Summary
Currently severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) transmission has been on the rise worldwide. Predicting outcome in COVID‐19 remains challenging, and the search for more robust predictors continues. We made a systematic meta‐analysis on the current literature from 1 January 2020 to 15 August 2020 that independently evaluated 32 circulatory immunological signatures that were compared between patients with different disease severity was made. Their roles as predictors of disease severity were determined as well. A total of 149 distinct studies that evaluated ten cytokines, four antibodies, four T cells, B cells, NK cells, neutrophils, monocytes, eosinophils and basophils were included. Compared with the non‐severe patients of COVID‐19, serum levels of Interleukins (IL)‐2, IL‐2R, IL‐4, IL‐6, IL‐8, IL‐10 and tumor necrosis factor α were significantly up‐regulated in severe patients, with the largest inter‐group differences observed for IL‐6 and IL‐10. In contrast, IL‐5, IL‐1β and Interferon (IFN)‐γ did not show significant inter‐group difference. Four mediators of T cells count, including CD3+ T, CD4+ T, CD8+ T, CD4+CD25+CD127‐ Treg, together with CD19+ B cells count and CD16+CD56+ NK cells were all consistently and significantly depressed in severe group than in non‐severe group. SARS‐CoV‐2 specific IgA and IgG antibodies were significantly higher in severe group than in non‐severe group, while IgM antibody in the severe patients was slightly lower than those in the non‐severe patients, and IgE antibody showed no significant inter‐group differences. The combination of cytokines, especially IL‐6 and IL‐10, and T cell related immune signatures can be used as robust biomarkers to predict disease severity following SARS‐CoV‐2 infection.
Keywords: antibody, COVID‐19, cytokines, disease severity, innate immunity, meta‐analysis
Abbreviations
- ARDS
acute respiratory distress syndrome
- CLIA
chemiluminescence immunoassay
- COVID‐19
coronavirus disease 2019
- CSS
Churg–Strauss syndrome
- DCs
dendritic cells
- ELISA
enzyme‐linked immunosorbent assay
- ICU
intensive care unit
- IFN
interferon
- Ig
immunoglobulin
- IL
interleukins
- IQR
interquartile range
- MERS
Middle East respiratory syndrome
- MMFI
multiple microsphere flow immunofluorescence
- NK cell
natural killer cell
- NOQAS
Newcastle–Ottawa Quality Assessment Scale
- PD
programmed cell death protein
- PD‐L
programmed cell death protein ligand
- PRISMA
preferred reporting items for systematic reviews and meta‐analyses statement
- SARS
severe acute respiratory syndrome
- SD
standard deviation
- SMD
standardized mean difference
- TNF‐α
tumour necrosis factor‐α
1. INTRODUCTION
Currently, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) transmission has been on the rise in the worldwide range, with more than 32,000,000 cases and more than 990,000 deaths documented to 28 September 2020. Intensive efforts have been put forward to study the clinical process and outcome of the disease. 1 Predicting outcome in coronavirus disease 19 (COVID‐19) remains challenging, and the search for more robust methods continues. A broad range of signs and symptoms have been investigated in COVID‐19 to predict the disease outcome, while showing divergent results.2, 3, 4, 5, 6 Inclusion more specific biomarkers is urgently needed to develop a robust algorithm. Previous studies have suggested that lymphocytopenia and inflammatory cytokine storm are typical abnormalities in infections caused by highly pathogenic coronavirus, such as SARS and MERS.7, 8 Similarly, numerous studies on COVID‐19 patients have reported a decrease in peripheral blood lymphocyte count and an increase in serum inflammatory cytokines,9, 10, 11, 12 which is suggested that the inflammatory factors may be the main reason for adverse progression and poor treatment response in COVID‐19, but mostly proposed from small sample studies. 13 If these biomarkers are validated in a large patient cohort, their incorporation into algorithms might prove sufficiently sensitive and specific to be clinically useful, particularly when they can be related to the disease outcome.
In the current study, we attempted to address these issues by conducting a systematic meta‐analysis using the pooled data for the immune indicators that were evaluated at early disease and among patients with various disease severity. The inclusion of various studies allowed more statistical power for a holistic view of SARS‐CoV‐2‐induced immune mediators among patients with different disease severity, and across various geographic locations. This will also help to identify the immune signatures that better distinguish the development of COVID‐19 outcome.
2. MATERIALS AND METHODS
2.1. Protocol registration
This systematic review was not registered. The format of the review used the preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) (Table S1), and addressed the following question: ‘Are the immune mediators different in severe and non‐severe groups of COVID‐19 patients?’ according to PICOS (P—Patient, Problem or Population; I—Intervention; C—Comparison, control or comparator; O—Outcome; S—Study design) (Table S2).
2.2. Search strategy and study selection
We performed a comprehensive systematic review and meta‐analysis to identify the associations of immune cells, cytokines and the severity of COVID‐19. Identification of relevant existing literature was performed by an online search in PubMed, Web of Science and EMBASE, for studies published from 1 January 2020 to 15 August 2020. The MESH headings (keywords) searched were ‘nCoV’ or ‘coronavirus’ or ‘SARS‐CoV‐2’ or ‘COVID’ and ‘cytokine’ or ‘immunological or ‘immunity’ or ‘Cellular immunity’ or ‘T cell’ or ‘B cell’ or ‘NK cell’ or ‘antibody’. In addition, the same search strategy was applied to the database of bioRxiv and medRxiv for the unpublished studies (Table S3). Two reviewers (TY and XFP) independently screened the list of titles and abstracts, and the full text of chosen manuscripts related the immune mediators. Disagreements on which manuscripts to include during both title and abstract screen, and the subsequent full‐text analysis, were discussed until a conclusion was reached with two other reviewers (SML and KL).
2.3. Inclusion and exclusion criteria
All studies evaluating individual measurement of immunological indicators in predicting severe infection (as measured by disease severity criteria, or ICU admission or fatal/survived) were included. All studies of any design, from any time since the outbreak started were eligible. To avoid selection bias, no subjective quality criteria were applied to the studies for inclusion. The immunological signatures that were measured at the acute phase of infection were used, and if there was more than one evaluation for the same patient, only the first test results were used. Only those immune signatures investigated in at least three papers were used in the subsequent analysis. Exclusion criteria included the following: (1) Case reports of individual patients, literature reviews, nonhuman studies, editorials, comments, expert opinions or articles with number of patients ≤10; (2) Studies of exclusively paediatric or pregnant patients, due to the varying presentation of the disease in these groups and (3) Studies without adequate baseline information, such as age, sex or geographic region.
2.4. Data extraction
All the search results were evaluated according to the PRISMA statement. 14 From each study, various details including the baseline information of study population (age, sex, interval from disease onset to hospitalization, intervals from disease onset to the sample collection, study areas), the number of patients in each study group, the measured immunological indicators and their test methods and the definitions used to measure outcome, were extracted into Microsoft Excel. These details are presented in Table 1. The Newcastle‐Ottawa Quality Assessment Scale (NOQAS) was used to assess the quality of the studies included in the meta‐analysis and performed by two reviewers (TY and XFP) with a third reviewer (SML) consulted in case of discrepancy.
TABLE 1.
Characteristics of the association studies included in the meta‐analysis
| Author | Publish date | Country | Journal | Detection method | Patients group | Sample size | Mean ± SD or IQR | ||
|---|---|---|---|---|---|---|---|---|---|
| Severe | No‐severe | Severe | No‐severe | ||||||
| IL‐2 (unit: ng/L) | |||||||||
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 9.48 ± 4.87 | 6.7 ± 4.42 |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 2.69 ± 0.14 | 2.51 ± 0.16 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 4.2 (4.0–4.4) | 3.8 (3.6–4.3)/3.7 (3.5–4.0) |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 5.12 ± 1.64 | 4.47 ± 0.29 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 1 (0.8–1.9) | 1 (0.7–2.0) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.52 (0.33–0.66) | 0.36 (0.22–1.23) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐sever | 69 | 135 | 4.06 (3.28–4.09) | 3.55 (3.38–3.65) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 2.8 ± 0.7 | 9 ± 53.4 |
| 2.9 ± 0.9 | |||||||||
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 0.90 (0.47–1.60) | 0.93 (0.55–1.73) |
| IL‐2R (unit: ng/L) | |||||||||
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 902 ± 51/1185 ± 80 | 631 ± 37 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 1209.33 ± 421.86 | 448.97 ± 186.35 |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 1189.0 (901.0–1781.0) | 566.5 (448.0–858.3) |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 1166.5 (898.8–1788.5)/1076.5 (671.8–1699.5) | 571.5 (353.0–821.8)/454.5 (270.3–563.0) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 757 (528.5–1136.3) | 663.5 (473.3–862.8) |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 46 | 1451 (879–2768) | 579 (429–1432) | |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 5.00 (5.00–25.88) | 5.00 (5.00–5.00) |
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 766 (595–1050) | 546 (455–743) |
| 1026 (378–1260) | |||||||||
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 833.33 ± 620.21 | 666.77 ± 334.12 |
| 250.23 ± 750.12 | |||||||||
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 2 | 27 | 1729.50 (1277.25–2181.75) | 529.00 (385.00–754.50) |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 1098 (721–1512) | 716 (458–954) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 905.08 ± 441.45 | 787.88 ± 313.40 | |
| 1077.16 ± 551.21 | |||||||||
| IL‐4 (unit: ng/L) | |||||||||
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 3.49 ± 1.27 | 2.90 ± 1.28 |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 2.02 ± 0.10 | 1.88 ± 0.24 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 4.5 (4.1–4.8) | 4.2 (3.8–4.9)/4.1 (3.8–4.6) |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 1.42 ± 0.27 | 1.47 ± 0.2 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 1.8 (1.4–1.8) | 1.8 (1.2–1.8) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 21 | 102 | 1.83 ± 0.1849 | 1.69 ± 0.07049 |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.11 (0.00–0.42) | 0.24 (0.10–0.48) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 4.30 (4.01–4.60) | 3.75 (3.70–3.85) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 2.3 ± 0.8 | 2.6 ± 1 |
| 8.4 ± 20 | |||||||||
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 3.25 ± 0.81 | 1.49 ± 0.22 |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 1.99 (1.26–2.73) | 1.87 (1.43–2.55) |
| IL‐6 (unit: ng/L) | |||||||||
| Cai et al. 36 | 2020/4/2 | China | Allergy | – | Severe/no‐severe | 58 | 240 | 38.8 (22.7–57.2) | 12 (6.4–19.7) |
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 52 ± 11/108 ± 12 | 34 ± 7 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 72.39 ± 71.64 | 18.66 ± 15.80 |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 72.0 (35.6–146.8) | 13.0 (4.0–26.2) |
| Gao et al. 37 | 2020/4/10 | China | J Med Virol | Severe/no‐severe | 15 | 28 | 36.1 (23–59.2) | 10.6 (5.13–24.18) | |
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 29.42 ± 41.34 | 12.47 ± 22.05 |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 48.4 (12.6–154.1)/65.1 (11.3–154.1) | 4.2 (1.9–16.4)/3.3 (1.4–16.7) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 36.52 ± 5.54 | 2.61 ± 0.65 |
| Mo et al. 38 | 2020/3/16 | China | Clin Infect Dis | – | Severe/no‐severe | 85 | 70 | 64 (31–165) | 23 (9–57) |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 9.93 (8.58–11.92) | 5.78 (5.10–7.19)/6.03 (5.39–7.93) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 25.2 (9.5–54.5) | 13.3 (3.9–41.1) |
| Ruan et al. 39 | 2020/3/3 | China | Intensive Care Med | – | Death/no‐death | 68 | 82 | 13.47 ± 15.89 | 6.78 ± 8.78 |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 445.83 ± 204.85 | 312.61 ± 24.27 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 24.2 (11.6–47.0) | 21.6 (8.7–57.2) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 18 | 45 | 37.77 ± 7.801 | 13.41 ± 1.84 |
| Wu et al. 9 | 2020/3/13 | China | JAMA Intern Med | – | ARDS/no‐ARDS | 84 | 117 | 7.39 (5.63–10.89) | 6.29 (5.36–7.83) |
| Xiao et al. 40 | 2020/2/27 | China | Acta Acad Med Mil Tert | – | Severe/no‐severe | 36 | 107 | 15.29 ± 4.54/28.06 ± 8.38 | 6.21 ± 1.04 |
| Xu et al. 41 | 2020/3/8 | China | medRxiv | – | Severe/no‐severe | 25 | 44 | 14.8 (7.5–45.3) | 5.9 (2.8–10.9) |
| Zheng et al. 42 | 2020/3/17 | China | Cellular & Molecular Immunology | – | Severe/no‐severe | 6 | 10 | 28.3 ± 22.64 | 50.94 ± 31.13 |
| Zhou et al. 43 | 2020/3/9 | China | Lancet | – | Death/no‐death | 54 | 137 | 11 (7.5–14.4) | 6.3 (5.0–7.9) |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 46 | 29.1 (2–89.3) | 7.1 (2.79–25.7) | |
| Sun et al. 44 | 2020/5/8 | China | J Am Geriatr Soc | – | Death/no‐death | 121 | 123 | 75.2 (35.2–162.9) | 12.7 (3.3–41.5) |
| Fan et al. 45 | 2020/4/19 | China | Metabolism | Death/no‐death | 4 | 15 | 195 (127–280) | 12 (4–18) | |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 18.15 (5.91–49.24) | 2.21 (0.83–13.22) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 57.33 ± 111.5/116.47 ± 141.9 | 24.69 ± 39.72 | |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 154.55 ± 315.11 | 9.21 ± 10.12 |
| Dong et al. 46 | 2020/5/29 | China | Transbound Emerg Dis | – | Severe/no‐severe | 53 | 94 | 21.85 (11.77–38.68) | 8.54 (3.52–17.29) |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 33.22 ± 31.90/34.09 ± 26.47 | 5.26 ± 1.25/14.17 ± 11.37 |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 22.88 (18.90–27.76) | 9.50 (1.79–18.09) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 14.3 (7.8–11.6) | 14.0 (7.2–15.3) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | CLIA | Severe/no‐severe | 26 | 43 | 24.6 (17.9–45.0) | 8.4 (5.7–15.9) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 150.7 ± 449.2 | 64.6 ± 137.7 |
| 57.4 ± 105.6 | |||||||||
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 27.1 (11.8–60.0) | 13.2 (3.8–23.1) |
| 32.8 (17.8–62.6) | |||||||||
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 16.9 ± 25.32 | 67.71 ± 56.33 |
| 25.35 ± 33.15 | |||||||||
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 44.51 ± 12.45 | 7.06 ± 3.55 |
| Burian et al. 49 | 2020/5/18 | Germany | J Clin Med | – | ICU/no‐ICU | 12 | 25 | 103.9 ± 43.6 | 51.7 ± 65.6 |
| Gayam et al. 50 | 2020/7/16 | USA | J Med Virol | – | Death/no‐death | 132 | 276 | 84.5 (53.3–205) | 53.1 (23.9–97.4) |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 43.8 (20.1–62.6) | 3.9 (2.2–9.6) |
| Xu et al. 52 | 2020/6/13 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 30 | 125 | 75.85 ± 37.64 | 19.16 ± 10.53 |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 4 | 27 | 22.88 (18.90–27.76) | 9.50 (1.79–18.09) |
| Xie et al. 53 | 2020/6/13 | China | Circ J | – | Severe/no‐severe | 24 | 38 | 14.1 (4.3–26.7) | 5.0 (4.3–8.2) |
| 17.5 (8.4–27.9) | 6.7 (4.2–9.3) | ||||||||
| Morrison et al. 54 | 2020/7/3 | USA | J Autoimmun | – | Death/no‐death | 16 | 22 | 47.5 (15.5–82) | 12 (5–32) |
| Wang et al. 55 | 2020/3/24 | China | Int J Infect Dis | – | Severe/no‐severe | 25 | 100 | 39.80 (23.75–60.6) | 16.80 (5.55–29.7) |
| Zheng et al. 56 | 2020/3/27 | China | Int J Infect Dis | – | Severe/no‐severe | 21 | 34 | 64.3 (3.8–439) | 27.6 (3.6–280) |
| Wang et al. 57 | 2020/3/15 | China | J Infect | – | Death/no‐death | 65 | 274 | 93.8 (35.9–182.3) | 10.5 (4.9–18.8) |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 61.1 (29.9–132.2) | 10.8 (2.7–37.4) |
| Chen et al. 58 | 2020/4/17 | China | Clin Infect Dis | – | Severe/no‐severe | 27 | 21 | 5.8 (3.1–16.9) | 10.4 (3.8–31.0) |
| 64.0 (25.6–111.9) | |||||||||
| Liu et al. 59 | 2020/7/31 | China | Ann Intensive Care | – | Death/no‐death | 157 | 1033 | 31.9 (11.1–1487.0) | 13.2 (7.7–366.2) |
| Arunachalam et al. 60 | 2020/8/11 | China and USA | Science | Flow cytometry | Severe/no‐severe | 18 | 4 | 41.89 ± 68.33 | 9.87 ± 5.74 |
| Wei et al. 61 | 2020/4/16 | China | J Infect | – | Severe/no‐severe | 30 | 137 | 36.20 (16.25–59.90) | 15.40 (5.05–28.90) |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 24.11 (1.14–54.37) | 3.82 (2.19–9.87) |
| Shi et al. 62 | 2020/4/23 | China | medRxiv | – | Severe/no‐severe | 46 | 88 | 23.0 (7.2–49.7) | 5.7 (5.0–9.9) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 11.30 (4.34–28.43) | 14.60 (4.21–22.30) |
| 17.40 (7.18–50.20) | |||||||||
| Pereira et al. 64 | 2020/4/24 | USA | Am J Transplant | – | Severe/no‐severe | 27 | 41 | 32 (11–90) | 18 (5–45) |
| IL‐8 (unit: ng/L) | |||||||||
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 20 ± 16/30 ± 16 | 16 ± 11 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 61.62 ± 73.07 | 24.74 ± 26.86 |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 28.3 (18.7–72.1) | 11.4 (7.8–20.2) |
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 49.74 ± 76.59 | 18.19 ± 16.24 |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 22.0 (14.0–28.4)/27.6 (14.1–64.9) | 9.3 (6.4–18.6)/9.4 (5.7–15.9) |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 46 | 21.5 (5–125.6) | 8.66 (5.41–17.5) | |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 18.4 (11.3–28.4) | 13.7 (8.9–21) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 29.05 (14.35–56.75) | 9.40 (6.55–15.85) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | CLIA | Severe/no‐severe | 26 | 43 | 13.1 (11.4–15.9) | 7.8 (6.4–10.4) |
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 32.21 ± 34.88 | 29.78 ± 43.11 |
| 55.99 ± 78.34 | |||||||||
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 4 | 27 | 29.05 (14.35–56.75) | 9.40 (6.55–15.85) |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 28.3 (14.7–59.1) | 12.5 (6.9–20.8) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 32.58 ± 23.79 | 36.55 ± 54.97 | |
| 57.23 ± 61.01 | |||||||||
| IL‐10 (unit: ng/L) | |||||||||
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 11.0 ± 9.2/11.4 ± 2.6 | 8.0 ± 3.2 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 10.93 ± 2.10 | 6.67 ± 2.65 |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 12.8 (8.8–19.6) | 5.0 (5.0–8.4) |
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 19.38 ± 37.95 | 5.51 ± 4.31 |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 4.9 (4.0–10.0)/8.3 (4.9–17.0) | 4.9 (4.0–4.9)/4.9 (4.0–4.9) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 5.48 ± 0.48 | 3.06 ± 0.16 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 6.54 (5.96–7.44) | 4.93 (4.25–5.55)/4.78 (4.28–5.51) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 6.6 (5.0–11.3) | 5 (5.0–7.0) |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 25.43 ± 12.71 | 19.21 ± 1.89 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 6.7 (3.3–8.2) | 4.3 (3.0–8.1) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 21 | 102 | 4.59 ± 0.3777 | 2.464 ± 0.08506 |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 30.25 (15.57–67.13) | 24.79 (16.64–36.92) |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 46 | 7.32 (<5–11.23) | 5 (<5–5.87) | |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 5.23 (3.31–10.64) | 2.34 (1.16–4.41) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 10.16 ± 4.96 | 36.55 ± 54.97 | |
| 23.85 ± 26.57 | |||||||||
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 14.28 ± 16.92 | 4.52 ± 3.71 |
| Dong et al. 46 | 2020/5/29 | China | Transbound Emerg Dis | – | Severe/no‐severe | 53 | 94 | 4.50 (3.91–5.45) | 4.51 (3.48–6.23) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 22.00 (14.73–60.00) | 5.00 (5.00–7.90) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 4.3 ± 1.7 | 3.9 ± 1.8 |
| 5.6 ± 3.6 | |||||||||
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 7.25 (6.20–8.05) | 6.37 (5.71–6.67) |
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 6.4 (5.0–10.4) | 5.0 (5.0–8.1) |
| 8.0 (5.0–15.1) | |||||||||
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 7.28 ± 3.71 | 13.88 ± 12.95 |
| 9.18 ± 8.52 | |||||||||
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 7.45 ± 2.64 | 0.91 ± 0.7 |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 4 | 27 | 22.00 (14.73–60.00) | 5.00 (5.00–7.90) |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 10.5 (5.9–18.5) | 2.5 (2.5–7.0) |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 6.41 (3.24–11.02) | 3.13 (2.15–4.57) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 8.52 (4.90–15.80) | 5.00 (4.90–7.16) |
| 9.56 (5.14–14.80) | |||||||||
| TNF‐α (unit: ng/L) | |||||||||
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 10.8 ± 6.5/10.1 ± 1.5 | 8.3 ± 1.9 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 10.93 ± 3.30 | 7.56 ± 1.85 |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 11.8 (8.6–17.6) | 7.9 (6.7–9.6) |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 13.0 (8.3–23.3)/21.3 (13.2–28.9) | 7.3 (5.6–9.4)/5.7 (3.8–7.9) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 2.26 ± 0.15 | 2.11 ± 0.10 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 2.98 (2.76–3.41) | 2.85 (2.51–3.35)/2.89 (2.55–3.28) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 8.7 (7.1–11.6) | 8.4 (6.9–10.4) |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 1.23 ± 0.30 | 0.93 ± 0.20 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 12.2 (12.2–54.4) | 19.7 (2.5–67.5) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 21 | 102 | 2.948 ± 0.4432 | 4.077 ± 1.588 |
| Zheng et al. 42 | 2020/3/17 | China | Cellular & Molecular Immunology | – | Severe/no‐severe | 6 | 10 | 97.06 ± 30.88 | 202.94 ± 70.59 |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.1 (0.00–0.24) | 0.10 (0.10–0.26) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 10.16 ± 2.94 | 10.34 ± 3.12 | |
| 13.26 ± 14.02 | |||||||||
| Dong et al. 46 | 2020/5/29 | China | Transbound Emerg Dis | – | Severe/no‐severe | 53 | 94 | 2.07 (1.81–2.22) | 2.18 (1.93–2.35) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 23.00 (9.65–44.23) | 7.60 (5.65–9.00) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 2.98 (2.63–3.11) | 2.50 (2.44–2.73) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | CLIA | Severe/no‐severe | 26 | 43 | 7.4 (6.7–8.7) | 5.0 (4.8–6.08) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 5.5 ± 6.1 | 5.6 ± 6.6 |
| 3.2 ± 2 | |||||||||
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 9.3 (7.6–11.6) | 8.1 (6.8–9.8) |
| 9.3 (6.8–11.1) | |||||||||
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 10.41 ± 4.73 | 9.03 ± 4.11 |
| 4.48 ± 8.13 | |||||||||
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 1.74 ± 0.4 | 0.91 ± 0.49 |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 4 | 27 | 23.00 (9.65–44.23) | 7.60 (5.65–9.00) |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 10.7 (7.5–15.9) | 8.2 (6.1–10.2) |
| Arunachalam et al. 60 | 2020/8/11 | China and USA | Science | Flow cytometry | Severe/no‐severe | 18 | 4 | 7.11 ± 1.65 | 5.66 ± 2.94 |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 1.48 (1.39–1.74) | 1.35 (1.12–1.73) |
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 94.09 ± 20.40 | 72.01 ± 20.96 |
| IL‐5 (unit: ng/L) | |||||||||
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 13.61 ± 12.57 | 12.62 ± 12.75 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 2.22 (2.11–2.33) | 2.16 (2.07–2.22)/2.13 (2.05–2.18) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 2.27 (2.12–2.35) | 2.39 (2.30–3.05) |
| IL‐1β (unit: ng/L) | |||||||||
| Chen et al. 23 | 2020/2/4 | China | Chinese Medical Association | ELISA | Severe/no‐severe | 14 | 15 | 5.0 ± 1.1/6.2 ± 2.4 | 5.5 ± 1.9 |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | CLIA | Severe/no‐severe | 9 | 7 | 5.32 ± 0.96 | 5 ± 0.21 |
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 1.16 ± 0.54 | 1.40 ± 1.52 |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Death/no‐death | 26 | 108 | 4.5 (4.0–4.9)/4.9 (4.2–4.9) | 4.9 (4.0–4.9)/4.9 (4.7–4.9) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 5 (5.0–5.0) | 5 (5.0–5.0) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 4.90 (4.90–5.42)/4.90 (4.90–5.61) | 4.90 (4.90–5.21) |
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 1.65 ± 0.38 | 0.85 ± 0.14 |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | CLIA | Severe/no‐severe | 26 | 43 | 9.9 (6.0–18.3) | 7.5 (6.8–8.7) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 7 | 27 | 5.00 (5.00–25.88) | 5.00 (5.00–5.00) |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | – | Severe/no‐severe | 30 | 46 | 5.69 (<5–11.6) | 5 (<5–10.1) |
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | CLIA | Severe/no‐severe | 221 | 168 | 6.43 ± 3.01/10.71 ± 6.02 | 5.57 ± 2.13 |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 4 | 27 | 5 (5–25.88) | 5 (5–5) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | – | Severe/no‐severe | 35 | 30 | 6.48 ± 3.83/5.32 ± 0.63 | 6.11 ± 2.92 |
| IFN‐γ (unit: ng/L) | |||||||||
| Huang et al. 1 | 2020/1/24 | China | Lancet | – | ICU/no‐ICU | 13 | 28 | 16.062 ± 20.752 | 0.849 ± 5.472 |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry and ELISA | Severe/no‐severe | 69 | 11 | 2.49 ± 0.18 | 1.87 ± 0.09 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 3.99 (3.61–4.44) | 3.76 (3.53–4.19)/3.64 (3.38–4.07) |
| Shi et al. 17 | 2020/3/16 | China | medRxiv | – | Severe/no‐severe | 25 | 31 | 5.27 ± 1.91 | 4.9 ± 0.85 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 9 (5.7–24.3) | 12.2 (5.8–37.9) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 21 | 97 | 6.904 ± 1.247 | 5.132 ± 0.8413 |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 86.37 (47.01–255.91) | 80.06 (36.63–129.08) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.58 (0.11–1.69) | 0.66 (0.11–1.57) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 3.8 (3.8–3.93) | 3.93 (3.51–4.61) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | CLIA | Severe/no‐severe | 121 | 131 | 2.9 ± 4.5 | 2.5 ± 1.1 |
| 9.5 ± 24.7 | |||||||||
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 10 | 30 | 13.48 ± 4.84 | 0.87 ± 0.72 |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | Flow cytometry | Severe/no‐severe | 16 | 111 | 1.93 (1.25–2.29) | 1.24 (0.93–1.57) |
| IgA (unit: g/L) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 2.18 (1.84–3.68) | 2.38 (1.85–3.04) |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 2.4 (1.6–3.3) | 2.1 (1.6–2.8) |
| Han et al. 67 | 2020/3/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 3.08 ± 1.08 | 1.01 ± 0.64 |
| Liu et al. 68 | 2020/2/16 | China | EBioMedicine | – | Severe/no‐severe | 13 | 27 | 2.4 ± 0.6 | 2.2 ± 0.8 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 1.97 (1.55–2.41) | 1.90 (1.41–2.52) |
| 1.93 (1.30–2.39) | |||||||||
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 2.26 (1.57–2.89) | 2.14 (1.66–2.71) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | Death/no‐death | 14 | 71 | 3.30 (1.68–4.50) | 2.55 (1.81–3.01) | |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 2.10 (1.43–2.85) | 1.84 (1.45–2.44) | |
| IgG (unit: g/L) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 12.4 (10.9–13.8) | 11.8 (10.3–13.6) |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 12.3 (10.1–14.5) | 11.3 (9.3–13.0) |
| Han et al. 67 | 2020/3/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 12.50 (9.82–15.20) | 11.05 (9.34–12.53) |
| Liu et al. 68 | 2020/2/16 | China | EBioMedicine | – | Severe/no‐severe | 13 | 27 | 11.5 ± 2 | 10.8 ± 2 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 12 (10–14) | 12 (11–16)/13 (11–15) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 11.7 (9.53–13.8) | 11.85 (10.13–13.40) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | Death/no‐death | 14 | 71 | 12.20 (10.60–14.30) | 10.00 (11.70–13.40) | |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 13.4 (10.5–16.5) | 11.6 (9.9–13.8) | |
| IgM (unit: g/L) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 0.86 (0.68–0.99) | 0.96 (0.69–11.24) |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 1.0 (0.7–1.4) | 1.0 (0.7–1.4) |
| Han et al. 67 | 2020/3/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 1.01 ± 0.36 | 1.01 ± 0.44 |
| Liu et al. 68 | 2020/2/16 | China | medRxiv | – | Severe/no‐severe | 13 | 27 | 1.1 ± 0.3 | 1.1 ± 0.5 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 1.05 (0.74–1.52) | 1.16 (0.74–1.36)/1.20 (0.96–1.86) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 0.9 (0.69–1.28) | 1.02 (0.77–1.37) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | Death/no‐death | 14 | 71 | 0.93 (0.72–1.16) | 0.86 (0.67–1.09) | |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 0.94 (0.66–1.22) | 1.11 (0.86–1.38) | |
| IgE (unit: IU/mL) | |||||||||
| Han et al. 67 | 2020/3/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 36.00 (0.00–103.5) | 0.00 (0.00–33.98) |
| Liu et al. 68 | 2020/2/16 | China | EBioMedicine | – | Severe/no‐severe | 13 | 27 | 43.9 (27–105.5) | 26.5 (12.8–76.1) |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 28.0 (17.3–58.0) | 17.5 (17.3–98.2)/32.2 (17.3–65.0) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 30.85 (17.3–68.9) | 21.9 (17.3–84.3) | |
| CD3+T cells count (unit: cells/μL) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 411.0 (198.0–537.0) | 801.0 (561.5–1087.0) |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 294.0 (169.3–415.3) | 640.5 (588.3–789.5) |
| Diao et al. 70 | 2020/5/1 | China | Front Immunol | – | ICU/no‐ICU | 43 | 212 | 261 (157–457) | 652 (351–977) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 378.10 ± 142.33 | 973.46 ± 298.92 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 461.6 ± 264.7 | 663.8 ± 291.3 |
| Shi et al. 17 | 2020/3/12 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 19 | 738 ± 512.15 | 1073.38 ± 464.14 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 269.0 (158.0–410.0) | 504.5 (262.0–918.8) |
| Wu et al. 9 | 2020/3/13 | China | JAMA Intern Med | – | ARDS/no‐ARDS | 84 | 117 | 446.50 (231.00–633.75) | 633.00 (467.00–846.00) |
| Xu et al. 41 | 2020/3/8 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 44 | 306 (185–464) | 734 (445–1036) |
| Zeng et al. 71 | 2020/3/8 | China | medRxiv | Flow cytometry | ICU/no‐ICU | 65 | 113 | 503 ± 187 | 1056 ± 191 |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 530.25 ± 255.417 | 1245.105 ± 619.531 |
| Zheng et al.(b) 11 | 2020/3/19 | China | Cell Mol Immunol | – | Severe/no‐severe | 13 | 55 | 583.94 ± 328.97 | 857.66 ± 737.83 |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 427.86 ± 253.74 | 571.23 ± 270.10 | |
| 259.85 ± 155.97 | |||||||||
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 707.55 ± 538.45 | 1047.17 ± 481.21 |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 305 (198–525) | 1066 (804–1321) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 378 (258–576) | 991 (740–1154) |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 266.5 (173.8–579.8)/297.0 (139.0–433.0) | 706.0 (491.5–1004.5)/657.5 (431.0–1035.3) |
| Liu et al. 74 | 2020/5/13 | China | Clin Chim Acta | Flow cytometry | Severe/no‐severe | 105 | 49 | 358.15 (73.71–1019.43)/511.78 (120.54–1739.49) | 512.03 (118.69–1746.61) |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 522.57 ± 318.73/464.67 ± 339.68 | 1210.75 ± 408.81/808.97 ± 371.22 |
| Liu et al. 59 | 2020/7/31 | China | Ann Intensive Care | – | Death/no‐death | 157 | 1033 | 367 (267–409) | 647 (468–991) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 339.50 (217.50–524.25) | 609.00 (410.00–905.00) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 593.00 (412.00–725.00) | 894.50 (662.75–1192.00) |
| 287.50 (240.50–528.50) | |||||||||
| CD4+T cells count (unit: cells/μL) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 198.0 (116.0–340.0) | 468.0 (309.5–679.5) |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 177.5 (104.0–249.8) | 381.5 (255.0–451.0) |
| Diao et al. 70 | 2020/5/1 | China | Front Immunol | – | ICU/no‐ICU | 43 | 212 | 198 (100–279) | 342 (192–559) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 230.50 ± 86.68 | 610.15 ± 178.30 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 285.1 ± 168.0 | 420.5 ± 207.8 |
| Shi et al. 17 | 2020/3/12 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 19 | 384.72 ± 270.99 | 616.62 ± 294.09 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 139.0 (72.0–206.0) | 288.5 (142.5–504.0) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | – | Severe/no‐severe | 21 | 102 | 263.2 ± 28.83 | 451.3 ± 23 |
| Wu et al. 9 | 2020/3/13 | China | JAMA Intern Med | – | ARDS/no‐ARDS | 84 | 117 | 234.00 (136.75–398.00) | 371.00 (283.00–572.00) |
| Xu et al. 41 | 2020/3/8 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 44 | 201 (127–251) | 422 (244–593) |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 329 (200.25–438.5) | 559.5 (377–784) |
| Zeng et al. 71 | 2020/3/8 | China | medRxiv | Flow cytometry | ICU/no‐ICU | 65 | 113 | 290 ± 87 | 599 ± 163 |
| Zheng et al. 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 140.798 ± 336.375 | 416.618 ± 622.589 |
| Zhou et al. 75 | 2020/3/17 | China | Ann Palliat Med | Aggravation/no‐aggravation | 5 | 12 | 377.2 ± 229.6 | 698.2 ± 267.4 | |
| Fan et al. 45 | 2020/4/19 | China | Metabolism | Death/no‐death | 4 | 15 | 168 (108–250) | 416 (172–557) | |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 60 | 125 (60–107) | 462 (239–636) | |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 392.27 ± 267.42 | 612.83 ± 296.34 |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 257.86 ± 129.48/270.11 ± 162.75 | 689.38 ± 251.29/436.8 ± 225.08 |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 199 (128–325) | 544 (364–667) |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 130.5 (92.0–369.8)/130.0 (103.0–277.0) | 396.0 (293.0–599.0)/442.5 (264.5–676.0) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 184 (103–293) | 645 (461–794) |
| Yang et al. 76 | 2020/4/29 | China | J Allergy Clin Immunol | – | Severe/no‐severe | 36 | 14 | 377 (200.75–492.5)/246 (176–315.5) | 561 (367–826) |
| Liu et al. 74 | 2020/5/13 | China | Clin Chim Acta | Flow cytometry | Severe/no‐severe | 105 | 49 | 230.24 (40.13–760.24)/315.4 (54.96–1098.12) | 311.34 (60.07–1134.24) |
| Yang et al. 77 | 2020/5/15 | China | J Med Virol | – | Severe/no‐severe | 68 | 65 | 234.5 (155.5–353.5) | 478 (326–571) |
| Xu et al. 52 | 2020/6/13 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 30 | 125 | 330.43 ± 211.00 | 481.12 ± 243.60 |
| Zheng et al. 78 | 2020/4/6 | China | J Clin Virol | – | Severe/no‐severe | 26 | 63 | 273.92 ± 185.21 | 553.25 ± 377.81 |
| Wang et al. 57 | 2020/3/15 | China | J Infect | – | Death/no‐death | 65 | 274 | 191 (107–282) | 349 (217–516) |
| Liu et al. 59 | 2020/7/31 | China | Ann Intensive Care | – | Death/no‐death | 157 | 1033 | 211 (275–645) | 388 (275–645) |
| Wei et al. 61 | 2020/4/16 | China | J Infect | – | Severe/no‐severe | 30 | 137 | 282.00 (183.00–574.75) | 490.40 ± 232.64) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 203.00 (126.50–284.25) | 368.00 (246.00–549.00) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 299.00 (249.00–460.00) | 573.50 (426.75–771.00) |
| 168.50 (125.25–255.00) | |||||||||
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 244.57 ± 135.87 | 342.39 ± 173.91 | |
| 146.74 ± 125 | |||||||||
| CD8+T cells count (unit: cells/μL) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 128.0 (65.0–182.0) | 217.0 (176.0–415.0) |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 89.0 (61.5–130.3) | 254.0 (183.3–312.8) |
| Diao et al. 70 | 2020/5/1 | China | Front Immunol | – | ICU/no‐ICU | 43 | 212 | 64.3 (40.7–160) | 208 (118–356) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 125.98 ± 84.71 | 345.00 ± 194.10 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 154.7 ± 116.5 | 201.9 ± 107.1 |
| Shi et al. 17 | 2020/3/12 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 19 | 311.33 ± 222.67 | 317.6 ± 150.67 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 117.0 (59.0–177.0) | 234.0 (122.3–367.8) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | – | Severe/no‐severe | 21 | 102 | 179 ± 23.87 | 288.6 ± 14.23 |
| Wu et al. 9 | 2020/3/13 | China | JAMA Intern Med | – | ARDS/no‐ARDS | 84 | 117 | 157.50 (76.00–289.50) | 241.00 (159.0–323.00) |
| Xu et al. 41 | 2020/3/8 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 44 | 88 (60–145) | 266 (166–401) |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 139 (97–183) | 453.5 (232.8–586) |
| Zeng et al. 71 | 2020/3/8 | China | medRxiv | Flow cytometry | ICU/no‐ICU | 65 | 113 | 207 ± 142 | 455 ± 127 |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 109.694 ± 161.125 | 312.704 ± 432.54 |
| Zhou et al. 75 | 2020/3/17 | China | Ann Palliat Med | Aggravation/no‐aggravation | 5 | 12 | 147 (116–446) | 364 (111–799) | |
| Zheng et al.(b) 11 | 2020/3/19 | China | Cell Mol Immunol | – | Severe/no‐severe | 13 | 55 | 206.52 ± 117.72 | 336.96 ± 725.87 |
| Liu et al. 27 | 2020/4/10 | China | Viral Immunol | Severe/no‐severe | 30 | 60 | 65 (33–112) | 267 (210–405) | |
| Fan et al. 45 | 2020/4/19 | China | Metabolism | Death/no‐death | 4 | 15 | 33 (23–135) | 273 (122–377) | |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 297.55 ± 223.32 | 301.03 ± 159.44 |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 205.14 ± 153.09/202.22 ± 199.10 | 462.88 ± 154.43/355.33 ± 166.86 |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 121 (54–197) | 366 (274–482) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 134 (91–237) | 417 (309–539) |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 106.5 (42.0–212.5)/68.0 (52.0–156.0 | 268.0 (157.0–396.0)/221.0 (128.3–312.0) |
| Yang et al. 76 | 2020/4/29 | China | J Allergy Clin Immunol | – | Severe/no‐severe | 36 | 14 | 146 (97–225.25) 139 (107–171.5) | 453.5 (232.8–586) |
| Liu et al. 74 | 2020/5/13 | China | Clin Chim Acta | Flow cytometry | Severe/no‐severe | 105 | 49 | 97.34 (21.82–733.95)/220.95 (49.45–833.76) | 175.62 (40.73–865.47) |
| Xu et al. 52 | 2020/6/13 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 30 | 125 | 233.50 ± 149.63 | 359.12 ± 191.26 |
| Zheng et al. 78 | 2020/4/6 | China | J Clin Virol | – | Severe/no‐severe | 26 | 63 | 202.31 ± 144.31 | 349.13 ± 256.5 |
| Wang et al. 57 | 2020/3/15 | China | J Infect | – | Death/no‐death | 65 | 274 | 73 (42–160) | 204 (97–298) |
| Liu et al. 59 | 2020/7/31 | China | Ann Intensive Care | – | Death/no‐death | 157 | 1033 | 129 (87–144) | 242 (156–356) |
| Wei et al. 61 | 2020/4/16 | China | J Infect | – | Severe/no‐severe | 30 | 137 | 191.00 (135.75–326.50) | 316.00 (234.50–452.25) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 145.00 (70.00–213.00) | 205.00 (111.00–303.00) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 188.00 (134.00–274.00) L 92.50 (70.75–141.50) | 323.50 (232.75–448.75) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 156.52 ± 123.91 | 198.91 ± 120.65 | |
| 110.87 ± 88.04 | |||||||||
| Treg cell count (unit: cells/μL) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 4.7 (2.6–5.4) | 3.9 (3.6–4.3) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 3. 7 ± 1.3 | 4.5 ± 0.9 |
| Shi et al. 17 | 2020/3/12 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 19 | 7.13 ± 2.49 | 8.54 ± 2.09 |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Severe/no‐severe | 25 | 31 | 7.15 ± 3.84 | 8.58 ± 3.19 | |
| CD3+T cells ratio (unit: %) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 55.1 (52.2–60.5) | 68.8 (64.7–75.2) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 65.85 ± 2.05 | 79.27 ± 1.94 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 60 (50–71) | 72 (69–77)/73 (69–78) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 60.0 ± 10.8 | 63.4 ± 8.5 |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 29 | 31 | 64.75 (52.75–76.36) | 66.85 (57.53–75.05) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 59.71 ± 15.21 | 65.58 ± 9.66 | |
| 57.77 ± 11.95 | |||||||||
| Xie et al. 79 | 2020/4/24 | China | J Med Virol | Severe/no‐severe | 34 | 22 | 74.68 (70.81–78.92) | 77.18 (68.35–82.03) | |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 70.2 ± 13.41 | 70.21 ± 9.88 |
| Zheng et al. 56 | 2020/3/27 | China | Int J Infect Dis | – | Severe/no‐severe | 21 | 34 | 70.5 (39.5–86.8) | 76.8 (62.9–89.6) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 60.49 (45.30–64.45) | 69.00 (55.48–74.82) |
| CD4+T cells ratio (unit: %) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 36.7 (30.7–37.3) | 36.4 (32.0–40.6) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 40.24 ± 1.46 | 45.61 ± 1.95 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 33 (25–42) | 40 (33–43)/40 (37–46) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 37.2 ± 8.4 | 39.8 ± 7.5 |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 38.31 ± 7.31 | 42.82 ± 7.58 |
| Xie et al. 79 | 2020/4/24 | China | J Med Virol | Severe/no‐severe | 34 | 22 | 44.92 (40.46–53.49) | 46.29 (40.7–52.36) | |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 35.61 ± 8.93 | 38.47 ± 6.07 | |
| 33.06 ± 14.05 | |||||||||
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 20.0 (20.0–30.0) | 50.0 (30.0–70.0) |
| Xie et al. 53 | 2020/6/13 | China | Circ J | – | Severe/no‐severe | 24 | 38 | 36.7 (30.6–52.6) | 41.4 (37.5–50.3) |
| 42.2 (36.0–50.8) | |||||||||
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 33.90 (27.09–39.58) | 41.46 (32.95–46.58) |
| CD8+T cells ratio (unit: %) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 17.4 (14.7–23.4) | 25.2 (22.8–34.2) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 23.29 ± 1.35 | 32.05 ± 2.53 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 20 (16–25) | 26 (24–30)/26 (23–30) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 19.7 ± 9.2 | 19.5 ± 6.2 |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 30.92 ± 13.32 | 24.64 ± 10.68 |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 10.0 (10.0–30.0) | 30.0 (20.0–40.0) |
| Xie et al. 53 | 2020/6/13 | China | Circ J | – | Severe/no‐severe | 24 | 38 | 17.3 (14.1–25.4)/22.8 (17.6–25.4) | 27.6 (23.8–31.8)/23.5 (19.2–28.6) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 20.65 (13.36–32.06) | 22.20 (16.52–29.90) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 21.76 ± 8.1 | 22.85 ± 9.5 | |
| 25.76 ± 12.07 | |||||||||
| Xie et al. 79 | 2020/4/24 | China | J Med Virol | Severe/no‐severe | 34 | 22 | 23.52 (17.8–30.23) | 25.16 (16.15–31.41) | |
| CD4+CD8+ (ThTs) ratio (unit: %) | |||||||||
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 173 | 1.78 (1.29–2.15) | 1.68 (1.23–2.32) |
| Diao et al. 70 | 2020/5/1 | China | Front Immunol | – | ICU/no‐ICU | 43 | 212 | 2.43 (1.5–4.25) | 1.6 (1.17–2.28) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 2.32 ± 0.24 | 1.65 ± 0.19 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 2.2 ± 0.6 | 2.5 ± 1.5 |
| Shi et al. 17 | 2020/3/12 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 19 | 1.51 ± 0.71 | 2.01 ± 0.8 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 1.2 (1.1–1.7) | 1.2 (0.9–1.6) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | – | Severe/no‐severe | 21 | 102 | 1.509 ± 0.1701 | 1.671 ± 0.05941 |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 2.26 (1.35–2.82) | 1.71 (1.21–2.17) |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 2.277 ± 3.164 | 0.965 ± 1.516 |
| Fan et al. 45 | 2020/4/19 | China | Metabolism | Death/no‐death | 4 | 15 | 5.0 (2.0–6.2) | 1.6 (1.3–2.4) | |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 29 | 31 | 1.99 (1.28–3.75) | 1.46 (0.78–2.11) |
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 1.52 ± 0.71 | 2.03 ± 0.81 |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 1.28 ± 0.76/2.42 ± 1.56 | 1.53 ± 0.41/1.62 ± 1.86 |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 135 | 1.57 (1.10–2.36) | 1.66 (1.37–2.16) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 1.40 (0.79–2.08) | 1.18 (0.96–1.58) |
| Yang et al. 77 | 2020/5/15 | China | J Med Virol | – | Severe/no‐severe | 68 | 65 | 1.42 (1–2.02) | 1.23 (0–1.68) |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 1.5 (0.9–2.4) | 1.6 (1.1–2.4) |
| Xu et al. 52 | 2020/6/13 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 30 | 125 | 1.80 ± 0.92 | 1.54 ± 0.67 |
| Wei et al. 61 | 2020/4/16 | China | J Infect | – | Severe/no‐severe | 30 | 137 | 1.51 ± 0.71 | 1.51 (1.11–1.91) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 1.59 (1.13–2.47) | 1.93 (1.26–2.68) |
| Xie et al. 79 | 2020/4/24 | China | J Med Virol | Severe/no‐severe | 34 | 22 | 1.88 (1.39–2.85) | 1.99 (1.52–3.19) | |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 2.17 ± 1.6 | 2.14 ± 1.17 | |
| 1.66 ± 1.16 | |||||||||
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 1.96 (1.02–2.70)/1.75 (1.06–2.28) | 1.68 (0.96–2.18) |
| CD19+ B cells count (unit: cells/μL) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 184.0 (42.8–273.3) | 115.5 (102.8–133.5) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 124.59 ± 62.64 | 167.03 ± 94.32 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 169 ± 140.9 | 196.1 ± 144.9 |
| Shi et al. 17 | 2020/3/12 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 19 | 131.3 ± 112.3 | 187.17 ± 133.69 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 82 (45.0–149.0) | 115.5 (83.0–161.5) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | MMFI | Severe/no‐severe | 21 | 102 | 125.3 ± 13.49 | 166 ± 11.98 |
| Xu et al. 41 | 2020/3/8 | China | medRxiv | Flow cytometry | Severe/no‐severe | 25 | 44 | 74 (45–196) | 124 (72–240) |
| Zeng et al. 71 | 2020/3/8 | China | medRxiv | Flow cytometry | ICU/no‐ICU | 65 | 113 | 126 ± 52 | 155 ± 51 |
| Zheng et al. 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 109.5 ± 57.756 | 230.21 ± 217.257 |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | Death/no‐death | 14 | 71 | 106.00 (55.00–142.75) | 128.00 (91.00–187.00) | |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 91 (54–139) | 190 (139–268) | |
| Xu et al. 63 | 2020/4/18 | China | J Infect | Flow cytometry | Severe/no‐severe | 107 | 80 | 97.00 (74.00–162.00)/73.00 (36.50–101.75) | 213.50 (152.25–314.25) |
| Fan et al. 45 | 2020/4/19 | China | Metabolism | Death/no‐death | 4 | 15 | 84 (34–134) | 104 (49–236) | |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 155.65 ± 98.21 | 174.86 ± 145.77 | |
| 58.44 ± 37.21 | |||||||||
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 128.83 ± 42.44/119.38 ± 59.07 | 330.71 ± 177.65/148.92 ± 89.33 |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 92 (56–135) | 163 (126–224) |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 88.5 (54.8–175.0)/75.0 (45.0–163.0) | 139.0 (91.5–221.5)/149.5 (111.3–237.0) |
| CD16+CD56+ NK cells count (unit: cells/μL) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 60.5 (27.5–109.0) | 180.5 (115.0–228.0) |
| Han et al. 67 | 2020/3/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 115.65 ± 76.06 | 179.85 ± 80.27 |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 113 ± 71.8 | 160.2 ± 90.8 |
| Shi et al. 17 | 2020/3/12 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 19 | 90.32 ± 86.02 | 189.25 ± 75.27 |
| Song et al. 18 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 100 (54.0–178.0) | 232.5 (100.5–286.3) |
| Wan et al. 34 | 2020/2/10 | China | Br J Haematol | Multiple microsphere flow immunofluorescence | Severe/no‐severe | 21 | 102 | 119.6 ± 16.5 | 147 ± 10.36 |
| Zeng et al. 71 | 2020/3/8 | China | medRxiv | Flow cytometry | ICU/no‐ICU | 65 | 113 | 239 ± 133 | 283 ± 131 |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 537.5 ± 674.557 | 250.706 ± 193.328 |
| Zheng et al.(b) 11 | 2020/3/19 | China | Cell Mol Immunol | – | Severe/no‐severe | 13 | 55 | 105.11 ± 79.05 | 188.32 ± 130 |
| Xu et al. 63 | 2020/4/18 | China | J Infect | Flow cytometry | Severe/no‐severe | 107 | 80 | 93 (60–161)/55.5 (32–91.25) | 107.5 (82.75–149.75) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | Severe/no‐severe | 69 | 135 | 105 (66–168) | 144 (93–231) | |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐sever | 35 | 30 | 127.42 ± 107.41 | 133.92 ± 101.73 | |
| 142.59 ± 96.63 | |||||||||
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐sever | 25 | 31 | 89.14 ± 86.21 | 192.01 ± 73.14 |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 185.00 ± 180.11/102.88 ± 72.28 | 288 ± 175.93/203.63 ± 209.433 |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 122 (51–162) | 186 (122–302) |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 51.0 (24.3–124.0)/100.0 (40.0–157.0) | 132.5 (71.8–196.3)/137.5 (81.3–224.8) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 88.00 (39.5–176.25) | 119.00 (74.00–171.00) |
| CD19+ B cells ratio (unit: %) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 20.2 (17.6–39.5) | 10.8 (10.3–12.4) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 14.63 ± 1.83 | 14.63 ± 1.46 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 12 (9–22) | 12 (10–16)/11 (9–15) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 21.8 ± 12.2 | 18.5 ± 8.1 |
| Zheng et al. 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 11.448 ± 5.666 | 12.537 ± 5.571 |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | Death/no‐death | 14 | 71 | 17.30 (10.33–40.30) | 15.23 (11.55–21.22) | |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 29 | 31 | 21.59 (12.03–29.31) | 14.88 (9.6023.87) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 22.38 ± 12.65/25.62 ± 12 | 18.49 ± 8.76 | |
| CD16+CD56+ NK cells ratio (unit: %) | |||||||||
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | Flow cytometry | Severe/no‐severe | 11 | 10 | 14.7 (7.5–21.0) | 15.1 (11.6–22.8) |
| Liu et al. 15 | 2020/3/1 | China | medRxiv | Flow cytometry | Severe/no‐severe | 69 | 11 | 13.87 ± 1.22 | 3.19 ± 0.82 |
| Nie et al. 16 | 2020/3/24 | China | medRxiv | – | Severe/no‐severe | 25 | 72 | 18 (12–31) | 12 (8–19)/12 (9–19) |
| Qin et al. 10 | 2020/3/12 | China | Clin Infect Dis | Flow cytometry | Severe/no‐severe | 27 | 17 | 16.9 ± 10.1 | 17.2 ± 10.1 |
| Zheng et al. 72 | 2020/2/19 | China | medRxiv | Flow cytometry | Severe/no‐severe | 8 | 95 | 38.2 ± 18.427 | 15.128 ± 10.337 |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 29 | 31 | 7.71 (4.95–16.07) | 11.77 (7.53–23.12) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | Severe/no‐severe | 35 | 30 | 16.78 ± 10.48 | 15.03 ± 9.81 | |
| 29.95 ± 12.11 | |||||||||
| Tan et al. 41 | 2020/5/27 | China | Immunology | Flow cytometry | Severe/no‐severe | 25 | 31 | 14.99 ± 6.38 | 14.22 ± 9.77 |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 17.32 (11.59–26.48) | 13.24 (8.79–19.03) |
| Neutrophils count (unit: cells/μL) | |||||||||
| Huang et al. 80 | 2020/5/8 | China | medRxiv | – | Severe/no‐severe | 27 | 321 | 4.06 (3.26–6.42) | 2.85 (2.28–3.79) |
| Huang et al. 81 | 2020/5/8 | China | PLoS Negl Trop Dis | – | Severe/no‐severe | 23 | 179 | 4.5 (2.8–5.9) | 2.8 (2.1–3.6) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 7.66 (6.16–11.6) | 3.65 (2.58–5.80) |
| Wang et al. 33 | 2020/4/23 | China | JCI Insight | – | Severe/no‐severe | 35 | 30 | 5.7 ± 3.7 | 3.8 ± 2.4 |
| 7.7 ± 3.9 | |||||||||
| Tan et al. 41 | 2020/5/27 | China | Immunology | – | Severe/no‐severe | 25 | 31 | 7.21 ± 5.25 | 4.49 ± 3.64 |
| Xie et al. 79 | 2020/4/24 | China | J Med Virol | – | Severe/no‐severe | 34 | 22 | 4.31 (2.88–5.47) | 2.78 (2.35–3.56) |
| Dong et al. 46 | 2020/5/29 | China | Transbound Emerg Dis | – | Severe/no‐severe | 53 | 94 | 3.46 (2.42–5.40) | 2.32 (1.75–3.51) |
| Zhang et al. 82 | 2020/5/30 | China | Eur Radiol | – | Death/no‐death | 10 | 50 | 8.6 ± 5.1 | 5.2 ± 3.4 |
| Li et al. 83 | 2020/5/15 | China | Theranostics | – | Death/no‐death | 25 | 68 | 3.8 (2.7–5.2) | 2.8 (2.2–3.6) |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 3.76 ± 1.85/5.54 ± 3.70 | 3.25 ± 0.82/2.70 ± 1.01 |
| Sun et al. 84 | 2020/4/24 | China | Clin Chim Acta | – | Severe/no‐severe | 27 | 89 | 6.07 (3.10–7.60) | 2.90 (2.15–3.80) |
| Qi et al. 85 | 2020/5/20 | China | Gut | – | Death/no‐death | 5 | 16 | 4.01 (1.54–7.45) | 2.48 (1.64–4.22) |
| He et al. 20 | 2020/4/14 | China | J Clin Virol | – | Severe/no‐severe | 69 | 136 | 3.87 (2.49–6.11) | 2.69 (2.03–3.61) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 13 | 40 | 5.58 (1.76–5.87) | 2.63 (1.98–4.19) |
| Shang et al. 86 | 2020/5/21 | China | J Med Virol | – | Severe/no‐severe | 139 | 304 | 4.27 (2.65–6.24) | 3.07 (2.35–4.15) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 4.65 (2.11–8.79) | 2.83 (1.98–3.51) |
| Yip et al. 87 | 2020/5/18 | Singapore | Br J Haematol | – | Severe/no‐severe | 20 | 56 | 4.56 (1.79–14.75) | 3.15 (0.98–16.76) |
| Zhao et al. 88 | 2020/5/14 | China | EPMA J | – | Death/no‐death | 29 | 503 | 6.3 ± 3.3 | 3.8 ± 2.9 |
| Shi et al. 73 | 2020/5/14 | China | Diabetes Care | – | Death/no‐death | 47 | 259 | 8.0 (5.1–11.7)/6.6 (4.2–12.4 | 3.3 (2.5–4.9)/8.0 (5.1–11.7) |
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 4.06 (2.84–5.56) | 2.99 (2.14–4.13) |
| 5.79 (3.79–8.59) | |||||||||
| Wang et al. 89 | 2020/4/30 | China | Crit Care | – | Death/no‐death | 19 | 88 | 5.4 (3.2–8.5) | 2.8 (2.0–3.9) |
| Yang et al. 76 | 2020/4/29 | China | J Allergy Clin Immunol | – | Severe/no‐severe | 36 | 14 | 2.74 (1.81–3.13) | 2.8 (2.17–4.43) |
| 3.53 (2.29–5.56) | |||||||||
| Hou et al. 30 | 2020/5/4 | China | Clin Exp Immunol | – | Severe/no‐severe | 221 | 168 | 4.71 ± 2.66 | 3.43 ± 2.55 |
| 9.86 ± 5.97 | |||||||||
| Yu et al. 90 | 2020/4/27 | China | Clin Ther | – | ARDS/no‐ARDS | 24 | 71 | 3.21 ± 1.34 | 3.36 ± 1.51 |
| Hong et al. 35 | 2020/5/7 | South Korea | Yonsei Med J | – | ICU/no‐ICU | 13 | 85 | 7.7 ± 3.3 | 4.1 ± 3.2 |
| Wang et al. 91 | 2020/2/7 | China | JAMA | – | ICU/no‐ICU | 36 | 102 | 4.6 (2.6–7.9) | 2.7 (1.9–3.9) |
| Liu et al. 2 | 2020/2/12 | China | medRxiv | – | Severe/no‐severe | 17 | 44 | 2.8 (2.3–4.4) | 2.4 (1.9–3.4) |
| Liu et al. 68 | 2020/2/12 | China | medRxiv | – | Severe/no‐severe | 13 | 27 | 4.7 (3.6–5.8) | 2.0 (1.5–2.9) |
| Huang et al. 92 | 2020/5/14 | China | J Med Virol | – | Death/no‐death | 16 | 283 | 5.6 ± 3.4 | 3.2 ± 2 |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | – | Severe/no‐severe | 8 | 95 | 2.465 ± 0.91 | 2.98 ± 1.26 |
| Fu et al. 93 | 2020/5/6 | China | Thromb Res | – | Severe/no‐severe | 16 | 59 | 5.63 ± 3.50 | 2.92 ± 1.21 |
| Lu et al. 94 | 2020/2/19 | China | medRxiv | – | Severe/no‐severe | 22 | 243 | 3.3 (2.7–4.8) | 2.8 (2.3–3.8) |
| Liu et al. 95 | 2020/2/23 | China | medRxiv | – | Severe/no‐severe | 7 | 44 | 5.2 (3.2–9.9) | 3.5 (2.4–5.6) |
| Feng et al. 3 | 2020/2/23 | China | medRxiv | – | Progressive/Stable | 15 | 126 | 3.2 (2.6–5.2) | 3.4 (2.2–4.3) |
| Mao et al. 96 | 2020/2/23 | China | medRxiv | – | Severe/no‐severe | 88 | 126 | 3.8 (0.0–18.7) | 2.6 (0.7–11.8) |
| Qian et al. 97 | 2020/2/25 | China | QJM | – | Severe/no‐severe | 9 | 82 | 3.32 (3–5.82) | 2.8 (2.18–3.49) |
| Wang et al. 98 | 2020/3/17 | China | medRxiv | – | Severe/no‐severe | 38 | 72 | 4.26 (2.84–4.84) | 3.38 (2.33–5.24) |
| Liang et al. 99 | 2020/5/12 | China | JAMA Intern Med | – | Severe/no‐severe | 131 | 1459 | 6.4 (3.6) | 3.9 (1.9) |
| Rica et al. 100 | 2020/6/24 | Spain | Microorganisms | – | ICU/no‐ICU | 21 | 27 | 6.76 (3.58) | 5.62 (3.12) |
| Xiong et al. 101 | 2020/5/8 | China | J Am Soc Nephrol | – | Severe/no‐severe | 30 | 101 | 5.3 (3.4–6.6) | 3.7 (2.6–5.6) |
| Huang et al. 102 | 2020/5/5 | China | J Med Virol | – | Progressive/stable | 45 | 299 | 4.7 ± 3.3 | 3 ± 1.7 |
| Giacomelli et al. 103 | 2020/5/6 | Italy | Pharmacol Res | – | Death/no‐death | 48 | 185 | 5.7 (3.8−8.3) | 3.9 (2.8−5.3) |
| Liu et al. 104 | 2020/2/29 | China | Chin Med J | – | Progression/stabilization | 11 | 67 | 4.69 (2.96–7.06) | 2.94 (2.20–4.60) |
| Li et al. 105 | 2020/5/5 | China | Invest Radiol | – | Severe/no‐severe | 25 | 58 | 4.36 (2.87–6.48) | 3.50 (2.64–4.46) |
| Ji et al. 106 | 2020/5/6 | China | Epidimiol Infect | – | Severe/no‐severe | 69 | 88 | 3.3 (2.5–6.1) | 3.2 (2.2–4.2) |
| 8.5 (4.2–10.6) | |||||||||
| Fan et al. 107 | 2020/2/29 | Singapore | Am J Hematol | – | ICU/no‐ICU | 9 | 58 | 4.40 ± 4.14 | 2.8 ± 1.33 |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 2.98 (2.12–3.7) | 2.32 (1.75–4.28) |
| Luo et al. 108 | 2020/5/23 | China | Clin Infect Dis | – | Death/no‐death | 84 | 214 | 6.92 (4.33–10.79) | 3.20 (2.53–4.56) |
| Buckner et al. 109 | 2020/5/22 | USA | Clin Infect Dis | – | Severe/no‐severe | 51 | 54 | 5.4 (3.3–8.4) | 3.8 (2.8–5.1) |
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 24.1 (2.7–5.6) | 2.9 (1.9–3.9) |
| Shi et al. 111 | 2020/6/3 | China | BMC Med | – | Progressive/Stable | 16 | 69 | 3.5 ± 1.5 | 3.1 ± 1.6 |
| Gayam et al. 50 | 2020/7/16 | USA | J Med Virol | – | Death/no‐death | 132 | 276 | 7.2 (4.7–10.35) | 5.6 (3.9–8.4) |
| Lee et al. 112 | 2020/7/21 | South Korea | Int J Infect Dis | – | Severe/no‐severe | 137 | 557 | 4.57 (3.00) | 2.93 (1.36) |
| Yu et al. 113 | 2020/7/17 | China | J Infect Public Health | – | Severe/no‐severe | 864 | 799 | 3.9 (2.8−5.7) | 3.6 (2.6−4.9) |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 4.7 (3.1–8.7) | 3.3 (2.2–4.5) |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 10 | 40 | 5.58 (1.76–5.87) | 2.63 (1.98–4.19) |
| Chen et al. 114 | 2020/5/29 | China | medRxiv | – | Severe/no‐severe | 50 | 241 | 3.34 (2.17–4.18) | 3.56 (2.55–4.62)/2.80 (2.14–3.56) |
| Cao et al. 66 | 2020/3/4 | China | medRxiv | – | ICU/no‐ICU | 19 | 174 | 3.47 (2.97–4.74) | 2.81 (2.33–3.81) |
| Xie et al. 53 | 2020/6/13 | China | Circ J | – | Severe/no‐severe | 24 | 38 | 3.2 (3.0–3.8) | 3.0 (2.1–4.0) |
| 3.5 (3.0–4.5) | 3.5 (2.5–4.6) | ||||||||
| Cao et al. 115 | 2020/6/17 | China | PLoS One | – | Death/no‐death | 27 | 53 | 3.3 (1.9–5.5) | 2.2 (1.7–2.8) |
| Zhang et al. 116 | 2020/3/6 | China | J Clin Virol | – | Severe/no‐severe | 55 | 166 | 5.4 (2.8–8.4) | 2.6 (1.8–4.0) |
| Wang et al. 117 | 2020/5/19 | China | Open Forum Infect Dis | – | Severe/no‐severe | 45 | 230 | 3.7 (2.7–5.2) | 2.7 (2–3.5) |
| Liu et al. 118 | 2020/5/1 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 42 | 236 | 4.4 ± 3.1 | 2.8 ± 1.2 |
| 4.9 ± 2.5 | 2.9 ± 1.3 | ||||||||
| Song et al. 18 | 2020/4/9 | China | medRxiv | – | Severe/no‐severe | 42 | 31 | 5.8 (2.8–10.2) | 2.8 (1.8–4.1) |
| Li et al. 119 | 2020/6/1 | China | Am J Med Sci | – | Death/no‐death | 14 | 60 | 6.3 (2.8–10.0) | 5.0 (2.9–7.1) |
| Xu et al. 41 | 2020/3/5 | China | medRxiv | – | Severe/no‐severe | 25 | 44 | 2.9 (2.4–4.6) | 2.3 (1.8–3.3) |
| Zhang et al. 120 | 2020/7/8 | China | Infect Dis Poverty | – | Severe/no‐severe | 78 | 710 | 3.2 (2.6–5.0) | 3.6 (2.0–5.0) |
| 5.8 (2.8–8.0) | 2.9 (2.2–3.8) | ||||||||
| Zheng et al. 78 | 2020/4/6 | China | J Clin Virol | – | Severe/no‐severe | 32 | 67 | 63.81 ± 16.51 | 42.51 ± 15.11 |
| Zhang et al. 121 | 2020/7/23 | China | Int J Lab Hematol | – | Severe/no‐severe | 162 | 251 | 6.35 ± 3.96 | 3.22 ± 1.67 |
| 8.39 ± 3.37 | 5.02 ± 3.27 | ||||||||
| Qin et al. 10 | 2020/3/8 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 4.3 (2.9–7.0) | 3.2 (2.1–4.4) |
| Levy et al. 122 | 2020/6/2 | USA | medRxiv | – | Death/no‐death | 1185 | 4048 | 6.36 (4.37–9.13) | 5.05 (3.59–7.09) |
| Myers et al. 123 | 2020/4/24 | USA | JAMA | – | ICU/no‐ICU | 113 | 264 | 5.6 (3.9–7.4) | 4.3 (3.1–5.9) |
| Hadjadj et al. 12 | 2020/4/23 | France | medRxiv | – | Severe/no‐severe | 35 | 15 | 5.37 (3.23–6.38) | 3.3 (2.76–4.0) |
| 7.36 (4.54–9.18) | |||||||||
| Ouyang et al. 124 | 2020/4/17 | China | Clin Infect Dis | – | Severe/no‐severe | 6 | 5 | 6.135 (1.80–9.24) | 2.34 (1.2–2.81) |
| Gao et al. 37 | 2020/4/10 | China | J Med Virol | – | Severe/no‐severe | 15 | 28 | 2.65 ± 1.49 | 3.43 ± 1.63 |
| Gong et al. 125 | 2020/4/16 | China | Clin Infect Dis | – | Severe/no‐severe | 28 | 161 | 3.7 (2.8–5.2) | 2.8 (2.0–3.6) |
| Lei et al. 126 | 2020/4/4 | China | EClinicalMedicine | – | ICU/no‐ICU | 15 | 19 | 7.9 (4.1–10.7) | 4.1 (3.1–5.8) |
| Wang et al. 55 | 2020/3/24 | China | Int J infect Dis | – | Severe/no‐severe | 25 | 100 | 3.86 ± 2.18 | 3.49 ± 1.62 |
| Wan et al. 127 | 2020/3/18 | China | J Med Virol | – | Severe/no‐severe | 40 | 95 | 4.1 (3.1–5.7) | 3.6 (3.0–3.9) |
| Feng et al. 128 | 2020/4/10 | China | Am J Respir Crit Care Med | – | Severe/no‐severe | 124 | 352 | 3.6 (2.59–5.99) | 3.39 (2.5–4.64) |
| 5.99 (3.47–9.55) | |||||||||
| Yang et al. 129 | 2020/6/26 | China | medRxiv | – | Death/no‐death | 16 | 53 | 7.(50.6–8.4) | 4 (4.0.0–5.9) |
| Bai et al. 130 | 2020/3/27 | China | medRxiv | – | Severe/no‐severe | 54 | 79 | 4.15 ± 2.29 | 3.54 ± 1.9 |
| Yan et al. 131 | 2020/3/23 | China | medRxiv | – | Severe/no‐severe | 35 | 131 | 4.2 (3.0–7.7) | 2.9 (2.2–3.9) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 7.34 ± 4.10 | 3.03 ± 1.53 |
| Wang et al. 132 | 2020/3/27 | China | medRxiv | – | Death/no‐death | 15 | 101 | 8.2 (6.2–10.0) | 5.2 (2.8–5.7) |
| Li et al. 26 | 2020/3/23 | China | medRxiv | – | Severe/no‐severe | 15 | 87 | 8.0 (3.5–10.6) | 4.1 (2.8–6.2) |
| Chen et al. 24 | 2020/3/27 | China | J Clin Invest | – | Severe/no‐severe | 11 | 10 | 6.9 (4.9–9.1) | 2.7 (2.1–3.7) |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 9.0 (5.4–12.7) | 3.2 (2.4–4.5) |
| Huang et al. 133 | 2020/3/30 | China | BMJ | – | Severe/no‐severe | 32 | 93 | 3.50 ± 1.77 | 3.26 ± 1.28 |
| Lo et al. 134 | 2020/3/15 | China | Int J Biol Sci | – | Severe/no‐severe | 4 | 6 | 3.82 ± 1.81 | 2.49 ± 0.9 |
| Zheng et al. 56 | 2020/3/27 | China | Int J Infect Dis | – | Severe/no‐severe | 21 | 34 | 3.46 (0.56–9.29) | 2.77 (0.93–5.93) |
| Wang et al. 57 | 2020/3/15 | China | J Infect | – | Death/no‐death | 65 | 274 | 7.65 (4.35–11.74) | 4.01 (2.63–5.97) |
| Cai et al. 36 | 2020/4/17 | China | Allergy | – | Severe/no‐severe | 58 | 240 | 7.35 (5.4–9.6) | 6.65 (5.3–8.7) |
| Xie et al. 135 | 2020/4/2 | China | Liver Int | – | Severe/no‐severe | 28 | 51 | 3.8 (3.2–5.7) | 3.7 (2.7–5.1) |
| Du et al. 136 | 2020/4/7 | China | Ann Am Thorac Soc | ICU/no‐ICU | 51 | 58 | 8.3 ± 5.2 | 6.9 ± 4.1 | |
| Wang et al. 32 | 2020/6/1 | China | Am J Respir Crit Care Med | – | Death/no‐death | 133 | 211 | 8.0 (5.5–12.2) | 3.7 (2.5–5.3) |
| Feng et al. 137 | 2020/4/10 | China | medRxiv | – | Severe/no‐severe | 69 | 495 | 4.4 (2.7–6.8) | 2.9 (2.2–3.9) |
| Du et al. 138 | 2020/5/7 | China | Eur Respir J | – | Death/no‐death | 21 | 158 | 7.7 (3.0–11.5) | 3.9 (2.6–6.1) |
| Zhang et al. 139 | 2020/4/11 | China | Eur Radiol | – | Severe/no‐severe | 30 | 90 | 3.1 ± 2.6 | 1.6 ± 1.1 |
| Jiang et al. 140 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 8 | 47 | 3.39 (1.82–9.52) | 3.01 (2.34–3.51) |
| Wang et al. 141 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 30 | 131 | 10.51 ± 5.10 | 6.69 ± 3.83 |
| Chen et al. 142 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 8 | 24 | ||
| Xie et al. 143 | 2020/6/20 | China | Allergy | – | Severe/no‐severe | 12 | 85 | 3.4 (2.2–4.1) | 3.3 (2.3–3.8) |
| Liu et al. 59 | 2020/7/31 | China | Ann Intensive Care | – | Death/no‐death | 157 | 1033 | 14.7 (9.9–20.3) | 4.1 (2.8–6.2) |
| Chen et al. 58 | 2020/4/17 | China | Clin Infect Dis | – | Severe/no‐severe | 27 | 21 | 2.9 (2.0–3.78)/7.1 (5.3–9.2) | 3.4 (2.8–4.3) |
| Yang et al. 144 | 2020/4/13 | China | Int Immunopharmacol | – | Severe/no‐severe | 24 | 69 | 7.73 ± 5.4 | 4.55 ± 0.21 |
| Brill et al. 145 | 2020/6/25 | UK | BMC Med | – | Death/no‐death | 173 | 237 | 6.6 (4.178–9.750) | 5.32 (3.48–7.82) |
| Wei et al. 61 | 2020/4/16 | China | J Infect | – | Severe/no‐severe | 30 | 137 | 3.93 (2.23) | 3.43 (2.39–4.40) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 10.10 (6.58–13.49) | 3.96 (2.85–5.72) |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | – | Severe/no‐severe | 16 | 111 | 3.89 (2.25–6.57) | 3.29 (2.54–4.40) |
| Shi et al. 62 | 2020/4/23 | China | medRxiv | – | Severe/no‐severe | 46 | 88 | 3.0 (2.3–4.3) | 2.9 (2.1–4.0) |
| Yao et al. 146 | 2020/4/24 | China | Pol Arch Intern Med | – | Death/no‐death | 12 | 96 | 6.55 (3.39–9.66) | 2.53 (1.89–3.78)/3.33 (1.99–5.07) |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 4.87 (3.43–7.64) | 3.12 (2.18–4.20) |
| 6.14 (3.33–10.15) | |||||||||
| Pereira et al. 64 | 2020/4/24 | USA | Am J Transplant | – | Severe/no‐severe | 27 | 41 | 3.64 (1.62–7.27) | 4.1 (2.02–5.42) |
| Neutrophils ratio (unit:%) | |||||||||
| Huang et al. 80 | 2020/5/8 | China | medRxiv | – | Severe/no‐severe | 27 | 321 | 72.48 ± 13.70 | 63.29 ± 11.44 |
| Zhang et al. 147 | 2020/5/9 | China | medRxiv | – | ICU/no‐ICU | 30 | 105 | 83.9 (80.7–92.5) | 70.0 (59.8–78.9) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 91.1 (82.9–93.8) | 77.1 (69.1–82.8) |
| Li et al. 83 | 2020/5/15 | China | Theranostics | – | Death/no‐death | 25 | 68 | 74.2 (12.0) | 64.7 (11.6) |
| Yang et al. 76 | 2020/4/29 | China | J Allergy Clin Immunol | – | Severe/no‐severe | 36 | 14 | 69.3 (57–75.3)/69.3 (66.65–82.1) | 58.8 (52.75–71.4) |
| Sun et al. 148 | 2020/5/5 | China | J Med Virol | – | Severe/no‐severe | 15 | 40 | 15 ± 100 | 29 ± 72.5 |
| Liu et al. 105 | 2020/5/5 | China | Invest Radiol | – | Severe/no‐severe | 5 | 58 | 80.08 ± 9.51 | 67.84 ± 10.00 |
| Chen et al. 114 | 2020/5/29 | China | medRxiv | – | Severe/no‐severe | 50 | 241 | 73.15 (63.45–82.85) | 70.30 (59.80–78.40)/62.70 (56.10–70.45) |
| Shi et al. 149 | 2020/5/11 | China | Eur Heart J | – | Death/no‐death | 62 | 609 | 91 (86–93) | 68 (59–76) |
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 76.3 (66.1–84.9) | 64.1 (56.6–73.6) |
| Yang et al. 150 | 2020/5/25 | China | J Clin Pharm Ther | – | Severe/no‐severe | 33 | 103 | 77.8 (64.1–88.5) | 65.9 (57.7–74.6) |
| Yang et al. 65 | 2020/3/2 | China | medRxiv | – | Severe/no‐severe | 34 | 19 | 69.95 (61.35–79.93) | 60.90 (52.95–69.30) |
| Yu et al. 113 | 2020/7/17 | China | J Infect Public Health | – | Severe/no‐severe | 864 | 799 | 70.8 (60.8–79.7) | 67.4 (59.0–75.9) |
| Liu et al. 118 | 2020/5/1 | China | Zhonghua Wei Zhong Bing Ji Jiu Yi Xue | – | Severe/no‐severe | 42 | 236 | 0.72 ± 0.13/0.73 ± 0.14 | 0.51 ± 0.12/0.59 ± 0.11 |
| Li et al. 119 | 2020/6/1 | China | Am J Med Sci | – | Death/no‐death | 14 | 60 | 0.9 (0.8–0.9) | 0.8 (0.7–0.9) |
| Zhang et al. 121 | 2020/7/23 | China | Int J Lab Hematol | – | Severe/no‐severe | 162 | 251 | 78.01 ± 11.31 | 61.48 ± 6.65 |
| 86.79 ± 6.01 | 71.02 ± 12.64 | ||||||||
| Qin et al. 10 | 2020/3/8 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 77.6 (68.9–86.5) | 67.5 (57.8–75.8) |
| Levy et al. 122 | 2020/6/2 | USA | medRxiv | – | Death/no‐death | 1185 | 4048 | 81.00 (73.47–86.50) | 76.25 (68.38–82.30) |
| Bai et al. 130 | 2020/3/27 | China | medRxiv | – | Severe/no‐severe | 54 | 79 | 74.60 ± 13.42 | 66.94 ± 12.16 |
| Tao et al. 151 | 2020/3/23 | medRxiv | China | – | Severe/no‐severe | 22 | 143 | 65.50 ± 16.15 | 61.64 ± 32.24 |
| Yan et al. 131 | 2020/3/23 | China | medRxiv | – | Severe/no‐severe | 35 | 132 | 74.8 (67.6–83.1) | 62.1 (55.6–69.2) |
| Xie et al. 143 | 2020/6/20 | China | Allergy | – | Severe/no‐severe | 12 | 85 | 71.9 (52.6–77.8) | 71.3 (56.2–78.5) |
| Zhu et al. 22 | 2020/4/22 | China | Int J Infect Dis | – | Severe/no‐severe | 16 | 111 | 75.70 (64.53–88.98) | 66.50 (59.60–73.90) |
| Fu et al. 69 | 2020/4/22 | China | medRxiv | – | Death/no‐death | 14 | 71 | 89.65 (85.63–92.28) | 69.30 (62.10–79.10) |
| Yang et al. 77 | 2020/5/15 | China | J Med Virol | – | Severe/no‐severe | 68 | 65 | 76.6 (45.3–97) | 58.1 (18–83.2) |
| Monocytes count (unit: cells/μL) | |||||||||
| Huang et al. 80 | 2020/5/8 | China | medRxiv | – | Severe/no‐severe | 27 | 321 | 0.50 (0.24–1.07) | 0.41 (0.35–0.58) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.33 (0.24–0.56) | 0.41 (0.27–0.56) |
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 0.33 ± 0.19/0.37 ± 0.19 | 0.46 ± 0.16/0.55 ± 0.99 |
| Sun et al. 84 | 2020/4/24 | China | Clin Chim Acta | – | Severe/no‐severe | 27 | 89 | 0.42 (0.31–0.76) | 0.38 (0.29–0.48) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 13 | 40 | 0.51 (0.37–0.60) | 0.39 (0.31–0.51) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 0.32 (0.14–0.42) | 0.39 (0.30–0.50) |
| Yip et al. 87 | 2020/5/18 | Singapore | Br J Haematol | – | Severe/no‐severe | 20 | 56 | 0.48 (0.17–1.36) | 0.54 (0.19–1.35) |
| Wei et al. 21 | 2020/4/29 | China | J Med Virol | Severe/no‐severe | 121 | 131 | 0.6 ± 0.7 | 0.51 ± 0.25 | |
| 0.6 ± 0.3 | |||||||||
| Chen et al. 152 | 2020/4/28 | China | Infection | – | Severe/no‐severe | 43 | 102 | 0.4 (0.3–0.5) | 0.4 (0.3–0.5) |
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 0.36 (0.26–0.52) | 0.41 (0.30–0.53) |
| 0.38 (0.22–0.49) | |||||||||
| Huang et al. 92 | 2020/5/14 | China | J Med Virol | – | Death/no‐death | 16 | 283 | 0.5 ± 0.9 | 0.3 ± 0.2 |
| Rica et al. 100 | 2020/6/24 | Spain | Microorganisms | – | ICU/no‐ICU | 21 | 27 | 0.40 (0.20) | 0.58 (0.33) |
| Huang et al. 102 | 2020/5/5 | China | J Med Virol | – | Progressive/stable | 45 | 299 | 0.3 ± 0.1 | 0.3 ± 0.2 |
| Ji et al. 106 | 2020/5/6 | China | Epidimiol Infect | – | Severe/no‐severe | 69 | 88 | 0.4 (0.2–0.5) | 0.5 (0.3–0.6) |
| 0.3 (0.1–0.6) | |||||||||
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 0.4 (0.2–0.5) | 0.3 (0.2–0.4) |
| Lee et al. 112 | 2020/7/21 | South Korea | Int J Infect Dis | – | Severe/no‐severe | 137 | 557 | 0.47 (0.24) | 0.45 (0.16) |
| Yu et al. 113 | 2020/7/17 | China | J Infect Public Health | – | Severe/no‐severe | 864 | 799 | 0.5 (0.4−0.6) | 0.5 (0.4−0.6) |
| Huang et al. 31 | 2020/6/13 | China | J Med Virol | – | Death/no‐death | 10 | 40 | 0.51 (0.37–0.60) | 0.39 (0.31–0.51) |
| Wang et al. 117 | 2020/5/19 | China | Open Forum Infect Dis | – | Severe/no‐severe | 45 | 230 | 0.3 (0.2–0.4) | 0.4 (0.3–0.5) |
| Zhang et al. 121 | 2020/7/23 | China | Int J Lab Hematol | – | Severe/no‐severe | 162 | 251 | 0.44 ± 0.23 | 0.35 ± 0.1 |
| 0.43 ± 0.18 | 0.42 ± 0.2 | ||||||||
| Levy et al. 122 | 2020/6/2 | USA | medRxiv | – | Death/no‐death | 1185 | 4048 | 0.47 (0.30–0.68) | 0.46 (0.32–0.65) |
| Hadjadj et al. 12 | 2020/4/23 | France | medRxiv | – | Severe/no‐severe | 35 | 15 | 0.35 (0.30–0.43) | 0.40 (0.28–0.52) |
| 0.38 (0.20–0.77) | |||||||||
| Gao et al. 37 | 2020/4/10 | China | J Med Virol | – | Severe/no‐severe | 15 | 28 | 0.37 ± 0.16 | 0.43 ± 0.19 |
| Lei et al. 126 | 2020/4/4 | China | EClinicalMedicine | – | ICU/no‐ICU | 15 | 19 | 0.6 (0.3–1.1) | 0.5 (0.4–0.70) |
| Gong et al. 125 | 2020/4/16 | China | Clin Infect Dis | – | Severe/no‐severe | 28 | 161 | 0.3 (0.3–0.4) | 0.4 (0.3–0.5) |
| Wang et al. 55 | 2020/3/24 | China | Int J Infect Dis | – | Severe/no‐severe | 25 | 100 | 0.30 (0.235–0.52) | 0.36 (0.26–0.51) |
| Yan et al. 131 | 2020/3/23 | China | medRxiv | – | Severe/no‐severe | 35 | 130 | 0.4 (0.3–0.6) | 0.4 (0.3–0.5) |
| Han et al. 67 | 2020/6/24 | China | Aging (Albany NY) | – | Severe/no‐severe | 24 | 23 | 0.39 ± 0.20 | 0.61 ± 0.24 |
| Wang et al. 132 | 2020/3/27 | China | medRxiv | – | Death/no‐death | 15 | 101 | 0.5 (0.3–0.7) | 0.5 (0.4–0.6) |
| Chen et al. 25 | 2020/3/26 | China | BMJ | – | Death/no‐death | 113 | 161 | 0.4 (0.2–0.6) | 0.4 (0.3–0.5) |
| Wang et al. 57 | 2020/3/15 | China | J Infect | – | Death/no‐death | 65 | 274 | 0.32 (0.22–0.49) | 0.43 (0.30–0.62) |
| Jiang et al. 140 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 8 | 47 | 0.28 (0.18–0.60) | 0.49 (0.40–0.61) |
| Wang et al. 141 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 30 | 131 | 0.43 ± 0.27 | 0.50 ± 0.25 |
| Xie et al. 143 | 2020/6/20 | China | Allergy | – | Severe/no‐severe | 12 | 85 | 0.6 (0.2–0.7) | 0.5 (0.3–0.6) |
| Yang et al. 144 | 2020/4/13 | China | Int Immunopharmacol | – | Severe/no‐severe | 24 | 69 | 0.5 ± 0.84 | 0.41 ± 0.2 |
| Xu et al. 63 | 2020/4/18 | China | J Infect | – | Severe/no‐severe | 107 | 80 | 0.42 (0.29–0.61) | 0.39 (0.31–0.52) |
| 0.32 (0.18–0.44) | |||||||||
| Monocytes ratio (unit: %) | |||||||||
| Huang et al. 80 | 2020/5/8 | China | medRxiv | – | Severe/no‐severe | 27 | 321 | 7.2 (4.0–13.6) | 9.5 (7.3–11.3) |
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 3.9 (2.6–5.4) | 8.8 (5.4–10.0) |
| Zheng et al.(a) 72 | 2020/2/19 | China | medRxiv | – | Severe/no‐severe | 8 | 95 | 8.063 ± 3.478 | 8.12 ± 2.92 |
| Liu et al. 105 | 2020/5/5 | China | Invest Radiol | – | Severe/no‐severe | 25 | 58 | 6.16 ± 4.00 | 7.60 ± 2.23 |
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 7.0 (4.5–8.8) | 7.7 (5.7–9.8) |
| Yu et al. 113 | 2020/7/17 | China | J Infect Public Health | – | Severe/no‐severe | 864 | 799 | 8.2 (6.3−10.6) | 8.7 (6.9−10.9) |
| Li et al. 119 | 2020/6/1 | China | Am J Med Sci | – | Death/no‐death | 14 | 60 | 0.01 (0.04–0.08) | 0.01 (0.03–0.06) |
| Zhang et al. 121 | 2020/7/23 | China | Int J Lab Hematol | – | Severe/no‐severe | 162 | 251 | 6.1 ± 2.62/4.7 ± 1.85 | 7.54 ± 2.63/6.94 ± 2.72 |
| Qin et al. 10 | 2020/3/8 | China | Clin Infect Dis | – | Severe/no‐severe | 286 | 166 | 6.6 (4.3–8.8) | 8.4 (6.5–10.8) |
| Levy et al. 122 | 2020/6/2 | USA | medRxiv | – | Death/no‐death | 1185 | 4048 | 12.70 (11.10–14.30) | 13.40 (12.20–14.50) |
| Xie et al. 143 | 2020/6/20 | China | Allergy | – | Severe/no‐severe | 12 | 85 | 8.3 (5.4–10.1) | 7.9 (5.8–9.2) |
| Eosinophils count (unit: cells/μL) | |||||||||
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.00 (0.00–0.00) | 0.00 (0.00–0.38) |
| Cheng et al. 153 | 2020/4/27 | China | medRxiv | Severe/no‐severe | 8 | 51 | 0.01 (0.01–0.33) | 0.02 0.01–026) | |
| 0.02 (0.00–0.05) | |||||||||
| Sun et al. 47 | 2020/4/24 | China | J Autoimmun | – | Severe/no‐severe | 19 | 44 | 0.01 ± 0.00/0.09 ± 0.14 | 0.14 ± 0.06/0.03 ± 0.04 |
| Sun et al. 84 | 2020/4/24 | China | Clin Chim Acta | – | Severe/no‐severe | 27 | 89 | 0.01 (0.00–0.02) | 0.03 (0.01–0.05) |
| Zhang et al. 28 | 2020/5/21 | China | J Med Virol | – | Death/no‐death | 13 | 40 | 0 | 0.01 (0–0.05) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 0.00 (0.00–0.01) | 0.04 (0.01–0.11) |
| Yip et al. 87 | 2020/5/18 | Singapore | Br J Haematol | – | Severe/no‐severe | 20 | 56 | 0.01 (0–0.24) | 0.05 (0–0.42) |
| Pei et al. 29 | 2020/4/28 | China | J Am Soc Nephrol | – | Severe/no‐severe | 189 | 144 | 0.00 (0.00–0.06) | 0.00 (0.00–0.09) |
| 0.00 (0.00–0.01) | |||||||||
| Qian et al. 97 | 2020/2/25 | China | QJM | – | Severe/no‐severe | 9 | 82 | 0.01 (0–0.01) | 0.02 (0.01–0.06) |
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 0.00 (0.00–0.01) | 0.01 (0.00–0.03) |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 0.00 (0.00–0.02) | 0.01 (0.00–0.04) |
| Chen et al. 114 | 2020/5/29 | China | medRxiv | – | Severe/no‐severe | 50 | 241 | 0.00 (0.00–0.01) | 0.02 (0.00–0.06)/0.02 (0.00–0.05) |
| Wei et al. 154 | 2020/7/29 | China | BMC Infect Dis | – | Severe/no‐severe | 14 | 262 | 0 (0–0.01) | 0.01 (0–0.03) |
| Levy et al. 122 | 2020/6/2 | USA | medRxiv | – | Death/no‐death | 1185 | 4048 | 0.00 (0.00–0.01) | 0.00 (0.00–0.02) |
| Yan et al. 131 | 2020/3/23 | China | medRxiv | – | Severe/no‐severe | 35 | 130 | 0 (0–0.02) | 0.04 (0.01–0.1) |
| Wang et al. 132 | 2020/3/27 | China | medRxiv | – | Death/no‐death | 15 | 101 | 0.0 (0.0–0.0) | 0.1 (0.0–0.1) |
| Huang et al. 133 | 2020/3/30 | China | BMJ | – | Severe/no‐severe | 32 | 93 | 0 (0–0) | 0.04 (0.1–0.12) |
| Cai et al. 36 | 2020/4/17 | China | Allergy | – | Severe/no‐severe | 58 | 240 | 0.01 (0–0.03) | 0.02 (0–0.05) |
| Wang et al. 141 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 30 | 131 | 0.00 ± 0.01 | 0.04 ± 0.06 |
| Basophils count (unit: cells/μL) | |||||||||
| Wu et al. 19 | 2020/7/15 | China | mSphere | – | Severe/no‐severe | 39 | 32 | 0.01 (0.01–0.02) | 0.01 (0.00–0.02) |
| Li et al. 48 | 2020/5/19 | China | JCI Insight | – | Severe/no‐severe | 26 | 43 | 0.01 (0.01–0.02) | 0.01 (0.01–0.03) |
| Yip et al. 87 | 2020/5/18 | Singapore | Br J Haematol | – | Severe/no‐severe | 20 | 56 | 0.01 (0–0.10) | 0.02 (0–0.09) |
| Qian et al. 97 | 2020/2/25 | China | QJM | – | Severe/no‐severe | 9 | 82 | 0 (0–0.01) | 0.01 (0.01–0.02) |
| Wu et al. 110 | 2020/5/7 | China | Eur Respir J | – | Severe/no‐severe | 82 | 217 | 0.01 (0.01–0.02) | 0.01 (0.01–0.01) |
| Chen et al. 51 | 2020/6/4 | China | Clin Transl Med | – | Death/no‐death | 82 | 578 | 0.01 (0.01–0.02) | 0.01 (0.01–0.02) |
| Wang et al. 141 | 2020/4/14 | China | medRxiv | – | Severe/no‐severe | 30 | 131 | 0.02 ± 0.02 | 0.02 ± 0.01 |
Abbreviations: CLIA, chemiluminescence immunoassay; ELISA, enzyme‐linked immunosorbent assay; MMFI, multiple microsphere flow immunofluorescence.
2.5. Predictors and outcome
The included studies varied in their differentiation of patients' disease status, with classifications of ‘mild, moderate, severe and critical’, ‘ordinary and severe/critical’, ‘common and severe’, ‘acute respiratory distress syndrome (ARDS) and non‐ARDS’ and ‘non‐severe and severe’. To allow comparability between studies for meta‐analysis, these were grouped into a single disease severity, with the outcome measure used was severe (including both severe and critical cases, ICU admission, death, ARDS, etc.) versus non‐severe disease (including non‐severe, mild disease, ordinary disease, non‐ICU admission and non‐ARDS, etc.).
2.6. Statistical analysis
Quantitative syntheses and meta‐analyses were analysed using the meta package in the R statistical language (Version 3.6.3). First, we collected the mean and standard deviation (SD) from each value of immune mediators in severe and non‐severe groups of COVID‐19 patients. Where necessary, the mean and SD were converted from the median and interquartile range (IQR) using a previously standard approach. 155 For some articles, data regarding the immunological signature were extracted from the figures by measuring the pixel positions of the electronic figures and then computing the actual values. For box plots, medians and ranges were used to compute means and SDs, and for scatter plots, the individual values were used to compute means and SDs. Second, forest plots were conducted to illustrate the differences in the two groups. For fear of that the recruited studies used different experiment methods, for which means and differences cannot be pooled directly to estimate the effect, we calculated a dimensionless effect measure from each study for the pooling use. The standardized mean difference (SMD) was computed from means and SDs, and used as the effect size. 156 Finally, we undertook the meta‐analyses for each immune mediator. The heterogeneity of the studies was tested by the Cochran Chi‐square test and I 2 index, and the pooled SMD were calculated by using the random‐effects model. All results were pooled and presented in the forest plots. Leave‐one‐out sensitivity analysis was applied to detect the robustness of the results. Funnel plot method and Egger's regression were used to test the publication bias. If the funnel plot was asymmetric or p < 0.05, the trim‐and‐fill method was adopted to further test publication bias. The statistical testing with p < 0.05 was considered to be significant (two‐sided).
3. RESULTS
3.1. Review of the included studies
A detailed flow diagram of study selection and the selected number are shown in Figure 1. Our literature search identified 19,802 records through 15 August 2020. After removing duplicates, the title and abstract of the remaining 19,688 articles were screened, and 16,613 records were excluded. For 3075 potentially relevant studies, full‐text was retrieved and evaluated for eligibility, and then 2861 studies were excluded from the meta‐analysis: 1305 studies contained data from only case series, 1,312 studies were literature reviews, 52 studies provided no comparison data between disease severity, and 192 studies didn't provide enough data. As five studies were further excluded because the described immune mediators were investigated in <3 studies (Table S4), at last 214 studies were included in the qualitative synthesis. Those remained in the study were collated for the meta‐analysis consisted of 149 distinct studies that were performed in China (133), the United States (6), South Korea (2), Singapore (2), the United Kingdom (1), France (1), Germany (1), Italy (1), Spain (1), and both China and USA (1) (Table 1). All the included studies had reported patients with severe patients and non‐severe patients. These articles included data from 33,691 patients, 25.96% (n = 8746) with severe COVID‐19 disease and 74.04% (n = 24,945) with non‐severe disease. Of these studies, 55 studies had evaluated the data on 10 cytokines, including interleukins 2 (IL‐2), IL‐2R, IL‐4, IL‐5, IL‐6, IL‐8, IL‐10, interferon γ (IFN‐γ), tumour necrosis factor α (TNF‐α) and IL‐1β,1, 9, 10, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 157 8 studies investigated the antibodies (IgA, IgG, IgM and IgE)10, 16, 20, 25, 66, 67, 68, 69 and 40 studies assessed the T cells [CD3+ T cells count, CD4+ T cells count, CD8+ T cells count, CD4+CD25+CD127−Treg cells count, CD3+ T cells ratio, CD4+ T cells ratio, CD8+ T cells ratio and CD4+/CD8+ (Th/Ts)],9, 10, 11, 15, 16, 17, 18, 19, 20, 24, 27, 33, 34, 41, 45, 47, 48, 51, 52, 53, 56, 57, 59, 61, 63, 65, 66, 67, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 157 and 22 studies estimated the B cells and NK cells (CD16+CD56+ NK cells count, CD19+ B cells count,CD16+CD56+ NK cells ratio and CD19+ B cells ratio),10, 11, 15, 16, 17, 18, 19, 20, 24, 33, 34, 41, 45, 47, 48, 63, 67, 69, 71, 72, 73, 157 124 studies on the evaluation of neutrophils, eosinophils and basophils cells (comprised of neutrophils cells counts/cells ratio, monocytes cells counts/cells ratio, eosinophils cells counts and basophils cells counts).2, 3, 10, 12, 18, 19, 20, 21, 22, 24, 25, 26, 28, 29, 30, 31, 32, 33, 35, 36, 37, 41, 46, 47, 48, 50, 51, 53, 55, 56, 57, 58, 59, 61, 62, 63, 64, 65, 66, 67, 68, 69, 72, 73, 76, 77, 78, 79, 157 , 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144, 145, 146, 147, 148, 149, 150, 151, 152, 153, 154 For each study, various details including the baseline information of study population, study design, the number of patients in each study group, the measured immunological indicators and their test methods, and the definitions used to measure outcome, were extracted into Table S5. For these studies, only the measurements acquired in the acute phase of infection were used for the analysis. Table 1 summarizes the detailed characteristics of the included studies for each immune mediator. The quality scores by NOQAS of the included studies ranged from 5 to 8, and 116 out of 149 was greater than or equal to six stars, indicating good quality (Table S6).
FIGURE 1.
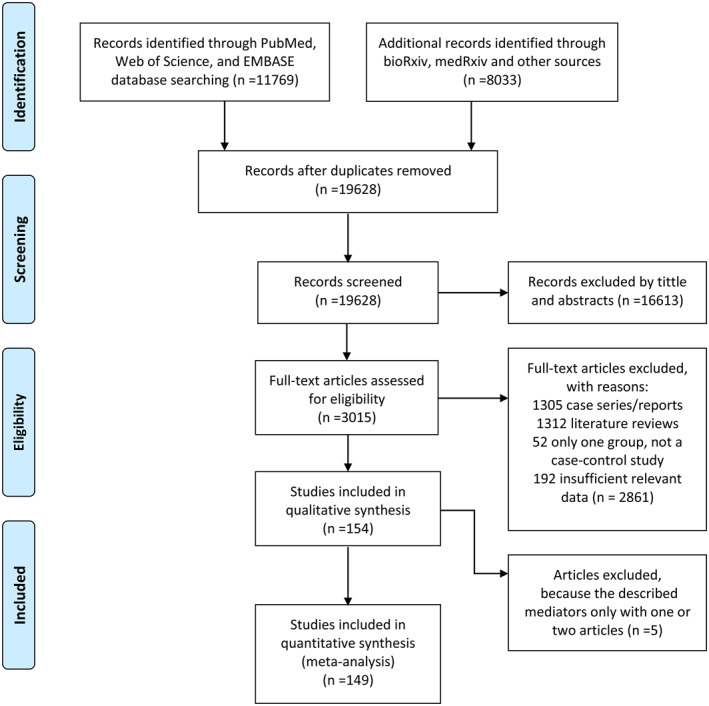
A flow diagram of the inclusion criteria for the study selection process
3.2. Cytokines and COVID‐19 severity
A total of 55 studies were evaluated 10 mediators of cytokines between the severe (n = 3038) and non‐severe groups of COVID‐19 patients (n = 5895), including IL‐2, IL‐2R, IL‐4, IL‐5, IL‐6, IL‐8, IL‐10, IFN‐γ, TNF‐α and IL‐1β with three or more studies included (Figure S1).1, 9, 10, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 157 Compared with the non‐severe patients of COVID‐19, we found that serum levels of seven cytokines were significantly up‐regulated in severe patients, including IL‐2 (SMD, 0.40; 95% CI, 0.10–0.71; p < 0.01), IL‐2R (SMD, 1.12; 95% CI, 0.80–1.44; p < 0.01), IL‐4 (SMD, 0.71; 95% CI, 0.10–1.33; p = 0.02), IL‐6 (SMD, 1.16; 95% CI, 0.94–1.38; p < 0.01), IL‐8 (SMD, 0.75; 95% CI, 0.49–1.00; p < 0.01), IL‐10 (SMD, 1.26; 95% CI, 0.92–1.59; p < 0.01) and TNF‐α (SMD, 0.55; 95% CI, 0.32–0.78; p < 0.01), respectively (Figure S1a–g). In contrast, serum IL‐5, IL‐1β and IFN‐γ did not showed significant inter‐group differences with the SMDs of 0 (95% CI, −0.94 to 0.95, p = 0.99), 0.33 (95% CI, 0.00–0.67, p = 0.05), and 0.46 (95% CI, −0.25 to 1.17, p = 0.20), respectively (Figure S1h–j).
3.3. SARS‐CoV‐2‐specific antibodies and COVID‐19 severity
Four SARS‐CoV‐2‐specific antibody mediators were included in the meta‐analysis between severe and non‐severe COVID‐19 patients, immunoglobulin A (IgA), IgG, IgM and IgE.10, 16, 20, 25, 66, 67, 68, 69 A total of eight studies evaluated the levels of IgA, IgG and IgM involving 563 severe and 828 non‐severe cases, and the levels of IgE involving 131 severe and 257 non‐severe cases (Figure S2). Compared with the non‐severe patients, the severe patients had significantly higher levels of IgA and IgG with SMDs of 0.39 (95% CI, 0.10–0.68; p < 0.01; Figure S2a), and 0.22 (95% CI, 0.01–0.42; p = 0.04; Figure S2b), respectively. The level of IgM in the severe patients was slightly lower than those in the non‐severe patients of COVID‐19 (SMD, −0.18; 95% CI, −0.32 to −0.03, p = 0.02; Figure S2c). No significant differences were noted in the serum levels of IgE between two groups (SMD, 0.16; 95% CI, −0.16 to 0.43, p = 0.43; Figure S2d).
3.4. T cells and COVID‐19 severity
A total of 40 studies involving 1623 severe cases and 4342 non‐severe cases evaluated the T cells count or percent in relation to the COVID‐19 disease severity.9, 10, 11, 15, 16, 17, 18, 19, 20, 24, 27, 33, 34, 41, 45, 47, 48, 51, 52, 53, 56, 57, 59, 61, 63, 65, 66, 67, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 157 Eight measurements of T cells were described in over three studies, including CD3+ T cells count, CD4+ T cells count, CD8+ T cells count, CD4+CD25+CD127− Treg cells count, CD3+ T cells ratio, CD4+ T cells ratio, CD8+ T cells ratio and CD4+/CD8+ (Th/Ts) in Figure S3. Compared with the non‐severe group, severe group had significantly lower CD3+ T cells count (SMD, −1.14; 95% CI, −1.41 to −0.88; p < 0.01; Figure S3a) as well as CD4+ T cells count (SMD, −116; 95% CI, −1.44 to −0.89; p < 0.01; Figure S3b), CD8+ T cells count (SMD, −1.03; 95% CI, −1.27 to −0.79; p < 0.01; Figure S3c), CD4+CD25+CD127‐ Treg cells count (SMD, −0.45; 95% CI, −0.76 to −0.13; p < 0.01; Figure S3d), CD3+ T cells ratio (SMD, −1.10; 95% CI, −1.77 to −0.42; p < 0.01; Figure S3e), and CD4+ T cells ratio (SMD, −0.61; 95% CI, −1.02 to −0.19; p < 0.01; Figure S3f). In contrast, no significant difference was attained for CD8+ T cells ratio (SMD, −0.61; 95% CI, −1.35 to 0.12; p = 0.10; Figure S3g), or CD4+/CD8+ (Th/Ts) (SMD, 0.16; 95% CI, −0.10 to 0.42; p = 0.23; Figure S3h).
3.5. The B cells, NK cells and COVID‐19 severity
A total of 22 studies on the evaluation of B cells and NK cells between severe and non‐severe COVID‐19 patients were included.10, 11, 15, 16, 17, 18, 19, 20, 24, 33, 34, 41, 45, 47, 48, 63, 67, 69, 71, 72, 73, 157 As shown in Figure S4, the CD19+ B cells count and CD16+CD56+ NK cells count in the severe group were significantly lower than those in the non‐severe group with SMDs of −0.74 (95% CI, −1.05 to −0.42; p < 0.01; Figure S4a), and −0.61 (95% CI, −0.84 to −0.38; p < 0.01; Figure S4b), respectively. In contrast, the CD19+ B cells ratio and CD16+CD56+ NK cells ratio were significantly higher in the severe patients than in the non‐severe patients with SMDs of 0.35 (95% CI, 0.15–0.55; p < 0.01; Figure S4c), and 1.19 (95% CI, 0.30–2.07; p < 0.01; Figure S4d), respectively.
3.6. The neutrophils, monocytes, eosinophils, basophils and COVID‐19 severity
About 124 studies on the evaluation of neutrophils, monocytes, eosinophils and basophils cells between severe and non‐severe COVID‐19 patients were included.2, 3, 10, 12, 18, 19, 20, 21, 22, 24, 25, 26, 28, 29, 30, 31, 32, 33, 35, 36, 37, 41, 46, 47, 48, 50, 51, 53, 55, 56, 57, 58, 59, 61, 62, 63, 64, 65, 66, 67, 68, 69, 72, 73, 76, 77, 78, 79, 157 , 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144, 145, 146, 147, 148, 149, 150, 151, 152, 153, 154 As shown in Figure S5, the neutrophils cells count and neutrophils cells ratio in the severe group were significantly higher than those in the non‐severe group with SMDs of 0.72 (95% CI, 0.61–0.82; p < 0.01; Figure S5a), and 0.62 (95% CI, 0.35–0.88; p < 0.01; Figure S5b), respectively. The monocytes cells ratio and eosinophils cells count were significantly lower in the severe patients than in the non‐severe patients of COVID‐19 with SMDs of −0.36 (95% CI, −0.51 to −0.21; p < 0.01; Figure S5c), and −0.45 (95% CI, −0.59 to −0.31; p < 0.01; Figure S5d), while the monocytes cells count and basophils cells count were comparable between the two groups with SMDs of −0.06 (95% CI, −0.15 to 0.04; p = 0.24; Figure S5e), and −0.14 (95% CI, −0.43 to 0.15; p = 0.34; Figure S5f), respectively.
3.7. Sub‐analysis of only peer reviewed studies
The sub‐analysis considering only peer‐reviewed studies for each immune mediator was performed, and the results were presented in Table 2, but without obvious difference with those of all the included literatures analysed.
TABLE 2.
The results of meta‐analyses for each immune indicator in the study
| Variables | Number of studies included | Heterogeneity I 2 | SMD (95% CI) | p * | Publication bias | |
|---|---|---|---|---|---|---|
| T | p # | |||||
| Cytokines | ||||||
| IL‐2 | 9 | 77% | 0.40 (0.10, 0.71) | <0.01 | 0.721 | 0.495 |
| IL‐2R | 12 | 89% | 1.12 (0.80, 1.44) | <0.01 | 3.146 | 0.011 |
| IL‐4 | 11 | 95% | 0.71 (0.10, 1.33) | 0.02 | 1.406 | 0.193 |
| IL‐6 | 54 | 94% | 1.16 (0.94, 1.38) | <0.01 | 2.435 | 0.018 |
| IL‐8 | 13 | 80% | 0.75 (0.49, 1.00) | <0.01 | 1.301 | 0.220 |
| IL‐10 | 27 | 95% | 1.26 (0.92, 1.59) | <0.01 | 3.236 | 0.003 |
| TNF‐α | 26 | 88% | 0.55 (0.32, 0.78) | <0.01 | 0.856 | 0.400 |
| IL‐5 | 3 | 92% | 0.00 (−0.94, 0.95) | 0.99 | 1.052 | 0.484 |
| IL‐1β | 13 | 79% | 0.33 (0.00, 0.67) | 0.05 | 0.841 | 0.425 |
| IFN‐γ | 12 | 96% | 0.46 (−0.25, 1.17) | 0.20 | 1.724 | 0.116 |
| Specific antibodies | ||||||
| IgA | 8 | 79% | 0.39 (0.10, 0.68) | <0.01 | 1.902 | 0.106 |
| IgG | 8 | 59% | 0.22 (0.01, 0.42) | 0.04 | 0.626 | 0.555 |
| IgM | 8 | 22% | −0.18 (−0.32, −0.03) | 0.02 | 0.376 | 0.719 |
| IgE | 4 | 26% | 0.16 (−0.11, 0.43) | 0.24 | 3.307 | 0.081 |
| T cells | ||||||
| CD3+ T cells count | 22 | 88% | −1.14 (−1.41, −0.88) | <0.01 | −0.712 | 0.485 |
| CD4+ T cells count | 32 | 92% | −1.16 (−1.44, −0.89) | <0.01 | −2.857 | 0.008 |
| CD8+ T cells count | 32 | 89% | −1.03 (−1.27, −0.79) | <0.01 | −0.938 | 0.356 |
| CD4+CD25+CD127− Treg cells count | 4 | 0% | −0.45 (−0.76, −0.13) | <0.01 | 1.317 | 0.319 |
| CD3+ T cells ratio | 10 | 92% | −1.10 (−1.77, −0.42) | <0.01 | −3.268 | 0.012 |
| CD4+ T cells ratio | 10 | 85% | −0.61 (−1.02, −0.19) | <0.01 | −1.125 | 0.293 |
| CD8+ T cells ratio | 10 | 95% | −0.61 (−1.35, 0.12) | 0.10 | −3.784 | 0.005 |
| CD4+/CD8+ (Th/Ts) | 23 | 87% | 0.16 (−0.10, 0.42) | 0.23 | 0.575 | 0.571 |
| B cells, NK cells | ||||||
| CD19+B cells count | 17 | 86% | −0.74 (−1.05, −0.42) | <0.01 | 0.798 | 0.437 |
| CD16+CD56+NK cells count | 17 | 74% | −0.61 (−0.84, −0.38) | <0.01 | 0.664 | 0.517 |
| CD19+ B cells ratio | 8 | 0% | 0.35 (0.15, 0.55) | <0.01 | 0.113 | 0.913 |
| CD16+CD56+NK cells ratio | 9 | 95% | 0.19 (0.30, 2.07) | <0.01 | 5.821 | 0.001 |
| Neutrophils, monocytes, eosinophils and basophils | ||||||
| Neutrophils cells count | 114 | 91% | 0.72 (0.61, 0.82) | <0.01 | 1.590 | 0.115 |
| Neutrophils cells ratio | 25 | 96% | 0.62 (0.35, 0.88) | <0.01 | 0.793 | 0.436 |
| Monocytes cells count | 36 | 70% | −0.06 (−0.15, 0.04) | 0.24 | −1.148 | 0.259 |
| Monocytes cells ratio | 11 | 79% | −0.36 (−0.51, −0.21) | <0.01 | −0.418 | 0.686 |
| Eosinophils cells count | 19 | 62% | −0.45 (−0.59, −0.31) | <0.01 | 0.079 | 0.937 |
| Basophils cells count | 7 | 62% | −0.14 (−0.43, 0.15) | 0.34 | −1.332 | 0.254 |
Note: p*, p value for the variable in the forest plot analysis; p #: p value for the variable in the publication bias analysis.
Abbreviations: IFN‐γ, interferon γ; IL, interleukin; SMD, standardized mean difference; TNF‐α, tumour necrosis factor α.
3.8. Sensitivity analysis
The results showed that none of the exclusions altered the results of the previous analysis for cytokines (except for IL‐4 and IL‐10), four specific antibodies, T cells, B cells, NK cells (except for CD16+CD56+ NK cells ratio), neutrophils, monocytes, eosinophils and basophils, indicating the good reliability and stability of the results of this meta‐analysis (Figure S6). For IL‐4, one study by Hong et al. 35 had a strong influence on the result of the meta‐analysis. For IL‐10, Wan et al. 37 study had a strong influence on the result of the meta‐analysis. For CD16+CD56+ NK cells ratio, one study by Liu et al. 15 had a strong influence on the result of the meta‐analysis. However, the results of meta‐analysis were not badly altered to be the opposite.
3.9. Publication bias
The p value from Egger's regression and funnel plots suggested that the publication bias presented in seven mediators including IL‐2R, IL‐6, IL‐10, CD4+ T cells count, CD3+ T cells ratio, CD8+ T cells ratio and CD16+CD56+ NK cells ratio (Table S5 and Figure S7). Therefore, we adopted the trim‐and‐fill method to further test publication bias. As shown in Table S6, the results showed that there was no significant change in the pooled value change before (p < 0.05) and after (p < 0.05) trim‐and‐fill, indicating that the original pooled SMD was relatively robust.
4. DISCUSSION
Inflammation is the body's first coordinated line of defense against tissue damage caused by either injury or infection, involving both the innate and adaptive immune responses. 57 However, exuberant immune responses following infection have been frequently associated with excessive levels of pro‐inflammatory cytokines and widespread tissue damage including ARDS.158, 159, 160
In most previous studies, patients with SARS‐CoV‐2 infection are associated with a cytokine storm, which is characterized by increased production of IL‐2, IL‐7 and IL‐10, granulocyte‐colony stimulating factor, interferon‐α‐inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1 alpha and TNF‐α.16, 18, 157 However, there had been conflicting opinion as to whether the cytokine storm was responsible for the severe outcome. One argument was that the pathological process of severe COVID‐19 disease was mainly due to the direct lung injury that induced the subsequent ARDS, and respiratory depression. In addition to the virus‐induced direct lung injury, it is also considered that COVID‐19 invasion triggers the immune responses that lead to the activation of immune cells to release many pro‐ and anti‐inflammatory cytokines including TNF‐α, IL‐1β, IL‐6 and so on. Overwhelming secretion of cytokines causes severe lung damage, which manifest as extensive damage of pulmonary vascular endothelial and alveolar epithelial cells as well as increased pulmonary vascular permeability, leading to the pulmonary oedema and hyaline membrane formation.15, 25, 36, 66
Multiple studies have been conducted to characterize the profiles of immune mediator during different phases of the COVID‐19 disease in different geographic locations.43, 161, 162, 163 However, results varied, which might be due to the difference in clinical sample preparations, assay platforms and recursion criteria of the patients among studies. Here by performing meta‐analysis on studies that explored the association between cytokine storm and disease severity, we have determined that several cytokines, including IL‐2, IL‐2R, IL‐4, IL‐6, IL‐8, IL‐10 and IFN‐γ, were induced to significantly higher levels in severe cases than in non‐severe cases, but not for IL‐1β or TNF‐α.
It is notable that IL‐6 and IL‐10 were two of the cytokines that were most consistently enhanced in severe patients, and with large intergroup differences. The direction of association remained consistent in 20 of the 22 studies for IL‐6, and in all 13 studies for IL‐10. Extensive studies have been conducted to characterize the profile of IL‐6 in patients with SARS‐CoV‐2 infection, as well as for their relation with the clinical outcome.9, 10, 15, 23, 24, 25, 36, 37, 38, 39, 66 For example, IL‐6 was reported to be elevated during the acute phase of SARS‐CoV‐2 infection,9, 25, 26 and also associated with high viremia in COVID‐19 patients. The plasma IL‐6 level was increased dramatically in SARS‐CoV‐2‐infected patients with cardiac injury, which was associated with fatal outcome induced by fulminant myocarditis. 164 Significantly elevated systemic level of IL‐6 have been reported in several COVID‐19 patient cohorts and shown to correlate with disease severity. 165 IL‐6 level diverges profoundly between non‐survivors and survivors in the third week after symptom onset and is a predictor of COVID‐19 severity and in‐hospital mortality,15, 58 which suggest that IL‐6 production might play a more important role than viral burden in the pathogenesis COVID‐19, since high viral loads were observed at the early clinical process.65, 166, 167, 168 In a consistent manner, a study performed on medical staff with COVID‐19 disease in Wuhan disclosed normal IL‐6 levels on admission were favourable for discharge after infection. 169 Until now, there had been only two studies that showed a reversed direction for the IL‐6‐severe disease association according to our meta‐analysis.18, 42 All these evidences had supported a critical role of IL‐6 in determining the outcome. Transcriptional profiling found that SARS‐CoV‐2 infection in addition to activating type‐I interferon and IL‐6‐dependent inflammatory responses, also results in robust engagement of the complement and coagulation pathway activation. 170 As a simple, fast and readily available screen, we propose it reasonable to take an immediate evaluation of IL‐6 and IL‐10 levels upon hospital admission of COVID‐19 patients, due to its potential benefits to assess worsening clinical features and disease progression in COVID‐19. For example, a notably elevated IL‐6 value over a certain level by using a predetermined detection kit and following a standard protocol should alert clinicians to adopt aggressive therapeutic approaches without delay.
Accompanying the inflammatory process is the lymphopenia depressed CD4+, CD8+ T cells, NK and B cells in COVID‐19 patients. Studies found that acute SARS‐CoV‐2 infection resulted in broad immune cell reduction including T, NK, monocyte, and dendritic cells (DCs). 171 In the meta‐analysed studies, lymphopenia was ubiquitous in severe COVID‐19 infection and was associated with adverse outcome. CD3+, CD4+ and CD8+ T cells counts were always below normal range, and CD19+ B cells and CD16+56+ NK cells counts were consistently depressed in the severe versus non‐severe cases. Recently studies have shown that the extent of lymphopenia seemingly correlates with COVID‐19‐associated disease severity and mortality.2, 4, 24, 68, 70, 71, 172, 173, 174, 175 Patients with mild symptoms, however, typically present with normal or slightly higher T cell counts.176, 177 The presence of lymphopenia and depressed T cell counts seems to correlate with serum IL‐6, IL‐10 and TNF‐α, which might also act as a signature of severe COVID‐19.34, 70 SARS‐CoV‐2‐specific antibodies production in COVID‐19 patients suggested the mounting of humoral responses, especially with a higher level of IgA antibody in the severe patients. However, insignificant difference of IgG, IgM or IgE antibody between severe and non‐severe patients was observed. The role of adaptive immunity in COVID‐19 patients cannot be deciphered according to the current analysis.
These findings have potential application in the effective therapy choice. Until recently, anti‐viral drugs with proven safety profiles are lacking, thus targeting the hyper‐inflammation might be promising and critical for reducing mortality. For example, Tocilizumab, a monoclonal antibody targeting the IL‐6 receptor, is currently being investigated for the treatment of patients with COVID‐19‐CSS. 159 The approved randomized controlled trial that evaluates the efficacy and safety of tocilizumab in the treatment of COVID‐19 might bring about potential benefit soon. The lymphopenia plays an important role in the pathogenesis of the disease, thus the drugs targeting lymphocyte proliferation or apoptosis (IL‐7 and PD1/PD‐L1 inhibitors) could help to restore lymphocyte counts in severe patients suffering COVID‐19.
The recruited studies evaluated by NOQAS in the meta‐analysis revealed good quality, which provided the strong evidence for the association between immune signatures and SARS‐CoV‐2 infection. However, our study was subject to limitations that were inherent to meta‐analysis. All types of severe diseases, such as ARDS development, ICU entrance, the critical ill patients, were pooled into one for comparison. This broad range of severe disease, although been defined according to standard criteria, might cause bias away from the actual estimation of the association. However, with all association with these complications undoubtedly toward the same direction, we would consider these results adaptable for the disease severity prediction. Age and comorbidities are important risk determinants of severity and mortality of COVID‐19 patients, which effects however was not measured, as there were only few literatures presenting the subgrouping data on the immune signatures and disease severity, based on age or comorbidities. We also failed to consider the effect of therapy on the disease outcome, because most of the therapy information was missing from the included studies, for which further investigation are warranted.
5. CONCLUSION
Our systematic review and meta‐analysis are the first to reveal that multiple immune mediators were significantly associated with clinical outcome in COVID‐19 patients in a comprehensive way. A dysregulated immunological response with hypercytokinemia and lymphopenia assembled among severe COVID‐19 disease was disclosed. The screening for the currently significant biomarkers, especially cytokine of IL‐6, IL‐10 and the T cells counts, have important implication in assisting prompt recognition of severe patients and guiding early treatment.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
Wei Liu, Jing‐Yun Li and Qing‐Bin Lu conceived the idea. Tong Yang and Xue‐Fang Peng searched the studies. Kun Liu, Tong Yang, Xue‐Fang Peng, Shou‐Ming Lv, Tian‐Shuo Zhao, Xiao‐Lei Ye, Jia‐Chen Li and Zhong‐Jun Shao collected and analysed the data. Wei Liu and Kun Liu wrote the manuscript. All authors read and approved the final manuscript.
6.
Supporting information
Supplementary Material 1
Supplementary Material 2
Supplementary Material 3
Supplementary Material 4
Supplementary Material 5
Supplementary Material 6
Supplementary Material 7
Supplementary Material 8
Supplementary Material 9
Supplementary Material 10
Supplementary Material 11
Supplementary Material 12
ACKNOWLEDGEMENTS
We thank all medical staff and health practitioners who have contributed to fight against the disease of COVID‐19. This work was supported by the China Mega‐Project on Infectious Disease Prevention (No. 2018ZX10713002, 2018ZX10101003 and 2017ZX10103004), and the National Natural Science Foundation of China (81803289, 81825019). The funding agencies had no role in the study design, data collection and analysis, or preparation of the manuscript.
Liu K, Yang T, Peng X‐F, et al. A systematic meta‐analysis of immune signatures in patients with COVID‐19. Rev Med Virol. 2021;31(4):e2195. 10.1002/rmv.2195
Kun Liu and Tong Yang contributed equally to this study.
Contributor Information
Qing‐Bin Lu, Email: lwbime@163.com.
Jing‐Yun Li, Email: lwbime@163.com.
Wei Liu, Email: lwbime@163.com.
DATA AVAILABILITY STATEMENT
All data used for analysis are available upon a proper request from the corresponding author Wei Liu at lwbime@163.com.
References
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu J, Liu Y, Xiang P, et al. Neutrophil‐to‐lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Feng Z, Yu Q, Yao S, et al. Early prediction of disease progression in 2019 novel coronavirus pneumonia patients outside Wuhan with CT and clinical characteristics. medRxiv. 2020. [Google Scholar]
- 4. Tan L, Wang Q, Zhang D, Ding J, Miao H. Lymphopenia predicts disease severity of COVID‐19: a descriptive and predictive study. Signal Transduct Target Ther 2020;5:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou Y, Yang Z, Guo Y, et al. A new predictor of disease severity in patients with COVID‐19 in Wuhan, China. medRxiv. 2020. [Google Scholar]
- 6. Abu Raya B. Predictors of refractory coronavirus disease (COVID‐19) pneumonia. Clin Infect Dis. 2020;71:895‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID‐19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26:729‐734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rokni M, Ghasemi V, Tavakoli Z. Immune responses and pathogenesis of SARS‐CoV‐2 during an outbreak in Iran: comparison with SARS and MERS. Rev Med Virol. 2020;30:e2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID‐19 in Wuhan, China. Clin Infect Dis. 2020;71:762‐768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zheng M, Gao Y, Wang G, Song G, Tian Z. Functional exhaustion of antiviral lymphocytes in COVID‐19 patients. Cell Mol Immunol. 2020;17:533‐535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid‐19 patients. Science. 2020;369:718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen M, Tu C, Tan C, et al. Key to successful treatment of COVID‐19: accurate identification of severe risks and early intervention of disease progression. medRxiv. 2020. [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu T, Zhang J, Yang Y, Zhang L, Yi J. The potential role of IL‐6 in monitoring coronavirus disease 2019. medRxiv. 2020. [Google Scholar]
- 16. Nie S, Zhao X, Zhao K, Zhang Z, Zhang Z, Zhang Z. Metabolic disturbances and inflammatory dysfunction predict severity of coronavirus disease 2019 (COVID‐19): a retrospective study. medRxiv. 2020. [Google Scholar]
- 17. Shi Y, Tan M, Chen X, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. Immunology. 2020;160:261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Song C, Xu J, He J, Lu Y. COVID‐19 early warning score: a multi‐parameter screening tool to identify highly suspected patients. medRxiv. 2020. [Google Scholar]
- 19. Wu Y, Huang X, Sun J, et al. Clinical characteristics and immune injury mechanisms in 71 patients with COVID‐19. mSphere. 2020;5(4):e00362‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. He R, Lu Z, Zhang L, et al. The clinical course and its correlated immune status in COVID‐19 pneumonia. J Clin Virol. 2020;127:104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wei X, Su J, Yang K, et al. Elevations of serum cancer biomarkers correlate with severity of COVID‐19. J Med Virol. 2020;29:2036–2041. https://doi:10.1002/jmv.25957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhu Z, Cai T, Fan L, Lou K, Gao G. Clinical value of immune‐inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020;95:332‐339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen L, Liu H, Liu W, et al. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:203‐208. [DOI] [PubMed] [Google Scholar]
- 24. Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620‐2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen T, Wu D, Chen H, Yan W, Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li K, Chen D, Chen S, et al. Predictors of fatality including radiographic findings in adults with COVID‐19. Respir Res. 2020;21(1):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu Y, Liao W, Wan L, Xiang T, Zhang W. Correlation between relative nasopharyngeal virus RNA load and lymphocyte count disease severity in patients with COVID‐19. Viral Immunol. 2020. [DOI] [PubMed] [Google Scholar]
- 28. Zhang F, Xiong Y, Wei Y, Hu Y, Zhu W. Obesity predisposes to the risk of higher mortality in young COVID patients. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pei G, Zhang Z, Peng J, et al. Renal Involvement and early prognosis in patients with COVID‐19 pneumonia. J Am Soc Nephrol. 2020;31:1157‐1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hou H, Zhang B, Huang H, Luo Y, Sun Z. Using IL‐2R/lymphocyte for predicting the clinical progression of patients with COVID‐19. Clin Exp Immunol. 2020;201:76‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Huang H, Zhang M, Chen C, et al. Clinical characteristics of COVID‐19 in patients with preexisting ILD: a retrospective study in a single center in Wuhan, China. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 Intensive care patients with COVID‐19. Am J Respir Crit Care Med. 2020;201:1430‐1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang F, Hou H, Luo Y, Tang G, Sun Z. The laboratory tests and host immunity of COVID‐19 patients with different severity of illness. JCI Insight. 2020;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wan S, Yi Q, Fan S, et al. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP). medRxiv. 2020. [Google Scholar]
- 35. Hong KS, Lee KH, Chung JH, Shin KC, Ahn JH. Clinical features and outcomes of 98 patients hospitalized with SARS‐CoV‐2 infection in Daegu, South Korea: a brief descriptive study.Yonsei Med J. 2020;61:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cai Q, Huang D, Ou P, et al. COVID‐19 in a designated infectious diseases hospital outside Hubei province, China. Allergy. 2020;75(7):1742–1752. [DOI] [PubMed] [Google Scholar]
- 37. Gao Y, Li T, Han M, et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID‐19. J Med Virol. 2020;92:791‐796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID‐19 pneumonia in Wuhan, China. Clin Infect Dis. 2020;16:ciaa270. [Google Scholar]
- 39. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID‐19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Xiao K, Lili S, Pang X, et al. The clinical features of the 143 patients with COVID‐19 in North‐East of Chongqing. J Third Military Med Univ. 2020;42:549‐554. [Google Scholar]
- 41. Xu Y, Li Y‐r, Zeng Q, et al. Clinical characteristics of SARS‐CoV‐2 pneumonia compared to controls in Chinese Han population. medRxiv. 2020. [Google Scholar]
- 42. Zheng H, Zhang M, Yang C, et al. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID‐19 patients. Cell Mol Immunol. 2020;17:541‐543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhou F, Yu T, Du R, Fan G, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sun H, Ning R, Tao Y, Yu C, Xu D. Risk factors for mortality in 244 Older adults with COVID‐19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68:E19‐E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fan J, Wang H, Ye G, et al. Letter to the Editor: low‐density lipoprotein is a potential predictor of poor prognosis in patients with coronavirus disease 2019. Metab Clin Exp. 2020;107:154243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dong Y, Zhou H, Li M, et al. A novel simple scoring model for predicting severity of patients with SARS‐CoV‐2 infection. Transbound Emerg Dis. 2020;29. https://doi:10.1111/tbed.13651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sun Y, Dong Y, Wang L, Xie H, Wang FS. Characteristics and prognostic factors of disease severity in patients with COVID‐19: the Beijing experience. J Autoimmun. 2020;112:102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Li S, Jiang L, Li X, et al. Clinical and pathological investigation of patients with severe COVID‐19. JCI Insight. 2020;5(12):e138070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Burian E, Jungmann F, Kaissis GA, et al. Intensive care risk estimation in COVID‐19 pneumonia based on clinical and imaging parameters: experiences from the Munich cohort. J Clin Med. 2020;18:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gayam V, Chobufo MD, Merghani MA, Lamichanne S, Adler MK. Clinical characteristics and predictors of mortality in African‐Americans with COVID‐19 from an inner‐city community teaching hospital in New York. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chen F, Sun W, Sun S, Li Z, Wang Z, Yu L. Clinical characteristics and risk factors for mortality among inpatients with COVID‐19 in Wuhan, China. Clin Transl Med. 2020;10:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Xu J, Zhao F, Han M, Ma L, Zhang T. Analysis of the clinical characteristics and early warning model construction of severe/critical coronavirus disease 2019 patients. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32:401‐406. [DOI] [PubMed] [Google Scholar]
- 53. Xie Y, You Q, Wu C, Cao S, Zhang H. Impact of cardiovascular disease on clinical characteristics and outcomes of coronavirus disease 2019 (COVID‐19). Circ J. 2020;84:1277‐1283. [DOI] [PubMed] [Google Scholar]
- 54. Morrison AR, Johnson JM, Griebe KM, Jones MC, Smith ZR. Clinical characteristics and predictors of survival in adults with coronavirus disease 2019 receiving tocilizumab. J Autoimmun. 2020:102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wang R, Pan M, Zhang X, Fan X, Shen L. Epidemiological and clinical features of 125 hospitalized patients with COVID‐19 in Fuyang, Anhui, China. Int J Infect Dis. 2020;95:421‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zheng C, Wang J, Guo H, Lu Z, Xu Y. Risk‐adapted treatment strategy for COVID‐19 patients. Int J Infect Dis. 2020;94:74‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4‐week follow‐up. J Infect. 2020;80:639‐645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen X, Zhao B, Qu Y, et al. Detectable serum severe acute respiratory syndrome coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically ill Patients with coronavirus disease 2019. Clin Infect Dis. 2020;71(8):1937–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Liu J, Zhang S, Wu Z, et al. Clinical outcomes of COVID‐19 in Wuhan, China: a large cohort study. Ann Intensive Care. 2020;10:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Arunachalam P, Wimmers F, Mok C, et al. Systems biological assessment of immunity to mild versus severe COVID‐19 infection in humans. Science. 2020;369:1210‐1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wei YY, Wang RR, Zhang DW, Tu YH, Fei GH. Risk factors for severe COVID‐19: evidence from 167 hospitalized patients in Anhui, China. J Infect. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shi P, Ren G, Yang J, et al. Clinical characteristics of imported and second‐generation COVID‐19 cases outside Wuhan, China: a multicenter retrospective study. Epidemiol Infect. 2020;148:e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Xu B, Fan C, Wang A, et al. Suppressed T cell‐mediated immunity in patients with COVID‐19: a clinical retrospective study in Wuhan, China. J Infect. 2020;81:e51‐e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Pereira MR, Mohan S, Cohen DJ, Husain SA, Verna EC. COVID in solid organ transplant recipients: initial report from the US epicenter. Am J Transplant. 2020;20:1800‐1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Yang Y, Shen C, Li J, et al. Exuberant elevation of IP‐10, MCP‐3 and IL‐1ra during SARS‐CoV‐2 infection is associated with disease severity and fatal outcome. medRxiv. 2020. [Google Scholar]
- 66. Cao M, Zhang D, Wang Y, et al. Clinical features of patients infected with the 2019 novel coronavirus (COVID‐19) in Shanghai, China. medRxiv. 2020. [Google Scholar]
- 67. Han Y, Zhang H, Mu S, et al. Lactate dehydrogenase, an independent risk factor of severe COVID‐19 patients: a retrospective and observational study. Aging (Albany NY). 2020;12(12):11245–11258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Liu J, Li S, Liu J, et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS‐CoV‐2 infected patients. EBioMedicine. 2020;55:102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Fu Y, Sun Y, Lu S, Yang Y, Wang Y, Xu F. Effect of blood analysis and immune function on the prognosis of patients with COVID‐19. PLoS One. 2020;15(10):e0240751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Diao B, Wang C, Tan Y, Chen X, Chen Y. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID‐19). Front Immunol. 2020;11:827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Zeng Q, Li Y, Huang G, Wu W, Dong S, Xu Y. Mortality of COVID‐19 is associated with cellular immune function compared to immune function in Chinese Han population. medRxiv. 2020. [Google Scholar]
- 72. Zheng Y, Huang Z, Ying G, et al. Study of the lymphocyte change between COVID‐19 and non‐COVID‐19 pneumonia cases suggesting other factors besides uncontrolled inflammation contributed to multi‐organ injury. medRxiv. 2020. [Google Scholar]
- 73. Shi Q, Zhang X, Jiang F, et al. Clinical characteristics and risk factors for mortality of COVID‐19 patients with diabetes in Wuhan, China: a two‐center, retrospective study. Diabetes Care. 2020;43:1382‐1391. [DOI] [PubMed] [Google Scholar]
- 74. Liu R, Wang Y, Li J, Han H, Zhu C. Decreased T cell populations contribute to the increased severity of COVID‐19. Clin Chim Acta. 2020;508:110‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zhou Y, Zhang Z, Tian J, Xiong S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann Palliat Med. 2020;9:428‐436. [DOI] [PubMed] [Google Scholar]
- 76. Yang Y, Shen C, Li J, et al. Plasma IP‐10 and MCP‐3 levels are highly associated with disease severity and predict the progression of COVID‐19. J Allergy Clin Immunol. 2020;146:119‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yang P, Wang P, Song Y, Zhang A, Yuan G, Cui Y. A retrospective study on the epidemiological characteristics and establishment of an early warning system of severe COVID‐19 patients. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zheng Y, Xu H, Yang M, Zeng Y, Wang D. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID‐19 in Chengdu. J Clin Virol. 2020;127:104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Xie J, Ding C, Li J, Wang Y, He H. Characteristics of patients with coronavirus disease (COVID‐19) confirmed using an IgM‐IgG antibody test. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Huang S, Huang M, Li X, Zhang T, Lu H. Significance of neutrophil‐to‐lymphocyte ratio, platelet‐to‐lymphocyte ratio for predicting clinical outcomes in COVID‐19. medRxiv. 2020. [Google Scholar]
- 81. Huang R, Zhu L, Xue L, Liu L, Wu C. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: a retrospective, multi‐center study. PLoS Negl Trop Dis. 2020;14:e0008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Zhang N, Xu X, Zhou LY, Chen G, Sun Z. Clinical characteristics and chest CT imaging features of critically ill COVID‐19 patients. Eur Radiol. 2020;30(11):6151–6160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Li L, Yang L, Gui S, et al. Association of clinical and radiographic findings with the outcomes of 93 patients with COVID‐19 in Wuhan, China. Theranostics. 2020;10:6113‐6121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sun S, Cai X, Wang H, He G, Hu X. Abnormalities of peripheral blood system in patients with COVID‐19 in Wenzhou, China. Clin Chim Acta. 2020;507:174‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Qi X, Liu Y, Wang J, Fallowfield JA, Rockey DC. Clinical course and risk factors for mortality of COVID‐19 patients with pre‐existing cirrhosis: a multicentre cohort study. Gut. 2020;20:321666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Shang WF, Dong JW, Ren YL, et al. The value of clinical parameters in predicting the severity of COVID‐19. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Yip CY, Yap ES, Mel SD, Teo WZY, Lee SY. Temporal changes in immune blood cell parameters in COVID‐19 infection and recovery from severe infection. Br J Haematol. 2020;190:33‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zhao X, Wang K, Zuo P, et al. Early decrease in blood platelet count is associated with poor prognosis in COVID‐19 patients‐indications for predictive, preventive, and personalized medical approach. EPMA J. 2020;11:139‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wang D, Yin Y, Hu C, et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS‐CoV‐2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Yu T, Cai S, Zheng Z, Cai X, Xu X. Association between clinical manifestations and prognosis in patients with COVID‐19. Clin Ther. 2020;42:964‐972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Huang J, Cheng A, Kumar R, et al. Hypoalbuminemia predicts the outcome of COVID‐19 independent of age and co‐morbidity. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fu J, Kong J, Wang W, Wu M, Yu X. The clinical implication of dynamic neutrophil to lymphocyte ratio and D‐dimer in COVID‐19: a retrospective study in Suzhou China. Thromb Res. 2020;192:3‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lu H, Ai J, Shen Y, et al. A descriptive study of the impact of diseases control and prevention on the epidemics dynamics and clinical features of SARS‐CoV‐2 outbreak in Shanghai, lessons learned for metropolis epidemics prevention. medRxiv. 2020. [Google Scholar]
- 95. Liu L, Gao JY. Clinical characteristics of 51 patients discharged from hospital with COVID‐19 in Chongqing, China. medRxiv. 2020. [Google Scholar]
- 96. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Qian GQ, Yang NB, Ding F, et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID‐19 in Zhejiang, China: a retrospective, multi‐centre case series. QJM. 2020;113:474‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wang Y, Zhou Y, Yang Z, Xia D, Geng S. Clinical characteristics of patients with severe pneumonia caused by the SARS‐CoV‐2 in Wuhan, China. Respiration. 2020;99(8):649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Liang W, Liang H, Ou L, Chen B, He J. Development and validation of a clinical risk score to predict the Occurrence of critical illness in hospitalized patients with COVID‐19. JAMA Intern Med. 2020;180 (8):1081–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. De la Rica R, Borges M, Aranda M, et al. Low albumin levels are associated with poorer outcomes in a case series of COVID‐19 patients in Spain: a retrospective cohort study. Microorganisms. 2020;8(8):1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Xiong F, Tang H, Liu L, et al. Clinical characteristics of and medical Interventions for COVID‐19 in Hemodialysis patients in Wuhan, China. J Am Soc Nephrol. 2020;31:1387‐1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Huang JF, Cheng AG, Lin S, Zhu Y, Chen G. Individualized prediction nomograms for disease progression in mild COVID‐19. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Giacomelli A, Ridolfo AL, Milazzo L, Oreni L, Galli M. 30‐day mortality in patients hospitalized with COVID‐19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res. 2020;158:104931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Liu W, Tao Z, Wang L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133:1032‐1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID‐19 pneumonia. Invest Radiol 2020;55:327‐331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Ji M, Yuan L, Shen W, Lv J, Dong W. Characteristics of disease progress in patients with coronavirus disease 2019 in Wuhan, China. Epidemiol Infect. 2020;148:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Fan BE, Chong VCL, Chan SSW, et al. Hematologic parameters in patients with COVID infection. Am J Hematol. 2020;95:E131‐E134. [DOI] [PubMed] [Google Scholar]
- 108. Luo XM, Zhou W, Yan XJ, et al. Prognostic value of C‐reactive protein in patients with COVID‐19. Clin Infect Dis. 2020:ciaa641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Buckner FS, Mcculloch DJ, Vidya A, et al. Clinical features and outcomes of 105 hospitalized patients with COVID‐19 in Seattle, Washington. Clin Infect Dis. 2020:ciaa632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Wu G, Yang P, Xie Y, Woodruff HC, Lambin P. Development of a clinical decision support system for severity risk prediction and triage of COVID‐19 patients at hospital admission: an International multicenter study. Eur Respir J. 2020;56:2001104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Shi J, Li Y, Zhou X, Zhang Q, Zhang W. Lactate dehydrogenase and susceptibility to deterioration of mild COVID‐19 patients: a multicenter nested case‐control study. BMC Med. 2020;18:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Lee J, Hong S, Hyun M, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020;98:462‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Yu C, Lei Q, Li W, Wang X, Li W, Liu W. Epidemiological and clinical characteristics of 1663 hospitalized patients infected with COVID‐19 in Wuhan, China: a single‐center experience. J Infect Public Health. 2020;13(9):1202–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Chen X, Zheng F, Qing Y, et al. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double‐center observational study. medRxiv. 2020. [Google Scholar]
- 115. Cao Z, Li T, Liang L, Wang H, Jin R. Clinical characteristics of coronavirus disease 2019 patients in Beijing, China. PLoS One. 2020;15:e0234764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Zhang G, Hu C, Luo L, Fang F, Pan H. Clinical features and short‐term outcomes of 221 patients with COVID‐19 in Wuhan, China. J Clin Virol. 2020;127:104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Wang YP, Liao BL, Guo Y, et al. Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS‐Cov‐2) in Guangzhou, China. Open Forum Infect Dis. 2020;7:ofaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Liu C, Deng X, Pan Y, et al. Clinical characteristics and CT imaging features of patients with different clinical types of coronavirus disease 2019. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32:548‐553. [DOI] [PubMed] [Google Scholar]
- 119. Li J, Xu G, Yu H, Peng X, Cao CA. Clinical characteristics and outcomes of 74 patients with severe or critical COVID‐19. Am J Med Sci. 2020;360(3):229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Zhang SY, Lian JS, Hu JH, Zhang XL, Yang YD. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID‐19 in Zhejiang, China. Infect Dis Poverty. 2020;9:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Zhang H, Cao X, Kong M, et al. Clinical and hematological characteristics of 88 patients with COVID‐19. Int J Lab Hematol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Levy TJ, Richardson S, Coppa K, et al. Development and validation of a survival calculator for hospitalized patients with COVID‐19. medRxiv. 2020. [Google Scholar]
- 123. Myers L, Parodi S, Escobar G, Liu V. Characteristics of hospitalized adults with COVID‐19 in an Integrated health care system in California. JAMA. 2020;323(21):2195–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Ouyang YB, Yin J, Wang W, et al. Down‐regulated gene expression spectrum and immune responses changed during the disease progression in patients with COVID‐19. Clin Infect Dis. 2020:ciaa462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Gong J, Ou J, Qiu X, et al. A tool for early prediction of severe coronavirus disease 2019 (COVID‐19): a multicenter study using the risk nomogram in Wuhan and Guangdong, China. Clin Infect Dis. 2020;71(15):833–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID‐19 infection. EClinicalMedicine. 2020;21:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Wan SX, Xiang Y, Fang W, et al. Clinical features and treatment of COVID patients in northeast Chongqing. J Med Virol. 2020;92:797‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Feng Y, Ling Y, Bai T, Xie Y, Qu J. COVID‐19 with different severity: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201:1380‐1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Yang JK, Jin JM, Liu S, et al. New onset COVID‐19‐related diabetes: an indicator of mortality. Medrixv. 2020. [Google Scholar]
- 130. Bai X, Fang C, Zhou Y, et al. Deep learning for predicting COVID‐19 malignant progression. Medrixv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Yan S, Song X, Lin F, et al. Clinical characteristics of coronavirus disease 2019 in Hainan, China. medRxiv. 2020. [Google Scholar]
- 132. Wang ZH, Li HJ, Li JJ, et al. Elevated serum IgM levels indicate poor outcome in patients with coronavirus disease 2019 pneumonia: a retrospective case‐control study. Medrixv. 2020. [Google Scholar]
- 133. Huang H, Cai S, Li Y, et al. Prognosticfactors for COVID‐19 pneumonia progression to severe symptoms based on earlier clinical features: a retrospective analysis. Front Med (Lausanne). 2020;7:557453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Lo IL, Lio CF, Cheong HH, Lei CI, Sin NN. Evaluation of SARS‐CoV‐2 RNA shedding in clinical specimens and clinical characteristics of 10 patients with COVID‐19 in Macau. Int J Biol Sci. 2020;16:1698‐1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Xie H, Zhao J, Lian N, Lin S, Zhuo H. Clinical characteristics of non‐ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. 2020;40:1321‐1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Du RH, Liu LM, Yin W, Wang W, Shi HZ. Hospitalization and critical care of 109 decedents with COVID‐19 pneumonia in Wuhan, China. Ann Am Thorac Soc. 2020;17:839‐846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Feng Z, Li J, Yao S, et al. The use of adjuvant therapy in preventing progression to severe pneumonia in patients with coronavirus disease 2019: a multicenter data analysis. medRxiv. 2020. [Google Scholar]
- 138. Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID‐19 pneumonia caused by SARS‐CoV‐2: a prospective cohort study. Eur Respir J. 2020;55:2000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Zhang R, Ouyang H, Fu L, et al. CT features of SARS‐CoV‐2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. 2020;30:4417‐4426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Jiang X, Tao J, Wu H, et al. Clinical features and management of severe COVID‐19: a retrospective study in Wuxi, Jiangsu Province, China. medRxiv. 2020. [Google Scholar]
- 141. Wang C, Deng R, Gou L, et al. Preliminary study to identify severe from moderate cases of COVID‐19 using combined hematology parameters. Ann Transl Med. 2020;8(9):593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Chen W, Li Z, Yang B, et al. Delayed‐phase thrombocytopenia in patients with coronavirus disease 2019 (COVID‐19). Br J Haematol. 2020;190(2):179–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Xie G, Ding F, Han L, Yin D, Lu H, Zhang M. The role of peripheral blood eosinophil counts in COVID patients. Allergy. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Yang AP, Liu J, Tao W, Li HM. The diagnostic and predictive role of NLR, d‐NLR and PLR in COVID‐19 patients. Int Immunopharmacol. 2020;84:106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Brill SE, Jarvis HC, Ozcan E, Burns TLP, Creer DD. COVID‐19: a retrospective cohort study with focus on the over‐80s and hospital‐onset disease. BMC Med. 2020;18:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Yao Q, Wang P, Wang X, Qie G, Chu Y. Retrospective study of risk factors for severe SARS‐Cov‐2 infections in hospitalized adult patients. Polskie Archiwum Medycyny Wewntrznej. 2020. [DOI] [PubMed] [Google Scholar]
- 147. Zhang J, Ding D, Cao C, et al. Myocardial characteristics as the prognosis for COVID‐19 patients. medRxiv. 2020. [Google Scholar]
- 148. Sun L, Shen L, Fan J, et al. Clinical features of patients with coronavirus disease 2019 from a designated hospital in Beijing, China. J Med Virol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Shaobo S, Mu Q, Yuli C, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41:2070‐2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Yang Q, Xie L, Zhang W, Zhao L, Wu J. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. 2020;45:609‐616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Tao Y, Cheng P, Chen W, et al. High incidence of asymptomatic SARS‐CoV‐2 infection, Chongqing, China. medRxiv. 2020. [Google Scholar]
- 152. Chen QQ, Zheng ZC, Zhang C, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID‐19) in Taizhou, Zhejiang, China. Infection. 2020;48:543‐551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Cheng Y, Zhou Y, Zhu M, et al. Eosinopenia phenotype in patients with coronavirus disease 2019: a multi‐center retrospective study from Anhui, China. medRxiv. 2020. [Google Scholar]
- 154. Wei Y, Zeng W, Huang X, et al. Clinical characteristics of 276 hospitalized patients with coronavirus disease 2019 in Zengdu District, Hubei Province: a single‐center descriptive study. BMC Infect Dis. 2020;20:549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Chang H, Sung C, Lin M. Serum lipids and risk of atherosclerosis in xanthelasma palpebrarum: a systematic review and meta‐analysis. J Am Acad Dermatol. 2019;82:596‐605. [DOI] [PubMed] [Google Scholar]
- 157. Tan M, Liu Y, Zhou R, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. Immunology. 2020;160:261‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. D'Elia R, Harrison K, Oyston P, Lukaszewski R, Clark G. Targeting the ‘cytokine storm’ for therapeutic benefit. Clin Vaccine Immunol. 2013;20:319‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Ben Salem C. Acute respiratory distress syndrome. N Engl J Med. 2017;377:1904. [DOI] [PubMed] [Google Scholar]
- 160. Thompson B, Chambers R, Liu K. Acute respiratory distress syndrome. N Engl J Med. 2017;377:562‐572. [DOI] [PubMed] [Google Scholar]
- 161. Yu L, Tong Y, Shen G, et al. Immunodepletion with hypoxemia: a potential high risk subtype of coronavirus disease 2019. medRxiv. 2020. [Google Scholar]
- 162. Zhang B, Zhou X, Zhu C, et al. Immune phenotyping based on the neutrophil‐to‐lymphocyte ratio and IgG level predicts disease severity and outcome for patients With COVID‐19. Front Mol Biosci. 2020;7:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of coronavirus 2019 (COVID‐19) pneumonia with other pneumonias. Clin Infect Dis. 2020;71:756‐761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Chen C, Zhou Y, Wang D. SARS‐CoV‐2: a potential novel etiology of fulminant myocarditis. Herz. 2020;45:230‐232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Mehta P, McAuley D, Brown M, Sanchez E, Tattersall R, Manson J. COVID‐19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033‐1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Zou L, Ruan F, Huang M, et al. SARS‐CoV‐2 viral load in Upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177‐1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Pan Y, Zhang D, Yang P, Poon LLM, Wang Q. Viral load of SARS‐CoV‐2 in clinical samples. Lancet Infect Dis. 2020;20:411‐412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. To KW, Tsang TY, Leung WS, Tam AR, Yuen KY. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS‐CoV‐2: an observational cohort study. Lancet Infect Dis. 2020;20:565‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Liu J, Ouyang L, Guo P, et al. Epidemiological, clinical characteristics and outcome of medical staff infected with COVID‐19 in Wuhan, China: a retrospective case series analysis. medRxiv. 2020. [Google Scholar]
- 170. Ramlall V, Thangaraj P, Meydan C, et al. Immune complement and coagulation dysfunction in adverse outcomes of SARS‐CoV‐2 infection. Nat Med. 2020;26(10):1609–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Zhou R, To K, Wong Y, et al. Acute SARS‐CoV‐2 infection Impairs dendritic cell and T cell responses. Immunity. 2020;53(4):864–877.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Wang F, Nie J, Wang H, et al. Characteristics of peripheral lymphocyte Subset alteration in COVID‐19 pneumonia. J Infect Dis. 2020;221:1762‐1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Wang W, He J, Lie p, et al. The definition and risks of cytokine release syndrome‐Like in 11 COVID‐19‐infected pneumonia critically ill patients: disease characteristics and retrospective analysis. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Zhou Y, Fu B, Zheng X, et al. Pathogenic T‐cells and inflammatory monocytes incite inflammatory storms in severe COVID‐19 patients. Natl Sci Rev 2020;7:998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Vabret N, Britton G, Gruber C, et al. Immunology of COVID‐19: current state of the science. Immunity. 2020;52:910‐941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Thevarajan I, Nguyen T, Koutsakos M, et al. Breadth of concomitant immune responses prior to patient recovery: a case report of nonsevere COVID‐19. Nat Med. 2020;26:453‐455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Liu B, Han J, Cheng X, et al. Persistent SARS‐CoV‐2 presence is companied with defects in adaptive immune system in nonsevere COVID‐19 patients. medRxiv. 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1
Supplementary Material 2
Supplementary Material 3
Supplementary Material 4
Supplementary Material 5
Supplementary Material 6
Supplementary Material 7
Supplementary Material 8
Supplementary Material 9
Supplementary Material 10
Supplementary Material 11
Supplementary Material 12
Data Availability Statement
All data used for analysis are available upon a proper request from the corresponding author Wei Liu at lwbime@163.com.


