Abstract
Background
Stress, anxiety, and depression are some of the most important research and practice challenges for psychologists, psychiatrists, and behavioral scientists. Due to the importance of issue and the lack of general statistics on these disorders among the Hospital staff treating the COVID-19 patients, this study aims to systematically review and determine the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients.
Methods
In this research work, the systematic review, meta-analysis and meta-regression approaches are used to approximate the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients. The keywords of prevalence, anxiety, stress, depression, psychopathy, mental illness, mental disorder, doctor, physician, nurse, hospital staff, 2019-nCoV, COVID-19, SARS-CoV-2 and Coronaviruses were used for searching the SID, MagIran, IranMedex, IranDoc, ScienceDirect, Embase, Scopus, PubMed, Web of Science (ISI) and Google Scholar databases. The search process was conducted in December 2019 to June 2020. In order to amalgamate and analyze the reported results within the collected studies, the random effects model is used. The heterogeneity of the studies is assessed using the I2 index. Lastly, the data analysis is performed within the Comprehensive Meta-Analysis software.
Results
Of the 29 studies with a total sample size of 22,380, 21 papers have reported the prevalence of depression, 23 have reported the prevalence of anxiety, and 9 studies have reported the prevalence of stress. The prevalence of depression is 24.3% (18% CI 18.2–31.6%), the prevalence of anxiety is 25.8% (95% CI 20.5–31.9%), and the prevalence of stress is 45% (95% CI 24.3–67.5%) among the hospitals’ Hospital staff caring for the COVID-19 patients. According to the results of meta-regression analysis, with increasing the sample size, the prevalence of depression and anxiety decreased, and this was statistically significant (P < 0.05), however, the prevalence of stress increased with increasing the sample size, yet this was not statistically significant (P = 0.829).
Conclusion
The results of this study clearly demonstrate that the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients is high. Therefore, the health policy-makers should take measures to control and prevent mental disorders in the Hospital staff.
Keywords: Anxiety, Stress, Depression, COVID-19, Healthcare workers
Background
On 31st December 2019, China reported an acute pneumonia outbreak that had emerged from Wuhan. In a short span of time, the disease caused by the new coronavirus (COVID-19) spread from China to other countries, and caused several health, socio-economic and political challenges globally [1, 2]. On 30th January 2020, the World Health Organization (WHO) declared the 2019 New Coronavirus as a Public Health Emergency of International Concern (PHEIC). On February 11, 2020, WHO declared a global pandemic, and officially named the new coronavirus as COVID-19 [2–4]. On the same day, the International Committee on Virus Classification (ICTV) modified the 2019-nCoV name to SARS-CoV-2 [4]. As of June 25, 2020, the WHO reported more than 8.5 million infections worldwide. Nevertheless, the number of the infected people is still increasing. Moreover, the lack of a definitive treatment has led to more than 457,000 fatalities during this period [4, 5]. The outbreak of the disease has put a lot of psychological pressure on different communities and keyworkers, especially Hospital staff who are in a direct contact with the patients [5].
Stress, anxiety, and depression are some of the key challenges for psychologists, psychiatrists, and behavioral scientists globally. Among physical and mental illnesses, depression is common mental disorder in the world depression [6], according to the World Health Organization, is one of the most common behavioral disorders associated with low mood, loss of interest, guilt and worthlessness, sleep and appetite disorders, decreased energy and decreased concentration. Depression and anxiety are the most common psychiatric disorders with a prevalence of 10 to 20% in the general population [6–9]. Stress is in fact an integral part of human life and is perhaps one of the most common issues in modern societies [6, 11]. Anxiety is a disorder often associated with fear and unease and is accompanied by symptoms such as fatigue, restlessness and palpitations. In the etiology of anxiety, genetic, hereditary, environmental, psychological, social and biological factors are considered [6, 12, 13]. A person who is exposed to constant anxiety and worry loses self-confidence and becomes depressed while feeling humiliated, and these in turn increase workplace stress and performance reduction. The latter itself intensifies anxiety, and the continuation of this cycle can eventually erode people's mental and physical abilities and, after a while, lead to unstable neuropsychiatric disorders [6, 14].
Nurses and physicians are affected by a variety of stressors in their workplaces because of their responsibility to provide health and treatment to patients, the National Institutes of Health (NIH) said after studying the relative prevalence of health disorders in high-stress occupations. Out of 130 jobs surveyed, nursing is ranked 27th due to mental health problems [15]. Other studies report that 7.4% of nurses are absent from work each week due to burnout or disability due to stress, which is 80% more than other occupational groups [15].
Hospital Hospital staff in charge of admitting and caring for patients with COVID-19 have been subjected to a variety of individual, and organizational stresses that have adversely affected their health and job satisfaction. Therefore, recognizing stressors, and periodic training will be an effective step towards prevention, treatment and stress reduction [10–14]. Stress can increase depression and anxiety, reduce job satisfaction, impair individual relationships, and even lead to suicidal thoughts. It can also reduce the effects of psychological interventions due to the reduction in concentration and decision-making skills, and by influencing the mental health professional's ability to communicate strongly with clients [15].
Due to the impact of various factors on the prevalence of stress, anxiety and depression in hospitals’ Hospital staff directly faced with the COVID-19 patients, and the lack of general statistics in this regard, we attempted to systematically review the literature. We statistically analyzed the reported results of the collected studies to provide a set of general statistics on the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients, with a view to inform other related programs for reducing the complications of these disorders.
Methods
This work has followed the systematic review, meta-analysis, and meta-regression methods. In order to identify relevant studies from literature the SID, MagIran, IranMedex, IranDoc, ScienceDirect, Embase, Scopus, PubMed, Web of Science (ISI) and Google Scholar databases were searched. The keywords of prevalence, anxiety, stress, depression, psychopathy, mental illness, mental disorder, doctor, physician, nurse, Hospital staff, 2019-nCoV, COVID-19, SARS-CoV-2 and Coronaviruses and all possible combinations of these words were used in the search strategy and for each of the above-mentioned databases. No lower time limit was considered in the search process, and articles published in December 2019 to June 2020 were among the search pool. Once all related studies were identified, the identifying information about the selected sources was transferred into the EndNote bibliography management software. In order to maximize the comprehensiveness of the search, the reference lists within all selected articles were manually reviewed.
Inclusion criteria
Criteria for entering studies included: studies examining the prevalence of stress, anxiety, and depression in the hospital Hospital staff caring for COVID-19 patients based on the diagnostic criteria in each study (SDS, SAS, SASR, DASS-21, BDI-II, BAI, PSS, HAD, GAD-7) (Table 1).
Table 1.
Characteristic of the collected studies related to the prevalence of depression, anxiety and stress
| Author, year, references | Age (years) | Country | Sample size | Prevalence% | Mean ± standard deviation | Diagnostic criteria | Population | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Female | Male | Depression | Anxiety | Stress | Depression | Anxiety | Stress | |||||
| Zhu-1, 2020 [7] | 34.16 ± 8.06 | China | 79 | – | – | 45.6 | 11.4 | – | – | – | – |
SDSa SASb |
Doctor |
| Zhu-2, 2020 [7] | – | China | 86 | – | – | 43 | 27.9 | – | – | – | – |
SDS SAS |
Nurse |
| Xiao-1, 2020 [8] | – | China | 180 | 129 | 51 | – | 29.4 | 29.4 | – | 55.25 ± 14.18 | 77.58 ± 29.52 |
SAS SASRc |
Hospital staff |
| Chew, 2020 [9] | 29 (25–35) | Singapore | 906 | 583 | 323 | 10.6 | 15.7 | 5.2 | – | – | – | DASS-21d | Hospital staff |
| Zhang-1, 2020 [10] | – | Hong Kong | 564 | 478 | 77 | 39.5 | 30.0 | – | – | – | – | DASS-21 | Doctor |
| Zhang-2, 2020 [10] | – | Hong Kong | 999 | 804 | 195 | 31.0 | 25.4 | – | – | – | – | DASS-21 | Nurse |
| Wang-1, 2020 [11] | – | China | 194 | – | – | – | – | – | 6.25 ± 1.93 | 6.16 ± 2.22 | 7.76 ± 15.2 |
BDI-IIe BAIf PSSg |
Doctor |
| Wang-2, 2020 [11] | – | China | 1304 | – | – | – | – | – | 6.38 ± 1.66 | 6.15 ± 2.36 | 7.86 ± 17.5 |
BDI-II BAI PSS |
Nurse |
| Liu-1, 2020 [13] | – | China | 512 | 433 | 79 | – | 12.5 | – | – | 39.56 ± 8.91 | – | SAS | Hospital staff |
| Du, 2020 [17] | 36.00 ± 8.05 | China | 134 | 81 | 53 | 12.7 | 20.1 | – | 5.76 ± 7.04 | 4.96 ± 8.13 | – |
BDI-II BAI |
Hospital staff |
| Kazmi, 2020 [18] | – | Iran | 1000 | 620 | 380 | 61.1 | 57.0 | 64.3 | – | – | – | DASS-21 | Hospital staff |
| Gautam, 2020 [19] | – | China | 187 | – | – | – | 23.0 | – | – | – | – | SAS | Hospital staff |
| Ong, 2020 [20] | – | China, Indian, Others | 158 | 111 | 47 | 0.6 | 0.6 | – | – | – | – | DASS-21 | Hospital staff |
| Xiao-2, 2020 [21] | – | China | 958 | 644 | 314 | 42.7 | 39.9 | – | – | – | – | HADh | Hospital staff |
| Guixia, 2020 [22] | – | China | 86 | – | – | 54.7 | 44.2 | 45.3 | 5.78 ± 4.36 | 46.89 ± 10.47 | 50.7 ± 12.11 |
BDI-II SAS SASR |
Hospital staff |
| Aghili, 2020 [23] | – | Iran | 289 | – | – | 44.6 | 33.9 | 71.3 | – | – | – |
SDS SAS SASR |
Hospital staff |
| Dimitriu, 2020 [24] | 27.92 ± 2.66 | Romania | 100 | 50 | 50 | 9.0 | – | – | – | – | – |
SDS SAS |
Hospital staff |
| Sharif, 2020 [25] | – | India | 375 | – | – | 13.9 | – | – | – | – | – | SDS | Hospital staff |
| Geoffroy, 2020 [26] | 32.7 ± 11.00 | France | 149 | – | – | 4.0 | 49.0 | 70.5 | – | – | – | DASS-21 | Hospital staff |
| Abdulah, 2020 [27] | 35.06 (33–70) | Australia | 268 | 80 | 188 | – | – | 93.7 | – | – | 4.20 ± 2.46 | PSS | Doctor |
| Yin, 2020 [28] | 35.30 ± 9.48 | China | 371 | 228 | 143 | – | – | 44.5 | – | – | – | SASR | Hospital staff |
| Gao, 2020 [29] | – | China | 118 | 88 | 30 | 44.9 | 44.9 | – | – | – | – |
SDS SAS |
Hospital staff |
| Huang-1, 2020 [30] | – | China | 230 | 187 | 43 | – | 23.0 | – | – | – | – | SAS | Hospital staff |
| Huang-2, 2020 [31] | 49(41–58) | China | 2250 | 1642 | 608 | 19.8 | 35.6 | – | – | – | – | GAD-7i | Hospital staff |
| Lai, 2020 [32] | 26–40 | China | 1257 | 964 | 293 | 50.4 | 44.6 | – | – | – | – | GAD-7 | Hospital staff |
| Liu-2, 2020 [33] | – | China | 4679 | 3851 | 828 | 34.6 | 16.0 | – | – | – | – |
SDS SAS |
Nurse |
| Lu, 2020 [34] | – | China | 2299 | 1779 | 512 | 11.7 | 24.7 | – | – | – | – |
SDS SAS |
Nurse |
| Tan, 2020 [35] | – | China | 470 | 321 | 149 | 8.9 | 14.5 | 6.6 | – | – | – | DASS-21 | Hospital staff |
| Zhang-3, 2020 [36] | – | China | 2178 | 1401 | 781 | 10.7 | 10.5 | – | – | – | – |
SDS SAS |
Hospital staff |
aSelf-rating Depression Scale (SDS)
bSelf-rating Anxiety Scale (SAS)
cStanford Acute Stress Reaction (SASR)
dDepression Anxiety Stress Scales (DASS-21)
eBeck Depression Inventory-II (BDI-II)
fBeck Anxiety Inventory (BAI)
gPerceived Stress Scale (PSS)
hHospital Anxiety/Depression Scale (HAD)
iThe 7-item Generalized Anxiety Disorder (GAD-7) Scale (range, 0–21)
Exclusion criteria
Criteria for excluding a study were: research works without sufficient data, duplicate papers, and studies with unclear methods (diagnostic methods other than those listed in the inclusion criteria).
Study selection
Initially, studies that were repeated in various databases were removed from the list. Subsequently, a list of the titles of all the remaining articles was prepared, so that the quality of articles could be evaluated. For the systematic review, the PRISMA guidelines were followed; in the first stage, screening, the title and abstract of the remaining articles were carefully examined and a number of irrelevant articles were excluded, considering the inclusion and exclusion criteria. In the second stage, i.e., eligibility evaluation, the full text of the possible related articles remaining from the screening stage were examined, and similarly, at this stage, several other irrelevant studies were removed. To prevent bias, all stages of resource review and data extraction were performed by two reviewers independently. If an article was not included, the reason for the exclusion was mentioned. In cases where there was a disagreement between the two reviewers, the third person reviewed the article.
Quality evaluation of articles
In order to evaluate the quality of articles (i.e., with respect to the methodological validity and results), a checklist appropriate to the type of study was used. The STROBE checklists are commonly used to critique and evaluate the quality of observational studies. The Strengthening the Reporting of Observational studies in Epidemiology (STROBE checklist) consists of six scales/general sections that include: title, abstract, introduction, methods, results, and discussion. Some of these scales have subscales, resulting in a total of 32 subscales (items). Some of these 32 items represent different methodological aspects of the study, and include title, problem statement, study objectives, study type, study statistical community, sampling strategy, sample size, definition of variables and procedures, data collection tools, statistical analysis methods, and findings. Accordingly, the maximum score that can be obtained from the evaluation using the checklist is 32. Considering the score of 16 as the cut-off point [16], all articles with scores of 16 and above were considered as medium or high-quality articles. Sixteen articles were considered as low quality, and were therefore excluded from the study.
Data extraction
Information on all final papers entered into the systematic review, meta-analysis, and meta-regression process were extracted using another pre-prepared checklist. The checklist included the title of the article, the name of the first author, the year of publication, the place of study, the study population, the research instrument, the sample size, the prevalence of stress, anxiety and depression.
Statistical analysis
To assess the heterogeneity of the selected articles, the I2 index was used [heterogeneity was considered in three categories: less than 25% (low heterogeneity), 25–75% (medium heterogeneity), and more than 75% (high heterogeneity)]. In order to investigate the publication bias and also due to the high volume of samples entered in the study, Begg's test (Begg and Mazumdar) was performed at the significance level of 0.1, and the corresponding Funnel plots were included. In this study, in order to investigate the factors affecting the heterogeneity of studies, meta-regression analysis was used to investigate the effect of the sample size on meta-analysis. Data analysis was performed using the Comprehensive Meta-Analysis (version 2) software.
Results
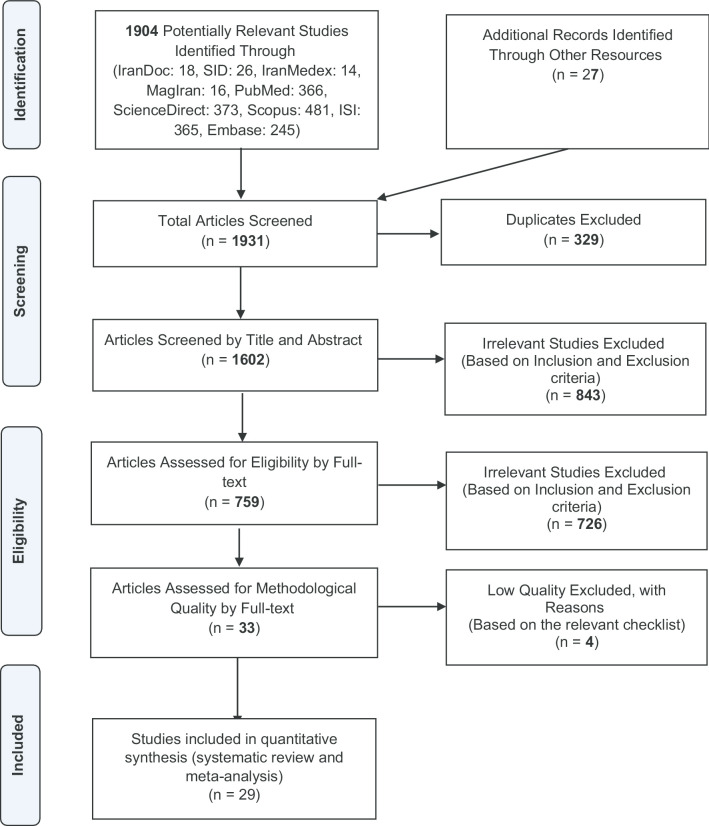
As mentioned earlier, the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA guidelines) were used to conduct the systematic review, meta-analysis, and the meta-regression. At the identification stage, 1904 possible related articles were identified and transferred into the EndNote bibliography management software. Another 27 studies were included following the examination of list of sources and gray literature. Of the total 1931 studies identified, 329 were duplicate and were therefore excluded. In the screening stage, of the 1602 remaining studies, 843 articles were omitted by studying their title and abstract and based on the inclusion and exclusion criteria. In the evaluation eligibility stage, out of 759 remaining articles, 726 ineligible articles were removed following the examination of their full text, and similarly according to the inclusion and exclusion criteria. In the quality evaluation stage, by reading the full text of the article and based on the score obtained from STROBE checklist, out of 33 remaining studies, four studies were assessed as low quality and excluded (i.e., STROBE checklist score below 16). Finally, 29 articles that are published until June 2020 were entered into the final analysis (Fig. 1).
Fig. 1.
The flowchart on the stages of including studies in the systematic review and meta-analysis (PRISMA 2009)
The I2 test results for depression, anxiety, and stress were 98.9, 98.5, and 99.1, respectively. Due to the heterogeneity of the selected studies, the random effects model was used to amalgamate the reported results and to estimate the overall prevalence of each disorder. The reason for the heterogeneity between studies can be due to different sample size, sampling error, study time, or study location. Of the 29 studies with the total sample size of 22,380, 21 studies had a focus on depression, 23 studies reported anxiety, and 9 articles studied stress in Hospital staff caring for the COVID-19 patients. The lowest and highest sample sizes were related to the studies of Zhu et al. [7] (79 participants), and Liu et al. [33] (4679 participants), respectively. The specifications of the meta-analysis studies are provided in Table 1.
The publication bias in reporting the results of the prevalence of depression, anxiety, and stress using funnel diagrams and Begg’s tests at the significance level of 0.1 indicates no bias in the present study (P = 0.349, P = 0.711, and P = 0.916, respectively).
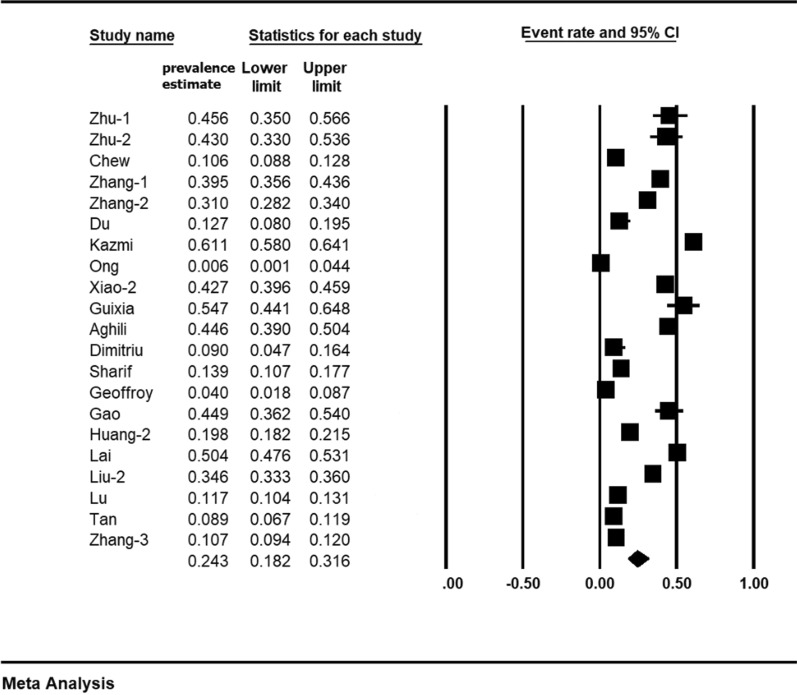
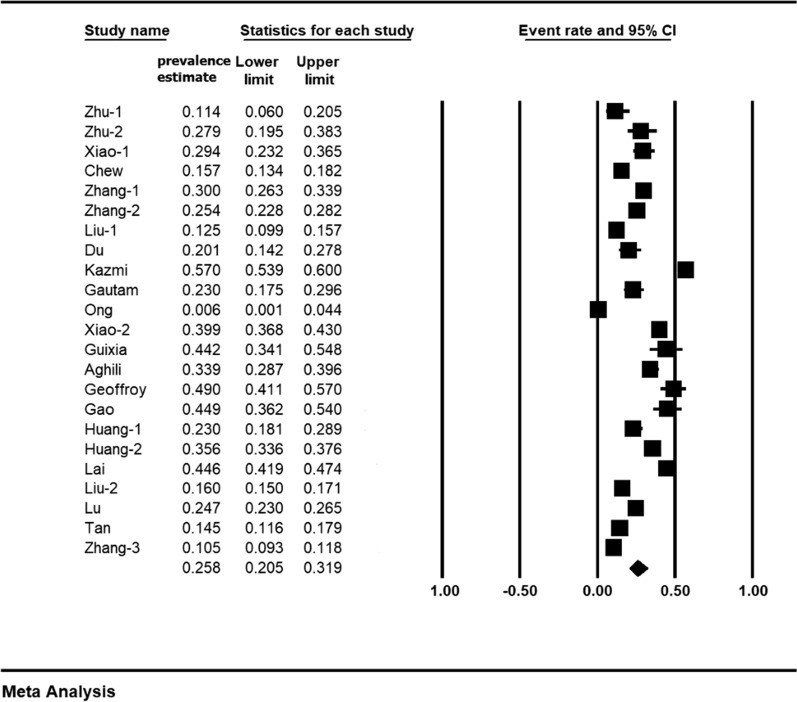
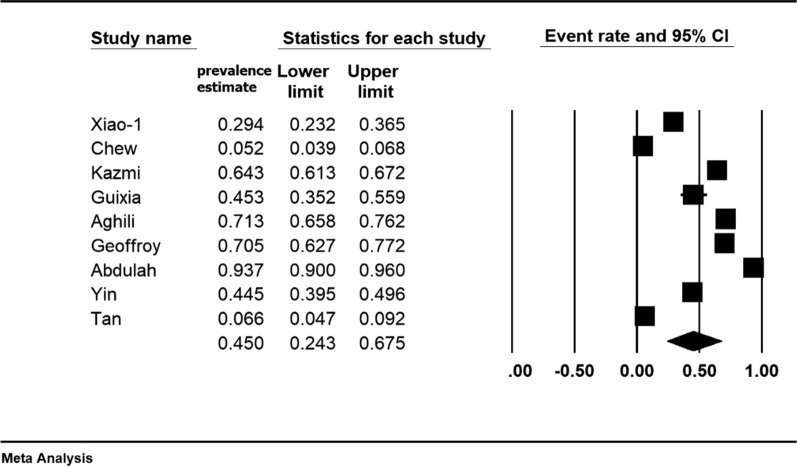
Our findings show that the prevalence of depression is 24.3% (95% CI 18.2–31.6%), the prevalence of anxiety is 25.8% (95% CI 20.5–31.9%), and the prevalence of stress is 45% (95% CI 24.3–67.5%) in the hospital Hospital staff caring for the COVID-19 patients. The midpoint of each square in the following forest plots indicates ‘prevalence’ in each study, and the diamond shape denotes the overall prevalence in the total population and for all studies combined (Figs. 2, 3 and 4).
Fig. 2.
Forest plot demonstrating the prevalence of depression within front-line healthcare workers caring for COVID-19 patients; 95% CI
Fig. 3.
Forest plot demonstrating the prevalence of anxiety within front-line healthcare workers caring for COVID-19 patients; 95% CI
Fig. 4.
Forest plot demonstrating the prevalence of stress within front-line healthcare workers caring for COVID-19 patients; 95% CI
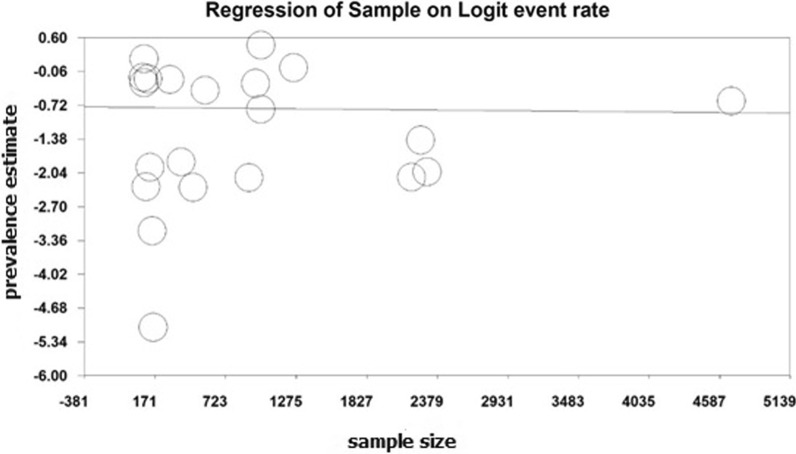
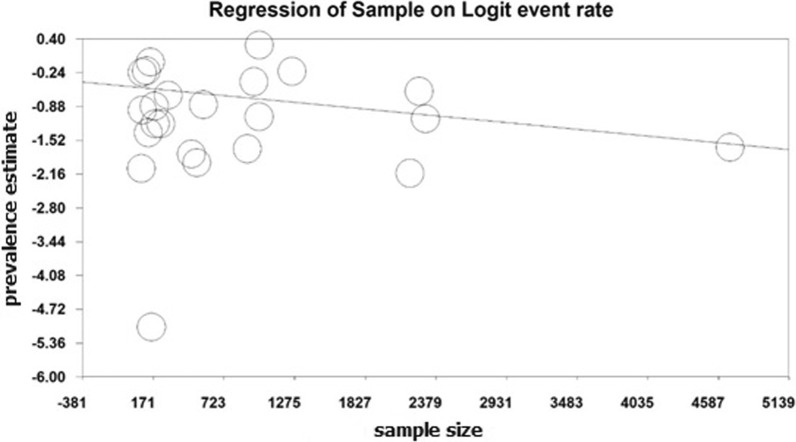
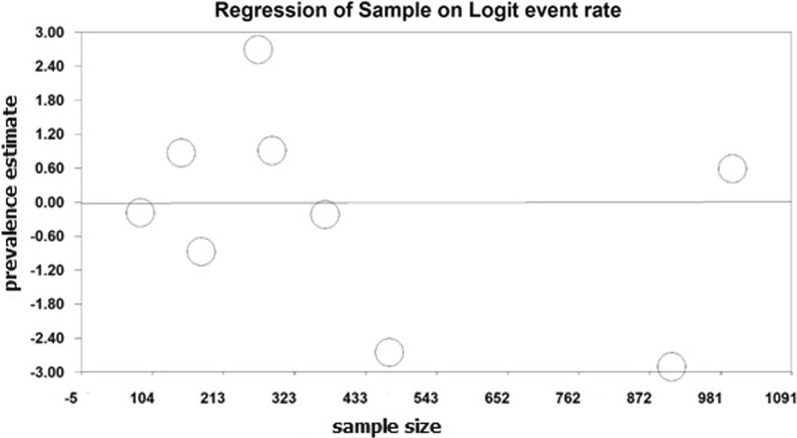
Meta-regression test
In order to investigate potential factors affecting the heterogeneity of depression, anxiety and stress prevalence, and to assess study effect size, meta-regression technique was used (Figs. 5, 6 and 7). According to Fig. 5, the prevalence of depression decreases with increasing sample size, and this is statistically significant (P < 0.05). Considering Fig. 6, increasing the sample size, decreases the prevalence of anxiety, which is statistically significant (P < 0.05). Moreover, according to Fig. 7, there was no significant relationship between sample size and the prevalence of stress (P = 0.829).
Fig. 5.
Meta-regression chart of the prevalence of depression by sample size
Fig. 6.
Meta-regression chart of the prevalence of anxiety by sample size
Fig. 7.
Meta-regression chart of the prevalence of stress by sample size
Subgroup analysis based on the type of job of the hospital’s Hospital staff
Considering the results presented in Table 2, in Hospital staff other than physicians and nurses, the prevalence of depression is 20.6% (95% CI 13.1–30.9%), the prevalence of anxiety is 27% (95% CI 20.1–35.3%), and the prevalence of stress is 36.4% (95% CI 18.3–59.5%). Moreover, in physicians, the prevalence of depression is 40.4% (95% CI 36.4–44.5%), the prevalence of anxiety 19.8% (95% CI 7.1–44.3%), and the prevalence of stress is 93.7% (95% CI 90–96%). Furthermore, the prevalence of depression, and anxiety in nurses is 28% (95% CI 16–44.2%). and 22.8% (95% CI 17–29.8%), respectively (Table 2).
Table 2.
Subgroup analysis
| Hospital medical staff | Type of disorder | Number of articles | Sample size | I2 | Begg and Mazumdar | Prevalence (95% CI) |
|---|---|---|---|---|---|---|
| Hospital staff (non-physicians and nurses) | Depression | 15 | 10,658 | 99.1 | 0.317 | 20.6 (95% CI 13.1–30.9) |
| Anxiety | 17 | 11,062 | 95.5 | 0.258 | 27 (95% CI 20.1–35.3) | |
| Stress | 8 | 3551 | 99 | 0.180 | 36.4 (95% CI 18.3–59.5) | |
| Physicians | Depression | 2 | 643 | 4.2 | – | 40.4 (95% CI 36.4–44.5) |
| Anxiety | 2 | 643 | 90.7 | – | 19.8 (95% CI 7.1–44.3) | |
| Stress | 1 | 268 | 0 | – | 93.7 (95% CI 90–96) | |
| Nurses | Depression | 4 | 8063 | 99.2 | 0.667 | 28 (95% CI 16–44.2) |
| Anxiety | 4 | 8063 | 96.5 | 0.514 | 22.8 (95% CI 17–29.8) |
Accordingly, it is reported that the prevalence of depression in physicians is much higher than nurses and Hospital staff, and the prevalence of anxiety in Hospital staff is much higher than other groups studied. Also, only one study reviewed by Australian physicians shows a much higher prevalence of stress than the results of other studies in nurses and Hospital staff.
Discussion
The aim of the present study was to conduct a systematic review, meta-analysis and meta-regression, to determine the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients. According to our findings, the overall prevalence of stress is 45%, and also according to the analysis of subgroups, the prevalence of stress in physicians is higher than other groups of Hospital staff. The highest prevalence of stress was reported in the study of Abdulah et al. [27] with 93.7%, and the lowest prevalence was related to the study of Chew et al. [9] with 5.2%. The most comprehensive study in terms of sample size was related to a research conducted by Kazmi et al. [18] in Iran, who reported the prevalence of stress as 64.3%, among Hospital staff dealing with the COVID-19 patients. Anxiety, depression and stress have been studied in Hospital staff treating other groups of patients. For instance, in the meta-analysis performed by Costello et al. [37], the prevalence of stress in staff caring for patients with dementia was 18.34%, and in the study of Cheung et al. [38], the prevalence of stress in Hong Kong nurses was reported to be 8.73%. A different piece of research conducted by Kulsoom et al. [39] stated that the prevalence of stress in medical students in Saudi Arabia was 30–41%%. The findings of our work demonstrate a higher prevalence of behavioral disorders in Hospital staff caring for the COVID-19 patients. This indicates urgent attention and possible interventions are required by related policy-makers and authorities.
In modern societies, stress at work is an important factor to consider in the healthcare sector [40]. Stress at workplaces raises concerns about people’s mental health [41]. Workplace stress is defined as an emotional, perceptual, behavioral, and physiological response pattern to adverse aspects of work, organization, and the workplace environment [42]. The effect of job stress on physical and mental illness is significant [43]. Job or job-related stresses are undoubtedly one of the leading causes of mental health concerns globally [44]. High levels of stress can impair employees’ performance as well as negatively affect their attitudes and behaviors [45, 46]. Additionally, occupational stress has been shown to impose a cost of 300 to 400 million dollars on healthcare systems [47]. For this reason, identifying the causes and the prevalence of workplace stress among Hospital staff caring for the COVID-19 patients is important, and can help to protect and safeguard the workforce as well as to improve the quality of service provided to patients.
According to our systemic review and meta-analysis, the overall prevalence of anxiety is 25.8%. Considering the subgroups analysis, the prevalence of anxiety in physicians is lower than other Hospital staff, although the CI is wide and the difference is not significant. The highest prevalence of anxiety was related to the study of Kazmi et al. [18] with 57%, and the lowest prevalence was related to the work of Ong et al. [20] with 0.6%. The most comprehensive study in terms of the sample size was conducted by Liu-2 et al. in China [33], which reported a 16% prevalence of anxiety among Hospital staff caring for the COVID-19 patients. The prevalence of anxiety as a disorder has also been assessed in other contexts. For instance, in a meta-analysis conducted by Fawzy et al. [48], the prevalence of anxiety in Egyptian medical students was 73%, and in the study of Cheung et al. [38], prevalence of anxiety in Hong Kong nurses was reported to be 50.1%, which is higher than the current study reporting the prevalence of anxiety. Nevertheless, Kisely et al. [49] reported that the prevalence of anxiety in the general American population was 10.5%, indicating that the prevalence of anxiety in the Hospital staff caring for the COVID-19 patients is higher than in the general population. Such differences may be due to the selection of more specialized keywords in search, review of study quality and evaluation of articles by two researchers in order to prevent the entry of irrelevant articles.
Anxiety is caused by the inability to resolve mental conflicts, and largely parts of a person's mental strength are spent on resolving psychological conflicts. For this reason, people with psychological illnesses are unable to properly use their abilities and talents to the optimum levels. Such psychological contradictions and conflicts, deteriorate their strength and mental energy, and cause inconsistencies in mental investments in all psychological needs and dimensions [50]. The key negative consequences of anxiety include reduced quality of life, inability and greater need for health services and increased mortality. Therefore, early detection and appropriate treatment prevent such consequences [51–53]. Hitherto, various methods have been identified that reduce anxiety, such as support from family and friends, socialization, proper nutrition [54], mental preparation, light exercise, music, psychotherapy [55], adequate rest, use of sleep medicine, prescription of anti-anxiety drugs [54], relaxation training [56], and aerobic exercise [57].
Similarly, according to our findings, the prevalence of depression is 24.3% and also according to the subgroup's analysis, the prevalence of depression in physicians is higher than in other Hospital staff. The highest prevalence of depression was related to a study conducted by Kazmi et al. [18] with 61.1%, and the lowest prevalence was reported in work of Ong et al. [20] with 0.6%. The most comprehensive study in terms of sample size was performed in the research of Liu-2 et al. [33] that reported the prevalence of anxiety among Hospital staff caring for the COVID_19 patients as 34.6%. Research works on the depression prevalence have been done in other contexts as well. For instance, in a meta-analysis conducted by Costello et al. [37], the prevalence of depression in patients with dementia was reported as 6.29%, and in the piece of research by Lei et al. [58], the prevalence of depression in Chinese physicians was reported as 23.8%. Sarokhani et al. [59] demonstrated that the prevalence of depression in Iranian medical students was 23%. Moreover, in a meta-analysis study by Mata et al. [60], the prevalence of depression in physicians was reported as 20.9%. Our study demonstrates that the prevalence of depression in the hospitals’ Hospital staff caring for the COVID-19 patients is higher than in the above-mentioned contexts. Yet, it reports less of depression prevalence than the depression rates reported in the studies of Kisely et al. [49] and Tung et al. [61].
Depression is among the five most debilitating disorders, and it is predicted to be one of the key challenges in the developed nations by 2030 [36]. Depression is often conceptualized as a set of negative symptoms such as negative mood, negative cognition, and avoidance behaviors. Accordingly, effective psychological therapies for depression, such as cognitive–behavioral therapy and interpersonal therapies, have focused on reducing or improving these negative aspects by shifting dysfunctional beliefs, identifying avoidance behaviors, and resolving interpersonal problems [62, 63].
The results of this study show that the prevalence of depression, anxiety and stress in the Hospital staff caring for the COVID-19 patients is high. Our work has also discussed the importance of treating these disorders and their potential impact on all aspects of a medical worker’s life. Therefore, interventions are necessary to improve such workers’ lifestyles, through regular monitoring of potential depression, anxiety and stress disorders, and to reduce the associated side effects. In addition, since depression, anxiety and stress can be prevented in the first place, and can also be controlled and treated if they advance, it is necessary to offer full training to Hospital staff on depression, anxiety and stress, and how they could be prevented. Moreover, it is essential to control and treat these disorders as early as possible, and through timely diagnosis. Due to the high prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients, it is recommended that physicians be more attentive to the symptoms of these disorders. Furthermore, media should provide related information with the aim of raising people's awareness to prevent delayed diagnosis.
Limitations
One of the limitations of this research is the lack of uniform reporting in the selected studies, the non-uniformity of the methodologies. Moreover, due to the limitation in finding articles from different continents, and the lack of uniform distribution of articles in different geographical locations, subgroup analysis was not performed on different continents, or ethnic groups. Also, given that the COVID-19 pandemic started in China, most of the studies reviewed include articles from this country, and this situation affects the generalization of results worldwide.
Conclusions
The results of this study clearly demonstrate that the prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients are high. Therefore, the healthcare authorities, and decision-makers, nationally and internationally, should take measures to reduce these disorders in Hospital staff treating the COVID-19 patients. This increases the productivity of the Hospital staff, speeds up the measures to control the pandemic, and provides more effective treatment procedures for the COVID-19 patients.
Acknowledgements
By Student Research Committee of Kermanshah University of Medical Sciences.
Abbreviations
- SARS
Severe Acute Respiratory Syndrome
- MERS
Middle East Respiratory Syndrome
- WHO
World Health Organization
- PHEIC
Public Health Emergency of International Concern
- ICTV
International Committee on Virus Classification
- STROBE
Strengthening the Reporting of Observational studies in Epidemiology
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Authors’ contributions
NS and HKH and MK contributed to the design, MM statistical analysis, participated in most of the study steps. BKH and SHSH and AD and SE prepared the manuscript. All authors read and approved the final manuscript.
Funding
By Student Research Committee of Kermanshah University of Medical Sciences, Deputy for Research and Technology, Kermanshah University of Medical Sciences (IR) (3010299). This deputy has no role in the study process.
Availability of data and materials
Datasets are available through the corresponding author upon reasonable request.
Ethics approval and consent to participate
Ethics approval was received from the ethics committee of deputy of research and technology, Kermanshah University of Medical Sciences (3010299).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nader Salari, Email: n_s_514@yahoo.com.
Habibolah Khazaie, Email: hakhazaie@gmail.com.
Amin Hosseinian-Far, Email: amin.hosseinian-far@northampton.ac.uk.
Behnam Khaledi-Paveh, Email: bkhaledi@ymail.com.
Mohsen Kazeminia, Email: mohsenkaz221@gmail.com.
Masoud Mohammadi, Email: Masoud.mohammadi1989@yahoo.com.
Shamarina Shohaimi, Email: shamarina@upm.edu.my.
Alireza Daneshkhah, Email: ac5916@coventry.ac.uk.
Soudabeh Eskandari, Email: sodabeh.eskandari@gmail.com.
References
- 1.Alavi-Moghadam M. A novel coronavirus (COVID-19) outbreak from Wuhan City in China, rapid need for emergency departments preparedness and response; a Letter to Editor. Arch Acad Emerg Med. 2020;8(1):2645–4904. [PMC free article] [PubMed] [Google Scholar]
- 2.Al- Mandhari A, et al. Coronavirus disease 2019 outbreak: preparedness and readiness of countries in the Eastern Mediterranean Region. East Mediterr Health J. 2020;26(2):136–137. doi: 10.26719/2020.26.2.136. [DOI] [PubMed] [Google Scholar]
- 3.Lai CC, et al. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020;55(4):105946. doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai CC, Shih TP, Ko WC, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Cov-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020; 105924. [DOI] [PMC free article] [PubMed]
- 5.World Health Organization . Laboratory testing of human suspected cases of novel coronavirus (nCoV) infection: interim guidance. Geneva: World Health Organization; 2020. [Google Scholar]
- 6.Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for depression in the general population with the center for epidemiologic studies depression (CES-D): a systematic review with meta-analysis. PLoS ONE. 2016;11(5):e0155431. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line hospital staff fighting against COVID-19 in Gansu. Front Psychiatry. 2020;11:386. doi: 10.3389/fpsyt.2020.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of Hospital staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e923549–e923551. doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immunity. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among Hospital staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azizi M, Lamyian M, Faghihzadeh S, NEMAT EM. The effect of counseling on anxiety after traumatic childbirth in nulliparous women; a single blind randomized clinical trial. 2010.
- 13.Liu C-Y, Yang Y-Z, Zhang X-M, Xu X, Dou Q-L, Zhang W-W, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020:1–17. [DOI] [PMC free article] [PubMed]
- 14.Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor SH, Mohammadi M, Rasoulpoor SH, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noorbala AA, Mohammad K, Bagheri Yazdi SA, Yasami MT. Study of mental health status of individuals above 15 years of age in Islamic Republic of Iran in the year 1999. Hakim Res J. 2002;5(1):1–10. [Google Scholar]
- 16.Salari N, Mohammadi M, Vaisi-Raygani A, Abdi A, Shohaimi S, Khaledipaveh B, Daneshkhah A, Jalali R. The prevalence of severe depression in Iranian older adult: a meta-analysis and meta-regression. BMC Geriatr. 2020;20(1):39. doi: 10.1186/s12877-020-1444-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;67:144–145. doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kazmi SSH, Hasan K, Talib S, Saxena S. COVID-19 and lockdown: a study on the impact on mental health. SSRN 3577515. 2020.
- 19.Gautam M, Kaur M, Mahr G. COVID-19 associated psychiatric symptoms in healthcare workers: viewpoint from internal medicine and psychiatry residents. Psychosomatics. 2020;61(5):579–581. doi: 10.1016/j.psym.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ong JJ, Bharatendu C, Goh Y, Tang JZ, Sooi KW, Tan YL, et al. Headaches associated with personal protective equipment—a cross-sectional study among frontline healthcare workers during COVID-19. Headache J Head Face Pain. 2020;60(5):864–877. doi: 10.1111/head.13811. [DOI] [PubMed] [Google Scholar]
- 21.Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guixia L, Hui Z. A study on burnout of nurses in the period of COVID-19. Psychol Behav Sci. 2020;9(3):31–36. doi: 10.11648/j.pbs.20200903.12. [DOI] [Google Scholar]
- 23.Aghili SM, Arbabi M. The COVID-19 pandemic and the health care providers; What does it mean psychologically? Adv J Emerg Med. 2020;4(2s):e63-e. [Google Scholar]
- 24.Dimitriu MC, Pantea-Stoian A, Smaranda AC, Nica AA, Carap AC, Constantin VD, et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. 2020:109972. [DOI] [PMC free article] [PubMed]
- 25.Sharif S, Amin F, Hafiz M, Benzel E, Peev NA, Dahlan RH, et al. COVID 19-depression and neurosurgeons. World Neurosurg. 2020;140:401–410. doi: 10.1016/j.wneu.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geoffroy PA, Le Goanvic V, Sabbagh O, Richoux C, Weinstein A, Dufayet G, et al. Psychological support system for hospital workers during the Covid-19 outbreak: rapid design and implementation of the Covid-Psy hotline. Front Psychiatry. 2020;11:511. doi: 10.3389/fpsyt.2020.00511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdulah DM, Musa DH. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med: X. 2020:100017. [DOI] [PMC free article] [PubMed]
- 28.Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, et al. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019 (COVID-19) Clin Psychol Psychother. 2020;27(3):384–395. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposureduring COVID-19 outbreak. PLoS ONE. 2020 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang J, Han M, Luo T, Ren A, Zhou X. Mental health survey of 230 Hospital staff in a tertiary infectious disease hospital for COVID-19. Zhonghua lao dong wei shen zhi ye bing za zhi= Zhonghua laodong weisheng zhiyebing zazhi= Chin J Ind Hyg Occup Dis. 2020;38:E001-E. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- 31.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976-e. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):790–798. doi: 10.1016/S2214-109X(20)30204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry research. 2020:112936. [DOI] [PMC free article] [PubMed]
- 35.Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang W-R, Wang K, Yin L, Zhao W-F, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Costello H, Walsh S, Cooper C, Livingston G. A systematic review and meta-analysis of the prevalence and associations of stress and burnout among staff in long-term care facilities for people with dementia. Int Psychogeriatr. 2019;31(8):1203–1216. doi: 10.1017/S1041610218001606. [DOI] [PubMed] [Google Scholar]
- 38.Cheung T, Wong SY, Wong KY, Law LY, Ng K, Tong MT, et al. Depression, anxiety and symptoms of stress among baccalaureate nursing students in Hong Kong: a cross-sectional study. Int J Environ Res Public Health. 2016;13(8):779. doi: 10.3390/ijerph13080779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kulsoom B, Afsar NA. Stress, anxiety, and depression among medical students in a multiethnic setting. Neuropsychiatr Dis Treat. 2015;11:1713. doi: 10.2147/NDT.S83577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4:e004185. doi: 10.1136/bmjopen-2013-004185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nakao M. Work-related stress and psychosomatic medicine. BioPsychoSoc Med. 2010;4:1. doi: 10.1186/1751-0759-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zoni S, Lucchini RG. European approaches to work-related stress: a critical review on risk evaluation. Saf Health At Work. 2012;3:43–49. doi: 10.5491/SHAW.2012.3.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shirazi A, Rasekhnia M, Ajdari GH. An empirical examination of the relationship between occupational stress and mental health. Interdiscip J Contemp Res Bus. 2011;3:101–109. [Google Scholar]
- 44.Nakao M. Work-related stress and psychosomatic medicine. BiopsychoSoc Med. 2010;4:4. doi: 10.1186/1751-0759-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gilboa S, Shirom A, Fried Y, Cooper C. A meta-analysis of work demand stressors and job performance: examining main and moderating effects. Pers Psychol. 2008;61:227–271. doi: 10.1111/j.1744-6570.2008.00113.x. [DOI] [Google Scholar]
- 46.Barling J, Kelloway EK, editors. Handbook of work stress. London: Sage Publication; 2004. p. 710. [Google Scholar]
- 47.Mohammadi M, Vaisi-Raygani A, Jalali R, Salari N. Prevalence of job stress in nurses working in Iranian hospitals: a systematic review, meta-analysis and meta-regression study. JHSW. 2020;10(2):119–128. [Google Scholar]
- 48.Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017;255:186–194. doi: 10.1016/j.psychres.2017.05.027. [DOI] [PubMed] [Google Scholar]
- 49.Kisely S, Alichniewicz KK, Black EB, Siskind D, Spurling G, Toombs M. The prevalence of depression and anxiety disorders in indigenous people of the Americas: a systematic review and meta-analysis. J Psychiatr Res. 2017;84:137–152. doi: 10.1016/j.jpsychires.2016.09.032. [DOI] [PubMed] [Google Scholar]
- 50.Akbari B. Relationship between commitment to prayer and anxiety, according to sociodemographic variables among students of Islamic Azad University Anzali. J Psychol Relig. 2009;2(3):145–155. [Google Scholar]
- 51.Boyd MA. Psychiatric nursing: contemporary practice. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 52.Bergua V, Meillon C, Potvin O, Bouisson J, Le Goff M, Rouaud O, Ritchie K, Dartigues J-F, Amieva H. The STAI-Y trait scale: psychometric properties and normative data from a large population-based study of elderly people. Int Psychogeriatr. 2012;24(7):1163–1171. doi: 10.1017/S1041610212000300. [DOI] [PubMed] [Google Scholar]
- 53.Smalbrugge M, Pot A, Jongenelis K, Beekman A, Eefsting J. Prevalence and correlates of anxiety among nursing home patients. J Affect Disord. 2005;88(2):145–153. doi: 10.1016/j.jad.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 54.Rafii F. Effect of aerobic exercise group on the mental health of nulliparous women. Thesis in Persian. Mashhad: Mashhad School of Nursing and Midwifery. 2002.
- 55.Sedaghati P. Effects of regular exercise on anxiety level of the second and third trimester of pregnancy in Qom. Thesis in Persian. Tehran: Tarbiat Modarres University. 2003.
- 56.Teixeira J, Martin D, Prendiville O, Glover V. The effects of acute relaxation on indices of anxiety during pregnancy. J Psychosom Obstetr Gynecol. 2005;26(4):271–276. doi: 10.1080/01674820500139922. [DOI] [PubMed] [Google Scholar]
- 57.Marie J. Birthing Ball During pregnancy. 2010. 2012. http://www.livestrong.com. Accessed 1(6).
- 58.Lei X-Y, Xiao L-M, Liu Y-N, Li Y-M. Prevalence of depression among Chinese University students: a meta-analysis. PLoS ONE. 2016;11(4):e0153454. doi: 10.1371/journal.pone.0153454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sarokhani D, Delpisheh A, Veisani Y, Sarokhani MT, Manesh RE, Sayehmiri K. Prevalence of depression among university students: a systematic review and meta-analysis study. Depress Res Treat. 2013;2013. [DOI] [PMC free article] [PubMed]
- 60.Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373–2383. doi: 10.1001/jama.2015.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tung Y-J, Lo KK, Ho RC, Tam WSW. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Educ Today. 2018;63:119–129. doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 62.Fava M. Diagnosis and definition of treatment-resistant depression. Biol Psychiatry. 2003;53(8):649–659. doi: 10.1016/S0006-3223(03)00231-2. [DOI] [PubMed] [Google Scholar]
- 63.Raes F, Williams GM, Hermans D. Reducing cognitive vulnerability to depression: a preliminary investigation of Memory Specificity Training (MEST) in inpatients with depressive symptomology. J Behav Ther Exp Psychiatry. 2009;40:24–38. doi: 10.1016/j.jbtep.2008.03.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available through the corresponding author upon reasonable request.