Description
Oral focal mucinosis (OFM) is a relatively rare, benign soft tissue lesion of unknown aetiology. It invariably presents as a localised sessile or pedunculated gingival mass. This paper highlights a case of large OFM involving the left hemimandible in a 37-year-old otherwise healthy patient. The large-sized lesion resulted in tongue displacement and difficulty in speech and mastication. The clinical differential diagnosis included peripheral ossifying fibroma, peripheral giant cell lesion, soft tissue sarcoma, pyogenic granuloma, gingival hyperplasia and traumatic fibroma. Imaging revealed mild resorption of the alveolar bone of the mandible. Final diagnosis was based on the histopathological evaluation using H&E and silver stained sections of the lesion. Immunohistochemistry (IHC) analysis was conducted to rule out neural tumour with myxoid degeneration. The lesion was managed by surgical excision, through a transoral approach. No recurrence was seen at the end of 2-year follow-up.
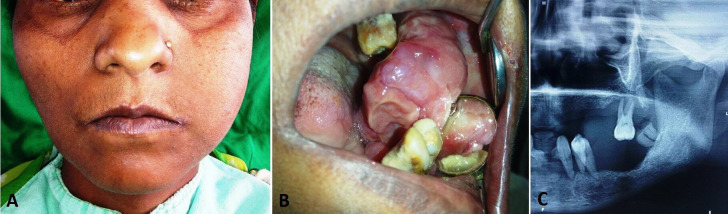
A 37-year-old woman presented to oral surgery clinic with a chief complaint of painless, slow-growing intraoral mass. No contributing medical or dental history was reported. No history of trauma or drug therapy was present. On extraoral clinical examination, a diffuse swelling on the lower face was present, extending from below the ala-tragus line to the lower border of the mandible (figure 1A). The overlying skin appeared normal with no tenderness and local rise in temperature. Intraoral examination revealed a large mucosal growth occupying the left posterior half of the oral cavity, spanning anterior-posteriorly from the retromolar area to the lower left canine tooth and extending over to the floor of the mouth buccolingually (figure 1B). The surface of the lesion appeared inflamed, with areas of indentation from the adjoining tooth. The speech of the patient was altered, with limitations in tongue movement. The lesion readily bled on manipulation. Oral hygiene was poor, with presence of halitosis and severe periodontally compromised teeth. Orthopantomogram revealed smooth, saucer-like resorption of the alveolar bone in the left premolar-molar region, possibly due to pressure effect from the growth (figure 1C).
Figure 1.
Photographs showing presentation of the lesion: extraoral view showing swelling on the left side of the lower face (A), intraoral presentation of the lesion as a large space-occupying mass (B) and orthopantomogram showing the resorbed alveolar bone over the left body of the mandible (C).
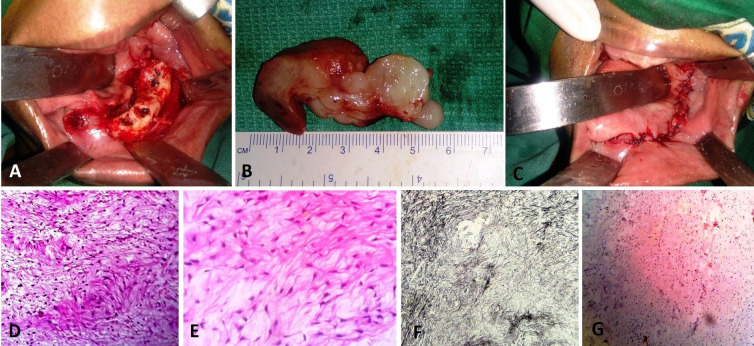
Based on the clinical and imaging findings, differential diagnosis of the lesion included peripheral ossifying fibroma, peripheral giant cell lesion, soft tissue sarcoma, pyogenic granuloma, gingival hyperplasia and traumatic fibroma. An incision biopsy of the lesion revealed squamous epithelium with underlying dermis having multiple plump fusiform fibroblasts within the myxomatous stroma. The finding was suggestive of OFM. Wide excision of the lesion was planned and executed under general anaesthesia. The lesion was approached intraorally and removed in toto, along with the periodontally compromised teeth (figure 2A, B). The alveolar bone underlying the lesion was exposed and superficial ostectomy was done to achieve smooth and flat crestal bone. The mental nerve was identified and preserved. The mucosal tissue was undermined and advanced to attain primary closure (figure 2C).
Figure 2.
Intraoperative images showing the surgical site after removal of the lesion: the mental nerve was preserved and can be appreciated on the buccal aspect of the alveolar bone (A); the excised lesion measuring about 6 cm in its largest dimension (B); and closure of the surgical site by advancement of the buccal and lingual mucosa (C). Photomicrographs showing the connective tissue with stellate-shaped fibroblasts interspersed between thin collagen fibre bundles (H&E, ×10) (D); multiple plump fusiform fibroblasts within myxomatous background (H&E, ×40) suggestive of oral focal mucinosis (E); silver impregnated stained section showing the myxoid area with delicate collagen fibres separated by mucinous material (×100) (F); and immunohistochemistry showing negativity for S-100 in the myxoid area ruling out myxomatous lesion of neural origin (G).
The excised specimen was submitted for histological evaluation. H&E stained sections of the specimen showed connective tissue with stellate-shaped cells in an abundant myxoid stroma. Deeper sections showed multiple plump fibroblasts with thin collagen fibre bundles distributed within myxomatous background (figure 2D, E). No evidence of granulomatous changes, nuclear atypia, mitosis or necrosis was seen in the excised specimen. Besides conventional H&E stain, special connective tissue staining is often required for confirmatory diagnosis of OFM. This includes reticulin stain, which uses silver and relies on the argyrophilic properties of the connective tissue fibres. The silver impregnated staining showed delicate collagen fibrils separated by mucinous material and myxoid tissue area surrounded by dense collagenous connective tissue (figure 2F). The above findings were suggestive of OFM. IHC analysis for S-100 protein was conducted to rule out neural tumour with myxoid degermation. IHC study was negative for this marker in the mucinous area, ruling out other myxomatous lesions of neural origin and confirming the diagnosis of OFM (figure 2G). The patient was kept on periodic recall visit. Normal healing was seen with no recurrence at 2-year follow-up.
Myxoid tumour is a connective tissue neoplasm composed of a clear, mucoid substance.1 2 Myxoid lesion of the oral cavity may be benign in nature and originate from adipose cells (eg, myxolipoma, myxiliposarcoma), muscles (eg, myxoid leiomyosarcoma), nerves (eg, myxoid neurofibroma, neurothekeoma) or odontogenic tissues (eg, odontogenic myxoma). Malignant myxoid lesion includes myxofibrosarcoma, myxoid chondrosarcoma, myxoid leiomyosarcoma and malignant ossifying fibromyxoid tumour.3 OFM is a rare, benign myxoid tumour of unknown aetiology. It clinically manifests as a small mucosal growth, with more than three-fourths of cases involving the gingiva and the hard palate.2 Clinically, it presents as a small pedunculated or sessile mass.1 However, large lesions like the one reported in the present case have been infrequently reported. Histologically, it consists of non-encapsulated but well-localised nidus of loose, myxomatous connective tissue. OFM may show histological similarity with nerve sheath myxoma and should be differentiated from the same using IHC analysis.2 In the present case, the lesion was negative for S-100 protein marker, ruling out neurogenic origin. Other staining methods used for histological assessment include Alcian blue and silver impregnated staining.4 Management of the lesion is primarily by conservative surgical excision and recurrence is unlikely.
Learning points.
OFM is a rare disease and should be differentiated from other regular pathologies of oral cavity like giant cell lesion, pyogenic granuloma, gingival hyperplasia and traumatic fibroma, which has similar clinical presentation.
Histological differential diagnosis includes; soft-tissue myxoma, nerve sheath myxoma, odontogenic myxoma and fibroepithelial hyperplasia with myxoid degeneration and beside H & E study, alcian blue and sliver impregnated staining along with IHC analysis play an important role in final diagnosis of the pathology.
A large lesion (larger than 5 cm), as highlighted in the present case is extremely rare and when present can cause facial asymmetry, difficulty in swallowing, speech and maintenance of oral hygiene.
Footnotes
Contributors: KN was involved in the management of the case, manuscript writing and finalising the draft. RP and SRK conducted the literature review and provided histological assessment of the pathology.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Moghadam S, Lotfi A, Moghadam F, et al. Large ulcerated oral focal mucinosis: a rare case report. J Clin Diagnos Res 2017;11:ZJ01–2. [Google Scholar]
- 2.Kumar SM, Kumar HM, Sivakumar V, et al. A diagnostic challenge: pyogenic granuloma or oral focal mucinosis. BMJ Case Rep 2015;2015:bcr2015210150. 10.1136/bcr-2015-210150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bajpai M, Pardhe N. A simplified working classification proposed for myxoid tumors of oral cavity. Iran J Pathol 2017;12:413–4. 10.30699/ijp.2017.28324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nilesh K, Kothi HS, Patil R, et al. Oral focal mucinosis of posterior maxilla. J Oral Maxillofac Pathol 2017;21:273–6. 10.4103/jomfp.JOMFP_242_15 [DOI] [PMC free article] [PubMed] [Google Scholar]