Abstract
BACKGROUND/OBJECTIVES:
Many older persons with chronic illness use Physician Orders for Life-Sustaining Treatment (POLST) to document portable medical orders for emergency care. However, some POLSTs contain combinations of orders that do not translate into a cohesive care plan (eg, cardiopulmonary resuscitation [CPR] without intensive care, or intensive care without antibiotics). This study characterizes the prevalence and predictors of POLSTs with conflicting orders.
DESIGN:
Retrospective cohort study.
SETTING:
Large academic health system.
PARTICIPANTS:
A total of 3,123 POLST users with chronic life-limiting illness who died between 2010 and 2015 (mean age = 69.7 years).
MEASUREMENTS:
In a retrospective review of all POLSTs in participants’ electronic health records, we describe the prevalence of POLSTs with conflicting orders for cardiac arrest and medical interventions, and use clustered logistic regression to evaluate potential predictors of conflicting orders. We also examine the prevalence of conflicts between POLST orders for antibiotics and artificial nutrition with orders for cardiac arrest or medical interventions.
RESULTS:
Among 3,924 complete POLSTs belonging to 3,123 decedents, 209 (5.3%) POLSTs contained orders to “attempt CPR” paired with orders for “limited interventions” or “comfort measures only”; 745/3169 (23.5%) POLSTs paired orders to restrict antibiotics with orders to deliver non-comfort-only care; and, 170/3098 (5.5%) POLSTs paired orders to withhold artificial nutrition with orders to deliver CPR or intensive care. Among POLSTs with orders to avoid intensive care, orders to attempt CPR were more likely to be present in POLSTs completed earlier in the patient’s illness course (adjusted odds ratio = 1.27 per twofold increase in days from POLST to death; 95% confidence interval = 1.18–1.36; P < .001).
CONCLUSION:
Although most POLSTs are actionable by clinicians, 5% had conflicting orders for cardiac arrest and medical interventions, and 24% had one or more conflicts between orders for cardiac arrest, medical interventions, antibiotics, and artificial nutrition. These conflicting orders make implementation of POLST challenging for clinicians in acute care settings.
Keywords: POLST, advance care planning, goals of care, health policy, quality improvement
Physician Orders for Life-Sustaining Treatment (POLST) is a widely implemented paradigm of portable, durable medical orders for emergency care.1 POLSTs are intended to guide clinicians caring for patients with chronic life-limiting illness.2 Implementation of POLST varies by state, with differences in content, order entry, storage, and uptake.3,4
Treatment-limiting POLST orders are associated with less in-hospital death, hospitalization, intensive care unit admission, and unwanted cardiopulmonary resuscitation (CPR).2,5 However, to be effective, POLSTs must be interpretable and actionable by clinicians, and they should be informed by patients’ values and goals. In many states, it is possible for a POLST to contain combinations of orders that do not translate into a cohesive care plan (eg, performing CPR but forgoing post-arrest intensive care, or delivering intensive care without antibiotics). POLSTs with such conflicting orders direct clinicians toward divergent goals and may lead to confusion and potentially inappropriate treatment.6 This study examines the prevalence of POLSTs with conflicting orders, and predictors of conflicting orders for cardiac arrest among patients with POLST orders to avoid intensive care, from a cohort of deceased POLST users in the state of Washington.
METHODS
We conducted a retrospective review of all POLSTs uploaded to the electronic health record (EHR) for a cohort of deceased adults with chronic life-limiting illness.7–9 Participants included all adults with chronic life-limiting illness who died in Washington between January 1, 2010, and December 31, 2015, and received care through UW Medicine, a large academic health system. Chronic life-limiting illness was defined by having any of the nine chronic conditions used by the Dartmouth Atlas Project to study end-of-life care10,11: cancers with poor prognosis, chronic lung disease, coronary artery disease, congestive heart failure, peripheral vascular disease, chronic renal failure, severe chronic liver disease, diabetes mellitus with end-organ damage, and dementia. Data were collected from death certificates, EHR data, and manual abstraction of scanned POLSTs. A waiver of consent was approved by the University of Washington institutional review board (STUDY00002590).
The Washington POLST contains four order sections: (1) cardiac arrest, with options for “attempt CPR” and “Do Not Attempt Resuscitation (DNAR)”; (2) medical interventions, with options for “full treatment,” “limited additional interventions” [no intensive care or intubation], and “comfort measures only”; (3) antibiotics, with options to use antibiotics to extend life, to use antibiotics only for symptom relief, or to withhold all antibiotics; and (4) artificial nutrition, with options to provide long-term, time-limited, or no artificial nutrition.12 The text and format of the Washington POLST orders for cardiac arrest and medical interventions are similar to most states’ POLSTs; many states also have similar antibiotic and artificial nutrition orders.3 Washington does not have electronic POLST order entry or a statewide registry.
The primary outcome was conflicting POLST orders for cardiac arrest and medical interventions, as defined by orders to “attempt CPR” paired with orders to avoid intensive care (“comfort measures only” or “limited additional interventions”). We considered these orders to be in conflict because most patients who survive CPR require intensive care and life-sustaining treatments. We also described the frequency of (1) orders to restrict antibiotic use paired with orders to provide non-comfort-only care, and (2) orders to withhold artificial nutrition paired with orders to attempt CPR or deliver intensive care.
Among POLSTs with orders to avoid intensive care, we evaluated for independent relationships between potential predictors and the primary outcome using clustered multivariable logistic regression with exposures of age at POLST completion, sex, non-White race or Hispanic ethnicity, educational attainment, POLST signatory, and timing with respect to illness course (measured as log2-days from POLST completion to death). These variables were previously associated with differences in advance care planning.13,14 To examine temporal trends, we also included date of POLST completion in the model. Because POLSTs with medical interventions orders for “full treatment” may be paired with either cardiac arrest order,15 we excluded POLSTs with “full treatment” orders to identify relationships other than those driven by the absence of treatment limitations. Because some patients had multiple POLSTs, estimates of variance were clustered by patient. Age, log2-days from POLST to death, and date of POLST were modeled continuously. Educational attainment was scaled from an eight-category death certificate field to a continuous variable approximating years of education.16 All other predictors were modeled as binary variables. Multiple imputation with chained equations was used to impute missing data for race/ethnicity, educational attainment, and POLST signatory (Supplementary Text S1). Analyses were performed using Stata v.16.1 (StataCorp, stata.com).
RESULTS
In the EHR of 22,098 decedents meeting inclusion criteria, there were 4,011 POLSTs completed by 3,123 patients; 3,924 contained order selections for cardiac arrest and medical interventions, 79% had antibiotic orders, and 77% had artificial nutrition orders. Table 1 describes participant and POLST characteristics, and the frequency distribution of POLST orders is presented in Supplementary Table S1. Notably, 274 (6.8%) POLSTs bore no signature at all from a patient or surrogate. Although some such POLSTs were completed by telephone with surrogate decision makers, others bore no explanation for the missing signature, rendering them invalid. Missing data are described in Supplementary Table S2.
Table 1.
Characteristics of Patients and POLSTs
| Patient characteristic | Patients (N = 3,123) |
|---|---|
| Age at death, y, mean (SD) | 69.7 (14.5) |
| Sex, n (%) | |
| Male | 1,802 (58) |
| Female | 1,321 (42) |
| Race, n (%) (N = 2,924) | |
| White | 2,312 (79) |
| Black | 254 (9) |
| Asian | 259 (9) |
| Othersa | 99 (3) |
| Ethnicity, n (%) (N = 2,924) | |
| Non-Hispanic | 2,875 (98) |
| Hispanic | 49 (2) |
| Educational attainment, n (%) (N = 2,820) | |
| Less than high school | 388 (14) |
| High school or GED | 948 (34) |
| Some college | 731 (26) |
| Bachelor’s degree or more | 753 (27) |
| Number of unique POLSTs in EHR, n (%) | |
| 1 | 2,507 (80) |
| 2 | 436 (14) |
| ≥3 | 180 (6) |
| Chronic life-limiting illnesses, n (%)b | |
| Cancer with poor prognosis | 1,462 (47) |
| Chronic lung disease | 1,070 (34) |
| Coronary artery disease | 1,037(33) |
| Congestive heart failure | 985 (32) |
| Chronic renal failure | 891 (29) |
| Dementia | 606 (19) |
| Peripheral vascular disease | 574(18) |
| Severe chronic liver disease | 393 (13) |
| Diabetes with end-organ damage | 383 (12) |
| No. of chronic life-limiting illnesses, n (%) | |
| 1 | 1,074(34) |
| 2 | 844 (27) |
| 3 | 566 (18) |
| ≥4 | 639 (20) |
| POLST characteristic | POLSTs (N = 4,011) |
| Completed order sections, n (%) | |
| Cardiac arrest | 3,999 (>99) |
| Medical interventions | 3,936 (98) |
| Antibiotics | 3,169 (79) |
| Artificial nutrition | 3,098 (77) |
| POLST signatory, n (%)c | |
| Patient | 2,114(53) |
| Legal surrogate | 877 (22) |
| Unclear (illegible signature, treated as missing) | 746 (19) |
| Unsigned (treated as missing) | 274 (7) |
| Days from POLST completion to death, median (IQR) | 137 (32–486) |
Abbreviations: EHR, electronic health record; GED, General Educational Development; IQR, interquartile range; POLST, Physician Orders for Life-Sustaining Treatment; SD, standard deviation.
Includes Native American, Pacific Islander, and mixed race.
Chronic life-limiting illness diagnoses are not mutually exclusive.
The Washington State POLST specifies that the POLST should always be signed by the patient unless the patient is “decisionally incapacitated,” in which case a legal surrogate may sign the POLST.
Among 3,924 POLSTs with cardiac arrest and medical interventions orders, 209 (5.3%) POLSTs completed by 199 patients had conflicting cardiac arrest and medical interventions orders. Orders to “attempt CPR” were present in 186 of 1,470 (12.7%) of POLSTs with orders for “limited additional interventions,” and 23 of 1,345 (1.7%) of POLSTs with orders for “comfort measures only” (Figure 1A).
Figure 1.
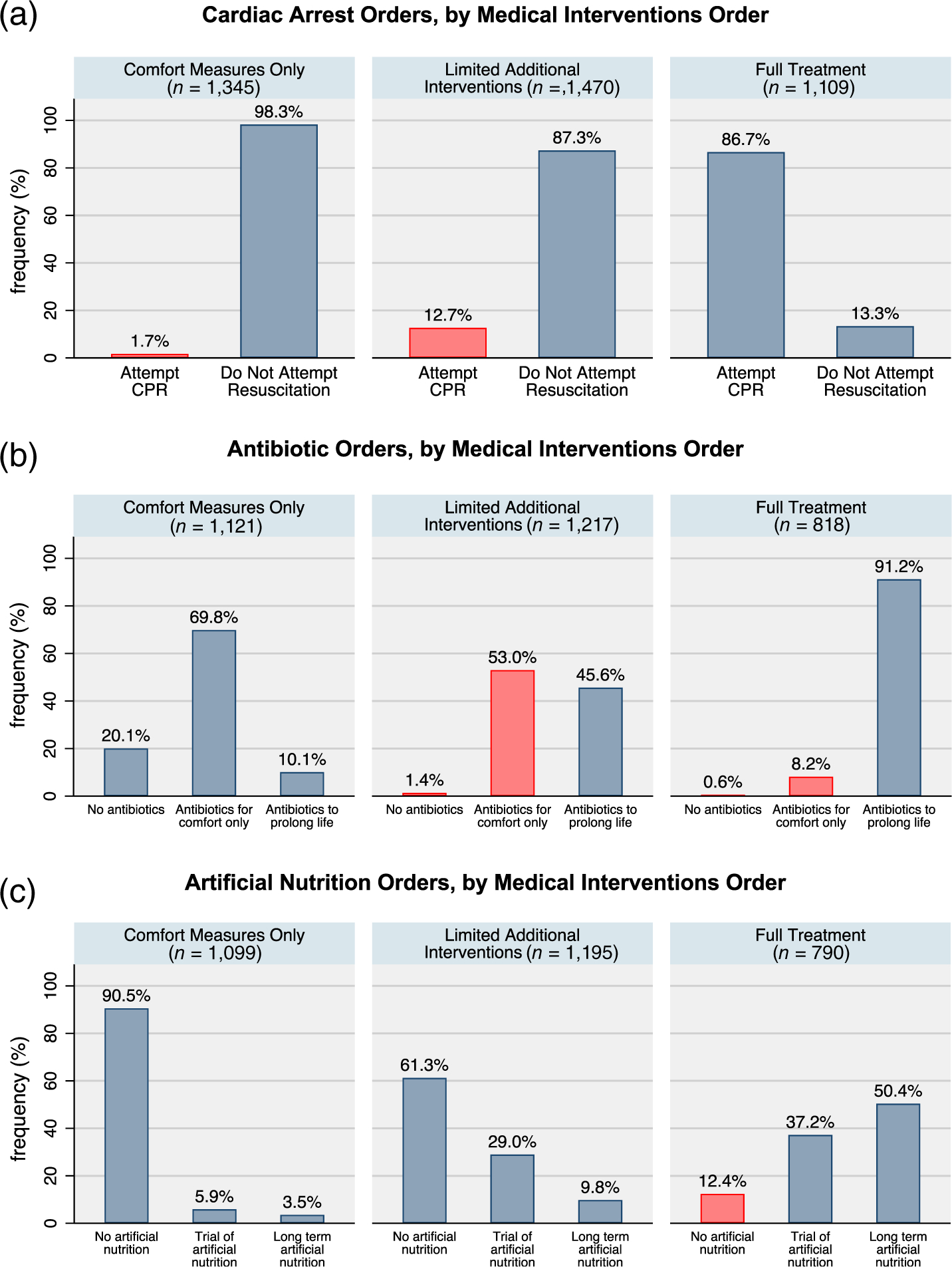
Physician Orders for Life-Sustaining Treatment (POLST) order combinations, by medical interventions order. Frequencies represent the proportion of POLSTs with complete medical interventions order and complete (A) cardiac arrest, (B) antibiotics, or (C) artificial nutrition orders. Denominators of POLSTs with complete orders are shown in the header of each plot. Red bars denote POLST orders that conflict with the medical interventions order. CPR, cardiopulmonary resuscitation.
Among 3,169 POLSTs with antibiotic orders, 745 (23.5%) POLSTs completed by 698 patients had antibiotic orders that conflicted with either cardiac arrest or medical interventions orders. Orders that restricted antibiotic use were present in 118 of 879 (13.4%) of POLSTs with orders to “attempt CPR,” 72 of 818 (8.8%) of POLSTs with orders for “full treatment,” and 662 of 1,217 (54.4%) of POLSTs with orders for “limited additional interventions” (Figure 1B).
Among 3,098 POLSTs with artificial nutrition orders, 170 (5.5%) POLSTs completed by 166 patients had nutrition orders that conflicted with either cardiac arrest or medical interventions orders. Orders precluding all artificial nutrition were present in 141 of 860 (16.4%) of POLSTs with orders to “attempt CPR,” and 98 of 790 (12.4%) of POLSTs with orders for “full treatment” (Figure 1C).
Altogether, 967 of 4,011 (24.1%) of all POLSTs, completed by 890 of 3,123 (28.5%) participants, had at least one pair of conflicting orders.
In evaluating potential predictors of orders to “attempt CPR” among patients with treatment-limiting medical interventions orders, POLSTs completed earlier in a patient’s illness course (greater log2-days from POLST to death) were significantly more likely to contain conflicting cardiac arrest and medical interventions orders (adjusted odds ratio [aOR] = 1.27 per twofold increase in days from POLST to death, 95% confidence interval [CI] = 1.18–1.36; P < .001; Table 2). Age, sex, race/ethnicity, educational attainment, and POLST signatory were not significantly associated with conflicting cardiac arrest and medical interventions orders (Table 2). Although unadjusted analyses suggested a temporal association between later date of POLST completion and lower likelihood of conflicting POLST orders (unadjusted odds ratio [OR] = .86 per year; 95% CI = .80–.92; P < .001), this association was not significant in multivariable analyses (aOR = .98 per year; 95% CI = .90–1.06; P = .56). To explore this, we conducted a post hoc analysis adjusted for days to death that found no significant temporal trend in the primary outcome when adjusted for days to death (aOR = .99 per year; 95% CI = .91–1.06; P = .70; Supplementary Table S3). Sensitivity analyses excluding unsigned POLSTs yielded the same conclusions.
Table 2.
Associations of Patient and POLST Characteristics with Orders to Attempt CPR in Patients with Treatment-Limiting Medical Interventions Orders
| Characteristic | Unadjusted OR (95% CI) | P | Adjusted ORa (95% CI) | P |
|---|---|---|---|---|
| Age at POLST, per 10 y | 1.07 (.97–1.18) | .17 | .98 (.88–1.09) | .71 |
| Female sex | .85 (.63–1.14) | .27 | .79 (.58–1.07) | .13 |
| Non-White race or Hispanic ethnicity | 1.02 (.71–1.45) | .93 | 1.12 (.77–1.62) | .56 |
| Educational attainment, per yearb | .99 (.94–1.05) | .77 | 1.00 (.95–1.06) | .91 |
| Patient signed own POLSTc | 1.34 (.93–1.92) | .12 | 1.26 (.87–1.83) | .21 |
| Days from POLST to death, log2 dd | 1.27 (1.20–1.35) | <.001 | 1.27 (1.18–1.36) | <.001 |
| Date of POLST completion, per yeare | .86 (.80–.92) | <.001 | .98 (.90–1.06) | .56 |
Abbreviations: CI, confidence interval; CPR, cardiopulmonary resuscitation; OR, odds ratio; POLST, Physician Orders for Life-Sustaining Treatment.
Adjusted for all exposures presented in the table.
Educational attainment was converted from an eight-category variable to approximate number of years of formal education, and modeled continuously.
The Washington State POLST specifies that the POLST should always be signed by the patient unless the patient is “decisionally incapacitated,” in which case a legal surrogate may sign the POLST.
OR reflects the change in odds per twofold increase in days from POLST to death.
Date of POLST completion is modeled as number of days since January 1, 2000, divided by 365.
DISCUSSION
In this study of POLSTs completed by chronically ill decedents in a single healthcare system, most POLSTs contained actionable combinations of orders. However, 5% had conflicting orders for cardiac arrest and medical interventions, and 24% had at least one pair of conflicting orders. Among POLSTs with orders that preclude intensive care, those completed earlier in a patient’s illness course were more likely to contain orders to attempt CPR. This may reflect greater heterogeneity of treatment preferences, or uncertainty about how to prioritize or translate goals of care, earlier in patients’ illness courses. Notably, the prevalence of conflicting POLST orders did not decrease over time. Although unadjusted analyses suggested a temporal trend in the primary outcome, this appeared to arise from confounding by days to death due to enrollment of decedents.
Our findings are consistent with prior studies of the Oregon and West Virginia POLST registries that report frequencies of conflicting orders for cardiac arrest and medical interventions of 2.5% to 7.3%.17,18 Although one of these studies reported a very low prevalence (.11%) of conflicting orders in the Oregon registry,17 that study did not consider orders to “attempt CPR” and deliver “limited interventions” to be in conflict. We believe that the incoherence of this combination of orders in most clinical scenarios renders such POLSTs ineffective for most patients.
Our findings also provide insights into the frequency with which POLST antibiotic and artificial nutrition orders may conflict with cardiac arrest or medical interventions orders. Our findings are consistent with a 2017 convenience sample of 100 New York MOLSTs (Medical Orders for Life-Sustaining Treatment) that found that 14% contained conflicting orders.19 In contrast, a 2017 sample of 2,064 Maryland MOLSTs found that only 1.5% had conflicting orders.20 However, this is likely due to significant differences between the Maryland MOLST (which has no medical interventions order) and most states’ POLST forms.21
Conflicting POLST orders may arise for several reasons. First, patients may express conflicting treatment preferences to clinicians, who may document these preferences as stated despite the conflicting goals they represent. Prior research has shown that many patients who explicitly prioritize palliation over life extension nevertheless express treatment preferences that appear discordant with their stated goals.22,23 Second, clinicians may not be fully aware of the likelihood of requiring intensive care and mechanical ventilation following successful CPR. Both the structure of the POLST and the frequent separation of do-not-resuscitate from do-not-intubate orders contribute to a false perception that these orders are independent.24,25 Third, the text of POLST orders may be confusing to patients and clinicians, leading to differences between the ordering clinician’s intent and what is actually ordered. Fourth, conflicting POLST orders may reflect entry errors.
Whatever the cause of conflicting POLST orders, the result is a POLST that is not actionable by clinicians during acute illness, which can lead to confusion and uncertainty about what types of treatment to deliver. We believe these findings call for a multifaceted approach to improving the implementation of POLST completion. First and foremost, there should be a renewed emphasis on identifying and incorporating patients’ values and goals into all discussions of treatment preferences including discussions of POLST orders.26,27 Rather than placing patients and surrogates in the position of selecting treatment orders that may or may not be actionable, clinicians should first elicit patients’ values and goals, and then guide patients in translating these values and goals into POLST orders.28 In support of this, the National POLST program has developed revised language under consideration by several states that begins each medical interventions order with a statement of its intended treatment goals.29 Second, adoption of electronic POLST order entry interfaces and registries would allow real-time identification of conflicting orders upon entry, and it would present opportunities to provide both communication-priming interventions and clinical decision support to clinicians completing POLSTs during patient encounters. Third, POLST orders should be made as simple as possible to achieve their intended function. We believe the Washington State POLST antibiotic order is potentially confusing to patients and clinicians because two of the options (“use antibiotics if life can be prolonged” vs “determine use or limitation of antibiotics when infection occurs, with comfort as goal”) differ over a singular goal of antibiotic therapy, when in fact antibiotics are typically prescribed toward multiple goals. To reduce opportunities for confusion, it seems appropriate to remove antibiotic orders from POLSTs entirely, in accordance with recommendations from the National POLST program.29
This study has several limitations. First, we did not measure patients’ true preferences, goals, or values, and so we cannot make inferences about the fidelity of POLST orders to patients’ wishes. Second, the study only captures POLSTs on file in the EHR at UW Medicine. Although it is standard practice at UW Medicine to scan all POLSTs, our sampling may nevertheless introduce bias. Third, as a single-health system study in Washington State, our findings may not generalize to other systems or regions.
In conclusion, in this study of POLSTs in Washington State, most POLSTs had combinations of orders that are actionable by clinicians. However, 5% of POLSTs had conflicting combinations of cardiac arrest and medical interventions orders; and, 24% had at least one conflict between the cardiac arrest, medical interventions, antibiotics, and artificial nutrition orders. Conflicting POLST orders may lead to challenges for clinicians trying to follow POLST orders during an acute illness. Our findings highlight an important opportunity for quality improvement in the implementation of POLST completion.
Supplementary Material
Supplementary Table S1: Participants’ POLST orders.
Supplementary Table S2: Summary of missing covariates.
Supplementary Table S3: Associations between date of POLST and orders to attempt CPR in patients with treatment-limiting medical interventions orders, without and with adjustment for log-days from POLST to death.
ACKNOWLEDGMENTS
Financial Disclosure: This study was supported by the National Institutes of Health and the Cambia Health Foundation. Robert Y. Lee was supported by an F32 award (HL142211) and a K12 award in implementation science (HL137940), Robert Y. Lee and Matthew E. Modes by a palliative care T32 training fellowship (HL125195), and Matthew E. Modes by a pulmonary/critical care T32 training fellowship (HL007287), all from the National Heart, Lung, and Blood Institute. Seelwan Sathitratanacheewin was supported by the Prince Mahidol Youth Program Award, Bangkok, Thailand. Infrastructure support was provided by the University of Washington Institute of Translational Health Sciences, funded by the National Center for Advancing Translational Sciences through the Clinical and Translational Science Awards (CTSA) Program (UL1 TR002319).
Sponsor’s Role: The National Institutes of Health and the Cambia Health Foundation had no role in study design, methods, data collection, analysis, or preparation of the manuscript. The views expressed in this article are those of the authors and do not necessarily represent the views of the sponsors.
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Tolle SW, Tilden VP, Nelson CA, Dunn PM. A prospective study of the efficacy of the physician order form for life-sustaining treatment. J Am Geriatr Soc. 1998;46(9):1097–1102. [DOI] [PubMed] [Google Scholar]
- 2.Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: a systematic review of the literature. J Am Geriatr Soc. 2015;63(2):341–350. [DOI] [PubMed] [Google Scholar]
- 3.The National POLST Paradigm. POLST programs in your state. http://www.polst.org/programs-in-your-state/. Accessed September 4, 2018.
- 4.Tark A, Agarwal M, Dick AW, Stone PW. Variations in physician orders for life-sustaining treatment program across the nation: environmental scan. J Palliat Med. 2019;22(9):1032–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee RY, Brumback LC, Sathitratanacheewin S, et al. Association of physician orders for life-sustaining treatment with ICU admission among patients hospitalized near the end of life. JAMA. 2020;323(10):950–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosslet GT, Pope TM, Rubenfeld GD, Lo B, Truog RD, Rushton CH, Curtis JR, Ford DW, Osborne M, Misak C, Au DH, Azoulay E, Brody B, Fahy BG, Hall JB, Kesecioglu J, Kon AA, Lindell KO, White; American Thoracic Society ad hoc Committee on Futile and Potentially Inappropriate Treatment; American Thoracic Society; American Association for Critical Care Nurses; American College of Chest Physicians; European Society for Intensive Care Medicine; Society of Critical Care. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015;191(11):1318–1330. [DOI] [PubMed] [Google Scholar]
- 7.Lavin K, Davydow DS, Downey L, et al. Effect of psychiatric illness on acute care utilization at end of life from serious medical illness. J Pain Symptom Manage. 2017;54(2):176.e1–185.e1. [DOI] [PubMed] [Google Scholar]
- 8.Hicks K, Downey L, Engelberg RA, et al. Predictors of death in the hospital for patients with chronic serious illness. J Palliat Med. 2018;21(3): 307–314. [DOI] [PubMed] [Google Scholar]
- 9.Sathitratanacheewin S, Engelberg RA, Downey L, et al. Temporal trends between 2010 and 2015 in intensity of care at end-of-life for patients with chronic illness: influence of age under vs. over 65 years. J Pain Symptom Manage. 2018;55(1):75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goodman DC, Esty AR, Fisher ES, et al. Trends and Variation in End-of-Life Care for Medicare Beneficiaries with Severe Chronic Illness: A Report of the Dartmouth Atlas Project Hanover, NH: The Dartmouth Institute for Health Policy and Clinical Practice; 2011. https://www.dartmouthatlas.org/downloads/reports/EOL_Trend_Report_0411.pdf. Accessed June 7, 2017. [PubMed] [Google Scholar]
- 11.Dartmouth Institute for Health Policy and Clinical Practice. Crosswalk File of ICD9 Diagnosis Codes to Risk Group Assessment. 2015. http://archive.dartmouthatlas.org/downloads/methods/Chronic_Disease_Codes.pdf. Accessed August 24, 2016.
- 12.Washington State Medical Association. Physician Orders for Life-Sustaining Treatment (POLST). https://wsma.org/POLST. Accessed September 19, 2019.
- 13.Harrison KL, Adrion ER, Ritchie CS, Sudore RL, Smith AK. Low completion and disparities in advance care planning activities among older Medicare beneficiaries. JAMA Intern Med. 2016;176(12):1872–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enguidanos S, Ailshire J. Timing of advance directive completion and relationship to care preferences. J Pain Symptom Manage. 2017;53(1):49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Council on Ethical and Judicial Affairs, American Medical Association. Guidelines for the appropriate use of do-not-resuscitate orders. JAMA. 1991;265(14):1868–1871. [PubMed] [Google Scholar]
- 16.Wolf C, Joye D, Smith TW, et al. The SAGE Handbook of Survey Methodology. Los Angeles, CA: SAGE Publications; 2016. [Google Scholar]
- 17.Moss AH, Zive DM, Falkenstine EC, et al. The quality of POLST completion to guide treatment: a 2-state study. J Am Med Dir Assoc. 2017;18(9): 810.e5–810.e9. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt TA, Zive D, Fromme EK, Cook JNB, Tolle SW. Physician orders for life-sustaining treatment (POLST): lessons learned from analysis of the Oregon POLST Registry. Resuscitation. 2014;85(4):480–485. [DOI] [PubMed] [Google Scholar]
- 19.Clemency B, Cordes CC, Lindstrom HA, Basior JM, Waldrop DP. Decisions by default: incomplete and contradictory MOLST in emergency care. J Am Med Dir Assoc. 2017;18(1):35–39. [DOI] [PubMed] [Google Scholar]
- 20.Tarzian AJ, Cheevers NB. Maryland’s medical orders for life-sustaining treatment form use: reports of a statewide survey. J Palliat Med. 2017;20(9): 939–945. [DOI] [PubMed] [Google Scholar]
- 21.National POLST Paradigm Task Force. Letter explaining Maryland nonconformity with National POLST. 2013. https://polst.org/wp-content/uploads/2020/02/2013.09.26-Maryland-Letter-Final.pdf. Accessed July 29, 2020.
- 22.Heyland DK, Heyland R, Dodek P, et al. Discordance between patients’ stated values and treatment preferences for end-of-life care: results of a multicentre survey. BMJ Support Palliat Care. 2017;7(3):292–299. [DOI] [PubMed] [Google Scholar]
- 23.Modes ME, Engelberg RA, Downey L, et al. Toward understanding the relationship between prioritized values and preferences for cardiopulmonary resuscitation among seriously ill adults. J Pain Symptom Manage. 2019;58(4):567–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Breu AC, Herzig SJ. Differentiating DNI from DNR: combating code status conflation. J Hosp Med. 2014;9(10):669–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rubins JB. Use of combined do-not-resuscitate/do-not intubate orders without documentation of intubation preferences: a retrospective observational study at an academic Level 1 trauma center code status and intubation preferences. Chest. 2020;158(1):292–297. [DOI] [PubMed] [Google Scholar]
- 26.Boyd C, Smith CD, Masoudi FA, et al. Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society guiding principles on the care of older adults with multimorbidity. J Am Geriatr Soc. 2019;67(4):665–673. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 28.Sudore RL, Lum HD, You JJ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary Delphi panel. J Pain Symptom Manage. 2017;53(5):821.e1–832.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National POLST. National POLST Form Guide. 2020. https://polst.org/wp-content/uploads/2020/04/2020.04-Form-Guidance.pdf. Accessed May 14, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Participants’ POLST orders.
Supplementary Table S2: Summary of missing covariates.
Supplementary Table S3: Associations between date of POLST and orders to attempt CPR in patients with treatment-limiting medical interventions orders, without and with adjustment for log-days from POLST to death.


