load and capacity and the changes in external load and internal capacity that the runner experienced before the onset of symptoms.
Assessing runners with PFP in the clinic does not necessarily provide accurate information on what actually caused the injury but rather on what can potentially be targeted in the treatment approach. One could argue that it does not matter whether reduced strength is the cause or consequence of pain because exercise programs successfully improve symptoms and functional limitations. Though the disparity between cross-sectional and prospective study results should not affect the decision whether to prescribe exercises, it should change the mindset of clinicians when implementing the educational component with patients. Telling runners that their PFP was caused by muscle weakness or faulty or abnormal running mechanics (or both) may stimulate kinesiophobia and catastrophization. Ensuring that patients understand the concept of load and capacity and linking them with training and psychosocial factors that were identified in the individual's history are likely to empower patients and break the vicious cycle of less movement, more anxiety, more pain, and less movement.
It is time to move away from a model based solely on alignment, patellar maltracking, muscle weakness, and faulty or abnormal movement patterns to explain the onset of PFP. Although some studies showed the benefits of biomechanical interventions on PFP symptoms in runners, a contemporary multimodal approach to treating runners with PFP should also consider an overall balance between external loads and internal capacity. Patient education on these concepts should represent the main component of the clinical approach, supplemented by exercises and gait or footwear (or both) modifications and addressing psychosocial factors when judged necessary. Recommendations for temporary or long-term interventions may be informed by the recent or persistent nature of PFP. Ultimately, the individualized clinical approach will be based on graded exposure through movement and exercise by maintaining load within the capacity for adaptation, empowering the patient, and accounting for personal preferences.
FINANCIAL DISCLOSURE
Salary support was provided to J.F.E. by the Canadian Institutes for Health Research.
REFERENCES
- 1.Crossley KM, Stefanik JJ, Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839–843. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macintyre JG, Taunton JE, Clement DB, Lloyd-Smith DR, McKenzie DC, Morrell RW. Running injuries: a clinical study of 4,173 cases. Clin J Sport Med. 1991;1(2):81–87. [Google Scholar]
- 4.Powers CM, Witvrouw E, Davis IS, Crossley KM. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: part 3. Br J Sports Med. 2017;51(24):1713–1723. doi: 10.1136/bjsports-2017-098717. [DOI] [PubMed] [Google Scholar]
- 5.Barton CJ, Crossley KM. Sharing decision-making between patient and clinician: the next step in evidence-based practice for patellofemoral pain? Br J Sports Med. 2016;50(14):833–834. doi: 10.1136/bjsports-2015-095607. [DOI] [PubMed] [Google Scholar]
- 6.Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52(15):956. doi: 10.1136/bjsports-2017-098106. [DOI] [PubMed] [Google Scholar]
- 7.Hotfiel T, Seil R, Bily R, et al. Nonoperative treatment of muscle injuries—recommendations from the GOTS expert meeting. J Exp Orthop. 2018;5(1):24. doi: 10.1186/s40634-018-0139-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med. 2016;50(19):1187–1191. doi: 10.1136/bjsports-2015-095422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hainline B, Derman W, Vernec A, et al. International Olympic Committee consensus statement on pain management in elite athletes. Br J Sports Med. 2018;51(17):1245–1258. doi: 10.1136/bjsports-2017-097884. [DOI] [PubMed] [Google Scholar]
- 10.Hamill J, Bates BT, Knutzen KM, Sawhill JA. Variations in ground reaction force parameters at different running speeds. Hum Mov Sci. 1983;2(1–2):47–56. [Google Scholar]
- 11.Willy RW, Halsey L, Hayek A, Johnson H, Willson JD. Patellofemoral joint and Achilles tendon loads during overground and treadmill running. J Orthop Sports Phys Ther. 2016;46(8):664–672. doi: 10.2519/jospt.2016.6494. [DOI] [PubMed] [Google Scholar]
- 12.Neumann DA. Kinesiology of the Musculoskeletal System Foundations for Physical Rehabilitation. St. Louis, MO: Mosby;; 2002. [Google Scholar]
- 13.Post WR, Dye SF. Patellofemoral pain: an enigma explained by homeostasis and common sense. Am J Orthop (Belle Mead NJ) 2017;46(2):92–100. [PubMed] [Google Scholar]
- 14.De Oliveira Silva D, Rathleff MS, Petersen K, Azevedo FM, Barton CJ. Manifestations of pain sensitization across different painful knee disorders: a systematic review including meta-analysis and metaregression. Pain Med. 2019;20(2):335–358. doi: 10.1093/pm/pny177. [DOI] [PubMed] [Google Scholar]
- 15.Ho KY, Hu HH, Colletti PM, Powers CM. Recreational runners with patellofemoral pain exhibit elevated patella water content. Magn Reson Imaging. 2014;32(7):965–968. doi: 10.1016/j.mri.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Ho KY, Hu HH, Colletti PM, Powers CM. Running-induced patellofemoral pain fluctuates with changes in patella water content. Eur J Sport Sci. 2014;14(6):628–634. doi: 10.1080/17461391.2013.862872. [DOI] [PubMed] [Google Scholar]
- 17.Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res. 2005;436:100–110. doi: 10.1097/01.blo.0000172303.74414.7d. [DOI] [PubMed] [Google Scholar]
- 18.Dye SF. The knee as a biologic transmission with an envelope of function: a theory. Clin Orthop Relat Res. 1996;323:10–18. doi: 10.1097/00003086-199604000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Damsted C, Glad S, Nielsen RO, Sorensen H, Malisoux L. Is there evidence for an association between changes in training load and running-related injuries: a systematic review. Int J Sports Phys Ther. 2018;13(6):931–942. [PMC free article] [PubMed] [Google Scholar]
- 20.Nielsen RO, Parner ET, Nohr EA, Sorensen H, Lind M, Rasmussen S. Excessive progression in weekly running distance and risk of running-related injuries: an association which varies according to type of injury. J Orthop Sports Phys Ther. 2014;44(10):739–747. doi: 10.2519/jospt.2014.5164. [DOI] [PubMed] [Google Scholar]
- 21.Orendurff MS, Kobayashi T, Tulchin-Francis K, et al. A little bit faster: lower extremity joint kinematics and kinetics as recreational runners achieve faster speeds. J Biomech. 2018;71:167–175. doi: 10.1016/j.jbiomech.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 22.Khassetarash A, Vernillo G, Martinez A, et al. Biomechanics of graded running: Part II-Joint kinematics and kinetics. Scand J Med Sci Sports. 2020;30(9):1642–1654. doi: 10.1111/sms.13735. [DOI] [PubMed] [Google Scholar]
- 23.Kulmala JP, Avela J, Pasanen K, Parkkari J. Forefoot strikers exhibit lower running-induced knee loading than rearfoot strikers. Med Sci Sports Exerc. 2013;45(12):2306–2313. doi: 10.1249/MSS.0b013e31829efcf7. [DOI] [PubMed] [Google Scholar]
- 24.Bonacci J, Hall M, Fox A, Saunders N, Shipsides T, Vicenzino B. The influence of cadence and shoes on patellofemoral joint kinetics in runners with patellofemoral pain. J Sci Med Sport. 2018;21(6):574–578. doi: 10.1016/j.jsams.2017.09.593. [DOI] [PubMed] [Google Scholar]
- 25.Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports. 2010;20(suppl 2):103–111. doi: 10.1111/j.1600-0838.2010.01195.x. [DOI] [PubMed] [Google Scholar]
- 26.Johnston R, Cahalan R, Bonnett L, et al. General health complaints and sleep associated with new injury within an endurance sporting population: a prospective study. J Sci Med Sport. 2020;23(3):252–257. doi: 10.1016/j.jsams.2019.10.013. [DOI] [PubMed] [Google Scholar]
- 27.Gao B, Dwivedi S, Milewski MD, Cruz AI., II Chronic lack of sleep is associated with increased sports injury in adolescents: a systematic review and meta-analysis. Orthop J Sports Med. 2019;7(3 suppl) doi: 10.1097/BPO.0000000000001306. 2325967119S00132. [DOI] [PubMed] [Google Scholar]
- 28.de Oliveira Silva D, Pazzinatto MF, Rathleff MS, et al. Patient education for patellofemoral pain: a systematic review. J Orthop Sports Phys Ther. 2020;50(7):388–396. doi: 10.2519/jospt.2020.9400. [DOI] [PubMed] [Google Scholar]
- 29.Rathleff MS, Thomsen JL, Barton CJ. Patient education in patellofemoral pain: potentially potent and essential, but under-researched. Br J Sports Med. 2018;52(10):623–624. doi: 10.1136/bjsports-2017-098298. [DOI] [PubMed] [Google Scholar]
- 30.Esculier JF, Bouyer LJ, Dubois B, et al. Is combining gait retraining or an exercise program with education better than education alone in treating runners with patellofemoral pain? A randomised clinical trial. Br J Sports Med. 2018;52(10):659–666. doi: 10.1136/bjsports-2016-096988. [DOI] [PubMed] [Google Scholar]
- 31.Rathleff MS, Graven-Nielsen T, Hölmich P, et al. Activity modification and load management of adolescents with patellofemoral pain: a prospective intervention study including 151 adolescents. Am J Sports Med. 2019;47(7):1629–1637. doi: 10.1177/0363546519843915. [DOI] [PubMed] [Google Scholar]
- 32.Van Cant J, Pineux C, Pitance L, Feipel V. Hip muscle strength and endurance in females with patellofemoral pain: a systematic review with meta-analysis. Int J Sports Phys Ther. 2014;9(5):564–582. [PMC free article] [PubMed] [Google Scholar]
- 33.Rathleff MS, Rathleff CR, Crossley KM, Barton CJ. Is hip strength a risk factor for patellofemoral pain? A systematic review and meta-analysis. Br J Sports Med. 2014;48(14):1088. doi: 10.1136/bjsports-2013-093305. [DOI] [PubMed] [Google Scholar]
- 34.Willy RW, Hoglund LT, Barton CJ, et al. Patellofemoral pain. J Orthop Sports Phys Ther. 2019;49(9):CPG1–CPG95. doi: 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
- 35.Neal BS, Lack SD, Lankhorst NE, Raye A, Morrissey D, van Middelkoop M. Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med. 2019;53(5):270–281. doi: 10.1136/bjsports-2017-098890. [DOI] [PubMed] [Google Scholar]
- 36.Finnoff JT, Hall MM, Kyle K, Krause DA, Lai J, Smith J. Hip strength and knee pain in high school runners: a prospective study. PM R. 2011;3(9):792–801. doi: 10.1016/j.pmrj.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 37.van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SM, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2015;1 doi: 10.1002/14651858.CD010387.pub2. CD010387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lack S, Barton C, Sohan O, Crossley K, Morrissey D. Proximal muscle rehabilitation is effective for patellofemoral pain: a systematic review with meta-analysis. Br J Sports Med. 2015;49(21):1365–1376. doi: 10.1136/bjsports-2015-094723. [DOI] [PubMed] [Google Scholar]
- 39.Bolgla LA, Boling MC, Mace KL, DiStefano MJ, Fithian DC, Powers CM. National Athletic Trainers' Association position statement: management of individuals with patellofemoral pain. J Athl Train. 2018;53(9):820–836. doi: 10.4085/1062-6050-231-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Collins NJ, Barton CJ, van Middelkoop M, et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br J Sports Med. 2018;52(18):1170–1178. doi: 10.1136/bjsports-2018-099397. [DOI] [PubMed] [Google Scholar]
- 41.Willy RW, Davis IS, Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther. 2011;41(9):625–632. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 42.Holden S, Rathleff MS, Jensen MB, Barton CJ. How can we implement exercise therapy for patellofemoral pain if we don't know what was prescribed? A systematic review. Br J Sports Med. 2018;52(6):385. doi: 10.1136/bjsports-2017-097547. [DOI] [PubMed] [Google Scholar]
- 43.Hochreiter B, Hess S, Moser L, Hirschmann MT, Amsler F, Behrend H. Healthy knees have a highly variable patellofemoral alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):398–406. doi: 10.1007/s00167-019-05587-z. [DOI] [PubMed] [Google Scholar]
- 44.Ho KY, Epstein R, Garcia R, Riley N, Lee SP, Turner C. Effects of patellofemoral taping on patellofemoral joint alignment and contact area during weight bearing. J Orthop Sports Phys Ther. 2017;47(2):115–123. doi: 10.2519/jospt.2017.6936. [DOI] [PubMed] [Google Scholar]
- 45.Neal BS, Barton CJ, Gallie R, O'Halloran P, Morrissey D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: a systematic review and meta-analysis. Gait Posture. 2016;45:69–82. doi: 10.1016/j.gaitpost.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 46.Noehren B, Hamill J, Davis I. Prospective evidence for a hip etiology in patellofemoral pain. Med Sci Sports Exerc. 2013;45(6):1120–1124. doi: 10.1249/MSS.0b013e31828249d2. [DOI] [PubMed] [Google Scholar]
- 47.Chan ZYS, Zhang JH, Au IPH, et al. Gait retraining for the reduction of injury occurrence in novice distance runners: 1-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(2):388–395. doi: 10.1177/0363546517736277. [DOI] [PubMed] [Google Scholar]
- 48.Creaby MW, Franettovich Smith MM. Retraining running gait to reduce tibial loads with clinician or accelerometry guided feedback. J Sci Med Sport. 2016;19(4):288–292. doi: 10.1016/j.jsams.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Garofolini A, Taylor S. The effect of running on foot muscles and bones: a systematic review. Hum Mov Sci. 2019;64:75–88. doi: 10.1016/j.humov.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 50.Van Ginckel A, Baelde N, Almqvist KF, Roosen P, McNair P, Witvrouw E. Functional adaptation of knee cartilage in asymptomatic female novice runners compared to sedentary controls. A longitudinal analysis using delayed Gadolinium Enhanced Magnetic Resonance Imaging of Cartilage (dGEMRIC) Osteoarthritis Cartilage. 2010;18:1564–1569. doi: 10.1016/j.joca.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 51.Anderson LM, Bonanno DR, Hart HF, Barton CJ. What are the benefits and risks associated with changing foot strike pattern during running? A systematic review and meta-analysis of injury, running economy, and biomechanics. Sports Med. 2019;50(5):885–917. doi: 10.1007/s40279-019-01238-y. [DOI] [PubMed] [Google Scholar]
- 52.Bazett-Jones DM, Huddleston WE, Cobb S, O'Connor K, Earl-Boehm JE. Increasing and decreasing pain causes acute responses of strength and running mechanics in patellofemoral pain. J Athl Train. 2017;52(5):411–421. doi: 10.4085/1062-6050-53.3.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 54.Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691–696. doi: 10.1136/bjsm.2009.069112. [DOI] [PubMed] [Google Scholar]
- 55.Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol Avon) 2012;27(10):1045–1051. doi: 10.1016/j.clinbiomech.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dos Santos AF, Nakagawa TH, Lessi GC, et al. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys Ther Sport. 2019;36:92–100. doi: 10.1016/j.ptsp.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 57.Cheung RT, Davis IS. Landing pattern modification to improve patellofemoral pain in runners: a case series. J Orthop Sports Phys Ther. 2011;41(12):914–919. doi: 10.2519/jospt.2011.3771. [DOI] [PubMed] [Google Scholar]
- 58.Roper JL, Harding EM, Doerfler D, et al. The effects of gait retraining in runners with patellofemoral pain: a randomized trial. Clin Biomech (Bristol Avon) 2016;35:14–22. doi: 10.1016/j.clinbiomech.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 59.Gerrard JM, Bonanno DR. Increasing preferred step rate during running reduces plantar pressures. Scand J Med Sci Sports. 2018;28(1):144–151. doi: 10.1111/sms.12886. [DOI] [PubMed] [Google Scholar]
- 60.Willy RW, Meardon SA, Schmidt A, Blaylock NR, Hadding SA, Willson JD. Changes in tibiofemoral contact forces during running in response to in-field gait retraining. J Sports Sci. 2016;34(17):1602–1611. doi: 10.1080/02640414.2015.1125517. [DOI] [PubMed] [Google Scholar]
- 61.Pairot de Fontenay B, Roy JS, Dubois B, Bouyer LJ, Esculier JF. Validating commercial wearable sensors for running gait parameters estimation. IEEE Sens J. 2020;20(14):7783–7791. [Google Scholar]
- 62.Bramah C, Preece SJ, Gill N, Herrington L. A. 10% increase in step rate improves running kinematics and clinical outcomes in runners with patellofemoral pain at 4 weeks and 3 months. Am J Sports Med. 2019;47(14):3406–3413. doi: 10.1177/0363546519879693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Davis I. Optimising the efficacy of gait retraining. Br J Sports Med. 2018;52(10):624–625. doi: 10.1136/bjsports-2017-098297. [DOI] [PubMed] [Google Scholar]
- 64.Napier C, Willy RW. Logical fallacies in the running shoe debate: let the evidence guide prescription. Br J Sports Med. 2018;52(24):1552–1553. doi: 10.1136/bjsports-2018-100117. [DOI] [PubMed] [Google Scholar]
- 65.Esculier JF, Dubois B, Dionne CE, Leblond J, Roy JS. A consensus definition and rating scale for minimalist shoes. J Foot Ankle Res. 2015;8:42. doi: 10.1186/s13047-015-0094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Esculier JF, Dubois B, Bouyer LJ, McFadyen BJ, Roy JS. Footwear characteristics are related to running mechanics in runners with patellofemoral pain. Gait Posture. 2017;54(6):144–147. doi: 10.1016/j.gaitpost.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 67.Yang C, Xiao S, Yang Y, Zhang X, Wang J, Fu W. Patellofemoral joint loads during running immediately changed by shoes with different minimalist indices: a cross-sectional study. Appl Sci (Basel) 2019;9(19):4176. [Google Scholar]
- 68.Sinclair J, Richards J, Selfe J, Fau-Goodwin J, Shore H. The influence of minimalist and maximalist footwear on patellofemoral kinetics during running. J Appl Biomech. 2016;32(4):359–364. doi: 10.1123/jab.2015-0249. [DOI] [PubMed] [Google Scholar]
- 69.Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of step rate manipulation on joint mechanics during running. Med Sci Sports Exerc. 2011;43(2):296–302. doi: 10.1249/MSS.0b013e3181ebedf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lenhart RL, Thelen DG, Wille CM, Chumanov ES, Heiderscheit BC. Increasing running step rate reduces patellofemoral joint forces. Med Sci Sports Exerc. 2014;46(3):557–564. doi: 10.1249/MSS.0b013e3182a78c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Willson JD, Sharpee R, Meardon SA, Kernozek TW. Effects of step length on patellofemoral joint stress in female runners with and without patellofemoral pain. Clin Biomech (Bristol Avon) 2014;29(3):243–247. doi: 10.1016/j.clinbiomech.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 72.Neal BS, Barton CJ, Birn-Jeffrey A, Daley M, Morrissey D. The effects & mechanisms of increasing running step rate: a feasibility study in a mixed-sex group of runners with patellofemoral pain. Phys Ther Sport. 2018;32:244–251. doi: 10.1016/j.ptsp.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 73.Warne JP, Gruber AH. Transitioning to minimal footwear: a systematic review of methods and future clinical recommendations. Sports Med Open. 2017;3(1):33. doi: 10.1186/s40798-017-0096-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Messier SP, Martin DF, Mihalko SL, et al. A 2-year prospective cohort study of overuse running injuries: The Runners and Injury Longitudinal Study (TRAILS) Am J Sports Med. 2018;46(9):2211–2221. doi: 10.1177/0363546518773755. [DOI] [PubMed] [Google Scholar]
- 75.de Oliveira Silva D, Barton CJ, Briani RV, et al. Kinesiophobia, but not strength is associated with altered movement in women with patellofemoral pain. Gait Posture. 2019;68:1–5. doi: 10.1016/j.gaitpost.2018.10.033. [DOI] [PubMed] [Google Scholar]
- 76.Maclachlan LR, Collins NJ, Matthews MLG, Hodges PW, Vicenzino B. The psychological features of patellofemoral pain: a systematic review. Br J Sports Med. 2017;51(9):732–742. doi: 10.1136/bjsports-2016-096705. [DOI] [PubMed] [Google Scholar]
- 77.Luedke LE, Wallace BJ, Puleo ML, Rauh MJ. Perfectionist concerns predict injury risk in collegiate distance runners—preliminary findings from a prospective study. Poster presented at: American College of Sports Medicine's 65th Annual Meeting; June 1; Minneapolis, MN: 2018. [Google Scholar]
- 78.Verschueren J, Tassignon B, De Pauw K, et al. Does acute fatigue negatively affect intrinsic risk factors of the lower extremity injury risk profile? A systematic and critical review. Sports Med. 2020;50(4):767–784. doi: 10.1007/s40279-019-01235-1. [DOI] [PubMed] [Google Scholar]
- 79.Main LC, Landers GJ, Grove JR, Dawson B, Goodman C. Training patterns and negative health outcomes in triathlon: longitudinal observations across a full competitive season. J Sports Med Phys Fitness. 2010;50(4):475–485. [PubMed] [Google Scholar]
- 80.Nussbaum ED, Bjornaraa J, Gatt CJ., II Identifying factors that contribute to adolescent bony stress injury in secondary school athletes: a comparative analysis with a healthy athletic control group. Sports Health. 2019;11(4):375–379. doi: 10.1177/1941738118824293. [DOI] [PMC free article] [PubMed] [Google Scholar]