Abstract
Introduction:
Data from several sources revealed that huge incongruity persists in nutritional status across the states in India. Thus, this study was undertaken to generate a nutritional index, so that these disparities could be quantified and comparison be done.
Materials and Methods:
A nutritional index for 21 major states of India has been constructed on the basis of eight important nutrition-related indicators. The scaled value of each indicator for all the states was calculated. Each indicator was assigned an arbitrary weight (Wi) on the basis of its impact on nutritional status. On the basis of the scaled value and weight given to the particular indicator, a composite-weighted index was thus calculated.
Results:
States were ranked on their nutritional status as per the final composite score they attained. Out of 21 major states, Kerala took the top position followed by Jammu and Kashmir and Himachal Pradesh on the 2nd and 3rd position, respectively, while Uttar Pradesh got the lowest rank followed by Bihar and Jharkhand on the 2nd and 3rd lowest positions.
Conclusion:
Our study concludes that not taking an account of the burden of malnutrition when disbursing funds leads to ineffective implementation of various nutritional programs. Integrated Child Development Services has already been brought in mission mode under Poshan Abhiyan. Other determinants, i.e., illiteracy, poor sanitation, diseases, and infections, should also be considered and addressed through nutritional programs.
Keywords: Composite score, malnutrition, NITI Aayog, nutrition index, Poshan Abhiyan
INTRODUCTION
Good nutrition is among the basic human needs, also addressed in the second sustainable development goal (end hunger, achieve food security, and improved nutrition).[1] However, progress to improve nutrition remains inordinately slow.[2] According to recent estimates by UNICEF, malnutrition is the root cause of virtually half of all deaths occurring globally among children under 5.[3] Undernutrition not only jeopardizes the healthy survival of children by increasing the susceptibility for common infections but also makes them vulnerable to increased frequency and severity of such infections and thereby leading to delayed recovery.[4] It is an impenetrable truth that India accommodates largest numbers of malnourished children and every year malnutrition contributes to about half of the 1.3 million deaths occurring in under-five children.[5] NFHS-4 data disclosed that 35.7% children below 5 years are underweight, 38.4% are stunted, and 21% are wasted in the country.[6] Furthermore, malnutrition is among one of the foremost causes of anemia. Several studies have identified stunting and low BMI as one of the risk factors of anemia in under-five.[7] While continuing to focus on undernourishment, substantial efforts are indispensable for addressing anemia among children. Due to the towering prevalence of malnutrition and anemia in India, Children aged 0-5 years have been granted sizable program attention GOI launched Integrated Child Development Services (ICDS) scheme in 1975, which emerged as one of the premier programs to alleviate malnutrition burden.[8] Even though four decades have elapsed since the program was set in motion, still malnutrition persists to be a major public health problem.[9] The ICDS program suffered from several crunches such as inadequate data management, weak accountability, and varying practices across the states. Besides this, in many states, Anganwadi centers (AWCs) were dispensing services to more beneficiaries than they can afford, compromising the services, whereas in some states, AWCs failed to achieve 100% registration of children. Thus, the undernourished children remained unspotted. To acknowledge these challenges, a more ambitious program, i.e., Poshan Abhiyan derived by a National Nutritional Strategy, has been launched in 2018 to successfully reach to MALNUTRITION-FREE INDIA by 2022.[10]
Data from several sources revealed that huge incongruity persists in nutritional status across the states in India.[11,12] Thus, this study was undertaken to generate a nutritional index, so that these disparities could be quantified and comparisons be done. Second, this study was done to bring about appropriate and cost-effective interventions needed to improve the nutrition of vulnerable children.
MATERIALS AND METHODS
A nutritional index for 21 major states of India has been constructed on the basis of eight important nutrition-related indicators. These eight indicators were grouped into two categories, namely, key input indicators and nutritional outcome indicators. The scaled value of each indicator for all the states was calculated. For positive indicator i.e. % children breastfed within 1 hr of birth (source: NFHS 4)[13], % children exclusively breastfed under age of 6 months (source: NFHS 4)[13], and per capita fund released under ICDS for supplementary nutrition (Authors calculation; numerator has been taken from data available from Ministry of Consumer Affairs, Food and Public Distribution[14] and denominator has been taken from census 2011); scaled value was calculated as follows:[15]
where Si = Scaled value for positive indicator and Xi = Data value of the indicator.
Similarly, For negative indicator i.e. % stunted children under 5 years age (source: NFHS 4)[13], % wasted children under 5 years age (source: NFHS 4)[13], % anaemic children under 5 years age (source: NFHS 4)[13] and population covered per AWC (Source: Authors calculation; numerator has been taken from census 2011 and denominator has been taken from data available from Ministry of Women and Child Development)[16]; scaled value was calculated as follows:[15]
where Si = Scaled value for negative indicator and Xi = Data value of the indicator.
*The minimum and maximum value for each of the positive and negative indicator was determined based on the values for that indicator across states. As all the indicators included in the study do not have an equal importance. So, each indicator was assigned an arbitrary weight (Wi) on the basis of its impact on nutritional status. Finally, on the basis of the above-scaled value and weight given to the particular indicator, a composite-weighted index was thus calculated as follows:[15]
Composite -weighted index 
Table 1 provides the value of arbitrary weight given to each indicator for calculating the final score and ranking of states. The highest weight, i.e., 100, was given to indicators which are directly linked to health and have maximum impact on nutrition.
Table 1.
Value of arbitrary weight given to the particular indicator
| Key input |
Nutritional outcome |
||
|---|---|---|---|
| Indicator | Weight | Indicator | Weight |
| % children breastfed within 1 h of birth* | 100 | % stunted children (<5 years) | 100 |
| % children exclusively breastfed under age of 6 months* | 100 | % wasted children (<5 years) | 75 |
| Per capita fund released under ICDS for supplementary nutrition | 25 | % underweight children (<5 years) | 50 |
| Population covered per AWC (operational) | 25 | % anemic children (<5 years) | 25 |
ICDS: Integrated Child Development Services, AWC: Anganwadi center
RESULTS
A total of four indicators for each state were selected to reflect the key input in alleviation of malnutrition. Table 2 depicts the state-wise list of key input indicators. Only one indicator, i.e., population covered per AWC, was considered as a negative indicator, and the rest three indicators (% children breastfed within 1 h of birth, % children exclusively breastfed under age of 6 months, and per capita fund released under ICDS for supplementary nutrition) were positive. Similarly, four indicators for each state were selected to evaluate the nutritional outcome [Table 3]. All the four nutritional outcome indicators were considered as a negative indicator, e.g., lower the value, better is the performance.
Table 2.
State wise list of key input indicators
| State | % children breastfed within 1 h of birth* | % children exclusively breastfed under age of 6 months* | Per capita fund released under ICDS for supplementary nutrition (in rupees)** | Population covered per AWC (operational)*** |
|---|---|---|---|---|
| Andhra Pradesh | 40 | 70.2 | 0.8136 | 1521.07 |
| Assam | 64.4 | 63.5 | 2.9793 | 502.08 |
| Bihar | 34.9 | 53.4 | 0.9834 | 1135.50 |
| Chhattisgarh | 47.1 | 77.2 | 2.0024 | 506.37 |
| Delhi | 28 | 49.6 | 0.8205 | 1540.60 |
| Gujarat | 49.9 | 55.8 | 1.0620 | 1139.75 |
| Haryana | 42.4 | 50.3 | 0.6343 | 976.48 |
| Himachal Pradesh | 41.1 | 67.2 | 2.8417 | 362.73 |
| Jammu and Kashmir | 46 | 65.4 | 2.1818 | 423.71 |
| Jharkhand | 33.1 | 64.8 | 1.4010 | 858.35 |
| Karnataka | 56.3 | 54.2 | 1.5778 | 926.94 |
| Kerala | 64.3 | 53.3 | 0.8548 | 1004.87 |
| Madhya Pradesh | 34.4 | 58.2 | 1.4963 | 747.71 |
| Maharashtra | 57.5 | 56.6 | 0.9270 | 1023.64 |
| Odisha | 68.5 | 65.6 | 1.5639 | 578.26 |
| Punjab | 30.7 | 53 | 0.4934 | 1027.99 |
| Rajasthan | 28.4 | 58.2 | 0.7272 | 1106.08 |
| Tamil Nadu | 54.7 | 48.3 | 0.8835 | 1325.28 |
| Uttar Pradesh | 25.2 | 41.6 | 1.4083 | 1062.85 |
| Uttaranchal | 27.8 | 51.2 | 3.5405 | 502.63 |
| West Bengal | 47.4 | 52.3 | 0.8706 | 791.06 |
Maximum value of the Indicator, Minimum value of the indicator. ICDS: Integrated Child Development Services, AWC: Anganwadi center, NFHS: National Family Health Survey
Table 3.
State wise list of nutritional outcome indicators
| State | *% Stunted children (<5 years) | *% wasted children (<5 years) | *% underweight children (<5 years) | *% Anemic children (<5 years) |
|---|---|---|---|---|
| Andhra Pradesh | 31.4 | 17.2 | 31.9 | 58.6 |
| Assam | 36.4 | 17 | 29.8 | 35.7 |
| Bihar | 48.3 | 20.8 | 43.9 | 63.5 |
| Chhattisgarh | 37.6 | 23.1 | 37.7 | 41.6 |
| Delhi | 31.9 | 15.9 | 27 | 59.7 |
| Gujarat | 38.5 | 26.4 | 39.3 | 62.6 |
| Haryana | 34 | 21.2 | 29.4 | 71.7 |
| Himachal Pradesh | 26.3 | 13.7 | 21.2 | 53.7 |
| Jammu and Kashmir | 27.4 | 12.1 | 16.6 | 54.5 |
| Jharkhand | 45.3 | 29 | 47.8 | 69.9 |
| Karnataka | 36.2 | 26.1 | 35.2 | 60.9 |
| Kerala | 19.7 | 15.7 | 16.1 | 35.7 |
| Madhya Pradesh | 42 | 25.8 | 42.8 | 68.9 |
| Maharashtra | 34.4 | 25.6 | 36 | 53.8 |
| Odisha | 34.1 | 20.4 | 34.4 | 44.6 |
| Punjab | 25.7 | 15.6 | 21.6 | 56.6 |
| Rajasthan | 39.1 | 23 | 36.7 | 60.3 |
| Tamil Nadu | 27.1 | 19.7 | 23.8 | 50.7 |
| Uttar Pradesh | 46.3 | 17.9 | 39.5 | 63.2 |
| Uttaranchal | 33.5 | 19.5 | 26.6 | 59.8 |
| West Bengal | 32.5 | 20.3 | 31.6 | 54.2 |
Minimum value of the indicator, Maximum value of the indicator. NFHS: National Family Health Survey
Figure 1 shows ranking of states based on their nutritional status according to the final composite score. Out of 21 major states, Kerala took the top position followed by Jammu and Kashmir and Himachal Pradesh on the 2nd and 3rd position, respectively, whereas Uttar Pradesh got the lowest rank followed by Bihar and Jharkhand on the 2nd and 3rd lowest position, respectively.
Figure 1.
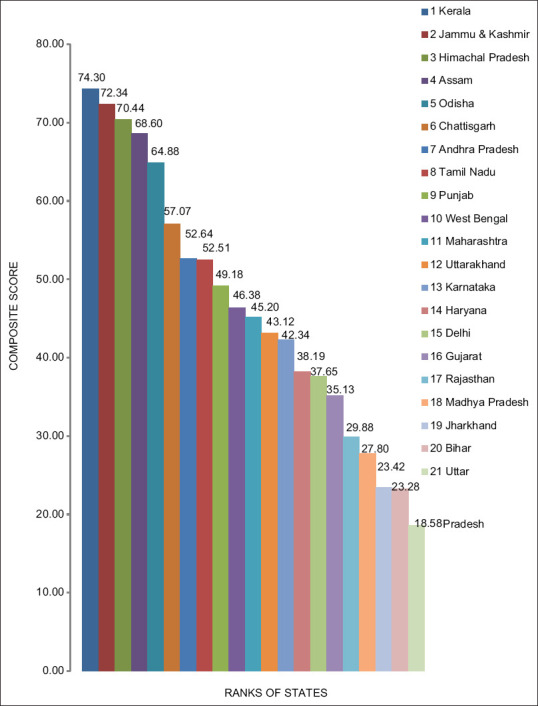
Ranking of states within India from highest to lowest composite score
Table 4 shows the categorization of states on the basis of composite score obtained. Good performing states were the ones achieving top one-third scores (score >55.72), moderate performing states were the ones falling in middle one-third (score between 55.72 and 37.15), and poor performing states were the ones falling in the lowest one-third score (score < 37.15).
Table 4.
Categorization of states on the basis of composite score
| Good performing states | Moderate performing states | Poor performing states |
|---|---|---|
| Kerala Jammu &kashmir Himachal Pradesh Assam Odisha Chattisgarh |
Andhra Pradesh Tamil Nadu Punjab West Bengal Maharastra Uttarakhand Karnataka Haryana Delhi |
1. Uttarpradesh 2. Bihar 3. Jharkhand 4. Madhya Pradesh 5. Rajasthan 6. Gujarat |
The categorization of states is done using the same score cutoffs as the NITI Ayog Healthy states progressive India.
DISCUSSION
The present study underpins an attempt to compile data on malnutrition from various secondary sources and compares the disparities in the nutritional status of states across India. While stunting and wasting indicate chronic and acute malnutrition, respectively, underweight is a composite indicator and includes both acute (wasting) and chronic (stunting) malnutrition.[17] Limited reduction in the prevalence of malnutrition has been achieved by the country from 48% (stunting), 19.8% (wasting), and 42.5% (underweight) in 2006 to 38%, 21%, and 35.8% in 2016.[18,19] States such as Kerala, Punjab, and Himachal Pradesh who are performing well in most of the health indicators have also sustained their status in nutrition, but at the same time, states such as Bihar, UP, and Jharkhand are still struggling with the wide prevalence of malnutrition. This is in concordance with the UNICEF report, which documented that all the districts in Bihar have prevalence above 30%, while 36 out of 38 districts have 40% and 13 out of 38 districts have unacceptable high prevalence of 50%.[20] The impressive picture of states like Kerala is attributed to high female literacy and remarkable reach of public distribution system.[21,22] On the same place, the gloomy picture of states such as Bihar, Jharkhand, and Uttar Pradesh is attributed to poverty, high fertility rate, and low female literacy.[23] Furthermore, poor and inappropriate infant and young child feeding practices play a significant role in the occurrence of malnutrition, especially in children under 2 years of age.[24,25,26] In consonance with this, our study also noted higher prevalence of initiation of breastfeeding and exclusive breastfeeding among the top ranking states (Odisha, Assam, etc.). In support of our finding, Masare et al.[26] also concluded in their study in Maharashtra that nonoptimal breastfeeding practices are significant risk factor for underweight infants. Similar finding was recognized by Das and Barua,[27] Ukarande et al.,[28] and Kumar and Singh.[29] Statistics of anemia among under 5 age group at national level achieved no exception gain with 69.4% in 2006 to 58.6% in 2016. As per the NFHS-4 data, Haryana emerged as the state with the highest number of anemic children, holding it accountable for standing at rank 14 (moderate performing state) in our list. Kumar et al.[30] also identified in their study in Haryana that most of the anemic patients were suffering from different grades of malnutrition. Another study conducted in Haryana by Narayan and Singh,[31] revealed that children aged 6 to 24 months belonging to low socioeconomic group and not receiving breastfeed in first 4–6 months of their life are at significant risk of anemia.
Another matter of concern in our study was pertaining to per capita fund released under ICDS. Allocating the funds equally to both, high performing as well as poor performing states, falls shorts to fix the higher malnutrition status of poor performing states like Bihar, Jharkhand and UP. Thus, indicating the need for higher fund allocation for states with high malnutrition prevelance as compared to states with lower prevelance. It is also observed that states such as Gujarat and Tamil Nadu are spending more than the required amount, but still they are lagging behind as moderate performers, indicating that effective implementation of the ICDS program is a matter of equal concern than just the funding constraint.[32]
During the current decade, Odisha and Chhattisgarh have emerged as an exemplary state. Despite being a poor state, Odisha has managed to make a worthy improvement in nutrition (Rank-5). Adequate allocation of fund for supplementary nutrition, skilled and motivated Anganwadi worker, and prioritization of disadvantaged population were important contributory factors toward increasing their health coverage.[9]
It is worth noting in our study finding that in states such as Delhi, Gujarat, Tamil Nadu, and Bihar, AWCs were catering to population higher than the usual ICDS norm, i.e., 1540.60, 1139.75, 1135.5, and 1325.25, respectively, thus overburdening the Anganwadi worker which eventually brings down their efficiency and performance.[33] Furthermore, the quality of service is adversely hampered where the AWC is reaching out to populations more than the authorized usual norms. Kochar et al. mentioned in their study that providing an additional worker of higher ability to a cluster of AWCs might address this human resource constraint at low cost.[34]
CONCLUSION
The study brings forth a composite index, an important tool, that brings all the 21 states at one platform and reveals the fair picture to then analyze the status. Our study concludes that not taking an account of the burden of malnutrition when disbursing funds leads to ineffective implementation of various nutritional programs. ICDS has already been brought in mission mode under Poshan Abhiyan, emphasizing on convergence, targeted approach, use of information technology, social audit, and service delivery for the first 1000 days of life. Apart from these, it is desirable that other determinants, i.e., illiteracy, poor sanitation, diseases, and infections should also be considered and addressed through nutritional programs.
Limitation
The current study has some limitations which are required to be marked. First, inclusion of all the states could not be done. Only 21 major states (categorized as per Niti Aayog report for genesis of health index) were included in the study. Second, only limited number of input and output indicators could be used due to nonavailability of data of the others. Thus, the indicators covering diseases and infections contributing to malnutrition could not be incorporated in the study. Third, the weights assigned to each indicator for the calculation of composite index are not standardized and the importance of each indicator to the composite could not be analyzed statistically.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alamgir K, Sami UK, Salahuddin K. Nutritional complications and its effects on human health. J Food Sci Nutr. 2018;1:17–20. [Google Scholar]
- 2.FAO, IFAD, UNICEF, WFP and WHO. The State of Food Security and Nutrition in the World. 2017. [Last accessed on 2019 Sep 01]. Available from: http://www.fao.org/3/a-I7695e.pdf .
- 3.UNICEF DATA. Malnutrition in Children. UNICEF. 2019 [Google Scholar]
- 4.Arya AK, Lal P, Kumar P. Co-morbidities in children with severe acute malnutrition – A tertiary care centre experience. Int J Contemp Med Res. 2017;4:1086–8. [Google Scholar]
- 5.Yadav SS, Yadav ST, Mishra P, Mittal A, Kumar R, Singh J. An epidemiological study of malnutrition among under five children of rural and urban Haryana. J Clin Diagn Res. 2016;10:LC07–10. doi: 10.7860/JCDR/2016/16755.7193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta V, Chawla S, Mohapatra D. Nutritional assessment among children (1–5 years of age) using various anthropometric indices in a rural area of Haryana, India. Indian J Community Fam Med. 2019;5:39–43. [Google Scholar]
- 7.Rahman MS, Mushfiquee M, Masud MS, Howlader T. Association between malnutrition and anemia in under-five children and women of reproductive age: Evidence from Bangladesh Demographic and Health Survey 2011. PLoS One. 2019;14:e0219170. doi: 10.1371/journal.pone.0219170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sachdev Y, Dasgupta J. Integrated child development services (ICDS) scheme. Med J Armed Forces India. 2001;57:139–43. doi: 10.1016/S0377-1237(01)80135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahoo J, Mahajan PB, Paul S, Bhatia V, Patra AK, Hembram DK. Operational assessment of ICDS scheme at grass root level in a rural area of Eastern India: Time to introspect. J Clin Diagn Res. 2016;10:LC28. doi: 10.7860/JCDR/2016/23059.9041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NITI AYOG. Nourishing India. National Nutrition Strategy, Government of India. [Last accessed on 2019 Sep 01]. Available from: http://www.niti.gov.in/writereaddata/files/document_publication/Nutrition_Strategy_Booklet.pdf .
- 11.Raykar N, Majumder M, Laxminarayan R, Menon P. India Health Report: 2015. New Delhi, India: Public Health Foundation of India; 2015. [Google Scholar]
- 12.Menon P, Deolalikar A, Bhaskar A. India State Hunger Index: Comparisons of Hunger Across States. Washington, D.C.: Bonn, and Riverside; 2009. [Google Scholar]
- 13.(NFHS.4) Fact Sheets- National Family Health Survey. Key Findings from NFHS-4. [Last accessed on 2019 Sep 01]. Available from: http://rchiips.org/nfhs/factsheet_nfhs.4-shtml .
- 14.Funds Released under Integrated Child Development Services (ICDS) Scheme for the Year 2015-16 (From: Ministry of Women and Child Development) [Google Scholar]
- 15.NITI AYOG. Healthy States Progressive India. Report on the Ranks of States and Union Territories. [Last accessed on 2019 Sep 01]. Available from: http://social.niti.gov.in/uploads/sample/health_index_report.pdf .
- 16.Number of Sanctioned, Operational Anganwadi Centres (AWCs) as on 31.12.2015 (From: Ministry of Women and Child Development) [Google Scholar]
- 17.Khan S, Zaheer S, Safdar NF. Determinants of stunting, underweight and wasting among children<5 years of age: Evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health. 2019;19:358. doi: 10.1186/s12889-019-6688-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinha RK, Dua R, Bijalwan V, Rohatgi S, Kumar P. Determinants of stunting, wasting, and underweight in five high-burden pockets of four Indian states. Indian J Community Med. 2018;43:279. doi: 10.4103/ijcm.IJCM_151_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.UNICEF. Childhood Stunting Across Districts in Eight Indian States: Burden, Determinants and Rate of Decline. Nutrition Reports. 2017. [Last accessed on 2019 Sep 01]. Available from: https://unicef.in/Uploads/Publications/Resources/pub_doc143.pdf .
- 20.Gopalan C. Child survival and child nutrition. NFI Bull. 1984;5:1–3. [PubMed] [Google Scholar]
- 21.Chandran KP. Health and nutrition profile of children in rural Kerala: A call for an action. MPRA Paper No. 27132, 2010. [Last accessed on 2019 Sep 02]. Available from: https://mpra.ub.uni-muenchen.de/27132/1/health_and_nutrtion_pofile_of_children_in_rural_kerala.pdf .
- 22.Som KS, Mishra RP. BIMARU states: Need a rethinking. JHSS. 2014;19:34–41. [Google Scholar]
- 23.Saha KK, Frongillo EA, Alam DS, Arifeen SE, Persson LA, Rasmussen KM. Appropriate infant feeding practices result in better growth of infants and young children in rural Bangladesh. Am J Clin Nutr. 2008;87:1852–9. doi: 10.1093/ajcn/87.6.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Udoh EE, Amodu OK. Complementary feeding practices among mothers and nutritional status of infants in Akpabuyo Area, Cross River State Nigeria. Springer Plus. 2016;5:2073. doi: 10.1186/s40064-016-3751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mwase I, Mutoro A, Owino V, Garcia AL, Wright CM. Poor infant feeding practices and high prevalence of malnutrition in urban slum child care centres in Nairobi: A pilot study. J Trop Pediatr. 2015;62:46–54. doi: 10.1093/tropej/fmv071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masare MS, Soyam G, Hiwarkar PA. A cross-sectional study of determinants and impact of breastfeeding and complementary feeding practices on nutritional status and common illnesses among infants in urban slum. Int J Res Med Sci. 2017;5:4563–6. [Google Scholar]
- 27.Das N, Barua A. Influence of breastfeeding practices on nutritional status of children among tea garden workers. Natl J Community Med. 2016;7:286–91. [Google Scholar]
- 28.Ukarande BV, Nagaonkar AS. A study of protein energy malnutrition with respect to breast feeding practices in less than six year children. Natl J Community Med. 2015;6:626–8. [Google Scholar]
- 29.Kumar A, Singh VK. A study of exclusive breastfeeding and its impact on nutritional status of child in EAG states. J Stat Appl Probab. 2015;4:435–45. [Google Scholar]
- 30.Kumar R, Sangwan L, Peter R, Bansal S, Malik T. Prevalence and aetiology of nutritional anaemia in children aged 6 month to 60 month in Fatehabad district of Haryana. J Basic Applied Sci. 2014;4:317–21. [Google Scholar]
- 31.Narayan R, Singh S. A study of severity and frequency of anemia in different age group in 6 months to 5 years children at a teaching hospital in rural Haryana, India. J Med Sci Clin Res. 2017;5:28086–9. [Google Scholar]
- 32.Kanjilal B, Mazumdar PG, Mukherjee M, Rahman MH. Nutritional status of children in India: household socio-economic condition as the contextual determinant. Int J Equity Health. 2010;9:19. doi: 10.1186/1475-9276-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaur D, Thakur M, Singh A, Saini SK. Workload and perceived constraints of anganwadi workers. Nurs Midwifery Res J. 2016;12:18–24. [Google Scholar]
- 34.Kochar A, Sharma A, Sharma A. Impact of the Uddeepan programme on child health and nutrition in India, 3ie Impact Evaluation Report 65. New Delhi: International Initiative for Impact Evaluation (3ie); 2017. [Google Scholar]


