Background: Coronavirus disease 2019 (COVID-19) has spread, causing a worldwide pandemic, and prolonged effects are emerging (1, 2). The term “long COVID” describes illness in persons who continue to report lasting effects after infection (3, 4). To date, little information exists about outpatient settings in this novel disease where 81% of cases are reportedly on the mild end of the spectrum (5). Informing patients and physicians about COVID-19 symptom evolution may help them recognize the time course of the disease, legitimize patients' concerns, and reassure them when possible. Messages around potentially persisting symptoms could also assist in reinforcing public health measures to avoid the spread of infection.
Objective: To describe COVID-19 symptom evolution and persistence in an outpatient setting in Geneva, Switzerland, from day 1 through day 30 to 45 after diagnosis.
Methods: From 18 March to 15 May 2020, the Geneva University Hospitals (sole and largest public hospital in Geneva) was 1 of 5 available testing centers and served more than 50% of patients with COVID-19 in the Geneva canton. Only symptomatic persons were tested during that period. Because many practices were closed, persons who were not hospitalized at baseline could benefit from remote follow-up with an ambulatory care center (a process called COVICARE) in case their primary care physician was unavailable for follow-up care (a full description is available at www.covicare24.com). Exclusion criteria were refusal to provide consent and administrative reasons (living outside the Geneva canton).
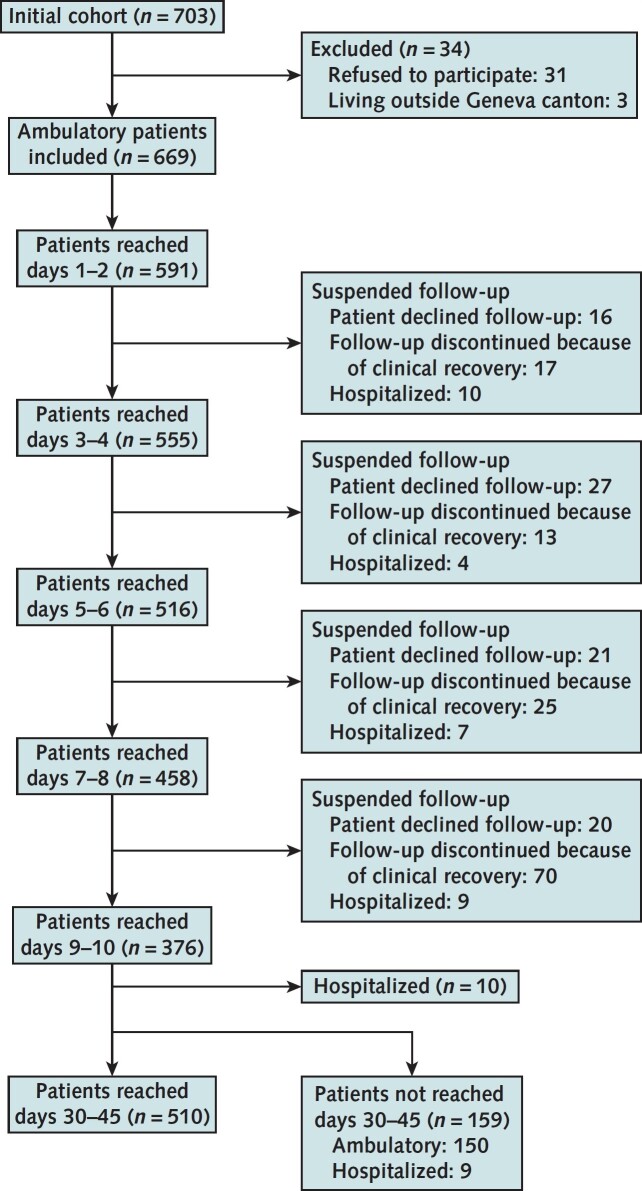
Most patients were called every 48 hours for the first 10 days with a standardized interview inquiring about self-reported symptoms (Supplement). Follow-up during the 10 days was suspended if patients declined follow-up, clinically recovered, or were hospitalized (Figure 1). Participants were called every 24 hours if they reported deteriorating clinical symptoms; those who were unreachable (eligible minus reached) were called again the next day. All patients were then contacted again 30 to 45 days after diagnosis. To address the varying frequency of contacts during the first 10 days, we combined assessments into 2-day intervals: days 1 to 2 through days 9 to 10. When 2 measurements were available, we included only the first observation per assessment interval.
Figure 1. Study flow diagram.
Out of the initial cohort of 703 participants, 669 ambulatory patients were ultimately included, excluding those who declined to participate (n = 31) or who lived outside the Geneva canton (n = 3). Reasons to suspend follow-up during the first 10 d were clinical recovery (≥10 d from symptom onset and 48 h without symptoms), patient wish, or hospitalization during follow-up. Attempts were made to assess all 669 participants at day 30–45 from diagnosis.
Findings: Of 30 557 persons tested in Geneva during the study period, 18.1% tested positive (n = 5534); 22.2% of these were hospitalized (n = 1229), and 703 enrolled in COVICARE follow-up. Out of the initial cohort, 669 persons were ultimately included (Figure 1). The mean age was 42.8 years (SD, 13.7); 60% of included patients were women, 24.6% were health care workers, and 68.8% had no underlying risk factors. Forty participants were hospitalized during the study period. We included their data when available (up to hospitalization and again at day 30 to 45). Hospitalized patients were significantly older (mean age, 53.2 years [SD, 11.7]); 55% were male, 12.5% were health care workers, and 62.5% had underlying risk factors.
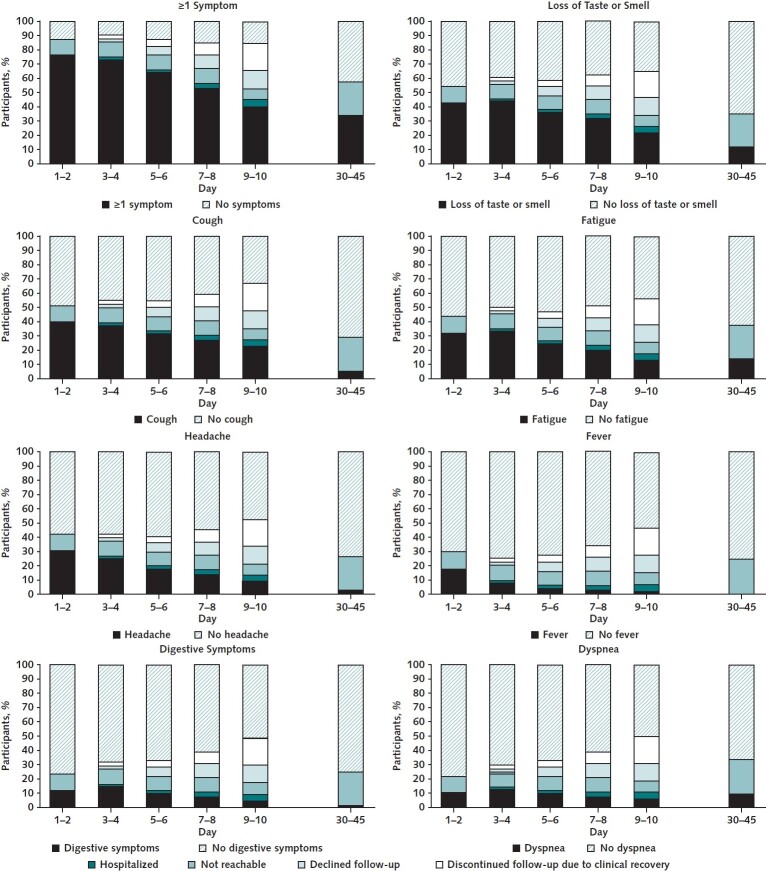
Figure 2 presents the proportion of the 669 patients with various symptoms over time. Cough and loss of taste or smell were common early in the clinical course. At 30 to 45 days (mean, 43 days) from diagnosis, at least 32% of the 669 originally included patients reported 1 or more symptoms. Fatigue, dyspnea, and loss of taste or smell were the main persistent symptoms. Participants not reached between days 30 and 45 (n = 159) had similar characteristics to those reached in that period (mean age, 41.8 years [SD, 14.8]; 58% were female, 25.9% were health care workers, and 67.9% had no risk factors).
Figure 2. Longitudinal evolution of COVID-19 symptoms in outpatient settings (n = 669).
Forty of the participants were hospitalized during follow-up. Their data were included in the reported symptoms when available (up to hospitalization and again at day 30-45). COVID-19 = coronavirus disease 2019.
Discussion: Coronavirus disease 2019 can persist and result in prolonged illness. Our study shows persistence of symptoms in a third of ambulatory patients 30 to 45 days after diagnosis even if we assume that those lost to follow-up were all asymptomatic. Fatigue, dyspnea, and loss of taste or smell were the main persistent symptoms. These results are in line with a recent study of 274 participants that reported the persistence of symptoms 14 to 21 days after diagnosis (2).
Our study has several limitations, including missing data and ascertainment bias at each assessment interval. Baseline characteristics were similar overall between participants reached and not reached on day 30 to 45.
In conclusion, this study shows that patients with COVID-19 develop an array of symptoms that evolve over time. Recognizing the persistence of symptoms could legitimize patients' concerns in an unknown and new disease. Adequate communication can provide reassurance, reduce anxiety, and potentially optimize recovery.
Supplementary Material
Appendix: Members of the COVICARE TEAM
Members of the COVICARE TEAM who authored this work: Mayssam Nehme, Olivia Braillard, and Delphine Courvoisier (Geneva University Hospitals, Geneva, Switzerland); Gabriel Alcoba (Geneva University Hospitals and Médecins Sans Frontières, Geneva, Switzerland); Idris Guessous and François Chappuis (Geneva University Hospitals and University of Geneva, Geneva, Switzerland); and Sigiriya Aebischer Perone (Geneva University Hospitals and International Committee of the Red Cross, Geneva, Switzerland).
Members of the of the COVICARE TEAM who contributed to this work but did not author it: Marwene Grira, Giovanni Innaurato, Jennifer Socquet, Chloé Chevallier-Lugon, Luisa Carnino, Bruno Lab, Jose Sandoval, Silvia Stringhini, Pierre Chopard, Flora Koegler, and Dan Lebowitz (Geneva University Hospitals, Geneva, Switzerland); Simon Regard and Aglaé Tardin (Cantonal Health Service, General Directorate for Health, Geneva, Switzerland); and Camille Genecand (Cantonal Health Service, General Directorate for Health, and Geneva University Hospitals, Geneva, Switzerland).
Footnotes
This article was published at Annals.org on 8 December 2020.
References
- 1. Carfì A , Bernabei R , Landi F ; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603-605. [PMID: ] doi: 10.1001/jama.2020.12603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tenforde MW , Kim SS , Lindsell CJ , et al; IVY Network Investigators. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network — United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:993-998. [PMID: ] doi: 10.15585/mmwr.mm6930e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mahase E . Covid-19: What do we know about “long covid”. BMJ. 2020;370:m2815. [PMID: ] doi: 10.1136/bmj.m2815 [DOI] [PubMed] [Google Scholar]
- 4. Crosby SS . My COVID-19. Ann Intern Med. 2020. doi: 10.7326/M20-5126 [DOI] [PubMed] [Google Scholar]
- 5. Wu Z , McGoogan JM . Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [PMID: ] doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.