Abstract
Background:
Micronutrient deficiencies such as iron, Vitamin A, and iodine are important public health problems in India.
Objective:
The objective of the study was to assess subclinical Vitamin A deficiency (VAD) and anemia among women and preschool children from Northeast India. Methodology: A community-based cross-sectional study was carried out by adopting systematic sampling in Phek district of Nagaland. Data were collected from women on sociodemographic particulars, and finger prick blood was collected for hemoglobin and free-flowing drop for Vitamin A estimation on Whatman no. 1 filter paper.
Results:
The overall prevalence of anemia was 27%, 40%, 44%, and 52% among preschool children, nonpregnant nonlactating women, lactating mothers, and pregnant women, respectively, whereas VAD was 37% among preschool children and 24%–32% among adult women. The prevalence of VAD was observed high among those living in kutcha house, illiteracy of head of households, big family size, and low per capita income.
Conclusions:
Anemia and VAD are important public health problems among tribal population in spite of the rich biodiversity.
Keywords: Anemia, preschool children, Vitamin A deficiency, women of reproductive age
INTRODUCTION
Vitamin A deficiency (VAD) and anemia are the important micronutrient deficiency of public health significance in India. Globally, anemia affects 1.62 billion people, which corresponds to 24.8% of the population. The World Health Organization (WHO) estimated that 43% of children aged 6–59 months, 29% of nonpregnant women, and 38% of pregnant women were anemic in 2011, of which 54% of children, 42% of nonpregnant women, and 49% of pregnant women were from Southeast Asian countries. Of these, 59% of children, 48% of nonpregnant women, and 54% of pregnant women were from India.[1] It is estimated that about 20%–40% of maternal deaths in India are attributed to anemia, and one in every two Indian women (56%) suffers from some form of anemia.[2]
The main causes for anemia are nutritional deficiencies and infections. Among the nutritional factors, the most common is iron deficiency, aggravated by poor nutritional status, associated with deficiencies in folic acid, Vitamin A, or Vitamin B12. Malaria is one of the major causes of anemia, affecting 300–500 million people, and in endemic areas, it may be the primary cause of half of all severe anemias.[2]
Anemia resulting from iron deficiency adversely affects cognitive and motor development, causes fatigue and low productivity,[1,3,4] and when it occurs in pregnancy, it may be associated with low birth weight and increased risk of maternal and perinatal mortality.[5,6]
VAD is also an important public health problem in India and the leading cause of preventable blindness in young children in low-income countries. In addition, it can impair growth, weaken the immune system and thus increase susceptibility to infection, and thus increase morbidity and mortality.[7] As per the WHO, globally, VAD was affecting about a third of children aged 6–59 months, with 50% in Southeast Asia with more than 90 million preschool children with subclinical VAD and about 44% in Africa.[8]
Northeast (NE) India is inhabited by various indigenous groups whose culture and dietary patterns are distinct and closely associated with nature and the environment. Phek district in Nagaland is inhabited by Chakhesang and Pochury Tribes.[9] The present study was carried out in Phek district of Nagaland to assess nutritional status, Vitamin A, and anemia among the preschool children and women of reproductive age groups.
METHODOLOGY
A community-based, cross-sectional study was carried out in Phek district of Nagaland by adopting systematic sampling procedure. A total of twenty villages and thirty households (HHs) from each village were selected. The data were collected from mothers who consented for blood collections for Vitamin A and hemoglobin estimation.
Data were collected on predesigned and pretested pro forma by trained field investigators recruited locally, on HH socioeconomic and demographic particulars. A 1 day 24 h recall method of dietary survey[10] and food frequency was carried out in every sixth HH covered for nutritional assessment. Nutrient intakes were computed using “Nutritive value of Indian foods.”[11] Foods and nutrients were compared against recommended dietary intakes (RDI) and recommended dietary allowances (RDA) for Indians.[12,13]
A volume of 20 μL of blood was collected by finger prick using hemoglobin pipette on Whatman no. 1 filter paper, and dry blood spot of blood samples was prepared, dried, and sent to the National Institute of Nutrition (NIN) for hemoglobin estimation. Hemoglobin estimation was done using indirect cyanmethemoglobin method.[14]
A free-flowing drop of blood was collected on filter paper for Vitamin A estimation, which was done using high-performance liquid chromatography method.[15]
The data were scrutinized before entering into the computer. Descriptive and appropriate statistical analyses were carried out using IBM SPSS Statistics for Windows, Version 19.0. (Armonk, New York: IBM Corp). Associations were carried out between anemia and VAD as dependent variable and socioeconomic and demographic particulars as independent variable using Chi-square test. Logistic regression was done with VAD as dependent variable and sociodemographic variable as independent variable.
The criterion recommended by the WHO (2001)[16] was used to diagnose anemia. A cutoff value of <1 g/dl for 1–5 years' old children and pregnant women and <12 g/dl for nonpregnant nonlactating (NPNL) women was considered anemic.
For VAD, cutoff value <20 μg/dl was considered.
Ethical clearance was obtained from the institutional ethical review board, and written informed consent was obtained from the mothers who participated in the study.
RESULTS
A total of 557 HHs were covered in Phek district of Nagaland, out of which 227 children of 1–5 years and 526 women of 15–49 years responded for blood drawings for hemoglobin and Vitamin A estimation.
Sociodemographic particulars of the study participants
Nearly 50% of participants were living in kutcha, and only 13% were having pucca houses. Majority (97.5%) of the HHs were nuclear families, with an average family size of 5.2 ± 1.97. Majority (89.5%) of the adult men (head of HH) and 80% of adult women were literate. More than half (56%) of the men were engaged in cultivation, 29% were engaged in service, whereas 61% of women were housewife. The average per capita income (PCI) of HH was Rs. 1847. Nearly, all (97%) the HHs had sanitary latrine.
Haemoglobin and Vitamin A levels
Table 1 shows the average levels of Haemoglobin in study subjects. Figure 1 shows prevalence of anaemia and VAD among study subjects. No difference was observed in the prevalence of anaemia and VAD with nutritional status..
Table 1.
Mean±standard deviation of hemoglobin and Vitamin A value in different physiological groups
| Physiological groups | n | Hemoglobin (g/dl), mean±SD | n | Vitamin A (µg/dl), mean±SD |
|---|---|---|---|---|
| Preschool children | 185 | 11.33±0.93 | 227 | 22.4±6.89 |
| Boys | 97 | 11.15±1.00 | 123 | 23.2±6.66 |
| Girls | 88 | 11.43±0.83 | 104 | 21.5±7.10 |
| NPNL women | 249 | 12.01±1.25 | 274 | 25.71±8.11 |
| Lactating mothers | 151 | 11.93±1.29 | 198 | 23.68±7.68 |
| Pregnant women | 46 | 10.93±1.21 | 53 | 22.9±6.13 |
NPNL: Nonpregnant nonlactating, SD: Standard deviation
Figure 1.
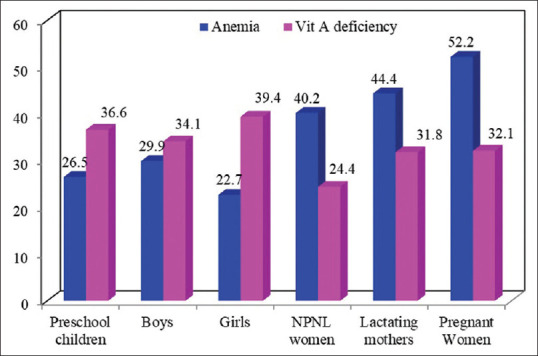
Prevalence of Vitamin A deficiency and anemia among different physiological groups
The prevalence of VAD was observed to be higher among participants living in Kutcha houses, with occupation of women as cultivators, illiterate head of HHs, low PCI, and big family size.
The prevalence of anemia was higher among participants living in kutcha houses, whereas other sociodemographic variables were not observed to be associated with anemia [Table 2].
Table 2.
Association between anemia and Vitamin A deficiency with sociodemographic variables
| Characteristics (n) | Vitamin A (µg/dl) |
Hemoglobin (g/dl) |
||||
|---|---|---|---|---|---|---|
| ≥20 | <20 | Normal | Anemia | |||
| Type of house | ||||||
| Pucca (99) | 78.4 | 21.6 | 70.2 | 29.8 | ||
| Semi pucca (276) | 69.3 | 30.7 | 60.4 | 39.6 | ||
| Kutcha (377) | 67.1 | 32.9 | 53.0 | 47.0 | ||
| χ2, P | 4.9, 0.08 | 5.86, 0.05 | ||||
| Education of Women | ||||||
| Illiterate (165) | 66.8 | 33.2 | 56.8 | 43.2 | ||
| 1-8th class (350) | 68.4 | 31.6 | 56.2 | 43.8 | ||
| 9th and above (237) | 72.5 | 27.5 | 61.3 | 38.7 | ||
| χ2, P | 1.89,0.38 | 0.91, 0.63 | ||||
| Occupation of women | ||||||
| Cultivation (260) | 63.2 | 36.8 | 60.7 | 39.3 | ||
| Others (41) | 84.4 | 15.6 | 56.7 | 43.3 | ||
| HW (450) | 71.3 | 28.7 | 57.1 | 42.9 | ||
| χ2, P | 10.7, 0.01 | 0.45, 0.79 | ||||
| Education of HHH | ||||||
| Illiterate (85) | 61.3 | 38.7 | 52.4 | 47.6 | ||
| 1-8th class (269) | 64.8 | 35.2 | 52.9 | 47.1 | ||
| 9th and above (398) | 74.2 | 25.8 | 62.6 | 37.4 | ||
| χ2, P | 10.5, 0.001 | 3.93, 0.14 | ||||
| Occupation of HHH | ||||||
| Labour (91) | 72.7 | 27.3 | 61.1 | 38.9 | ||
| Cultivation (311) | 65.0 | 35.0 | 44.9 | 55.1 | ||
| Service (350) | 72.3 | 27.7 | 58.1 | 41.9 | ||
| χ2,P | 5.11, 0.07 | 4.11, 0.12 | ||||
| PCI tertile | ||||||
| 1 (254) | 64.4 | 35.4 | 57.8 | 42.2 | ||
| 2 (238) | 71.2 | 28.8 | 58.2 | 41.8 | ||
| 3 (238) | 72.3 | 27.7 | 58.3 | 41.7 | ||
| χ2, P | 4.79, 0.09 | 0.00, 0.99 | ||||
| Family Size | ||||||
| 1-4 (323) | 77.4 | 22.6 | 61.9 | 38.1 | ||
| 5-8 (398) | 68.2 | 31.8 | 57.7 | 42.3 | ||
| >9 (31) | 67.6 | 32.4 | 27.8 | 72.2 | ||
| χ2, P | 8.55, 0.01 | 7.81, 0.20 | ||||
| BMI of women | ||||||
| <18.5 (58) | 72.7 | 27.3 | 45.9 | 54.1 | ||
| 18.55-24.99 (406) | 75.1 | 24.9 | 57.9 | 42.1 | ||
| >25.0 (59) | 70.8 | 29.2 | 68.8 | 31.3 | ||
| P | NS | NS | ||||
PCI: Per capita income, BMI: Body mass index, NS: Not significant, HHH: Head of Household, HW: Housewife
Logistic regression analysis showed that the odds of VAD was 1.67 (1.16–2.41) times higher among woman engaged in cultivation as compared to those engaged in service or business and 1.65 (1.17–2.32) times higher among HHs with family size of 5–8 as compared to family size of 1–4 members.
Food and nutrient intakes
The mean intakes of cereals, pulses, milk and milk products, fat and oils, and sugar and jaggery were below the recommended level of RDI. However, the intakes of green leafy vegetables, other vegetables and roots, and tubers and flesh foods were above the RDI.
The median intake of proteins and Vitamin C was above the recommended level of RDA. Fat intake was observed low in spite of the flesh food intake in diet may be due to low intake of fats and oils [Table 3].
Table 3.
Average consumption of nutrients (g/day) and percent RDA among children and women
| Particulars | Protein (g) | Total Fat (g) | Energy(Kcal) | Calcium(mg) | Iron(mg) | Vit.-A (µg) | Thiamine (mg) | Riboflavin (mg) | Niacin (mg) | Vit.-C (mg) | Dietary folate (µg) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-3 year children | |||||||||||
| Mean | 22.6 | 5.7 | 766.9 | 327.1 | 3.7 | 48.0 | 0.4 | 0.5 | 5.5 | 56.7 | 43.0 |
| RDA | 17 | 27 | 1060 | 600 | 9.0 | 400 | 0.5 | 0.6 | 8.0 | 40 | 80 |
| % RDA | 132.9 | 21.1 | 72.3 | 54.5 | 41.1 | 12.0 | 80.0 | 83.3 | 68.8 | 141.8 | 34.4 |
| 4-6 yrs children | |||||||||||
| Mean | 23.9 | 6.6 | 907.8 | 273.1 | 3.6 | 41.1 | 0.5 | 0.5 | 5.9 | 63.7 | 32.4 |
| RDA | 20 | 25 | 1350 | 600 | 13.0 | 400 | 0.7 | 0.8 | 11.0 | 40 | 100 |
| % RDA | 119.5 | 26.4 | 67.2 | 45.5 | 27.7 | 10.3 | 71.4 | 62.5 | 53.6 | 159.3 | 32.4 |
| NPNL women Sedentary work | |||||||||||
| Mean | 52.6 | 10.6 | 1726.6 | 648.8 | 9.9 | 128.2 | 0.9 | 0.9 | 12.5 | 99.4 | 60.0 |
| RDA | 55.0 | 20.0 | 1900 | 600 | 21.0 | 600 | 1.0 | 1.1 | 12.0 | 40 | 200 |
| %RDA | 95.6 | 53.0 | 90.9 | 108.1 | 47.1 | 21.4 | 90.0 | 81.8 | 104.2 | 248.5 | 30.0 |
| NPNL women Moderate work | |||||||||||
| Mean | 54.5 | 12.7 | 1806.5 | 555.7 | 5.6 | 89.2 | 0.8 | 0.9 | 12.3 | 95.0 | 54.2 |
| RDA | 55.0 | 25.0 | 2230 | 600 | 21.0 | 600 | 1.1 | 1.3 | 14.0 | 40 | 200 |
| %RDA | 99.1 | 50.8 | 81.0 | 92.6 | 26.7 | 14.9 | 72.7 | 69.2 | 87.9 | 237.5 | 27.1 |
DISCUSSION
The present study revealed that the prevalence of subclinical VAD was 37% among preschool children and 25% among NPNL women and 32% among pregnant and lactating women. A review by Akhtar et al.[17] reported 31%–57% prevalence of VAD among preschool children in India. A study carried out by NIN, Hyderabad, in eight states of India reported 62% (confidence interval [CI]: 60.3–63.3) prevalence of subclinical VAD among preschool children ranging from 88% in Madhya Pradesh and 79% in Kerala to 49%–62% in Tamil Nadu, Karnataka, Maharashtra, Odisha, and Andhra Pradesh.[18] Neighboring countries such as Bangladesh (28%), Bhutan (32%), Nepal (33%), and Pakistan (35%) had a low prevalence of subclinical VAD compared[17] to the low prevalence of VAD observed in this study, which may be attributed to the high intake of green leafy vegetables and animal food in diet as observed by food frequency and diet survey among the study population. The nutritive value for some of the Green leafy vegetables (GLV) consumed in Nagaland is not mentioned in the nutritive value of Indian foods, which may be the reason for low intakes through 24 h recall diet.
Stevens et al. in their study estimated 44% prevalence of VAD (CI: 13–79), which was significantly associated with the occupation of woman and family size,[19] similar to our study.
The prevalence of anemia observed in the present study is similar to that reported by National Family Health Survey-4 for Nagaland, which is 37% for children (6–59 months), 49% for NPNL women (15–49 years), and 48% for pregnant women,[20] whereas it was 72% among pregnant, 86% among lactating mothers, and 67% among preschool children as per the National Nutrition Monitoring Bureau (NNMB) (2003) survey.[21]
Selvam et al. reported 64% (95% CI: 58.0, 69.9) prevalence of anemia among urban preschool children in Tamil Nadu with no significant difference between boys and girls.[22]
No difference was observed in the prevalence of VAD and anemia with nutritional status. This may be due to the low prevalence of undernutrition (chronic energy deficiency body mass index <18.5) among women (10%) and children (14%).
Vitamin A supplementation was observed only among 31% of children aged 12–59 months, with the important reason being nonavailability of Vitamin A supply in the area.
CONCLUSIONS AND RECOMMENDATIONS
Anemia and VAD were observed low in the study population, which may be due to high biodiversity in the NE region in spite of low Vitamin A coverage. Therefore, there is a need to strengthen the existing national program for Vitamin A and Iron and folic acid tablets (IFA) supplementation and encourage people to eat Vitamin A-rich food and impart health and nutrition education.
Financial support and sponsorship
This study was financially supported by Bioversity International, Rome and North East Slow Food and Agrobiodiversity Society, Shillong, Meghalaya.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. The Global Prevalence of Anaemia in 2011 WHO. Geneva: WHO; 2015. [Google Scholar]
- 2.Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123–35. doi: 10.1016/S0140-6736(10)62304-5. [DOI] [PubMed] [Google Scholar]
- 3.Stoltzfus RJ, Mullany L, Black RE. Iron deficiency anaemia. In: Ezzati M, Lopez AD, Rodgers A, Murray CJ, editors. Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Vol. 1. Geneva: World Health Organization; 2004. [Last accessed on 20 May 2020]. pp. 163–210. Available from: http://www.who.int/publications/cra/chapters/volume1/0163.0210.pdf?ua=1 . [Google Scholar]
- 4.Haas JD, Brownlie T. Iron deficiency and reduced work capacity: A critical review of the research to determine a causal relationship. J Nutr. 2001;131:676S–88. doi: 10.1093/jn/131.2.676S. [DOI] [PubMed] [Google Scholar]
- 5.Kozuki N, Lee AC, Katz J. Child Health Epidemiology Reference Group. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J Nutr. 2012;142:358–62. doi: 10.3945/jn.111.149237. [DOI] [PubMed] [Google Scholar]
- 6.Steer PJ. Maternal hemoglobin concentration and birth weight. Am J Clin Nutr. 2000;71:1285S–7. doi: 10.1093/ajcn/71.5.1285s. [DOI] [PubMed] [Google Scholar]
- 7.Vijayaraghavan K. Vitamin A deficiency: Consequences and control programs. In: Sachdev HP, Choudhury P, editors. Nutrition in Children: Developing Country Concerns. 1st ed. New Delhi, India: Convenors; 1994. pp. 536–44. [Google Scholar]
- 8.World Health Organization. Global Prevalence of Vitamin A Deficiency in Populations at Risk 1995-2005. Geneva: WHO; 2009. [Google Scholar]
- 9.Phek district. [Last accessed on 2019 Dec 16]. Available from: https://en.wikipedia.org/wiki/Phek_district .
- 10.Thimmayamma BV, Rao DH. A comparative study of oral questionnaire method with actual observation of the dietary intake of preschool children. J Nutr Dietet. 1969;6:177–81. [Google Scholar]
- 11.Gopalan C, Ramaswamy BV, Balasubramanyam SC, Rao BS, Deosthale YG, Pant KV. Nutritive Value of Indian Foods, National Institute of Nutrition, Indian Council of Medical Research (ICMR), Hyderabad, India. 1989 [Google Scholar]
- 12.Expert Group of Indian Council of Medical Research. Recommended Dietary Intakes for Indians. ICMR. 1981 [Google Scholar]
- 13.Expert Group of the Indian Council of Medical Research. Nutrient Requirements and Recommended Dietary Allowances for Indians. New Delhi: ICMR; 2011. [Google Scholar]
- 14.Sari M, de Pee S, Martini E, Herman S, Sugiatmi, Bloem MW, et al. Estimating the prevalence of anaemia: A comparison of three methods. Bull World Health Organ. 2001;79:506–11. [PMC free article] [PubMed] [Google Scholar]
- 15.Craft NE, Haitema T, Brindle LK, Yamini S, Humphrey JH, West KP., Jr Retinol analysis in dried blood spot by HPLC. J Nutr. 2000;130:882–5. doi: 10.1093/jn/130.4.882. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. WHO/NHD/UNICEF/UNU, Report No. 01.3. Geneva: WHO; 2001. Iron Deficiency Anaemia: Assessment, Prevention, and Control. A Guide for Programme Managers. [Google Scholar]
- 17.Akhtar S, Ahmed A, Randhawa MA, Atukorala S, Arlappa N, Ismail T, et al. Prevalence of vitamin A deficiency in South Asia: Causes, outcomes, and possible remedies. J Health Popul Nutr. 2013;31:413–23. doi: 10.3329/jhpn.v31i4.19975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Nutrition Monitoring Bureau. Prevalence of Vitamin A deficiency among Pre-School Children in rural Areas. TRS No. 23. Hyderabad: National Institute of Nutrition; 2006. [Google Scholar]
- 19.Stevens GA, Bennett JE, Hennocq Q, Lu Y, De-Regil LM, Rogers L, et al. Trends and mortality effects of vitamin A deficiency in children in 138 low-income and middle-income countries between 1991 and 2013: A pooled analysis of population-based surveys. Lancet Glob Health. 2015;3:e528–36. doi: 10.1016/S2214-109X(15)00039-X. [DOI] [PubMed] [Google Scholar]
- 20.International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-2016, India, Mumbai: IIPS. 2017. [Last accessed on 2019 Dec 16]. Available from: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf .
- 21.National Nutrition Monitoring Bureau. Prevalence of Micronutrient deficiency. National Institute of Nutrition, Hyderabad. Technical Report No. 22. 2003 [Google Scholar]
- 22.Selvam S, Swaminathan S, Srinivasan K, Kurpad AV. Prevalence of anemia, sub-clinical vitamin D and vitamin A deficiencies and its relationship with anthropometric measures and diet pattern among Urban South Indian Preschool Children. Indian J Nutri. 2016;3:142. [Google Scholar]


