Highlights
-
•
Pterygoid hamulus elongation syndrome is an extremely rare condition, existed around in 1% of humanity.
-
•
Pain in the soft palate and pharynx can originate from numerous related pathological or anatomical structures.
-
•
The diagnosis of hamular elongation should be based on the detailed history, clinical examination, and correlation with radiographic imaging.
-
•
Management of hamular elongation is preferably to be done with surgical resection, and the conservative solution should be used in limited circumstances.
Keywords: Case report, Pterygoid hamulus elongation, Bursitis, Facial pain, Palatal muscles
Abstract
Introduction
Pain in the soft palate and pharynx can originate from numerous related anatomical structures. Therefore, the diagnosis of patients who complain of pain in these areas is also difficult and challenging. One of the anatomic disorders that causes pain and discomfort in this region is pterygoid hamulus elongation syndrome.
Presentation of case
We report a rare case of pterygoid hamulus elongation with persistent sharp localized pain in the hamular region radiating to the temporal area for four years that was treated successfully by surgical resection of elongated hamulus.
Discussion
Pterygoid Hamulus elongation syndrome is a unique disease presenting many symptoms in the palatal and pharyngeal areas. May caused by injury, infection, or a pre-existing condition. The diagnosis of hamular elongation should be based on detailed history, clinical examination, and correlation with radiographic imaging.
Conclusion
Due to the rarity, PHE syndrome should be diagnosed accurately. Management of hamular elongation is either surgical or conservative but resection of the pterygoid hamulus is usually preferred.
1. Introduction
Pterygoid hamulus elongation syndrome is a rare condition that existed around 1% of humanity [1]. It may produce pain radiating to the soft palate, oropharynx, and temporal area. It generates a similar symptomatic manifestation as trigeminal neuralgia impacted third molar, stylohyoid ligament classification, salivary gland tumors, cysts, and otitis media [2]. Thereby, the diagnosis of the PH is problematic and challenging based mainly based on exclusion. Some authors have suggested infiltration of local anaesthesia can be an excellent diagnostic aid when differentiating hamular pain from possible causes as trigeminal neuralgia [3]. At the same time, the presence of a tender erythematous bony prominence excluded the need for local anaesthetic infiltration. Besides, the presence of an elevated soft-tissue area is not enough for diagnosis, as authors have previously found asymptomatic elongated hamulus as swelling in this region [4]. Treatment may be either conservative or surgical, depending on the actual cause of the pain [1]. The hamular zone needs special clinical assessment because of the wide variety in the differential diagnosis, and due to its complex anatomy Thereby, Clinicians should understand the anatomy, etiology, clinical features, and differential diagnosis for the management of pterygoid hamular elongation [3,5].
This case report has been reported in line with the SCARE 2018 criteria [6].
2. Case presentation
A fifty-five years old female patient presented to the Maxillofacial Department at Nasser Institute for Treatment and Research in Cairo-Egypt.With a chief complaint of tiny bony swelling in the left area of the soft palate. With no history of trauma or injury. However, after being asymptomatic for four years, in 2019, the patient noticed that the swelling became painful with a burning sensation in the region of the left palate radiating to her left head & neck regions. Pain becomes worse when she touched the area with her tongue or finger. This tiny projection became very painful, and she had been under treatment that involved administering several medications like antibiotics and nonsteroidal anti-inflammatory drugs over the past year for otic pain and has several appointments at otorhinolaryngology clinics. The patient reported that pain radiating to the left temporal area causing headache which kept her awake at night our clinical oral examination is made by oral access, manually with a blunt instrument carefully touching the posterior and medial zone of the maxillary tuberosity. The reported pain is frequently localized to the ear zone, but it must be asked if a local or referred pattern is present during the examination, palpation procedure was very painful for the patient. A palpable spike was felt in the left soft palate just medial and posterior to the maxillary tuberosity. The overlying palatal mucosa was of normal shape, texture, and color. On palpation, the spike under the soft palate mucosa was hard, resulting in a burning sensation of the hard and soft palate.
Finally, we requested a CT scan to confirm the diagnosis and made a correlation with clinical examination. We tried a single corticosteroid injection at the site of hamulus elongation, but it failed to cure the symptoms and pain persisted. Thereby, the patient asked for surgical intervention, the procedure explained carefully for the patient, and consented for publication of this case report and accompanied photographs. The surgical procedure consisted of multiple steps performed under strict aseptic precautions under general anaesthesia with nasotracheal intubation was performed then injection of local anaesthesia with vasoconstrictor at the site of pterygoid hamulus, slit incision over the area of pterygoid hamulus was done to expose the spike then resection of hamulus by bone rounger and Smoothening of sharp bony edges with a bone file followed by irrigation of the wound with normal saline and complete hemostasis was achieved and primary closure was performed. Then suturing with resorbable suturing material vicryl 3-0. There were no complaints postoperatively, and the patient was discharged the next day following surgery with necessary post-operative medications as analgesic and mouth wash.
2.1. Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request (Fig. 1, Fig. 2, Fig. 3).
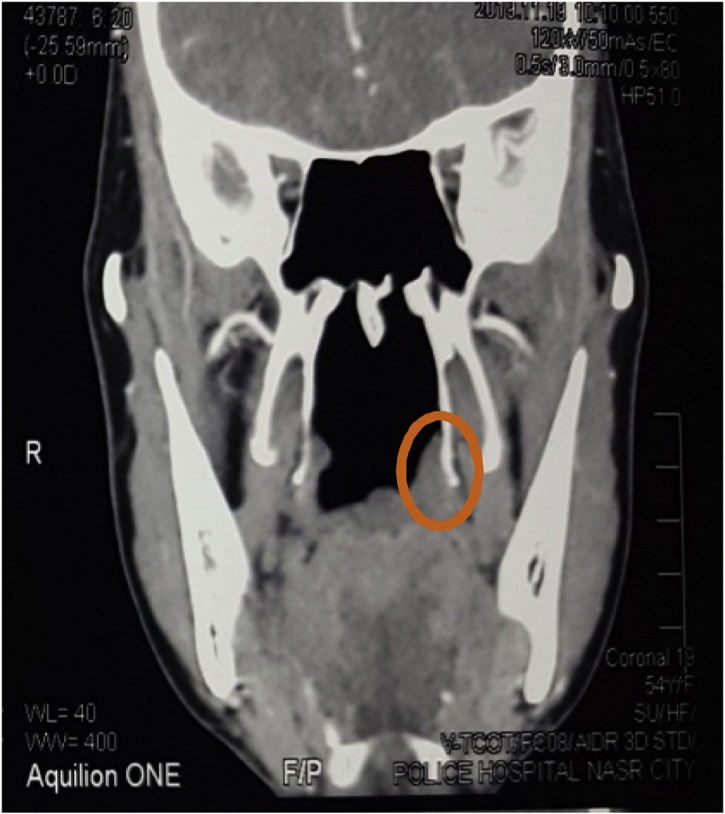
Fig. 1.
Computed tomography scans showing elongated pterygoid hamulus at the area of chief complaining.
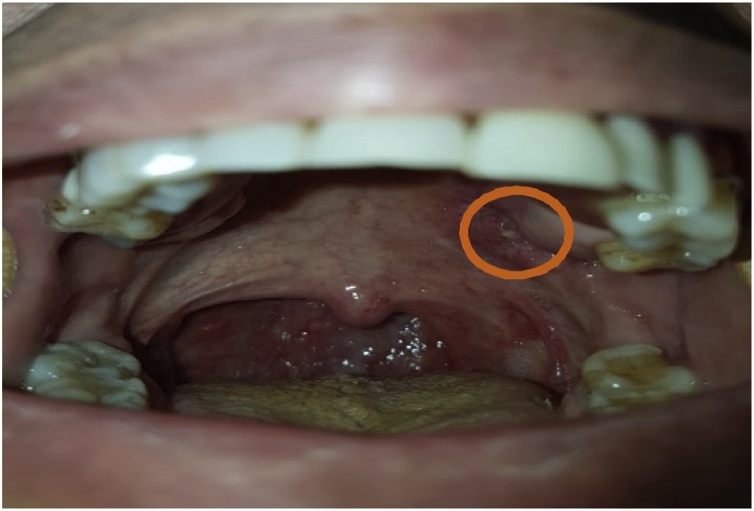
Fig. 2.
Preoperative intraoral photograph, Circle indicates an area of tenderness on palpation.
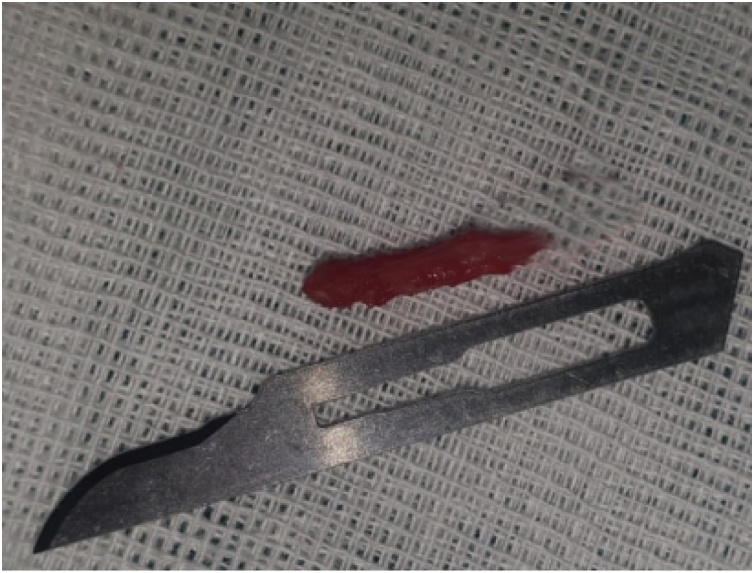
Fig. 3.
The resected pterygoid hamulus measured 9 mm in length.
3. Discussion
Pterygoid hamulus syndrome is a rare condition, with nearly 40 cases reported till now [7]. Symptoms are thought to be caused by underlying bursitis or osteophytes while from an anatomical point of view pterygoid hamulus is a unique, sandwich-shaped structure, which is made up of a denser medial plate made of compact bone and a finer lateral plate [1,8]. These plates communicate with each other by trabecula. The average length of the left hamulus is 5.0 mm, and that of the right is 4.9 mm in normal individuals [9,10]. There is no consensus on the etiology of this syndrome till now, but one of the following might be responsible to cause PHE, as two theories are trying to explain the pterygoid hamulus elongation syndrome. The first one depends on the topography of PH, and its structure is considered the main cause of the chronic pain. However, there is another syndrome termed pterygoid Hamulus bursitis (PHB), Bursae are fluid-filled compacted sacs with synovial fluid that acts as a cushion between bones, tendons, joints, and muscles [11,3]. Thereby, (PHB) is due to Bursitis of the tensor veli palatini while in pterygoid hamulus elongation, there is an osteophyte elongation of the pterygoid hamulus [12,1]. The pain may spread to the temporal region or neck simulating tension headache or imitating dental disease [13,9]. There are also cases of PHE spreading of pain to the orbital area, the pain may move apart to half of the face in the literature [10], PH morphology may be correlated to the development of Muscles attached to the Hamulus exert on it a dorsal and medial pressure while in contrast, the pterygomandibular raphe exerts pressure in dorsal and lateral direction.
Most forces bending the PH in the medial direction. Therefore, the huger thickness of the medial plate of the pterygoid process is correlated to a greater pressure produced by numerous forces [14,8]. While the second theory that tries to explain the pain on theses area depend on the fact that Bursitis can be triggered by an injury, infection, or a pre-existing condition. Minor infection or trauma can produce an increase in the amount of bursa fluid, leading to an expansion of the bursa causing pain and limitation in movement [3,9]. Bursitis produced by an injury mostly takes time to develop. Traumatic injury is very common in the hamular bursitis patients [15]. Anaesthesia intubation, swallowing a huge bolus, yawning, overextended maxillary prosthesis as a complete or partial denture, and the traumatic hitting during teeth brushing, all of these can produce this pathological condition. Individuals with extra prominent hamular are recognized to be more liable to mechanical trauma [3]. The expression of pterygoid Hamulus syndrome was first described as a source of pain in the palatal and pharyngeal regions produced by an atypically shaped pterygoid Hamulus by Hjorting Hansen [16]. Bursitis of the tensor veli palatini muscle produced by an osteophyte on the pterygoid hamulus, or bursitis of the tendon of the tensor veli palatini muscle as it twists around pterygoid hamulus depending on the repetition of minimal trauma to the overlying soft tissue. Thereby, we suggested that as reported in our case the cause of pterygoid hamulus elongation syndrome mainly depends on the first theory which suggests the tomography and anatomical structure variation to be the main cause of PHE as our patient doesn’t exposed to any source of trauma or infection along this period. The diagnosis of the PHE depends on a comprehensive discussion with clinical and radiographic assessment of the head and neck region due to the rarity of the disease, exclusion from the diagnosis becomes a rule rather than the exception with focusing on the oral cavity, hard and soft palate, upper dental arch, maxillary tuberosity, temporomandibular joints, and masticatory muscles [16,10]. As the differential diagnosis of pterygoid hamulus elongation syndrome may include Elongated styloid processes (Eagle’s syndrome), Parotid gland tumors, Existence of a foreign body, and Impacted third molar [17,16]. conventional radiographic imaging such as lateral cephalometric, submentovertex, and advanced imaging including computed tomography scan in axial and coronal planes with three-dimensional views can be used. Because of the availability of advanced imaging modalities such as CBCT, measurements of the length and inclination became more possible so CBCT should be desired over a CT image when possible [16,18]. Generally, there is no accepted protocol in the management of the PHE for calming treatment, the local trauma origin must be eliminated, and a soft diet is recommended. Injection of synthetic cortisone into the Hamulus region can be an extra choice of conservative treatment [5]. As the Conservative approaches (Medical) based on patient education, dietary counseling, and avoidance of soft palate irritation. When medical treatment fails, surgical treatment should be established [13,14,1].
4. Conclusions
Pterygoid hamulus elongation is a source of pain in the palatopharyngeal area, which may cause radiating pain in the maxilla, which could be misleading in diagnosis due to unpopularity and difficulty in clinical judgment. Evaluation of patients with orofacial pain should be done meticulously to identify the precise nature of pain. As pain in the maxillofacial region may be caused by many factors such as odontogenic and non-odontogenic pathology, or variation in anatomical structure as through the assessment should be based on the clinical examination and radiographic imaging when needed.
Conflicts of interest
There is no conflict of interests.
Funding
There were no sources of Funding.
Ethical approval
There was no ethical approval needed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Omar Elmonofy: Writing original draft, review & editing, investigation, data curation
Ahmed ElMinshawi: Review & editing
Ahmed ElMinshawi: Review & editing
Fahmy Mobarak: Review & editing
Fahmy Mobarak: Review & editing
Registration of research studies
researchregistry6249 available at: https://www.researchregistry.com/browse-the-registry#home/registrationdetails/5fabbc5b9b5913001574520c/.
Guarantor
Omar Elmonofy.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Shankland W.E., II Pterygoid hamulus bursitis: one cause of craniofacial pain. J. Prosthet. Dent. 1996;75:205–210. doi: 10.1016/s0022-3913(96)90100-6. [DOI] [PubMed] [Google Scholar]
- 2.Scully C., Sebastián J.V.B., Carrozzo M. Elsevier Health Sciences; 2012. Pocketbook of Oral Disease-E-Book. [Google Scholar]
- 3.Arya S., Singhal P., Vengal M. Hamular bursitis: difficult to diagnose in orofacial pain. Pak. Oral Dent. J. 2015;35 [Google Scholar]
- 4.Chaitow L. Elsevier Health Sciences; 2005. Cranial Manipulation: Theory and Practice: Osseous and Soft Tissue Approaches. [Google Scholar]
- 5.Cho J.-Y., Cheon K.-Y., Shin D.-W. Pterygoid hamulus bursitis as a cause of craniofacial pain: a case report. J. Korean Assoc. Oral Maxillofac. Surg. 2013;39:134–138. doi: 10.5125/jkaoms.2013.39.3.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Sharma N.A., Garud R.S. Greater palatine foramen–key to successful hemimaxillary anaesthesia: a morphometric study and report of a rare aberration. Singapore Med. J. 2013;54:152–159. doi: 10.11622/smedj.2013052. [DOI] [PubMed] [Google Scholar]
- 8.Galvez P., Moreau N., Fenelon M. Pterygoid hamulus syndrome: a case report. J. Oral Med. Oral Surg. 2020;26(42) [Google Scholar]
- 9.Firdouse A., Firdoose N., Ghousia S. An unusual clinical vignette of oro-pharyngeal discomfort: Pterygoid Hamulus syndrome. Med. Pharm. Reports. 2020;93:306. doi: 10.15386/mpr-1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Motiwale T., Motiwale G., Motiwale S. 2020. Pterygoid Hamulus Bursitis: A Rare Case Report. [Google Scholar]
- 11.Shetty S.S., Shetty P., Shah P.K. Pterygoid hamular bursitis: a possible link to craniofacial pain. Case Rep. Surg. 2018;2018 doi: 10.1155/2018/5108920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thukral H., Nagori S.A., Rawat A., Jose A. Pterygoid Hamulus Bursitis: A rare intra-oral pain syndrome. J. Craniofac. Surg. 2019;30:e643–e645. doi: 10.1097/SCS.0000000000005700. [DOI] [PubMed] [Google Scholar]
- 13.Barchetta N.F., de Oliveira R.L.B., Silveira V.Á.S, Faig-Leite H. Clinical and morphofunctional aspects of pterygoid hamulus: literature review. Braz. Dent. Sci. 2015;18:5–11. [Google Scholar]
- 14.Sasaki T., Imai Y., Fujibayashi T. A case of elongated pterygoid hamulus syndrome. Oral Dis. 2001;7:131–133. [PubMed] [Google Scholar]
- 15.Salins P.C., Bloxham G.P. Bursitis: a factor in the differential diagnosis of orofacial neuralgias and myofascial pain dysfunction syndrome. Oral Surg. Oral Med. Oral Pathol. 1989;68:154–157. doi: 10.1016/0030-4220(89)90183-7. [DOI] [PubMed] [Google Scholar]
- 16.Roode G.J., Butow K.-W. 2014. Pterygoid Hamulus Syndrome–undiagnosed. [PubMed] [Google Scholar]
- 17.Öztunç H., Evlice B., Tatli U., Evlice A. Cone-beam computed tomographic evaluation of styloid process: a retrospective study of 208 patients with orofacial pain. Head Face Med. 2014;10(5) doi: 10.1186/1746-160X-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Montalbetti L., Ferrandi D., Pergami P., Savoldi F. Elongated styloid process and Eagle’s syndrome. Cephalalgia. 1995;15:80–93. doi: 10.1046/j.1468-2982.1995.015002080.x. [DOI] [PubMed] [Google Scholar]