Abstract
Background:
The purpose of this systematic review is to examine cooling intervention research in outdoor occupations, evaluate the effectiveness of such interventions, and offer recommendations for future studies. This review focuses on outdoor occupational studies conducted at worksites or simulated occupational tasks in climatic chambers.
Methods:
This systematic review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. PubMed, Embase, and Web of Science were searched to identify original research on intervention studies published in peer-reviewed journals that aimed at reducing heat stress or heat-related illness from January 2000 to August 2020.
Results:
A systematic search yielded a total of 1042 articles, of which 21 met the inclusion criteria. Occupations with cooling intervention studies included agriculture (n = 5), construction (n = 5), industrial workers (n = 4), and firefighters (n = 7). The studies focused on multiple types of cooling interventions cooling gear (vest, bandanas, cooling shirts, or head-cooling gel pack), enhanced heat dissipation clothing, forearm or lower body immersion in cold water, water dousing, ingestion of a crushed ice slush drink, electrolyte liquid hydration, and modified Occupational Safety and Health Administration recommendations of drinking water and resting in the shade.
Conclusion:
Current evidence indicates that using multiple cooling gears along with rest cycles may be the most effective method to reduce heat-related illness. Occupational heat-related illnesses and death may be mitigated by targeted cooling intervention and workplace controls among workers of vulnerable occupational groups and industries.
Keywords: cooling interventions, heat-related illness, occupational health
1 |. INTRODUCTION
Outdoor workers, especially those with physically demanding jobs that expose them to increasingly hot temperatures, are identified as occupational groups at increased risk of heat stress and heat-related illness (HRI) associated with climate change.1 Heat stress is the net heat load a worker is exposed to from combined factors such as metabolic heat, environmental factors, and clothing worn that contribute to increased heat storage in the body.2 Exposure to a hot environment for a prolonged period while working can result in the body’s inability to cool itself, causing an elevation of heat strain and in severe cases, death. HRI is a preventable condition that exists along a continuum from less severe signs and symptoms, such as muscle cramps to heat exhaustion, and heat stroke.3
A systematic review, including 111 studies conducted in 30 countries, found that working in hot environments increases the likelihood of experiencing occupational HRI and has negative effects on health and productivity.4 The risk of heat-related mortality in agricultural workers is 35 times greater than the general workforce population5 followed by construction workers who are 13 times more at risk of heat-related mortality compared with workers in other industries.5 Both occupational groups are exposed to increasingly hotter temperatures due to climate change and thus are especially vulnerable. While there is much descriptive research on the prevalence and risk of HRI among occupational groups, less work has been published on interventions to decrease the risk of HRI.
The United States Occupational Safety and Health Administration (OSHA) launched a Heat Illness Prevention campaign in 2011.6 The campaign focused on raising awareness about the hazards of working outdoors in hot weather and to encourage workers to take precautions. OSHA has also published the OSHA Technical Manual (OTM) that provides technical information about heat hazards, illnesses, and prevention methods.7 The primary safety recommendations are to drink water and rest in the shade with a simple message Water. Rest. Shade. OSHA recommends outdoor workers drink eight ounces of water every 20 min and drink electrolyte-containing beverages. For rest breaks, OSHA generally recommends resting every hour and taking a long enough rest break for a worker to recover from HRI or prevent HRI. Rest breaks should take place in a shaded area such as under a tent or canopy, or in an air-conditioned automobile or building. While drinking water and resting in the shade along with increased worker knowledge of heat hazards are essential to prevent HRI, heat-related morbidity and mortality rates remain high for vulnerable occupational groups. Additional studies are needed to ascertain the effectiveness of interventions that may augment the beneficial effects of drinking water and resting in the shade.
Systematic reviews of cooling intervention studies have analyzed controlled exercise trials in climatic chambers, typically with athletes running on treadmills, cycling, or other types of aerobic exercises.8,9 Cooling interventions with athletes have focused on the effects of cooling before an exercise test to create a larger heat storage capacity.8,10 The number of studies of cooling interventions with athletes during an exercise test has recently grown, examining methods such as cooling vests, neck cooling, ingestion of cold fluids or ice slurries, menthol cooling, and water spray cooling.10 The results of these cooling interventions during exercise trials have been mixed with one meta-analysis10 reporting that ingestion of cold fluids or ice slurries, followed by the use of cooling vests, is the most effective at improving exercise performance in hot ambient temperature. Another analysis reported unclear effects on biological indicators of heat strain while using cooling interventions during exercise trials.9 However, studies of athletes are difficult to generalize or apply to outdoor occupational groups with varying physical movements, exertion, and environmental conditions. Thus, little is known about cooling interventions in occupational settings, and field studies are needed to validate the effectiveness and practicality of cooling interventions in outdoor occupational groups.
The purpose of this paper is to review previous cooling intervention research in outdoor occupations, evaluate the effectiveness of such interventions, and offer recommendations for future studies. The focus on cooling intervention on outdoor occupations, in particular, is to preserve focus on protecting the health of workers in light of projected increases in the frequency of heat waves and severity due to climate change. This comprehensive review of the literature focuses on outdoor occupational studies conducted at worksites or simulated occupational tasks in climatic chambers.
2 |. METHODS
This systematic review was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.11 PubMed, Embase, and Web of Science were searched to identify original research on intervention studies published in peer-reviewed journals that aimed at reducing heat stress or HRI (see Table 1). Search terms included a combination of words and closely related words “heat stress,” “heat strain,” “heat stroke,” “heat-related illness,” “body temperature changes,” “occupational, outdoors,” “manual labor,” “cooling intervention,” and “heat intervention.” Additional search terms are outlined in Table S1.
TABLE 1.
Definitions
| Term | Definition |
|---|---|
| Heat stress | The net heat load a worker is exposed to from the combination of metabolic heat, environmental factors, and clothing worn2 |
| Heat strain | The overall physiological response resulting from heat stress2 |
| Heat-related illnesses (HRI) | Conditions that exist along a continuum from less severe illnesses, such as muscle cramps to heat exhaustion, and heat stroke3 |
| Physiological strain index (PSI) | An index that evaluates heat strain based on physiological parameters of heart rate and rectal temperature, that depicts the combined strain reflected by the cardiovascular and thermoregulatory systems. The index ranges from 0 to 10, where “0” presents no strain and “10” very strenuous physiological conditions12 |
| Perceptual strain index (PeSI) | Measures the thermal strain in individuals through the thermal sensation (TS) and the Rating of Perceived Exertion (RPE)13 |
| Rated perceived exertion (RPE) | A scale that measures the perceived intensity of physical exertion14 |
| Thermal sensation (TS) | Perceived temperature sensation related to skin and ambient air temperature15 |
The initial search was limited to studies published in the English language from January 2000 to May 2019. The electronic database search was updated on 14 August 2020 to include studies through August 2020. We limited our search for studies published since 2000 to provide an overview of current scientific knowledge and the current direction in the field of inquiry and to avoid unnecessary descriptions of studies whose relevance has decreased over time. Studies with adult humans participating in cooling interventions at occupational worksites outdoors or simulated occupational tasks in climatic chambers were included. The focus was on outdoor environmental and occupational heat exposure and cooling interventions to prevent HRI. Outcomes of focus were dehydration, body temperature, heart rate (HR), physiological strain index (PSI), HRI symptoms, and subjective measures. Dehydration (urine specific gravity [USG]), body temperature measurements, HR, and PSI are physiological indicators of heat strain on the human body. We excluded animal studies, indoor heat exposure, or exercise trials in climatic chambers. Studies with indoor occupations or exercise trials in climatic chambers were excluded as these are difficult to generalize to outside occupational groups with different environmental heat exposures, and physical movements during exercise trials vary from the physical movement at work. Case reports, editorial letters, case series studies, and intervention studies without a comparison group were also excluded.
All searches were conducted by author R. C. and collated using Endnote software (Thomas Reuters, New York), and duplicates were removed. All titles and abstracts from the literature search were evaluated according to the above inclusion criteria (R. C.). All full-text articles were assessed independently for eligibility by two authors (R. C./N. X.) according to the inclusion criteria. The selection of articles included was reviewed by the remaining authors.
3 |. RESULTS
A systematic search of PubMed, Embase, and Web of Science yielded a total of 1042 articles published from January 2000 to August 2020. There were 259 duplicate articles removed. After removing duplicates, 783 articles were eligible for a preliminary title and abstract screening. After screening titles and abstracts, 32 full-text articles were reviewed and 11 were removed for not meeting inclusion criteria. A total of 21 peer-reviewed papers met the inclusion criteria and were selected to be part of this review (see Table 2). A summary of the PRISMA protocol and reasons for excluding articles are shown in Figure 1.
TABLE 2.
Characteristics of cooling intervention studies of outside occupational groups (n = 21)
| Authors (year) | Occupation/sample size | Study design | Intervention | Tc | HR | PSI or PeSI | Hydration/renal | HRI symptoms | Subjective evaluations |
|---|---|---|---|---|---|---|---|---|---|
| Water, Rest, and Shade | |||||||||
| Bodin et al.16 | Agriculture | Nonrandomized | H2O (3 L backpack) | NR | NR | NR | NR | Decrease symptoms reported in coastland intervention group | Workers reported positive comments about resting in the shade, improved work satisfaction, and productivity |
| n = 60 | Worksites over harvest period | Rest (15 min/h) Shade (canopy) | |||||||
| Butler-Dawson et al.19 | Agriculture | Nonrandomized | H2O (~16 L) | NR | NR | NR | Higher electrolyte solution intake was associated with lower odds of developing an AKI (OR 0.94, 95% CI, 0.89–0.99) | NR | NR |
| n = 517 | Worksites over harvest period | Electrolyte solution | |||||||
| Three 20-min breaks + 60-min lunch | |||||||||
| Shade wellness incentive | |||||||||
| Glaser et al.18 | Agriculture | Nonrandomized | Enhanced and more evenly distributed scheduled rests Shade tents | NR | NR | NR | eGFR decline lessened from harvest #1 (−9 [−12 to −7]) to harvest #2 (−4 [−6 to −1]) | NR | Self-reported increase in water and electrolyte solution intake in harvest period #2 |
| Harvest #1 n = 427 | Worksites over harvest period | Improve fluid taste | |||||||
| Harvest #2 n = 488 | Electrolyte solution | ||||||||
| Wegman et al.17 | Agriculture | Nonrandomized | H2O (3 L backpack) | NR | NR | NR | Smaller decrease in eGFR: −3.4 ml/min/1.73m2 (95% CI, −5.5 to −1.3) | NR | NR |
| n = 80 | Worksites over harvest period | Rest (15 min/h) | |||||||
| Shade (canopy) | |||||||||
| Antiheat stress uniform | |||||||||
| Chan et al.22 | Constructio | Randomized | Antiheat stress work uniform: Coolmax collar shirt in light blue and Nano-tex Dry-inside fabric in khaki color | NR | NR | NR | NR | NR | Improved work performance by over 35% |
| n = 184 | Worksite 2 work days | ||||||||
| Control/intervention | |||||||||
| Yang and Chan23 | Construction | Randomized | Antiheat stress work uniform: Shirt (65% cotton and 35% polyester) and pants (100% cotton) | NR | No difference | PeSI 4.47 ± 1.8- 5 for Intervention vs. 4.78 ± 1.8- 2 for Control, (p < .05) | NR | NR | Improved comfort and less work performance interference |
| n = 16 | Worksite135-min of wear trial | ||||||||
| Cooling devices | |||||||||
| Ashtekar et al.25 | Construction | Nonrandomized | Vest - liquid ice-chilled coolant recirculated via a small battery-operated motor pump | Nodifference | HR 89.7 ± 34.- 3 (p < .05) | NR | NR | NR | Cooling vest kept them comfortable and cool |
| n = 29 | Worksites 210 min = 90-min intervention, 30-min rest, and 90-min control | ||||||||
| Butts et al28 | Industrial | Randomized Counter-balanced | Compression clothing with phase change materials (PCM) inserts | Intervention group lower rectal temperature (p < .05) | HR lower in intervention group (p < .05) | PSI lower in intervention group (p < .05) | NR | NR | Rate of perceived exertion lower with PCM (p < .05) |
| n = 20 | Industrial simulated work in climatic chamber 85 min (30 min spent resting) | ||||||||
| Chan et al.31 | Construction | No report of randomization | Hybrid cooling vest with PCM with ventilation fans | NR | HR mean 5.64 ± 7.8- 3 (p < .001) BPM lower | PeSI scores improved group (p < .001) | NR | NR | 91% preferred PCM cooling vest as method for cooling during rest time |
| n = 140 | Worksites; Vest worn at 15-min break in the am and 30-min break in the pm | ||||||||
| Furtado et al.27 | Industrial | Simulated work outdoors - 3–30 min trials | Randomized | Tympanic temperature lower (p = .003). | No difference | NR | NR | NR | Higher productivity with cooling suit vs. no cooling suit (p = .011) |
| n = 12 | Cooling suit - liquid ice-chilled coolant recirculated via a small battery-operated motor pump | ||||||||
| Shirish et al.26 | Foundry | Work site 90-min intervention and 90-min control 75% work-25% rest each hour | Non-randomized | Nodifference | No difference | NR | NR | NR | Mean score of 4.5 out of 5 points in comfort, efficacy and efficiency |
| n = 24 | Vest - liquid ice-chilled coolant recirculated via a small battery-operated motor pump | ||||||||
| Zhao et al.20 | Construction | Randomized counterbalance order | Cooling vest with PCM with ventilation fans | Lower estimated core temperature (F = 17.95, p < .01) | HR lower (F = 16.01, p < .01), | PSI statistically lower | NR | NR | Thermal comfort was significantly better p < .05 |
| n = 14 | Worksite Vest worn at 15-min break in the am and 30-min break in the pm | ||||||||
| Water immersion | |||||||||
| Burgess et al.37 | Firefighters | Randomized | Postfire forearm immersion in 10°C water for 15 min in 32.5°C ambient temperature. | Rate of core temperature decrease 0.28°C (95% CI, 0.06–0.50) | Rate of HR decrease by 19.4 (95% CI, 12.0–26.8) BPM | NR | NR | NR | NR |
| n = 50 | Live-fire drill 12 min | ||||||||
| Nutritional cooling | |||||||||
| Horn et al.39 | Firefighters | Randomized | Consumed 500 ml of water, 355 ml sport drink, 355 ml of recovery drink, and applied cold towels during 15-min rehabilitation period | Nodifference | No difference | NR | NR | NR | NR |
| n = 23 | Live-fire drill 18 min | ||||||||
| Water poured on head and hands | |||||||||
| Fujii et al.40 | Steel workers | Randomized | 2 L of water at 23.5°C, poured on the head and hands every hour | No difference | No difference | NR | NR | One report of limb fatigue during intervention days | Tiredness statistically lower in the intervention group (p < .05). |
| n = 8 | Worksite of 4 days = 2 days intervention, 2 days control | ||||||||
| Multiple cooling | |||||||||
| Carter et al.33 | Firefighters | Randomized | During simulation PCM cooling vest worn. Postsimulation forearms immersed in cold water (10°C) for 20 min | No difference | No difference | NR | NR | NR | No difference in RPE or TS |
| n = 10 | 3 Trials of simulated fire and rescue activities 20–88 min | ||||||||
| Choi et al.24 | Agriculture | Randomized |
1. Control 2. Scarf A 3. Scarf B 4. Hat 5. Vest 6. Hat + scarf B 7. Hat + vest 8. Hat + scarf B + vest |
Combination groups did not have rectal temperatures ≥ 38°C | No difference | Heat storage was significant better in the intervention groups than the control group | NR | NR | 80% reported all cooling gear was “comfortable” or “a little uncomfortable” |
| n = 12 | Simulated agricultural work in climatic chamber 120 min = two bouts of 50-min harvest work with a 10-min rest | Group 4, 5, 6, 7, and 8 had significantly lower rectal temperature than groups 1, 2, and 3 | |||||||
| Colburn et al.36 | Firefighters | Randomized | 30-min recovery period using a cooling vest, forearm immersion in water (20°C), or passive cooling in 22°C room | Forearm water immersion provided better rate of cooling (p = .036) | No difference | NR | NR | NR | NR |
| n = 25 | Live-fire drill 20 min | ||||||||
| Hemmatjo et al.34 | Firefighters | Randomized |
1. No cooling device 2. Cooling gel containing menthol 3. PCM cooling vest 4. Cooling gel and PCM cooling vest |
Temporal temperature significantly lower for the PCM cooling vest group (p < .05) | HR significantly lower for the PCM cooling vest group (p < .05) | NR | NR | NR | NR |
| n = 15 | Simulated firefighting activities in smoke-diving room 45–50 min | ||||||||
| Yeargin et al. 21 | Firefighters | Randomized | Head-cooling gel pack in helmet during simulation, or forearm-cooling in 5°C water during 15-min recovery period. | Forearm cooling had better rate of lowering CT compared with control group (−1.61°C vs. −0.23°C; p < .001) | No difference | Forearm cooling had lower PSI (−7.9) versus (−2.6) in the control group | NR | NR | NR |
| n = 38 | Four 15-min simulated fire drills | ||||||||
| Walker et al.38 | Firefighter | Randomized | Lower body immersed in coldwater 15°C or ingestion of 7 g/kg of body weight crushed ice slush drink (−1°C) during 15-min recovery session (19°C). | CT significantly lower in coldwater immersion (−0.5°C, 95% CI, −1.0 to 0.0) and crushed ice slush drink (−0.5°C 95% CI, −0.9 to −0.2) groups compared with control | NR | NR | NR | NR | No difference in RPE |
| n = 74 | Two 20-min fire drills in climatic chamber |
Abbreviations: AKI, acute kidney injury; BPM, beat per minute; CI, confidence interval; eGFR, estimated glomerular filtration rate; HR, hazard ratio; HRI, heat-related illness; NR, not reported; OR, odds ratio; PeSI, perceptual strain index; PSI, physiological strain index; RPE, Rated perceived exertion; TS, thermal sensation.
FIGURE 1.
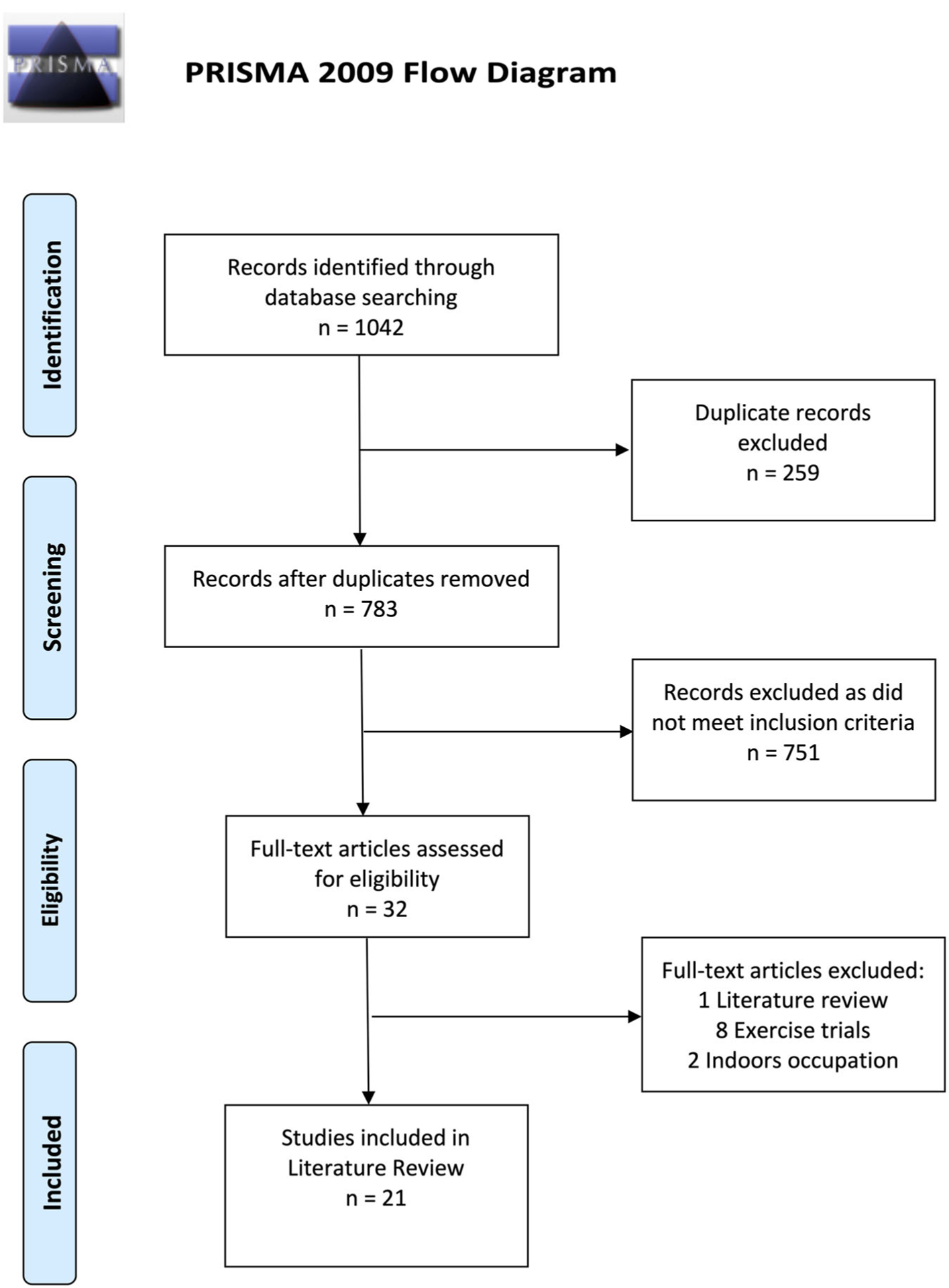
PRISMA flow diagram of study selection. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Studies with a variety of cooling interventions, protocols used, and health outcomes were included in this review. Most studies were conducted in the USA (n = 6, 29%) followed by China (n = 4, 19%), and India (n = 2, 10%). One study in El Salvador resulted in two publications, one examining the outcomes of dehydration, HRI symptoms, and productivity, while the second paper examined estimated glomerular filtration rate (eGFR).16,17 In Guatemala and Nicaragua, enhanced measures to prevent heat stress were implemented to assess renal health outcomes in agricultural workers.18,19 The United Kingdom, Korea, Brazil, Iran, and Australia each had one published cooling intervention study. Randomization assignment of the intervention was used in 15 (71%) studies.
Occupations with cooling intervention studies included agriculture (n = 5), construction (n = 5), industrial workers (n = 4), and firefighters (n = 7). Only five studies enrolled female workers, though with a small proportion of females compared to mostly male workers. The studies focused on multiple types of cooling interventions cooling gear (vest, bandanas, cooling shirts, or head-cooling gel pack), enhanced heat dissipation clothing, forearm or lower body immersion in cold water, water dousing, ingestion of a crushed ice slush drink, electrolyte liquid hydration, and modified OSHA recommendations of drinking water and resting in the shade.
Biological indicators of heat stress such as body temperature, HR, and PSI were measured, though only two studies measured all three indicators.20,21 Two studies did not record objective measures of body temperature, HR, or PSI.16,17,22,22,23 The remaining studies had a combination of objective and/or subjective measures of heat stress. Body temperature was assessed via oral, rectal, or tympanic thermometers, or ingestible sensors. HR was measured primarily with a chest strap monitor.
All firefighter cooling intervention studies (n = 7) were done during simulated fire-drills on field training sites, which is part of normal training for firefighters. Participants in firefighter studies wore their full personal protective equipment and self-contained breathing apparatus. Of the remaining occupational sector jobs, nine of the 12 studies were conducted at the worksite, while three were conducted in a climatic chamber simulating work activity.
Longitudinal intervention studies have been conducted in Central America over an agricultural harvest period.16–19 In contrast, four of the 16 studies at worksites examined cooling interventions on one to four workdays. Among the agricultural, construction, and industrial cooling interventions studies, five of the trials were 2 h or less.24–28 Due to the nature of the extreme heat exposure (82–309°C) firefighters encounter, those trials were less than 2 h.
The majority of the cooling intervention studies included a modified OSHA work-to-rest ratio protocol that was adhered to both in climatic chambers and at worksites. Firefighter studies all included a recovery period at the end of the fire drills. The time range of the fire drills ranged from 12 to 88 min with heat exposure ranging from 82°C to 309°C. The recovery period in three of the studies was 15 min, while a study in the United Kingdom had a recovery period of 20 min, and another study in the USA provided 30 min of recovery. The minimum industry standard is a 10-min recovery period.29
3.1 |. Water, Rest, Shade
In El Salvador, a longitudinal study over a harvest period implemented modified recommendations from OSHA’s Water, Rest, Shade guidelines.16,17 The authors measured serum creatinine to calculate eGFR, an indicator of kidney function, using the Chronic Kidney Disease Epidemiology Collaboration. Originally the investigators planned on implementing the modified OSHA recommendations with two groups of workers in coastal low-lands where ambient temperatures and humidity are high, and among inland workers who are exposed to less severe climatic conditions. Due to security concerns the investigators were unable to test the intervention in the coastal group. Agricultural workers (n = 41) in the inland area began the interventions two months into a 5-month harvest by wearing 3-L backpacks with water to drink from while working. They were instructed to rest 15 min every hour in a shaded canopy that was moved through the field, and they used an ergonomic machete for cutting sugarcane. While a strength of the study was a longitudinal design to study the effectiveness of the intervention, there was no inland area control group nor a comparison group in the coastal area. However, workers reported less HRI symptoms and increased self-reported water consumption at postintervention compared with preintervention.16
Wegman et al.17 reported on the effect of the intervention on biomarkers of dehydration and kidney damage. At the end of the harvest, the intervention group (located inland) showed a decline in eGFR of −3.4 ml/min/1.73m2 (95% CI −5.5, −1.3) from baseline levels. The investigators compared this drop in renal function to the group of workers in the coastal area without the intervention, in whom they observed a greater decline in eGFR of −5.3 ml/min/1.73 m2 (95% CI, −7.9 to −2.7) over the harvest period.17 The authors concluded that the intervention, applied only in the inland worker group, lessened the decrease in eGFR during a harvest period. While these reports provide insight on the potential for rest–water–shade interventions to decrease HRI symptoms and indicators of renal dysfunction, the validity of comparing pre- and post-harvest measures in workers from two different climatic regions, of which only one region received the intervention, is a serious limitation in the study design. However, the ability to assess the effect of an intervention over a harvest period, albeit in only one group, is a strength.
In Nicaragua18 and Guatemala,19 regularly scheduled breaks in the shade, with increased access to water and electrolyte solutions have been implemented in sugar mills, allowing for the examination of their effects on dehydration and kidney injury. The authors in both studies measured serum creatinine, an indicator of acute kidney injury, using the Kidney Disease Improving Global Outcomes criteria, which is defined as serum creatinine change of at least 0.3 mg/dL, or serum creatinine increase of at least 1.5 times baseline value. In Guatemala, 517 agricultural workers were given access to water and electrolyte solutions and three 20-min breaks plus a 60-min lunch break in the shade.19 In addition, workers who were hydrated at preshift (USG ≤ 1.020) or who maintained or improved hydration status across the work shift were given tokens to enter a raffle to win small prizes as an incentive.19 Although acute kidney injury (AKI) was observed in well-hydrated workers, electrolyte solutions were protective against developing AKI (odds ratio [OR] 0.94, 95% CI 0.89–0.99).19 In Nicaragua, the authors compared improvements in water-rest-shade practices between two harvest seasons. Improvements included scheduled breaks begun earlier in the day and distributed throughout the workday, green vs. black canopy tents, and water positioned close to workers, along with improved taste of water and electrolyte solutions.18 The cohort consisted of cane cutters, seed cutters, irrigation repair workers, and field support staff, which had the lowest physical workload. The authors report cross-harvest kidney injury incidence and decline in eGFR were lessened with improved access to shaded rest, water, and electrolyte solution in the cane cutters group. Mean decrease in eGFR (6 ml/min/1.73 m2 [95% CI, 2–9 ml/min/1.73 m2]) was reduced compared with the first harvest period. It is important to note a potential for healthy worker selection bias, due to the prescreening of workers before gaining employment, that may identify and not hire at-risk workers for kidney dysfunction.
3.2 |. Enhanced heat dissipation clothing
Two reports described the results of a study of the effectiveness of an enhanced heat dissipation shirt and work pants uniform that used fabric with thermal-moisture properties and loose-fitting design for Chinese construction workers.22,23 Chan et al.22 described the acceptability of a loose-fitting enhanced heat dissipation collar shirt made of 100% polyester light blue fabric with moisture-wicking technology (COOLMAX® by Invista, Wichita, Kansas). The moisture-wicking fabric pulls moisture away from the skin to the outer surface of the fabric, which makes it easier to evaporate and avoids saturating the fabric. The pants were a khaki color made of 40% polyester and 60% cotton. Perception of performance was based on a rating scale of “1” (the poorest possible rating) to “7” (the best possible rating). Participants (184 construction workers of which 7 were females) rated work performance interference (did not interfere - performance interfered) and resulted in 35% performance improvement using the enhanced heat dissipation uniform.22
In another study, construction workers (n = 16) were randomized to either the enhanced heat dissipation uniform or usual work uniform group in a counterbalance order in the morning and afternoon on 1 workday.23 The enhanced heat dissipation shirt was made of 65% cotton, 35% polyester with thermal-moisture properties, porous reflective strips, and meshed fabric on the sides. The pants were 100% cotton and loose-fitting. Participants worked for 135 min in the morning and afternoon. Participants rested for 30 min in an air-conditioned room (22°C) before the start of the workday, had lunch in an air-conditioned room, and recovered for 30 min at the end of the trial in an air-conditioned room. Participants wore a monitor that captured the heart rate (HR) every minute. Rated perceived exertion (RPE) and thermal sensation (TS) were reported by participants every 5 min which would not be a practical protocol in most occupational settings. It is also reasonable to infer that stopping every 5 min to report RPE and TS can contribute to lower heat strain and does not reflect the actual work routine of workers. There was no difference observed in HR and RPE between groups. The perceptual strain index (PeSI) was calculated from TS and RPE. TS was assessed with a scale ranging from 1 (cold) to 7 (hot) every 5 min. Yang and Chan23 reported that PeSI was statistically lower in the intervention group (4.47 ± 1.85) compared with the control group (4.78 ± 1.82, p < .05). However, the mean PeSI for both groups was still within the same category of “low heat strain.”30 Also, noteworthy, is that air-conditioned rooms may have confounded the results and were not controlled for in the analysis. Moreover, air-conditioned rooms are not always accessible in real-work settings.
3.3 |. Gel and phase change material cooling gear
In Korea, 12 participants were randomized to multiple cooling gears that included bandanas, hat, vest, combination groups, and a control group.24 The participants simulated agricultural work by picking red peppers in a climatic chamber (WBGT 33°C) for 120 min (two bouts of 50-min work with a 10-min rest) and the interval between successive experiments were a minimum of three days. Rectal temperature was measured with a thermometer every minute by remaining inserted at the depth of about 13 cm in the rectum during each experiment. The study had eight intervention groups (1) the control group; (2) another group used a neck bandana with 60 oz of frozen gel; (3) one used a neck bandana with 180 oz of frozen gel; (4) one used a hat made of reflective fabric with a pocket around the neck to insert a 180 oz frozen gel pack; (5) one used a vest with pockets for inserting four 180 oz gel packs; (6) one combined the hat used in Group 4 and the bandana used in Group 3; (7) one combined the hat used in Group 4 and the vest used in Group 5; and (8) one combined the hat used in Group 4, the vest from Group 5, and the bandana from Group 3. The three combination groups (Groups 6–8) had greater body surface areas exposed to cooling gear and had no participants with rectal temperatures of more than or equal to 38°C (p < .05). Eight out of 12 participants in the group without a cooling intervention spent an average time of 37 min with a rectal temperature at more than or equal to 38°C. The average time spent at more than or equal to 38°C ranged from 2 to 18 min in the groups with a single cooling item. No difference in HR was reported among the eight groups. Over 80% of the participants in each intervention group reported the cooling gear was “comfortable” or “a little uncomfortable.” Limitations of this study are the small sample size and that a 120-min trial is not reflective of an entire work shift.
Two cooling intervention studies with construction workers assessed the effectiveness of cooling vests in China (WBGT range 29–33°C).20,31 The vests had built in fans and phase change material (PCM) inserts that were tested at worksites where WBGT ranged from 29 to 31°C.20,31 PCM melts at a lower temperature, therefore, maintaining its cooling effect longer. Important to note is that the vest was worn only during the workers’ scheduled rest breaks. In addition, participants in both studies wore enhanced heat dissipation work uniforms with thermal-moisture properties (the same uniform in the intervention study by Chan et al.31 discussed above).
A construction field study with 140 workers examined PCM vest over a 2-day trial with a mean WBGT of 30°C.31 On Day 1, participants wore a PCM vest during two rest breaks—15 min in the morning and 30 min in the afternoon—and the second day no PCM vest was worn during the two rest breaks. The method of allocating participants to the groups (intervention and control) on the 2-day trial were not reported. Heart rate was monitored with a belt around their chest. The t test showed a significant difference in the average drop per minute of HR while resting while wearing the vest as compared with the control group (10.43 ± 6.63, 4.79 ± 6.55, p < .001). Participants reported their ratings for measurements of PeSI, TS, and RPE. TS and RPE were improved in the intervention group but was not significant. PeSI scores improved in both groups after 15-min rest break and improved even more after the 30-min rest break. However, PeSI scores improved significantly in the intervention group (p < .001). The interaction of time and using enhanced heat dissipation work uniforms showed a significant influence on the alleviation of PeSI.31
In another study in China, 14 construction workers participated in a 2-day consecutive trial (WBGT 31.56 ± 1.87°C) where they were allocated to either the control group or the PCM vest intervention group in a counter-balanced order.20 The protocol for this study included a mandatory 15-min break in the morning, 1-h lunch, and a 30-min break in the afternoon during a 7-h work shift. Participants were encouraged to drink water to rehydrate in a structured manner by placing fluids near the worksite. Core temperature was estimated with tympanic temperature measured every 5 min. HR was monitored at 1-s intervals with a monitor around their chest. RPE was taken every 5-min using the Borg CR-10 scale. TS was assessed with a scale ranging from 1 (cold) to 7 (hot) every 5 min. The protocol of measuring TS, RPE, and tympanic temperature provides an additional respite time from heat stress that most workers in occupational settings do not have. PSI and PeSI were also measured. The intervention group wearing PCM vests had lower estimated core temperatures (F = 17.95, p < .01), HR (F = 16.01, p < .01), and PSI (1.03 ± 0.53, p = .02) when compared with the control group not wearing the PCM vest.20 However, core temperature was estimated using a tympanic thermometer, which should be interpreted with caution. Tympanic thermometers have been reported to fail at accurately predicting core body temperature after exertion.32 HR was significantly lower in the cooling group (F = 9.75, p = .04; F = 16.01, p < .01), as was PSI, PeSI, RPE, and TS compared with the control group. Although PSI was reported to be significantly lower in the intervention group, both groups had a PSI range of 1–2 which is categorized as little to low strain. The 14 participants had a mean age of 29 ± 3.32 and normal weight (body mass index was 21.2 ± 2.17). Interestingly, the site managers were responsible for ensuring PCM remained cold in an insulated box.
In a simulated, intervention study, PCM inserts were placed in the pockets of compression undergarments in 20 college-aged, nonsmoking, and healthy males.28 Simulated industrial tasks were conducted in a climatic chamber at WBGT 34°C for 85 min, which included OSHA work-to-rest ratios recommendations. They were tasked with carrying boxes, loosening and tightening nuts and bolts, and walking over steps while carrying weights. Participants were required to have a USG less than 1.025 before starting the trial. A USG of less than 1.025 was an indication of adequate hydration before initiating the trial. The intervention group had a lower mean rectal temperature and PSI than the control group (p < .05). The performance was measured based on the number of work cycles completed. No difference in performance was noted in both groups.
A study with 10 firefighters (male n = 6 and female n = 4) with a randomized two-group design was used to examine the effect of a cooling vest during simulated fire and rescue activities in 170°C firehouse.33 The trials ranged from 34 to 39 min. Core body temperature was recorded in 20-s intervals with an ingestible temperature sensor. HR was monitored every 5 s with a chest strap monitor. RPE and TS were obtained pre- and posttrial. The PCM cooling vest had no significant effect on HR or core temperature, RPE, or TS.33 In Iran, 15 firefighters participated in four 45-min simulated firefighting activities in a smoke-diving room at 28–30°C with relative humidity (RH) 55–60%.34 All participants were randomized to (1) control (no cooling device); (2) cooling gel containing menthol; (3) PCM cooling vest; and (4) combination of both the cooling gel with menthol and PCM cooling vest to use during the trials. Menthol cooling gel was applied to the forehead and neck. HR was measured in 1-min intervals with a chest strap monitor. Temporal artery temperature was measured pre and post each trial. HR and temporal temperature were significantly lower in the PCM vest group at the end of the trials (p < .05).34 An important consideration is that temporal artery temperature has been shown to be an inaccurate measure of core temperature under heat stress conditions.35
3.4 |. Recirculated liquid ice-chilled coolant vest
In India, construction workers (n = 29) used a vest that recirculated liquid ice-chilled coolant through silicone rubber tubing via a small battery-operated motor pump for 90-min followed by 30-min rest and then 90-min without the vest (control).25 The chilled water circulated the participant’s chest area to absorb excess heat from the participant’s body. HR was significantly lower at the end of the trial of wearing the cooling vest compared with at the end of the trial without wearing the cooling vest (p < .05).25 The protocol included a work-rest cycle of 75% work and 25% rest each hour and stopped participants from working every 15-min to obtain oral temperature.25 HR was lower in cooling vest group compared with the control group at the end of the trial, (106 ± 13, 117 ± 12, p < .05, respectively). No difference was observed in oral temperature at the end of the trial. Participants reported the cooling vest kept them comfortable and cool. The control grouped reported feeling uncomfortable and hot. This was the only study to report the cost ($50) of the vest. The authors did not report how long the small battery-operated motor pump runs on a single use. Therefore, battery run time may have limited application in certain outside occupational settings.
A study with 24 foundry workers in India similarly to Ashtekar et al.’s25 examined a vest that also recirculated liquid ice-chilled coolant through silicone rubber tubing via a small battery-operated motor pump for 90-min followed by a period of 90-min without the vest (control).26 The protocol included a work-rest cycle of 75% work and 25% rest each hour. Similarly, to the study in India with construction workers, this study also measured oral temperature every 15-min and monitored HR with a chest strap monitor. No difference was observed over 90-min trials in oral temperature or HR between the cooling vest group and the control group. Participants in the intervention group reported a mean score of 4.5 out of 5 points in perceived comfort, efficacy, and efficiency indicating workers could perform their routine work without disturbance.
Another study examined a shirt that recirculated ~15 L of liquid ice-chilled coolant via a small battery-operated motor pump with 12 participants who simulated 30 min of power utility tasks outdoors in WBGT ranging from 32°C to 38°C.27 Simulated tasks included installing insulators with bolts, washers, and nuts and uninstalling, cutting wires, and constructing a double tie using aluminum conductors steel reinforced. HR was monitored with a chest strap monitor and was not statistically different between the group with the cooling shirt and the group without it. Tympanic temperature was significantly lower with the cooling shirt (p = .003) although the mean tympanic temperature for the outdoor group not using the cooling suit was 37.4°C which is under the 38°C recommended limit. Furthermore, the accuracy after the exertion of tympanic thermometers to predict core body temperature has been called into question.32 Higher productivity was reported while using the cooling shirt compared with not using the cooling shirt outdoors (p = .011).
Twenty-five firefighters completed a simulated fire suppression and then 30 min of recovery time.36 At the start of recovery time, participants were randomized into one of three groups: (1) liquid perfused cooling vest; (2) forearm immersion in cold water (20°C); or (3) passive cooling in an air condition medical trailer at 22.2 ± 0.6°C. The participants in the cooling vest group and forearm immersion group recovered outdoors in the shade in 22.5 ± 2.9°C, RH 47.2 ± 11.0%. Core temperature was measured with an ingestible temperature sensor and HR with a chest monitor strap every 5 min during the recovery period. Cooling rates (°C/min) among the groups were significantly different with the forearm water immersion group with a cooling rate of 0.05 ± 0.04, followed by the cooling vest group at 0.03 ± 0.04, and the passive cooling group had a cooling rate of 0.03 ± 0.02. However, survival analysis of the cooling interventions did not differ in HR and core temperature during the 30-min recovery period.36 The majority of participants did not reach the set criteria of HR less than 80 bpm at the 30-min rest interval for full recovery from heat stress exposure.
3.5 |. Cold water immersion
After a 12-min live-fire drill (190–309°C), 50 firefighters were randomized to either standard rehabilitation procedure of resting in the shade (33°C, RH 33%) and drinking cool beverages ad libitum for 15-min or to the intervention group that included standard rehabilitation procedure and forearm immersion in 10°C water.37 Core temperature was monitored with an ingestible sensor and HR with a chest strap monitor. The mean core temperature at the end of the rehabilitation period was 38.5°C for the control and 38.2°C for the intervention group (p < .001). Forearm immersion resulted in a 0.28°C (95% CI, 0.06–0.50) decrease in core temperature and a 19.4 bpm (95% CI, 12.0–26.8) decrease in mean HR at the end of rehabilitation period.37
Twenty-seven firefighters were randomized into one of three groups: (1) one wearing a cold gel pack in the helmet during the live-fire drill, (2) another with forearm water (5°C) immersion for 15 min during the rehabilitation period, and (3) the control group without active cooling.21 All participants completed two sets of two 15-min drills followed by a 15-min recovery period outside in the shade. The recovery period began when all participants were seated in the recovery area. No difference was observed in HR, core temperature, or PSI in the cold gel helmet group. Core body temperature was monitored with an ingestible pill sensor and HR was measured with a chest strap monitor. Mean core temperature was significantly lower at the end of the rehabilitation period in the forearm cold water immersion group (37.68 ± 0.28°C) compared with the head cooling group (38.62 ± 0.28°C) and the control group (38.36 ± 0.46°C). PSI was significantly reduced in the forearm immersion group compared with the other two groups, but HR was not different among the three groups.
In another multi-intervention study, firefighters conducted two 20-min simulated search and rescue drills in 105°C climatic chamber.38 Participants were randomly allocated to one of three groups for the 15-min recovery period: (1) one immersing the lower body up to the umbilicus level in 15°C water (upper limbs were not immersed in water) pool with a portable chilling unit outside in the shade at 19.3°C; (2) another consuming crushed ice (−1°C) slush drink at 7 g/kg of body weight; and (3) one sitting in the shade after removing their boots and specialized personal protective clothing. Core temperatures were monitored via an ingestible temperature sensor and RPE was assessed with the Borg scale. Core temperature and cooling rates were significantly lower at the end of the 15-min cooling period in both interventions as compared to the control group. However, no difference was observed between lower body immersion in cold water and consuming crushed ice slush drink. No difference was detected in RPE among the three groups.
3.6 |. Nutritional intervention
Twenty-one firefighters participated in a counterbalance randomized trial that examined the effectiveness of reducing physiologic heat strain with an enhanced cooling nutritional intervention.39 Participants performed two 18-min fire drills (71–82°C) separated by 48 h between the two drills. After the drill, all participants recovered in a 20°C room and were allocated to the control group or the enhanced cooling nutritional group. The intervention group required participants to drink up to 355 ml of a recovery drink with 20 g of carbohydrate and 5 g of protein within the first 10-min of recovery. In addition, the intervention group also could drink up to 500 ml of water and at least 355 ml of sports drink, and they also used cold towels. The authors did not report if the fluids consumed were cold or room temperature, nor did they report where on the body the cold towels were placed. An ingestible sensor was used to monitor core temperature and a chest strap to monitor HR. It was not reported at what intervals core temperature and HR were monitored. There was no difference observed in HR or core temperature.
3.7 |. Water dousing
In Brazil, eight steel workers exposed to WBGT of 26–29°C at the worksite poured 2 L of water at 23.5°C on their head and hands over 1-min 10 times during the work shift.40 The steel workers participated in a 4-day trial and were randomized to one of the two groups. The first group participated in the control (usual work practices) for two consecutive days followed by 2 days of pouring water on their hands and head at scheduled times. The second group followed the same protocol but in inverse order. No differences were reported in tympanic temperature or HR. The intervention group had a lower report of tiredness, which was measured with an analog scale that ranged from “much better” to “same” to “much worse” (p < .05). Although HRI symptoms were assessed during the trials, the authors reported that during the intervention days only one complaint of limb fatigue was reported but there was no mention of whether this was statistically significant. There was no report on the number of HRI symptoms reported on the control days.
4 |. DISCUSSION
The aim of this review was to evaluate existing cooling intervention research in outdoor occupations, assess the effectiveness of such interventions, and offer recommendations for further research. The present work is the first study to compare cooling interventions among outdoor occupational sectors. While cooling intervention studies with vulnerable occupational groups has become of interest to researchers as rates of heat-related morbidity and mortality are high and expected to get worse with frequent heat waves due to climate change,1 research in the field of inquiry is limited.
PCM cooling studies included in this review were shown to be effective cooling interventions at mitigating occupational heat stress.20,31,34 Two of the studies successfully examined PCM vests during full work-days with construction workers suggesting PCM vests have the potential to be implemented in other outdoor occupational sectors, such as in agriculture or industrial sectors. However, it is important to note that the PCM vests were used on top of enhanced heat dissipation work uniforms, while resting for 15-min in the morning and 30 min in the afternoon resulted in significant improvement of HR, temperature, PSI, and/or worker comfort.20,22,31
Cooling vests work by conductive cooling when heat flows from an object that is hot to an object in physical contact that is cooler, to create thermal equilibrium. The cooling vest and enhanced heat dissipation work uniforms performed well in surveys measuring subjective responses of work performance and usability. Specifically, Zhao et al.’s20 study with 14 construction workers showed improvements in estimated core temperature, HR, and PSI as well as a significant improvement in subjective measures of perceived cooling and thermal sensation. It is important to highlight that this study had administrative controls in place that encouraged workers to drink water by placing water near workers and the site manager ensured the PCM inserts remained cold in an insulated box for use by workers during the two scheduled rest breaks. That is, work practices instituted by employers also affect the work conditions of the employees.
Zhao et al.’s20 study shows how a combination of administrative controls, personal cooling gear, and the participation of worksite managers can work in synergy to reduce occupational heat stress and protect workers. Although this is a field-based study, the construction industry in China adheres to a heat stress policy to protect workers, unlike the majority of outdoor jobs where neither industry nor government regulations implement structured mandatory rest breaks and work heat thresholds are not used to monitor safe working conditions. In 2012, China implemented administrative measures for an occupational heat stress policy to protect workers from heat stress at the national level.41 This policy is a threshold system that stops all work outdoors once the temperature reaches more than or equal to 40°C, at more than or equal to 37°C to less than 40°C work is limited to less than or equal to 6 h a day, and when the maximum temperature is more than or equal to 35°C to less than 37°C outside workers receive a high-temperature hazard pay.41 Nonetheless, there are no reports on the impact these regulations have had themselves. Similar administrative measures passed in California and Washington State in the United States differ in extent of protections afforded to outside workers, with only California requiring mandatory scheduled breaks. We are, however, unaware of any cooling intervention studies undertaken at either of these two sites. While more difficult to implement, administrative support may go to greater lengths in ensuring cooling interventions work and future research is needed.
Longitudinal studies in Central America with agricultural workers over harvest periods, have showed a smaller reduction in eGFR and kidney dysfunction, improved work performance and hydration, and a reduction in HRI symptoms with OSHA modified water, rest, shade, and electrolyte solution interventions.16–19 Initially, resting in the shade every hour was met with skepticism by the workers in El Salvador.16 Taking 15-min breaks every hour during high temperature may be perceived as a barrier to work efficiency and production. Nonetheless, in El Salvador, the individual daily average production increased along with improved work satisfaction suggesting that harsh working conditions can be modified to protect agricultural workers without negatively impacting production.16 Countries in Central America do not have heat stress prevention standards. However, the sugar mills where the studies were carried out contributed to fund the interventions.
Forearm water immersion for 15 min was shown to be better at decreasing core body temperature and HR after fire drills compared to the other interventions examined.21,36–38 Forearm immersion in cold water decreases core temperature by exchanging heat between superficial blood vessels in the extremity and the water. While this protocol may be appropriate for the firefighter industry, it may be challenging to implement in the agricultural, construction, and industrial sectors unless the employer implemented a work practice to have a collapsible chair with water-immersion arm holders and large amounts of cold (<20°) water readily available. Many fire agencies follow the National Firefighter Protection Association (NFPA) standard 1584, which requires a structured rehabilitation period, rehydration, and monitoring by a member of the fire department; however, the guidelines for cooling are not specific.29 Nonetheless, the adoption by fire agencies of NFPA standard 1584 is a commitment by the fire agency to protect its workforce and mitigate the negative health effects of occupational heat stress. A similar commitment is needed among employers of other outside occupational groups.
Among the agricultural, construction, and industrial worker cooling interventions studies, 41% of the trials were 2 h or less.24–28 Working in direct sunlight and performing 2 h of prolonged or strenuous work increases the risk of HRI. Agricultural, construction, and industrial workers have strenuous jobs and work long hours in direct sunlight. Future protocols should have minimal interference in the work routine by not stopping workers every 5 or 15 min to obtain measures. Thus, it is important to assess the all-day work use of cooling interventions to determine the efficacy and usability of the cooling gear. Even though some cooling interventions have shown a reduction in HRI, improved body temperature, and HR, the sample size of several of the studies were small and of short work duration. Therefore, the successful implementation of cooling interventions in large occupational groups with diverse characteristics and work hours and routines remains uncertain and future research should be conducted on a large scale.
At the same time, it also needs to be recognized that despite the broad range of cooling interventions reviewed for this study, cultural differences can and do play a part in the type of intervention that can be implemented in any particular country. Moreover, workforce migration should also be taken into consideration. In the United States, for example, it is estimated that 75% of agricultural workers are immigrants, and the vast majority are from Mexico and Central America.42 An incompatibility of hot and cold foods permeates the worldviews in Mexican and Central American perceptions since pre-Hispanic times. Some of these practices endure among rural and indigenous communities who have migrated from these countries to the United States.43
More female participants are needed in occupational cooling studies in light of changing demographics of the outdoor occupational sectors that have led to increased workforce diversity.44,45 In addition, there are sex-related differences in heat stress tolerance and previous results have shown females report three or more symptoms more frequently than males (OR = 2.67, 95% CI, 1.1–6.6).46 Therefore, examining for differences in the effect of cooling gear at reducing the occurrence of HRI is needed. Female anthropometrics must be regarded in cooling interventions where properly fitting personal protective equipment is necessary to safeguard efficacy and usability. Studies with females are needed as they represent a significant portion of outside workers and also have high rates of HRI.46–48
Implementation of work-rest cycles at worksites is a barrier in light of the unwillingness of sectors to incorporate them due to the perception of potential loss in production and revenue and lack of heat prevention standards. Many of the studies included work-rest cycles without a significant decrease in performance or production losses. Cooling gear has the capacity to protect workers from HRI and to augment the protectiveness of water, rest, and shade.20,24,31 Only one study reported the cost of the vest as $5025 while none of the other studies reported the cost of the cooling devices. Future cooling intervention studies should report the costs of cooling gear. In addition, research of economic evaluation that measures productivity and cost-benefit analysis to determine if investment in cooling gear benefits outweigh the cost of implementing such interventions.
Heat stress prevention standards from government bodies across the globe are lacking, and even where standards do exist enforcement is minimal as HRI rates remain high.49,50 Some countries have launched heat prevention educational campaigns and have made strong recommendations for employers to protect workers from heat stress, but recommendations are not easily enforceable.6,51,52 In the United States, OSHA has recommended more water, rest, and shade, which are meant to help prevent HRI. Administrative measures to ensure worker safety may be effective but are not enough and are difficult to implement without regulatory standards in place for enforcement. Cooling interventions can thus serve as an additional tool to complement those recommendations and help keep workers safe from HRI. Practical implementation of cooling interventions will be limited by the acceptability of the cooling gear within the context of the cultural practices in which it is applied, as well as occupational practices and the demands of the work being performed. Water immersion, for example, though effective for firefighters, may find some resistance where these practices conflict with cultural practices or are not feasible in certain occupational settings. At the same time, bandanas may prove cumbersome for construction workers who have to wear hard hats but not to workers in areas where that requirement is not in place. Moreover, biological differences in bodies’ response to heat also need to be taken into consideration, especially in the apparent more marked response to heat by women than men.46 It is vital that future research implements biomonitoring protocols that have minimal interference with work routines to better assess the effectiveness of cooling interventions. Biomonitoring should include measuring HR, core temperature, work intensity, and pre and posturine specific gravity for dehydration assessment, as well as self-reported HRI symptoms and perceived thermal comfort. While cooling interventions can complement the recommended OSHA guidelines for more water, more frequent rest, and access to shade, they must be appropriate to occupational activities and limitations as well as take into consideration cultural practices and individual acceptance to increase their effectiveness.
5 |. CONCLUSION
Exposure to a hot environment for a prolonged period while working can result in the body’s inability to cool itself, and lead to HRI and in severe cases heat-related death. It is projected that there will be a rise in heat-related illness and injuries and death along with productivity losses due to extreme hot temperatures associated with climate change. The use of cooling interventions in the outside occupational setting along with hydration and resting in the shade may reduce disproportionate rates of HRI and heat-related mortality among vulnerable occupational groups. That is, targeted cooling interventions with work-rest cycles may attenuate heat strain while improving the comfort of workers. Thus, it is challenging to recommend one cooling intervention over another to all outside occupational groups due to the diversity of occupational settings and occupational tasks performed. Coldwater immersion seems to be the most effective method for firefighters, while cooling vests seem more appropriate and effective in the construction industry. However, what remains constant in the majority of the studies included in this review is that hydration and work-rest cycles are important to the effectiveness of cooling gear. Further industry-specific cooling intervention research that includes worker participant feedback is required to determine best practice recommendations for protecting vulnerable occupational groups to HRI and heat-related death.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by Sunshine Education and Research Center at University of South Florida Grant 5T42OH008438-13, North Carolina Occupational Safety and Health Education and Research Center at University of North Carolina Chapel Hill Grant 5T42OH008673-13, and the National Institute of Diabetes and Digestive and Kidney Diseases Grant T32-DK-07656.
Funding information
Sunshine Education and Research Center at University of South Florida, Grant/Award Number: 5T42OH008438-13; North Carolina Occupational Safety and Health Education and Research Center at University of North Carolina Chapel Hill, Grant/Award Number: 5T42OH008673-13; National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: T32 - DK 07656
Footnotes
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
SUPPORTING INFORMATION
Additional Supporting Information may be found online in the supporting information tab for this article.
REFERENCES
- 1.USGCRP. Impacts, risks, and adaptation in the United States: Fourth national climate assessment In: Program USGCR, ed. Vol 2 Washington, DC: U.S. Global Change Research Program; 2018. [Google Scholar]
- 2.NIOSH. Criteria for a recommended standard: occupational exposure to heat and hot environments In: Health NIfOSa, ed. Cincinnati, OH: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH); 2016. [Google Scholar]
- 3.Atha WF. Heat-related illness. Emerg Med Clin North Am. 2013;31(4): 1097–1108. [DOI] [PubMed] [Google Scholar]
- 4.Flouris AD, Dinas PC, Ioannou LG, et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018;2(12):e521–e531. [DOI] [PubMed] [Google Scholar]
- 5.Gubernot DM, Anderson GB, Hunting KL. Characterizing occupational heat-related mortality in the United States, 2000–2010: an analysis using the Census of Fatal Occupational Injuries database. Am J Ind Med. 2015;58(2):203–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.OSHA. Heat Illness Prevention Campaign. Occupational Safety and Health Administration; 2011. https://www.osha.gov/heat/. Accessed July 15, 2020. [Google Scholar]
- 7.OSHA. OSHA Technical Manual In: Labor USDo, ed: Occupational Safety and Health Administration; 2017. [Google Scholar]
- 8.Stevens CJ, Taylor L, Dascombe BJ. Cooling during exercise: an overlooked strategy for enhancing endurance performance in the heat. Sports Med. 2017;47(5):829–841. [DOI] [PubMed] [Google Scholar]
- 9.Ruddock A, Robbins B, Tew G, Bourke L, Purvis A. Practical cooling strategies during continuous exercise in hot environments: a systematic review and meta-analysis. Sports Med. 2017;47(3):517–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bongers CC, Hopman MT, Eijsvogels TM. Cooling interventions for athletes: an overview of effectiveness, physiological mechanisms, and practical considerations. Temperature. 2017;4(1):60–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. [DOI] [PubMed] [Google Scholar]
- 12.Moran DS, Shitzer A, Pandolf KB. A physiological strain index to evaluate heat stress. Am J Physiol. 1998;275(1):R129–R134. [DOI] [PubMed] [Google Scholar]
- 13.Tikuisis P, McLellan TM, Selkirk G. Perceptual versus physiological heat strain during exercise-heat stress. Med Sci Sports Exerc. 2002; 34(9):1454–1461. [DOI] [PubMed] [Google Scholar]
- 14.Borg G Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990; 16(Suppl 1):55–58. [DOI] [PubMed] [Google Scholar]
- 15.Gagge AP, Stolwijk JA, Saltin B. Comfort and thermal sensations and associated physiological responses during exercise at various ambient temperatures. Environ Res. 1969;2(3):209–229. [DOI] [PubMed] [Google Scholar]
- 16.Bodin T, García-Trabanino R, Weiss I, et al. Intervention to reduce heat stress and improve efficiency among sugarcane workers in El Salvador: phase 1. Occup Environ Med. 2016;73(6):409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wegman DH, Apelqvist J, Bottai M, et al. Intervention to diminish dehydration and kidney damage among sugarcane workers. Scand J Work Environ Health. 2018;44(1):16–24. [DOI] [PubMed] [Google Scholar]
- 18.Glaser J, Hansson E, Weiss I, et al. Preventing kidney injury among sugarcane workers: promising evidence from enhanced workplace interventions. Occup Environ Med. 2020;77(8):527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butler-Dawson J, Krisher L, Yoder H, et al. Evaluation of heat stress and cumulative incidence of acute kidney injury in sugarcane workers in Guatemala. Int Arch Occup Environ Health. 2019;92(7):977–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao Y, Yi W, Chan APC, Wong DP. Impacts of cooling intervention on the heat strain attenuation of construction workers. Int J Biometeorol. 2018;62(9):1625–1634. [DOI] [PubMed] [Google Scholar]
- 21.Yeargin S, McKenzie AL, Eberman LE, Kingsley JD, Dziedzicki DJ, Yoder P. Physiological and perceived effects of forearm or head cooling during simulated firefighting activity and rehabilitation. J Athl Train. 2016;51(11):927–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan A, Guo Y, Wong F, Li Y, Sun S, Han X. The development of antiheat stress clothing for construction workers in hot and humid weather. Ergonomics. 2016;59(4):479–495. [DOI] [PubMed] [Google Scholar]
- 23.Yang Y, Chan APC. Role of work uniform in alleviating perceptual strain among construction workers. Ind Health. 2017;55(1): 76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi JW, Kim MJ, Lee JY. Alleviation of heat strain by cooling different body areas during red pepper harvest work at WBGT 33 degrees C. Ind Health. 2008;46(6):620–628. [DOI] [PubMed] [Google Scholar]
- 25.Ashtekar S, Mishra S, Kapadia V, Nag P, Singh G. Workplace heat exposure management in Indian construction workers using cooling garment. Workplace Health Saf. 2019;67(1):18–26. [DOI] [PubMed] [Google Scholar]
- 26.Shirish A, Kapadia V, Kumar S, Kumar S, Mishra S, Singh G. Effectiveness of a cooling jacket with reference to physiological responses in iron foundry workers. Int J Occup Saf Ergon. 2016; 22(4):487–493. [DOI] [PubMed] [Google Scholar]
- 27.Furtado AL, Craig BN, Chard JT, Zaloom VA, Chu HW. Cooling suits, physiological response, and task performance in hot environments for the power industry. Int J Occup Saf Ergon. 2007;13(3):227–239. [DOI] [PubMed] [Google Scholar]
- 28.Butts CL, Smith CR, Ganio MS, McDermott BP. Physiological and perceptual effects of a cooling garment during simulated industrial work in the heat. Appl Ergon. 2017;59(Pt A):442–448. [DOI] [PubMed] [Google Scholar]
- 29.NFPA. NFPA 1584: Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises. Quincy MA: National Fire Protection Association; 2007. [Google Scholar]
- 30.Dehghan H, Ghanbary Sartang A. Validation of perceptual strain index to evaluate the thermal strain in experimental hot conditions. Int J Prev Med. 2015;6:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan A, Zhang Y, Wang F, Wong F, Chan D. A field study of the effectiveness and practicality of a novel hybrid personal cooling vest worn during rest in Hong Kong construction industry. J Therm Biol. 2017;70:21–27. [DOI] [PubMed] [Google Scholar]
- 32.Pryor RR, Seitz JR, Morley J, et al. Estimating core temperature with external devices after exertional heat stress in thermal protective clothing. Prehosp Emerg Care. 2012;16(1):136–141. [DOI] [PubMed] [Google Scholar]
- 33.Carter JM, Rayson MP, Wilkinson DM, Richmond V, Blacker S. Strategies to combat heat strain during and after firefighting. J Therm Biol. 2007;32(2):109–116. [Google Scholar]
- 34.Hemmatjo R, Motamedzade M, Aliabadi M, Kalatpour O, Farhadian M. The effect of practical cooling strategies on physiological response and cognitive function during simulated firefighting tasks. Health Promot Perspect. 2017;7(2):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Low DA, Vu A, Brown M, et al. Temporal thermometry fails to track body core temperature during heat stress. Med Sci Sports Exerc. 2007;39(7):1029–1035. [DOI] [PubMed] [Google Scholar]
- 36.Colburn D, Suyama J, Reis SE, et al. A comparison of cooling techniques in firefighters after a live burn evolution. Prehosp Emerg Care. 2011;15(2):226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burgess JL, Duncan MD, Hu C, et al. Acute cardiovascular effects of firefighting and active cooling during rehabilitation. J Occup Environ Med. 2012;54(11):1413–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walker A, Driller M, Brearley M, Argus C, Rattray B. Coldwater immersion and iced-slush ingestion are effective at cooling firefighters following a simulated search and rescue task in a hot environment. Appl Physiol Nutr Metab. 2014;39(10):1159–1166. [DOI] [PubMed] [Google Scholar]
- 39.Horn GP, Gutzmer S, Fahs CA, et al. Physiological recovery from firefighting activities in rehabilitation and beyond. Prehosp Emerg Care. 2011;15(2):214–225. [DOI] [PubMed] [Google Scholar]
- 40.Fujii RK, Horie S, Tsutsui T, Nagano C. Heat exposure control using non-refrigerated water in Brazilian steel factory workers. Ind Health. 2007;45(1):100–106. [DOI] [PubMed] [Google Scholar]
- 41.Jia AY, Rowlinson S, Loosemore M, Xu M, Li B, Gibb A. Institutions and institutional logics in construction safety management: the case of climatic heat stress. Constr Manag Econ. 2017;35(6):338–367. [Google Scholar]
- 42.US Department of Labor. Findings from the National Agricultural Workers Survey (NAWS) 2015–2016: A Demographic and Employment Profile of United States Farmworkers In: Labor UDo, ed.; 2018. [Google Scholar]
- 43.Barker JC, Guerra C, Gonzalez-Vargas MJ, Hoeft KS. An ethnographic study of salt use and humoral concepts in a Latino farm worker community in California’s Central Valley. J Ethnobiol Ethnomed. 2017;13(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Department of Labor . Findings from the National Agricultural Workers Survey (NAWS) 2013–2014 In: Labor UDo, ed.; 2016. [Google Scholar]
- 45.US Department of Labor. Employment and Earnings in Select Occupations In: Labor UDo, ed.; 2017. [Google Scholar]
- 46.Mutic AD, Mix JM, Elon L, et al. Classification of heat-related illness symptoms among Florida farmworkers. J Nurs Scholarsh. 2018;50(1): 74–82. [DOI] [PubMed] [Google Scholar]
- 47.Sett M, Sahu S. Effects of occupational heat exposure on female brick workers in West Bengal, India. Glob Health Action. 2014;7: 21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onyebeke LC, Papazaharias DM, Freund A, et al. Access to properly fitting personal protective equipment for female construction workers. Am J Ind Med. 2016;59(11):1032–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moyce S, Mitchell D, Armitage T, Tancredi D, Joseph J, Schenker M. Heat strain, volume depletion and kidney function in California agricultural workers. Occup Environ Med. 2017;74(6):402–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crowe J, Nilsson M, Kjellstrom T, Wesseling C. Heat-related symptoms in sugarcane harvesters. Am J Ind Med. 2015;58(5):541–548. [DOI] [PubMed] [Google Scholar]
- 51.Al-Bouwarthan M, Quinn MM, Kriebel D, Wegman DH. Assessment of heat stress exposure among construction workers in the hot desert climate of Saudi Arabia. Ann Work Expo Health. 2019;63(5):505–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hendel-Blackford TWorking in excessive heat: regulations from around the world. Safety and Health Practitioner. June 30 2014 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


