Abstract
The national prevalence of employment changes after a cancer diagnosis has not been fully documented. Cancer survivors who worked for pay at or since diagnosis (n = 1490) were identified from the 2011, 2016, and 2017 Medical Expenditure Panel Survey and Experiences with Cancer supplement. Analyses characterized employment changes due to cancer and identified correlates of those employment changes. Employment changes were made by 41.3% (95% confidence interval [CI] = 38.0% to 44.6%) of cancer survivors, representing more than 3.5 million adults in the United States. Of these, 75.4% (95% CI = 71.3% to 79.2%) took extended paid time off and 46.1% (95% CI = 41.6% to 50.7%) made other changes, including switching to part-time or to a less demanding job. Cancer survivors who were younger, female, non-White, or multiple races and ethnicities, and younger than age 20 years since last cancer treatment were more likely to make employment changes. Findings highlight the need for patient-provider communication about the effects of cancer and its treatment on employment.
Cancer treatment can lead to functional limitations that interfere with the ability to work (1–4). Job loss, extended absences, and lost productivity are experienced by many cancer survivors, leading to difficulty paying for cancer treatment and financial hardship (5–7). The National Cancer Institute and others have called for more research to prepare health-care providers to assess and address employment limitations and concerns with their patients (8–11).
Many studies of employment outcomes after cancer have been based on convenience or geographically limited samples in the United States or data collected internationally. These studies do not fully estimate the magnitude of employment changes due to cancer in the United States. Cross-sectional data from the 2011, 2016, and 2017 Medical Expenditure Panel Survey (MEPS) and Experiences with Cancer supplement were analyzed (12,13). Cancer survivors were defined as individuals who had been told by a doctor or other health professional that they had cancer or a malignancy of any kind. Extended paid time-off and other employment changes were assessed by asking survivors if they took extended paid time off from work or unpaid time off or made a change to their hours, duties, or employment status at any time since diagnosis and whether those changes were because of cancer. Survivors were then asked whether they took extended paid leave from work and when that leave was taken. Extended time off was defined as more than an occasional day off. Survivors were also asked if they changed from working full- to part-time or to a less demanding job and whether they changed from a set to a flexible work schedule. Changes to career trajectory was assessed with questions asking if survivors decided to not pursue an advancement or promotion or retired earlier than planned because of their cancer, its treatment, or lasting effects. Sociodemographic characteristics and health status were also captured, including survivors’ age, sex, race and ethnicity, marital status, education, cancer type, and number of MEPS priority conditions (14). Survivors who replied they were not currently being treated for cancer (including chemotherapy, radiation therapy, or hormonal therapy) were asked about the number of years since their last cancer treatment.
Eligible respondents worked for pay at or since diagnosis and provided data about employment changes due to cancer (n = 1490). Respondents reporting only nonmelanoma skin cancer were excluded. Descriptive statistics characterized the sample, and multivariable logistic regression identified correlates of extended paid time off or other employment changes, after adjusting for the year respondents participated in the survey and other variables. Regression results are presented as odds ratios with 95% confidence intervals (CIs). Analyses were conducted using SUDAAN 11.0.1 and weighted to account for multistage probability sampling and nonresponse.
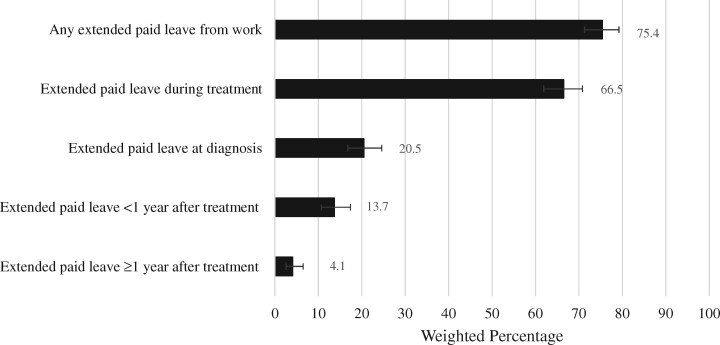
Among cancer survivors who worked for pay at or since diagnosis, 41.3% (95% CI = 38.0% to 44.6%) took extended leave or made other employment changes at some point since diagnosis, representing more than 3.5 million adults in the United States. Among survivors who took extended leave or made other employment changes, 75.4% (95% CI = 71.3% to 79.2%) took extended paid leave from work, with leave occurring most frequently during treatment or diagnosis (Figure 1). Among survivors who made other employment changes, 46.1% (95% CI = 41.6% to 50.7%) made changes to their schedule, role, or career trajectory. Changes included switching from a fixed to a flexible schedule (24.8%, 95% CI = 20.9% to 29.1%), moving from full- to part-time work or to a less demanding job (22.2%, 95% CI = 18.3% to 26.6%), not pursuing a promotion (16.7%, 95% CI = 13.6% to 20.4%), or retiring earlier than planned (15.3%, 95% CI = 12.4% to 18.8%).
Figure 1.
Extended paid leave among cancer survivors participating in the 2011, 2016, and 2017 Medical Expenditure Panel Survey who reported extended paid leave or other employment changes (n = 642)
Table 1 describes cancer survivors who did and did not take extended leave or make other employment changes. Extended leave and other employment changes were more common among survivors aged 51-64 years at the time of the survey, women, and those reporting non-White or multiple races or ethnicities. Compared to survivors who were older than 20 years since last treatment, never received treatment, or missing data on time since last treatment, survivors who were younger than 20 years since last treatment were more likely to take extended leave or make other employment changes.
Table 1.
Characteristics of the sample and predictors of taking extended leave or making other employment changes due to cancera
| Sample characteristics | Extended leave or otheremployment changes due to cancer (n = 642) |
No extended leave and no other employment changes (n = 848) |
Multivariable logistic regression |
|---|---|---|---|
| No. (unadjusted row %) | No. (unadjusted row %) | Adjusted odds ratioc (95% CI) | |
| Age at the time of the survey, y | |||
| ≤50 | 138 (49.1) | 157 (50.9) | 1.49 (1.04 to 2.45) |
| 51-64 | 289 (46.9) | 288 (53.1) | 1.46 (1.12 to 2.04) |
| 65+ | 215 (32.8) | 403 (67.2) | 1.00 (Referent) |
| Sex | |||
| Male | 222 (34.2) | 374 (65.8) | 1.00 (Referent) |
| Female | 420 (46.7) | 474 (53.3) | 1.76 (1.27 to 2.25) |
| Race/ethnicity | |||
| Non-Hispanic White | 451 (38.5) | 684 (61.5) | 1.00 (Referent) |
| Non-White/multiple | 191 (56.3) | 164 (43.7) | 2.01 (1.51 to 2.83) |
| Marital status at the time of the survey | |||
| Married | 379 (42.1) | 476 (57.9) | 1.27 (0.98 to 1.69) |
| Not married | 263 (40.0) | 372 (60.0) | 1.00 (Referent) |
| Education at the time of the survey | |||
| Less than high school degree | 47 (32.8) | 70 (67.2) | 1.00 (Referent) |
| High school graduate/GEDd | 181 (38.8) | 253 (61.2) | 1.36 (0.76 to 2.46) |
| Some college or other degree | 190 (46.9) | 222 (53.1) | 1.83 (1.06 to 3.37) |
| Bachelor’s degree or higher | 224 (40.0) | 303 (60.0) | 1.38 (0.80 to 2.48) |
| No. of cancers | |||
| Single cancer | 593 (41.7) | 778 (58.3) | 1.00 (Referent) |
| Multiple cancers | 49 (36.8) | 70 (63.2) | 0.90 (0.56 to 1.45) |
| Years since last cancer treatment | |||
| <1 | 158 (45.5) | 162 (54.5) | 1.95 (1.26 to 3.03) |
| 1-<3 | 228 (47.4) | 226 (52.6) | 2.56 (1.51 to 4.34) |
| 3-<5 | 70 (52.1) | 64 (47.9) | 1.67 (1.01 to 2.78) |
| 5-20 | 59 (42.7) | 85 (57.3) | 1.67 (1.14 to 2.46) |
| >20/never received treatment/missing | 256 (42.3) | 317 (57.7) | 1.00 (Referent) |
| No. of MEPS priority conditions other than cancerb,c | |||
| 0 | 83 (42.4) | 98 (57.6) | 1.00 (Referent) |
| 1 | 104 (47.4) | 117 (52.6) | 1.35 (0.83 to 2.18) |
| 2+ | 455 (39.8) | 633 (60.2) | 1.22 (0.79 to 1.89) |
| Survey year | |||
| 2011 | 284 (42.2) | 342 (57.8) | 0.89 (0.64 to 1.24) |
| 2016 | 206 (36.7) | 318 (63.3) | 0.71 (0.49 to 1.01) |
| 2017 | 152 (44.6) | 188 (55.4) | 1.00 (Referent) |
Extended leave refers to time off lasting longer than an occasional day. CI = confidence interval; MEPS = Medical Expenditure Panel Survey.
MEPS priority conditions include cancer, hypertension, coronary heart disease, angina, myocardial infarction, other heart disease, high cholesterol, emphysema, diabetes, arthritis, asthma, stroke, joint pain, and chronic bronchitis.
Odds ratios were simultaneously adjusted for survey year and all other variables listed in Table 1.
d General Educational Development.
Cancer-related employment changes are experienced by more than 40% of cancer survivors who were employed at or after diagnosis, equating to more than 3.5 million adults in the United States. Consistent with other research, younger survivors, women, and racial and ethnic minorities were more likely to make employment changes after cancer (6,15). This may be because of their representation in jobs where workers have limited options for a flexible schedule or schedule adjustments (16–18). More recent treatment was associated with a greater likelihood of extended employment changes. This may reflect the relatively good employment outcomes experienced by long-term survivors treated more than 20 years ago.
It is common for cancer survivors to take extended leave during treatment and make other decisions that could adversely impact their career trajectory, including changing to a part-time or less demanding job, foregoing pursuit of a promotion, or retiring early (19,20). Interventions are needed to help survivors navigate cancer and employment responsibilities, mitigate employment disruption, and downstream effects on access to health insurance and financial hardship (15,21). In particular, fostering meaningful communication between survivors, health-care providers, and employers can inform cancer care delivery that accommodate survivors’ employment schedules, access to sick leave, and opportunities for flexible work (8, 22–26).
These findings should be considered in the context of some limitations. Newly diagnosed survivors and those with advanced disease or more lethal cancers are underrepresented in household surveys. Thus, our study likely underestimates the impact of cancer on employment. MEPS does not capture cancer stage or treatment modality, so we were unable to explore employment outcomes by these factors. Because of the small sample size for most cancers, we were also unable to fully explore sociodemographic differences in employment at the level of individual cancer types. However, this study provides population-level data about the prevalence of cancer-related employment changes in the United States, which complements previous work (8).
In conclusion, cancer has wide-ranging impacts on survivors’ work lives. Future research should continue to characterize the nature and trajectory of cancer-related employment changes, especially for understudied populations, and inform interventions to improve employment outcomes throughout treatment and survivorship care.
Funding
Not applicable.
Notes
Disclosures: The authors have no conflicts of interest to disclose.
Disclaimers: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Cancer Institute or the Centers for Disease Control and Prevention.
Availability of data: The data that supports the findings of this study are publicly available from the Agency for Healthcare Research and Quality at https://www.meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp.
Author contributions: EEK: Conceptualization; Writing—original draft; Writing—review & editing. TSM: Data curation; Formal analysis; Writing—original draft; Writing—review & editing. KSV: Conceptualization; Writing—original draft; Writing—review & editing. JS: Conceptualization; Writing—original draft; Writing—review & editing. JKT: Conceptualization; Writing—original draft; Writing—review & editing. MPB: Conceptualization; Writing—original draft; Writing—review & editing. XH: Conceptualization; Writing—original draft; Writing—review & editing. JQ: Conceptualization; Writing—original draft; Writing—review & editing. KRY: Conceptualization; Writing—original draft; Writing—review & editing.
References
- 1. Fossa SD, Vassilopoulou-Sellin R, Dahl AA.. Long term physical sequelae after adult-onset cancer. J Cancer Surviv. 2008;2(1):3–11. [DOI] [PubMed] [Google Scholar]
- 2. Duijts SF, van Egmond MP, Spelten E, van Muijen P, Anema JR, van der Beek AJ.. Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psycho-oncology. 2014;23(5):481–492. [DOI] [PubMed] [Google Scholar]
- 3. Stone DS, Ganz PA, Pavlish C, Robbins WA.. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. 2017;11(6):765–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tavan H, Azadi A, Veisani Y.. Return to work in cancer patients: a systematic review and meta-analysis. Indian J Palliat Care. 2019;25(1):147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Altice CK, Banegas MP, Tucker-Seeley RD, Yabroff KR.. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109(2):djw205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol/Hematol. 2011;77(2):109–130. [DOI] [PubMed] [Google Scholar]
- 7. Zajacova A, Dowd JB, Schoeni RF, Wallace RB.. Employment and income losses among cancer survivors: estimates from a national longitudinal survey of American families. Cancer. 2015;121(24):4425–4432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. de Moor JS, Alfano CM, Kent EE, et al. Recommendations for research and practice to improve work outcomes among cancer survivors. J Natl Cancer Inst. 2018;110(10):1041–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yagil D, Eshed-Lavi N, Carel R, Cohen M.. Health care professionals’ perspective on return to work in cancer survivors. Psycho-oncology. 2018;27(4):1206–1212. [DOI] [PubMed] [Google Scholar]
- 10. Bains M, Yarker J, Amir Z, Wynn P, Munir F.. Helping cancer survivors return to work: what providers tell us about the challenges in assisting cancer patients with work questions. J Occup Rehabil. 2012;22(1):71–77. [DOI] [PubMed] [Google Scholar]
- 11. Murphy KM, Nguyen V, Shin K, Sebastian-Deutsch A, Frieden L.. Health care professionals and the employment-related needs of cancer survivors. J Occup Rehabil. 2017;27(2):296–305. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality. MEPS-HC Panel Design and Collection Process . https://meps.ahrq.gov/mepsweb/survey_comp/hc_data_collection.jsp. Accessed April 11, 2019.
- 13. Banegas MP, Guy GP Jr, de Moor JS, et al. For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff (Project Hope). 2016;35(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. https://meps.ahrq.gov/mepsweb/. Accessed April 11, 2019.
- 15. Yabroff KR, Zhao J, Zheng Z, Rai A, Han X.. Medical financial hardship among cancer survivors in the United States: What do we know? What do we need to know? Cancer Epidemiol Biomarkers Prev. 2018;27(12):1389–1397. [DOI] [PubMed] [Google Scholar]
- 16. Shaw E, Hegewisch A, Williams-Baron E, Gault B.. Undervalued and Underpaid in America: Women in Low-Wage, Female-Dominated Jobs. Institute for Women’s Policy Research; 2016. IWPR #D508. [Google Scholar]
- 17. Byars-Winston A, Fouad N, Wen Y.. Race/ethnicity and sex in U.S. occupations, 1970-2010: implications for research, practice, and policy. J Vocat Behav. 2015;87:54–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Bureau of Labor Statistics. Characteristics of minimum wage workers, 2017; 2018. Report 1072.
- 19. Stergiou-Kita M, Pritlove C, Kirsh B.. The “Big C”-stigma, cancer, and workplace discrimination. J Cancer Surviv. 2016;10(6):1035–1050. [DOI] [PubMed] [Google Scholar]
- 20. Stepanikova I, Powroznik K, Cook KS, Tierney DK, Laport GG.. Exploring long-term cancer survivors’ experiences in the career and financial domains: interviews with hematopoietic stem cell transplantation recipients. J Psychosoc Oncol. 2016;34(1-2):2–27. [DOI] [PubMed] [Google Scholar]
- 21. Garfield R, Rudowitz R, Musumeci M.. Implications of a Medicaid work requirement: national estimates of potential coverage losses. In: Issue Brief. Kaiser Family Foundation. [Google Scholar]
- 22. Walling A, Lorenz KA, Dy SM, et al. Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008;26(23):3896–3902. [DOI] [PubMed] [Google Scholar]
- 23. Alfano CM, Kent EE, Padgett LS, Grimes M, de Moor JS.. Making cancer rehabilitation services work for cancer patients: recommendations for research and practice to improve employment outcomes. PM & R. 2017;9(9 Suppl 2):S398–S406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. de Boer AG, Taskila TK, Tamminga SJ, Feuerstein M, Frings-Dresen MH, Verbeek JH.. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015;2015(9):Cd007569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blinder V, Eberle C, Patil S, Gany FM, Bradley CJ.. Women with breast cancer who work for accommodating employers more likely to retain jobs after treatment. Health Aff (Project Hope). 2017;36(2):274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stergiou-Kita M, Pritlove C, van Eerd D, et al. The provision of workplace accommodations following cancer: survivor, provider, and employer perspectives. J Cancer Surviv. 2016;10(3):489–504. [DOI] [PubMed] [Google Scholar]