Highlights
-
•
Mucinous adenocarcinoma of the perianal region is extremely rare (6.9% of anal neoplasms and 2–3% of all gastrointestinal malignancies).
-
•
Given the low incidence of this tumor, it is often missed at initial evaluation.
-
•
Association with chronic perianal fistula are common and inflammatory symptoms can be misleading with delay in diagnosis.
-
•
The paucity of publications leads to a lack of consensus on both diagnostic and therapeutic approaches.
-
•
The understanding of the etiopathogenic mechanisms may lead to the development of novel diagnostic and therapeutic protocols.
Keywords: Anal fistula, Mucinous adenocarcinoma, Colonic polyps, Case report
Abstract
Introduction
Perianal mucinous adenocarcinoma is rarely encountered in the setting of anal neoplasms. The rarity of the disease and the paucity of publications on this topic are responsible for a lack of diagnostic and therapeutic guidelines.
Presentation of case
An 80-year-old man with mucinous adenocarcinoma of the anal canal associated with dysplastic polyps of the colon was treated by multiple endoscopic polypectomies and abdomino-perineal resection of the rectum. We discuss the management of this rare case from the diagnosis up to one-year follow-up.
Discussion
Perianal mucinous adenocarcinoma is a very rare entity frequently combined with chronic fistulas. Inflammatory symptoms may mislead its diagnosis, which is often delayed. The unique association between perianal mucinous adenocarcinoma and dysplastic polyps of the colon, that we have reported, may suggest a secondary etiology. High clinical suspicion is important for early and correct diagnosis, which should be based on endoanal ultrasound and/or magnetic resonance imaging followed by deep tissue biopsies.
Conclusion
We stress the importance of accumulating such cases in the literature. The understanding of the etiopathogenic mechanisms may lead to the development of novel diagnostic and therapeutic protocols.
1. Introduction
Mucinous adenocarcinoma of the perianal region is an extremely rare entity, accounting for only 6.9% of anal neoplasms and representing 2–3% of all gastrointestinal malignancies [1]. Its pathogenesis can be related to either dysplastic degeneration in a chronic recurrent fistula or seeding of tumor cells from a colorectal malignancy directly into a fistula tract [2]. Perianal fistulas, on the other hand, are common pathologies which affect 12.3/100000 men and 8.6/100000 women [3]. Given the low incidence of this tumor, it is often missed at initial evaluation. Symptoms from a chronic perianal fistula are common and can be misleading with delay in diagnosis and therapeutic decision-making. The biological behavior of this tumor is still unclear; however, it is known to be locally aggressive with poor prognosis and there is no consensus on its potential systemic dissemination. In this uncertain scenario, the paucity of publications leads to a lack of consensus on both diagnostic and therapeutic approaches.
The aim of our study was to discuss diagnostic and therapeutic options of a rare case of perianal mucinous adenocarcinoma associated with multiple dysplastic polyps of the colon. This report is compliant with the SCARE 2018 criteria [4].
2. Case report
An 80-year-old man was referred to our institution for a perianal swelling (Fig. 1) with jelly-like discharge and painful defecation of one-year duration. Past medical history was remarkable for hypertension, type 2 diabetes, and recurrent anal fistula over several years, though he never sought treatment. The patient had a negative family history of cancer. Digital examination revealed an elastic hard lesion in the left posterior quadrant with multiple external openings and gelatinous discharge upon squeezing. Immediate skin biopsy of an ulcerated external opening was performed, but pathological examination showed only non-specific inflammatory material. The patient underwent examination under anesthesia; a trans-sphincteric fistula and multiple cavities filled with gelatinous material were found. A fistulectomy with seton insertion was performed, and the hard tissue lining the multicystic lesion was sent for histopathological examination that revealed a moderately differentiated mucinous adenocarcinoma.
Fig. 1.
Perianal swelling with multiple external openings.
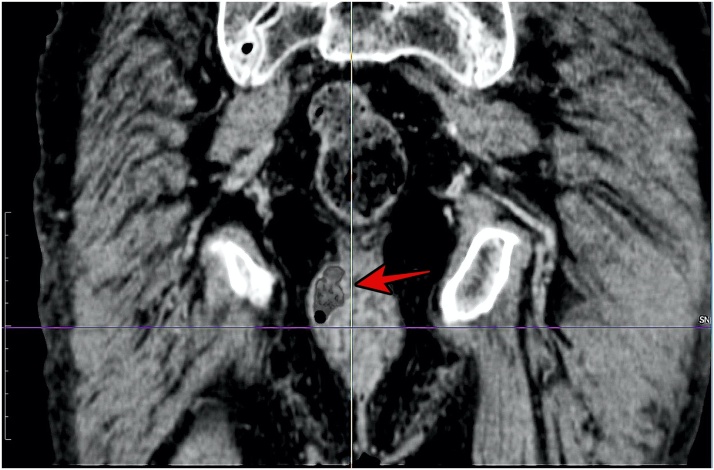
Chest and abdominal computed tomography (CT) scan showed hypodense areas of fluid density around the anal canal (Fig. 2) with no evidence of lymph node or distant metastases. Colonoscopy showed no mucosal lesions in the anal canal and multiple polyps of the colon. Tumor markers (CEA, Ca 19.9) were in the normal values range.
Fig. 2.
CT scan showing hypodense areas of fluid density around the anal canal.
The patient was informed and involved in the decision-making process. He underwent multiple endoscopic polypectomies and open abdomino-perineal resection (APR) of the rectum (Fig. 3). The main procedure (APR) was performed by an experienced colorectal surgeon (senior assistant with more of 10 years of specialized training). The histopathological diagnosis revealed an extramucosal mucinous adenocarcinoma with no lymph node metastasis (pT3N0) and multiple dysplastic polyps of the colon. Immunohistochemical study was positive for CK7, CK20, CDX2 and MUC5AC and negative for BRST2. The postoperative recovery was uneventful, and the patient was discharged home after seven days. After multidisciplinary evaluation, the patient was submitted to adjuvant radiotherapy (45 Gy given in 5 weekly fractions) followed by chemotherapy (Capecitabine) which was discontinued a few months later because of intolerable side effects. He was satisfied for the treatment results.
Fig. 3.
Surgical specimen showing the integrity of mucosal area.
One year later, the patient is in good health except for an incisional hernia, tumor markers (Ca 19.9, CEA) are still normal in range, and there is no evidence of local or distant recurrence at CT scan.
3. Discussion
Perianal mucinous adenocarcinoma is a very rare entity among anorectal tumors as confirmed by the scarcity of reports in the literature with less than 150 cases published in the literature [5]. This leads to the need for deeper knowledge to help in the development of diagnostic and therapeutic algorithms. A very recent review on mucinous adenocarcinomas found that tumors of the anal region are more frequent in men (61.3 vs. 38.7%), with a mean age of 66.5 ± 14.8 years [6].
The pathogenesis of this pathology is still unknown. In 1934, Rosser firstly tried to better understand and classify this rare entity [7]. Today, the main and most accepted theory refers to the malignant degeneration of chronic inflammatory perianal fistulas (primary) [8]. However, another theory links the origin of this tumor with the seeding of premalignant cells originated in the adjacent colon (secondary) into the fistula tract [9,10]. Association with benign chronic inflammatory processes is common, such as perianal fistulas or abscesses and Crohn’s disease. Nonetheless, this report shows the coexistence of the adenocarcinoma with dysplastic polyps of the colon and, to the best of our knowledge, this is the first report of this association. Premalignant cells from a proximal polyp could have seeded into the perianal fistula tract and chronic inflammation may have promoted tumorigenesis. Though this connection is in favor of the ‘seeding theory’, it is not possible to draw a definitive conclusion unless other similar cases are described.
Another crucial point is the frequent delayed diagnosis. The malignant degeneration is often hidden by inflammatory symptoms from the benign overlaying disease, leading to late diagnosis. Imaging studies may guide and direct therapy. Abdominal CT scan may reveal a solid lesion with hypodense areas of fluid density. Magnetic Resonance Imaging (MRI) has been described to be more precise, showing hyperintense fluid on T2-weighted images, enhanced solid components and a fistula between the mass and the anus [11]. Positron Emission Tomography (PET) has limited use for the diagnosis, because there is a negative correlation between the amount of mucin present and tumor fluorodeoxyglucose (FDG) uptake [12]. Finally, endoanal ultrasonography (EUS) has been suggested in patients with recurrent fistulas, to find the malignant lesion and to better guide tissue biopsy [13]. Histopathological study is mandatory to rule out malignancy. However, in our patient the first tissue biopsy was negative and misled our initial therapeutic approach. Therefore, we believe that a high index of clinical suspicion is important for early and appropriate diagnosis, which should be based on EUS and/or MRI examination. As already reported [2,13], we also suggest taking deep biopsies of any recurrent fistulas with cytology of mucin obtained by drainage of mucous lakes.
There is general consensus on the need for a radical surgical approach, such as the APR of the rectum. On the other hand, greater uncertainty is found when deciding the timing for radio-chemotherapy. In such concern, several studies favor neoadjuvant radio-chemotherapy [14]. However, in our case, the difficulties of tumor diagnosis prevented us to propose a neoadjuvant protocol and we were forced to choose an adjuvant regimen. The rationale for selecting either neoadjuvant, adjuvant, or combined therapies is still weak, and further investigation with more patients is required.
In conclusion, perianal mucinous adenocarcinoma is a very rare entity frequently combined with chronic fistulas. Inflammatory symptoms may mislead its diagnosis, which is often delayed. The unique association between perianal mucinous adenocarcinoma and dysplastic polyps of the colon that we have reported may suggest a secondary etiology. There is still a lack of consensus on both diagnostic and therapeutic approaches to the disease.
Therefore, we stress the importance of accumulating such cases in the literature, because the understanding of the etiopathogenic mechanisms may lead to the development of novel diagnostic and therapeutic protocols.
Declaration of Competing Interest
All authors have no substantial direct or indirect commercial financial incentive associated with publishing the manuscript.
Funding
The study sponsors had no such involvement.
Ethical approval
Whether approval by Institutional Board has been given for this case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author’s contribution
Claudio F. Feo: Writing paper.
Simone Veneroni: Writing paper.
Antonio Santoru: Writing paper.
Antonio M Scanu: data analysis.
Maria L Cossu: Text edit.
Giorgio C. Ginesu: data collection.
Alberto Porcu: text edit.
Registration of research studies
Not applicable.
Guarantor
Giorgio C Ginesu; Claudio C Feo.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Claudio F. Feo, Email: cffeo@uniss.it.
Simone Veneroni, Email: simone.veneroni@gmail.com.
Antonio Santoru, Email: antonio.santoru@gmail.com.
Maria Laura Cossu, Email: mlcossu@uniss.it.
Antonio M. Scanu, Email: scanu@uniss.it.
Giorgio C. Ginesu, Email: ginesugc@uniss.it.
Alberto Porcu, Email: alberto@uniss.it.
References
- 1.Pai V.D., Jatal S., Engineer R., Ostwal V., Saklani A.P. Multidisciplinary management of colorectal adenocarcinoma associated with anal fistula: an Indian series. Colorectal Dis. 2015;17(11):240–246. doi: 10.1111/codi.13100. [DOI] [PubMed] [Google Scholar]
- 2.Okada K.-I., Shatari T., Sasaki T., Tamada T., Suwa T., Furuuchi T., Takenaka Y., Hori M., Takuma M. Is histopathological evidence really essential for making a surgical decision about mucinous carcinoma arising in a perianal fistula? Report of a case. Surg. Today. 2008;38:555–558. doi: 10.1007/s00595-007-3651-0. [DOI] [PubMed] [Google Scholar]
- 3.Göttgens K.W., Smeets R.R., Stassen L.P., Beets G., Breukink S.O. Systematic review and meta-analysis of surgical interventions for high cryptoglandular perianal fistula. Int. J. Color Dis. 2014;30:583–593. doi: 10.1007/s00384-014-2091-8. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Jee S.L., Amin-Tai H., Fathi N.Q., Jabar M.F. Perianal mucinous adenocarcinoma diagnosed by histological study of anorectal abscess with fistula. Case Rep. J. 2018;5:e21. doi: 10.14309/crj.2018.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benesch M.G.K., Mathieson A. Epidemiology of mucinous adenocarcinomas. Cancers (Basel) 2020;12(11):3193. doi: 10.3390/cancers12113193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosser C. The relation of fistula-in-ano to cancer of the anal canal. Trans. Am. Proc. Soc. 1934;35:65–71. [Google Scholar]
- 8.Alvarez-Laso C.J., Moral S., Rodríguez D., Carrocera A., Azcano E., Cabrera A., Rodriguez R. Mucinous adenocarcinoma on perianal fistula. A rising entity? Clin. Transl. Oncol. 2017;20:666–669. doi: 10.1007/s12094-017-1750-y. [DOI] [PubMed] [Google Scholar]
- 9.Rollinson P.D., Dundas S.A. Adenocarcinoma of sigmoid colon seeding into pre- existing fistula in ano. Br. J. Surg. 1984;71:664–665. doi: 10.1002/bjs.1800710904. [DOI] [PubMed] [Google Scholar]
- 10.Spiridakis K.G., Sfakianakis E.E., Flamourakis M.E., Intzepogazoglou D.S., Tsagataki E.S., Ximeris N.E., Rachmanis E.K., Gionis I.G., Kostakis G.E., Christodoulakis M.S. Synchronous mucinous adenocarcinoma of the rectosigmoid seeding onto a pre-existing anal fistula. Int. J. Surg. Case Rep. 2017;37:48–51. doi: 10.1016/j.ijscr.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamaguchi T., Kagawa R., Takahashi H., Takeda R., Sakata S., Nishizaki D. Diagnostic implications of MR imaging for mucinous adenocarcinoma arising from fistula in ano. Tech. Coloproctol. 2009;13(3):251–253. doi: 10.1007/s10151-009-0509-z. [DOI] [PubMed] [Google Scholar]
- 12.Wnorowski A.M., Menias C.O., Pickhardt P.J., Kim D.H., Hara A.K., Lubner M.G. Mucin-containing rectal carcinomas: overview of unique clinical and imaging features. Am. J. Roentgenol. 2019;2013:1–9. doi: 10.2214/AJR.18.20864. [DOI] [PubMed] [Google Scholar]
- 13.Toyonaga T., Mibu R., Matsuda H., Tominaga Y., Hirata K., Takeyoshi M., Tsuneyoshi M., Matsushima M. Endoanal ultrasonography of mucinous adenocarcinoma arising from chronic fistula-in-ano: three case reports. J. Anus Rectum Colon. 2017;1(3):100–105. doi: 10.23922/jarc.2017-011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaertner W.B., Hagerman G.F., Finne C.O., Alavi K., Jessurun J., Rothenberger D.A., Madoff R.D. Fistula-associated anal adenocarcinoma: good results with aggressive therapy. Dis. Colon Rectum. 2008;51:1061–1067. doi: 10.1007/s10350-008-9294-4. [DOI] [PubMed] [Google Scholar]