Abstract
The United States is facing an alarming and increasing obesity epidemic. Stress is associated with obesity, but specific longitudinal effects of life trauma on weight gain have not been assessed. Here we examined if life trauma and chronic stress predicted weight gain while also measuring the impact of body mass index (BMI). Life trauma and chronic stress were assessed with the Cumulative Adversity Interview (CAI). Weight and BMI were captured repeatedly over a two-year period. Results show significant increases in weight gain over time. Individuals with obesity (IOb) reported significantly higher levels of life trauma at the onset compared to overweight (IOw) and lean individuals (Il). Greater numbers of trauma events were associated with increased weight gain for both IOb and IOw but not for Il. Increased chronic stress was not consistently associated with weight gain over time. Current findings suggest the need to address trauma coping, especially in vulnerable individuals to prevent greater weight gain and curb obesity-related health outcomes.
Keywords: chronic stress, life trauma, obesity, longitudinal weight gain, body mass index
Introduction
The United States is currently facing an obesity epidemic, with predicted obesity rates rising to 51% by the year 2030.1 Factors contributing to obesity and weight gain are multiple and not clearly understood. Life traumas, or exposure to actual or threatened death, serious injury, or sexual violence,2 and chronic stressors, or repeated uncontrollable and upsetting events,3 are highly prevalent experiences.4 Prior research implicates life trauma and chronic stress as risk factors for obesity,5-11 as they are associated with metabolic and appetite changes.12,13 However, longitudinal studies to identify those most susceptible to the effects of stress on weight gain are rare.
Previous work supports some evidence of childhood and life trauma on weight gain,14,15 but longitudinal effects and the concurrent cumulative impact of body mass index (BMI), a standardized measure of obesity,16 have not been considered. Similarly, chronic stress, like life trauma, has also been associated with greater wanting of high fat foods and weight gain12,17,18 but not in all studies. These findings suggest that further prospective and longitudinal effects of life trauma and chronic stress on weight gain are needed.
Consideration of current BMI as a specific vulnerability factor in assessing the effects of life trauma and chronic stress is important, as higher weight alters stress, reward and metabolic biology in ways that may impact weight gain.19 Proposed theories suggest that individuals with obesity (IOb; i.e. those with a BMI of 30 kg/m2 or higher) may confuse the effects of stress with hunger cues, relative to how lean individuals (Il) process these cues, leading to increased future weight.20 IOb demonstrate alterations in hypothalamic pituitary adrenal (HPA) axis activity,21 which has been associated with increased eating, obesity and weight gain,18,19,22 supporting the model of weight-related adaptations in stress and metabolic processes that may in turn drive overeating and weight gain.19 IOb may also be more prone to external and emotional eating,23 which can be triggered in stressful situations.24 Despite the potential impact of present weight on future weight gain, only one study to our knowledge considered a baseline BMI interaction in conjunction with chronic stress25 and in fact saw an effect such that men with higher BMI and chronic stress at the onset experienced greater weight gain. Therefore, the purpose of the current study was to assess the effects of life trauma and chronic stress on weight gain over a prospective two-year period, and to investigate BMI as a potential moderator of these relationships. In congruence with past literature demonstrating that trauma and chronic stress affect weight gain, we hypothesized that life trauma and chronic stress would predict weight gain, and more so for those with higher weight, i.e., IOb and overweight individuals (IOw) relative to Il.
Methods
Participants
Community adults with a mean age of 27.68 ± 6.72 years, who were 53.6% female, and 42.0% Caucasian, 31.9% African American, and 26.1% other races (N=138) recruited from the greater New Haven community in Connecticut via advertisements in local newspapers and flyers at nearby churches/community centers participated in the study. Participants were eligible if they were between the ages of 18 and 45 years and were able to read and write English. Exclusion criteria were the following: current use of or dependence on any psychoactive drug, including nicotine, diagnosis of a current psychotic disorder or current psychiatric symptoms requiring immediate attention, presence of any significant medical condition, current use of any medication for any medical condition, use of oral contraceptives, peri and post-menopausal status, history of a hysterectomy, and pregnancy or lactation.
Procedure
Potential participants underwent a phone screening to determine initial eligibility. All interested eligible participants completed two Intake appointments to provide informed consent (during the first appointment) and baseline information (during both appointments, following consent). Baseline information included questions about medical, psychiatric, and drug use history, as well as collecting height and weight measurements, and urine drug testing. Participants then began the ‘Study Period,’ within 6 weeks following Intake, where they completed stress and metabolic assessments and additional stress provocation sessions.26 Participants were then scheduled for follow-up weight assessments every six months over a two-year period. Participants were paid for their study participation at each stage of the experiment. The Yale University Institutional Review Board approved all study procedures.
Measures
Demographics
Demographic measures of age, gender, race and ethnicity, drug use, education and medical/psychiatric history were assessed using a structured demographics interview.
Physical Health Functioning
Participants underwent a breath alcohol test (Intoximeter Alco-Sensor FST®) and urine toxicology (EZ Key Cup®) screening to confirm alcohol sobriety at the time of assessment and ensure that participants were not using illicit drugs. The research nurse completed a physical health assessment and cleared participants as healthy for study participation.
Body Mass Index (BMI)
Height and weight were measured multiple times and with multiple tools to ensure completeness and accuracy. BMI group was determined based on intake measurements. BMI was calculated using the standard;16 i.e. dividing weight in kilograms by height in meters squared (weight (kg) / height (m)2). Weight was then measured at the end of the Study Period and at each of the four follow-up assessments over the two-year period.
Life Trauma and Chronic Stress
Life trauma events and chronic stress scores were assessed with the Cumulative Adversity Interview (CAI).27 The Life Trauma subscale consists of 34 items that asks whether participants have experienced events such as “a serious accident, injury, or illness that was life threatening or caused long-term disability” and any other traumatic events not specifically asked about. Life trauma scores indicated the number of traumatic events endorsed by the participant. Overall Cronbach’s reliability of the Life Trauma Scale was good (Cronbach’s α = 0.72)
The Chronic Stress subscale consists of 62 items related to ongoing life problems and sources of stress, including social and interpersonal, familial, and financial difficulties (Cronbach’s α = 0.76). Participants were asked to rate if statements such as “too much is expected of you by others,” were “not true,” “somewhat true,” or “very true.” For items that were somewhat true or very true, participants provided information on how long the event was ongoing. Chronic stress scores reflected a sum of the statements that participants endorsed as somewhat or very true.
Supplemental Table 1 provide an overview of trauma and chronic stress events endorsed in the current sample.
Follow Up and Weight Gain
Measured weight at Intake was subtracted from measured weight at Study Period and at each follow-up assessment time point. Overall rates of follow up with participation in at least one follow-up assessment across the two-year period was 89.9%, with average attendance at each follow-up timepoint being 82.6% at 6 months, 74.6% at 12 months, 68.8% at 18 months and 63.8% at the 24 month assessment period. These follow-up participation rates are similar to or slightly better than those reported in other studies.28,29
Data Analysis
All analyses were conducted in R version 3.6.1. To consider differences between BMI groups at baseline measures, generalized linear models for continuous outcomes and Fischer’s exact tests for categorical outcomes were employed. Linear mixed effects models30 with a random intercept were used to examine whether there was an effect of life trauma or chronic stress on weight change. Model residuals were assessed to ensure that criteria for normality were met. Exploratory mediational analyses for the effects of trauma and chronic stress on weight gain were conducted using the Lavaan package.31
Results
Demographic and Individual Characteristics
Table 1 provides demographic information for our sample. No race or gender differences were seen between the BMI groups. However, congruent with the general population, IOb and IOw were significantly older than Il (F(2,135)=4.57, p <.02). Participants who missed any timepoint did not significantly differ from those who completed all time points on an any baseline demographic and stress measures (p’s > 0.05).
Table 1.
Baseline descriptive statistics of total sample and by BMI class
| Total (N = 138) | Il (N = 56) | IOw (N = 44) | IOb (N = 38) | |
|---|---|---|---|---|
| Gender | ||||
| Female | 74 (53.6) | 26 (18.8) | 23 (16.7) | 25 (18.1) |
| Male | 64 (46.4) | 30 (21.7) | 21 (15.2) | 13 (9.4) |
| Race and Ethnicity | ||||
| Caucasian | 58 (42.0) | 24 (17.4) | 18 (13.0) | 16 (11.6) |
| African American | 44 (31.9) | 11 (8.0) | 17 (12.3) | 16 (11.6) |
| Other | 36 (26.1) | 21 (15.2) | 9 (6.5) | 6 (4.3) |
| Age* | 27.68 (6.72) | 25.64 (5.11) | 29.06 (7.16) | 29.08 (7.63) |
| BMI*** | 27.03 (4.77) | 22.65 (1.98) | 27.27 (1.72) | 33.21 (2.57) |
| Life Trauma** | 5.78 (3.70) | 5.04 (3.05) | 5.41 (3.39) | 7.32 (4.49) |
| Chronic Stress | 10.22 (5.47) | 9.63 (5.63) | 9.98 (5.14) | 11.39 (5.56) |
Note. BMI = Body Mass Index (kg/m2). For all categorical variables, totals and percentages of totals are listed. Means and standard deviations are listed for all continuous variables.
p <.05,
p <.01,
p < .001
The number of life trauma events significantly differed by BMI group (F(2,135) = 4.88, p < 0.01), such that IOb displayed significantly higher life trauma scores (mean = 7.32 SEM = 0.73) than IOw (mean = 5.41, SEM = 0.51, p < 0.02) and Il (mean = 5.04, SEM = 0.41, p < 0.01). IOw and Il showed no significant difference from one another (p = 0.61). There were no significant differences in chronic stress scores by BMI group (p = 0.29), however, patterns of results were similar to those of the life trauma scores (see Figures 1a and 1b).
Figure 1.
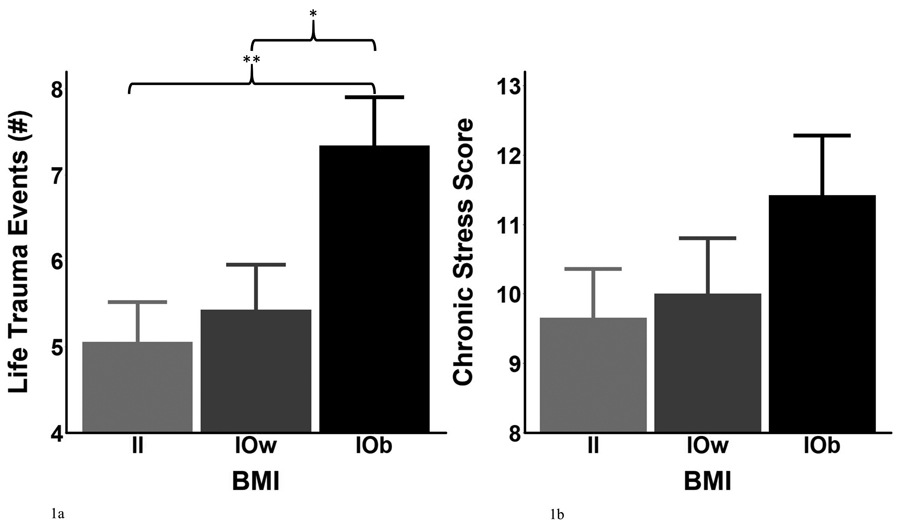
a. Significantly higher life trauma events in IOb compared to IOw and Il. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. BMI = Body mass index. *p < .05. **p < .01
b. No significant differences in chronic stress by BMI group. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. BMI = Body mass index.
Overall Changes in Weight
Overall, participants gained weight over two years (F(4, 402) = 7.96, p < 0.001). Patterns of weight change did not differ by BMI group (BMI: p = 0.68) nor by BMI group over time (Time x BMI: p = 0.64). Participants gained 4.57 lbs by 24 months across BMI groups (see Figure 2).
Figure 2.
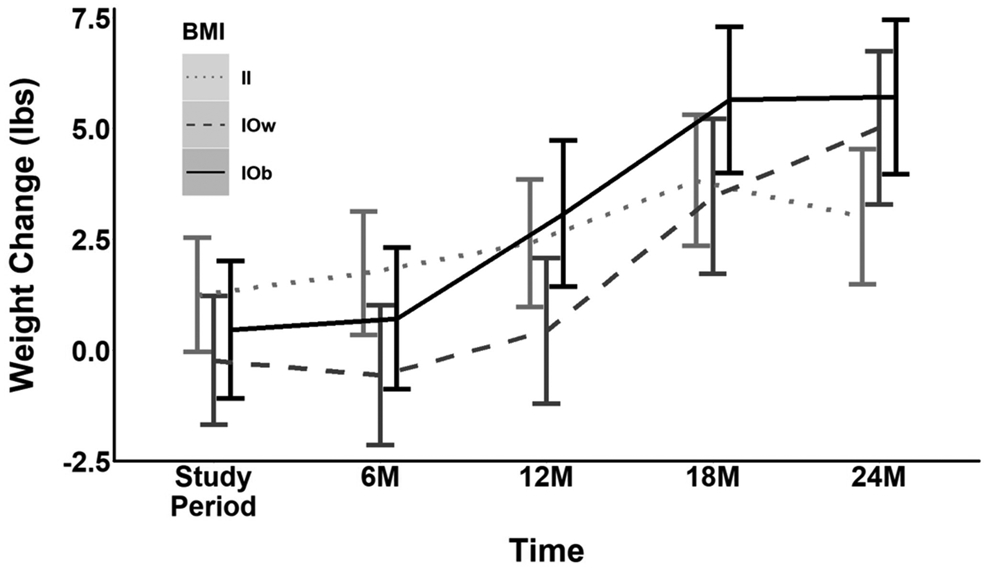
Significant increases in weight change over the course of the study. Timeframes represent change from Baseline intake to the Study Period (6 weeks post intake), and 6, 12, 18, and 24 months post study period. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. BMI = Body mass index. On average, participants gained 0.44 ± 3.60 pounds during the study period, 0.74 ± 9.95 pounds at 6 months, 1.99 ± 10.80 pounds at 12 months, 4.19 ± 10.46 pounds at 18 months, and 4.57 ± 12.61 pounds at 24 months.
Life Trauma by BMI and Time Effects
A significant main effect of time (F(4, 389) = 6.06, p < 0.001) and a significant life trauma by BMI interaction (F(2, 127) = 4.67, p < 0.02) was observed, such that, across all time points, more life trauma events led to a significant increase in weight for IOb (b = 3.06, SE = 1.04, p < 0.01) and a trending increase for IOw (b = 2.41, SE = 1.31, p < 0.07). The effect was non-significant for Il (p = 0.18). Furthermore, a significant three way interaction between life trauma x BMI group x time was observed (F(8, 389) = 1.99, p < 0.05). More life trauma events significantly predicted more weight gain in IOb at 12 months (b = 3.64, SE = 1.46, p < 0.02), trending at 18 months (b = 2.61, SE = 1.46, p < 0.08) and significantly at 24 months (b = 6.46, SE = 1.52, p < 0.001). Life trauma significantly predicted weight gain in IOw at 24 months (b = 4.66, SE = 1.94, p < 0.02). There were no significant associations between life trauma and weight change in Il (p’s > 0.1) (see Figures 3a and 3b).
Figure 3.
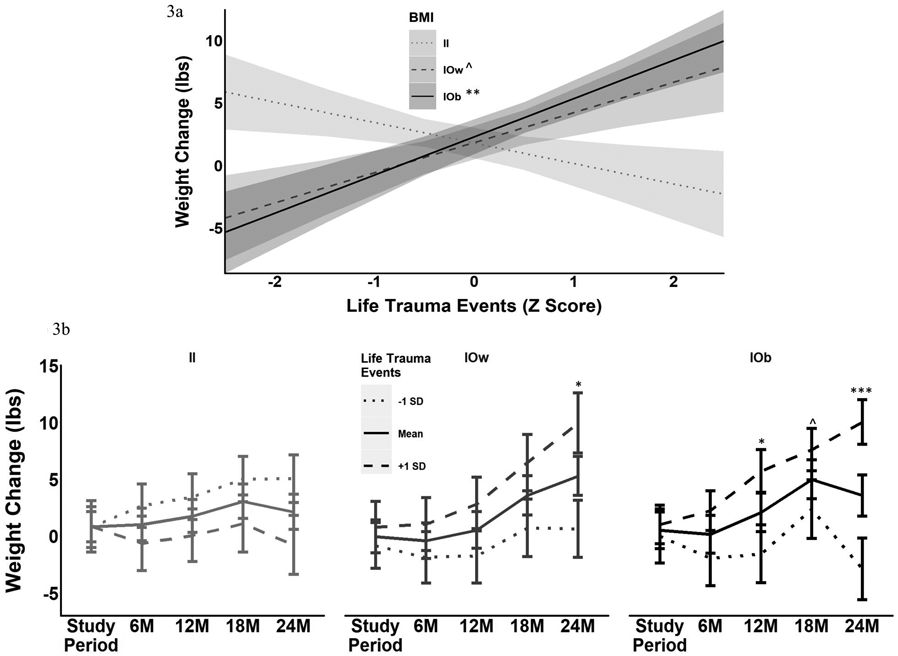
a. Higher life trauma events predicted greater weight gain in those with higher weight. Higher life trauma predicts increased weight change in IOb, at trending levels in IOw, but not in Il group. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. BMI = Body mass index. ^p < .1. **p < .01.
b. Higher life trauma predicted greater weight gain in IOw and IOb over specific time periods. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. ^p < .1. *p < .05. ***p < .001.
Chronic Stress by BMI and Time Effects
A significant main effect of time (F(4, 390) = 9.18, p <0.001) but no other significant main effects or two-way interactions (p’s > 0.35) were present. A significant three-way interaction between chronic stress, BMI group, and time was found (F(8, 391) = 2.31, p < 0.02). The source of the three-way interaction was that while no significant relationships between chronic stress and weight changes for Il or IOw at any time point (p’s > 0.12) was observed, IOb showed a variable relationship such that higher chronic stress scores predicted weight gain at trending levels at 6 months (b = 2.92, SE = 1.66, p < 0.08) and predicted weight loss at the 18 month mark (b = −4.1, SE = 1.78, p < 0.03; See Figure 4).
Figure 4.
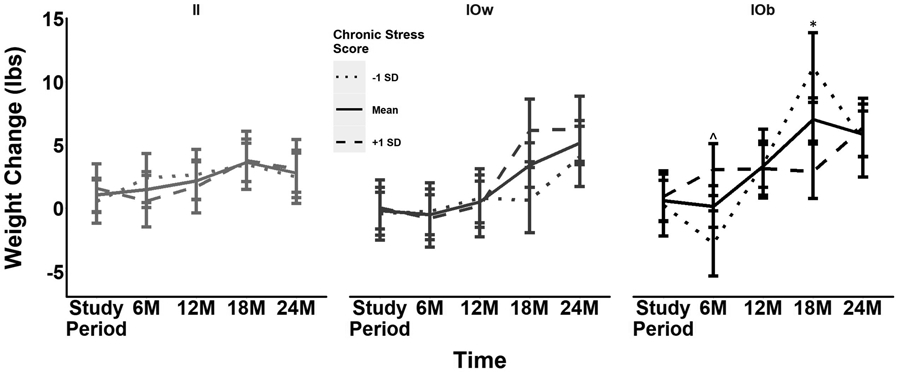
Higher chronic stress predicts variable weight gain over time for IOb. Il = Lean individuals. IOw = Overweight individuals. IOb = Individuals with obesity. ^p < .1. *p < .05.
Exploratory Analysis: Life Trauma, Chronic Stress, and Weight Interaction or Mediation
An exploratory mediation analysis using the Lavaan package was also conducted to better understand if chronic stress may contribute to the relationship between life trauma and weight gain in the final timepoint (24 months). These analyses revealed a significant relationship between trauma and weight change (b = 0.93, p < 0.02) and trauma and chronic stress (b = 0.42, p < 0.01), but no significant mediational effect of chronic stress on the relationship between life trauma and weight change (b = −0.03, p > 0.88). This suggests chronic stress was not a relevant mediator of life trauma effects on weight change. An exploratory moderation of the conjoined effects of life trauma and chronic stress on weight change, controlling for age, gender and BMI, was also completed. No significant three way interaction between life trauma, chronic stress, and time or between life trauma and chronic stress was seen (p’s > 0.15).
Discussion
The current study assessed the effects of life trauma and chronic stress over a longitudinal two-year period in a community cohort of young and middle-aged adults in the 18-45 age group range. Findings indicated that participants generally gained weight regardless of BMI group. This is not surprising given the increasing levels of obesity in the United States and that people tend to put on weight with age, particularly so when the average age of the sample represents young adults.1,18,32 Furthermore, IOb at intake reported a significantly greater number of traumatic events relative to the IOw and Il. Prior research supports this effect as presence of early life trauma is associated with an increased likelihood of obesity later in life.5,6,33,34 For example, in a nationally representative sample of US men and women, those with a history of childhood maltreatment were at increased risk for obesity in adulthood.35 Chronic stress may be linked to increased desire for high calorie foods (and thus higher weight) as well.36 However, we saw no BMI differences in baseline chronic stress levels (as depicted in Figure 1b). Weight gain due to chronic stress may depend on the intensity of the chronic stressor 36,37 as well as the duration. Not accounting for this variability may help to understand these null findings.
Remarkably, we found a significant interaction of life trauma with BMI as well as a three-way interaction of life trauma with BMI and time. More specifically, a greater number of traumatic events was associated with more weight gain in IOb and IOw while no such relationship was present in Il. Since IOb had a significantly greater number of traumatic events at the onset, it is possible that their baseline obesity is both a consequence of and a vulnerability factor for the effects of life trauma on weight gain. The effects of weight gain associated with trauma appeared by 12 months for IOb and 24 months for IOw. The non-significantly greater number of life trauma events for IOw may explain why these effects took longer to appear in this group. Our finding that trauma and high BMI can impact weight gain later is congruent with current literature. In one recent population based sample, childhood trauma and obesity predicted adulthood obesity.35 Trauma itself may also confer vulnerability to weight gain for two main reasons. First, trauma events, by definition, are severe stressors, and stress is linked to greater emotional eating38 and weight gain directly.39 For instance, women who had experienced intimate partner violence (a type of trauma included in our assessment as well) showed a significant increase in BMI over 5 years relative to women who had not.39 Second, when individuals undergo traumatic experiences, they are more likely to experience comorbid problems and illnesses later in life such as body image issues,40 low self-esteem,41 depression,42 and anxiety.43 These psychological difficulties may contribute to weight gain in and of themselves44-46 and, although not specifically studied here, were likely present in our general population based sample.
Finally, while we saw no significant main effect of chronic stress, it too interacted with BMI and time in predicting future weight gain. Il and IOw showed no significant relationship. However, IOb showed a variable relationship with chronic stress over time, with a trending positive relationship 6 months after the Study Period and a significant negative relationship after 18 months. Congruent with our findings at 6 months, men in a cohort based study showed increased weight gain when they had higher BMI at the onset and experienced greater job strain (one facet of chronic stress that went into our assessment as well).25,28 There is also evidence to suggest that the effect of stress may become more pronounced over time, congruent with our delayed weight change findings.47 Increased weight gain due to chronic stress may be seen in IOb rather than IOw or Il as stress is thought to accentuate weight gain in already socially and metabolically vulnerable individuals.48 The negative association at 18 months may be attributable to several factors. For instance, the chronic stressors experience in our sample may have ranged in intensity, as extremely intense chronic stressors are linked with weight loss/restrained gain in animal literature8,49 and mixed weight changes in human literature.50-54 Individual differences in affect, cognitive demands, and coping strategies employed may moderate the effects of stress on weight gain.53 It is also possible that the chronic stress prevalent at intake had resolved by the later time periods, and that this resolution may actually have positive effects on health.55 Taken together, our variable findings over time highlight the importance of frequently assessing intensity and timing of chronic stress when considering impacts on weight, and while not specifically assessed in our study, may represent an explanation for findings in our sample.
The current study had several limitations. First, we had a modest sample of young to mid-life adults, and thus the current findings may not generalize to samples of men and women with a broader age range. While we accounted for gender in all analyses, specific sex and gender factors will also need to be considered in future studies, as some studies suggest that men may be more vulnerable to the effects of chronic stress on weight gain.56 Also, participants did not have current medical conditions, and thus, the current findings may not be applicable to those groups with current stress-related and obesity-related medical illnesses. On the other hand, this study had several strengths in investigating the role of life trauma and chronic stress on prospective weight gain. First, this study provided a longitudinal design following participants over the course of two years, allowing for a more robust assessment of weight fluctuations. Second, we used in laboratory measures rather than self-reported weight. This was important as self-report methodologies tend to underestimate weight.57 Third, we recruited community-based healthy participants, thereby increasing the generalizability of the current findings. Finally, unique to many previous studies, we considered the impact of life trauma and chronic stress on weight gain in the context of initial baseline BMI in our analyses. This is important as existing weight patterns, even those existing as early as childhood, can predict adulthood weight.58
Conclusions
Our study is the first to our knowledge to identify life trauma and current BMI as key vulnerability factors impacting prospective weight gain over time in community adults. These findings suggest that obesity prevention programs could benefit from specific trauma-related interventions designed to prevent weight gain, particularly in individuals with higher weights who may be more vulnerable for subsequent weight gain.
Supplementary Material
Acknowledgments
Funding: This study was funded by NIH-NIDDK, R01-DK099039 (RS)
Footnotes
Conflict of Interests: There was no conflict of interest present for the current study.
References
- 1.Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. American journal of preventive medicine. 2012;42(6):563–570. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. Washington, DF 2013. [Google Scholar]
- 3.Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior. 1995;36(4):360–376. [PubMed] [Google Scholar]
- 4.American Psychological Association. Stress in America: Stress and Current Events. apa.org2019. [Google Scholar]
- 5.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19(5):544–554. [DOI] [PubMed] [Google Scholar]
- 6.Gunstad J, Paul RH, Spitznagel MB, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. 2006;142(1):31–37. [DOI] [PubMed] [Google Scholar]
- 7.Noll JG, Zeller MH, Trickett PK, Putnam FW. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics. 2007;120(1):e61–e67. [DOI] [PubMed] [Google Scholar]
- 8.Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic Stress Promotes Palatable Feeding, which Reduces Signs of Stress: Feedforward and Feedback Effects of Chronic Stress. Endocrinology. 2004;145(8):3754–3762. [DOI] [PubMed] [Google Scholar]
- 9.Dallman, Pecoraro N, Akana S, et al. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003;100(20):11696–11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dallman, Pecoraro NC, la Fleur SEJB, behavior,. Chronic stress and comfort foods: self-medication and abdominal obesity. Brain, behavior, immunity. 2005;19(4):275–280. [DOI] [PubMed] [Google Scholar]
- 11.Harrington EF, Crowther JH, Payne Henrickson HC, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultural Diversity and Ethnic Minority Psychology. 2006;12(2):212. [DOI] [PubMed] [Google Scholar]
- 12.Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biological psychiatry. 2013;73(9):827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chrousos GP. Stress and disorders of the stress system. Nature reviews endocrinology. 2009;5(7):374. [DOI] [PubMed] [Google Scholar]
- 14.Kubzansky LD, Bordelois P, Jun HJ, et al. The weight of traumatic stress: a prospective study of posttraumatic stress disorder symptoms and weight status in women. JAMA psychiatry. 2014;71(1):44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roenholt S, Beck N, Karsberg S, Elklit A. Post-traumatic stress symptoms and childhood abuse categories in a national representative sample for a specific age group: associations to body mass index. European Journal of Psychotraumatology. 2012;3(1):17188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC. About Adult BMI. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Published 2017. Accessed. [Google Scholar]
- 17.Adam TC, Epel ES. Stress, eating and the reward system. Physiology & behavior. 2007;91(4):449–458. [DOI] [PubMed] [Google Scholar]
- 18.Chao AM, Jastreboff AM, White MA, Grilo CM, Sinha R. Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight. Obesity (Silver Spring). 2017;25(4):713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinha R Role of addiction and stress neurobiology on food intake and obesity. Biological psychology. 2018;131:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greeno CG, Wing RR. Stress-induced eating. Psychological bulletin. 1994;115(3):444. [DOI] [PubMed] [Google Scholar]
- 21.Björntorp P, Rosmond R. Obesity and cortisol. Nutrition. 2000;16(10):924–936. [DOI] [PubMed] [Google Scholar]
- 22.Epel E, Lapidus R, McEwen B, Brownell KJP. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. 2001;26(1):37–49. [DOI] [PubMed] [Google Scholar]
- 23.van Strien T, Herman CP, Verheijden MW. Eating style, overeating and weight gain. A prospective 2-year follow-up study in a representative Dutch sample. Appetite. 2012;59(3):782–789. [DOI] [PubMed] [Google Scholar]
- 24.Slochower J, Kaplan SP, Mann L. The effects of life stress and weight on mood and eating. Appetite. 1981;2(2):115–125. [DOI] [PubMed] [Google Scholar]
- 25.Kivimäki M, Head J, Ferrie JE, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. International journal of obesity. 2006;30(6):982. [DOI] [PubMed] [Google Scholar]
- 26.Sinha R, Gu P, Hart R, Guarnaccia J. Food craving, cortisol and ghrelin responses in modeling highly palatable snack intake in the laboratory. Physiology & behavior. 2019;208:112563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turner RJ, Wheaton BJ. Checklist measurement of stressful life events. 1995:29–58. [Google Scholar]
- 28.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial Stress and Change in Weight Among US Adults. American Journal of Epidemiology. 2009;170(2):181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song Y-M, Lee K, Sung J. Eating behaviors and weight over time in a prospective study: the Healthy Twin Study. Asia Pacific journal of clinical nutrition. 2014;23(1):76. [DOI] [PubMed] [Google Scholar]
- 30.Kuznetsova A, Brockhoff PB, Christensen RHB. lmerTest package: tests in linear mixed effects models. Journal of statistical software. 2017;82(13). [Google Scholar]
- 31.Rosseel Y Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of statistical software. 2012;48(2):1–36. [Google Scholar]
- 32.Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. International journal of obesity. 2013;37(6):889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gustafson T, Sarwer D. Childhood sexual abuse and obesity. Obesity reviews. 2004;5(3):129–135. [DOI] [PubMed] [Google Scholar]
- 34.D’Argenio A, Mazzi C, Pecchioli L, Di Lorenzo G, Siracusano A, Troisi A. Early trauma and adult obesity: is psychological dysfunction the mediating mechanism? Physiology & behavior. 2009;98(5):543–546. [DOI] [PubMed] [Google Scholar]
- 35.Wall MM, Mason SM, Liu J, Olfson M, Neumark-Sztainer D, Blanco CJTp. Childhood psychosocial challenges and risk for obesity in US men and women. 2019;9(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894. [DOI] [PubMed] [Google Scholar]
- 37.Razzoli M, Bartolomucci A. The dichotomous effect of chronic stress on obesity. Trends in Endocrinology & Metabolism. 2016;27(7):504–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tan CC, Chow CM. Stress and emotional eating: The mediating role of eating dysregulation. Personality and Individual Differences. 2014;66:1–4. [Google Scholar]
- 39.Mason SM, Ayour N, Canney S, Eisenberg ME, Neumark-Sztainer D. Intimate partner violence and 5-year weight change in young women: a longitudinal study. Journal of Women’s Health. 2017;26(6):677–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scheffers M, Hoek M, Bosscher RJ, van Duijn MA, Schoevers RA, van Busschbach JT. Negative body experience in women with early childhood trauma: associations with trauma severity and dissociation. European journal of psychotraumatology. 2017;8(1):1322892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Briere J, Runtz M. Differential adult symptomatology associated with three types of child abuse histories. Child abuse & neglect. 1990;14(3):357–364. [DOI] [PubMed] [Google Scholar]
- 42.Suliman S, Mkabile SG, Fincham DS, Ahmed R, Stein DJ, Seedat S. Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive psychiatry. 2009;50(2):121–127. [DOI] [PubMed] [Google Scholar]
- 43.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological psychiatry. 2001;49(12):1023–1039. [DOI] [PubMed] [Google Scholar]
- 44.Megel ME, Wade F, Hawkins P, Norton J. Health promotion, self-esteem, and weight among female college freshmen. Health Values: The Journal of Health Behavior, Education & Promotion. 1994. [Google Scholar]
- 45.Harring HA, Montgomery K, Hardin J. Perceptions of body weight, weight management strategies, and depressive symptoms among US college students. Journal of American College Health. 2010;59(1):43–50. [DOI] [PubMed] [Google Scholar]
- 46.Anderson SE, Cohen P, Naumova EN, Must A. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Archives of pediatrics & adolescent medicine. 2006;160(3):285–291. [DOI] [PubMed] [Google Scholar]
- 47.Berset M, Semmer NK, Elfering A, Jacobshagen N, Meier LL. Does stress at work make you gain weight? A two-year longitudinal study. Scandinavian journal of work, environment & health. 2011:45–53. [DOI] [PubMed] [Google Scholar]
- 48.Swinburn B, Egger G. The runaway weight gain train: too many accelerators, not enough brakes. Bmj. 2004;329(7468):736–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martí O, Martí J, Armario A. Effects of chronic stress on food intake in rats: influence of stressor intensity and duration of daily exposure. Physiology & behavior. 1994;55(4):747–753. [DOI] [PubMed] [Google Scholar]
- 50.Beesley VL, Price MA, Webb PM. Loss of lifestyle: health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Supportive Care in Cancer. 2011;19(12):1949–1956. [DOI] [PubMed] [Google Scholar]
- 51.Kwarteng JL, Schulz AJ, Mentz GB, Israel BA, Perkins DWJJoUH. Independent effects of neighborhood poverty and psychosocial stress on obesity over time. 2017;94(6):791–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mason AE, Schleicher S, Coccia M, Epel ES, Aschbacher KJO. Chronic stress and impulsive risk‐taking predict increases in visceral fat over 18 months. 2018;26(5):869–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Araiza AM, Lobel MJS, Compass PP. Stress and eating: Definitions, findings, explanations, and implications. 2018;12(4):e12378. [Google Scholar]
- 54.Tenk J, Mátrai P, Hegyi P, et al. Perceived stress correlates with visceral obesity and lipid parameters of the metabolic syndrome: A systematic review and meta-analysis. 2018;95:63–73. [DOI] [PubMed] [Google Scholar]
- 55.Reynolds JR, Turner RJ. Major life events: Their personal meaning, resolution, and mental health significance. Journal of Health and Social Behavior. 2008;49(2):223–237. [DOI] [PubMed] [Google Scholar]
- 56.Jones A, Pruessner JC, McMillan MR, et al. Physiological adaptations to chronic stress in healthy humans–why might the sexes have evolved different energy utilisation strategies? 2016;594(15):4297–4307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McCabe RE, McFarlane T, Polivy J, Olmsted MP. Eating disorders, dieting, and the accuracy of self-reported weight. International Journal of Eating Disorders. 2001;29(1):59–64. [DOI] [PubMed] [Google Scholar]
- 58.Simmonds M, Llewellyn A, Owen C, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obesity reviews. 2016;17(2):95–107. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


