Abstract
It is unclear how broadly aware parents are of the concept of herd immunity and whether parents consider community benefits of vaccination when making decisions about their child’s vaccinations. We aimed to determine whether educating parents about community-level benefits of measles, mumps, and rubella (MMR) vaccination and local vaccination rates would impact concern about their child’s risk of measles and risk of a measles outbreak.
We conducted an electronic survey among Minnesota parents of children aged 6–18 years in August 2016. We assessed baseline knowledge of herd immunity, asked participants to estimate MMR vaccination coverage in their county, and asked participants to estimate the minimum coverage needed to prevent measles outbreaks. We then delivered a short, educational intervention via the survey to inform participants about the benefits of herd immunity, the actual MMR vaccination coverage in their county, and that at least 95% MMR vaccination coverage is needed to prevent measles outbreaks. Pre- and post-intervention, participants were asked to report how concerned they were that their child might get measles. We used logistic regression models to assess factors associated with awareness of herd immunity, change in concern about one’s child’s measles risk, and overall concern for a measles outbreak.
Among 493 participants, 67.8% were aware of herd immunity at baseline. Post-intervention, 40.2% (n = 198) of parents learned that MMR vaccination rates in their county were higher than they expected. All participants found out that their county MMR rates were lower than the measles herd immunity threshold of 95%. Overall, 27.0% (n = 133) of participants reported an increase in concern that their child might get measles after learning about local vaccination coverage and the coverage needed to achieve herd immunity.
We found that our short, educational intervention aimed to increase awareness about herd immunity and local vaccination led to an increase in concern about disease risk among less than a third of parents.
Keywords: MMR vaccination, Herd immunity, Indirect protection, Vaccination coverage, Measles
1. Introduction
Measles is a vaccine-preventable, viral infectious disease that was declared eliminated in the United States (US) in 2000 [1]. However, declining uptake of the measles, mumps, and rubella (MMR) vaccine in the years since has led to recent outbreaks, and in 2019, the US reported the highest number of annual cases since 1992 [2]. The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommends that children in the US receive two doses of the MMR vaccine: the first dose between 12 and 15 months of age and the second dose between 4 and 6 years of age [3]. Nationwide estimates suggest that vaccination with at least one dose of MMR is relatively high in the United States (91.9% in 2015, among children aged 19–35 months), but there is substantial geographic heterogeneity in coverage [4]. In Minnesota, statewide MMR coverage of one or more doses was 94.3% for children 19–35 months of age, as of January 1, 2016, based on statewide registry data. Two dose MMR coverage for children up to 7 years of age varied substantially by county and ranged from 52.9% to 93.0% [5].
Vaccination provides direct protection to the individual who is vaccinated and indirect protection to the community through the benefits of herd immunity, also called community immunity. When a sufficiently high proportion of the population is vaccinated, the overall reduction of disease transmission in the community can prevent outbreaks and thus protect unvaccinated individuals [6,7]. Given the transmissibility of measles and the effectiveness of the vaccine, it is estimated that at least 93–95% of a population needs to be vaccinated with two doses of measles-containing vaccine to reach the herd immunity threshold and prevent outbreaks [8]. When vaccination coverage is below this threshold, there is a higher risk of a measles outbreaks, with the greatest concern for outbreaks in areas where unvaccinated persons are in close proximity and introductions of cases through travel are most likely [2].
Parents and legal guardians play a key role in decisions about their child’s immunizations. Previous research has shown that a parent’s main motivation for vaccinating their child is related to the desire to directly benefit the child, often based on concerns about the disease and/or complications related to the disease [9,20]. It is unclear how broadly aware parents are of the concept of herd immunity and whether parents consider community benefits to vaccination when making decisions about their own child’s vaccinations. In a 2014 national survey of parents of infants less than 12 months old, parents who received information emphasizing MMR vaccine’s benefits to both their child and society reported significantly higher levels of intention to vaccinate than those who received the standard Centers for Disease Prevention and Control (CDC) Vaccine Information Statement (VIS) [9]. The relative importance of vaccinating for the benefit of others as a motivator in vaccine decision-making is largely unknown [9–11]. Furthermore, little is known about the relationship between knowledge of community benefits of vaccination, knowledge of local vaccination rates, and concern about outbreaks [10,11]. Understanding more about the relationships between these factors has the potential to increase awareness among parents about the benefits of vaccination and herd immunity and to improve knowledge about local vaccination rates and risk of measles. Ensuring that the public has accurate perceptions of measles risk and knowledge of vaccination gaps is especially important.
With these factors in mind, we administered a survey with an embedded educational component to examine the relationships between knowledge of herd immunity, knowledge of local vaccination coverage, and concern about the risk of measles for one’s child and one’s community. Our aims were to (1) assess parents’ baseline knowledge about herd immunity, their estimate of the MMR vaccination coverage in their county, and their estimate of the minimum vaccination coverage needed to prevent measles outbreaks (herd immunity threshold), (2) determine which factors were associated with awareness of herd immunity, and (3) assess whether education about the benefits of herd immunity and the actual vaccination rates in one’s own county impacts parents’ concern about their own child’s measles risk and the risk of a measles outbreak in their county.
2. Materials and methods
2.1. Study design and setting
We conducted a cross-sectional study with embedded educational content and recruited participants to complete the survey at the University of Minnesota Driven to Discover Research Facility at the Minnesota State Fair from August 29 through September 1, 2016. The Minnesota State Fair is an annual event in the capital city of St. Paul, Minnesota, and is visited by more than two million people over a 12-day period every year [12].
2.2. Participant recruitment
Potential participants were recruited on-site through the Minnesota State Fair mobile app [13] and in-person at the research site by the study team. The study was advertised with the title “What have you heard about the herd?” without reference to vaccines. Individuals were eligible for the survey if they were at least 18 years of age, a parent/guardian (hereafter referred to as “parent”) of at least one child aged 6–18 years, a Minnesota resident, and able to read, write and understand English. Eligible participants provided informed consent prior to participation. The anonymous, 22-question interactive survey was self-administered on electronic tablets.
2.3. Survey design and educational intervention
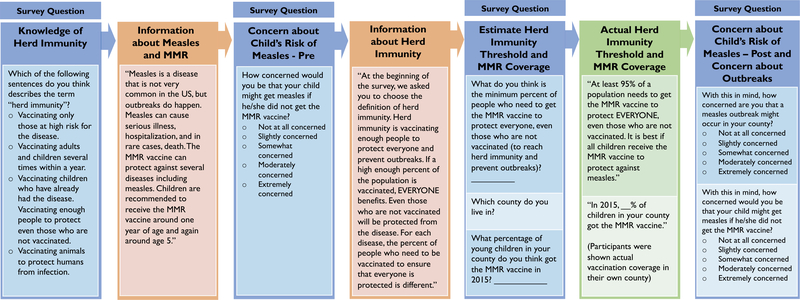
We designed the survey and educational content specifically to achieve the aims of this study. First, participants self-reported basic socio-demographic information, such as age and sex. The survey then consisted of four sections (Fig. 1). In the pre-intervention section, we asked participants to select the correct definition of herd immunity from a list of options. Following their response, on the next screen, participants received basic information about measles and MMR vaccine. With this information in mind, participants were asked to think about their youngest child who was at least six years old and to report on a five-point Likert scale how concerned they would be that their child might get measles if he/she did not get the MMR vaccine (“not at all,” “slightly,” “somewhat,” “moderately,” or “extremely” concerned) (Fig. 1). This question was designed to measure how concerned the parent was about their child’s measles risk at the start of the survey, prior to receiving specific information about the herd immunity threshold or their county’s MMR vaccination rates.
Fig. 1.
Summary of the survey intervention designed to address the aims of this study and the timing at which they were delivered during the survey. Participants were asked questions and then provided with educational information to increase knowledge about the concept of herd immunity, the MMR vaccination coverage in their county, and the herd immunity threshold for measles.
Next, in the educational intervention section, participants were presented with information describing the concept of herd immunity and why it is beneficial (Fig. 1). Immediately following, participants were asked to guess the herd immunity threshold for MMR by responding to the question “What do you think is the minimum percent of people who need to get the MMR vaccine to protect everyone, even those who are not vaccinated (to reach herd immunity and prevent outbreaks)?”. Then they were asked to estimate the MMR vaccination coverage in their own county. On the next screen, participants were informed that the herd immunity threshold for measles is 95% [8] and told the actual MMR vaccine coverage in their county as of January 1, 2016.
In the post-intervention section, participants were again asked to report how concerned they would be that their child might get measles if he/she did not get the MMR vaccine, using a 5-point Likert scale. This question was designed to measure how concerned the respondent was about their child’s measles risk post-intervention. They were also asked how concerned they were that a measles outbreak might occur in their county using the same scale (Fig. 1).
2.4. Participant characteristics
Participants reported their age, sex, race, ethnicity, highest level of education completed, and the number of adults and children in their household. They also reported their area of residence by zip code. We categorized participants as living within the metropolitan area of Minneapolis-St.Paul-Bloomington if their reported zip code was in any of the 14 Minnesota counties defined by the National Center for Health Statistics (NCHS) as “metro areas” [14]. Residents of zip codes in all other counties were categorized as residing in “non-metro areas.”
2.5. Assessment of awareness of local MMR vaccination coverage
Participants also selected their county from a drop-down list of all Minnesota counties. Participant estimates of the MMR vaccination coverage in their county were compared to the county-specific MMR vaccination rates, which were provided by the Minnesota Immunization Information Connection (MIIC), a statewide electronic immunization registry developed and maintained by the Minnesota Department of Health [5]. MMR vaccination rates available from MIIC indicate the proportion of children 7 years old as of January 1, 2016 who had received two or more valid doses of MMR vaccine. We categorized a participant’s estimate of local MMR vaccine coverage as “correct” if it was within 5 percentage points of the reported coverage in their county, as an “overestimate” if it was more than 5 percentage points higher than the reported coverage, and as an “underestimate” if it was more than 5 percentage points lower than the reported coverage.
2.6. Assessment of awareness of herd immunity
We categorized participants as “aware of herd immunity” if they chose the correct definition (i.e. “vaccinating enough people to protect even those who are not vaccinated”) when asked about the concept and “not aware” if they chose any of the other incorrect options (Fig. 1). Incorrect options for the definition of herd immunity were: “Vaccinating only those at high risk for the disease”; “Vaccinating adults and children several times within a year”; “Vaccinating children who already had the disease”; and “Vaccinating animals to protect humans from infection.” We categorized participants as having correctly estimated the herd immunity threshold if they estimated the threshold to be 95%, plus or minus 5 percentage points, and to have incorrectly estimated the threshold if they gave a response of less than 90%.
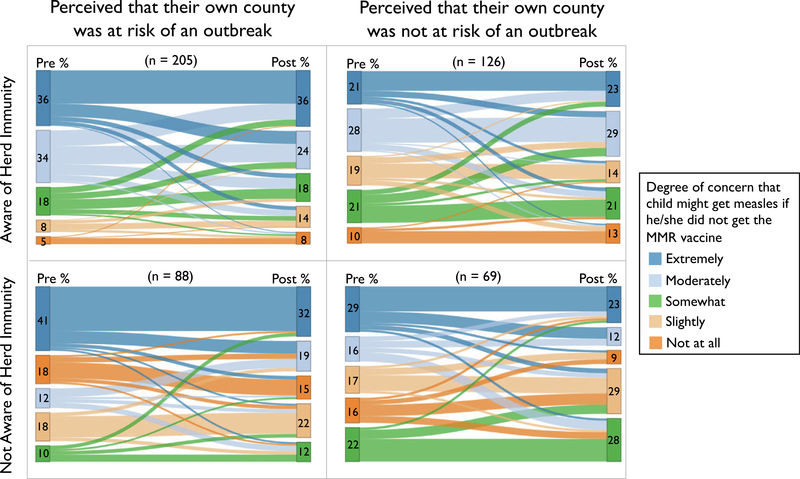
2.7. Construction of the Sankey plots
Here, we use Sankey plots to illustrate how participant responses (measured on a 5-point ordinal scale) changed pre- and post-intervention for multiple groups of participants. This visualization allows us to graphically illustrate the change in concern among survey participants pre- and post-intervention, while at the same time, descriptively comparing change across groups defined by their awareness of herd immunity and their perception of their own county’s risk of an outbreak; we hypothesized that these groups may differ.
2.8. Factors associated with awareness of herd immunity
To assess factors associated with being aware of the concept of herd immunity, we fit a multivariable logistic regression model with the following covariates: sex (male vs. female), age (years, continuous), highest level of education (associate degree or more vs. high school degree or less), race (white vs. another race), ethnicity (Hispanic or Latino vs. not Hispanic or Latino), area of residence (metro area vs. non-metro area), and whether they perceived that their own community was at risk of an outbreak, as defined below.
2.9. Assessment of concern about measles
Based on responses to the question “How concerned would you be that your child might get measles if he/she did not get the MMR vaccine?”, we categorized a participant as “concerned that their child is at risk of measles” if they selected “somewhat,” “moderately,” or “extremely,” and “not concerned that their child is at risk of measles” if they answered “not at all” or “slightly,” both pre- and post-intervention.
Participants were categorized as those who “perceived that their own county was at risk of an outbreak” if their own estimate of the MMR vaccine coverage in their county of residence was lower than their estimate of the herd immunity threshold for MMR. Conversely, we categorized participants as “perceived that their own county was not at risk of an outbreak” if a participant estimated that the MMR vaccine coverage in their county was equal to or higher than their estimate of the herd immunity threshold. Participants were informed via the text in the survey how their guesses compared to the actual herd immunity threshold and compared to the actual coverage level in their county immediately after they guessed these values and prior to the rest of the survey.
Based on the answer to the question “How concerned are you that a measles outbreak might occur in your county?”, we categorized a participant as “concerned that a measles outbreak could occur in their county” if they selected “somewhat,” “moderately,” or “extremely,” and “not concerned that a measles outbreak could occur in their county” if they selected “not at all” or “slightly.”
2.10. Factors associated with change in concern about child’s risk of measles and concern about risk of a measles outbreak in their county post-intervention
To assess factors associated with an increase in concern about their child’s risk of getting measles before and after the educational intervention, we fit a multivariable logistic regression model. The outcome measure was the difference in concern in their pre- compared to post-intervention responses to this same question. Responses were categorized as either “concern decreased or remained the same” or “concern increased.” We assessed the association between the outcome and two measures: perceived risk of an outbreak in one’s own community and awareness of herd immunity, both defined above. We adjusted a priori for demographic characteristics (sex (male vs. female), age (years, continuous), highest level of education (associate degree or more vs. high school degree or less), race (white vs. another race), ethnicity (Hispanic or Latino vs. not Hispanic or Latino), area of residence (metro area vs. non-metro area)). We report the point estimates for the odds ratios and 95% confidence intervals. To assess factors associated with a participant’s concern about risk of a measles outbreak in their county after receiving the educational intervention, we fit another multivariable logistic regression model. The outcome measure was “concerned about an outbreak” vs. “not concerned about an outbreak,” as defined above. We assessed the association between the outcome and whether participants perceived their own community was at risk of an outbreak and whether they were aware of herd immunity, both defined above. We decided a priori to adjust for the demographic characteristics described above. We report the point estimates for the odds ratios and 95% confidence intervals.
2.11. Analysis
Surveys were designed and administered by the study team using the REDCap electronic data capture software [15,16]. Stata 14 was used for data management and analysis [17]. The Sankey diagrams were developed in R version 3.6.1 [18], using the flipPlots package in Displayr [19].
2.12. Ethical review
This study was reviewed and approved as exempt by the University of Minnesota Institutional Review Board.
3. Results
3.1. Participant characteristics
Of the 493 participants who completed the survey, the majority were female (71.0%), white (89.7%), not Hispanic or Latino (94.3%), and had at least a bachelor’s degree (60.1%). Nearly all (95.3%) reported that their youngest child over 6 years of age had previously received at least one vaccine, with 92.7% reporting that their child had received at least one previous MMR vaccine (Table 1).
Table 1.
Demographic characteristics of 493 survey respondents who completed the survey at the University of Minnesota Driven to Discover research facility in August 2016.
| n | %a | ||
|---|---|---|---|
| Age | 18–39 years | 107 | 21.7 |
| 40–59 years | 357 | 72.4 | |
| ≥60 years | 26 | 5.3 | |
| Missing | 3 | 0.6 | |
| Sex | Male | 141 | 28.6 |
| Female | 350 | 71.0 | |
| Other | 1 | 0.2 | |
| Missing | 1 | 0.2 | |
| Race | African American | 10 | 2.0 |
| Native American or Alaska Native | 8 | 1.6 | |
| Asian | 20 | 4.1 | |
| Hawaiian or Other Pacific Islander | 1 | 0.2 | |
| Multiracial | 6 | 1.2 | |
| White | 442 | 89.7 | |
| Other | 5 | 1.0 | |
| Missing | 1 | 0.2 | |
| Ethnicity | Hispanic or Latino | 14 | 2.8 |
| Not Hispanic or Latino | 465 | 94.3 | |
| Missing | 14 | 2.8 | |
| Highest Education Level | Graduate degree | 100 | 20.3 |
| Bachelor’s degree | 196 | 39.8 | |
| Associate degree | 100 | 20.3 | |
| High school diploma or GED | 94 | 19.1 | |
| Elementary school | 2 | 0.4 | |
| Missing | 1 | 0.2 | |
| Has your child ever had any type of vaccine? | Yes | 470 | 95.3 |
| No | 15 | 3.0 | |
| Don’t know | 8 | 1.6 | |
| Missing | 0 | 0 | |
| Has your child had at least one dose of MMR vaccine?b | Yes | 443 | 89.9 |
| No | 6 | 1.2 | |
| Don’t know | 29 | 5.9 | |
| Missing | 15 | 3.0 | |
Row percentages may not equal 100, due to rounding.
Among the 478 participants who responded to this question, 92.7% (n = 443) indicated that their child had received at least one dose of MMR vaccine.
3.2. Awareness of herd immunity and factors associated
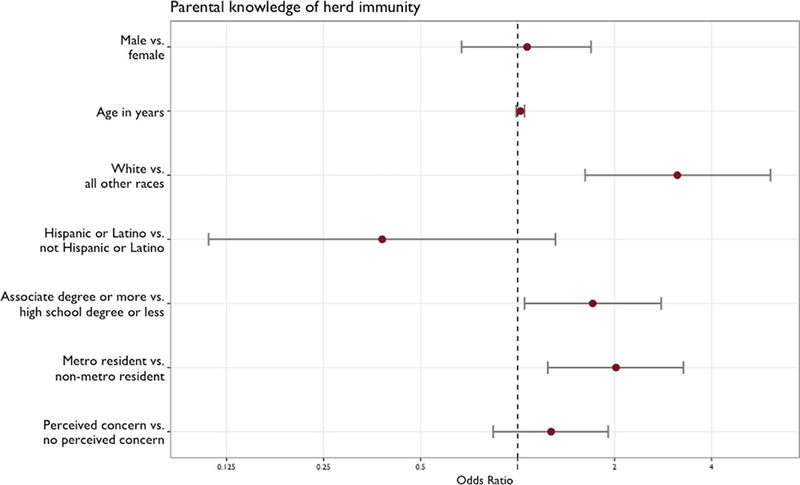
Two thirds of survey participants (67.8%; n = 334) were aware of herd immunity (Table 2). Of the factors assessed, those who identified as white (compared to another race, [OR = 3.13; 95% CI: 1.62, 6.09]), live in the metro area (compared to elsewhere, [OR = 2.02; 95% CI: 1.24, 3.27]), and have an associate degree or more (compared to high school or less; [OR = 1.71; 95% CI: 1.05, 2.79]) had greater odds of being aware of herd immunity (Fig. 2).
Table 2.
Knowledge of herd immunity and estimates of local MMR vaccine coverage among the 493 participants who completed the survey.
| n | % | ||
|---|---|---|---|
| Aware of herd immunity a | Yes | 334 | 67.8 |
| No | 159 | 32.3 | |
| Missing | 0 | ||
| Estimate of herd immunity threshold for measles | 95% ±5 percentage points (correct estimate) | 201 | 40.8 |
| Underestimated (<90%) | 291 | 59.0 | |
| Missing | 1 | 0.2 | |
| Estimate of MMR vaccine coverage in participant’s county of residence | Correct coverage estimate (±5 percentage points) | 156 | 31.6 |
| Overestimate (>5 percentage points higher than actual) | 135 | 27.4 | |
| Underestimate (<5 percentage points lower than actual) | 198 | 40.2 | |
| Missing | 4 | 0.8 | |
| Perceived that their own county was at risk of an outbreak b | Yes | 293 | 59.4 |
| No | 195 | 39.6 | |
| Missing | 5 | 1.01 | |
Participants were categorized as being “aware of herd immunity” if they chose “vaccinating enough people to protect even those who are not vaccinated”, the correct definition of herd immunity, when asked about the definition of the concept and not aware if they chose any other option.
Participants were categorized as those who “perceived that their own county was at risk of an outbreak” if their estimate of the MMR vaccine coverage in their county of residence was lower than their estimate of the herd immunity threshold for MMR. This is a construct of the two previous variables. Participants were informed during the survey about how their estimates compared with actual coverage levels and the actual herd immunity threshold.
Fig. 2.
Adjusted odds ratio and 95% confidence intervals for the association between each demographic covariate, perception of concern about measles, and awareness of herd immunity as estimated from a multivariate logistic regression model.
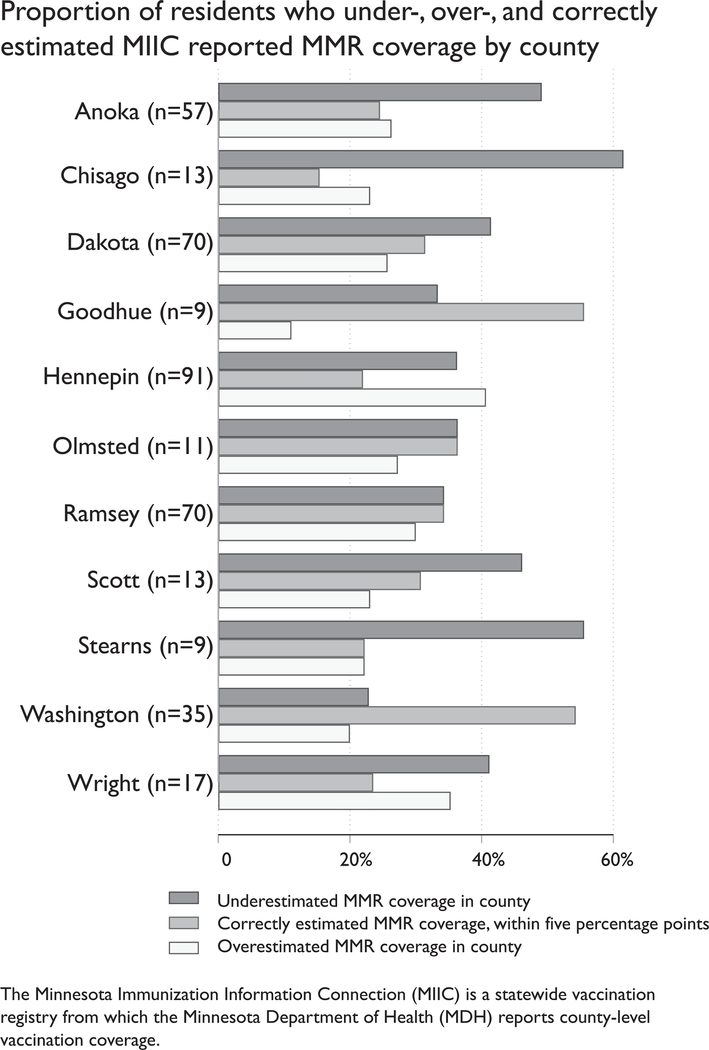
3.3. Awareness of local MMR vaccination coverage
Forty-one percent of participants (n = 201) correctly estimated that the herd immunity threshold for MMR vaccine was 95% ±5% while 59% of participants (n = 291) incorrectly believed that the herd immunity threshold was lower than 90% coverage. In every county, on average, participants underestimated the true MMR coverage in their county. In total, 40.5% (n = 198) of participants underestimated, 27.6% (n = 135) overestimated, and 31.9% (n = 156) correctly estimated the true MMR coverage in their county. The proportion of participants who underestimated, overestimated and correctly estimated MMR coverage in their county varied greatly by county (Fig. 3). Based on these two estimates that participants gave, nearly two-thirds (60.0%; n = 293) perceived that their own community was at risk of an outbreak, given that their estimate of the MMR vaccine coverage in their county of residence was lower than their estimate of the herd immunity threshold for MMR (Table 2). Participants were informed via the text in the survey how their guesses compared to the actual herd immunity threshold and compared to the actual coverage level in their county.
Fig. 3.
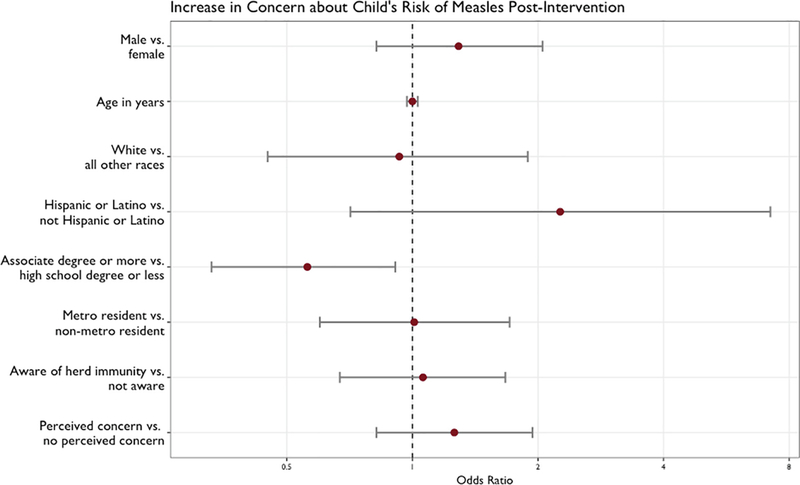
Adjusted odds ratio and 95% confidence intervals for the association between each demographic covariate, awareness of herd immunity, perception of concern about measles, and increase in concern about one’s child’s risk of measles post-intervention as estimated from a multivariate logistic regression model.
3.4. Concern about child’s risk of measles, concern about risk of a measles outbreak, and factors associated with concern
Before receiving any information regarding the benefits of herd immunity, the MMR vaccine herd immunity threshold, and the current MMR vaccination coverage in their county, 76% (n = 373) of all respondents reported being concerned (selected “somewhat,” “moderately,” or “extremely” concerned) that their child might get measles if he/she did not get the MMR vaccine. After receiving information regarding the MMR vaccine and herd immunity, slightly fewer respondents (72%; n = 354) reported being concerned that their child might get measles if he/she did not get the MMR vaccine. In addition, after receiving information regarding MMR vaccine and herd immunity, 62% (n = 304) reported being concerned that a measles outbreak might occur in their county. The Sankey plots provide a detailed categorization across the Likert scale of participant’s change in level of concern about their child’s measles risk (Fig. 4).
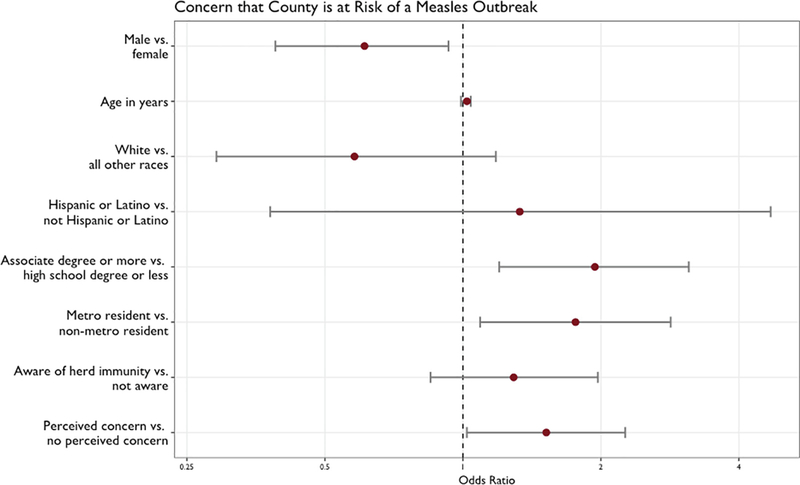
Fig. 4.
Adjusted odds ratio and 95% confidence intervals for the association between each covariate, awareness of herd immunity, perception of concern about measles, and an individual’s concern that their county is at risk for a measles outbreak as estimated from a multivariate logistic regression model.
After the educational intervention, whereby participants learned the actual herd immunity threshold for measles and the actual MMR vaccination coverage in their county, plus how these values compared to their estimates, over a quarter of survey participants overall (27.0%; n = 133) reported an increase in their concern that their child might get measles if he/she did not get the MMR vaccine (Fig. 4).
The odds of having an increase in concern that their child might get measles, compared to no increase or a decrease in concern, for those who perceived that there was a risk of an outbreak was 1.26 times higher than for those who did not perceive a risk of an outbreak (95% CI: 0.82–1.94), though the confidence interval was wide and included an estimate of no difference. The odds of concern increasing among those who were aware of the concept of herd immunity was very similar to the odds for those who were not aware of herd immunity (OR: 1.06; 95% CI: 0.67–1.67) (Fig. 5), though the confidence interval was wide.
Fig. 5.
The dark grey bars represent the proportion of participants who underestimated MMR vaccine coverage in their county of residence, the grey bars represent the proportion of participant who correctly estimated the MMR vaccine coverage in their county of residence, within five percentage points, and the light grey bars represent the proportion of participants who overestimated MMR coverage in their county of residence. Comparisons of MMR coverage per county were made based on the MDH MIIC report as of January 1, 2016. Only those counties that comprised more than 80% of the sample are displayed.
After the educational intervention, the majority of survey participants (61.7%; n = 304) reported that they were concerned that their county was at risk of a measles outbreak. The odds of reporting being concerned about a measles outbreak in their county was 1.52 times higher among those who perceived that there was a risk of an outbreak (they thought the vaccine coverage was lower than the level needed for herd immunity), compared to those that did not perceive a risk of an outbreak (95% CI: 1.03–2.26). The odds of reporting being concerned about a measles outbreak in their county was 1.29 times higher among those who were aware of herd immunity, compared to those who were not aware of herd immunity (95% CI: 0.85–1.97), though the confidence interval was wide and included an estimate of no difference (Fig. 6).
Fig. 6.
Sankey plots depicting the proportion of respondents reporting each degree of concern that their child’s measles risk (colored lines), both before receiving any information regarding the local MMR vaccine coverage or the herd immunity threshold (“Pre %”) and after receiving this information (“Post %”).
4. Discussion
In this study, we aimed to investigate the relationship between knowledge of herd immunity, knowledge of the herd immunity threshold for measles, knowledge of local MMR vaccination rates, and concern for one’s own child’s measles risk and concern for a measles outbreak. We also aimed to determine how concern about measles risk changed once participants were properly informed about local MMR vaccination coverage and the herd immunity threshold. Of note, all of the participants in this study were from counties with MMR coverage rates below the herd immunity threshold of 95% coverage. We found that the majority of participants in our survey were familiar with the concept of herd immunity, but that many underestimated the herd immunity threshold for measles; plus, many thought the MMR vaccination coverage in their county was lower than the actual coverage. We also found that this short educational intervention aimed at increasing awareness about herd immunity and MMR vaccination coverage led to an increase in concern about one’s child’s risk of the disease among 27% of participants. We observed that perceived risk of their child contracting measles was higher in those who perceived a risk of a community outbreak (those who estimated vaccination coverage to be lower than what they believed to be the level needed for herd immunity), regardless of their knowledge of herd immunity.
As part of this study, 40.2% of participants learned that vaccination coverage in their county was higher than they estimated, but that their county still did not reach the herd immunity threshold of 95% for measles. However, we did not see a corresponding increase in the proportion of individuals who reported being extremely concerned that their child might get measles if he/she did not get the MMR vaccine. This suggests that perhaps participants understood the importance of high vaccination coverage but did not internalize the importance of reaching the herd immunity threshold, or that the realization that MMR coverage was higher than expected provided reassurance and outweighed the fact that their county did not meet the herd immunity threshold. Here, we aimed to assess the relationship between coverage, herd immunity, and concern and to assess how these changed after participants became better informed about the actual coverage and the herd immunity threshold. Future studies might explore the ways to both increase awareness of herd immunity and establish the appropriate level of concern about the risk of measles and measles outbreaks.
Previous studies suggest that communicating the benefits of herd immunity and educating individuals about vaccination levels in their county lead to an increase in willingness to be vaccinated [9–11]. Our study went beyond these previous studies, as we sought to determine whether an educational intervention about the benefits of herd immunity and local MMR vaccination rates would change a parent’s concern about their child’s risk of contracting measles if he/she were unvaccinated. We did not ask whether the participant would be willing to vaccinate their child with MMR vaccine, because the study included parents of children who were already past the recommended age for receiving the MMR vaccine, and overall vaccination coverage in the state is high.
We took advantage of a unique opportunity to survey a larger number of participants over a short period of time by drawing a convenience sample of attendees at the Minnesota State Fair. As a result, our analysis is not based on a sample representative of the Minnesota adult population. For example, our participants included a higher proportion of more educated individuals and a higher proportion of female participants, compared to the state’s population. Therefore, we cannot conclude that our results are generalizable to the general population, because we do not know the external validity of our findings. While one might expect that participants who vaccinated their child with MMR vaccine would be more likely to self-select into the study, we found the level of self-reported MMR vaccination (at least one dose) to be 92.7% among participants who completed this question, very similar to the state-wide coverage of 92.6% of children aged 19–35 months vaccinated with at least one dose of MMR, estimated by the CDC in 2015 [4]. Since our study compares participant responses before and after learning about vaccination coverage and herd immunity, we aimed to maintain internal validity. Future studies could address the impact of similar interventions in representative samples and in more diverse populations and could explore the use of more tailored and specific information on herd immunity, relevant to the community in which the intervention is delivered.
5. Conclusions
Overall, a significant proportion of parents learned that MMR vaccination rates were higher than they expected, which may have reassured them that measles risk was low in their local areas, even though none of the counties had vaccination rates that met the herd immunity threshold. We found that our short, educational intervention aimed to increase awareness about herd immunity and local vaccination led to an increase in concern about disease risk among 27% of parents. Participants who believed that vaccination coverage in their county was lower than the herd immunity threshold needed to prevent outbreaks were more likely to be concerned about measles outbreaks.
Acknowledgements
We thank Miriam Muscoplat from the Minnesota Department of Health (MDH) for assistance with providing the Minnesota Immunization Information Connection (MIIC) MMR vaccination rates available from the Minnesota Department of Health.
Online: <https://www.health.state.mn.us/people/immunize/miic/stats/index.html>.
Funding source
This work was funded in part by the National Center for Advancing Translational Sciences of the National Institutes of Health Award [#UL1TR000114] and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R01 AI132496 (PI: Nicole E. Basta) and T32AI055433 (to Angela K. Ulrich). Additional support comes from the Eunice Kennedy Shriver National Institute of Child Health and Human Development under award numbers T32HD095134 and P2CHD041023. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
References
- [1].Centers for Disease Control and Prevention. Measles History In: Centers for Disease Control and Prevention, editor. Measles (Rubeola); 2018. [Google Scholar]
- [2].Centers for Disease Control and Prevention. Measles Cases and Outbreaks In: Centers for Disease Control and Prevention, editor. Measles (Rubeola); 2019. [Google Scholar]
- [3].McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62:1–34. [PubMed] [Google Scholar]
- [4].Centers for Disease Control and Prevention. 1995 through 2017 Childhood Measles, Mumps, and Rubella (MMR) Vaccination Coverage Trend Report In: ChildVaxView, editor; 2015. [Google Scholar]
- [5].Infectious Disease Epidemiology Prevention and Control Division(IDEPC) MIIC and the Public. In: Minnesota Department of Health, editor; 2019. [Google Scholar]
- [6].Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis Off Publ Infect Dis Soc Am 2011;52:911–6. [DOI] [PubMed] [Google Scholar]
- [7].Pigott N, Novelli V, Pooboni S, Firmin R, Goldman A. The importance of herd immunity against infection. Lancet (London, England) 2002;360:645. [DOI] [PubMed] [Google Scholar]
- [8].De Serres G, Gay NJ, Farrington CP. Epidemiology of transmissible diseases after elimination. Am J Epidemiol 2000;151:1039–48. discussion 49–52. [DOI] [PubMed] [Google Scholar]
- [9].Hendrix KS, Finnell SM, Zimet GD, Sturm LA, Lane KA, Downs SM. Vaccine message framing and parents’ intent to immunize their infants for MMR. Pediatrics 2014;134:e675–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Logan J, Nederhoff D, Koch B, Griffith B, Wolfson J, Awan FA, et al. ‘What have you HEARD about the HERD?’ Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate?. Vaccine 2018;36:4118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Betsch C, Böhm R, Korn L, Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav 2017;1:0056. [Google Scholar]
- [12].Minnesota State Agricultural Society. Minnesota State Fair; 2016.
- [13].Minnesota State Agricultural Society. Minnesota State Fair App; 2016.
- [14].National Center for Health Statistics (NCHS). NCHS Urban-Rural Classification Scheme for Counties In: Centers for Disease Control and Prevention, editor. Public-Use Data Files; 2013. [Google Scholar]
- [15].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].StataCorp. Stata Statistical Software: Release 14. 14 ed. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- [18].R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- [19].Displayr. Sydney, Australia; 2020. [Google Scholar]
- [20].Quadri-Sheriff M, Hendrix KS, Downs SM, Sturm LA, Zimet GD, Finnell SM. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics 2012;130(3):522–30. 10.1542/peds.2012-0140. [DOI] [PubMed] [Google Scholar]