Abstract
Background
Children with cancer were designated as clinically extremely vulnerable if they were to contract SARS‐CoV‐2 due to immune suppression in the early phase of the COVID‐19 pandemic. Our aim was to explore experiences, information and support needs, and decision making of parents with a child with cancer in response to this phase in the United Kingdom.
Methods
Parents of a child with cancer completed a survey at a time when the UK moved into a period of ‘lockdown’. An online survey was developed by the research team to capture parents’ experiences, information and support needs, and decision making, using closed statements and open text boxes. Descriptive quantitative analyses and qualitative thematic content analysis were undertaken.
Findings
One hundred seventy‐one parents/caregivers completed the survey. Eighty‐five percent were worried about the virus and they were vigilant about the virus (92%) or cancer symptoms (93.4%). For two‐thirds (69.6%), hospital was no longer considered a safe place. Eight overarching themes were identified related to the virus: (a) risk of infection; (b) information, guidance and advice; (c) health care provision; (d) fears and anxieties; or related to lockdown/isolation: (e) psychological and social impact; (f) keeping safe under lockdown; (g) provisions and dependence; and (h) employment and income.
Conclusions
This is the first study, to the best of our knowledge, to report experiences of parents of a child with cancer during the SARS‐CoV‐2/COVID‐19 pandemic. The majority of parents were worried about SARS‐CoV‐2 and transmitting the virus to their child. Hospital was no longer perceived to be a safe place, and parents were worried about suboptimal cancer care. Parents described fear and anxiety and the psychological, social and economic impact of isolation.
Keywords: cancer, child, COVID‐19, mental health, parents, well‐being, worries
Abbreviations
- ALL
acute lymphoblastic leukaemia
- CNS
central nervous system
- PPE
personal protective equipment
1. INTRODUCTION
In the United Kingdom (UK), the administrations in England, Wales and Scotland, initially considered children and young people with cancer to be ‘extremely clinically vulnerable’, a phrase used to designate individuals who were believed to be at high risk of developing severe COVID‐19 disease if they were to contract SARS‐CoV‐2. Children with cancer were designated as such due to immune suppression as a result of anticancer treatment. They were recommended to ‘shield’—to remain at home at all times and have no face‐to‐face contact with anyone outside of their household, except to attend to medical needs. The general population also entered ‘lockdown’ (23 March 2020), with restrictions of movement outside of the home other than for specific designated purposes (ie, exercise, shopping for essentials, and ‘key workers’ defined as employees who provide vital services maintaining health and essential infrastructure). During this period of time, the understanding of the transmissibility of SARS‐CoV‐2 was uncertain, and the nature of the symptoms was evolving. In the country at large panic buying (stockpiling) was seen, concerns increased about financial vulnerability, and availability and implementation of personal protective equipment (PPE) in the health care setting varied. Through this time, comprehensive and updated advice for parents of children with cancer was compiled and disseminated through national charities and professional organisations in the UK. 1
The experience of clinical and charity teams revealed families were worried about SARS‐CoV‐2 infection. This was in keeping with the documented experience of families under quarantine for recent severe respiratory viruses (SARS‐CoV‐1, Middle East respiratory syndrome ‐ MERS) where a systematic review showed very high levels of traumatic distress. 2 Parents believed their child with cancer was vulnerable to developing COVID‐19. 1 The data available show that, while cases are few 3 and the disease caused by infection has been relatively mild, ongoing surveillance of the disease manifestations is encouraged. 4 , 5 , 6
Children and young people undergoing treatment face ongoing compromises to the immune system, even without a pandemic, this forces families to manage infection risks regularly. The pandemic heightened the need to understand family decision making around continuing treatment, ‘shielding’ (isolation within the home) and accessing hospital. 7
This decision making is made even more difficult as new information emerges, for instance with the reporting on multisystem inflammatory disease in children. 8 , 9
In general, when information changes, choices change, producing inconsistencies and difficulties. 10 , 11 , 12 For example, fewer visits by children in emergency departments in the early phases of the pandemic were recorded. 13
Families of children with cancer indicated on social media groups, they felt forgotten, with their voice not represented in decision making by governments and health care systems. Existing professional networks of charities, clinicians, academics and parents were mobilised to develop the current study. The aim of the study was to use a survey to gather quantitative and qualitative data specifically about the experiences, information and support needs, as well as decision making of these families.
2. AIMS
To explore experiences, information and support needs, and decision making of parents of a child with cancer in response to COVID‐19.
3. METHODS
This study included survey of parents of a child with cancer, assessing experiences, information and support needs, and decision making. The findings presented here are part of a larger longitudinal study (the SHARE study) assessing experiences of parents and children with different paediatric conditions, over time (baseline, 2, 6 and 12 months), which will allow comparisons over time and between subgroups. The survey opened to responses on 6 April 2020 and closed on 4 May 2020, capturing experiences and needs of parents during the first wave and lockdown of the COVID‐19 pandemic within the UK. The study was approved by the University of Southampton and UK NHS Health Research Authority Research Ethics Committees (IRAS nr. 282176).
3.1. Participants
Participants were parents of a child with cancer aged between 0 and 18 years, able to read and respond in English. Parents were recruited through two principal treatment centres in the UK, by parents being directly contacted by their clinical team regarding the study (via email, text message or through outpatient clinics), and through social media, national charities and targeted closed Facebook groups, to minimise the burden on the health system during the pandemic. Electronic consent was obtained before completing the online survey. Approximately 150‐200 respondents were intended to be recruited to ensure sufficient number of participants to map the range of issues and experiences, identify common issues across them, 14 , 15 , 16 carry out meaningful subgroup analyses, and provide rich information from the open text qualitative data.
3.2. Survey
The survey content was developed based on currently available literature, 17 , 18 , 19 expert clinician input, and parental review. It contained the following sections and number of closed statement items: Experiences (n = 6), Information (n = 7), Decisions (n = 7) and Support needs (n = 5) (Figure 1). The response options for the closed statement items were Not at all, A little, Quite a bit, Very much (except for two conditional questions with Yes/No as response options). Each section started with a free text box for comments, with simple introductory questions. Experiences ‘Can you tell us about your experiences and views on the virus in relation to your child with cancer?’; Information: ‘Can you tell us where you get information on the virus and what other information you might need?’; Decisions: ‘Can you tell us how you make decisions about looking after your child in relation to the virus?’; Support: ‘What additional support would you like, at home or in hospital, in relation to the virus?’. These were intended to be completed prior to the closed questions, which guided the respondent's thinking. A final free text question asked respondents whether they had any further comments.
FIGURE 1.
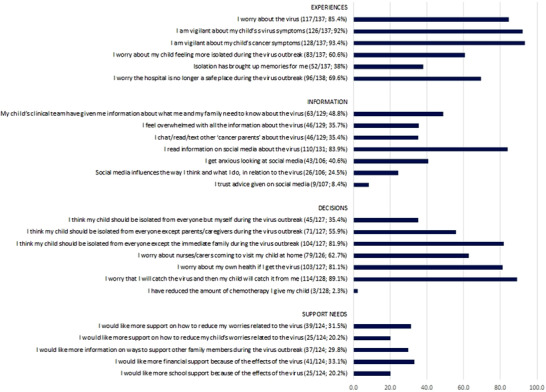
Closed statements percentages (of those who agree Quite a bit or Very much)
For simplicity, SARS‐CoV‐2 was referred to as ‘the virus’. Demographic information was collected from parents, including parent age, child age, child's diagnosis and child being on or off treatment. The number of items were purposely less, allowing for rapid analysis and dissemination and increased likelihood of completion. Prior to distributing the survey, feedback from parents in our parent/patient involvement group was sought about the value and timing of the research, along with detailed questions about the survey in terms of content, phrasing and completeness, and changes were made accordingly.
3.3. Data analysis
Descriptive statistics were carried out using IBM Statistical Package for Social Science (SPSS) 20 to summarise the demographic data, and undertake simple descriptive statistics of the closed statement items (collapsing the lowest two response options (Not at all, A little), and the highest two response options (Quite a bit, Very much) into a binary outcome).
Subgroup analyses were carried out on an item level, using chi‐square analyses, according to child's age (split around the median, age 7 years), treatment (on/off treatment), and diagnosis—acute lymphoblastic leukaemia (ALL), solid tumour, central nervous system (CNS) tumour, or other.
The open text box data were subjected to a thematic content analysis, informed by a three‐stage coding process. 21 , 22 Stage 1: initial sample of 35 comments were open coded into broad comment categories by two researchers (SS and RW), developing an initial framework, and resolving any conflicts with a third researcher (ASD); stage 2: the framework was used to categorise all comments from the data, with further refinement; stage 3: overarching themes were identified from analysis of similarities in the content between categories. The number of comments were counted to identify weight of themes. Given the overlap in comments to categories the total number of comments did not match the number of participants.
4. RESULTS
4.1. Participants
Total 171 respondents completed the survey, of which the majority were mothers (n = 143, 83.6%), and nine fathers (Table 1). The child's median age was 7 years (range 1‐24 years). The majority were on treatment (67.3%) and 28.7% were off treatment for less than 5 years. The majority of patients were children with ALL (75, 43.9%), and 43 (25.1%) with a solid tumour (Wilms, rhabdomyosarcoma, germ cell tumour, osteosarcoma, fibrolamellar hepatocellular carcinoma, neuroblastoma, retinoblastoma, Ewing's sarcoma, renal cell carcinoma), 12 lymphoma (7.0%), 11 CNS/brain (6.4%), and six with acute myeloid leukaemia (3.5%). The majority of parents (132; 77%) were recruited through Facebook (the specific Facebook site is not known), and the remaining participants through accessing survey directly (18, 10%; route of access, eg, via twitter link), through the UK charities Children with Cancer (n = 1) and CLIC Sargent (n = 1), University Hospitals Southampton (n = 2) and the University of Southampton (n = 15), with missing data from 15 participants (9%).
TABLE 1.
Sample characteristics
| Variables | Values |
|---|---|
| Completed by, n (%) | |
| Mothers | 143 (83.6%) |
| Father | 9 (5.3%) |
| Parent | 9 (5.3%) |
| Other | 4 (2.3%) |
| Missing | 6 (3.5%) |
| Caregiver mean age, years, median (range) | 39 (22‐67) |
| Child's age, years, median (range) | 7 (1‐24) |
| Child's treatment status, n (%) | |
| On treatment | 115 (67.3%) |
| Off treatment <5 years | 49 (28.7%) |
| Off treatment >5 years | 5 (2.9%) |
| Missing | 2 (1.2%) |
| Diagnosis, n (%) | |
| Acute lymphoblastic leukaemia | 75 (43.9%) |
| Solid tumour | 43 (25.1%) |
| Lymphoma | 12 (7.0%) |
| Brain tumour | 11 (6.4%) |
| Acute myeloblastic leukaemia | 6 (3.5%) |
| Other | 8 (4.7%) |
| Missing | 16 (9.4%) |
4.2. Closed statement items
A large percentage of parents—those responding ‘Quite a bit’ or ‘Very much’—worried about the virus (85.4%), and the majority of parents described being vigilant about virus symptoms (92%) or cancer symptoms (93.4%). For two‐thirds (69.6%) of the respondents, hospital was no longer considered a safe place. Parents received information from their clinical team (48.8%) and accessed information on social media (83.9%), which, for some, led to feeling anxious (40.6% of those who accessed social media information). Many parents indicated they isolated their child, except from immediate family (81.9%). Parents also worried about their own health (81.1%) and about the child contracting the virus from them (89.1%). The reported worries did not lead to parents stopping or reducing chemotherapy (only 2.3% did so). The desire for support to reduce worries for themselves or others was reported by 20‐30% of parents. Group differences in terms of age (0‐7 years vs 7‐18 years) were found for two items. Parents of younger children were more worried about nurses/carers visiting at home (P = .001), and more likely to want information on ways to support family members (P = .002). Parents with a child on treatment were more likely to report that the child should be isolated from everyone except parents/caregivers (P = .025). No differences were found according to the cancer type.
4.3. Open text boxes
A total of 591 comments were coded: 130 in the Experiences section, 124 in the Information section, 122 in the Decision‐Making section, and 112 in the Support section (and a final 103 in the ‘other’ box).
4.4. ‘Experiences’ free text response
In total, 130 parents (76% of the total) responded to the question about experiences. Overall, the responses to this question covered 38 subthemes (Table 2, including illustrative quotes) which were organised into the following eight overarching themes, related to the virus (four themes) or lockdown and isolation (four themes) (Figure 2). Virus: (a) risk of infection; (b) information, guidance and advice; (c) health care provision; (d) fears and anxieties; Lockdown and isolation: (e) psychological and social impact; (f) keeping safe under lockdown; (g) provisions and dependence; (h) employment and income (Table 2).
TABLE 2.
Themes and subthemes of open text boxes
| Theme | Subtheme | Number | Quotes |
|---|---|---|---|
| VIRUS | |||
| Risk of infection | Concern over child's low immunity | 44 | We are concerned that COVID‐19 could get to her easier than the average child |
| Concern over visiting hospitals | 22 | A place that once was considered safe for our son I now consider to be a great risk due to the risk of catching the virus; the thought of us having to go in overnight is keeping me awake at night | |
| Family member has/had COVID‐19 | 7 | It's very worrying more so now as my eldest child has symptoms of the virus | |
| Concern over infection entering the home from parent having to work or shop for provisions | 6 | I am very nervous about going into shops, etc in case I pick something up and take it home | |
| Concern over varied approach to wearing ersonal protective equipment (PPE) | 5 | Some staff are wearing PPE and some are not | |
| Vigilance of symptoms | 2 | Extremely on edge about a temperature spike | |
| Information, guidance and advice | Limited information/mixed messaging | 17 | All the information seemed geared at adults not families with vulnerable children. There was a lot of mixed information at the start of the isolation period and far too many grey areas |
| Need for targeted advice and support | 8 | Children within 2 years of transplant are high risk, those people with spleen issues are high risk. Where does this leave our 8 year old? Surely, she cannot be the same low risk as a child who has not had leukaemia, pneumonia, lung fungal infection, possible spleen issues. But we are left on our own in terms of guidance | |
| Information regarding child's vulnerability status not issued | 4 | We didn't receive a letter saying ‘X’ was at high risk but when I spoke to somebody at Macmillan they said she was high risk and should be shielding | |
| Good information from staff | 3 | Luckily our key workers and Leeds Children's Hospital have given more specific advice appropriate for children with working parents | |
| Feel need to seek info from other sources | 2 | Constantly researching the internet looking for case studies for reassurance | |
| Health care provision | Concern over strained hospital facilities, suboptimal treatment and care, and relapses might be missed | 14 | His next scan is likely to be cancelled so this is causing concern ‐ he has a high‐grade tumour which could return quickly so we are worried we could miss a recurrence |
| More support required | 6 | Would have preferred some more reassurance and advice from the primary care centre/oncologist as we mainly relied on watching government press conferences | |
| New ways of working in the hospital | 7 | Previously, for his chemo appointments, there's a dedicated entrance but now the hospital makes everyone enter through the main entrance which gives an increased possibility in coming into possible coronavirus patients | |
| I understand infection control and some things have to be done but telling us that both parents can be present for 1st chemo session, then that night being informed that wasn't the case and I would have to come alone was quite difficult | |||
| Priority of COVID‐19 over cancer care | 2 | Feel the virus takes priority over everything and we have been left without the same support we had prior to the virus | |
| Fears and anxieties | General expressions of fear | 6 | I think for me it is genuinely the unknown |
| Concern over ability to look after child if parent ill or dies | 5 | I am asthmatic and also fear that if I were to get it I couldn't care for her | |
| Concern child or parent will die | 4 | What if me and my husband get it and one of us dies, that can't happen | |
| Things could be worse | 3 | On the flip side, we are relishing this time together as a family and so grateful that we are not in the middle of treatment and needing to go to the hospital | |
| Separation if child becomes ill from rest of family | 3 | I worry that if he catches it I'll have to be in hospital with him away from my other children | |
| Child has had/possibly had COVID‐19 | 2 | My child has had the virus and it was very mild symptoms. I was very worried about him catching it and thought it would have a bad effect on him but it was very mild | |
| LOCKDOWN AND ISOLATION | |||
| Psychological and social impact | Psychological impact on child and family, missing out on life, boredom | 14 | The isolation has been quite triggering for him, he is bringing up emotions and questions from when he was on treatment. An additional worry, another thing to keep life from being normal |
| It has restricted any chance of normality during last months of my son's life. We know we only have months, have accepted that, but now we are unable to do the basic things, like go out for coffee, visit grandparents, simple things that bring him pleasure | |||
| Parental coping (struggles, strategies used) | 13 | Panic of not being in control again. As a single parent, it is tough. I need more support from family and friends, that I normally have, but cannot. Feels incredibly lonely | |
| Delayed resumption of normality after treatment | 9 | We were already isolated from August 19 but we were starting to look forward to that relaxing a bit in the next few months. That has made my daughter really sad | |
| Parallel with cancer treatment isolation | 7 | As a family we are coping well as isolation is not unusual due to cancer treatment | |
| Missing family and friends | 5 | It's been hard not seeing family and friends though, this is what has pulled us through our difficult journey and my son is too young to understand why he can only see his grandparents through a window | |
| Impractical nature of social distancing | 4 | We could not adhere to the ridiculous guidelines set out in the letter of keeping a 2 m distance from our young children… caused a lot of stress for families on top of our usual daily stresses | |
| Social and educational development | 3 | Worry of his social skills being reduced and the long‐term impact on him | |
| Missing emotional support for parents from friends and family | 3 | The virus has taken away my comfort blanket if I feel anxious, I don't have that physical access to family and friends that we did at diagnosis | |
| Use of technology to keep in touch | 3 | We are using technology to keep in touch with friends and family as that is the hardest bit | |
| Separation from partners/parents/children | 4 | My husband's work will also not furlough him due to him being a key worker so he has had to move out into the garage for the 12 weeks | |
| Keeping safe under lockdown | Concern over societal compliance in social distancing in society and delayed lockdown | 10 | I was very worried starting in January that nothing was being done to protect our children especially as it is a brand new disease and nobody knows enough about it |
| Being on lockdown keeps child safe | 6 | In some ways because society have restrictions it makes it easier | |
| Concern once restrictions are lifted/adjustment concerns | 3 | I worry about re‐interacting with society | |
| Provisions and dependence | Difficulty securing provisions (food, cleaning, medication) | 13 | The hardest with everything is probably the food shopping. We have bought our food online since diagnosis a year ago as we wanted to avoid the shops and now we can't get any delivery slots |
| Lack of priority status | 4 | One of us is having to go shopping as we are not able to access online shopping as the vulnerable status is in the child's name | |
| Reliance on friends and family to pick up provisions | 4 | Having to rely on others for everything is quite patronising | |
| Employment and income | 10 | Worry about finances as both my husband and I have decided to stay home to shield her | |
FIGURE 2.
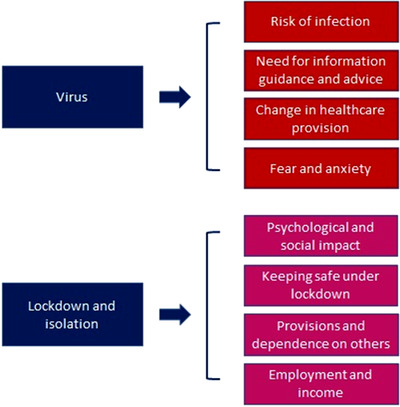
Overarching themes of open text boxes
4.4.1. Virus
The largest number of comments from parents (n = 44) related to the compromised immune system of their children and their perceived greater susceptibility to the virus. The second largest number of comments (n = 22) described safety concerns relating to hospital visits either for outpatient appointments or overnight stays.
Safety of the home environment was felt to be compromised by the virus being brought in by family members who were engaged in a designated ‘essential occupation’ (known as keyworkers in the UK), visiting (community) health professionals or visits to the hospital.
Concerns relating to limited or unclear information from both the hospital and the government were voiced by 17 parents.
Another strong theme (n = 14) involved a concern amongst parents that the response to the COVID‐19 situation would lead to suboptimal cancer care or had already led to postponed or cancelled clinic appointments, and several parents were concerned that relapses would be missed.
Parents described feeling ‘scared’, ‘terrified’ or ‘petrified’ of the risk of their child becoming infected.
4.4.2. Lockdown and isolation
Parents described the psychological impact (n = 14) of the emergence of the virus and subsequent lockdown and classification of the child as ‘shielded’, for both themselves and their children. They described their children struggling mentally, and missing out on life, particularly for those with a limited life expectancy. For parents with children who had recently completed treatment, the lockdown brought with it several frustrations relating to delayed resumption of normality. Parents also described difficulties in coping with the uncertainty of the situation, lack of control, and limited support mechanisms in place, which was particularly true for lone parents. Some parents described strategies for coping with the stressful situation, such as the avoidance of or restricted access to news broadcasts and social media.
While under lockdown, parents (n = 10) were also concerned about the lack of respect for social distancing shown by some members of the public, the delayed response by the government, and some (n = 3) expressed concern about how things might change when restrictions are relaxed.
Concerns were identified over access to food home delivery for families with a child classified as ‘shielded’ and lack of recognition of parents as needing priority status (rather than just the child) (n = 13).
Financial and employment concerns were also expressed (n = 10): parents described having to give up paid work to ‘shield’ their child. In addition, parents expressed frustration in terms of not being eligible for furlough (the government's Coronavirus Job Retention Scheme, which allowed employers to continue paying wages via a government subsidy).
4.5. ‘Information’ free text response
18 parents wanted more information, specifically (n = 4) in relation to safety of hospitals, information tailored to children with cancer rather than to adults, information relevant to children with rare cancers and those off treatment, and their child's level of risk of catching the virus given their particular situation (on or off treatment) or diagnosis.
For the majority of parents (n = 89), charities provided them with information regarding the virus, followed by clinical staff (n = 50) and news outlets (n = 41).
4.6. ‘Support’ free text response
Ninety‐nine parents described a need for additional support related to the provision of more information, specifically more guidance or support from the hospital. The need for information and reassurance surrounding the safety of the hospital environment including the availability and use of PPE as well as testing of staff was further reinforced by 22 parents. In addition, four parents proposed remote contact with hospital staff and services delivered within the community as an option to protect their child.
4.7. ‘Decisions’ free text response
Parents were more likely (n = 44) to turn to clinical staff when making decisions about their child's care, while 35 parents described relying on their own judgements based on their knowledge of their child and past experience, and six were also led by their child when making decisions.
4.8. ‘Other’ free text response
4.8.1. Positive
Some parents (n = 5) highlighted the positives of the lockdown in terms of bringing the family together and the social restrictions making them ‘feel safe at home’, providing them with a ‘protective bubble’. Some parents (n = 3) suggested that things could be worse or drew comparisons between the isolation imposed during cancer treatment and that of the virus and that they were better equipped than most to face the challenges. In addition, 12 parents took the opportunity to use the survey to communicate their gratitude to the hospital and charities for the care and support they had received.
5. DISCUSSION
This is the first study to report experiences of parents of a child with cancer during the SARS‐CoV‐2/COVID‐19 pandemic in the UK. The study has found that the majority of parents were worried about SARS‐CoV‐2, worried about their own health if they are infected, and worried about transmitting the virus to their child. They described vigilance about SARS‐CoV‐2 symptoms and cancer‐related symptoms, and, for a lot of parents, the hospital was no longer a safe place during the first month of the lockdown. The qualitative findings show that the threat of SARS‐CoV‐2 led to concerns about getting infected and therefore to a fear of the hospital and health care teams visiting the family at home. Parents received information from their medical team, and almost all parents looked at social media for information, which, for some, led to feeling anxious. Parents wanted clear information and guidance, which included the shielding policy in the UK. Changes in health care provision led some parents to think their care would be suboptimal, that care for COVID‐19 patients was prioritised over that of cancer patients, and that the health service was strained. Parents were anxious about the unknown, and about who would look after their child if they themselves became ill (or died). Remarkably, only around one quarter of parents expressed a wish for additional support, and some described how their experience with cancer treatment has made them better prepared for ‘lockdown’ than those without this background.
The lockdown and imposed isolation by the UK government led to parents worrying about the psychological impact in terms of children missing out, feeling bored, missing family and friends, as well as worrying about a delay in social and emotional development, mirroring evidence from studies focusing on young people's mental health during the pandemic. 23 , 24 , 25 Parents missed their support network, even though technology is available to help them connect with others. The designation of children as requiring ‘shielding’ provided particular challenges; the English Government advice described attempting to maintain complete isolation from all other people, even those living in the same household. This lack of age‐related nuance may have increased the level of anxiety for some families, particularly around food shopping. Parents struggled going out to grocery stores, as they did not want to expose themselves to the risk of getting the virus (and thus increasing the chances of the child becoming infected). In common with many people during the lockdown, parents were worried about employment and money; the study group of parents described the additional concern of transmitting the virus to their child.
Uncertainty and lack of clarity in communication were strong themes in the parents’ responses. A clearer, more open, and reasoned account of the various measures being planned and implemented may have assisted with reducing this distress. Much of the uncertainty arose from the true lack of knowledge about the effect of SARS‐CoV‐2, but few participants reflected this. The all‐age signalling of government guidelines placed families in an invidious position—to apparently defy the government guideline and risk adversely affecting their child through infection, or to follow the guidelines strictly and adversely affect their child with restriction on activity and reduce family contact to only one parent, and exclude any other parent or siblings. 26
Limitations of the study relate to the bias in the sample—although strenuous efforts were made to widely circulate the survey across children's cancer‐interested social media, the respondents may not be representative of the whole population. The responses were mostly from mothers (86%), and the largest group of patients had ALL (46%). While this is disproportionate compared to the diagnoses made in the UK (where it accounts for around one quarter of malignancies), ALL is also treated for 2‐3 years, in comparison with the shorter time frame (under 9 months) of most other treatment trajectories. No differences were noted between diagnostic groupings, but the low proportion of those with CNS tumours may mean this study has failed to clearly capture their unique concerns. The high proportion of mothers responding is in keeping with surveys about children, 27 as well as the observation mothers being the primary caregiver for the vast majority of children. In addition, parents responding to the survey could have self‐selected to represent those parents who were most concerned. Finally, subgroup analyses findings may be based on chance given the number of analyses carried out (n = 23 × 3) and the number of group differences (n = 3).
The information emerging from this survey was immediately placed into practice, shaping information delivery during this early phase of the pandemic. The data on concern about the safety of hospitals, along with reports of reduced attendances in paediatric emergency care facilities 13 led the charities involved in the research along with local health providers and national paediatric bodies to promote the message of hospitals being ‘safe to attend’. Worries about the possible reduction in anticancer therapy were addressed with information coproduced by parents and medical professionals and disseminated through the same routes, explaining the process of contingency planning and the routes to these planned recommendations. The most marked change in care provision was the move to more remote/virtual follow‐up appointments, and delay or omission of planned surveillance imaging for patients off treatment. Such imaging studies have rarely been shown to have significant survival advantage but contain great emotional weight. 28
We believe this study demonstrates how the views and experiences of a classically ‘vulnerable’ population can be captured by using existing research networks, an agile governance response, and inclusion of patient partners from the commencement of the study. We found high levels of concern about the consequences of SARS‐CoV‐2 infection in children with cancer and the consequences of presumed preventative interventions to the children and their families. We hypothesise that true uncertainty, coarse recommendations, and a lack of clarity behind decision‐making process in national administrations may have accentuated these experiences.
As the pandemic continues, survey studies such as this will be important in understanding the ongoing experience of families, and tuning support and information to their changing needs. They may allow us to understand if our response to the families’ concerns, which include providing trustworthy information highlighting the limits of our understanding and the current evolution of knowledge, has helped alleviate worries. Future research assessing modes of responding to uncertainty and delivering changing information to a special population is still required, along with comparative work with other chronic or life‐threatening conditions in children.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
We would like to thank all the parents who contributed their time and experiences to this study.
Darlington A‐SE, Morgan JE, Wagland R, et al. COVID‐19 and children with cancer: Parents’ experiences, anxieties and support needs. Pediatr Blood Cancer. 2021;68:e28790. 10.1002/pbc.28790
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Children's Cancer and Leukaemia Group . https://www.cclg.org.uk/Coronavirus-advice. Accessed July 1, 2020.
- 2. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pathak EB, Salemi JL, Sobers N, Menard J, Hambleton IR. COVID‐19 in children in the United States: intensive care admissions, estimated total infected, and projected numbers of severe pediatric cases in 2020. J Public Health Manag Pract. 2020;26:325‐333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kotecha RS. Challenges posed by COVID‐19 to children with cancer. Lancet. 2020;5:e235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Minotti C, Tirelli F, Barbieri E, Giaquinto C, Donà D. How is immunosuppressive status affecting children and adults in SARS‐CoV‐2 infection? A systematic review. J Infect. 2020;81(1):e61‐e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hrusak O, Kalina T, Wolf J, et al. Flash survey on severe acute respiratory syndrome coronavirus‐2 infections in paediatric patients on anticancer treatment. Eur J Cancer. 2020;132:11‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sung L, Feldman BM, Schwamborn G, et al. Inpatient versus outpatient management of low‐risk pediatric febrile neutropenia: measuring parents' and healthcare professionals' preferences. J Clin Oncol. 2004;22:3922‐3929. [DOI] [PubMed] [Google Scholar]
- 8. Paediatric Intensive Care Society . https://picsociety.uk/wp-content/uploads/2020/04/PICS-statement-re-novel-KD-C19-presentation-v2-27042020.pdf. Accessed July 1, 2020.
- 9. Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS‐CoV‐2. JAMA. 2020;324(3):259‐269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Reyna VF, Nelson WL, Han PK, Pignone MP. Decision making and cancer. Am Psychol. 2015;70:105‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rimer BK, Briss PA, Zeller PK, Chan ECY, Woolf SH. Informed decision making: what is its role in cancer screening? Cancer. 2004;101(5 Suppl):1214‐1228. [DOI] [PubMed] [Google Scholar]
- 12. Peters E, Klein W, Kaufman A, Meilleur L, Dixon A. More is not always better: intuitions about effective public policy can lead to unintended consequences. Soc Issues Policy Rev. 2013;7:114‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID‐19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. [DOI] [PubMed] [Google Scholar]
- 14. Hill R. What sample is ‘enough’ in internet survey. IPCT‐J. 1998;6. [Google Scholar]
- 15. Gay LR, Diehl PL. Research Methods for Business and Management. New York: Macmillan; 1992. [Google Scholar]
- 16. Safdar N, Abbo LM, Knobloch MJ, Seo SK. Research methods in healthcare epidemiology: survey and qualitative research. Infect Control Hosp Epidemiol. 2016;37:1272‐1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Robertson EG, Wakefield CE, Shaw J, et al. Decision‐making in childhood cancer: parents' and adolescents' views and perceptions. Support Care Cancer. 2019;27:4331‐4340. [DOI] [PubMed] [Google Scholar]
- 18. Morgan JE, Cleminson J, Stewart LA, Phillips RS, Atkin K. Meta‐ethnography of experiences of early discharge, with a focus on paediatric febrile neutropenia. Support Care Cancer. 2018;26:1039‐1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morgan JE, Phillips B, Stewart LA, Atkin K. Quest for certainty regarding early discharge in paediatric low‐risk febrile neutropenia: a multicentre qualitative focus group discussion study involving patients, parents and healthcare professionals in the UK. BMJ Open. 2018;8:e020324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. IBM Corp . IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 21. Mason J. Qualitative Researching. SAGE Publications; 2002. [Google Scholar]
- 22. Wagland R, Bracher M, Drosdowsky A, et al. Differences in experiences of care between patients diagnosed with metastatic cancer of known and unknown primaries: mixed‐method findings from the 2013 cancer patient experience survey in England. BMJ Open. 2017;7:e017881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID‐19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Saurabh K, Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid‐19 pandemic. Indian J Pediatr. 2020;29:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clerici CA, Massimino M, Ferrari A. On the clinical psychologist's role in the time of COVID‐19, with particular reference to experience gained in pediatric oncology. Psychooncology. 2020;29(9):1374‐1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. https://www.itv.com/news/2020-05-06/four-year-old-with-cancer-reunited-with-father-after-seven-weeks-kept-apart-in-lockdown/. Accessed July 1, 2020.
- 27. Phares V, Lopez E, Fields S, Kamboukos D, Duhig AM. Are fathers involved in pediatric psychology research and treatment? J Pediatr Psychol. 2005;30:631‐643. [DOI] [PubMed] [Google Scholar]
- 28. Morgan JE, Walker R, Harden M, Phillips RS. A systematic review of evidence for and against routine surveillance imaging after completing treatment for childhood extracranial solid tumors. Cancer Med. 2020;9(14):4949‐4961. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


