Abstract
Acute ankle sprain is the most common lower limb injury in athletes and accounts for 16%-40% of all sports-related injuries. It is especially common in basketball, American football, and soccer. The majority of sprains affect the lateral ligaments, particularly the anterior talofibular ligament. Despite its high prevalence, a high proportion of patients experience persistent residual symptoms and injury recurrence. A detailed history and proper physical examination are diagnostic cornerstones. Imaging is not indicated for the majority of ankle sprain cases and should be requested according to the Ottawa ankle rules. Several interventions have been recommended in the management of acute ankle sprains including rest, ice, compression, and elevation, analgesic and anti-inflammatory medications, bracing and immobilization, early weight-bearing and walking aids, foot orthoses, manual therapy, exercise therapy, electrophysical modalities and surgery (only in selected refractory cases). Among these interventions, exercise and bracing have been recommended with a higher level of evidence and should be incorporated in the rehabilitation process. An exercise program should be comprehensive and progressive including the range of motion, stretching, strengthening, neuromuscular, proprioceptive, and sport-specific exercises. Decision-making regarding return to the sport in athletes may be challenging and a sports physician should determine this based on the self-reported variables, manual tests for stability, and functional performance testing. There are some common myths and mistakes in the management of ankle sprains, which all clinicians should be aware of and avoid. These include excessive imaging, unwarranted non-weight-bearing, unjustified immobilization, delay in functional movements, and inadequate rehabilitation. The application of an evidence-based algorithmic approach considering the individual characteristics is helpful and should be recommended.
Keywords: Ankle sprain, Rehabilitation, Athlete, Sport injury, Return to play, Exercise therapy
Core Tip: Acute ankle sprain is the most common injury in athletes. Several interventions have been recommended in the management of acute ankle sprains, among them exercise and bracing have been recommended with higher level of evidence and should be incorporated in the rehabilitation process. An exercise program should be comprehensive and progressive including range of motion, stretching, strengthening, neuromuscular, proprioceptive and sport-specific exercises. The application of an evidence-based algorithmic approach considering the individual characteristics is helpful and should be recommended.
INTRODUCTION
Acute ankle injury is one of the most prevalent musculoskeletal injuries[1,2]. Ankle sprain is the most common lower limb injury in physically active individuals[3,4]. Each day, almost one ankle sprain occurs per 10000 persons in Western countries[1,5] and over two million ankle sprains are treated annually in emergency departments of the United States and United Kingdom[6]. In sport, the incidence is even higher, accounting for 16%-40% of all sport-related trauma cases[1,7,8].
Approximately 40% of all traumatic ankle injuries and nearly half of all ankle sprains occur during athletic activity[4,9,10], with basketball (41.1%), American football (9.3%), and soccer (7.9%) having the highest incidence[4,6,11]. Ankle sprain is more prevalent in females, children, and athletes taking part in indoor and court sports[9].
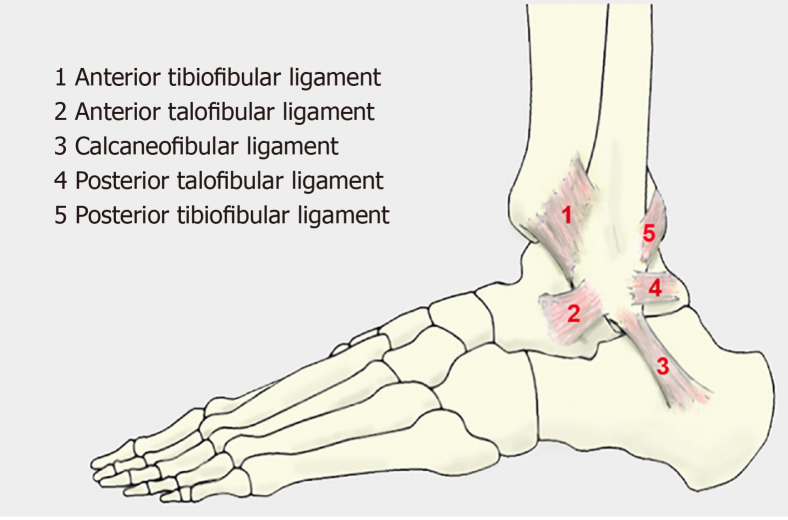
Besides the bony and muscular structures, several ligaments have a major contribution to the stability of the ankle joint, which are distributed in lateral, medial, and syndesmotic areas (Figure 1).
Figure 1.
Lateral ligaments of the ankle.
Almost 85% of ankle sprains involve the lateral ligaments. In about 65% of cases, isolated injury of the anterior talofibular ligament (ATFL) and in 20%, injury of both ATFL and the calcaneofibular ligament exist. Injuries of the posterior talofibular ligament are unusual[12]. The remaining 15% involves syndesmotic and medial ankle sprains[9]. A syndesmotic ankle sprain is an injury to one or more of the ligaments comprising the distal tibiofibular junction and is frequently known as "high ankle sprain"[10].
Despite its excessive prevalence, the long-term prognosis of an acute ankle sprain is not favorable and a high proportion of patients experience persistent residual symptoms (up to 40%-50%)[13,14] and injury recurrence[6]. Furthermore, the prevalence of underdiagnosed injuries associated with ankle sprain, such as tendinous and osteochondral injuries and midfoot fractures are high[15]. Therefore, direct and indirect financial and societal costs for managing lateral ankle sprains and their sequelae lead to a high socioeconomic burden[10,16,17].
In this review, we aimed to discuss different clinical aspects of lateral ankle sprain in athletes and introduce a novel and practical algorithmic approach for proper diagnosis and management.
RISK FACTORS
Several parameters have been suggested as potential risk factors for ankle sprain. These are classified as intrinsic or extrinsic. Some of the intrinsic risk factors are modifiable and their identification may be helpful in the prevention of potential injury[18].
Several studies have investigated proposed risk factors in athletic and military populations. These include demographic (including age[19], gender[20], weight[19-22], height[20,21], body mass index[20,21,23,24], limb dominance[20]), anatomical (foot type[20], foot and ankle alignment, including foot hyper-pronation)[20,21], laxity (generalized joint laxity[20,21,24], ankle-joint laxity[19-21,24]), range of motion (ROM), including ankle and first metatarsophalangeal ROM[21,24-27]), muscle strength[19,20,23,26,27], muscle-reaction time[20,23,24], balance (single leg balance and star excursion balance tests) and proprio-ception[20,21,23-26], previous history of ankle sprain[11,21,22,24,25], and sport-related parameters (including type of sport[25], level of competition[25], playing on artificial grass[25], playing position[25], type of sport shoe[11], lack of warm-up stretching[11], and landing technique after a jump[25]). There is no convincing evidence on how significant or effective these parameters are. However, previous history of an ankle sprain, being overweight, ankle joint laxity, and impaired balance are some exceptions that the majority of studies have agreement on their importance[11,20-22,24,25,28]. For example, it has been shown that an overweight player with a previous ankle sprain is 19 times more likely to sustain noncontact ankle sprain compared to a normal-weight player with no previous ankle sprain[22].
CLINICAL PRESENTATION
History
Accurate clinical assessment of the ankle injury needs a comprehensive and organized history[29]. Athletes usually report shifting the center of gravity over the lateral border of the weight-bearing leg as an injury mechanism. It may be caused by catching the lateral side of the foot on the ground, awkward landing on the opponent's foot, or contacting with the inside of the opponent's supporting leg during a slide tackle[30,31]. The patients typically complain of lateral ankle swelling (local or diffuse), pain, bruising, and limited ROM[32]. The ability of weight-bearing immediately after injury is important and may influence the decision to order standard radiology[33].
History must also include age, demographic data, time since injury, exact mechanism, nature of injury (acute or chronic), location of pain, previous history of ankle sprain or instability, history of other lower extremity pain or deformities, mechanical symptoms (locking or feeling of loose bodies) and paresthesia[33-36].
In the case of a suspected ankle sprain, the physician should probe risk factors such as previous injury, special activity, or sport during which the injury occurred, footwear, playing surface, and the use of taping or bracing[33].
Usually, plantar flexion and inversion of the ankle is the main mechanism of lateral sprain[33]. A history of other mechanisms (e.g., forced plantar flexion, eversion, and dorsiflexion) should alert the physician about uncommon ligament injuries or fractures[37].
Physical examination
After looking for a fracture by careful palpation of the critical anatomic check-points (especially lateral and medial malleoli, the base of the fifth metatarsal and navicular bones), ecchymosis, edema, point tenderness, ROM, ligamentous laxity, and muscle strength should be carefully evaluated in all suspected ankle sprains[1,32,36,38,39].
In a typical lateral ankle sprain, ecchymosis and tenderness are located over the ATFL and calcaneofibular (CFL) ligaments. Acute injuries do not have swelling or ecchymosis over the forefoot or toes. However, in the absence of appropriate treatment and after one day, bruising and swelling may be visible down the whole foot as a result of gravity, especially if the patient has been ambulating[37]. Edema may be measured with a tape using a figure of 8 method that includes four points of lateral and medial malleoli, the base of the fifth metatarsal and navicular bone[40]. Evaluation of active, passive, and resistive ROM can help to differentiate injury to ligaments, tendons, muscles, and nerves (level 3)[41]. Also, a typical antalgic gait to protect the ankle and avoid further pain is common[7].
The provocative tests are also important. Anterior drawer and talar tilt (inversion stress) tests are utilized to evaluate lateral ankle instability. These tests should be performed in comparison with the uninjured ankle. Tests are regarded as positive in cases of increased laxity[1,39].
The anterior drawer test (ADT) is applied to assess the integrity of ATFL as it prevents anterior translation of the talus under the distal tibia. Ten millimeters of displacement in the injured ankle or more than 3-4 mm of difference in translation compared with the healthy side indicate an ATFL tear[7]. In an ATFL tear, a dimple sign may also be visible in the anterior side of the joint in 50% of cases[42].
The talar tilt test evaluates the integrity of the CFL. In this test, the angle between the talar dome and the tibial plafond is measured during forced heel inversion while the tibiotalar joint is in the neutral position. If there is more than 5° of difference with the normal side, the test is considered positive[7].
It should be noted that during the few days after injury, in the acute condition (especially when joint effusion has occurred), the physical examination may be nonspecific due to pain and swelling[36]. Therefore, all patients should be examined again 3-5 d later[43]. It was demonstrated that the ADT in this delayed examination produced the best results in comparison to stress radiography, sonography, and arthrography with a sensitivity of 96% and a specificity of 84% (level 2)[10,43].
To rule out less common syndesmotic injuries, provocative tests are helpful. These tests including the squeeze test (lower leg squeeze at midcalf), crossed-leg test (asking the individual to cross the legs with the injured leg resting at midcalf on the other knee), external rotation stress test (concurrent external rotation and dorsiflexion), heel thump test (applying gentle but firm thump on the heel with the fist) and Cotton test (applying a medial and lateral translation force to the foot) to stress the syndesmosis and elicit pain above the ankle joint[37]. Otherwise, swelling and tenderness on the medial side of the ankle, positive eversion stress test, and/or defect palpation in the soft tissues just distal to the medial malleolus may suggest probable deltoid ligament injury[7].
Assessment of the patient’s neurovascular status in the injured extremity should also be included as an essential part of the physical examination[7]. For this purpose, light touch sensation, capillary refilling, and dorsal pedal pulse should be checked[31].
In the sports setting, the sports-specific functional level of the athlete should also be assessed. Proper objective interpretation of these findings is fundamental to correct injury grading[38].
Grading
Lateral ankle sprains are characteristically classified as grade I, II, or III, based on the severity of injury to the lateral ligaments. As mentioned earlier, provocative ligament tests are challenging to accomplish at the time of acute injury; thus, clinical grading is usually rather subjective and focused on the amount of existing swelling, pain, and ecchymosis[37].
Mild swelling, tenderness, and minimal difficulty in ROM are usually seen in lower grades. However, diffuse swelling, ecchymosis, tenderness, positive provocative tests, and inability of weight bearing are associated with substantial instability in a Grade III injury. Hemarthrosis may also complicate the clinical presentation[7].
According to a systematic review, 96% of patients with all four findings of swelling, ecchymosis, tenderness and a positive ADT have a lateral ligament rupture in contrast to only 14% of individuals without all these findings[44].
There is no definite end-point for unilateral joint laxity in the ADT or talar tilt test suggesting grade III injuries[44]. Therefore, due to this problem as well as limitations imposed by pain and dysfunction, precisely recognizing grade III sprains is clinically difficult[45].
A grading system has been introduced in which more severe grades need longer rehabilitation for full recovery of the athlete[32,38] (Table 1).
Table 1.
|
Grade
|
Hemorrhage
|
Point tenderness
|
Loss of function
|
Decreased total ankle motion
|
Swelling
|
Anterior drawer test
|
Talar tilt test
|
Stress radiography
|
| I | Little or No | No | No | ≤ 5° | ≤ 0.5 cm | - | - | - |
| II | Yes | Yes | Some | > 5° and < 10° | > 0.5 and < 2 cm | + | - | - |
| IIIA | Yes | Yes (extreme) | Near total | ≥ 10° | ≥ 2 cm | + | + | ADM ≤ 3 mm |
| IIIB | Yes | Yes (extreme) | Near total | ≥ 10° | ≥ 2 cm | + | + | ADM > 3 mm |
ADM: Anterior drawer movement.
This grading system can estimate the severity of an injury and predict the prognosis[38]. However, clinical grading does not change initial management and has a limited role in the acute setting[37].
IMAGING
Plain radiography
The Ottawa Ankle and Foot Rules are clinically recommended for all acute ankle injuries in order to accelerate patient care and reduce the number and costs of unnecessary radiographs[46-48].
According to these rules, plain ankle radiography is needed, if pain exists in the malleolar zone and there is at least one of the following signs: (1) Bone tenderness in the distal 6 cm of the posterior half of the tibia or tip of the medial malleolus; (2) Bone tenderness in the distal 6 cm of the posterior half of the fibula or tip of the lateral malleolus; and (3) Inability of weight-bearing for 4 steps both immediately after injury and in the physician’s office or emergency department.
In addition, if the midfoot is painful, plain foot radiography should be requested if any of the following exist: (1) Inability to bear weight for 4 steps just after the injury and at the medical service center or office; (2) Tenderness over the navicular bone; and (3) Tenderness at the base of the fifth metatarsal bone[37,48].
These rules are the most validated tool for exclusion of ankle or mid-foot fractures in first 7 d after injury (level 1)[46-48]. Multiple studies have shown a high sensitivity of 94.6% to 100%, but a variable specificity, ranging from 11.5% to 79%, in detecting fractures in adults and children with acute ankle injury[36,44,47,49,50].
As a result, negative findings indicate that radiography is not needed. Nevertheless, due to low specificity, positive findings do not essentially reveal the existing fracture, but do show that radiography is required to approve or rule out fracture[48].
If ankle radiographs are indicated, standard trauma views including anteroposterior (AP), mortise (AP with 10°-20° internal rotation) and lateral views should be obtained[1,48]. Imaging during weight-bearing would be ideal; however, the patient's tolerance and cooperation in the acute phase may be challenging[7,36].
In the case of tenderness on the proximal part of the fifth metatarsal, an oblique foot X-ray may also be necessary. AP and mortise views in ankle dorsiflexion and plantar-flexion may also be valuable in suspected osteochondral lesions of the talus[7].
In a skeletally immature patient, Salter-Harris type 1 fracture should not be overlooked, when there is tenderness over the distal growth-plate of the tibia or fibula[31].
Stress radiography
Ankle stress radiography is generally unnecessary, unreliable, and outdated to reveal acute ligamentous injuries after ankle sprain (level 2)[1,41,51].
The technique is painful and needs local anesthesia. The result is also inconclusive due to high variability in values defined as normal as well as mechanical or manual techniques to achieve optimal stress[1].
Two types of stress radiography may be used, which generally aid in the diagnosis of medial or syndesmotic ligament injuries: (1) Talar stress views may be helpful to detect lateral instability by taking an ankle mortise view while locating the ankle in plantarflexion and inversion; and (2) External rotation stress views may be used to diagnose the syndesmotic or deltoid ligament injuries. In this view, the ankle is forced to external rotation while obtaining an AP view. Increased medial clear space width (space between the medial malleolus and talus) of more than 4 mm is indicative of deep deltoid ligament rupture and tibiofibular clear space (measured 1 cm proximal to the tibial plafond) of more than 6 mm in both the AP and mortise views suggests syndesmotic injuries[52].
Ultrasound
Ultrasound may be useful for the diagnosis of ankle ligamentous injuries. Diagnostic accuracy of up to 95% for ATFL and 90% for CFL injuries has been reported for ultrasound[53]. Additionally, ultrasound permits the physician to obtain dynamic images to detect functional impairments or joint instability that could not be visualized with other imaging choices[7,53].
Nevertheless, it has two notable limitations: First, acute tears may be pictured in different forms such as hypo-echogenicity or swelling, which may not provide adequate information for correct diagnosis, and second, its accuracy is highly dependent on the operator and/or equipment.
Compared with magnetic resonance imaging (MRI), diagnostic ultrasonography is valuable but less precise and sensitive in the detection of acute lateral ligament injury (level 2)[41].
MRI
Despite the fact that MRI is a reliable method for revealing acute tears of the ATFL and CFL following acute injury (level 2)[41], it is not usually indicated in the routine investigation of acute ankle injuries due to high incidence, limited accessibility, high cost and false-positive findings[1].
However, as the gold standard imaging modality of ankle ligamentous and intra-articular injuries[1], MRI may be extremely beneficial in some particular patients with clinically suspected concomitant injuries, such as osteochondral lesions, syndesmotic injuries, and tendinous pathologies or when persistent symptoms and chronic ankle instability mandate further workup[33].
MRI has good accuracy to detect osteochondral lesions of the talus and determine the level of injury to the ankle syndesmotic ligaments (level 2)[41].
Other imaging techniques
Other techniques such as computed tomography (CT) scan, CT arthrogram, contrast-enhanced MRI, magnetic resonance arthrogram or bone scan are not routinely ordered for diagnosis. However, they may be valuable in the assessment of particular patients[7]. Arthrography within 48 h after an inversion trauma is highly sensitive, but not recommended (level 2)[25].
TREATMENT AND REHABILITATION
Rest, ice, compression, and elevation
Similar to many acute musculoskeletal injuries, the principles of rest, ice, compression, and elevation (RICE) are historically applied for patients with ankle sprain. However, there is limited evidence supporting the efficacy of this approach in reducing associated symptoms following injury[10,33]. Several studies have investigated the components of ice and compression[10].
Limited evidence has indicated that the effectiveness of cryotherapy for reducing symptoms of an ankle sprain is doubtful (level 1)[10,54,55]. Also, there is no evidence that the isolated application of ice can decrease pain and swelling, as well as improve function among persons with acute ankle sprain (level 2)[10,56,57]. However, cryotherapy for 3-7 d is routinely used to reduce pain, minimize swelling and bleeding due to vasoconstriction (especially when applied in the first hours), and decrease secondary injury[54,56,58].
Most statements have recommended a protocol of 20 min each two hours[59]. Intermittent immersion cold therapy in the first week after injury may also be helpful in short-term pain relief[38,56,59].
Due to lack of evidence and the potential for injury exacerbation as the result of vasodilation and inflammatory response, thermotherapy (application of heat) is not recommended during the acute and subacute phases of injury (level 3)[41,57].
Traditionally, compression is regarded as an effective tool to reduce swelling and improve quality of life[60], but current evidence concerning the effectiveness of compression after acute sprain is questionable (level 2)[10,61-64]. It may be explained by the poor quality of existing studies and the variety of treatments used. However, over 75% of hospitals still use tubular compression bandaging despite the lack of convincing evidence on its effectiveness at enhancing recovery[60]. Nevertheless, the application of an elastic bandage in acute ankle sprain was more effective than a splint in reducing edema. Therefore, an elastic bandage could be preferred over a splint for the treatment of acute ankle sprains[65].
There have been no controlled trials on the individual efficacy of rest or elevation in the management of acute ankle sprains[33]. Nevertheless, the injured leg with an acute sprain may be elevated 15-25 cm above the level of the heart to enhance venous and lymphatic drainage and minimize swelling[41,59].
Although there is no sufficient evidence, the use of RICE therapy is a reasonable, routine, and probably safe method in the acute setting for short-term pain relief to expedite early mobilization[33].
Analgesic and anti-inflammatory medications
Nonsteroidal anti-inflammatory drugs: Oral and topical nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to decrease pain and inflammation in the acute phase of ankle sprain[66].
Current studies indicate that the consumption of topical or oral NSAIDs in young and healthy athletes cause short-term improvement of pain and swelling (< 2 wk) without considerably raising the risk of unfavorable events compared with placebo (level 1)[10,41,67-70].
Although NSAIDs are generally considered safe, they should be prescribed prudently due to their potential gastrointestinal, renal, and cardiovascular adverse effects (level 2)[10,71]. Otherwise, they may delay the natural healing process caused by inhibition of the normal inflammatory response[33,71]. Therefore, before prescription, their effect on each individual case has to be weighed.
Regarding the selected NSAIDs for ankle sprains, a few studies have shown superior results for diclofenac at first and second days compared with piroxicam and ibuprofen for pain reduction in mild to severe acute sprains and equal side effects (levels 2 and 3)[10,72,73].
Acetaminophen: Acetaminophen seems to be equally effective as NSAIDs for pain, swelling, and ROM in the first two weeks following acute sprain (level 1)[10,33,74-76].
Opioid analgesics: Compared to NSAIDs, opioid analgesics are similarly effective for pain control, albeit with more adverse effects (level 2)[10,77,78].
Other pharmaceutical agents: Besides the routinely used analgesics, other pharmaceutical agents were investigated in the management of acute ankle sprains, such as hyaluronic acid or platelet-rich plasma (PRP) injections and topical Traumeel. Studies have shown that periarticular hyaluronic acid injections compared with placebo decreased the pain, but they did not result in a faster return to sport or reduced recurrence (level 2)[10,79,80]. Orthobiologics such as PRP injections were not better than placebo injections for pain and functional outcomes (level 3)[10,81]. Also, topical Traumeel was not more effective than diclofenac topical gel for ankle swelling, pain, and function (level 2)[10,82].
Bracing and Immobilization
According to the current evidence, early mobilization and functional ankle support are better than rigid immobilization in the management of acute ankle sprains, especially for grade I and II injuries (level 1)[10,83].
A randomized controlled trial showed that injured athletes who used functional support were able to return to sports activities earlier than those who were managed by casting, and they had fewer symptoms 3 to 6 mo after injury. Although the re-injury rate between the two groups was not significantly different, more ligamentous laxity was radiographically observed among the athletes who were managed with the cast[84]. In a meta-analysis comparing rigid immobilization and functional support, authors reported that a higher percentage of patients who were treated with functional support returned to sports than those managed with rigid immobilization (level 1). Studies have also shown, at intermediate follow-up that the functional support group had benefited from a greater ROM, earlier return to work, and less prevalence of ligamentous laxity and persistent swelling[83,85-88].
However, some evidence showed that a short episode of immobilization (less than 10 d) with a below-knee plaster cast or rigid stirrup brace may be of added value in grade III sprains to decrease pain and swelling and improve functional outcome (level 2)[10,33,89-92].
Functional supports are frequently used in the form of a brace, tape, or elastic bandage. These external supports are different from rigid immobilization and permit loading on damaged tissues in a protected manner[91]. The use of an ankle brace shows the greatest effects compared with other types of functional support such as non-elastic sports tape or elastic kinesiotape, with no side effects (level 2)[10,93]. The superiority of different types of external supports over each other is a matter of controversy[85,94,95].
In comparison between the brace and elastic bandage, a meta-analysis demonstrated that lace-up or semi-rigid braces are superior to the application of the elastic bandage (level 1)[85]. Any type of true ankle support is more efficient than the less adequate supports such as compression bandage (level 2)[91]. Therefore, it seems that compression bandage is not beneficial after the acute phase in the management process (level 3)[64]. The use of an elastic bandage is associated with a delayed return to sport and more perceived instability compared to semi-rigid ankle support[85].
Although outcomes following six months treatment of acute ankle sprain shows no difference between managements with tape, semi-rigid brace, or lace-up brace, in the short-term a lace-up brace or semi-rigid brace appears to be more effective in reducing swelling than a tape or elastic band (level 2)[85,96]. In addition, bracing is more cost-effective[93].
A small systematic review has shown that kinesiotape may not provide adequate mechanical support for unstable ankles (level 1)[97].
However, the success of functional support depends on the severity of the injury. For instance, outcomes may be worse in a sprain complicated by an avulsion fracture, compared to isolated ligament injuries[10,98].
As a conclusion, a lace-up brace or a semi-rigid brace seems suitable and are recommended for all athletes with a prior history of ankle sprain, especially when participating in high-risk activities and sports[99], although some authors believe that lace-up ankle supports are superior to semi-rigid ones[100,101]. In elite athletes, taping can also be a choice[25].
A brace should be used for a minimum of 6 mo following an acute moderate to severe ankle sprain to prevent recurrence[102]. Apart from the preventive effect, the rate of severe ankle sprain is reduced with the use of brace[6,16].
Regarding the protective effect of external supports in athletes returning to the sport after an ankle sprain, a systematic review revealed that athletes who taped or braced had 70% fewer ankle injuries compared to individuals without any prophylactic support[103,104].
Weight bearing and walking aid
Despite the traditional emphasis on non-weight bearing in the early phases of rehabilitation, a systematic review has shown that early weight-bearing with support reduced the symptoms of acute ankle sprain[105]. This early and progressive weight-bearing should include a proper walking-aid device such as a crutch, as needed[106]. Numerous studies have demonstrated that integrating early weight-bearing and movement has a positive influence on the reduction of swelling and restoration of normal ROM. In addition, it accelerates the return to normal activity[105,107,108]. These positive effects have also been reported in individuals with severe grade III sprains, without impeding long-term mechanical stability[109].
Foot orthosis
Foot orthoses may have a significant positive effect in athletes with acute ankle sprain[110]. Some studies have shown that they considerably diminished pain and increased postural control after an acute ankle sprain, possibly due to improved sensory inputs and improved muscular function[110-112]. Both custom made and prefabricated orthoses seem to be effective. Currently, the use of foot orthoses is endorsed by some experts as an important part in the rehabilitation process of ankle sprain[104].
Manual Therapy
The application of manual techniques in the rehabilitation process of acute ankle sprains may be beneficial in pain reduction[113,114] (level 1), ROM (especially dorsiflexion, level 1)[113,115,116], stride length, and functional recovery[113,114]. However, it is uncertain whether manual therapy was useful for the primary outcome of recurrence rate[6].
Common manual techniques include anterior to posterior talocrural glides and talocrural distraction in the neutral position[113]. Soft tissue massage and manual lymphatic drainage techniques can also be performed to reduce stiffness and swelling while improving ROM and proprioceptive awareness[117].
The combination of manual therapy and exercise therapy may provide better results compared with exercise therapy alone (level 3)[114]. Mobilization with movement of the ankle joint includes a combination of posterior talar glide mobilization and active dorsiflexion and can be performed in both positions of weight-bearing or non-weight-bearing[118]. This method may be performed to further increase dorsiflexion and improve function (level 2)[41,118,119].
Accordingly, the inclusion of manual therapy techniques into rehabilitation programs is recommended (level 3)[10,33].
Exercise therapy
Growing evidence supports the use of exercise therapy as the main component of the treatment program[25,115,120-122]. The efficacy of exercise therapy programs has been established, especially when initiated early following an acute ankle sprain[10,120,123].
These programs can reduce the prevalence of recurrent injuries[115,124,125], as well as functional ankle instability[115,126]. Moreover, they may result in an earlier time to recovery and improved self-reported function following acute ankle sprain (level 1)[6,121,124,126].
Both supervised[121,122,127] and home-based[25] exercise are recommended. However, supervised exercise compared with home-based programs may be more helpful in improving ankle strength and proprioception[127], and returning to work[122] and sport earlier[121] (level 1). Nevertheless, some articles disagree with these positive results and believe that the addition of supervised exercise therapy may not be more effective than the conventional program alone (level 2)[115,128-130]. Accordingly, it remains uncertain whether exercise therapy should be supervised or not and additional research is necessary (level 1)[10].
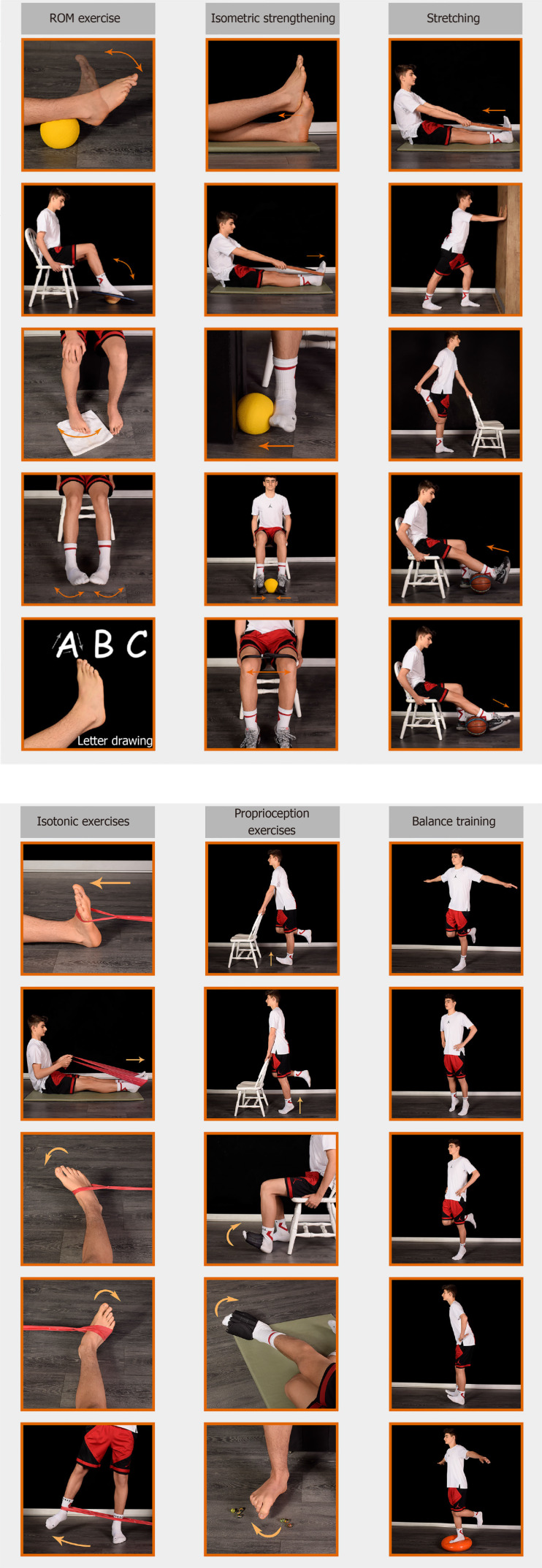
Exercise therapy should be comprehensive and progressive and include ROM, flexibility (stretching), resistance (strengthening), neuromuscular and proprioceptive, and finally sport-specific functional exercises (level 2)[10,41,88,92,120,131-135]. However, no consensus exists regarding the optimal exercise content and training volume in this area[136].
ROM exercises: Early ROM exercises should be started as soon as pain permits[100]. Such a program can frequently be commenced immediately in grade I and II injuries but may need to be postponed in a grade III injury[35]. As soon as the pain permits, individuals should begin weight-bearing and ROM rehabilitation[37,100].
However, it is better to minimize inversion and eversion in the early stages of rehabilitation. After decreasing tenderness over the ligament, inversion and eversion exercises should be added. Athletes are encouraged to do these exercises slowly, without pain, and to use high repetitions[137]. ROM should be resumed first, before functional rehabilitation starts[138].
Stretching exercises: These exercises should be started with open-chain ankle motions for all planes and non-weight bearing dorsiflexion stretch with upper extremity assist and progress to standing calf stretch and generalized ankle stretching in the closed chain[138,139]. Vigorous heel cord stretching should be initiated as soon as possible. It is hypothesized that tight heel cord may act as a bowstring and can increase the possibility of ankle sprains[140].
Strengthening exercises: After restoration of normal ROM, the athlete starts this phase, beginning with isometric exercises against an immobile object in both frontal and sagittal planes. Afterward, the athlete progresses to isotonic resistive exercises using weights, elastic bands or manual resistance by the therapist for dorsiflexion, plantar flexion, inversion, and eversion as tolerated by pain. It is recommended to start with dorsiflexion and plantar flexion isotonic exercises in the early phases, which do not compromise the ligaments. As the ligaments heal further and ROM normalizes, strengthening exercises may be begun in all planes of motion, using pain as the basic guideline[137]. These combine concentric (muscle shortening), and eccentric (muscle lengthening) exercises[37,141]. At first, light resistance with high repetitions are recommended (two to four sets of 10 repetitions)[137]. Strengthening the peroneal muscles is important because reduced eversion strength has been associated with recurrent injury and chronic instability[35]. Bilateral standing toe raised through the full range with use of an angle board or stairs may also be helpful[139]. Proprioceptive neuromuscular facilitation (PNF) strengthening exercises that isolate the desired motions at the talocrural joint may also be useful[137].
As an athlete progresses through the program, it is essential to include exercises that involve proximal muscles of the hip and trunk. It has been shown that low hip strength may increase the chance of lateral ankle sprains[28]. Merging hip and trunk exercises in the rehabilitation process may be useful in reducing the re-injury rate and hence should be considered in athletes with acute ankle sprain[38].
Neuromuscular and proprioceptive exercises: The next phase of rehabilitation involves neuromuscular and proprioceptive training to restore the balance and postural control[133,142].
It was demonstrated that neuromuscular activation patterns are altered after ankle sprain, which may contribute to adverse outcomes such as functional instability, gait abnormalities, and increased recurrence rate[143]. Therefore, these exercises may reduce subjective instability, improve functional outcome measures[126] and decrease the prevalence of recurrence[115,124,126,144].
Early application of neuromuscular training in the first week of injury gives rise to higher activity levels without consequences such as increased pain, swelling, or the rate of re-injury[120]. Therefore, early neuromuscular re-training is safe and effective and is recommended as an important part of the rehabilitation program for athletes suffering ankle sprain[33,38,126]. This type of training should be performed throughout the rehabilitation process (level 1)[41,132-135].
In the early phases, neuromuscular (sensorimotor) exercises may be started with intrinsic foot motion (toe extension with ankle plantar flexion/toe flexion with ankle dorsiflexion) and exercises performed on a foam surface, wedge board, Bosu or DynaDisc in the seated position[133,142,145]. Initially, the athlete should begin with a wedge board in the sagittal direction. As pain decreases, the board may be turned in the coronal direction. When the athlete can perform these movements without difficulty, a seated Biomechanical Ankle Platform System (BAPS) board may be used for full ROM exercises[137,139].
When seated exercises are done easily, standing balance exercises should be started. They may be initiated on one leg standing without a board. The patient then supports their weight with the hands and maintains balance on an unstable surface of a wedge board in either the sagittal or coronal direction with both and then the injured foot. Next, hand support may be eliminated while balancing on the wedge board. The same sequence is then used on the BAPS board[137]. In athletes, the exercise may be made more challenging with the addition of sport-specific perturbation (depending on specific sport; chest pass/overhead pass, volleyball passing, hand fighting for football/wrestling). In the last phases, full-speed planned movement drills (Ladder, Cone) and unilateral jumps to unstable surfaces (foam pad/Bosu) should be performed[139].
Sport-specific exercises: The last phase of the rehabilitation process involves sport-specific training. In a volleyball player, it may consist of plyometric training with jumping maneuvers and for a soccer player, this would include running and cutting drills[146]. Application of a brace or tape may be warranted during the early period of sport-specific training[35].
Although there is no convincing evidence to support better results of sports-specific training compared to neuromuscular training with regard to reducing the chance of re-injury, it seems prudent, based on existing evidence, that sport-specific training be incorporated in the rehabilitation program of athletes with acute ankle sprain[38,106].
This phase of the training program needs expert trainers or therapists with equipment and facilities simulating the real sporting milieu. Evaluation of mastery in sport-specific skills mandates good interaction between the rehabilitation team so that the treating physician can decide regarding return to play[104,147].
Samples of different suitable exercises in the rehabilitation of acute ankle sprain are illustrated in Figure 2.
Figure 2.
Ankle sprain exercises. ROM: Range of motion.
Electrophysical modalities
Traditionally, these modalities have been suggested to improve the healing process following acute ankle sprain; however, there is not enough evidence available to justify their application[34,148]. No effect on pain, edema, function and return to play has been reported for ultrasound[148,149] (level 1), laser therapy[150] (level 1), electrotherapy (level 1)[151-153] and shortwave diathermy (level 2)[154-157] in the management of acute ankle sprain[6].
A small cohort study demonstrated that local vibration therapy may be useful in ankle sprain by improving ROM (dorsiflexion and eversion) and reducing ankle stiffness (level 3)[158]. Another study showed the potential positive effect of Bioptron light therapy in addition to cryotherapy (level 3)[159].
Furthermore, no evidence exists that the addition of supervised physiotherapy to routine care may provide a clinically important change in outcome[160].
Therefore, these modalities are not recommended due to lack of convincing evidence on their effectiveness (level 2)[10].
Surgical therapy
In the past, surgical therapy for acute ankle sprains was common practice. However, it is now evident that the long-term effects of surgical treatment is similar to functional treatment in cases of acute ankle sprain and the majority of cases do not need surgery to resolve the complaints (level 1)[161-163]. Currently, non-operative functional treatment is the preferred method and surgery is only reserved for acute cases of unstable syndesmotic injuries, associated ankle fractures, chronic cases of refractory ankle instability (defined by varus tilt > 10° or > 5° compared to the contralateral side or 10 mm of anterior translation or 5 mm more than the contralateral side)[164], and in cases not responding to an adequate exercise-based rehabilitation[33]. However, treatment decisions should be individualized. In elite athletes, surgery may be chosen to ensure earlier return to play[10,163].
Surgical techniques emphasize anatomic repair/reconstruction to regain stability while trying to minimize complications such as limitation of joint motion and long term development of degenerative arthritis[165].
The modified Broström procedure is commonly used and comprises the direct anatomic repair of torn lateral ligaments together with reinforcement of the inferior extensor retinaculum[166]. This procedure has a success rate of > 90%[164]. Arthroscopic surgery may be preferred in order to treat or rule out a concomitant intra-articular lesion, avoid unnecessary exposure to a more invasive approach, and expedite recovery and return to play in the athletic population (level 1)[10,36,162].
Some studies have reported that surgical intervention may have a higher risk of complications (issues such as wound healing, infection, dystrophy, iatrogenic nerve damage and paresthesia) compared with a conservative intervention[6,161,163,167]. However, the evidence is limited for impaired ankle mobility, higher rate of ankle stiffness, extended recovery times, and other complications in patients who underwent surgical treatment (level 1)[161].
Surgery may be superior at decreasing the recurrence rate of sprain, thereby diminishing the risk for early osteoarthritis (level 2)[168]. However, most individuals (60%–70%) with acute ankle sprain will have a good response to the non-surgical approach[162], and hence surgical treatment would expose individuals to an invasive intervention regardless of the higher cost (level 1)[10].
Other therapies
Some other therapies have been theorized to be effective in the management of ankle sprains. However, such interventions like homeopathic therapy[162,169], hyperbaric oxygen therapy[170], or prolotherapy[171] were not effective or there was not sufficient data to support their use in the treatment of acute ankle sprain. Therefore, they should not be used as a part of the standard rehabilitation of acute ankle sprains[1].
Although a review concluded that acupuncture might have a therapeutic effect to decrease acute symptoms, evidence on the effectiveness of acupuncture is also inconclusive due to large heterogeneity between studies (level 1)[6,172,173].
RETURN TO SPORT
In an injured athlete, timely and safe return to training or competition is the desired outcome of the rehabilitation process. Sports physician should finally decide regarding the athlete’s readiness for return to sport. This decision can be a complex procedure and may need obtaining and interpreting evidence from multiple sources[174]. Obtaining feedback from all members of the rehabilitation team is very important, as many of the key parameters cannot be assessed or monitored in the practice or clinical setting[104]. The responsibility of the physician is to consider all relevant parameters and explain the consequences and risks to the athlete.
In accordance with the consensus statement from the American College of Sports Medicine, the team doctor should make a return to play (RTP) decision, when important criteria such as good sport-specific function of the injured ankle, normal cardiopulmonary and musculoskeletal function, and overall health, restored sports skills and psychosocial readiness were confirmed. In addition, the ability of the athlete to perform safely with a brace, orthosis, and equipment modification is critical. Furthermore, the team physician should ensure that the athlete does not pose an unjustified risk to herself/himself or the safety of other athletes and complies with applicable regulations and legislation[174].
To make an evidence-based RTP decision, the sports physician should consider all of the following parameters.
Self-reported variables
Although assessment of swelling, pain, and ROM by the physician was traditionally considered an important indicator of recovery, current evidence raises the question regarding its reliability[175]. Now, there is a discussion about whether the athlete rather than the physician may be in the best position to evaluate the quality of recovery from an ankle sprain[176]. Outcome studies highly emphasized the athlete’s subjective feeling of function and quality of life in relation to an injury[176-179]. Self-reported outcome tools may help clinicians to evaluate the effects of an injury as well as applied treatment on physical function and should be incorporated in any RTP decision making[41]. The relevance of several tools has been established in supervising recovery from an ankle sprain, including the foot and ankle disability index[180], foot and ankle ability measure[181], lower extremity function score[182], sports ankle rating system[183], lower limb task questionnaire[179], and Cumberland ankle instability tool[184].
These tools usually have a scoring scale and are designed to quantify an athlete’s alteration in health status (especially functional disability) over time[185,186]. However, many tools have some questions about ankle function when participating in sports, which could not be applied for RTP decision while the individual has not yet been eligible to participate[104].
Manual tests of ankle stability
Manual tests of the anterior drawer and talar tilt may be helpful in measuring residual laxity and mechanical instability of the ankle, especially after the remission of acute swelling and pain[7,104]. However, functional instability of the ankle may impede return to play without any mechanical instability. For this reason, the functional tests may be more important in decision-making.
Functional performance testing
In the final parts of rehabilitation, several performance tests should be carried out. Many of these tests have been established to recognize athletes with ankle functional instability, such as shuttle run and different hop tests (single-legged for distance, side, and up-and-down)[187]. These functional tests have not been precisely appraised for suitability in decision making about RTP. Therefore, it is generally recommended that the physician must compare the injured and non-injured ankles and verify that the injured one has attained at least a performance level of 80%[188]. To monitor recovery after an ankle sprain, evaluation of impairments in postural control and balance may be critical[189]. The single-leg balance test (modified Romberg test) is an easy tool to use in the clinic and has acceptable reliability for revealing balance deficits in athletes after an ankle sprain[190]. However, most clinicians believe that assessment of dynamic balance is more reliable for predicting post-sprain recovery[191]. The star excursion balance test (SEBT) is regarded as more specific than static tests in functional assessment[192,193]. This test concurrently evaluates the ROM, strength, neuromuscular control, and proprioception. To perform this test, the athlete stands on one foot and then reaches the other foot in 8 determined directions. In the simplified form of this test, only 3 reach directions of anteromedial, medial, and posteromedial are assessed[194]. The physician can rapidly apply this simplified test to evaluate dynamic balance by comparison of the injured and non-injured ankles.
Quantitative measurements are carried out for all tests, such as distance achieved with hopping or time to complete the task. Some of these tests such as single-legged hop for distance (lateral and forward), single-leg stance for time, SEBT, and heel rockers may be most feasible to administer and are recommended in the clinical setting[104,187,195-197]. Before the athlete restores sport-specific exercises, the functional performance of the injured limb should be equal or more than 80% of the uninjured limb[41,142].
PREVENTION OF RECURRENT SPRAINS
Several measures have been studied as possible interventions for lowering the incidence of recurrent ankle sprains. However, the evidence is limited and mostly concentrated on bracing, taping, and neuromuscular training.
Bracing and taping
Non-rigid bracing and prophylactic taping are effective methods in the prevention of recurrent ankle sprain[10]. In persons with a history of ankle sprain, these may decrease the risk of sprains by 50% to 70%[198]. Compared to taping, bracing is more cost-effective[199], but both seem to be efficient in the prevention of recurrent sprain, and the selection may be dependent on the athlete’s preference. No study has compared the concurrent application of both bracing and tape to either intervention alone[33].
Ankle bracing (especially non-rigid lace-up brace) may be effective for secondary prevention of acute sprain in soccer, basketball, volleyball, and American football. There is no available randomized controlled trial on this topic for other sports[200,201].
According to the existing evidence, lace-up brace or taping may be recommended for one year following ankle sprain to avoid recurrence[33].
Neuromuscular exercises
Neuromuscular exercise programs usually comprise proprioception and balance exercises with repeated involuntary or voluntary destabilization during exercise. These programs improve functional outcome scores, joint proprioception, and muscle reaction time[124]. They decrease the rate of recurrence up to 12 mo following acute sprain and should be considered in every athlete who experiences an ankle sprain as early as tolerated following injury[10,33].
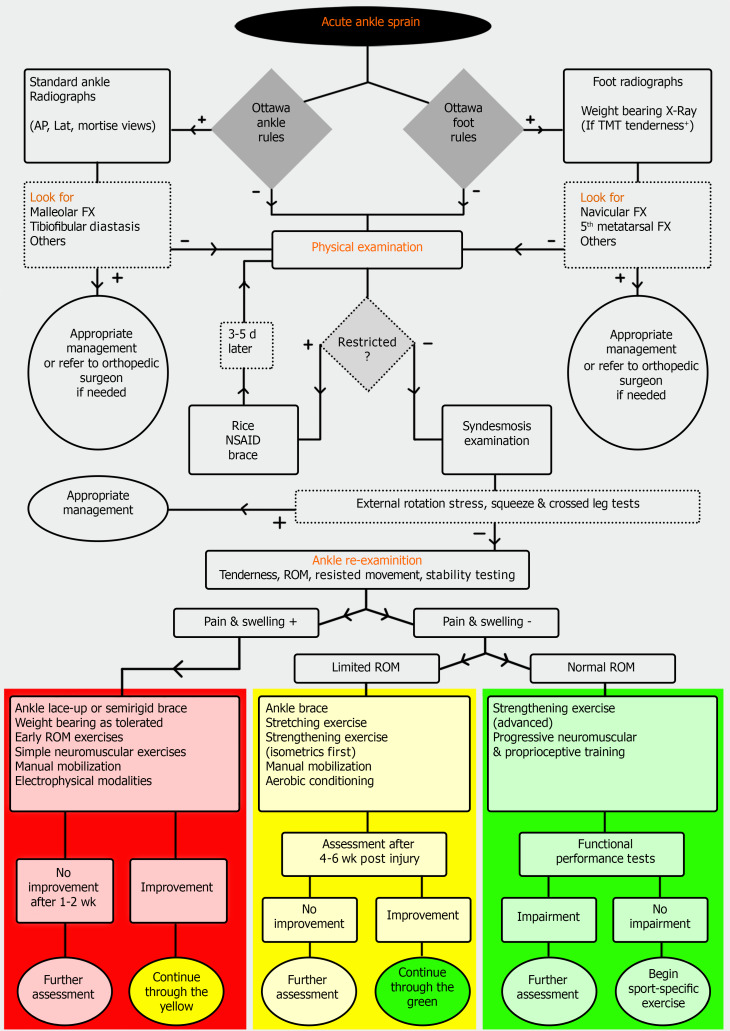
TAKING ALL TOGETHER IN AN ALGORITHMIC APPROACH
Although grading of ankle sprain has been considered an important determinant of the rehabilitation process and return to play, it seems that reliance on grading in elite athletes may be challenging and is of limited benefit (especially in the acute setting)[37] due to the following reasons: (1) As conventional grading systems rely mainly on the signs and symptoms such as hemorrhage, swelling, and tenderness[32,38], the proper and early application of first aid measures may significantly affect the grade identification by the physician. For example, swelling and tenderness may be less than expected with timely and due use of RICE and electrophysical modalities. This is particularly true for elite athletes who are regularly under the close supervision of expert team physicians and therapists; (2) The stability tests such as anterior drawer and talar tilt may be impractical and non-specific due to inflammation and pain in the acute stage (first 5 d)[36,43]. As these tests are so important in the existing grading systems, it seems that proper grading is not reliable, at least in the critical first days; (3) The stability tests should be judged in comparison with the uninjured ankle[1,39]. As many elite athletes (especially in high-risk sports such as basketball, volleyball, and soccer) may frequently have a history of ankle sprain and subsequent instability in the other side, this comparison may be less meaningful in this group; and (4) The healing response of athlete’s tissues may be dependent on important parameters such as genetics, age, co-existing injuries, rehabilitation protocol, nutrition, and pre-injury fitness level and has great inter-individual variation. Therefore, over-emphasis on the grading system to determine the exact time of return to play does not seem prudent and reliable.
According to the above-mentioned reasons, we recommend tailoring primary diagnostic and therapeutic interventions and rehabilitation programs based on the periodic assessments of athlete’s symptoms and signs in an individualized manner. This approach has been summarized in the following algorithm (Figure 3).
Figure 3.
Algorithmic approach to acute lateral ankle sprain. AP: Anteroposterior; RICE: Rest, ice, compression, and elevation; NSAID: Nonsteroidal anti-inflammatory drug; ROM: Range of motion; TMT: Tarsometatarsal.
CONCLUSION
There are some common mistakes in the management of ankle sprains among athletes, which all clinicians should be aware of and avoid. These include unnecessary imaging, undue non-weight-bearing, unwarranted immobilization, delay in functional movements, and insufficient rehabilitation. The use of an evidence-based algorithmic approach with consideration of individual characteristics is highly recommended.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interest.
Manuscript source: Invited manuscript
Peer-review started: February 25, 2020
First decision: September 21, 2020
Article in press: October 23, 2020
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Khodaee M, Lin JA S-Editor: Zhang H L-Editor: Webster JR P-Editor: Xing YX
Contributor Information
Farzin Halabchi, Department of Sports and Exercise Medicine, Tehran University of Medical Sciences, Tehran 14167-53955, Iran.
Mohammad Hassabi, Department of Sports and Exercise Medicine, Shahid Beheshti University of Medical Sciences, Tehran 19979-64151, Iran. hassabi@sbmu.ac.ir.
References
- 1.Polzer H, Kanz KG, Prall WC, Haasters F, Ockert B, Mutschler W, Grote S. Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm. Orthop Rev (Pavia) 2012;4:e5. doi: 10.4081/or.2012.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boruta PM, Bishop JO, Braly WG, Tullos HS. Acute lateral ankle ligament injuries: a literature review. Foot Ankle. 1990;11:107–113. doi: 10.1177/107110079001100210. [DOI] [PubMed] [Google Scholar]
- 3.Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, Hertel J, Hiller CE, Kaminski TW, McKeon PO, Refshauge KM, Verhagen EA, Vicenzino BT, Wikstrom EA, Delahunt E. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1496–1505. doi: 10.1136/bjsports-2016-096189. [DOI] [PubMed] [Google Scholar]
- 4.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 5.Ruth CJ. The surgical treatment of injuries of the fibular collateral ligaments of the ankle. J Bone Joint Surg Am. 1961;43:229–239. [Google Scholar]
- 6.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51:113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 7.Aslan A, Sofu H, Kirdemir V. Ankle ligament injury: current concept. OA Orthop . 2014;2:5–10. [Google Scholar]
- 8.Balduini FC, Vegso JJ, Torg JS, Torg E. Management and rehabilitation of ligamentous injuries to the ankle. Sports Med. 1987;4:364–380. doi: 10.2165/00007256-198704050-00004. [DOI] [PubMed] [Google Scholar]
- 9.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44:123–140. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 10.Vuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R, van Dijk CN, Krips R, Loogman MCM, Ridderikhof ML, Smithuis FF, Stufkens SAS, Verhagen EALM, de Bie RA, Kerkhoffs GMMJ. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52:956. doi: 10.1136/bjsports-2017-098106. [DOI] [PubMed] [Google Scholar]
- 11.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- 14.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? Am J Med. 2008;121:324–331.e6. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Debieux P, Wajnsztejn A, Mansur NSB. Epidemiology of injuries due to ankle sprain diagnosed in an orthopedic emergency room. Einstein (Sao Paulo) 2020;18:eAO4739. doi: 10.31744/einstein_journal/2020AO4739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verhagen EA, van Mechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med. 2000;10:291–296. doi: 10.1097/00042752-200010000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Gribble PA, Bleakley CM, Caulfield BM, Docherty CL, Fourchet F, Fong DT, Hertel J, Hiller CE, Kaminski TW, McKeon PO, Refshauge KM, Verhagen EA, Vicenzino BT, Wikstrom EA, Delahunt E. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1493–1495. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 18.Halabchi F, Mazaheri R, Mansournia MA, Hamedi Z. Additional Effects of an Individualized Risk Factor-Based Approach on Pain and the Function of Patients With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. Clin J Sport Med. 2015;25:478–486. doi: 10.1097/JSM.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 19.Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40:1842–1850. doi: 10.1177/0363546512449602. [DOI] [PubMed] [Google Scholar]
- 20.Beynnon BD, Murphy DF, Alosa DM. Predictive Factors for Lateral Ankle Sprains: A Literature Review. J Athl Train. 2002;37:376–380. [PMC free article] [PubMed] [Google Scholar]
- 21.Pourgharib Shahi MH, Selk Ghaffari M, Mansournia MA, Halabchi F. Risk Factors Influencing the Incidence of Ankle Sprain Among Elite Football and Basketball Players: A Prospective Study. Foot Ankle Spec. 2020:1938640020921251. doi: 10.1177/1938640020921251. [DOI] [PubMed] [Google Scholar]
- 22.Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34:471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi T, Tanaka M, Shida M. Intrinsic Risk Factors of Lateral Ankle Sprain: A Systematic Review and Meta-analysis. Sports Health. 2016;8:190–193. doi: 10.1177/1941738115623775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halabchi F, Angoorani H, Mirshahi M, Pourgharib Shahi MH, Mansournia MA. The Prevalence of Selected Intrinsic Risk Factors for Ankle Sprain Among Elite Football and Basketball Players. Asian J Sports Med. 2016;7:e35287. doi: 10.5812/asjsm.35287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kerkhoffs GM, van den Bekerom M, Elders LA, van Beek PA, Hullegie WA, Bloemers GM, de Heus EM, Loogman MC, Rosenbrand KC, Kuipers T, Hoogstraten JW, Dekker R, Ten Duis HJ, van Dijk CN, van Tulder MW, van der Wees PJ, de Bie RA. Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. Br J Sports Med. 2012;46:854–860. doi: 10.1136/bjsports-2011-090490. [DOI] [PubMed] [Google Scholar]
- 26.Hadzic V, Sattler T, Topole E, Jarnovic Z, Burger H, Dervisevic E. Risk factors for ankle sprain in volleyball players: a preliminary analysis. Isokinet Exerc Sci . 2009;17:155–160. [Google Scholar]
- 27.Baumhauer JF, Alosa DM, Renström AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 28.McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34:464–470. doi: 10.1177/0363546505280427. [DOI] [PubMed] [Google Scholar]
- 29.Strudwick K, McPhee M, Bell A, Martin-Khan M, Russell T. Review article: Best practice management of common ankle and foot injuries in the emergency department (part 2 of the musculoskeletal injuries rapid review series) Emerg Med Australas. 2018;30:152–180. doi: 10.1111/1742-6723.12904. [DOI] [PubMed] [Google Scholar]
- 30.Andersen TE, Floerenes TW, Arnason A, Bahr R. Video analysis of the mechanisms for ankle injuries in football. Am J Sports Med. 2004;32:69S–79S. doi: 10.1177/0363546503262023. [DOI] [PubMed] [Google Scholar]
- 31.Dubin JC, Comeau D, McClelland RI, Dubin RA, Ferrel E. Lateral and syndesmotic ankle sprain injuries: a narrative literature review. J Chiropr Med. 2011;10:204–219. doi: 10.1016/j.jcm.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malliaropoulos N, Papacostas E, Papalada A, Maffulli N. Acute lateral ankle sprains in track and field athletes: an expanded classification. Foot Ankle Clin. 2006;11:497–507. doi: 10.1016/j.fcl.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Chen ET, Borg-Stein J, McInnis KC. Ankle Sprains: Evaluation, Rehabilitation, and Prevention. Curr Sports Med Rep. 2019;18:217–223. doi: 10.1249/JSR.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 34.Al-Mohrej OA, Al-Kenani NS. Acute ankle sprain: conservative or surgical approach? EFORT Open Rev. 2016;1:34–44. doi: 10.1302/2058-5241.1.000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Welck M, Rafferty M, Eltz S, Al-Nammari SS, Eseonu KC. Management of ankle injuries. BMJ. 2015;351:h6698. doi: 10.1136/bmj.h6698. [DOI] [PubMed] [Google Scholar]
- 36.Lau BC, Moore LK, Thuillier DU. Evaluation and Management of Lateral Ankle Pain Following Injury. JBJS Rev. 2018;6:e7. doi: 10.2106/JBJS.RVW.17.00143. [DOI] [PubMed] [Google Scholar]
- 37.Tiemstra JD. Update on acute ankle sprains. Am Fam Physician. 2012;85:1170–1176. [PubMed] [Google Scholar]
- 38.McGovern RP, Martin RL. Managing ankle ligament sprains and tears: current opinion. Open Access J Sports Med. 2016;7:33–42. doi: 10.2147/OAJSM.S72334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Puffer JC. The sprained ankle. Clin Cornerstone. 2001;3:38–49. doi: 10.1016/s1098-3597(01)90068-7. [DOI] [PubMed] [Google Scholar]
- 40.Malliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009;37:1755–1761. doi: 10.1177/0363546509338107. [DOI] [PubMed] [Google Scholar]
- 41.Kaminski TW, Hertel J, Amendola N, Docherty CL, Dolan MG, Hopkins JT, Nussbaum E, Poppy W, Richie D National Athletic Trainers' Association. National Athletic Trainers' Association position statement: conservative management and prevention of ankle sprains in athletes. J Athl Train. 2013;48:528–545. doi: 10.4085/1062-6050-48.4.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aradi AJ, Wong J, Walsh M. The dimple sign of a ruptured lateral ligament of the ankle: brief report. J Bone Joint Surg Br. 1988;70:327–328. doi: 10.1302/0301-620X.70B2.3126191. [DOI] [PubMed] [Google Scholar]
- 43.van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78:958–962. doi: 10.1302/0301-620x78b6.1283. [DOI] [PubMed] [Google Scholar]
- 44.Ivins D. Acute ankle sprain: an update. Am Fam Physician. 2006;74:1714–1720. [PubMed] [Google Scholar]
- 45.Frey C, Bell J, Teresi L, Kerr R, Feder K. A comparison of MRI and clinical examination of acute lateral ankle sprains. Foot Ankle Int. 1996;17:533–537. doi: 10.1177/107110079601700904. [DOI] [PubMed] [Google Scholar]
- 46.Barelds I, Krijnen WP, van de Leur JP, van der Schans CP, Goddard RJ. Diagnostic Accuracy of Clinical Decision Rules to Exclude Fractures in Acute Ankle Injuries: Systematic Review and Meta-analysis. J Emerg Med. 2017;53:353–368. doi: 10.1016/j.jemermed.2017.04.035. [DOI] [PubMed] [Google Scholar]
- 47.Dowling S, Spooner CH, Liang Y, Dryden DM, Friesen C, Klassen TP, Wright RB. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and midfoot in children: a meta-analysis. Acad Emerg Med. 2009;16:277–287. doi: 10.1111/j.1553-2712.2008.00333.x. [DOI] [PubMed] [Google Scholar]
- 48.Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326:417. doi: 10.1136/bmj.326.7386.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stiell IG, McKnight RD, Greenberg GH, McDowell I, Nair RC, Wells GA, Johns C, Worthington JR. Implementation of the Ottawa ankle rules. JAMA. 1994;271:827–832. [PubMed] [Google Scholar]
- 50.Beckenkamp PR, Lin CC, Macaskill P, Michaleff ZA, Maher CG, Moseley AM. Diagnostic accuracy of the Ottawa Ankle and Midfoot Rules: a systematic review with meta-analysis. Br J Sports Med. 2017;51:504–510. doi: 10.1136/bjsports-2016-096858. [DOI] [PubMed] [Google Scholar]
- 51.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9:40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Van Heest TJ, Lafferty PM. Injuries to the ankle syndesmosis. J Bone Joint Surg Am. 2014;96:603–613. doi: 10.2106/JBJS.M.00094. [DOI] [PubMed] [Google Scholar]
- 53.Peetrons P, Creteur V, Bacq C. Sonography of ankle ligaments. J Clin Ultrasound. 2004;32:491–499. doi: 10.1002/jcu.20068. [DOI] [PubMed] [Google Scholar]
- 54.Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32:251–261. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 55.van den Bekerom MP, Struijs PA, Blankevoort L, Welling L, van Dijk CN, Kerkhoffs GM. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults? J Athl Train. 2012;47:435–443. doi: 10.4085/1062-6050-47.4.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bleakley CM, McDonough SM, MacAuley DC, Bjordal J. Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. Br J Sports Med. 2006;40:700–5; discussion 705. doi: 10.1136/bjsm.2006.025932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coté DJ, Prentice WE Jr, Hooker DN, Shields EW. Comparison of three treatment procedures for minimizing ankle sprain swelling. Phys Ther. 1988;68:1072–1076. doi: 10.1093/ptj/68.7.1072. [DOI] [PubMed] [Google Scholar]
- 58.Hubbard TJ, Aronson SL, Denegar CR. Does Cryotherapy Hasten Return to Participation? J Athl Train. 2004;39:88–94. [PMC free article] [PubMed] [Google Scholar]
- 59.Kennet J, Hardaker N, Hobbs S, Selfe J. Cooling efficiency of 4 common cryotherapeutic agents. J Athl Train. 2007;42:343–348. [PMC free article] [PubMed] [Google Scholar]
- 60.Hansrani V, Khanbhai M, Bhandari S, Pillai A, McCollum CN. The role of compression in the management of soft tissue ankle injuries: a systematic review. Eur J Orthop Surg Traumatol. 2015;25:987–995. doi: 10.1007/s00590-015-1607-4. [DOI] [PubMed] [Google Scholar]
- 61.Airaksinen O, Kolari PJ, Miettinen H. Elastic bandages and intermittent pneumatic compression for treatment of acute ankle sprains. Arch Phys Med Rehabil. 1990;71:380–383. [PubMed] [Google Scholar]
- 62.Rucinkski TJ, Hooker DN, Prentice WE, Shields EW, Cote-Murray DJ. The effects of intermittent compression on edema in postacute ankle sprains. J Orthop Sports Phys Ther. 1991;14:65–69. doi: 10.2519/jospt.1991.14.2.65. [DOI] [PubMed] [Google Scholar]
- 63.Tsang KK, Hertel J, Denegar CR. Volume Decreases After Elevation and Intermittent Compression of Postacute Ankle Sprains Are Negated by Gravity-Dependent Positioning. J Athl Train. 2003;38:320–324. [PMC free article] [PubMed] [Google Scholar]
- 64.Bendahou M, Khiami F, Saïdi K, Blanchard C, Scepi M, Riou B, Besch S, Hausfater P. Compression stockings in ankle sprain: a multicenter randomized study. Am J Emerg Med. 2014;32:1005–1010. doi: 10.1016/j.ajem.2014.05.054. [DOI] [PubMed] [Google Scholar]
- 65.Bilgic S, Durusu M, Aliyev B, Akpancar S, Ersen O, Yasar SM, Ardic S. Comparison of two main treatment modalities for acute ankle sprain. Pak J Med Sci. 2015;31:1496–1499. doi: 10.12669/pjms.316.8210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Struijs PA, Kerkhoffs GM. Ankle sprain: the effects of non-steroidal anti-inflammatory drugs. BMJ Clin Evid. 2015;2015:1115. [PMC free article] [PubMed] [Google Scholar]
- 67.van den Bekerom MPJ, Sjer A, Somford MP, Bulstra GH, Struijs PAA, Kerkhoffs GMMJ. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating acute ankle sprains in adults: benefits outweigh adverse events. Knee Surg Sports Traumatol Arthrosc. 2015;23:2390–2399. doi: 10.1007/s00167-014-2851-6. [DOI] [PubMed] [Google Scholar]
- 68.Predel HG, Hamelsky S, Gold M, Giannetti B. Efficacy and safety of diclofenac diethylamine 2.32% gel in acute ankle sprain. Med Sci Sports Exerc. 2012;44:1629–1636. doi: 10.1249/MSS.0b013e318257ed41. [DOI] [PubMed] [Google Scholar]
- 69.Serinken M, Eken C, Elicabuk H. Topical Ketoprofen Versus Placebo in Treatment of Acute Ankle Sprain in the Emergency Department. Foot Ankle Int. 2016;37:989–993. doi: 10.1177/1071100716650530. [DOI] [PubMed] [Google Scholar]
- 70.Predel HG, Giannetti B, Seigfried B, Novellini R, Menke G. A randomized, double-blind, placebo-controlled multicentre study to evaluate the efficacy and safety of diclofenac 4% spray gel in the treatment of acute uncomplicated ankle sprain. J Int Med Res. 2013;41:1187–1202. doi: 10.1177/0300060513487639. [DOI] [PubMed] [Google Scholar]
- 71.Stovitz SD, Johnson RJ. NSAIDs and musculoskeletal treatment: what is the clinical evidence? Phys Sportsmed. 2003;31:35–52. doi: 10.3810/psm.2003.01.160. [DOI] [PubMed] [Google Scholar]
- 72.Bahamonde LA, Saavedra H. Comparison of the analgesic and anti-inflammatory effects of diclofenac potassium versus piroxicam versus placebo in ankle sprain patients. J Int Med Res. 1990;18:104–111. doi: 10.1177/030006059001800205. [DOI] [PubMed] [Google Scholar]
- 73.Morán M. An observer-blind comparison of diclofenac potassium, piroxicam and placebo in the treatment of ankle sprains. Curr Med Res Opin. 1990;12:268–274. doi: 10.1185/03007999009111657. [DOI] [PubMed] [Google Scholar]
- 74.Lyrtzis C, Natsis K, Papadopoulos C, Noussios G, Papathanasiou E. Efficacy of paracetamol versus diclofenac for Grade II ankle sprains. Foot Ankle Int. 2011;32:571–575. doi: 10.3113/FAI.2011.0571. [DOI] [PubMed] [Google Scholar]
- 75.Dalton JD Jr, Schweinle JE. Randomized controlled noninferiority trial to compare extended release acetaminophen and ibuprofen for the treatment of ankle sprains. Ann Emerg Med. 2006;48:615–623. doi: 10.1016/j.annemergmed.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 76.Kayali C, Agus H, Surer L, Turgut A. The efficacy of paracetamol in the treatment of ankle sprains in comparison with diclofenac sodium. Saudi Med J. 2007;28:1836–1839. [PubMed] [Google Scholar]
- 77.Ekman EF, Ruoff G, Kuehl K, Ralph L, Hormbrey P, Fiechtner J, Berger MF. The COX-2 specific inhibitor Valdecoxib versus tramadol in acute ankle sprain: a multicenter randomized, controlled trial. Am J Sports Med. 2006;34:945–955. doi: 10.1177/0363546505283261. [DOI] [PubMed] [Google Scholar]
- 78.Aghababian RV. Comparison of diflunisal and acetaminophen with codeine in the management of grade 2 ankle sprain. Clin Ther. 1986;8:520–526. [PubMed] [Google Scholar]
- 79.Petrella MJ, Cogliano A, Petrella RJ. Original research: long-term efficacy and safety of periarticular hyaluronic acid in acute ankle sprain. Phys Sportsmed. 2009;37:64–70. doi: 10.3810/psm.2009.04.1684. [DOI] [PubMed] [Google Scholar]
- 80.Petrella RJ, Petrella MJ, Cogliano A. Periarticular hyaluronic acid in acute ankle sprain. Clin J Sport Med. 2007;17:251–257. doi: 10.1097/JSM.0b013e3180f6169f. [DOI] [PubMed] [Google Scholar]
- 81.Rowden A, Dominici P, D'Orazio J, Manur R, Deitch K, Simpson S, Kowalski MJ, Salzman M, Ngu D. Double-blind, Randomized, Placebo-controlled Study Evaluating the Use of Platelet-rich Plasma Therapy (PRP) for Acute Ankle Sprains in the Emergency Department. J Emerg Med. 2015;49:546–551. doi: 10.1016/j.jemermed.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 82.González de Vega C, Speed C, Wolfarth B, González J. Traumeel vs. diclofenac for reducing pain and improving ankle mobility after acute ankle sprain: a multicentre, randomised, blinded, controlled and non-inferiority trial. Int J Clin Pract. 2013;67:979–989. doi: 10.1111/ijcp.12219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Naeem M, Rahimnajjad MK, Rahimnajjad NA, Idrees Z, Shah GA, Abbas G. Assessment of functional treatment versus plaster of Paris in the treatment of grade 1 and 2 lateral ankle sprains. J Orthop Traumatol. 2015;16:41–46. doi: 10.1007/s10195-014-0289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ardèvol J, Bolíbar I, Belda V, Argilaga S. Treatment of complete rupture of the lateral ligaments of the ankle: a randomized clinical trial comparing cast immobilization with functional treatment. Knee Surg Sports Traumatol Arthrosc. 2002;10:371–377. doi: 10.1007/s00167-002-0308-9. [DOI] [PubMed] [Google Scholar]
- 85.Kerkhoffs GM, Struijs PA, Marti RK, Assendelft WJ, Blankevoort L, van Dijk CN. WITHDRAWN: Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2013:CD002938. doi: 10.1002/14651858.CD002938.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16:608–615. doi: 10.5435/00124635-200810000-00006. [DOI] [PubMed] [Google Scholar]
- 87.McCriskin BJ, Cameron KL, Orr JD, Waterman BR. Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop. 2015;6:161–171. doi: 10.5312/wjo.v6.i2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly K, Struijs PA, van Dijk CN. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002:CD003762. doi: 10.1002/14651858.CD003762. [DOI] [PubMed] [Google Scholar]
- 89.Uslu M, Inanmaz ME, Ozsahin M, Isık C, Arıcan M, Gecer Y. Cohesive taping and short-leg casting in acute low-type ankle sprains in physically active patients. J Am Podiatr Med Assoc. 2015;105:307–312. doi: 10.7547/13-130.1. [DOI] [PubMed] [Google Scholar]
- 90.Lamb SE, Marsh JL, Hutton JL, Nakash R, Cooke MW Collaborative Ankle Support Trial (CAST Group) Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373:575–581. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 91.Prado MP, Mendes AA, Amodio DT, Camanho GL, Smyth NA, Fernandes TD. A comparative, prospective, and randomized study of two conservative treatment protocols for first-episode lateral ankle ligament injuries. Foot Ankle Int. 2014;35:201–206. doi: 10.1177/1071100713519776. [DOI] [PubMed] [Google Scholar]
- 92.Beynnon BD, Renström PA, Haugh L, Uh BS, Barker H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34:1401–1412. doi: 10.1177/0363546506288676. [DOI] [PubMed] [Google Scholar]
- 93.Kemler E, van de Port I, Backx F, van Dijk CN. A systematic review on the treatment of acute ankle sprain: brace versus other functional treatment types. Sports Med. 2011;41:185–197. doi: 10.2165/11584370-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 94.van den Bekerom MP, van Kimmenade R, Sierevelt IN, Eggink K, Kerkhoffs GM, van Dijk CN, Raven EE. Randomized comparison of tape versus semi-rigid and versus lace-up ankle support in the treatment of acute lateral ankle ligament injury. Knee Surg Sports Traumatol Arthrosc. 2016;24:978–984. doi: 10.1007/s00167-015-3664-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kemler E, van de Port I, Schmikli S, Huisstede B, Hoes A, Backx F. Effects of soft bracing or taping on a lateral ankle sprain: a non-randomised controlled trial evaluating recurrence rates and residual symptoms at one year. J Foot Ankle Res. 2015;8:13. doi: 10.1186/s13047-015-0069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.van den Bekerom MP, Kerkhoffs GM, McCollum GA, Calder JD, van Dijk CN. Management of acute lateral ankle ligament injury in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21:1390–1395. doi: 10.1007/s00167-012-2252-7. [DOI] [PubMed] [Google Scholar]
- 97.Raymond J, Nicholson LL, Hiller CE, Refshauge KM. The effect of ankle taping or bracing on proprioception in functional ankle instability: a systematic review and meta-analysis. J Sci Med Sport. 2012;15:386–392. doi: 10.1016/j.jsams.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 98.Noh JH, Yang BG, Yi SR, Lee SH, Song CH. Outcome of the functional treatment of first-time ankle inversion injury. J Orthop Sci. 2010;15:524–530. doi: 10.1007/s00776-010-1481-1. [DOI] [PubMed] [Google Scholar]
- 99.Evans LJ, Clough A. Prevention of ankle sprain: a systematic review. Int Musculoskelet Med. 2012;34:146–158. [Google Scholar]
- 100.Kerkhoffs GM, Struijs PA, Marti RK, Blankevoort L, Assendelft WJ, van Dijk CN. Functional treatments for acute ruptures of the lateral ankle ligament: a systematic review. Acta Orthop Scand. 2003;74:69–77. doi: 10.1080/00016470310013699. [DOI] [PubMed] [Google Scholar]
- 101.Seah R, Mani-Babu S. Managing ankle sprains in primary care: what is best practice? Br Med Bull. 2011;97:105–135. doi: 10.1093/bmb/ldq028. [DOI] [PubMed] [Google Scholar]
- 102.Gilchrist J, Branche CM, Goodman RA, Stroup DF, Thacker SB. Prevention of ankle sprains in sports: an update. Int SportMed J. 2003;4:1–17. doi: 10.1177/03635465990270061201. [DOI] [PubMed] [Google Scholar]
- 103.Dizon JM, Reyes JJ. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport. 2010;13:309–317. doi: 10.1016/j.jsams.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 104.Richie DH, Izadi FE. Return to play after an ankle sprain: guidelines for the podiatric physician. Clin Podiatr Med Surg. 2015;32:195–215. doi: 10.1016/j.cpm.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 105.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly KD, Struijs PA, van Dijk CN. Immobilisation for acute ankle sprain. A systematic review. Arch Orthop Trauma Surg. 2001;121:462–471. doi: 10.1007/s004020100283. [DOI] [PubMed] [Google Scholar]
- 106.Martin RL, Davenport TE, Paulseth S, Wukich DK, Godges JJ Orthopaedic Section American Physical Therapy Association. Ankle stability and movement coordination impairments: ankle ligament sprains. J Orthop Sports Phys Ther. 2013;43:A1–40. doi: 10.2519/jospt.2013.0305. [DOI] [PubMed] [Google Scholar]
- 107.Eiff MP, Smith AT, Smith GE. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83–88. doi: 10.1177/036354659402200115. [DOI] [PubMed] [Google Scholar]
- 108.Dettori JR, Basmania CJ. Early ankle mobilization, Part II: A one-year follow-up of acute, lateral ankle sprains (a randomized clinical trial) Mil Med. 1994;159:20–24. [PubMed] [Google Scholar]
- 109.Lynch SA, Renström PA. Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999;27:61–71. doi: 10.2165/00007256-199927010-00005. [DOI] [PubMed] [Google Scholar]
- 110.Richie DH Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007;97:19–30. doi: 10.7547/0970019. [DOI] [PubMed] [Google Scholar]
- 111.Guskiewicz KM, Perrin DH. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23:326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- 112.Orteza LC, Vogelbach WD, Denegar CR. The effect of molded and unmolded orthotics on balance and pain while jogging following inversion ankle sprain. J Athl Train. 1992;27:80–84. [PMC free article] [PubMed] [Google Scholar]
- 113.Loudon JK, Reiman MP, Sylvain J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med. 2014;48:365–370. doi: 10.1136/bjsports-2013-092763. [DOI] [PubMed] [Google Scholar]
- 114.Cleland JA, Mintken PE, McDevitt A, Bieniek ML, Carpenter KJ, Kulp K, Whitman JM. Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2013;43:443–455. doi: 10.2519/jospt.2013.4792. [DOI] [PubMed] [Google Scholar]
- 115.van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in ankle sprain and functional instability: a systematic review. Aust J Physiother. 2006;52:27–37. doi: 10.1016/s0004-9514(06)70059-9. [DOI] [PubMed] [Google Scholar]
- 116.Cosby NL, Koroch M, Grindstaff TL, Parente W, Hertel J. Immediate effects of anterior to posterior talocrural joint mobilizations following acute lateral ankle sprain. J Man Manip Ther. 2011;19:76–83. doi: 10.1179/2042618610Y.0000000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eisenhart AW, Gaeta TJ, Yens DP. Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. J Am Osteopath Assoc . 2003;103:417–421. [PubMed] [Google Scholar]
- 118.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36:464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 119.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32:166–173. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- 120.Bleakley CM, O'Connor SR, Tully MA, Rocke LG, Macauley DC, Bradbury I, Keegan S, McDonough SM. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010;340:c1964. doi: 10.1136/bmj.c1964. [DOI] [PubMed] [Google Scholar]
- 121.van Rijn RM, van Ochten J, Luijsterburg PA, van Middelkoop M, Koes BW, Bierma-Zeinstra SM. Effectiveness of additional supervised exercises compared with conventional treatment alone in patients with acute lateral ankle sprains: systematic review. BMJ. 2010;341:c5688. doi: 10.1136/bmj.c5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.van Os AG, Bierma-Zeinstra SM, Verhagen AP, de Bie RA, Luijsterburg PA, Koes BW. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther. 2005;35:95–105. doi: 10.2519/jospt.2005.35.2.95. [DOI] [PubMed] [Google Scholar]
- 123.van Rijn RM, van Heest JA, van der Wees P, Koes BW, Bierma-Zeinstra SM. Some benefit from physiotherapy intervention in the subgroup of patients with severe ankle sprain as determined by the ankle function score: a randomised trial. Aust J Physiother. 2009;55:107–113. doi: 10.1016/s0004-9514(09)70040-6. [DOI] [PubMed] [Google Scholar]
- 124.Zech A, Hübscher M, Vogt L, Banzer W, Hänsel F, Pfeifer K. Neuromuscular training for rehabilitation of sports injuries: a systematic review. Med Sci Sports Exerc. 2009;41:1831–1841. doi: 10.1249/MSS.0b013e3181a3cf0d. [DOI] [PubMed] [Google Scholar]
- 125.Bleakley CM, McDonough SM, MacAuley DC. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Aust J Physiother. 2008;54:7–20. doi: 10.1016/s0004-9514(08)70061-8. [DOI] [PubMed] [Google Scholar]
- 126.Postle K, Pak D, Smith TO. Effectiveness of proprioceptive exercises for ankle ligament injury in adults: a systematic literature and meta-analysis. Man Ther. 2012;17:285–291. doi: 10.1016/j.math.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 127.Feger MA, Herb CC, Fraser JJ, Glaviano N, Hertel J. Supervised rehabilitation versus home exercise in the treatment of acute ankle sprains: a systematic review. Clin Sports Med. 2015;34:329–346. doi: 10.1016/j.csm.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 128.van Rijn RM, van Os AG, Kleinrensink GJ, Bernsen RM, Verhaar JA, Koes BW, Bierma-Zeinstra SM. Supervised exercises for adults with acute lateral ankle sprain: a randomised controlled trial. Br J Gen Pract. 2007;57:793–800. [PMC free article] [PubMed] [Google Scholar]
- 129.Hing W, Lopes J, Hume PA, Reid DA. Comparison of multimodal physiotherapy and" RICE" self-treatment for early management of ankle sprains. NZ J Physiother. 2011;39:13–19. [Google Scholar]
- 130.Punt IM, Ziltener JL, Monnin D, Allet L. Wii Fit™ exercise therapy for the rehabilitation of ankle sprains: Its effect compared with physical therapy or no functional exercises at all. Scand J Med Sci Sports. 2016;26:816–823. doi: 10.1111/sms.12509. [DOI] [PubMed] [Google Scholar]
- 131.Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33:310–314. [PMC free article] [PubMed] [Google Scholar]
- 132.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train. 2008;43:305–315. doi: 10.4085/1062-6050-43.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 134.Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 135.Bellows R, Wong CK. THE EFFECT OF BRACING AND BALANCE TRAINING ON ANKLE SPRAIN INCIDENCE AMONG ATHLETES: A SYSTEMATIC REVIEW WITH META-ANALYSIS. Int J Sports Phys Ther. 2018;13:379–388. [PMC free article] [PubMed] [Google Scholar]
- 136.Bleakley CM, Taylor JB, Dischiavi SL, Doherty C, Delahunt E. Rehabilitation Exercises Reduce Reinjury Post Ankle Sprain, But the Content and Parameters of an Optimal Exercise Program Have Yet to Be Established: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2019;100:1367–1375. doi: 10.1016/j.apmr.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 137.Prentice WE. Rehabilitation Techniques for Sports Medicine and Athletic Training. SLACK Incorporated, 2015. [Google Scholar]
- 138.Osborne MD, Rizzo TD Jr. Prevention and treatment of ankle sprain in athletes. Sports Med. 2003;33:1145–1150. doi: 10.2165/00007256-200333150-00005. [DOI] [PubMed] [Google Scholar]
- 139.Reider B, Davies G, Provencher MT. Orthopaedic rehabilitation of the athlete: Getting back in the game. Elsevier Health Sciences, 2014. [Google Scholar]
- 140.McCluskey GM, Blackburn TA Jr, Lewis T. Prevention of ankle sprains. Am J Sports Med. 1976;4:151–157. doi: 10.1177/036354657600400405. [DOI] [PubMed] [Google Scholar]
- 141.Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician. 2001;63:93–104. [PubMed] [Google Scholar]
- 142.Hupperets MD, Verhagen EA, van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised controlled trial. BMJ. 2009;339:b2684. doi: 10.1136/bmj.b2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Punt IM, Ziltener JL, Laidet M, Armand S, Allet L. Gait and physical impairments in patients with acute ankle sprains who did not receive physical therapy. PM R. 2015;7:34–41. doi: 10.1016/j.pmrj.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 144.Calatayud J, Borreani S, Colado JC, Flandez J, Page P, Andersen LL. Exercise and ankle sprain injuries: a comprehensive review. Phys Sportsmed. 2014;42:88–93. doi: 10.3810/psm.2014.02.2051. [DOI] [PubMed] [Google Scholar]
- 145.Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- 146.Mattacola CG, Dwyer MK. Rehabilitation of the Ankle After Acute Sprain or Chronic Instability. J Athl Train. 2002;37:413–429. [PMC free article] [PubMed] [Google Scholar]
- 147.. The team physician and return-to-play issues: a consensus statement. Med Sci Sports Exerc. 2002;34:1212–1214. doi: 10.1097/00005768-200207000-00025. [DOI] [PubMed] [Google Scholar]
- 148.Van Der Windt DA, Van Der Heijden GJ, Van Den Berg SG, Ter Riet G, De Winter AF, Bouter LM. Ultrasound therapy for acute ankle sprains. Cochrane Database Syst Rev. 2002:CD001250. doi: 10.1002/14651858.CD001250. [DOI] [PubMed] [Google Scholar]
- 149.van den Bekerom MP, van der Windt DA, Ter Riet G, van der Heijden GJ, Bouter LM. Therapeutic ultrasound for acute ankle sprains. Cochrane Database Syst Rev. 2011:CD001250. doi: 10.1002/14651858.CD001250.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.de Bie RA, de Vet HC, Lenssen TF, van den Wildenberg FA, Kootstra G, Knipschild PG. Low-level laser therapy in ankle sprains: a randomized clinical trial. Arch Phys Med Rehabil. 1998;79:1415–1420. doi: 10.1016/s0003-9993(98)90237-4. [DOI] [PubMed] [Google Scholar]
- 151.Mendel FC, Dolan MG, Fish DR, Marzo J, Wilding GE. Effect of high-voltage pulsed current on recovery after grades I and II lateral ankle sprains. J Sport Rehabil. 2010;19:399–410. doi: 10.1123/jsr.19.4.399. [DOI] [PubMed] [Google Scholar]
- 152.Feger MA, Goetschius J, Love H, Saliba SA, Hertel J. Electrical stimulation as a treatment intervention to improve function, edema or pain following acute lateral ankle sprains: A systematic review. Phys Ther Sport. 2015;16:361–369. doi: 10.1016/j.ptsp.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 153.Sandoval MC, Ramirez C, Camargo DM, Salvini TF. Effect of high-voltage pulsed current plus conventional treatment on acute ankle sprain. Rev Bras Fisioter. 2010;14:193–199. doi: 10.1590/s1413-35552010000300012. [DOI] [PubMed] [Google Scholar]
- 154.Pasila M, Visuri T, Sundholm A. Pulsating shortwave diathermy: value in treatment of recent ankle and foot sprains. Arch Phys Med Rehabil. 1978;59:383–386. [PubMed] [Google Scholar]
- 155.Pennington GM, Danley DL, Sumko MH, Bucknell A, Nelson JH. Pulsed, non-thermal, high-frequency electromagnetic energy (DIAPULSE) in the treatment of grade I and grade II ankle sprains. Mil Med. 1993;158:101–104. [PubMed] [Google Scholar]
- 156.Barker A, Barlow P, Porter J. A double-blind clinical trial of low power pulsed shortwave therapy in the treatment of a soft tissue injury. J Physiother. 1985;71:500–504. [Google Scholar]
- 157.Michlovitz SL, Smith W, Watkins M. Ice and high voltage pulsed stimulation in treatment of acute lateral ankle sprains*. J Orthop Sports Phys Ther. 1988;9:301–304. doi: 10.2519/jospt.1988.9.9.301. [DOI] [PubMed] [Google Scholar]
- 158.Peer KS, Barkley JE, Knapp DM. The acute effects of local vibration therapy on ankle sprain and hamstring strain injuries. Phys Sportsmed. 2009;37:31–38. doi: 10.3810/psm.2009.12.1739. [DOI] [PubMed] [Google Scholar]
- 159.Stasinopoulos D, Papadopoulos C, Lamnisos D, Stasinopoulos I. The use of Bioptron light (polarized, polychromatic, non-coherent) therapy for the treatment of acute ankle sprains. Disabil Rehabil. 2017;39:450–457. doi: 10.3109/09638288.2016.1146357. [DOI] [PubMed] [Google Scholar]
- 160.Brison RJ, Day AG, Pelland L, Pickett W, Johnson AP, Aiken A, Pichora DR, Brouwer B. Effect of early supervised physiotherapy on recovery from acute ankle sprain: randomised controlled trial. BMJ. 2016;355:i5650. doi: 10.1136/bmj.i5650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kerkhoffs GM, Handoll HH, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007:CD000380. doi: 10.1002/14651858.CD000380.pub2. [DOI] [PubMed] [Google Scholar]
- 162.Struijs PA, Kerkhoffs GM. Ankle sprain. BMJ Clin Evid. 2010;2010 [PMC free article] [PubMed] [Google Scholar]
- 163.Petersen W, Rembitzki IV, Koppenburg AG, Ellermann A, Liebau C, Brüggemann GP, Best R. Treatment of acute ankle ligament injuries: a systematic review. Arch Orthop Trauma Surg. 2013;133:1129–1141. doi: 10.1007/s00402-013-1742-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Shakked RJ, Karnovsky S, Drakos MC. Operative treatment of lateral ligament instability. Curr Rev Musculoskelet Med. 2017;10:113–121. doi: 10.1007/s12178-017-9391-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Guillo S, Bauer T, Lee JW, Takao M, Kong SW, Stone JW, Mangone PG, Molloy A, Perera A, Pearce CJ, Michels F, Tourné Y, Ghorbani A, Calder J. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411–S419. doi: 10.1016/j.otsr.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 166.Tourné Y, Mabit C. Lateral ligament reconstruction procedures for the ankle. Orthop Traumatol Surg Res. 2017;103:S171–S181. doi: 10.1016/j.otsr.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 167.Pijnenburg AC, Van Dijk CN, Bossuyt PM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: a meta-analysis. J Bone Joint Surg Am. 2000;82:761–773. doi: 10.2106/00004623-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 168.Pihlajamäki H, Hietaniemi K, Paavola M, Visuri T, Mattila VM. Surgical versus functional treatment for acute ruptures of the lateral ligament complex of the ankle in young men: a randomized controlled trial. J Bone Joint Surg Am. 2010;92:2367–2374. doi: 10.2106/JBJS.I.01176. [DOI] [PubMed] [Google Scholar]
- 169.Cucherat M, Haugh MC, Gooch M, Boissel JP. Evidence of clinical efficacy of homeopathy. A meta-analysis of clinical trials. HMRAG. Homeopathic Medicines Research Advisory Group. Eur J Clin Pharmacol. 2000;56:27–33. doi: 10.1007/s002280050716. [DOI] [PubMed] [Google Scholar]
- 170.Bennett M, Best TM, Babul S, Taunton J, Lepawsky M. Hyperbaric oxygen therapy for delayed onset muscle soreness and closed soft tissue injury. Cochrane Database Syst Rev. 2005:CD004713. doi: 10.1002/14651858.CD004713.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010;37:65–80. doi: 10.1016/j.pop.2009.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kim TH, Lee MS, Kim KH, Kang JW, Choi TY, Ernst E. Acupuncture for treating acute ankle sprains in adults. Cochrane Database Syst Rev. 2014:CD009065. doi: 10.1002/14651858.CD009065.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Park J, Hahn S, Park JY, Park HJ, Lee H. Acupuncture for ankle sprain: systematic review and meta-analysis. BMC Complement Altern Med . 2013;13:55. doi: 10.1186/1472-6882-13-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Herring SA, Kibler WB, Putukian M. The team physician and the return-to-play decision: a consensus statement-2012 update. Med Sci Sports Exerc. 2012;44:2446–2448. doi: 10.1249/MSS.0b013e3182750534. [DOI] [PubMed] [Google Scholar]
- 175.Cross KM, Worrell TW, Leslie JE, Van Veld KR. The relationship between self-reported and clinical measures and the number of days to return to sport following acute lateral ankle sprains. J Orthop Sports Phys Ther. 2002;32:16–23. doi: 10.2519/jospt.2002.32.1.16. [DOI] [PubMed] [Google Scholar]
- 176.Larmer PJ, McNair PJ, Smythe L, Williams M. Ankle sprains: patient perceptions of function and performance of physical tasks. A mixed methods approach. Disabil Rehabil. 2011;33:2299–2304. doi: 10.3109/09638288.2011.568668. [DOI] [PubMed] [Google Scholar]
- 177.Landorf KB, Keenan AM. An evaluation of two foot-specific, health-related quality-of-life measuring instruments. Foot Ankle Int. 2002;23:538–546. doi: 10.1177/107110070202300611. [DOI] [PubMed] [Google Scholar]
- 178.Cronkey J, LaPorta G. Rating systems for evaluation of functional ankle instability: prospective evaluation in a cohort of patients treated with monopolar capacitive-coupled radiofrequency. Foot Ankle Spec. 2012;5:293–299. doi: 10.1177/1938640012457941. [DOI] [PubMed] [Google Scholar]
- 179.McNair PJ, Prapavessis H, Collier J, Bassett S, Bryant A, Larmer P. The lower-limb tasks questionnaire: an assessment of validity, reliability, responsiveness, and minimal important differences. Arch Phys Med Rehabil. 2007;88:993–1001. doi: 10.1016/j.apmr.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 180.Hale SA, Hertel J. Reliability and Sensitivity of the Foot and Ankle Disability Index in Subjects With Chronic Ankle Instability. J Athl Train. 2005;40:35–40. [PMC free article] [PubMed] [Google Scholar]
- 181.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26:968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 182.Alcock G. Validation of the Lower Extremity Functional Scale on athletic subjects with ankle sprains. Physiother Can . 2002;54:233–240. [Google Scholar]
- 183.Williams GN, Molloy JM, DeBerardino TM, Arciero RA, Taylor DC. Evaluation of the Sports Ankle Rating System in young, athletic individuals with acute lateral ankle sprains. Foot Ankle Int. 2003;24:274–282. doi: 10.1177/107110070302400314. [DOI] [PubMed] [Google Scholar]
- 184.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87:1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 185.Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis. 1985;38:27–36. doi: 10.1016/0021-9681(85)90005-0. [DOI] [PubMed] [Google Scholar]
- 186.Munn J, Beard DJ, Refshauge KM, Lee RW. Do functional-performance tests detect impairment in subjects with ankle instability? J Sport Rehabil. 2002;11:40–50. [Google Scholar]
- 187.Buchanan AS, Docherty CL, Schrader J. Functional performance testing in participants with functional ankle instability and in a healthy control group. J Athl Train. 2008;43:342–346. doi: 10.4085/1062-6050-43.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19:653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 189.Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 190.Kaikkonen A, Kannus P, Järvinen M. A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med. 1994;22:462–469. doi: 10.1177/036354659402200405. [DOI] [PubMed] [Google Scholar]
- 191.Guskiewicz KM, Perrin DH. Research and clinical applications of assessing balance. J Sport Rehabil. 1996;5:45–63. [Google Scholar]
- 192.Kinzey SJ, Armstrong CW. The reliability of the star-excursion test in assessing dynamic balance. J Orthop Sports Phys Ther. 1998;27:356–360. doi: 10.2519/jospt.1998.27.5.356. [DOI] [PubMed] [Google Scholar]
- 193.Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the Star Excursion Balance Tests. J Sport Rehabil . 2000;9:104–116. [Google Scholar]
- 194.Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 195.Caffrey E, Docherty CL, Schrader J, Klossner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39:799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- 196.Docherty CL, Arnold BL, Gansneder BM, Hurwitz S, Gieck J. Functional-Performance Deficits in Volunteers With Functional Ankle Instability. J Athl Train. 2005;40:30–34. [PMC free article] [PubMed] [Google Scholar]
- 197.Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4:92–99. [PMC free article] [PubMed] [Google Scholar]
- 198.McKeon PO, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med. 2008;27:371–382, viii. doi: 10.1016/j.csm.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 199.Janssen KW, Hendriks MR, van Mechelen W, Verhagen E. The Cost-Effectiveness of Measures to Prevent Recurrent Ankle Sprains: Results of a 3-Arm Randomized Controlled Trial. Am J Sports Med. 2014;42:1534–1541. doi: 10.1177/0363546514529642. [DOI] [PubMed] [Google Scholar]
- 200.McGuine TA, Hetzel S, Wilson J, Brooks A. The effect of lace-up ankle braces on injury rates in high school football players. Am J Sports Med. 2012;40:49–57. doi: 10.1177/0363546511422332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Barelds I, van den Broek AG, Huisstede BMA. Ankle Bracing is Effective for Primary and Secondary Prevention of Acute Ankle Injuries in Athletes: A Systematic Review and Meta-Analyses. Sports Med. 2018;48:2775–2784. doi: 10.1007/s40279-018-0993-2. [DOI] [PubMed] [Google Scholar]