Abstract
Background:
Patients who sustain a rotator cuff retear after arthroscopic rotator cuff repair are generally considered to have worse clinical outcomes compared with patients with an intact rotator cuff. However, some patients have good clinical outcomes, even with a retorn rotator cuff.
Purpose:
To report the clinical outcomes of nonoperative treatment for rotator cuff retears and analyze the factors affecting clinical outcomes after a retear.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients who underwent arthroscopic rotator cuff repair between 2011 and 2017 were reviewed, and those with a full-thickness retear on postoperative magnetic resonance imaging (MRI) were included in this study. According to their pre- and postoperative scores on the pain visual analog scale (pVAS) and functional visual analog scale (fVAS), the patients were divided into 3 groups: (1) mild group (pVAS ≤ 1 and fVAS ≥ 8), (2) moderate group (pVAS ≤ 1 and fVAS ≤ 7 or pVAS 2-3 and fVAS ≥ 8), and (3) severe group (pVAS ≥ 3 and fVAS ≤ 7). Preoperative data (dominant hand involvement, heavy labor) and tear size on 6-month postoperative MRI were analyzed as factors affecting clinical outcomes.
Results:
A total of 712 patients were reviewed, and a retear was observed in 62 patients (8.7%). Of the patients with retears, 52 were included in this study: 25 men and 27 women with a mean age of 62.6 years (range, 49-80 years) and mean follow-up period of 40 months (range, 24-88 months). According to the pVAS and fVAS scores, 25 patients (48.1%) were classified into the mild group, 9 (17.3%) into the moderate group, and 18 (34.6%) into the severe group. There were no significant differences in preoperative data among the 3 groups. The tear size in the coronal and sagittal planes decreased by 5.1 and 6.6 mm, respectively, in the mild group but increased by 2.8 and 1.4 mm, respectively, in the severe group.
Conclusion:
In patients with retears, 48.1% had only mild symptoms at a mean of 40 months postoperatively. Patients with severe symptoms tended to have an increased tear size on postoperative MRI.
Keywords: shoulder, magnetic resonance imaging, arthroscopic surgery, rotator cuff repair, retear
Arthroscopic repair is the gold standard for symptomatic rotator cuff tears, with good outcomes reported.19 A retear after rotator cuff repair is a common complication and has been reported to occur in 7% to 17% of cases.4,13,14 Patients with full-thickness rotator cuff retears have poorer clinical outcomes than those with an intact rotator cuff after repair. In a meta-analysis, Yang et al24 found that rotator cuff retears correlated with lower clinical outcome scores and rotator cuff strength than an intact rotator cuff after repair. Yoo et al26 reported that both the healed and retear groups showed improved clinical outcomes, but the healed group showed better results.
Natural history studies have raised concerns about tear progression and irreversible fatty infiltration worsening over time.18,27 Revision rotator cuff repair can be considered in patients with a retear.23 However, symptoms related to rotator cuff retears are not easy to predict, and making the decision for a reoperation is difficult.6 Nonoperative treatment has been shown to be effective for some primary rotator cuff tears,5,17,27 and it has also been prescribed in cases of retears after rotator cuff repair. In our practice, we have encountered conflicting outcomes after nonoperative treatment in patients with retears: Some have improved symptoms and function, while some have persistent pain and loss of function. To the best of our knowledge, no study has compared patients with good clinical outcomes to those with poor outcomes after nonoperative treatment for rotator cuff retears.
The aims of this study were to (1) report the clinical outcomes of nonoperative treatment for rotator cuff retears and (2) analyze the factors affecting the clinical outcomes of patients with retears. Our hypotheses were that (1) many patients would have good clinical outcomes even with a retear and (2) that patients with severe symptoms would have an increased tear size on postoperative magnetic resonance imaging (MRI).
Methods
Patient Selection and Classification
This was a retrospective, nonrandomized comparative study. Our institutional review board approved the study protocol and waived the requirement for informed patient consent. We enrolled a consecutive series of patients who underwent arthroscopic rotator cuff repair at our center from 2011 to 2017 (N = 1306 patients). The inclusion criteria were as follows: (1) complete repair, with the tendon mobilized to the distal lateral end (type I) or within half of the distance to the proximal medial end (type II) of the greater tuberosity, according to the classification by Yoo et al25; (2) rotator cuff repair with a double-row technique (transosseous-equivalent repair)16; and (3) Sugaya classification21 type IV (presence of minor discontinuity) or V (presence of major discontinuity) on 6-month postoperative MRI. The exclusion criteria were as follows: (1) revision rotator cuff repair, (2) no postsurgical MRI, (3) osteoarthritis in the glenohumeral joint, and (4) <2 years of follow-up.
The patients enrolled in the study were divided into 3 groups according to the pain and functional scores at the last follow-up: (1) mild group, (2) moderate group, and (3) severe group. The criteria for dividing the groups were arbitrary. “Mild” was defined as the absence of retear symptoms. Patients with a pain visual analog scale (pVAS) score ≤1 and a functional visual analog scale (fVAS) score ≥8 were classified into the mild group. Conversely, “severe” was defined as the presence of severe discomfort related to a retear. Patients with a pVAS score ≥3 and an fVAS score ≤7 were classified into the severe group. Patients who underwent revisional surgery for a retear were also classified into the severe group regardless of the pVAS and fVAS scores. “Moderate” was defined as not mild and not severe. Patients with a pVAS score ≤1 and an fVAS score ≤7 or with a pVAS score 2-3 and an fVAS score ≥8 were classified into the moderate group.
In patients with retears, the defect size on coronary MRI was measured and the SD was 8.9 mm. We calculated that a sample size of 14 patients per group would be sufficient to detect a 10-mm difference in the retear size with 80% power.
Surgical Procedure and Rehabilitation
All surgical procedures were performed by a single surgeon (J.C.Y.). Rotator cuff repair was performed using the double-row transosseous-equivalent technique. After surgery, patients underwent standard rehabilitation.8 Muscle strengthening exercises were started at 12 weeks postoperatively. Exercise training consisted of shoulder extension, internal rotation, external rotation, and scaption exercises using a resistance band. All patients were instructed to perform each exercise daily for a total of 3 sets of 15 repetitions and received re-education for the exercise program at 6 months postoperatively.
Clinical Evaluation
Preoperative demographic data and operative findings were collected. Clinical evaluations were performed the day prior to surgery as well as postsurgically at 6 months, 1 year, 2 years, and final follow-up. Shoulder range of motion (ROM) measurements as well as pVAS, fVAS, American Shoulder and Elbow Surgeons (ASES), Constant, and Simple Shoulder Test (SST) scores were collected. The clinical scores were collected by a single physical therapist who was blinded to the nature of this study. ROM was measured at forward flexion, external rotation at the side, and internal rotation at the vertebral level during regular follow-up examinations by the surgeon. For statistical analysis, we converted the vertebral level to a number: T4-T7 was converted to 10, T8-T12 to 8, L1-L3 to 6, L4-L5 to 4, and sacrum and buttock to 2.
Radiological Evaluation
The patients underwent MRI examinations before surgery and at 6 months after surgery. MRI was performed with a 3.0-T magnetic resonance scanner (Gyroscan Intera Achieva; Philips). The MRI protocol used in this study included T2-weighted turbo spin echo sequences in the coronal and sagittal planes. The postoperative MRI findings were classified into 5 categories according to the criteria of Sugaya et al,21 and we considered type I to III as a healed rotator cuff and type IV and V as a full-thickness retear. In patients with retears, we measured (1) tear size, (2) fatty degeneration, and (3) tear pattern. The measurements were performed by 2 fellows-in-training in orthopaedic shoulder surgery. All reviewers were blinded to patient demographics, symptoms, and physical examination findings. Each scan was reviewed twice by both reviewers, and the interval between the first review and the second review was 1 month.
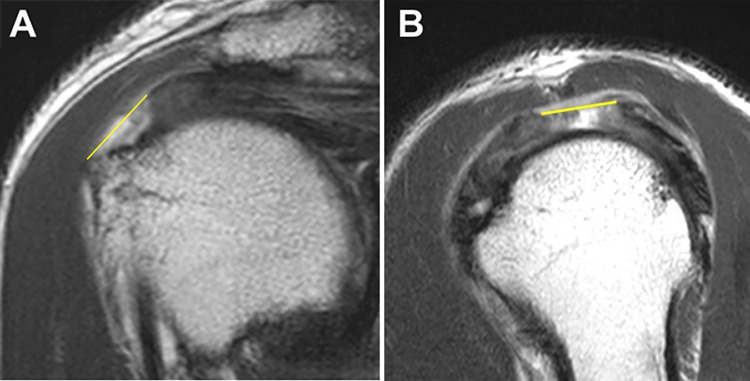
The preoperative tear size was classified as small (<1 cm), medium (1 to <3 cm), large (3 to <5 cm), and massive (≥5 cm). The size of the tear was measured in both the coronal and the sagittal planes, and the plane in which the tear was observed to be the largest was selected. For consistency, the measurements were performed according to the following principles: (1) the tendon margin of the bursa side was measured; (2) scar tissue was excluded; and (3) if tendon tissue was partially present, the degree of the tear was considered to be ≤50% (Figure 1). If the size measurement was ambiguous, such as in patients with previous surgery for severe tendinosis, it was excluded from the analysis. Tear sizes were further compared in terms of preoperative to postoperative difference (preoperative tear size – postoperative tear size): increased (<–5 mm), decreased (>5 mm), and unchanged (–5 to 5 mm).
Figure 1.
Magnetic resonance imaging scans obtained with T2-weighted turbo spin echo sequences. The size of the tear was measured in the (A) coronal and (B) sagittal planes (yellow line means the measured length). The measurements were performed according to the following principles: (1) the tendon margin of the bursa side was measured; (2) scar tissue was excluded; and (3) if tendon tissue was partially present, the degree of the tear was considered to be ≤50%.
The fatty degeneration of the supraspinatus, infraspinatus, and subscapularis in the Y view of the sagittal plane was measured and categorized according to the Goutallier classification.20
The postoperative rotator cuff retear patterns were divided into 2 types, as described by Cho and Rhee1: type I tissue repaired at the insertion site of the rotator cuff was not observed on the greater tuberosity, and type II residual rotator cuff tissue was observed at the insertion site despite a retear.
Statistical Analysis
Intraobserver reliability and interobserver agreement were analyzed using the intraclass correlation coefficient for continuous variables and the Cohen kappa coefficient (κ value) for categorical variables. The pre- and postoperative values were analyzed using the paired t test. To compare the groups, the chi-square or Fisher exact test was used for categorical variables, whereas analysis of variance or the Kruskal-Wallis test was used depending on the normality for continuous variables. Post hoc analysis was performed using the Bonferroni correction.
Results
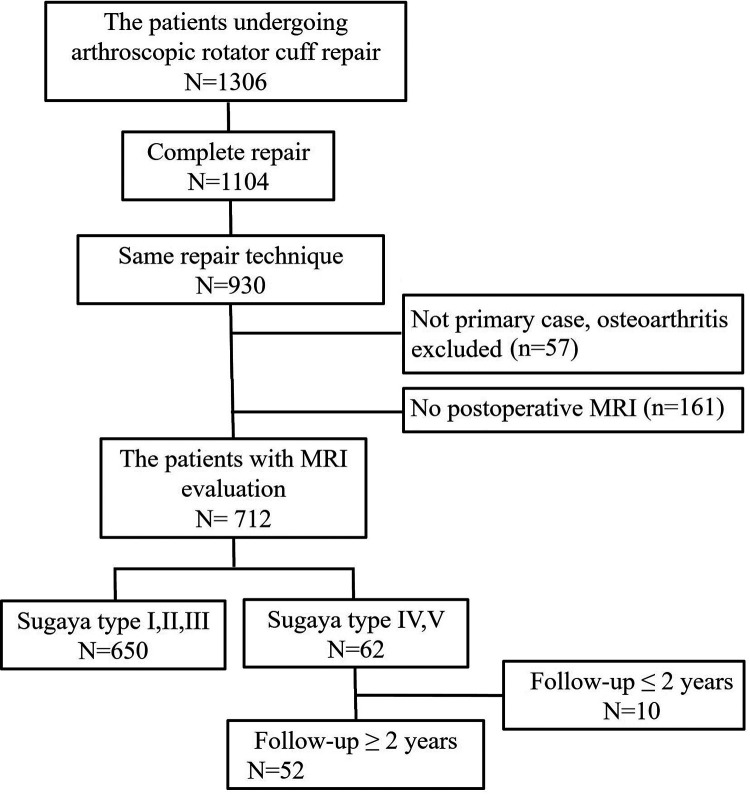
Of 1306 patients, 52 were ultimately included in this study (Figure 2). There were 25 men and 27 women with a mean age of 62.6 years (range, 49-80 years) and mean follow-up period of 40 months (range, 24-88 months).
Figure 2.
Flowchart of patient exclusion and selection.
Clinical Results
Of the 52 patients, 44 were available for final follow-up at our outpatient clinic at a minimum of 2 years postoperatively, and 8 patients were followed up via telephone. The pVAS, fVAS, and ASES scores were analyzed in all 52 patients, and the Constant score, SST score, and ROM were analyzed in the 44 patients who were followed up in person. The pre- and postoperative clinical data of all patients are summarized in Table 1. All clinical scores were significantly improved after surgery.
Table 1.
Pre- and Postoperative Clinical Data of All Patientsa
| Preoperative | Final Follow-up | P Value | |
|---|---|---|---|
| pVAS | 5.0 ± 2.2 | 2.0 ± 2.5 | <.001b |
| fVAS | 5.1 ± 2.2 | 7.7 ± 2.1 | <.001b |
| ASES | 48 ± 19 | 76 ± 21 | <.001b |
| Constantc | 53 ± 19 | 69 ± 14 | <.001b |
| SSTc | 4.6 ± 2.9 | 7.9 ± 2.8 | <.001b |
aData are presented as mean ± SD. ASES, American Shoulder and Elbow Surgeons; fVAS, functional visual analog scale; pVAS, pain visual analog scale; SST, Simple Shoulder Test.
bStatistically significant.
cExcludes 8 patients who were followed up via telephone.
The 52 patients were divided into 3 groups according to pVAS and fVAS scores, with 25 (48.1%) in the mild group, 9 (17.3%) in the moderate group, and 18 (34.6%) in the severe group. The demographic data of each group are summarized in Table 2. The proportion of patients with dominant arm involvement and that of heavy labor workers in the severe group tended to be high but not statistically significant. The moderate group showed significant differences in the proportion of male patients and the follow-up period. The operative data of each group are summarized in Table 3. There was no difference in repair type, preoperative tear size, and subscapularis repair.
Table 2.
Demographic Dataa
| Mild Group (n = 25) | Moderate Group (n = 9) | Severe Group (n = 18) | P Value | |
|---|---|---|---|---|
| Sex, male/female, n | 15/10 | 1/8 | 9/9 | .056 |
| Age, mean ± SD, y | 63 ± 7 | 63 ± 6 | 62 ± 7 | .929 |
| Follow-up period, mean ± SD, mo | 38 ± 17 | 29 ± 7 | 48 ± 20 | .027b |
| Dominant arm involvement | 13 (52) | 6 (67) | 15 (83) | .103 |
| Heavy labor worker | 6 (24) | 4 (44) | 10 (56) | .102 |
| Diabetes | 4 (16) | 1 (11) | 3 (17) | >.99 |
| Smoking history | 2 (8) | 0 (0) | 1 (6) | >.99 |
| Education level of college graduate or higher | 11 (44) | 1 (11) | 4 (22) | .122 |
aData are presented as n (%) unless otherwise specified.
bStatistically significant between moderate and severe groups.
Table 3.
Preoperative Tear Size and Operative Data
| Mild Group (n = 25) | Moderate Group (n = 9) | Severe Group (n = 18) | P Value | |
|---|---|---|---|---|
| Repair type, I/II, n | 19/6 | 6/3 | 14/4 | .831 |
| Preoperative tear size, n | .767 | |||
| Partial | 2 | 1 | 5 | |
| Small | 2 | 0 | 1 | |
| Medium | 13 | 5 | 7 | |
| Large | 8 | 3 | 5 | |
| Subscapularis repair, n (%) | 6 (24) | 2 (22) | 4 (22) | >.99 |
The pre- and postoperative clinical data of each group are summarized in Table 4. As we divided the patients into groups according to clinical scores, the clinical scores at the final follow-up showed a significant difference. Conversely, there was no difference between the groups for pre- and 6-month postoperative clinical scores. In the severe group, 4 patients eventually underwent revision surgery (3 patients underwent revision rotator cuff repair, and 1 patient underwent reverse total shoulder arthroplasty). The pre- and postoperative ROM measurements are summarized in Table 5. There was no significant difference in ROM between the groups at any time [c/u].
Table 4.
Pre- and Postoperative Clinical Data by Groupa
| Mild Group (n = 25) |
Moderate Group (n = 9) |
Severe Groupb
(n = 18) |
P Value | |
|---|---|---|---|---|
| Preoperative | ||||
| pVAS | 5.0 ± 2.2 | 4.6 ± 2.1 | 5.3 ± 2.3 | .746 |
| fVAS | 5.1 ± 2.4 | 5.7 ± 1.3 | 4.8 ± 2.3 | .656 |
| ASES | 48 ± 21 | 58 ± 13 | 42 ± 17 | .116 |
| Constant | 52 ± 23 | 54 ± 14 | 51 ± 18 | .926 |
| SST | 5.0 ± 3.8 | 5.5 ± 2.2 | 4.0 ± 2.9 | .393 |
| 6 mo | ||||
| pVAS | 3.2 ± 2.1 | 2.0 ± 1.2 | 3.9 ± 2.0 | .061 |
| fVAS | 6.4 ± 1.7 | 6.6 ± 1.1 | 6.3 ± 1.9 | .946 |
| ASES | 60 ± 17 | 67 ± 9 | 56 ± 15 | .243 |
| Constant | 56 ± 16 | 58 ± 12 | 54 ± 13 | .781 |
| SST | 6.6 ± 2.5 | 6.7 ± 1.0 | 5.1 ± 3.2 | .239 |
| Final follow-up | ||||
| pVAS | 0.2 ± 0.4 | 1.1 ± 0.8 | 4.9 ± 1.9 | .026c |
| fVAS | 9.2 ± 0.8 | 7.2 ± 1.4 | 5.7 ± 1.7 | <.001d |
| ASES | 92 ± 7 | 75 ± 6 | 53 ± 17 | <.001c |
| Constante | 79 ± 9 | 67 ± 8 | 56 ± 12 | <.001d |
| SSTe | 9.7 ± 1.5 | 7.9 ± 2.0 | 5.4 ± 2.3 | <.001f |
aData are presented as mean ± SD. ASES, American Shoulder and Elbow Surgeons; fVAS, functional visual analog scale; pVAS, pain visual analog scale; SST, Simple Shoulder Test.
bData of 4 patients with revision surgery were at the time of revision.
cStatistically significant between mild and severe, mild and moderate, and moderate and severe groups.
dStatistically significant between mild and severe groups and between mild and moderate groups.
eExcludes 8 patients who were followed up via telephone.
fStatistically significant between mild and severe groups.
Table 5.
Pre- and Postoperative Range of Motiona
| Mild Group (n = 25) |
Moderate Group (n = 9) |
Severe Group (n = 18) |
P Value | |
|---|---|---|---|---|
| Preoperative | ||||
| Forward flexion | 139 ± 44 | 153 ± 23 | 144 ± 33 | .393 |
| External rotation | 43 ± 16 | 53 ± 22 | 50 ± 14 | .100 |
| Internal rotationb | 8.2 ± 2.0 | 6.8 ± 3.0 | 8.7 ± 2.1 | .547 |
| 6 mo | ||||
| Forward flexion | 135 ± 27 | 149 ± 13 | 144 ± 17 | .258 |
| External rotation | 35 ± 17 | 42 ± 10 | 37 ± 21 | .443 |
| Internal rotationb | 7.6 ± 1.6 | 7.3 ± 2.4 | 8.0 ± 1.7 | .306 |
| Final follow-upc | ||||
| Forward flexion | 155 ± 16 | 164 ± 9 | 150 ± 17 | .065 |
| External rotation | 54 ± 12 | 51 ± 11 | 47 ± 16 | .375 |
| Internal rotationb | 8.8 ± 1.2 | 8.0 ± 1.9 | 8.4 ± 1.4 | .466 |
aData are presented as mean ± SD.
bInternal rotation measured at the vertebral level was converted to a number: T4-T7 to 10, T8-T12 to 8, L1-L3 to 6, L4-L5 to 4, and sacrum and buttock to 2.
cExcludes 8 patients who were followed up via telephone.
Radiological Results
There were 3 patients who were excluded as a result of ambiguous MRI measurements (2 tendinosis and 1 partial tear), and the data of 49 patients were analyzed. The intraobserver reliability and interobserver agreement values are summarized in Table 6. Except for interobserver agreement for the subscapularis, generally good reliability and agreement were found. MRI measurements were analyzed with observer 1’s measurements.
Table 6.
Intraobserver Reliability and Interobserver Agreementa
| Tear Size | Intraobserver Reliability, ICC (95% CI) | Interobserver Agreement, ICC (95% CI) |
|---|---|---|
| Preoperative | ||
| Coronal | 0.95 (0.92-0.97) | 0.95 (0.91-0.97) |
| Sagittal | 0.93 (0.88-0.96) | 0.93 (0.88-0.96) |
| Postoperative | ||
| Coronal | 0.95 (0.92-0.97) | 0.95 (0.91-0.97) |
| Sagittal | 0.95 (0.91-0.97) | 0.93 (0.89-0.96) |
| Goutallier Grade | Intraobserver Reliability, κ Value (95% CI) | Interobserver Agreement, κ Value (95% CI) |
| Preoperative | ||
| Supraspinatus | 0.85 (0.75-0.95) | 0.87 (0.78-0.97) |
| Infraspinatus | 0.69 (0.54-0.83) | 0.69 (0.55-0.83) |
| Subscapularis | 0.73 (0.57-0.88) | 0.51 (0.31-0.70) |
| Postoperative | ||
| Supraspinatus | 0.88 (0.78-0.98) | 0.55 (0.39-0.71) |
| Infraspinatus | 0.67 (0.53-0.81) | 0.72 (0.58-0.87) |
| Subscapularis | 0.77 (0.64-0.91) | 0.36 (0.13-0.60) |
aInterpretation of intraclass correlation coefficients (ICCs) and κ values: <0.00, no agreement; 0.00-0.20, slight agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, substantial agreement; and 0.81-1.00, almost perfect agreement.
The tear size values are summarized in Table 7. The preoperative tear sizes were not significantly different among the 3 groups in the coronal and sagittal planes. The tear size in the coronal and sagittal planes decreased by 5.1 and 6.6 mm, respectively, in the mild group but increased by 2.8 and 1.4 mm, respectively, in the severe group. The severe group tended to show an increased tear size but without statistical significance. A 5-mm increase in tear size was observed in the coronal and sagittal planes in 1 and 3 patients, respectively, in the mild group and in 8 and 6 patients, respectively, in the severe group. Statistical significance was obtained for only 2 tear size values. The tear size difference was statistically different between the mild and moderate groups in the sagittal plane (statistical power: 0.69), and the tear size change was statistically different between the mild and severe groups in the coronal plane (statistical power: 0.88).
Table 7.
Pre- and Postoperative Tear Size on Magnetic Resonance Imaginga
| Mild Group (n = 23) | Moderate Group (n = 9) | Severe Group (n = 17) | P Value | |
|---|---|---|---|---|
| Coronal | ||||
| Preoperative tear size, mm | 20.6 ± 8.8 | 20.4 ± 11.3 | 18.3 ± 8.8 | .798 |
| Postoperative tear size, mm | 15.5 ± 7.6 | 18.7 ± 12.1 | 21.2 ± 8.2 | .138 |
| Tear size difference,b mm | 5.1 ± 8.6 | 1.8 ± 13.6 | –2.8 ± 13.4 | .106 |
| Tear size change,c increased/decreased/unchanged, n | 1/11/11 | 3/3/3 | 8/5/4 | .026d |
| Sagittal | ||||
| Preoperative tear size, mm | 20.3 ± 9.6 | 15.1 ± 7.1 | 16.8 ± 8.4 | .244 |
| Postoperative tear size, mm | 13.8 ± 7.9 | 17.7 ± 10.7 | 18.2 ± 8.5 | .228 |
| Tear size difference,b mm | 6.6 ± 8.7 | –2.6 ± 9.6 | –1.4 ± 13.5 | .032e |
| Tear size change,c increased/decreased/unchanged, n | 3/13/7 | 4/2/3 | 6/4/7 | .135 |
aData are presented as mean ± SD unless otherwise specified.
bDifference = preoperative tear size – postoperative tear size.
cIncreased, <–5 mm; decreased, >5 mm; and unchanged, –5 to 5 mm.
dStatistically significant between mild and severe groups.
eStatistically significant between mild and moderate groups.
The fatty degeneration values are summarized in Table 8. There was no significant difference in the Goutallier classification of the supraspinatus, infraspinatus, and subscapularis in any of the 3 groups. In the analysis of retear patterns, types I and II were observed in 13 and 12 patients, respectively, in the mild group; in 6 and 3 patients, respectively, in the moderate group; and in 7 and 11 patients, respectively, in the severe group. There was no statistical difference among the 3 groups.
Table 8.
Pre- and Postoperative Fatty Degeneration on Magnetic Resonance Imaginga
| Mild Group (n = 23) | Moderate Group (n = 9) | Severe Group (n = 17) | P Value | |
|---|---|---|---|---|
| Supraspinatus | ||||
| Preoperative, 0/1/2/3/4 | 0/0/10/7/6 | 0/0/3/1/5 | 0/1/5/6/5 | .518 |
| Postoperative, 0/1/2/3/4 | 0/0/10/10/3 | 0/0/2/3/4 | 0/0/3/5/9 | .082 |
| Infraspinatus | ||||
| Preoperative, 0/1/2/3/4 | 3/13/4/2/1 | 1/5/2/1/0 | 1/4/9/2/1 | .329 |
| Postoperative, 0/1/2/3/4 | 2/13/6/2/0 | 1/5/2/1/0 | 0/4/7/5/1 | .201 |
| Subscapularis | ||||
| Preoperative, 0/1/2/3/4 | 6/11/5/1/0 | 2/5/2/0/0 | 3/9/3/1/1 | .987 |
| Postoperative, 0/1/2/3/4 | 6/11/5/1/0 | 1/5/3/0/0 | 1/11/4/0/1 | .620 |
aData are presented as No. According to the Goutallier classification: grade 0 = no fat; grade 1 = some thin fatty streaks; grade 2 = significant fatty infiltration but muscle tissue predominates; grade 3 = equal contribution of fat and muscle tissue; and grade 4 = more fat than muscle is present.
Discussion
We found that nonoperative treatment for retears after rotator cuff repair showed good clinical outcomes in 48.1% of patients. Changes in the tear size measured on MRI were the only factors we identified that affected clinical outcomes. The preoperative tear size on MRI did not differ among the 3 groups, although patients with severe symptoms tended to show an increased tear size on MRI.
Other studies have looked at patients with retears as a single group, while our study divided patients with retears according to clinical scores and compared them. In the study of Yoo et al,26 the retear group was compared with the healed group and showed inferior results compared with the healed group. The mean VAS and ASES scores in the retear group were 1.5 and 88.3, respectively, whereas those in the healed group were 1.1 and 93.1, respectively. Similar results were reported by Kim et al.9 The mean ASES and SST scores of the retear group were 69.2 and 6.5, respectively, whereas those of the intact group were 91.0 and 10.2, respectively. We divided patients into groups according to the pVAS and fVAS scores and found that 48.1% of patients had very mild symptoms. In our study, the mean pVAS, ASES, and SST scores of the mild group were 0.2, 92, and 9.7, respectively. These clinical outcomes were similar to those of the intact group in the abovementioned studies. Although the overall outcomes of patients with retears were inferior to those of patients with an intact rotator cuff, not all patients had inferior outcomes. Some patients with retears could have similar outcomes to those with an intact rotator cuff.
We classified patients with good clinical outcomes, and 48.1% sustained few symptoms of discomfort. Thus, when we treat a patient with a retear in the clinic, about 50% of the patients with retears may have good outcomes. The mild group had similar scores to the severe group at 6 months but made significant improvements as regards pain and function between 6 months and final follow-up. Therefore, the decision reagarding whether to reoperate should generally be made well after 6 months. However, patients were not ideally classified into groups. Some patients did not have good or poor clinical results; we classified these patients as the moderate group. By dividing into these 3 groups, the sample size was smaller and imbalanced. This can increase the probability of type I or II errors. In addition, repair type or preoperative tear size affects clinical outcomes.2,13 However, there was no significant difference in these values in each group in our study. This may also be because of the small sample size.
An important finding of this study was that patients with severe symptoms tended to show an increased tear size on MRI, although the preoperative tear size on MRI did not differ among the 3 groups. It has been reported that nonoperative treatment does not restore torn rotator cuffs but may improve clinical symptoms.11,12,17 Patients with retears in this study performed ROM and strengthening exercises. We recommended exercise training for more than 2 years. At the time of surgery, we performed several procedures, such as simultaneous bursectomy and acromioplasty. We performed the same nonoperative treatment and additional surgical procedures in all patients; however, patients with an increased tear size showed inferior outcomes. The tear size in the coronal and sagittal planes decreased by 5.1 and 6.6 mm, respectively, in the mild group, whereas in the severe group, it increased by 2.8 and 1.4 mm, respectively. In a study by Mall et al,15 pain in shoulders with an asymptomatic rotator cuff tear was associated with an increase in tear size. This result is similar to our finding. In our study, patients with an increased tear size showed poor outcomes.
The severity of a rotator cuff tear is not always associated with symptoms.6,9 Dunn et al6 reported that comorbidities, lower education level, and race were associated with clinical symptoms. In a study by Kim et al,9 nonanatomic factors, including younger age, lower education level, and workers’ compensation claims, were associated with poor outcomes in patients with retears. In our study, the proportions of heavy labor workers and patients with dominant arm involvement were 56% and 83%, respectively, in the severe group and 24% and 52%, respectively, in the mild group. Although there was no statistical difference, we believe that there may be a possibility of a type II error because of the small sample size. Sex, dominant arm, and heavy labor are factors that might have been significant with a larger sample size. Age has been reported to be associated with retears and affect symptoms after a retear.4,9 In our study, the mean ages of patients in the mild and severe groups were 63 and 62 years, respectively, with no significant difference.
Fatty degeneration has been shown to be a poor prognostic factor for rotator cuff repair.2,7 In this study, fatty degeneration was considered an important factor, and the supraspinatus, infraspinatus, and subscapularis were individually graded. However, we could not find any difference in fatty degeneration among the groups. In the study by Deniz et al,3 fatty degeneration and atrophy worsened in retear cases. In our study, the number of patients with supraspinatus grade 4 fatty degeneration in the severe group increased from 5 to 9; however, the sample size was small, and we could not obtain a statistically significant difference.
In our study, ROM was assessed preoperatively, 6 months after surgery, and at the final follow-up. The mean forward flexion at the final follow-up in the mild and severe groups was 155° and 150°, respectively, without statistical significance. In the study by Teratani,22 stiffness after surgery was associated with rotator cuff healing, and the final ROM of the retear group also did not show a significant difference from that of the healed group. Our results showed that the mild group had less ROM at 6 months after surgery, but the final ROM was better. However, we did not find a significant difference because of the small number of samples.
Our study had several limitations. First, it was designed as a retrospective study. Second, the number of included cases was small, which might increase the probability of a type II error. Third, there was no long-term follow-up. The patients in the mild group may have developed symptoms over time. More research on this may be needed. Fourth, we included only patients with complete repair and double-row repair for consistency in clinical outcomes, resulting in 29% of patients being excluded. Also, 17% of patients were excluded for not undergoing MRI after surgery. If the proportion of these exclusions is different in each group, it may be the result of bias. Fifth, there may be a bias in the MRI measurements. To reduce bias, we established our principles for measurements and checked their reliability and agreement. Finally, the timing of postoperative MRI and the collection of final clinical scores were different. Postoperative MRI examinations were performed within a mean of 6 months from surgery, whereas clinical scores were obtained at the final follow-up at a minimum of 2 years after surgery. However, a previous study10 showed that MRI at 6 months postsurgically was not significantly different from MRI at 2 years after surgery.
Conclusion
In the current study, 48.1% of patients with retears had only mild symptoms at a mean of 40 months postoperatively. The patients with severe symptoms tended to have an increased tear size on postoperative MRI. Our study suggests that even with retears, partial tear healing results in good clinical outcomes, whereas complete reruptures of the tendon will result in poor outcomes. This might be one reason why some patients do well and some do poorly after a retear.
Footnotes
Final revision submitted June 11, 2020; accepted June 26, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Samsung Medical Center (study No. 2019-07-018-001).
References
- 1. Cho NS, Rhee YG. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1(2):96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Choi S, Kim MK, Kim GM, Roh YH, Hwang IK, Kang H. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. 2014;23(11):1675–1681. [DOI] [PubMed] [Google Scholar]
- 3. Deniz G, Kose O, Tugay A, Guler F, Turan A. Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: does it improve, halt or deteriorate? Arch Orthop Trauma Surg. 2014;134(7):985–990. [DOI] [PubMed] [Google Scholar]
- 4. Diebold G, Lam P, Walton J, Murrell GAC. Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Joint Surg Am. 2017;99(14):1198–1205. [DOI] [PubMed] [Google Scholar]
- 5. Dunn WR, Kuhn JE, Sanders R, et al. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2016;25(8):1303–1311. [DOI] [PubMed] [Google Scholar]
- 6. Dunn WR, Kuhn JE, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity: a cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J Bone Joint Surg Am. 2014;96(10):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35(5):719–728. [DOI] [PubMed] [Google Scholar]
- 8. Jeong JY, Park KM, Sundar S, Yoo JC. Clinical and radiologic outcome of arthroscopic rotator cuff repair: single-row versus transosseous equivalent repair. J Shoulder Elbow Surg. 2018;27(6):1021–1029. [DOI] [PubMed] [Google Scholar]
- 9. Kim HM, Caldwell JM, Buza JA, et al. Factors affecting satisfaction and shoulder function in patients with a recurrent rotator cuff tear. J Bone Joint Surg Am. 2014;96(2):106–112. [DOI] [PubMed] [Google Scholar]
- 10. Koh KH, Laddha MS, Lim TK, Park JH, Yoo JC. Serial structural and functional assessments of rotator cuff repairs: do they differ at 6 and 19 months postoperatively? J Shoulder Elbow Surg. 2012;21(7):859–866. [DOI] [PubMed] [Google Scholar]
- 11. Kukkonen J, Joukainen A, Lehtinen J, et al. Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am. 2015;97(21):1729–1737. [DOI] [PubMed] [Google Scholar]
- 12. Lambers Heerspink FO, van Raay JJ, Koorevaar RC, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015;24(8):1274–1281. [DOI] [PubMed] [Google Scholar]
- 13. Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. [DOI] [PubMed] [Google Scholar]
- 14. Li H, Chen Y, Chen S. Postoperative residual pain is associated with a high magnetic resonance imaging (MRI)-based signal intensity of the repaired supraspinatus tendon. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):4014–4020. [DOI] [PubMed] [Google Scholar]
- 15. Mall NA, Kim HM, Keener JD, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92(16):2623–2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16(4):469–476. [DOI] [PubMed] [Google Scholar]
- 17. Ranebo MC, Bjornsson Hallgren HC, Holmgren T, Adolfsson LE. Surgery and physiotherapy were both successful in the treatment of small, acute, traumatic rotator cuff tears: a prospective randomized trial. J Shoulder Elbow Surg. 2020;29(3):459–470. [DOI] [PubMed] [Google Scholar]
- 18. Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39(4):710–714. [DOI] [PubMed] [Google Scholar]
- 19. Schmidt CC, Jarrett CD, Brown BT. Management of rotator cuff tears. J Hand Surg Am. 2015;40(2):399–408. [DOI] [PubMed] [Google Scholar]
- 20. Somerson JS, Hsu JE, Gorbaty JD, Gee AO. Classifications in brief: Goutallier classification of fatty infiltration of the rotator cuff musculature. Clin Orthop Relat Res. 2016;474(5):1328–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307–1316. [DOI] [PubMed] [Google Scholar]
- 22. Teratani T. Correlation between retear after arthroscopic rotator cuff repair and stiffness of the shoulder. J Orthop. 2019;16(5):426–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Valencia Mora M, Morcillo Barrenechea D, Martin Rios MD, Foruria AM, Calvo E. Clinical outcome and prognostic factors of revision arthroscopic rotator cuff tear repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2157–2163. [DOI] [PubMed] [Google Scholar]
- 24. Yang J, Jr, Robbins M, Reilly J, Maerz T, Anderson K. The clinical effect of a rotator cuff retear: a meta-analysis of arthroscopic single-row and double-row repairs. Am J Sports Med. 2017;45(3):733–741. [DOI] [PubMed] [Google Scholar]
- 25. Yoo JC, Ahn JH, Yang JH, Koh KH, Choi SH, Yoon YC. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2009;25(6):573–582. [DOI] [PubMed] [Google Scholar]
- 26. Yoo JH, Cho NS, Rhee YG. Effect of postoperative repair integrity on health-related quality of life after rotator cuff repair: healed versus retear group. Am J Sports Med. 2013;41(11):2637–2644. [DOI] [PubMed] [Google Scholar]
- 27. Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C. Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Joint Surg Am. 2007;89(9):1928–1934. [DOI] [PubMed] [Google Scholar]