Abstract
BACKGROUND:
The increase in the prescription of potentially inappropriate medication (PIM) in older adults with significant health consequences is a global concern. This study aimed to determine the prevalence of PIM prescription in older adults as identified by Beers criteria 2015 and 2019.
MATERIALS AND METHODS:
A cross-sectional study was carried out in older adults aged >65 years at a tertiary care postgraduate teaching hospital. All patients aged ≥65 years irrespective of their gender, admitted in the medical ward of the hospital with single/multiple comorbidities, and prescribed at least one daily medication, were included in the study. Data of patient history, patient case sheet, medication charts, laboratory reports, as well as radiological examinations test reports were retrieved from their files and were captured in a prevalidated data collection form. SPSS used for data analysis; multivariate logistic regression was used to determine the predictors of PIM prescribing and odds ratios (ORs) and 95% confidence intervals for ORs were computed.
RESULTS:
Study included 323 patients; 61.3% were male, 74% patients were 65–70 years of age, and 78% patients were illiterate. The overall prevalence of PIM uses according to the Beers criteria 2015 and 2019 was 60.1% and 61.9%, respectively. No association found between PIMs prescribes and diagnosis category. Male gender, age 76–80 years, and education 10–12th class were found to be significantly related to PIM prescription.
CONCLUSION:
This study reflects a critical view of noncompliance of Beers criteria for geriatric healthcare even in tertiary care hospitals in India. Creatinine clearance rate should be kept in view when prescribing medicines for elderly inpatients.
Keywords: Beers criteria, noncompliance, older adults, potentially inappropriate medication
Introduction
Potentially inappropriate medications (PIMs) are those medications whose adverse risk exceeds their health benefits when safer or equally effective alternatives are available.[1] PIM prescribing has been on the increase since the last 20 years.[2,3] It is associated with an increased incidence of adverse drug events (ADEs), increased hospital admissions, and increased health-related costs and economic burden for elderly patients, which, in turn, have led to a decrease in the quality of life of elderly patients.[4,5,6,7]
Older adults aged more than 65 years have a reduced performance capacity with advancing age. Moreover, physiologic and cognitive functions tend to change with the aging process.[8,9,10] Owing to their concomitant illness, most elderly patients are either on polypharmacy (5–9 medication per prescription) or on high-level polypharmacy (>10 medications per prescription), which increases the likelihood of a drug–drug interaction.[11,12] Prescribing for the elderly population is challenging because of altered pharmacokinetics (drug absorption, distribution, metabolism, and excretion), altered pharmacodynamics (physiological effects of the drug), and age-related changes in body composition and physiology.[13,14] Consequently, elderly patients are considered a special population and are mostly excluded from randomized controlled clinical trials. Therefore, prescribing decisions made with respect to elderly patients is without scientific evidence generated by rigorous randomized controlled trials.[15,16] Nevertheless, PIMs continue as first-line treatment on a daily basis especially in India and other developing countries, resulting in an overall increase in PIM prescribing in several countries.[17,18]
Beers et al. gave the first set of explicit criteria for the determination of inappropriate medication use by elderly patients.[19] The first published Beers guidelines had focused on elderly patients residing in nursing care homes. Beers criteria were regularly updated in 1994, 1997, and 2003, to cover the other significant areas of health care, but in 2012, the American Geriatric Society (AGS) assumed the responsibility of regularly updating and maintaining Beers criteria.[20,21,22,23] As a result, the AGS published the first set of guidelines in 2012 and regularly updated the same in 2015 and 2019.[24,25] The AGS guidelines addressed five major issues in elderly patients and gave advice on how to avoid PIM independent of diagnosis: consideration of diagnosis, use of caution, simultaneous prescription of drugs that could interact, and avoidance/or reduction of dosage according to individual kidney function. The quality of evidence and strength of recommendation have improved in the updated Beers criteria.
The Beers criteria have now become one of the most commonly used and reliable tools by clinicians, educators, researchers, health-care administrators, and regulators to identify PIM use in elderly patients. It has been observed that studies using the Beers Criteria 2003 and 2012 documented prevalence between 11% and 45% PIM in elderly patients,[2,3,26,27,28] whereas studies using the Beers criteria 2015 documented prevalence between 25% and 90% PIM in elderly patients.[29,30,31] Increased age, increased number of diagnosis, and increased length of hospital stay have been reported as important predictors of PIM prescribing. No study has been published to determine the prevalence of PIM using the Beers criteria 2019.
The objective of the present study was to evaluate the compliance level of updated Beers criteria 2019 in contrast to that of 2015 in a tertiary care hospital in Punjab. The present study was carried out to reflect geriatric care, and the authors were astonished with the frequency of prescribing PIMs for the elderly population.
Materials and Methods
A prospective observational study was conducted for a period of 6 months from July 2018 to January 2019 in the Department of Medicine, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, a constituent college of Baba Farid University of Health Sciences, Faridkot. Ethical approval was obtained from the Institutional Ethics Committee vide letter No. ERB/UCER/2018/9/3 dated 17/09/2018 and Informed written consent was taken from all the participants before data collection. The study was conducted according to the ethical guidelines for biomedical research on human participants by the Indian Council for Medical Research (ICMR).
All patients aged ≥65 years irrespective of their gender, admitted in the medical ward of the hospital with single/multiple comorbidities, and prescribed at least one daily medication, were included in the study.
Data of patient history, patient case sheet, medication charts, laboratory reports, as well as radiological examinations test reports were retrieved from their files and were captured in a prevalidated data collection form. Some risk factors (e.g., hypertension [HTN], elevated cholesterol, and cardiac arrhythmias) may cause cognitive function to decline. This in effect could negatively influence the physical functioning of older adults and their quality of life. In older populations, delirium and dementia are two of the most common causes of cognitive impairment. Psychiatrists used Delirium Rating Scale-revised version-98 to find out delirium in older adults.[32] The Mini–Mental State Examination that psychiatrists use extensively to measure cognitive impairment and to screen for dementia was applied.[33] The PIM was identified according to the AGS Beers criteria 2015 and Beers criteria 2019 as they all apply to the general population aged over 65 years regardless of the level of frailty or place of residence. According to Beers criteria, PIMs have been classified into four, which notably include the PIMs independent of diagnosis, dependent on diagnosis, drug–drug interactions, as well as consideration of the levels of kidney function test.
Statistical analysis was carried out by using CorIP. IBM Statistical Package for Social Science Statistics for Windows, Ver. 24.0. Armonk, NY, USA: IBM Corp.; 2016.[34] Categorical and continuous variables such as age, creatinine clearance (CrCl), number of medications during a hospital stay, number of diagnosis, and length of hospital stay were presented as numbers with percentages or median with interquartile range (IQR). Predictors of PIM prescribing such as gender, number of medications, CrCl, and age of the patient were assessed using the multivariate logistic regression analysis. The odds ratio (OR) with 95% confidence interval (CI) was used to determine the predictors for PIM prescribing. P < 0.05 was considered statistically significant.
Results
A total of 323 patients were included in the study in accordance with the inclusion criteria. In the present study, the prescription of PIM for elderly inpatients was determined by using two explicit criteria, such as AGS Beers criteria 2015 and 2019. The sociodemographic and clinical characteristics of the elderly inpatients are described in Table 1. The overall prevalence of PIM use has been calculated in a comparative manner using Beers criteria 2015 and 2019. The overall prevalence of PIM use, as identified in the present study, is shown in Table 2. Moreover, patients were grouped according to the total number of PIM prescribed as per Beers criteria 2015 and 2019, as described in Table 3.
Table 1.
Sociodemographic and clinical characteristics of the elderly inpatients at Guru Gobind Singh Medical College Hospital, Faridkot, Punjab, India 2015 and 2019
| Characteristics of patients | Number of patients (%) | Number of patients with PIM use | |
|---|---|---|---|
| As per 2015 Beers criteria | As per 2019 Beers criteria | ||
| Sex | |||
| Male | 198 (61.3) | 110 | 113 |
| Female | 125 (38.7) | 84 | 87 |
| Age (years) | |||
| 65-70 | 239 (74.0) | 143 | 148 |
| 71-75 | 38 (11.8) | 23 | 23 |
| 76-80 | 26 (8.0) | 13 | 13 |
| ≥81 | 20 (6.2) | 16 | 16 |
| Educational qualification | |||
| Illiterate | 252 (78.0) | 147 | 151 |
| <6th | 18 (5.6) | 12 | 13 |
| 6th-10th | 16 (5.0) | 9 | 9 |
| 11th-12th | 28 (8.7) | 23 | 23 |
| ≥12th | 9 (2.8) | 3 | 4 |
| Number of diagnosis in patients | |||
| 1 | 42 (13.0) | 22 | 23 |
| 2 | 79 (24.5) | 42 | 42 |
| ≥3 | 202 (62.5) | 130 | 135 |
| Length of hospital stay in days | |||
| 1-4 | 39 (12.1) | 16 | 16 |
| 5-9 | 256 (79.3) | 163 | 167 |
| 10-13 | 20 (6.2) | 9 | 11 |
| ≥14 | 8 (2.5) | 6 | 6 |
| Number of medications during a hospital stay | |||
| 1-4 | 36 (11.1) | 12 | 13 |
| 5-9 | 193 (59.7) | 117 | 122 |
| ≥10 | 94 (29.1) | 65 | 65 |
| CrCl (mL/min) | |||
| 0-30 | 120 (37.2) | 86 | 86 |
| 31-60 | 81 (25.1) | 47 | 51 |
| 61-90 | 93 (28.8) | 49 | 50 |
| 91-120 | 24 (7.4) | 11 | 11 |
| ≥120 | 5 (1.5) | 1 | 2 |
PIM=Potentially inappropriate medication, CrCl=Creatinine clearance
Table 2.
Potentially inappropriate medication use among elderly inpatients at Guru Gobind Singh Medical College Hospital, Faridkot, according to 2015 and 2019 Beers criteria (n=323)
| PIM | Recommendation | Number of Patients with PIM use | |
|---|---|---|---|
| As per Beers criteria 2015 N (%) | As per Beers criteria 2019 N (%) | ||
| Independent of diagnosis | |||
| Rabeprazole | Avoid scheduled use for >8 weeks unless for high-risk patients (e.g., oral corticosteroids or chronic NSAID use), erosive esophagitis, Barrett’s esophagitis, pathological hypersecretory condition, or demonstrated need for maintenance treatment | 18 (6.5) | 18 (6.2) |
| Pantoprazole | 54 (19.5) | 54 (18.8) | |
| Omeprazole | 45 (16.3) | 45 (15.6) | |
| Chlorpheniramine | Avoid | 1 (0.3) | 1 (0.3) |
| Zolpidem | Avoid | 4 (1.4) | 4 (1.3) |
| Prazosin | Avoid use as an antihypertensive | 5 (1.8) | 5 (1.7) |
| Ketorolac | Avoid | 3 (1.0) | 3 (1.0) |
| Naproxen | Avoid chronic use | 2 (0.7) | 2 (0.6) |
| Diclofenac | Avoid chronic use | 2 (0.7) | 2 (0.6) |
| Quetiapine | Avoid | 4 (1.4) | 4 (1.3) |
| Nortriptyline | Avoid | 3 (1.0) | 3 (1.0) |
| Olanzapine | Avoid | 2 (0.7) | 2 (0.6) |
| Clonazepam | Avoid | 26 (9.4) | 26 (9.0) |
| Clonidine | Avoid clonidine as first-line antihypertensive | 2 (0.7) | 2 (0.6) |
| Risperidone | Avoid except for schizophrenia, bipolar disorder | 1 (0.3) | 1 (0.3) |
| Trihexyphenidyl | Avoid | 4 (1.4) | 4 (1.3) |
| Insulin Sliding Scale | Avoid | 46 (16.6) | 46 (16.0) |
| Ergot mesyloids | Avoid | 1 (0.3) | 1 (0.3) |
| Chlordiazepoxide | Avoid | 4 (1.4) | 4 (1.3) |
| Glimepiride | Avoid | - | 10 (3.4) |
| Lorazepam | Avoid | 1 (0.3) | 1 (0.3) |
| Dependent of diagnosis | |||
| Delirium | |||
| Ranitidine | Avoid | 1 (0.3) | 1 (0.3) |
| Hydrocortisone | Avoid | 1 (0.3) | 1 (0.3) |
| Clonazepam | Avoid | 1 (0.3) | 1 (0.3) |
| Risperidone | Avoid except for schizophrenia, bipolar disorder | 1 (0.3) | 1 (0.3) |
| Dementia | |||
| Olanzapine | Avoid | 1 (0.3) | 1 (0.3) |
| Drug-drug interaction | |||
| Prazosin + furosemide=increased risk of urinary incontinence | Avoid in older women, unless conditions warrant both drugs | 2 (0.7) | 2 (0.6) |
| Hydrocortisone + ketorolac=increased risk of peptic ulcer or GI bleeding | Avoid; if not possible, provide gastrointestinal protection | 1 (0.3) | 1 (0.3) |
| As per CrCl of the patient (mL/min) | |||
| Gabapentin <60 | Reduced dose | 3 (1.0) | 3 (1.0) |
| Enoxaparin <30 | Reduced dose | 10 (3.6) | 10 (3.4) |
| Ranitidine <50 | Reduced dose | 13 (4.7) | 13 (4.5) |
| Tramadol <30 | Immediate release: reduce the dose Extended-release: avoid | 2 (0.7) | 2 (0.6) |
| Dabigatran <30 | Avoid; dose adjustment advised when CrCl >30 mL/min in the presence of drug-drug interaction | 2 (0.7) | 2 (0.6) |
| Spironolactone <30 | Avoid | 6 (2.1) | 6 (2.0) |
| Pregabalin <60 | Reduced dose | 5 (1.8) | 5 (1.7) |
| Total PIMs | 277 PIMs in 194 prescriptions | 287 PIMs in 200 prescriptions | |
PIM=Potentially inappropriate medication, CrCl=Creatinine clearance, GI=Gastrointestinal, NSAID=Nonsteroidal anti-inflammatory drug
Table 3.
Distribution of elderly inpatients at Guru Gobind Singh Medical College Hospital, Faridkot, according to the total number of potentially inappropriate medication prescribed
| Total number of PIMs in elderly inpatients | According to Beers criteria 2015 N (%) | According to Beers criteria 2019 N (%) |
|---|---|---|
| 0 | 129 (39.9) | 123 (38.1) |
| 1 | 129 (39.7) | 132 (40.7) |
| 2 | 48 (15.0) | 50 (15.5) |
| 3 | 13 (4.2) | 14 (4.5) |
| 4 | 2 (0.6) | 2 (0.6) |
| 5 | 1 (0.3) | 1 (0.3) |
| 6 | 1 (0.3) | 1 (0.3) |
PIM=Potentially inappropriate medication
The demographic details show that out of the 323 patients, 61.3% of the patients were male and 38.7% were female. Of the 323 patients, 74% (n = 239) were in the 65–70 years' age group; 11.8% (n = 38) belonged to the 71–75 years' age group; 8% (n = 26) were in the 76–80 years' age group; and a small proportion of 6.2% (n = 20) patients were aged over 80 years, as shown in Table 1, with an overall median (IQR) age of 65 years (range, 65–97 years). The demographic details also show that a significant 78% (252 patients out of 323) of the total population was illiterate.
It was observed that on an average, each patient had three diagnoses with a range of 1–9. Most of the patients (62.5%, n = 202) had ≥3 diagnosis, and 24.5% (n = 79) and 13% (n = 42) had two diagnoses simultaneously and single diagnosis, respectively. In our study, it was observed that a higher proportion of the elderly populations had multiple comorbidities and were, therefore, prescribed multiple drugs. Out of the 323 elderly inpatients, the majority suffered from chronic diseases such as diabetes mellitus (36.2%), cerebrovascular accident (10.5%), chronic kidney disease (18.2%), cardiovascular disease (31.5%), HTN (28.1%), and others. A separate PIM rate has been calculated and shown along with the prevalence of various chronic diseases present in patients, as shown in Figure 1.
Figure 1.
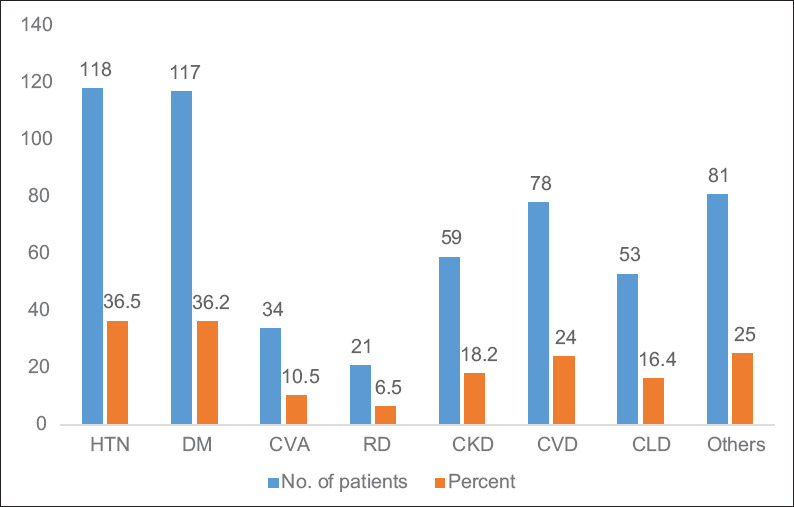
Representation of the prevalence of chronic diseases in elderly inpatients along with the PIM rate. *DM = Diabetes mellitus, CVA = Cerebrovascular accident, RD = Respiratory disorder, CKD = Chronic kidney disease, CVD = Cardiovascular disease, CLD = Chronic liver disease, HTN = Hypertension, PIM = Potentially inappropriate medication
Our study found that a significant proportion of the elderly patients were either on polypharmacy (i.e., 5–9 medicines on the prescription of the patient) or high-level polypharmacy (i.e., more than 10 medicines on the prescription of a patient). It was astonishing that the ratio of patients on polypharmacy and high-level polypharmacy was very high at 63% and 69%, respectively, for PIMs.
It was found that the median length of hospital stay was 6 days (range, 3–15). It was observed that with the increase in the length of hospital stay came an increase in the number of PIMs on the prescription. The number of patients with PIM as per Beers criteria 2015 and 2019 was the highest and very high in 63.6% and 65.2% of the patients who had a stay of 5–9 days, respectively.
The normal CrCl range was usually more than 120, but in this study, it was observed that the median of each patient had CrCl of 44 (range, 4–182) mL/min. Moreover, 37.2% of the patients (n = 120) had CrCl <30 mL/min followed by 25.1% (n = 81) with between 31 and 60 ml/min; 28.8% (n = 93) had CrCl between 61 and 90 mL/min; and a very low proportion of elderly patients (8.9%, n = 29) had CrCl above 90 mL/min. The Beers criteria 2015 and 2019 state that the CrCl levels should be taken into consideration when prescribing medications for the geriatric population. However, the present study shows that >71% of the population with a lower range of creatinine had been prescribed potentially inappropriate medicines, a reflection of little concern for geriatric health.
According to our study, male patients in the age group of 76–80 years educated up to the 10th–12th class were the most likely candidates for PIM. In addition, it is pertinent to mention that on the basis of multivariate regression and as per Beers criteria 2015, male sex (OR: 0.61, 95% CI: 0.38–0.97, P = 0.03), age of 76–80 years (OR: 0.25, 95% CI: 0.06–1.95, P = 0.04), and educational qualification of 11th–12th class (OR: 9.20, 95% CI: 1.69–49.85, P = 0.01) were found to be important predictors for PIM prescription [Table 4]. Similarly, according to Beers criteria 2019, male sex (OR: 0.58, 95% CI: 0.36–0.93, P = 0.02), age of 76–80 years (OR: 0.25, 95% CI: 0.06–1.95, P = 0.04), and educational qualification of 11th–12th class (OR: 5.75, 95% CI: 1.12–29.41, P = 0.03) [Table 4] were found to be the important predictors for PIM prescription.
Table 4.
Correlates of potentially inappropriate medication among elderly hospitalized patients at Guru Gobind Singh Medical College Hospital, Faridkot, Punjab, India
| Parameter | Total number of patients (n=323) N (%) | Beers criteria 2015 PIM OR (95% Cl) | P-value* | Beers criteria 2019 PIM OR (95% Cl) | P-value* |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 198 (61.3) | 0.61 (0.38-0.97) | 0.03 | 0.58 (0.36-0.93) | 0.02 |
| Female | 125 (38.7) | 1 (reference) | 1 (reference) | ||
| Age of the patient (years) | |||||
| 65-70 | 239 (74.0) | 0.37 (0.12-1.14) | 0.08 | 0.407 (0.13-1.25) | 0.11 |
| 71-75 | 38 (11.8) | 0.34 (0.09-1.22) | 0.10 | 0.38 (0.10-1.37) | 0.14 |
| 76-80 | 26 (8.0) | 0.25 (0.06-0.95) | 0.04 | 0.25 (0.06-0.95) | 0.04 |
| ≥81 | 20 (6.2) | 1 (reference) | 1 (reference) | ||
| Education qualification | |||||
| Illiterate | 252 (78.0) | 2.80 (0.685-11.45) | 0.32 | 1.86 (0.49-7.12) | 0.36 |
| <6th class | 18 (5.6) | 4.0 (0.73-21.83) | 0.10 | 3.25 (0.61-17.28) | 0.16 |
| 6th-10th class | 16 (5.0) | 2.57 (0.46-14.10) | 0.27 | 1.60 (0.31-8.32) | 0.57 |
| 11th-12th class | 28 (8.7) | 9.20 (1.69-49.85) | 0.01 | 5.75 (1.12-29.41) | 0.03 |
| More than 12th class | 9 (2.8) | 1 (reference) | 1 (reference) |
P<0.05 indicates statistically significant difference and P≥0.05 indicates statistically nonsignificant difference. AGS=American Geriatric Society, PIM=Potentially inappropriate medication, OR=Odds ratio, CI=Confidence interval
Discussion
The current evidence has shown the overall prevalence of PIM as 60.1% (194/323) and 61.9% (200/323) as identified by 2015 and 2019 Beers criteria, respectively.
To the best of our knowledge, this is the first study to report the PIM prescription in India using Beers criteria 2019. Besides, it is the first report that compares Beers criteria 2015 and 2019. It has also been observed that the rate of PIM prescription continues to increase as higher numbers of PIMs have been observed in recent years. A total of 277 PIMs in 194 prescriptions and 287 PIMs in 200 prescriptions were found for patients as per Beers criteria 2015 and 2019, respectively. The present study shows that the overall prevalence of PIM use as per 2019 Beers criteria was very high but only slightly more (i.e., 61.9%) than was observed with the 2015 Beers Criteria (i.e., 60%). The numbers reported in this study are remarkably higher than those reported in other studies.
Beers criteria 2015 and 2019 describe the list of medications which act as PIM and those to be avoided for elderly patients independent of diagnosis. However, according to the present study, a significant proportion of PIMs are prescribed independent of diagnosis. As per 2015 and 2019 criteria, 82.3% and 83% of PIM prescribed were independent of diagnosis. Hence, the present study reflects the failure of our authorities to give proper geriatric health care.
The most commonly prescribed PIMs were proton pump inhibitor (PPI), short acting insulin according to sliding scale, clonazepam, glimepiride, zolpidem, enoxaparin and spironolactone use in patients having CrCl <30ml/min, and ranitidine use in patients with CrCl <50 ml/min. PPIs such as pantoprazole, rabeprazole, and omeprazole approved for reduction of gastric acid production and the most commonly prescribed drugs in a hospital setting, are to be avoided as per 2015 as well as 2019 criteria. The primary reason for this is that the use of PPI is associated with the risk of Clostridium difficile infections and increased probability of bone loss as well as fractures.[35,36,37] The present study shows that a total of 117 PIMs out of 228 (i.e., 51.3%) were reported for PPI as per Beers criteria 2015 as well as 2019.
Apart from PPI, the study showed that the PIMs associated with Insulin Sliding Scale were quite high. Although the Insulin Sliding Scale is mentioned in both 2015 and 2019 criteria, it is more explicit in Beers criteria 2019. The Insulin Sliding Scale (insulin regimens containing only short- or rapid-acting insulin dosed according to the current blood glucose levels without concurrent use of basal or long-acting insulin) is an agent approved for diabetic patients. However, elderly patients may have a higher risk of hypoglycemia without an improvement in hyperglycemia management.[38,39] However, the present study indicates that 46 PIMs out of 228 (i.e., 19.7%) were reported for Insulin Sliding Scale as per Beers criteria 2015 and 2019. This shows neglect because instead of prescribing reduced short-acting insulin, Insulin Sliding Scales are routinely prescribed.
Another major PIM is associated with clonazepam, which is to be avoided for elderly patients independent of diagnosis. The drug is not only prescribed for the treatment of seizures, panic disorder, etc., but also acts as a long-acting benzodiazepine. The use of this drug is restricted to avoid increased sensitivity of geriatric patients to benzodiazepine and lowered metabolism of long-acting agents, resulting in the increased risk of cognitive impairment, delirium, falls, fractures, and motor vehicle crashes in older adults.[40,41] This drug should be avoided specifically by elderly patients with delirium.[42] Unfortunately, included in the PIM category were as many as 26 PIMs out of 228 PIMs (i.e., 11.4%) in both 2015 and 2019 criteria.
The PIMs associated with glimepiride were also observed in diabetic patients. Glimepiride, a commonly used agent for diabetic patients, has recently been included in the Beers criteria 2019 on the list of those in the category of independent diagnosis. The primary reason for its inclusion is that it was found to be associated with a higher risk of severe prolonged hypoglycemia in older adults.[43] Although it should not be prescribed for the elderly population, according to Beers criteria 2019, the study revealed 10 out of 228 PIMs for this drug.
The dosage of various drugs such as enoxaparin, ranitidine, and spironolactone should be adjusted or reduced for elderly patients after observing the CrCl data according to instructions and indications of Beers criteria. If CrCl level is 30 mL/min in a patient, there may be an increased risk of bleeding, possibly leading to a disturbed mental status. Despite definite indications of Beers criteria on CrCl, 41 PIMs were reported in the category. It has been observed that patients were prescribed a standard dose of enoxaparin, ranitidine, and spironolactone, despite a decrease in their CrCl.[44,45,46]
PIM prescribing, particularly for elderly patients, is not only of great concern, but it is also a significant public health issue because of its direct correlation to mortality, morbidity, and waste of health resources as a result of ADE, particularly in very elderly patients. The Beers criteria present tools that explain the use/avoidance of various drugs by elderly patients based on their health status. They also serve as a instrument for identifying medications whose potential risks outweigh potential benefits in elderly patients, particularly when compared to pharmacological and nonpharmacological alternatives.[2] To the best of our knowledge, this is the first study to report PIM prescription in India and around the world using Beers criteria 2019. In addition, it is the first report that compares all the Beers criteria 2015 and 2019 after the official patronage by the AGS in 2012.
The study was conducted in a tertiary care teaching government hospital of Punjab, therefore the results may not be applicable to other settings such as private hospitals. The findings of the study are based on the elderly patients hospitalized in a medical ward, therefore extrapolation to outpatients might not be appropriate.
Conclusion
The study also reflects a failure in the application of Beers criteria for geriatric health care even in tertiary care hospitals in India. There is a need to create awareness in physicians regarding the Beers criteria so that they can provide appropriate justifiable health care to the ailing population. The regulatory authorities should also take measures to make the implementation of Beers criteria mandatory. The study also indicates that CrCl rate should be definitely taken into account when prescribing medicines for elderly patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are thankful to Baba Farid University of Health Science, Faridkot, Punjab, India, for providing the authors with all the necessary facilities and timely guidance.
References
- 1.Jones JK. Assessing potential risk of drugs: The elusive target. Ann Intern Med. 1992;117:691–2. doi: 10.7326/0003-4819-117-8-691. [DOI] [PubMed] [Google Scholar]
- 2.Undela K, Bansal D, D'Cruz S, Sachdev A, Tiwari P. Prevalence and determinants of use of potentially inappropriate medications in elderly inpatients: A prospective study in a tertiary healthcare setting. Geriatr Gerontol Int. 2014;14:251–8. doi: 10.1111/ggi.12081. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt AN, Paul SS, Krishnamoorthy S, Baby BT, Mathew A, Nair BR. Potentially inappropriate medications prescribed for older persons: A study from two teaching hospitals in Southern India. J Family Community Med. 2019;26:187–92. doi: 10.4103/jfcm.JFCM_81_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cahir C, Fahey T, Teeling M, Teljeur C, Feely J, Bennett K. Potentially inappropriate prescribing and cost outcomes for older people: A national population study. Br J Clin Pharmacol. 2010;69:543–52. doi: 10.1111/j.1365-2125.2010.03628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fick DM, Mion LC, Beers MH, L Waller J. Health outcomes associated with potentially inappropriate medication use in older adults. Res Nurs Health. 2008;31:42–51. doi: 10.1002/nur.20232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyttinen V, Jyrkkä J, Valtonen H. A systematic review of the impact of potentially inappropriate medication on health care utilization and costs among older adults. Med Care. 2016;54:950–64. doi: 10.1097/MLR.0000000000000587. [DOI] [PubMed] [Google Scholar]
- 7.Fu AZ, Jiang JZ, Reeves JH, Fincham JE, Liu GG, Perri M., 3rd Potentially inappropriate medication use and healthcare expenditures in the US community-dwelling elderly. Med Care. 2007;45:472–6. doi: 10.1097/01.mlr.0000254571.05722.34. [DOI] [PubMed] [Google Scholar]
- 8.Rayner HC, Thomas ME, Milford DV. Understanding Kidney Diseases. Cham: Springer; 2020. Kidney anatomy and physiology: The basis of clinical nephrology. [Google Scholar]
- 9.Rowe JW, Andres R, Tobin JD, Norris AH, Shock NW. The effect of age on creatinine clearance in men: A cross-sectional and longitudinal study. J Gerontol. 1976;31:155–63. doi: 10.1093/geronj/31.2.155. [DOI] [PubMed] [Google Scholar]
- 10.Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29:496–507. doi: 10.1172/JCI102286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: A repeated cross-sectional study. BMJ Open. 2015;5:e008656. doi: 10.1136/bmjopen-2015-008656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: Results of the Kuopio 75+study: A cross-sectional analysis. Drugs Aging. 2009;26:493–503. doi: 10.2165/00002512-200926060-00006. [DOI] [PubMed] [Google Scholar]
- 13.Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br J Clin Pharmacol. 2004;57:6–14. doi: 10.1046/j.1365-2125.2003.02007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Boer A, Ter Horst GJ, Lorist MM. Physiological and psychosocial age-related changes associated with reduced food intake in older persons. Ageing Res Rev. 2013;12:316–28. doi: 10.1016/j.arr.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Ruscin JM. Drug Therapy for the Elderly. Vienna: Springer; Inappropriate prescribing in the hospitalized elderly patient; pp. 331–39. [Google Scholar]
- 16.O’Connor MN, Gallagher P, O’Mahony D. Inappropriate prescribing: Criteria, detection and prevention. Drugs Aging. 2012;29:437–52. doi: 10.2165/11632610-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 17.Gallagher P, O’Mahony D. Inappropriate prescribing in older people. Rev Clin Gerontol. 2008;18:65–76. [Google Scholar]
- 18.Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;32:113–21. doi: 10.1111/j.1365-2710.2007.00793.x. [DOI] [PubMed] [Google Scholar]
- 19.Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151:1825–32. [PubMed] [Google Scholar]
- 20.Stuck AE, Beers MH, Steiner A, Aronow HU, Rubenstein LZ, Beck JC. Inappropriate medication use in community-residing older persons. Arch Intern Med. 1994;154:2195–200. [PubMed] [Google Scholar]
- 21.Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997;157:1531–6. [PubMed] [Google Scholar]
- 22.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: Results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 23.Campanelli CM. American Geriatrics Society updated beers criteria for potentially inappropriate medication use in older adults: The American Geriatrics Society 2012 beers criteria update expert panel. J Am Geriatr Soc. 2012;60:616. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fick DM, Semla TP, Beizer J, Brandt N, Dombrowski R, DuBeau CE, et al. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–46. doi: 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 25.Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, Dombrowski R, et al. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–94. doi: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 26.Vishwas HN, Harugeri A, Parthasarathi G, Ramesh M. Potentially inappropriate medication use in Indian elderly: Comparison of beers' criteria and screening tool of older persons' potentially inappropriate prescriptions. Geriatr Gerontol Int. 2012;12:506–14. doi: 10.1111/j.1447-0594.2011.00806.x. [DOI] [PubMed] [Google Scholar]
- 27.Momin TG, Pandya RN, Rana DA, Patel VJ. Use of potentially inappropriate medications in hospitalized elderly at a teaching hospital: A comparison between Beers 2003 and 2012 criteria. Indian J Pharmacol. 2013;45:603–7. doi: 10.4103/0253-7613.121372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeenny R, Wakim S, Kuyumjian YM. Potentially inappropriate medications use in community-based aged patients: A cross-sectional study using 2012 Beers criteria. Clin Interv Aging. 2017;12:65–73. doi: 10.2147/CIA.S87564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Zhou S, Pan K, Li X, Zhao X, Zhou Y, et al. Potentially inappropriate medications in hospitalized older patients: A cross-sectional study using the Beers 2015 criteria versus the 2012 criteria. Clin Interv Aging. 2017;12:1697–703. doi: 10.2147/CIA.S146009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chandrappa S, Divya R, Rajarathna K. Assessing prescriptions for potentially inappropriate medications using Beer's criteria in elderly in-patients at a tertiary care hospital. Natl J Physiol Pharm Pharmacol. 2019;9:145–9. [Google Scholar]
- 31.Sheth AR, Dave RB, Rana D, Sheth D. Comparison of the Extent and Prevalence of Prescription of Potentially Inappropriate Medications Prescribed to Geriatric Age Group Residing in Old-Age Homes versus those Receiving Care from Tertiary Care Hospital Using Beers Criteria. 2019 doi: 10.4103/picr.PICR_144_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trzepacz PT, Mittal D, Torres R, Kanary K, Norton J, Jimerson N. Validation of the Delirium Rating Scale-revised-98: Comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13:229–42. doi: 10.1176/jnp.13.2.229. [DOI] [PubMed] [Google Scholar]
- 33.Pangman VC, Sloan J, Guse L. An examination of psychometric properties of the mini-mental status examination and the standardized mini-mental status examination: Implications for clinical practice. Appl Nurs Res. 2000;13:209–13. doi: 10.1053/apnr.2000.9231. [DOI] [PubMed] [Google Scholar]
- 34.Cor IP. IBM SPSS Statistics for Windows, Ver 240. Armonk, NY, USA: IBM Corp; 2016. [Google Scholar]
- 35.Freedberg DE, Salmasian H, Friedman C, Abrams JA. Proton pump inhibitors and risk for recurrent clostridium difficile infection among inpatients. Am J Gastroenterol. 2013;108:1794–801. doi: 10.1038/ajg.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dial S, Alrasadi K, Manoukian C, Huang A, Menzies D. Risk of clostridium difficile diarrhoea among hospital inpatients prescribed proton pump inhibitors: Cohort and case–control studies. CMAJ. 2004;171:33–8. doi: 10.1503/cmaj.1040876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang YX, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA. 2006;296:2947–53. doi: 10.1001/jama.296.24.2947. [DOI] [PubMed] [Google Scholar]
- 38.Umpierrez GE, Palacio A, Smiley D. Sliding scale insulin use: Myth or insanity? Am J Med. 2007;120:563–7. doi: 10.1016/j.amjmed.2006.05.070. [DOI] [PubMed] [Google Scholar]
- 39.Queale WS, Seidler AJ, Brancati FL. Glycemic control and sliding scale insulin use in medical in patients with diabetes mellitus. Arch Intern Med. 1997;157:545–52. [PubMed] [Google Scholar]
- 40.Madhusoodanan S, Bogunovic OJ. Safety of benzodiazepines in the geriatric population. Expert Opin Drug Saf. 2004;3:485–93. doi: 10.1517/14740338.3.5.485. [DOI] [PubMed] [Google Scholar]
- 41.Owen RT, Tyrer P. Benzodiazepine dependence. A review of the evidence. Drugs. 1983;25:385–98. doi: 10.2165/00003495-198325040-00003. [DOI] [PubMed] [Google Scholar]
- 42.Tune LE, Bylsma FW. Benzodiazepine-induced and anticholinergic-induced delirium in the elderly. Int Psychogeriatr. 1991;3:397–408. doi: 10.1017/s1041610291000832. [DOI] [PubMed] [Google Scholar]
- 43.Dills DG, Schneider J Glimepiride/glyburide research group. Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Horm Metab Res. 1996;28:426–9. doi: 10.1055/s-2007-979831. [DOI] [PubMed] [Google Scholar]
- 44.Hoffmann P, Keller F. Increased major bleeding risk in patients with kidney dysfunction receiving enoxaparin: A meta-analysis. Eur J Clin Pharmacol. 2012;68:757–65. doi: 10.1007/s00228-011-1149-6. [DOI] [PubMed] [Google Scholar]
- 45.Tawadrous D, Dixon S, Shariff SZ, Fleet J, Gandhi S, Jain AK, et al. Altered mental status in older adults with histamine2-receptor antagonists: A population-based study. Eur J Intern Med. 2014;25:701–9. doi: 10.1016/j.ejim.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 46.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]


