Abstract
Purpose of Review
To review and discuss the findings of systematic reviews that synthesized the evidence on the effect of preoperative exercises (prehabilitation) on postoperative functional recovery in older adults undergoing total knee or hip joint replacement.
Recent Findings
Ten systematic reviews (8 meta-analyses) were included in this review. Findings from the systematic reviews indicated that prehabilitation decreases length of hospital stay but does not improve postoperative functional recovery in older adults undergoing joint replacement. Individual studies in the systematic reviews varied considerably in prehabilitation protocol, assessment timepoints, and outcome measures. Most importantly, systematic reviews did not assess the outcomes pre-post prehabilitation as this timepoint was not addressed in most individual studies. Therefore, it is not known whether the prehabilitation programs improved outcomes preoperatively.
Summary
There is a need to develop comprehensive prehabilitation protocols and systematically assess the preoperative and postoperative effectiveness of prehabilitation protocols on functional outcomes (i.e., self-reported and performance-based) in older adults undergoing total joint replacement.
Keywords: prehabilitation, preoperative exercise, physical function, total knee replacement, total hip replacement, osteoarthritis
INTRODUCTION
Knee and hip Osteoarthritis (OA) are prevalent joint disorders in older adults, and contribute significantly to functional impairments, sedentary behavior, and low quality of life. Other than the burden to the individual, knee and hip OA also pose a significant burden to the health system. These conditions are amongst the most expensive to treat when joint replacement surgery is required. According to the Centers for Disease Control and Prevention, OA was the second most costly health condition treated at US hospitals in 2013, accounting for $16.5 billion in costs of hospitalizations. [1] Total joint replacement (TJR) is the most successful approach to decrease pain and improve mobility and quality of life in those suffering from severe OA. Despite the high cost, TJR is one of the most common elective surgical procedures in the United States. Total knee replacement (TKR) and total hip replacement (THR) surgeries may soon lead to a large economic burden in global health care, as they are expected to increase by 673% and 174%, respectively, between 2005 and 2030. [2, 3]. However, the elective nature of the surgery (i.e., long time gap between diagnosis and surgery) presents an opportune window for healthcare providers to improve function in individuals awaiting TJR and enhance postoperative functional recovery.
Preoperative exercises (prehabilitation) have gained significant attention in the last decade. The concept behind prehabilitation exercises is to prepare the individual for surgery by improving functional outcomes before surgery. Individuals with OA who are awaiting TJR have severe functional impairments and muscle weaknesses due to pain and lack of physical activity. Some studies suggested that a well-designed prehabilitation exercise program can improve pain, range of motion, physical function, and quality of life in individuals awaiting TJR. [4-7] These preoperative improvements seem to lead to improved outcomes postoperatively compared to individuals who followed the standard of care (i.e. no exercises done preoperatively). On the contrary, other studies have shown that prehabilitation exercises are not effective in improving postoperative outcomes.
To date, several systematic reviews and meta-analyses investigating the evidence about the effect of prehabilitation on postoperative outcomes have been published. These systematic reviews investigated the effect of prehabilitation on various postoperative outcomes such as pain, function, quality of life, lower extremity strength, and length of hospital stay. Due to discrepancies in original study findings, heterogeneity of outcomes and timepoints assessed, and type of question explored, several systematic reviews have reported inconclusive or contradicting results. The purpose of the current review is to synthesize the most recent evidence (past five years) on effectiveness of prehabilitation on postoperative functional recovery in older adults with knee or hip OA awaiting TJA from systematic reviews and meta-analysis. This review will examine the strengths and limitations of the current evidence and discuss applicability to clinical practice and recommendations for future research.
MATERIALS AND METHODS
We searched several relevant databases (PubMed, EMBASE and Cochrane) from inception up to June 2020. To avoid significant overlap in individual studies included in the systematic reviews and meta-analysis, and to present evidence from the most recent research as suggested by the journal, we included reviews from 2015 to present. Systematic reviews and met-analysis were included if they synthesized studies including preoperative exercises (prehabilitation) in older adults awaiting TKR and/or THR, and included functional outcomes such as muscle strength and physical function (e.g., self-reported or performance-based). To address our aim, we searched for relevant articles combining the following terms: (“arthroplasty, replacement, knee” [MESH] OR “arthroplasty, replacement, hip” [MESH]) AND (exercise OR “rehabilitation”) AND ("Preoperative Period" [Mesh] OR “prehabilitation” OR “pre-habilitation” OR “pre-rehabilitation” OR prerehabilitation) AND (“systematic review” OR “meta-analysis”). Two reviewers (GJA and SSK) reviewed all titles and abstracts identified through the search strategy and retrieved the full text when a study seemed appropriate to be included in this review. The reviewers also hand searched the reference lists of articles to identify potential studies not detected by the search strategy.
Data from eligible systematic reviews were examined and extracted independently by two reviewers (GJA and SSK). The data extracted included information on author(s), year, knee or hip TJR, number and characteristics of the studies included in the systematic review, timepoint and outcomes-assessed, whether a meta-analysis was conducted, and quality assessment of the systematic reviews. Quality Assessment was performed independently by two reviewers (GJA and SSK) using the Assessing the Methodological Quality of Systematic Reviews (AMSTAR-2) tool. [8] AMSTAR-2 contains 16-items that appraise the methodology used in the systematic reviews. Each item is scored as yes, partial yes, and no/NA. There is no total score. Presence of flaws and weaknesses translate in the overall confidence in the results of the systematic review. The overall confidence is rated as “critically low”, “low”, “moderate” or “high”.
RESULTS
A total of 28 titles and abstracts were reviewed. Most of the studies found in the literature search assessed outcomes of pain, range of motion, physical function, quality of life and strength. Studies that included surgeries other than TJR or did not include an exercise intervention preoperatively and outcomes related to functional capacity were excluded from this review: 4 studies included surgeries other than TJR; 6 studies did not have a prehabilitation intervention; 4 studies did not include outcomes related to functional capacity; and 4 studies were published before 2015. From our search strategy, we found 10 articles that met our inclusion criteria and were included in this narrative review: 5 in TKR only and 5 in THR and TKR combined. Eight of the studies included in this review performed a systematic review with meta-analyses (Table 1). [9-16] All ten studies performed a quality assessment of the original studies. Upon full-text review two of the systematic reviews used the same protocol (search strategy, selection criteria) and the same individual studies, but differed in their analysis. [9, 10] Cabilan et al assessed the effect of prehabilitation volume (number of minutes) on pain, function and quality of life, [9] while Cabilan et al assessed the effect of prehabilitation on pain at 1 and 3 months postoperatively and physical function at 3 months postoperatively. [10] These systematic reviews were treated as separate papers for the purpose of our review.
Table 1.
Characteristics of included studies.
| Systematic Review (SR) Study |
Number of studies included in SR and Sample size |
Characteristics of included studies in SR |
Time-points investigated |
Outcomes Assessed | Description of Intervention & Comparisons |
Meta-Analysis Performed? |
|---|---|---|---|---|---|---|
| Vasta et al 2020 | 14 studies (740 subjects) | RCTs, Cohort, case-control designs, knee and hip OA, Patients > 65 years | Not specified | Function (self and perform), ROM, QoL, Pain, LoS | Described intervention, but comparison groups not described | No |
| Sharma et al 2019 | 5 studies (707 subjects) | RCTs, knee OA | 3 months post TKA | Pain, stiffness, and function (self), QoL, LoS | Described intervention and comparison groups | Yes |
| Ma et al 2018 | 9 studies (777 subjects) | RCTs Knee OA | Not specified | Pain, ROM, QoL, function (self and perform), LoS | Described intervention | Yes |
| Chen et al 2018 | 16 studies (966 subjects) | RCTs, Knee OA, Patients > 18 years, English language | Not specified | LoS, strength, pain, stiffness, and function (self and perform), ROM | Partially described intervention (duration and type, not in detail) | Yes |
| Peer et al 2017 | 3 studies (82 subjects) | RCTs, Knee OA, Land-based prehabilitation programs, Full description of intervention dose, duration, frequency, English or German language | Pre-prehab Postop: 6 and 12 weeks |
Pain, stiffness, and function (self and perform), strength | Described intervention in full details along with mode, dosage, setting, frequency, duration | Yes |
| Moyer et al 2017 | 35 studies (2956 subjects) | RCTs, CPGs and SRs, Knee and hip OA, Published after 2000, English language | Pre-prehab Postop: <6 weeks, 3 mo, >6mo |
Pain, function (self), strength, anxiety, LoS | Described intervention adequately | Yes |
| Wang et al 2016 | 22 studies (1492 subjects) | RCTs Knee or Hip OA | Pre-prehab Postop: 1-12 mo |
Pain, function (self), QoL, LoS | Described intervention adequately | Yes |
| Cabilan et al 2016 | 17 studies (1424 subjects) | RCTs, Knee or Hip OA Patients > 18 years | Pre-prehab Postop: 1, 3, 6, 12 mo |
Function (self and perform), HC util, QoL, Pain | Described intervention, Dosage and volume provided | Yes |
| Kwok et al 2015 | 11 studies (741 subjects) | RCT or quasi-experimental design Knee OA | Not specified | Pain, stiffness, and function, QoL, strength, pain, ROM, LoS | Partially described intervention (duration and type, not in detail) | No |
| Cabilan et al 2015 | 17 studies (1424 subjects) | RCTs, Knee or Hip OA Patients > 18 years | Pre-prehab Postop: 1, 3, 6, 12 mo |
Function (self and perform), HC util, QoL, Pain | Described intervention, Dosage and volume provided | Yes |
Abbreviations: RCT – Randomized Clinical Trials; QoL – Quality of Life; LoS - Length of stay
Based on AMSTAR-2, the methodological quality of the systematic reviews ranged from low to moderate. The major flaws identified included not having an established review protocol a priori, lack of justification for selecting specific study designs for inclusion, not considering risk of bias when interpreting the results of the review, and not assessing publication bias (Figure).
Figure. Methodological Quality of Systematic Reviews and Meta-Analysis, assessed by AMSTAR 2.
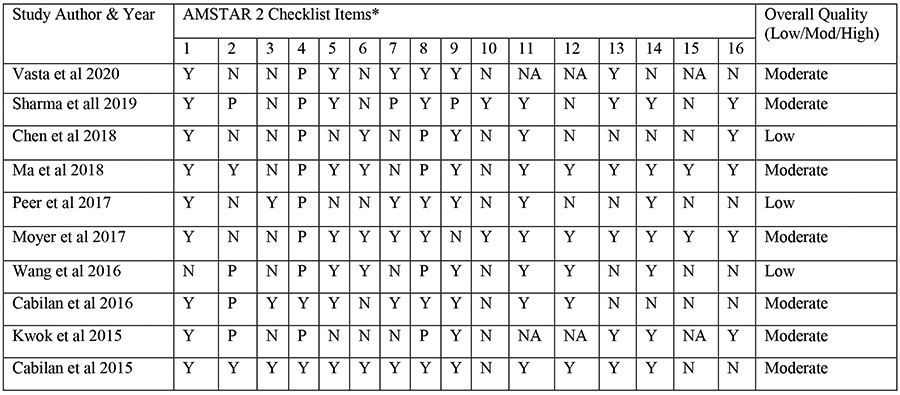
Abbreviations: Y – Yes; N – No; P – Partial Yes; NA – Not Applicable
*The AMSTAR 2 Checklist consists of 16 items and is rated based on the presence of weaknesses in critical domains. There is no overall score. [8]
Description of the numbered items:
1. Research question and inclusion criteria include components of PICO
2. Systematic review methods were established a priori
3. Selection of study design explained
4. Comprehensive literature strategy used
5. Study selection performed in duplicate
6. Data extraction performed in duplicate
7. List of excluded studies with explanation provided
8. Included studies described in adequate detail
9. Risk of Bias (RoB) in individual studies assessed
10. Funding source of included studies provided
11. Meta-analysis conducted using appropriate methods
12. Potential impact of RoB on the Meta-analysis assessed
13. Impact of RoB in individual studies on the review was discussed
14. Heterogeneity among studies was assessed and discussed
15. Publication bias assessed
16. Conflict of interest reported.
Five systematic reviews specified timepoints of interest, [9-13] which varied from prior to start of prehabilitation up to 12 months postoperatively. None of the systematic reviews reported the effectiveness of prehabilitation preoperatively, but one of them reported improvement in postoperative outcomes based on the preoperative effectiveness of the prehabilitation program. [12] Most studies described the prehabilitation programs in detail, although detailed information on exercise intensity or frequency was not always available. Prehabilitation programs varied by exercise modes (e.g., aerobic vs. anaerobic; land-based vs. water-based; proprioceptive training), delivery (home-based vs supervised), duration (range 4 to 12 weeks), and frequency (range once per week to daily). Comparison groups usually consisted of standard preoperative care, no preoperative care or restrictions, postoperative care only or education only. All the studies assessed pain and physical function (self-reported or performance-based). A few studies assessed length of hospital stay, [11, 12, 14-18] quality of life, [9-11, 13, 15-18] quadriceps strength, [12-14, 17] and range of motion [14, 17] (Table 2).
Table 2.
Effect of Prehabilitation on Post-Operative Outcomes Compared to Usual Care or no Prehabilitation
| Study | Physical Function | Quadriceps Strength | Range of Motion | Length of Hospital Stay | Pain | Quality of Life |
|---|---|---|---|---|---|---|
| Vasta et al 2020 | No difference | Not assessed | Not assessed | Significant reduction | No difference | No difference |
| Sharma et al 2019 | No difference | Not assessed | Significant reduction | No difference | No difference | |
| Ma et al 2018 | No difference | Not assessed | Significant reduction | No difference | No difference | |
| Chen et al 2018 | Improvement seen for sit-to-stand tests but not in other measures of physical function | No difference | Improved | Significant reduction | No difference | Not assessed |
| Peer et al 2017 | No difference | No difference | Not assessed | Not assessed | No difference | No difference |
| Moyer et al 2017 | Moderate and significant improvement overall (post TKA and THA). Subgroup analysis showed moderate improvements 3 months, and after effective prehabilitation programs in the THA subgroup | Moderate and significant improvement overall. Moderate and significant improvement 3 months post TKA, and after effective and ineffective programs in TKA subgroup | Not assessed | Significant reduction overall. Subgroup analysis showed significant reduction in patients post TKA | Subgroup analysis showed small but significant improvements 3 months post THA, and after effective prehabilitation programs for THA. No improvements post TKA | Not assessed |
| Wang et al 2016 | No difference | Not assessed | Not assessed | No difference | No difference | No difference |
| Cabilan et al 2016 | No difference | Not assessed | Not assessed | Not assessed | No difference | No difference |
| Kwok et al 2015 | No difference | No difference | No difference | No difference | No difference | No difference |
| Cabilan et al 2015 | No difference | Not assessed | Not assessed | Not assessed | No difference | No difference |
Effect of prehabilitation on postoperative functional recovery
Physical function was assessed in all ten systematic reviews. Only two systematic reviews reported that prehabilitation improved physical function compared to controls, [12, 14] while the remaining eight did not show significant postoperative differences in physical function between the prehabilitation and control groups. Moyer et al showed significant improvement in self-reported physical function 3 months (SMD=0.31, 95% CI [0.04, 0.59]) and over 6 months after THR (SMD=0.39, 95% CI [0.10, 0.69]) but not after TKR (SMD=0.39, 95% CI [−0.01, 0.79] and SMD=0.10, 95% CI [−0.15, 0.36], respectively). [12] Chen et al showed that prehabilitation improved sit-to-stand scores after TKR (mean difference=1.68, 95% CI [1.25–2.1]) but did not 6-minute walk test or self-reported function scores as compared to control group. [14] Quadriceps strength was assessed in four systematic reviews, and only one systematic review demonstrated that prehabilitation improved postoperative quadriceps strength. Moyer et al indicated that prehabilitation improved quadriceps strength 3 months after TKR compared to control group (SMD=0.59, 95% CI [0.17, 1.01]), but these improvements did not persist after 6 months (SMD=0.23, 95% CI [20.07, 0.52]). [12] Range of motion was assessed in two systematic reviews. Chen et al indicated that prehabilitation improved knee range of motion after TKR (mean difference=3.62, 95% CI [0.05, 7.19]) compared to control group, [14] while Kwok et al reported no significant differences between prehabilitation and control groups. [17]
Effect of prehabilitation on other postoperative outcomes
Length of hospital stay was assessed in seven systematic reviews. Five of those reviews indicated that prehabilitation reduced the length of hospital stay postoperatively by 1 to 2 days compared to control groups. [11, 12, 14-18] Pain was assessed in all systematic reviews. Only Moyer et al demonstrated that prehabilitation resulted in small but significant reduction in pain at 3 months after THR (SMD=0.34, 95% CI [0.07, 0.62]) but not after TKR (SMD=0.12, 95% CI [−0.13, 0.37]) compared to control groups. [12] The other studies reporting on pain did not show a significant difference between intervention and control groups. Lastly, none of the studies reported a significant difference between prehabilitation and control groups on quality of life measures.
DISCUSSION
The present review summarizes the current knowledge about the effect of prehabilitation on functional recovery in older adults undergoing joint replacement. The systematic reviews identified in our search had a considerable overlap of randomized clinical trials included. Yet, results of their syntheses varied across some of similar outcomes investigated. Results from the majority of the reviews did not find a positive effect of prehabilitation on outcomes related to function (i.e., physical function, quadriceps strength and range of motion). It is also relevant to mention that prehabilitation does not appear to improve pain or quality of life in those undergoing TJR. However, prehabilitation has shown effectiveness to reduce the length of hospital stay. We postulate that the reduction in hospital stay could be attributed to the individuals learning more about the surgery, familiarizing themselves with different exercises during the prehabilitation program and probably setting realistic postoperative expectations, which may have resulted in less days in the hospital. The reduction in length of hospital stay may be of significant interest to providers and healthcare systems as it can lead to lower healthcare costs and quicker transition to outpatient rehabilitation, which may accelerate postoperative recovery.
Evidence has shown that muscle volume, muscle strength, flexibility and functional ability are critical preoperative predictors for a successful early recovery in individuals undergoing TJR. [19-22] For years, researchers have strived to build evidence on the effectiveness of prehabilitation to accelerate functional recovery after orthopedic surgeries such as TJR. However, studies have not consistently found prehabilitation to improve postoperative function (as evident in our review). There are multiple reasons to justify the insufficient evidence regarding positive effects of prehabilitation programs: (1) systematic reviews have not assessed the effectiveness of prehabilitation programs preoperatively. This is key to learn whether the program was effective or not in improving strength and physical function preoperatively. If prehabilitation did not improve strength and physical function outcomes preoperatively it may not improve postoperative recovery; (2) systematic reviews have not assessed the influence of individual patient characteristics on outcomes post prehabilitation or postoperatively. Variation in severity of osteoarthritis, comorbidities, age, preoperative functional level may have contributed to the varied results; (3) Prehabilitation programs across studies reported in the systematic reviews were too heterogenous (in terms of mode, intensity, frequency, duration) to be combined; (4) Most studies reported in the systematic reviews did not appear to use recommended exercise dose/intensity to generate muscle gains. The American College of Sports Medicine recommends that resistance exercises be done at 70-80% of individual’s maximum effort (i.e., 1-repetition maximum) to improve muscle strength and volume. Such exercise intensity may not be tolerated by individuals with OA, which may reduce compliance to the prehabilitation program; and (5) None of the systematic reviews assessed compliance to the prehabilitation program, nor was there sufficient data to stratify effectiveness of prehabilitation programs based on exercise dosage.
Several studies tested different types of prehabilitation programs with very few being successful at improving postoperative functional outcomes. It appears that the biggest barrier encountered in those studies is tolerance to resistance exercises. Many individuals with osteoarthritis of the lower extremities are not able to tolerate the recommended dosage of resistance exercise (i.e. 70-80% of maximum effort). The recommended exercise load might exacerbate pain and lead to reduced compliance with exercise program. Based on the information from the studies assessed by the systematic reviews included in this review, it is not clear whether prehabilitation programs used the recommended exercise dosage. While studies have tested a variety of exercises to reduce the mechanical/joint load, they may not have achieved the desired exercise intensity and, therefore, were unsuccessful in improving functional recovery postoperatively. When designing a prehabilitation program for older adults awaiting TJR it is imperative to consider alternate exercise interventions that are tolerable and effective to improve muscle and physical function.
Alternative approaches to traditional resistance training that help minimize mechanical load while still providing the physiologic gains include neuromuscular electrical stimulation (NMES) and blood-flow restriction (BFR). NMES is one of the most common alternative resistance training modalities in the rehabilitation field. NMES has shown to improve quadriceps muscle volume, strength, and quality (i.e., amount of fat infiltration in the muscle) by applying a low NMES dosage of 10-20% of individual’s maximal quadriceps voluntary contraction. [23] It is hypothesized that the improvements in muscle strength resulted from NMES interventions are due to the metabolic stimuli that lead to neural adaptations. [24] Low resistance exercises with blood-flow restriction (BFR) is a more recent approach to resistance exercise and has garnered significant attention from rehabilitation professionals. The approach is attractive because resistance exercises using BFR require a low load (<50% of the individual’s maximum muscle voluntary contraction) to produce the same effect as volitional exercises applied at high loads (>70% of the individual’s maximum muscle voluntary contraction). [25] Studies have also shown that the low mechanical load with BFR also results in significant morphological and neuromuscular adaptations in the skeletal muscles (e.g. increase in growth hormone and insulin-like-growth-factor. [25-28] Therefore, switching from mechanical to a metabolic load during exercises may be beneficial in individuals with joint degeneration. [29] Implementing interventions such as NMES and low resistance BFR training during prehabilitation may be more tolerable to individuals awaiting TJR and may lead to an accelerated postoperative recovery.
This review has its limitations. Our conclusions were drawn based on systematic reviews of low to moderate quality. Even though the systematic reviews identified overlapped considerably in terms of original studies included, results from the reviews varied due to the different ways the outcomes were analyzed. Further, none of the systematic reviews assessed the effect of prehabilitation prior to surgery. To that end, future studies with rigorous methodology are warranted to test the effect of prehabilitation with adequate dosage and alternate exercise approaches such as NMES and BFR. One important consideration is assessing the effect of prehabilitation on outcomes prior to surgery, to determine whether the prehabilitation program was successful. Studies should standardize the reporting of outcomes, measure effectiveness of the prehabilitation programs preoperatively and assess compliance. To improve methodological quality, future studies should follow guidelines such as the CONSORT Statement (for randomized clinical trials) and the AMSTAR (for systematic reviews and meta-analyses).
CONCLUSIONS
Prehabilitation is effective in reducing the length of hospital stay in older adults undergoing TJR. However, there is little evidence supporting the effectiveness of prehabilitation in improving outcomes related to function and quality of life pre and postoperatively. Future studies should develop and test innovative interventions that are effective in improving muscle strength and function, and that can be well tolerated by older adults awaiting TJR.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
Gustavo J. Almeida, Samannaaz S. Khoja, and Boris A. Zelle declare that they have no conflict of interest.
Disclosures
Gustavo J. Almeida and Samannaaz S. Khoja have nothing to disclose.
Boris A. Zelle has consulted for KCI Inc. USA and DepuySynthes® and received compensation. Dr. Zelle has received speaker fees from AO North America, and research grants from DepuySynthes, KCI, Department of Defense, and the Orthopaedic Trauma Association. Dr. Zelle has received educational grants from Smith and Nephew Inc. and Arthrex®. None of these activities are related to the content of this article.
Contributor Information
Gustavo J. Almeida, Department of Physical Therapy, School of Health Professions, University of Texas Health Science Center at San Antonio; Department of Orthopaedics, Long School of Medicine, University of Texas Health Science Center at San Antonio.
Samannaaz S. Khoja, Department of Physical Therapy, School of Health and Rehabilitation Sciences, University of Pittsburgh.
Boris A. Zelle, Department of Orthopaedics, Long School of Medicine, University of Texas Health Science Center at San Antonio.
REFERENCES
- 1.Centers for Disease Control and Prevention. The Cost of Arthritis in US Adults. https://www.cdc.gov/arthritis/data_statistics/cost.htm (2020, February 27). [Google Scholar]
- 2.Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24(2):195–203. [DOI] [PubMed] [Google Scholar]
- 3.Fischer ES, Bell JS, Tomek IM, Esty AR, Godman DC. Trends and regional variation in hip, knee, and shoulder replacement. Hanover, NH: The Dartmouth Institute for Health Policy and Clinical Practice; 2010. April 6. [PubMed] [Google Scholar]
- 4.Brown K, Topp R, Brosky JA, Lajoie AS. Prehabilitation and quality of life three months after total knee arthroplasty: a pilot study. . Percept Mot Skills 2012;3:765–74. [DOI] [PubMed] [Google Scholar]
- 5.Gstoettner M, Raschner C, Dirnberger E, Leimser H, Krismer M. Preoperative proprioceptive training in patients with total knee arthroplasty. The Knee. 2011;18(4):265–70. [DOI] [PubMed] [Google Scholar]
- 6.McKay C, Prapavessis H, Doherty T. The effect of a prehabilitation exercise program on quadriceps strength for patients undergoing total knee arthroplasty: a randomized controlled pilot study. Phys Med Rehab. 2012;4(9):647–56. [DOI] [PubMed] [Google Scholar]
- 7.Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R, Roos EM. Postoperative effects of neuromuscular exercise prior to hip or knee arthroplasty: a randomised controlled trial. . Annals of the rheumatic diseases. 2014;73(6):1130–7. [DOI] [PubMed] [Google Scholar]
- 8.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed). 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cabilan CJ, Hines S, Munday J. The Impact of Prehabilitation on Postoperative Functional Status, Healthcare Utilization, Pain, and Quality of Life: A Systematic Review. . Orthopedic nursing. 2016;35(4):224–37. [DOI] [PubMed] [Google Scholar]
- 10.Cabilan CJ, Hines S, Munday J. The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. . JBI database of systematic reviews and implementation reports. 2015;13(1):146–87. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Lee M, Zhang Z, Moodie J, Cheng D, Martin J. Does preoperative rehabilitation for patients planning to undergo joint replacement surgery improve outcomes? A systematic review and meta-analysis of randomised controlled trials. . BMJ open. 2016;6(2):e009857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.••.Moyer R, Ikert K, Long K, Marsh J. The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev. 2017;5(12):e2.- This systematic review analyzed 35 individual studies (2956 subjects) and reported that prehabilitation exercises can improve physical function, quadriceps strengh, length of hospital stay and pain after total joint replacement.
- 13.Peer MA, Rush R, Gallacher PD, Gleeson N. Pre-surgery exercise and post-operative physical function of people undergoing knee replacement surgery: A systematic review and meta-analysis of randomized controlled trials. J Rehabil Med. 2017;49(4):304–15. [DOI] [PubMed] [Google Scholar]
- 14.••.Chen H, Li S, Ruan T, Liu L, Fang L. Is it necessary to perform prehabilitation exercise for patients undergoing total knee arthroplasty: meta-analysis of randomized controlled trials. The Physician and sportsmedicine. 2018;46(1):36–43.- This systematic review analyzed 16 studies (966 subjects) and reported that prehabilitation exercises can improve physical function, range of motion and length of hospital stay after total knee replacement.
- 15.•.Ma JX, Zhang LK, Kuang MJ, Zhao J, Wang Y, Lu B, et al. The effect of preoperative training on functional recovery in patients undergoing total knee arthroplasty: A systematic review and meta-analysis. . International journal of surgery (London, England). 2018;51:205–12.- This systematic review analyzed 9 individuals studies (777 subjects) and reported that prehabilitation exercises can reduce length of hospital stay after total knee replacement.
- 16.•.Sharma R, Ardebili MA, Abdulla IN. Does Rehabilitation before Total Knee Arthroplasty Benefit Postoperative Recovery? A Systematic Review. Indian journal of orthopaedics. 2019;53(1): 138–47.- This systematic review analyzed 5 individual studies (707 subjects) and reported that prehabilitation exercises can reduce length of hospital stay after total knee replacement.
- 17.Kwok IH, Paton B, Haddad FS. Does Pre-Operative Physiotherapy Improve Outcomes in Primary Total Knee Arthroplasty? - A Systematic Review. The Journal of arthroplasty. 2015;30 (9):1657–63. [DOI] [PubMed] [Google Scholar]
- 18.•.Vasta S, Papalia R, Torre G, Vorini F, Papalia G, Zampogna B, et al. The Influence of Preoperative Physical Activity on Postoperative Outcomes of Knee and Hip Arthroplasty Surgery in the Elderly: A Systematic Review. Journal of clinical medicine. 2020;9(4):969.- This systematic review analyzed 14 individual studies (740 subjects) and reported that prehabilitation exercises can reduce length of hospital stay after total joint replacement.
- 19.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum 1999. 42(8):1722–8 [DOI] [PubMed] [Google Scholar]
- 20.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86–A. [DOI] [PubMed] [Google Scholar]
- 21.Mizner RL, Petterson SC, Stevens JE, Axe MJ, Snyder-Mackler L. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. J Rheumatol. 2005;32(8):1533–9. [PubMed] [Google Scholar]
- 22.Whitehurst MA, Johnson BL, Parker CM, Brown LE, Ford AM. The benefits of a functional exercise circuit for older adults. . J Strength Cond Res. 2005. 19(3):647–51. [DOI] [PubMed] [Google Scholar]
- 23.Almeida GJ, Khoja SS, Piva SR. Dose-Response Relationship Between Neuromuscular Electrical Stimulation and Muscle Function in People With Rheumatoid Arthritis. Phys Ther 2019;99(9):1167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sillen MJ, Franssen FM, Gosker HR, Wouters EF, Spruit MA. Metabolic and structural changes in lower-limb skeletal muscle following neuromuscular electrical stimulation: a systematic review. . PLoS One. 2013;8(9):e69391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centner C, Wiegel P, Gollhofer A, Konig D. Effects of Blood Flow Restriction Training on Muscular Strength and Hypertrophy in Older Individuals: A Systematic Review and Meta-Analysis. Sports Med 2019;49(1):95–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franz A, Queitsch FP, Behringer M, Mayer C, Krauspe R, Zilkens C. Blood flow restriction training as a prehabilitation concept in total knee arthroplasty: A narrative review about current preoperative interventions and the potential impact of BFR. Medical hypotheses. 2018. 110:53–9. [DOI] [PubMed] [Google Scholar]
- 27.Takarada Y, Nakamura Y, Aruga S, Onda T, Miyazaki S, Ishii N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J Appl Physiol. 2000;88(1):61–5. [DOI] [PubMed] [Google Scholar]
- 28.Abe T, Yasuda T, Midorikawa T, Sato Y, Kearns CF, Inoue K, et al. Skeletal muscle size and circulating IGF-1 are increased after two weeks of twice daily “KAATSU” resistance training. Int J KAATSU Train Res. 2005;1(1):6–12. [Google Scholar]
- 29.Yasuda T, Abe T, Brechue WF, Iida H, Takano H, Meguro K, et al. Venous blood gas and metabolite response to low-intensity muscle contractions with external limb compression. Metabolism: clinical and experimental. 2010;59(10):1510–9. [DOI] [PubMed] [Google Scholar]


