Highlights
The COVID-19 pandemic has underscored the essential role of public safety personnel in serving and protecting all Canadians.
Public safety personnel were reporting challenges with mental health and well-being before the COVID- 19 pandemic; accordingly, the new stressors may mean public safety personnel need additional resources to sustainably help them help us.
This article suggests elements of support that may be attainable avenues for supporting the wellbeing of public safety personnel during the protracted stress caused by the COVID-19 pandemic.
Sustained self-care may be critical for maintaining the mental health and well-being of public safety personnel during the COVID-19 pandemic.
Introduction
The COVID-19 pandemic has underscored the essential role of public safety personnel (PSP) in serving and protecting all Canadians. PSP include professionals striving to ensure the safety and security of Canadians, such as border services officers, public safety communicators (e.g. emergency dispatchers), correctional workers, firefighters (career and volunteer), Indigenous emergency managers, operational and intelligence personnel, paramedics and police (municipal, provincial and federal).1,2 PSP often work alongside health care providers1 and are critical for managing the COVID-19 pandemic. Prior to COVID-19, PSP reported repeated exposures to potentially psychologically traumatic events (PPTE)2 and significant occupational stressors like staffing shortages, insufficient resources and fatigue.3,4 Therefore, pervasive COVID-19 pandemic stressors, such as the risk of personal and familial contagion (Commander S. Leduc, conversation with VT, 20 July, 2020), can be reasonably expected to further increase strain on PSP.
The different PSP sectors (e.g. police, fire, paramedics, corrections) require tailored supports to help sustainably manage the COVID-19 pandemic stressors. A growing literature documents the impact of previous epidemics (e.g. SARS, MERS) and the current pandemic on health care workers, 5,6 but there is very little literature delineating the impact of pandemics and epidemics on PSP. Collecting PSP-specific data to generate evidence amidst the COVID crisis would be informative, but would require shifting time and attention away from provision of essential services and towards research. An alternative approach for rapidly synthesizing evidence- informed, peer-reviewed knowledge and for disseminating strategies to support PSP was required; accordingly, the COVID-19 Readiness Resource Project (CRRP) of the Canadian Institute for Public Safety Research and Treatment (CIPSRT) was established with substantive resource support from Veterans Affairs Canada (VAC). The CRRP provides a national online knowledge hub for trusted information on PSP mental health and well-being based on consultations with PSP frontline staff, leadership and subject matter experts to identify challenges faced by PSP. Responses to the challenges are then derived from the extant peer-reviewed literature on the impact of pandemics and epidemics on health care workers, as well as general information on disaster mental health. The resulting derivations are then tailored for PSP and disseminated online by PSP, clinicians and researchers in various forms, including accessible written content; interactive virtual town halls led by subject matter experts and PSP panellists; videos; and guided audio-recorded stress management exercises.
Purpose
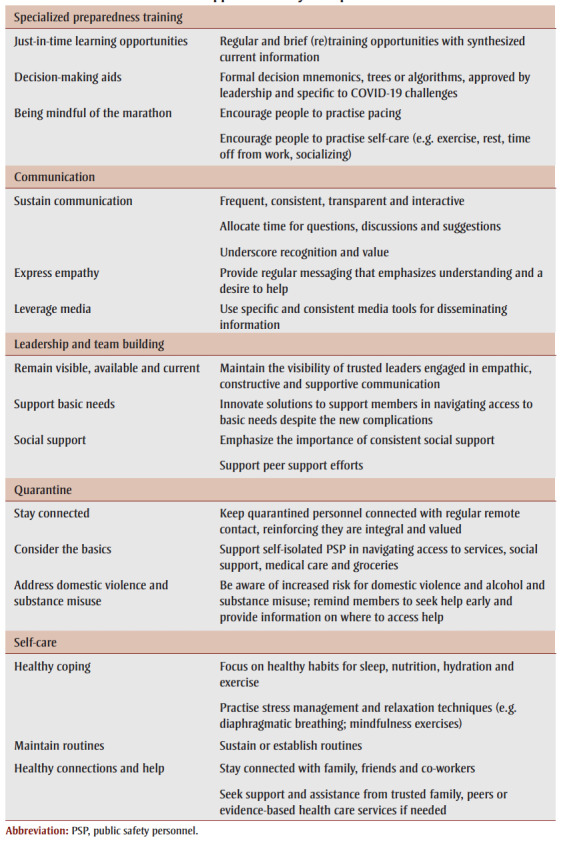
This article outlines five priority areas for supporting PSP during COVID-19, as identified by the CRRP. The intent is to raise awareness of PSP experiences and to encourage collective innovation in supporting PSP well-being. The listed priorities and recommendations are not exhaustive, definitive or mutually exclusive, and will not apply to every PSP sector or agency. Instead, this work offers recommendations for possible starting points to continue supporting PSP, their families and their leaders. Table 1 presents a summary of these recommendations.
Table 1. Support summary examples.
 |
Supporting PSP during COVID-19
Specialized preparedness training
PSP operate in environments of heightened uncertainty,7 potentiating the mental health risk of repeated PPTE exposures.3 PSP organizations may be able to support PSP functionality and mitigate risks of PPTEs3 through formal and informal preparedness training,8,9 as well as mental health training.4 Preparedness training through “rehearsal” may familiarize PSP with PPTEs, decrease surprise and mitigate the autonomic “fight, flight or freeze” stress response that might occur during a PPTE.10,11 The unexpected nature of the COVID-19 crisis may have compromised specific preparedness training capacities for many PSP; nevertheless, PSP are working successfully to meet the challenges and may benefit from additional supports to sustain their efforts as the pandemic continues to unfold.
Additional supports may include:
Just-in-time learning opportunities. Preparedness training for the COVID- 19 emergency response was necessarily compromised by the sudden outbreak of COVID-19, and the subsequently compressed time windows available to prepare staff. PSP, however, may continue to benefit from synthesized current information, provided with regular and brief (re)training opportunities (e.g. once weekly at a daily meeting; a brief video clip) from respected authorities on the latest guidelines, developments and intervention strategies.12-14 Regular training can help to decrease anxiety, increase trust in leadership, reinforce perceptions of agency, and decrease feelings of isolation.13,14
Decision-making aids. Formal decision mnemonics, trees or algorithms, if approved by leadership and specific to various COVID-19 challenges, may reduce uncertainty and anxiety for PSP navigating the current crisis.4,15 The information can be updated as new evidence becomes available.
Being mindful of the marathon. Preparedness during the current pandemic involves pacing to support the “marathon” of navigating the pandemic in the long term, while engaging in the intermittent “sprints” needed for emergency responses.16 PSP may need additional encouragement to monitor their own health and self-care, including exercise, rest, time off from work and socializing.
Communication
Getting the right information to the right people at the right time can be challenging at the best of times and may be even harder during a pandemic. “Crisis communication” is intended to effectively deliver information during the chaotic milieu of a crisis situation. Communications must be easily understood and consistent for people to remember key messages and take effective action.
Federal health authorities such as the US Centers for Disease Control and Prevention17provide guidelines for supporting efforts towards effective crisis communication. Additional supports may include:
Sustain communication. Keep communication frequent, consistent, transparent and interactive. New information is best retained and actioned when the content is concise, consistent and delivered by a respected source.18Allocating time for questions, discussions and suggestions creates spaces that can help leaders better understand PSP needs and is important to sustaining capacity during the marathon.7 Regular interactive communication with leadership can help reinforce team member’s self-esteem by underscoring that their efforts are recognized and valued.
Express empathy. The pandemic crisis may, at times, engender reactions of fear or anger in the public with whom PSP interact. Expressing empathic understanding and a wish to help may defuse these intense emotions.19 However, the pandemic might complicate PSP efforts to convey empathy (e.g. masks can interfere with nonverbal cues), requiring extra effort from PSP, which can increase their levels of strain. Despite the increased effort, overcoming the pandemic barriers to find ways to display empathy and caring may help facilitate positive outcomes for PSP and the people they serve.
Leverage media. Media can help to encourage altruistic, ethical and public-spirited behaviour, which will facilitate healthy communities during times of crisis.18 When possible, choose a small number of consistent sources for delivering information to maximize the number of people reached, while making it easy for PSP to know where to go for information. Traditional and social media can convey important information to help maximize public safety during the pandemic. Media communications can also be used to help mitigate hindsight bias and criticism that PSP and other frontline personnel can experience while making time-sensitive decisions in an unprecedented context that often require developing new best practices in real time.18
Leadership and team building
Leaders can play a critical role in supporting the psychological resilience and morale of their teams. Facilitating rapid access to evidence-based mental health services after a mental health injury remains important;5,20 however, reminding PSP that they can have support before, during and after a PPTE, particularly a protracted PPTE like the COVID-19 pandemic, may help to mitigate stress, burnout and other mental health injuries.21-23 Evidence-informed recommendations for leaders include:
Remain visible, available and current. The visibility of trusted leaders can bolster morale and underscore perceptions of available support, which may reinforce resilience. Leaders demonstrating, even briefly, that they have knowledge about shared stressors impacting their teams and unique stressors impacting individual team members can be particularly effective. Leaders can try to help by reminding PSP that COVID-19 is a protracted PPTE that requires attainable shortand long-term goals, as well as a focus on sustainable activities. Leaders can help their personnel to find meaning in the situation, to focus beyond the present crisis and to take pride in knowing they are contributing to the greater good of their community and country.16,24
Support basic needs. PSP always need their basic needs met in order to do their jobs effectively, but the pandemic has resulted in complications, such as self-isolation, that can compromise their ability to meet basic needs such as childcare and grocery shopping. Leaders and organizations may be able to help by working to identify such challenges and innovating solutions to offset the new complications.25
Social support. Social support can also be important for resilience, but aspects of social support can be compromised by necessary social distancing and self-isolation.25,26 PSP leaders can help reinforce positive relationships and morale by emphasizing their support for their teams, encouraging peer-to-peer support within teams and, where possible, supporting sustainable and consistent PSP work cycles and team composition.25-27
Quarantine
Evidence from previous epidemics has associated isolation with compromised mental health.6,18,28,29 Quarantine or selfisolation can lead to loneliness, boredom, fear, loss of routine and consequences such as alcohol and substance misuse.30-32 Multiple rounds of mandatory isolation during a pandemic can also exacerbate pre-existing mental health challenges.5 Following isolation, returning to work may be anxiety-provoking due to fears of (re)infection and reactions of colleagues who may have had to work overtime to cover short-staffing. Potential options for decreasing detrimental impacts of isolation include:
Stay connected. Workplaces can support isolated personnel by staying connected to them through regular remote check-ins. Reinforcing that people in isolation remain integral and valued members of the team can help mitigate potential mental health challenges.
Consider the basics. Measures that support PSP during self-isolation may include facilitating access to remote services and supplies (e.g. social support, medical care, groceries).
Address domestic violence and substance misuse. There have been increased incidents of domestic violence during the COVID-19 pandemic, as well as alcohol and substance misuse.30-32 PSP should be aware of the increased risk, reminded to seek help early and provided with access to resources.
Self-care
Maintaining self-care can be particularly challenging when facing occupational stressors such as shift work, irregular hours and exhaustion. The increased stress of COVID-19 may be partially mitigated by regularly encouraging PSP to engage in daily self-care practices to support their well-being, particularly their mental health and resilience.33,34 Suggestions for self-care include:
Healthy coping. Remind and encourage PSP to focus on maintaining healthy sleep, nutrition, exercise and regular rest. Practising stress management and relaxation techniques (e.g. diaphragmatic breathing; mindfulness exercises) can help to maintain a sense of well-being. Even 30 seconds of deep breathing or a five-minute mindfulness exercise during breaks and before sleep may help.
Maintain routines. Sustaining even simple routines, such as preparations before sleeping or scheduled physical training, can provide a sense of structure and predictability during the prolonged uncertainty generated by the pandemic.
Maintain healthy social connections and help. Staying connected with family, friends and co-workers can help preserve a sense of community, resilience and well-being. Where possible, prioritize positive online social media platforms and activities, and minimize platforms and activities that are distracting, distressing and frustrating.35 Seeking support from trusted family, peers or evidence-based health care services when needed can help PSP to manage the protracted stress caused by the pandemic.
Conclusion
The COVID-19 pandemic has underscored our dependence on the relative few who work to maintain public health, wellbeing and safety, and has highlighted the challenges to supporting PSP while they perform their critical roles. The unprecedented nature, size and scope of the pandemic has required ongoing, innovative and iteratively evaluated solutions. This article outlines clinically informed and, where available, evidence-informed recommendations to support PSP. The recommendations are being curated and disseminated by a national Canadian initiative, the COVID-19 Readiness Resource Project. As the COVID-19 pandemic evolves and new challenges arise, concerted efforts will be needed to provide and sustain psychosocial supports specific to PSP, allowing PSP not only to cope with the many challenges ahead, but to thrive in the face of them.
Acknowledgements
The authors sincerely thank the following individuals for their valued contributions: Dr. Cyd Courchesne, Health Professionals Division, Veterans Affairs Canada; Dr. Ron Martin, Faculty of Education, University of Regina; Dr. Rosemary Ricciardelli, Department of Sociology, Memorial University of Newfoundland; Lorraine Downey, Ottawa Paramedic Service, City of Ottawa/First Responder Mental Health Network Collaboration; Christine Godin, Ottawa Paramedic Service, City of Ottawa; Dr. Heather Hadjistavropoulos, Department of Psychology, University of Regina; Dr. Ruth Lanius, PTSD Research Unit, University of Western Ontario/Department of Psychiatry, University of Western Ontario/School of Rehabilitation Science, McMaster University; Dr. Margaret McKinnon, Department of Psychiatry and Behavioural Neurosciences, McMaster University/Mental Health and Addictions, St. Joseph’s Healthcare Hamilton/ Homewood Research Institute; Captain Alain Pellegroms, Ottawa Fire Service, City of Ottawa; Dr. James M. Thompson, Department of Public Health Sciences, Queen’s University/Canadian Institute for Military and Veteran Health Research; the CRRP committee members and Public Safety Personnel reviewers. Please visit the CRRP website for a full list acknowledging the many valued contributors to the COVID-19 Readiness Resource Project.
Conflicts of interest
The authors declare that they have no conflicts of interest to report.
Authors’ contributions and statement
AH, VT, LSM, SBP and NC informed the concept and contributed to the design, writing, and critical review of this commentary.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Catalogue No, et al. Federal framework on posttraumatic stress disorder. Ottawa (ON); Government of Canada; 2020. 2020 Available from: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/healthy-living/federal-framework-post-traumatic-stress-disorder/pub1-eng.pdf. [Google Scholar]
- CIPSRT. Regina(SK): 2019. Glossary of terms: a shared understanding of the common terms used to describe psychological trauma (version 2.1) Available from: https://www.cipsrt-icrtsp.ca/wp-content/uploads/2020/02/Glossary-of-Terms-Version-2.1.pdf. [Google Scholar]
- Carleton RN, Afifi TO, et al, et al. Exposures to potentially traumatic events among public safety personnel in Canada. Can J Behav Sci. 2019:37–52. [Google Scholar]
- Carleton RN, Afifi TO, Turner S, et al, et al. Mental health training, attitudes toward support, and screening positive for mental disorders. Cogn Behav Ther. 2020;49((1)):55–72. doi: 10.1080/16506073.2019.1575900. [DOI] [PubMed] [Google Scholar]
- Walton M, Murray E, Christian MD, et al. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020:241–7. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R, et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10((7)):1206–12. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp RD, Mellow R, et al. PSP Leadership and mental health. Camp RD, Mellow R. Available from: https://www.youtube.com/watch?v=97-mlI-ugE0. [Google Scholar]
- Government of Canada. Ottawa(ON): Emergency Preparedness [Internet] Available from: https://www.publicsafety.gc.ca/cnt/mrgnc-mngmnt/mrgnc-prprdnss/index-en.aspx. [Google Scholar]
- Perry RW, Lindell MK, et al. Preparedness for emergency response: guidelines for the emergency planning process. Disasters. 2003;27((4)):336–50. doi: 10.1111/j.0361-3666.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- Carleton RN, et al. Into the unknown: a review and synthesis of contemporary models involving uncertainty. J Anxiety Disord. 2016:30–43. doi: 10.1016/j.janxdis.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Koroll S, Wagner J, et al, et al. A prospective assessment of PTSD symptoms using analogue trauma training with nursing students. Can J Behav Sci. 2019;51((3)):181–91. [Google Scholar]
- Becker AL, et al. Center for Infectious Disease Research and Policy. Minneapolis(MN): World Health Assembly addresses pandemic flu [Internet] Available from: https://www.cidrap.umn.edu/news-perspective/2005/05/world-health-assembly-addresses-pandemic-flu. [Google Scholar]
- O’Donnel R, et al. When it comes to training, timing is everything. When it comes to training, timing is everything. HR Dive [Internet] Available from: https://www.hrdive.com/news/when-it-comes-to-training-timing-is-everything/506971/ [Google Scholar]
- Mason R, Pegler C, Weller M, et al. A learning object success story. J Asynchron Learn Netw. 2005;9((1)):97–105. [Google Scholar]
- Rosenbaum L, et al. Facing Covid-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020:1873–5. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- Wu AW, Connors C, GS Jr, et al. COVID-19: peer support and crisis communications strategies to promote institutional resilience. Ann Intern Med. 2020;172((12)):peer support and crisis communications strategies to promote institutional resilience–5. doi: 10.7326/M20-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services. U. 2014 Available from: https://emergency.cdc.gov/cerc/ppt/cerc_2014edition_Copy.pdf. [Google Scholar]
- Lunn PD, Belton CA, Lavin C, McGowan FP, Timmons S, et al. Using behavioral science to help fight the coronavirus. JBPA. 2020;3((1)):1–15. [Google Scholar]
- Decety J, Uzefovsky F, Knafo-Noam A, et al. Empathy as a driver of prosocial behaviour: highly conserved neurobehavioural mechanisms across species. Phil Trans R Soc Lond B Biol Sci [Internet] :20150077–15. doi: 10.1098/rstb.2015.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinman G, Teoh K, et al. Society of Occupational Medicine. London(UK): 2018. What could make a difference to the mental health of UK doctors. Available from: https://www.som.org.uk/sites/som.org.uk/files/What_could_make_a_difference_to_the_mental_health_of_UK_doctors_LTF_SOM.pdf. [Google Scholar]
- Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12((12)):1924–32. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Dunn R, t R, Rubin GJ, Greenberg N, et al. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018:248–57. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- Yassi A, Moore D, Fitzgerald JM, Bigelow P, Hon C, Bryce E, et al. Research gaps in protecting healthcare workers from SARS and other respiratory pathogens: an interdisciplinary, multi-stakeholder, evidence-based approach. J Occup Environ Med. 2005;47((1)):41–50. doi: 10.1097/01.jom.0000150207.18085.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt T, Ripp J, Trockel M, et al. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323((21)):2133–4. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Naushad VA, Bierens JJ, Nishan KP, et al, et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehosp Disaster Med. 2019;34((6)):632–43. doi: 10.1017/S1049023X19004874. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD, et al. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68((5)):748–66. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Ho C, Chee C, Ho R, et al. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49((3)):155–60. [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, et al, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder RG, Leszcz M, Savage D, et al, et al. Applying the lessons of SARS to pandemic influenza. Can J Public Heal. 2008;99((6)):486–8. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury-Jones C, Isham L, et al. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29((13-14)):2047–9. doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G, et al. Mitigating the wider health effects of covid-19 pandemic response. Mitigating the wider health effects of covid-19 pandemic response. BMJ [Internet] :m1557–9. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Myint MT, Zeanah CH, et al. Increased risk for family violence during the COVID-19 pandemic. Increased risk for family violence during the COVID-19 pandemic. Pediatrics [Internet] doi: 10.1542/peds.2020-0982. [DOI] [PubMed] [Google Scholar]
- Unadkat S, Farquhar M, et al. Doctors’ wellbeing: self-care during the covid- 19 pandemic. BMJ [Internet] doi: 10.1136/bmj.m1150. [DOI] [PubMed] [Google Scholar]
- Adams JG, Walls RM, et al. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323((15)):1439–40. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- Bansal P, Bingermann TA, Greenhawt M, et al, et al. Clinician wellness during the COVID-19 pandemic: extraordinary times and unusual challenges for the allergist/immunologist. J Allergy Clin Immunol Pract. 2020;8((6)):1781–90. doi: 10.1016/j.jaip.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


