Long-standing social inequities and health disparities have resulted in increased risk for coronavirus disease 2019 (COVID-19) infection, severe illness, and death among racial and ethnic minority populations. The Health Resources and Services Administration (HRSA) Health Center Program supports nearly 1,400 health centers that provide comprehensive primary health care* to approximately 30 million patients in 13,000 service sites across the United States.† In 2019, 63% of HRSA health center patients who reported race and ethnicity identified as members of racial ethnic minority populations (1). Historically underserved communities and populations served by health centers have a need for access to important information and resources for preventing exposure to SARS-CoV-2, the virus that causes COVID-19, to testing for those at risk, and to follow-up services for those with positive test results.§ During the COVID-19 public health emergency, health centers¶ have provided and continue to provide testing and follow-up care to medically underserved populations**; these centers are capable of reaching areas disproportionately affected by the pandemic.†† HRSA administers a weekly, voluntary Health Center COVID-19 Survey§§ to track health center COVID-19 testing capacity and the impact of COVID-19 on operations, patients, and personnel. Potential respondents can include up to 1,382 HRSA-funded health centers.¶¶ To assess health centers’ capacity to reach racial and ethnic minority groups at increased risk for COVID-19 and to provide access to testing, CDC and HRSA analyzed survey data for the weeks June 5–October 2, 2020*** to describe all patients tested (3,194,838) and those who received positive SARS-CoV-2 test results (308,780) by race/ethnicity and state of residence. Among persons with known race/ethnicity who received testing (2,506,935), 36% were Hispanic/Latino (Hispanic), 38% were non-Hispanic White (White), and 20% were non-Hispanic Black (Black); among those with known race/ethnicity with positive test results, 56% were Hispanic, 24% were White, and 15% were Black. Improving health centers’ ability to reach groups at increased risk for COVID-19 might reduce transmission by identifying cases and supporting contact tracing and isolation. Efforts to improve coordination of COVID-19 response-related activities between state and local public health departments and HRSA-funded health centers can increase access to testing and follow-up care for populations at increased risk for COVID-19.
HRSA administers a weekly voluntary Health Center COVID-19 Survey to track health center COVID-19 testing capacity and the impact of COVID-19 on operations, patients, and staff members. The 1,382 health centers asked to complete the survey are located in all 50 states, the District of Columbia (DC), and five territories and freely associated states.††† This analysis used survey data from the weeks ending June 5–October 2, 2020, to describe the patient population and, among all patients who received testing for SARS-CoV-2 with viral tests (i.e., polymerase chain reaction and antigen tests), the numbers and proportions of persons with tests and positive results by race/ethnicity and state of residence. State survey response rates ranged from 68% to 80% among health centers. Proportions of patients receiving SARS-CoV-2 tests and positive test results included unreported race/ethnicity as a separate category.
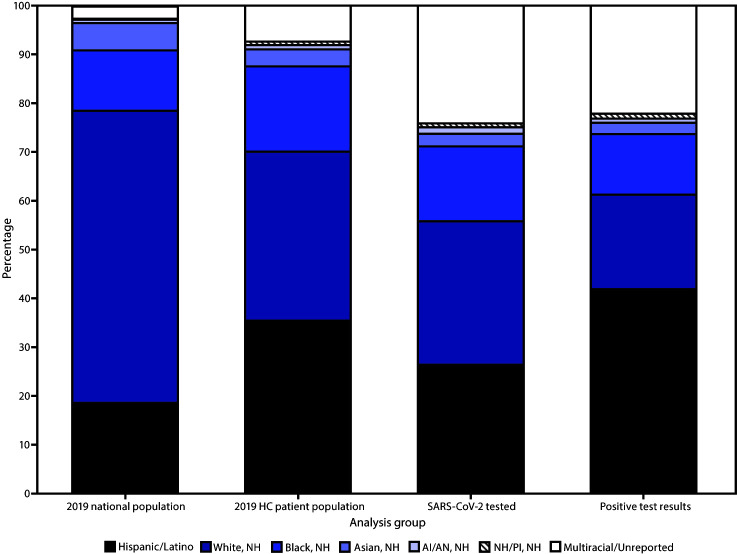
As reported in the HRSA Uniform Data System in 2019, HRSA-funded health centers reported that 35% of their national patient population was White, 35% Hispanic,§§§ 18% Black, 4% Asian, 1% American Indian/Alaska Native (AI/AN), 1% Native Hawaiian/Other Pacific Islander, and 1.3% multiracial persons; race/ethnicity was not reported for 6% of the patient population (Figure) (1). By comparison, the 2019 American Community Survey¶¶¶ estimated that the U.S. population comprises 60% White, 18% Hispanic, 12% Black, 6% Asian, 1% AI/AN, 0.2% Native Hawaiian/Other Pacific Islander, and 3% multiracial persons.
FIGURE.
Racial/ethnic distribution of 2019 national* and Health Resources and Services Administration (HRSA)–funded health center† patient populations§ and persons who received testing and had positive SARS-CoV-2 test results¶ — Health Center COVID-19 Survey, United States, June 5–October 2, 2020
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease 2019; HC = health center; NH/PI = Native Hawaiian/Other Pacific Islander; NH = non-Hispanic.
* Data from the 2019 American Community Survey (https://data.census.gov/cedsci/table?d=ACS%201-Year%20Estimates%20Data%20Profiles&tid=ACSDP1Y2019. DP05&hidePreview=false). Data include non-Hispanic NH/PI (0.2%), not visible in figure and do not include other race (0.3%). Persons with multiracial or unreported race/ethnicity have an unreported or non-Hispanic ethnicity.
† HRSA–funded health centers include both Federally Qualified Health Centers (FQHCs) and Health Center Program Look-Alikes (i.e, meets all Health Care Center Program requirements but does not receive federal funding). During the COVID-19 pandemic, HRSA provided one-time COVID-19 funding to FQHCs and Health Center Look-Alikes to purchase, administer, and expand capacity for testing to monitor and suppress COVID-19 testing and response-related activities.
§ HRSA 2019 Uniform Data System. https://data.hrsa.gov/tools/data-reporting/program-data/national.
¶ HRSA COVID-19 Survey, June 5–October 2, 2020. Data for the number tested or the number tested positive are aggregated by health centers before submission and cannot be deduplicated, which might inflate or misrepresent the number of patients tested or who had positive test results.
During June 5–October 2, 2020, health centers responding to the survey reported that 3,194,838 patients received testing and 308,780 had positive SARS-CoV-2 test results. Compared to other jurisdictions, Texas reported the highest number of patients who received testing (353,081; 11%), and California reported the highest number of patients who had positive test results (46,113; 15%). Based on data reported to the Health Center COVID-19 Survey, White and Hispanic patients each accounted for 29% of patients who received testing for SARS-CoV-2 (Table 1) and, among patients who received positive test results, 19% were White and 45% were Hispanic (Table 2). Overall, race was not reported for 22% (687,903) of patients tested and 19% of patients with positive test results (57,208); 1% (26,386) of patients receiving testing and 1% (2,378) of patients with positive test results were multiracial. In Puerto Rico, 96% of patients receiving testing were Hispanic; among other jurisdictions, the highest proportions of patients receiving testing who were Hispanic were in Nevada (9,990; 56%) and New Mexico (11,705; 56%). Compared with all other jurisdictions, California reported the most Hispanic patients who received testing (186,034) and the most positive test results among Hispanic patients (33,310; 18%). Among those with positive test results, Puerto Rico reported the largest proportion of Hispanic patients (2,095; 98%) and New Mexico the second highest proportion (531; 73%). Nationally, Black patients accounted for 15% of patients receiving testing and 12% of those who received positive test results. Mississippi reported the highest proportion of patients who received testing who were Black (25,850; 67%) and the highest proportion of those who had positive test results who were Black (2,348; 69%). Georgia reported the largest number of tests conducted (42,889; 43%) and positive test results (4,204; 32%) among Black patients.
TABLE 1. Viral testing for SARS-CoV-2,* by race/ethnicity and jurisdiction† — Health Center COVID-19 Survey, United States, June 5–October 2, 2020.
| Jurisdiction | No.§ of FQHCs¶ | Response range** (%) | Total no. patients tested†† | Race/Ethnicity, no. tested (row %) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hispanic/Latino | White, NH | Black, NH | Asian, NH | AI/AN, NH | NH/PI, NH | Multiracial | Unreported | ||||
|
United States
|
1,382–1,376
|
68–80
|
3,194,838
|
913,718 (29)
|
941,017 (29)
|
491,311 (15)
|
77,528 (2)
|
36,837 (1)
|
5,161 (—)
|
26,386 (1)
|
687,903 (22)
|
| Alabama |
17 |
59–94 |
46,146 |
3,393 (7) |
16,089 (35) |
21,262 (46) |
183 (—) |
139 (—) |
4 (—) |
241 (1) |
4,800 (10) |
| Alaska |
27 |
44–74 |
57,147 |
1,788 (3) |
11,510 (20) |
528 (1) |
967 (2) |
20,785 (36) |
83 (—) |
362 (1) |
21,080 (37) |
| American Samoa |
1 |
0–100 |
1,567 |
104 (7) |
46 (3) |
0 (—) |
55 (4) |
12 (1) |
0 (—) |
2 (—) |
8 (1) |
| Arizona |
23 |
65–83 |
53,455 |
27,220 (51) |
15,584 (29) |
1,509 (3) |
335 (1) |
1,741 (3) |
50 (—) |
392 (1) |
6,573 (12) |
| Arkansas |
12 |
50–100 |
51,488 |
7,855 (15) |
24,988 (49) |
13,061 (25) |
243 (—) |
152 (—) |
21 (—) |
189 (—) |
4,169 (8) |
| California |
175–178 |
59–74 |
336,454 |
186,034 (55) |
51,114 (15) |
26,371 (8) |
20,103 (6) |
949 (—) |
634 (—) |
4,891 (1) |
45,217 (13) |
| Colorado |
19 |
68–95 |
59,401 |
24,702 (42) |
19,064 (32) |
5,165 (9) |
1,166 (2) |
324 (1) |
31 (—) |
791 (1) |
8,123 (14) |
| Connecticut |
16 |
56–94 |
83,507 |
27,872 (33) |
15,803 (19) |
8,258 (10) |
1,190 (1) |
218 (—) |
20 (—) |
349 (—) |
29,613 (35) |
| Delaware |
3 |
33–100 |
2,356 |
894 (38) |
466 (20) |
850 (36) |
31 (1) |
9 (—) |
4 (—) |
14 (1) |
88 (4) |
| District of Columbia |
8 |
63–100 |
18,438 |
5,632 (31) |
1,628 (9) |
8,554 (46) |
274 (1) |
30 (—) |
2 (—) |
89 (—) |
2,215 (12) |
| Federated States of Micronesia |
4 |
25–100 |
198 |
0 (—) |
0 (—) |
0 (—) |
54 (27) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Florida |
47 |
62–87 |
257,119 |
97,542 (38) |
51,704 (20) |
38,483 (15) |
1,868 (1) |
189 (—) |
44 (—) |
2,431 (1) |
64,665 (25) |
| Georgia |
35 |
60–91 |
100,909 |
15,410 (15) |
32,664 (32) |
42,889 (43) |
1,119 (1) |
67 (—) |
11 (—) |
862 (1) |
7,861 (8) |
| Guam |
1 |
0–100 |
8,574 |
31 (—) |
199 (2) |
38 (—) |
2,572 (30) |
9 (—) |
4 (—) |
432 (5) |
268 (3) |
| Hawaii |
14 |
36–86 |
8,894 |
850 (10) |
911 (10) |
91 (1) |
1,325 (15) |
13 (—) |
2,833 (32) |
286 (3) |
1,081 (12) |
| Idaho |
14 |
71–100 |
12,111 |
3,014 (25) |
6,281 (52) |
168 (1) |
100 (1) |
1,028 (8) |
25 (—) |
26 (—) |
1,460 (12) |
| Illinois |
45 |
64–82 |
162,663 |
51,534 (32) |
37,781 (23) |
22,276 (14) |
3,097 (2) |
217 (—) |
44 (—) |
676 (—) |
46,966 (29) |
| Indiana |
27 |
48–78 |
20,639 |
6,031 (29) |
5,570 (27) |
2,035 (10) |
967 (5) |
34 (—) |
3 (—) |
112 (1) |
5,876 (28) |
| Iowa |
14 |
64–93 |
30,891 |
5,292 (17) |
14,786 (48) |
1,511 (5) |
447 (1) |
222 (1) |
16 (—) |
235 (1) |
8,357 (27) |
| Kansas |
19 |
53–100 |
25,472 |
6,582 (26) |
13,631 (54) |
1,972 (8) |
326 (1) |
336 (1) |
93 (—) |
212 (1) |
2,264 (9) |
| Kentucky |
25 |
76–96 |
64,494 |
3,453 (5) |
51,839 (80) |
4,141 (6) |
446 (1) |
36 (—) |
15 (—) |
506 (1) |
4,017 (6) |
| Louisiana |
36 |
61–81 |
48,007 |
5,297 (11) |
16,396 (34) |
21,333 (44) |
487 (1) |
143 (—) |
39 (—) |
323 (1) |
3,968 (8) |
| Maine |
18 |
50–89 |
9,049 |
600 (7) |
6,614 (73) |
515 (6) |
40 (—) |
40 (—) |
7 (—) |
43 (—) |
1,189 (13) |
| Marshall Islands |
1 |
0–100 |
121 |
0 (—) |
0 (—) |
0 (—) |
1 (1) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Maryland |
17 |
47–82 |
8,898 |
2,696 (30) |
1,824 (20) |
2,629 (30) |
117 (1) |
248 (3) |
3 (—) |
135 (2) |
1,242 (14) |
| Massachusetts |
37–38 |
59–89 |
153,411 |
51,639 (34) |
52,813 (34) |
16,444 (11) |
5,326 (3) |
181 (—) |
61 (—) |
817 (1) |
25,712 (17) |
| Michigan |
39 |
51–79 |
99,960 |
12,870 (13) |
53,804 (54) |
13,622 (14) |
1,799 (2) |
305 (—) |
46 (—) |
1,040 (1) |
16,412 (16) |
| Minnesota |
16 |
56–81 |
16,645 |
2,828 (17) |
5,093 (31) |
3,627 (22) |
1,178 (7) |
794 (5) |
5 (—) |
32 (—) |
3,077 (18) |
| Mississippi |
20 |
65–95 |
38,843 |
3,411 (9) |
8,300 (21) |
25,850 (67) |
218 (1) |
59 (—) |
9 (—) |
326 (1) |
605 (2) |
| Missouri |
28–29 |
66–90 |
78,075 |
7,414 (9) |
36,275 (46) |
16,802 (22) |
677 (1) |
207 (—) |
57 (—) |
567 (1) |
15,895 (20) |
| Montana |
14 |
43–86 |
18,377 |
368 (2) |
7,522 (41) |
31 (—) |
18 (—) |
441 (2) |
7 (—) |
60 (—) |
9,928 (54) |
| Nebraska |
7 |
57–86 |
9,224 |
3,585 (39) |
2,167 (23) |
2,008 (22) |
896 (10) |
40 (—) |
6 (—) |
97 (1) |
422 (5) |
| Nevada |
8 |
38–88 |
17,827 |
9,990 (56) |
4,102 (23) |
938 (5) |
1,145 (6) |
47 (—) |
157 (1) |
94 (1) |
1,322 (7) |
| New Hampshire |
10 |
70–100 |
3,535 |
936 (26) |
2,140 (61) |
88 (2) |
80 (2) |
6 (—) |
3 (—) |
10 (—) |
272 (8) |
| New Jersey |
23–24 |
33–67 |
51,393 |
26,433 (51) |
9,698 (19) |
7,173 (14) |
603 (1) |
62 (—) |
43 (—) |
398 (1) |
6,887 (13) |
| New Mexico |
16 |
75–100 |
20,857 |
11,705 (56) |
4,115 (20) |
295 (1) |
98 (—) |
1,427 (7) |
12 (—) |
208 (1) |
2,985 (14) |
| New York |
63 |
48–67 |
204,075 |
31,877 (16) |
32,798 (16) |
24,734 (12) |
5,972 (3) |
194 (—) |
30 (—) |
1,606 (1) |
106,749 (52) |
| North Carolina |
39 |
46–69 |
65,685 |
14,505 (22) |
18,118 (28) |
22,130 (34) |
661 (1) |
524 (1) |
66 (—) |
334 (1) |
9,326 (14) |
| North Dakota |
4 |
75–100 |
5,003 |
199 (4) |
2,425 (48) |
385 (8) |
170 (3) |
300 (6) |
9 (—) |
35 (1) |
1,476 (30) |
| Northern Mariana Islands |
1 |
0–100 |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Ohio |
51 |
67–82 |
72,400 |
7,604 (11) |
37,561 (52) |
13,461 (19) |
1,216 (2) |
443 (1) |
39 (—) |
550 (1) |
11,418 (16) |
| Oklahoma |
21 |
52–95 |
13,147 |
2,833 (22) |
5,284 (40) |
1,151 (9) |
86 (1) |
480 (4) |
16 (—) |
145 (1) |
3,117 (24) |
| Oregon |
30 |
73–90 |
17,782 |
6,771 (38) |
7,471 (42) |
474 (3) |
400 (2) |
686 (4) |
40 (—) |
145 (1) |
1,697 (10) |
| Palau |
1 |
0–100 |
1,612 |
0 (—) |
254 (16) |
4 (—) |
334 (21) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Pennsylvania |
43 |
67–91 |
54,143 |
9,563 (18) |
22,464 (41) |
13,911 (26) |
2,549 (5) |
118 (—) |
13 (—) |
651 (1) |
4,745 (9) |
| Puerto Rico |
21–22 |
73–91 |
28,909 |
27,709 (96) |
134 (—) |
5 (—) |
0 (—) |
3 (—) |
0 (—) |
260 (1) |
798 (3) |
| Rhode Island |
8 |
63–100 |
22,637 |
10,653 (47) |
4,907 (22) |
2,120 (9) |
388 (2) |
55 (—) |
9 (—) |
241 (1) |
4,228 (19) |
| South Carolina |
23 |
70–91 |
63,976 |
4,705 (7) |
15,311 (24) |
36,609 (57) |
686 (1) |
124 (—) |
12 (—) |
321 (1) |
6,097 (10) |
| South Dakota |
4 |
50–100 |
5,966 |
1,194 (20) |
3,536 (59) |
67 (1) |
223 (4) |
283 (5) |
14 (—) |
16 (—) |
631 (11) |
| Tennessee |
29 |
59–83 |
85,712 |
8,496 (10) |
53,673 (63) |
8,411 (10) |
430 (1) |
63 (—) |
53 (—) |
1,018 (1) |
13,549 (16) |
| Texas |
72 |
69–85 |
353,081 |
109,844 (31) |
55,515 (16) |
42,531 (12) |
10,324 (3) |
766 (—) |
170 (—) |
1,510 (—) |
132,353 (37) |
| U.S. Virgin Islands |
2 |
0–50 |
365 |
100 (27) |
45 (12) |
200 (55) |
0 (—) |
0 (—) |
0 (—) |
20 (5) |
0 (—) |
| Utah |
13 |
62–92 |
13,870 |
5,451 (39) |
4,663 (34) |
209 (2) |
65 (—) |
622 (4) |
26 (—) |
125 (1) |
2,671 (19) |
| Vermont |
11 |
64–100 |
5,017 |
143 (3) |
4,415 (88) |
42 (1) |
41 (1) |
16 (—) |
0 (—) |
10 (—) |
348 (7) |
| Virginia |
26 |
65–88 |
35,346 |
8,234 (23) |
15,027 (43) |
6,979 (20) |
381 (1) |
140 (—) |
4 (—) |
211 (1) |
4,350 (12) |
| Washington |
27 |
70–89 |
98,481 |
34,877 (35) |
30,972 (31) |
3,647 (4) |
3,844 (4) |
1,317 (1) |
240 (—) |
1,664 (2) |
20,566 (21) |
| West Virginia |
28 |
61–89 |
47,084 |
2,864 (6) |
39,019 (83) |
1,748 (4) |
48 (—) |
18 (—) |
12 (—) |
221 (—) |
3,153 (7) |
| Wisconsin |
16 |
69–100 |
23,098 |
10,532 (46) |
4,309 (19) |
1,962 (8) |
153 (1) |
150 (1) |
15 (—) |
33 (—) |
5,932 (26) |
| Wyoming | 6 | 33–83 | 1,304 | 559 (43) | 595 (46) | 14 (1) | 6 (—) | 25 (2) | 1 (—) | 22 (2) | 82 (6) |
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease 2019; FQHC = Federally Qualified Health Center; NH/PI = Native Hawaiian/Other Pacific Islander; NH = non-Hispanic.
* SARS-CoV-2 viral tests include polymerase chain reaction and antigen tests.
† The Health Resources Services Administration (HRSA) funds health centers in all 50 states, the District of Columbia, and the following U.S. territories and freely associated states: American Samoa, Federated States of Micronesia, Guam, Northern Mariana Islands, Marshall Islands, Puerto Rico, and U.S. Virgin Islands.
§ In June 2020, the number of HRSA-fund health centers was 1,382. By September, the number of HRSA-funded centers decreased to 1,376, by three in California and by one each in Massachusetts, Missouri, New Jersey, and Puerto Rico. By October, the number of Puerto Rico’s HRSA-funded health centers increased by one.
¶ FQHCs receive HRSA Health Center Program federal grant funding to improve the health of underserved populations
** The weekly response rate was calculated using the number of health centers that responded to the survey as the numerator and number of current HRSA-funded health centers as the denominator. The response range represents the lowest response rate and the highest response rate nationally and by state during June 5–October 2, 2020.
†† Data for the number of persons receiving testing or who had positive test results are aggregated by health center before submission and cannot be deduplicated, which might inflate or misrepresent the number of patients who received testing or who had positive test results.
TABLE 2. Positive viral tests for SARS-CoV-2,* by race/ethnicity and jurisdiction† — Health Center COVID-19 Survey, United States, June 5–October 2, 2020.
| Jurisdiction | Total positive§ | Race/Ethnicity, no. positive (row %) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Hispanic/Latino | White, NH | Black, NH | Asian, NH | AI/AN, NH | NH/PI, NH | Multiracial | Unreported | ||
|
United States
|
308,780
|
140,462 (45)
|
59,959 (19)
|
38,385 (12)
|
6,792 (2)
|
1,262 (—)
|
473 (—)
|
2,378 (1)
|
57,208 (19)
|
| Alabama |
5,097 |
710 (14) |
1,469 (29) |
2,296 (45) |
23 (—) |
14 (—) |
0 (—) |
32 (1) |
542 (11) |
| Alaska |
961 |
81 (8) |
167 (17) |
31 (3) |
18 (2) |
253 (26) |
0 (—) |
7 (1) |
399 (42) |
| American Samoa |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Arizona |
8,297 |
4,719 (57) |
1,857 (22) |
243 (3) |
25 (—) |
178 (2) |
9 (—) |
70 (1) |
1,190 (14) |
| Arkansas |
5,946 |
1,808 (30) |
1,738 (29) |
883 (15) |
14 (—) |
13 (—) |
7 (—) |
10 (—) |
886 (15) |
| California |
46,113 |
33,310 (72) |
4,075 (9) |
2,458 (5) |
997 (2) |
76 (—) |
63 (—) |
572 (1) |
4,470 (10) |
| Colorado |
4,656 |
3,234 (69) |
721 (15) |
142 (3) |
49 (1) |
14 (—) |
3 (—) |
10 (—) |
480 (10) |
| Connecticut |
3,904 |
2,032 (52) |
221 (6) |
229 (6) |
33 (1) |
2 (—) |
1 (—) |
3 (—) |
1,379 (35) |
| Delaware |
244 |
144 (59) |
19 (8) |
71 (29) |
4 (2) |
2 (1) |
0 (—) |
0 (—) |
4 (2) |
| District of Columbia |
1,697 |
737 (43) |
82 (5) |
696 (41) |
16 (1) |
4 (—) |
0 (—) |
6 (—) |
154 (9) |
| Federated States of Micronesia |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Florida |
43,859 |
17,913 (41) |
3,500 (8) |
3,347 (8) |
131 (—) |
9 (—) |
2 (—) |
142 (—) |
18,802 (43) |
| Georgia |
13,130 |
2,984 (23) |
4,213 (32) |
4,204 (32) |
69 (1) |
6 (—) |
2 (—) |
48 (—) |
1,597 (12) |
| Guam |
633 |
2 (—) |
5 (1) |
0 (—) |
222 (35) |
0 (—) |
0 (—) |
35 (6) |
2 (—) |
| Hawaii |
907 |
63 (7) |
27 (3) |
3 (—) |
144 (16) |
1 (—) |
234 (26) |
20 (2) |
78 (9) |
| Idaho |
2,938 |
1,185 (40) |
991 (34) |
119 (4) |
55 (2) |
94 (3) |
18 (1) |
9 (—) |
467 (16) |
| Illinois |
16,752 |
6,993 (42) |
3,571 (21) |
2,074 (12) |
151 (1) |
16 (—) |
1 (—) |
55 (—) |
3,874 (23) |
| Indiana |
3,274 |
1,372 (42) |
600 (18) |
238 (7) |
152 (5) |
2 (—) |
0 (—) |
12 (—) |
897 (27) |
| Iowa |
3,634 |
1,011 (28) |
1,550 (43) |
141 (4) |
68 (2) |
14 (—) |
1 (—) |
25 (1) |
821 (23) |
| Kansas |
2,810 |
1,345 (48) |
986 (35) |
177 (6) |
27 (1) |
30 (1) |
5 (—) |
3 (—) |
226 (8) |
| Kentucky |
4,191 |
579 (14) |
2,884 (69) |
306 (7) |
35 (1) |
0 (—) |
2 (—) |
22 (1) |
361 (9) |
| Louisiana |
4,922 |
734 (15) |
1,826 (37) |
2,088 (42) |
29 (1) |
11 (—) |
0 (—) |
37 (1) |
191 (4) |
| Maine |
119 |
28 (24) |
42 (35) |
43 (36) |
0 (—) |
0 (—) |
0 (—) |
1 (1) |
5 (4) |
| Marshall Islands |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Maryland |
1,472 |
763 (52) |
148 (10) |
410 (28) |
24 (2) |
13 (1) |
1 (—) |
19 (1) |
93 (6) |
| Massachusetts |
10,029 |
6,755 (67) |
1,167 (12) |
696 (7) |
312 (3) |
1 (—) |
1 (—) |
50 (—) |
1,031 (10) |
| Michigan |
3,931 |
1,060 (27) |
1,455 (37) |
460 (12) |
65 (2) |
9 (—) |
2 (—) |
48 (1) |
828 (21) |
| Minnesota |
2,194 |
991 (45) |
219 (10) |
527 (24) |
190 (9) |
22 (1) |
1 (—) |
2 (—) |
241 (11) |
| Mississippi |
3,412 |
255 (7) |
686 (20) |
2,348 (69) |
23 (1) |
7 (—) |
1 (—) |
29 (1) |
54 (2) |
| Missouri |
5,770 |
1,319 (23) |
2,310 (40) |
1,090 (19) |
48 (1) |
8 (—) |
0 (—) |
23 (—) |
916 (16) |
| Montana |
865 |
26 (3) |
323 (37) |
2 (—) |
1 (—) |
30 (3) |
1 (—) |
2 (—) |
480 (55) |
| Nebraska |
1,749 |
1,171 (67) |
160 (9) |
138 (8) |
131 (7) |
2 (—) |
0 (—) |
6 (—) |
140 (8) |
| Nevada |
2,893 |
2,029 (70) |
325 (11) |
121 (4) |
127 (4) |
7 (—) |
21 (1) |
14 (—) |
245 (8) |
| New Hampshire |
139 |
91 (65) |
32 (23) |
8 (6) |
4 (3) |
0 (—) |
0 (—) |
0 (—) |
4 (3) |
| New Jersey |
3,275 |
1,080 (33) |
266 (8) |
287 (9) |
40 (1) |
0 (—) |
0 (—) |
16 (—) |
1,584 (48) |
| New Mexico |
729 |
531 (73) |
89 (12) |
8 (1) |
2 (—) |
23 (3) |
0 (—) |
7 (1) |
66 (9) |
| New York |
10,697 |
1,404 (13) |
1,382 (13) |
1,507 (14) |
1,775 (17) |
6 (—) |
3 (—) |
75 (1) |
4,528 (42) |
| North Carolina |
8,467 |
3,922 (46) |
1,846 (22) |
1,623 (19) |
63 (1) |
53 (1) |
8 (—) |
40 (—) |
908 (11) |
| North Dakota |
402 |
13 (3) |
173 (43) |
49 (12) |
17 (4) |
8 (2) |
0 (—) |
0 (—) |
142 (35) |
| Northern Mariana Islands |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Ohio |
4,794 |
1,014 (21) |
1,881 (39) |
1,197 (25) |
88 (2) |
2 (—) |
21 (—) |
33 (1) |
556 (12) |
| Oklahoma |
1,264 |
500 (40) |
419 (33) |
70 (6) |
14 (1) |
46 (4) |
1 (—) |
10 (1) |
197 (16) |
| Oregon |
1,785 |
1,011 (57) |
266 (15) |
79 (4) |
346 (19) |
14 (1) |
1 (—) |
3 (—) |
62 (3) |
| Palau |
0 |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Pennsylvania |
3,573 |
1,105 (31) |
954 (27) |
719 (20) |
357 (10) |
7 (—) |
1 (—) |
87 (2) |
333 (9) |
| Puerto Rico |
2,137 |
2,095 (98) |
5 (—) |
5 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
32 (1) |
| Rhode Island |
2,808 |
1,943 (69) |
250 (9) |
196 (7) |
35 (1) |
0 (—) |
2 (—) |
19 (1) |
360 (13) |
| South Carolina |
5,399 |
1,087 (20) |
1,075 (20) |
2,602 (48) |
18 (—) |
18 (—) |
1 (—) |
16 (—) |
568 (11) |
| South Dakota |
857 |
167 (19) |
542 (63) |
5 (1) |
65 (8) |
18 (2) |
1 (—) |
1 (—) |
58 (7) |
| Tennessee |
13,014 |
2,726 (21) |
6,116 (47) |
1,544 (12) |
114 (1) |
22 (—) |
6 (—) |
432 (3) |
2,038 (16) |
| Texas |
22,444 |
15,079 (67) |
2,588 (12) |
1,725 (8) |
397 (2) |
47 (—) |
2 (—) |
180 (1) |
2,419 (11) |
| U.S. Virgin Islands |
2 |
0 (—) |
0 (—) |
2 (100) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
0 (—) |
| Utah |
1,597 |
1,099 (69) |
284 (18) |
20 (1) |
6 (—) |
48 (3) |
1 (—) |
17 (1) |
116 (7) |
| Vermont |
35 |
2 (6) |
20 (57) |
4 (11) |
5 (14) |
0 (—) |
0 (—) |
0 (—) |
4 (11) |
| Virginia |
3,966 |
1,684 (42) |
1,272 (32) |
633 (16) |
23 (1) |
6 (—) |
0 (—) |
17 (—) |
331 (8) |
| Washington |
9,601 |
6,115 (64) |
1,295 (13) |
265 (3) |
219 (2) |
92 (1) |
39 (—) |
95 (1) |
1,289 (13) |
| West Virginia |
1,792 |
249 (14) |
1,363 (76) |
78 (4) |
2 (—) |
0 (—) |
0 (—) |
8 (—) |
92 (5) |
| Wisconsin |
3,381 |
2,090 (62) |
418 (12) |
175 (5) |
19 (1) |
6 (—) |
10 (—) |
4 (—) |
650 (19) |
| Wyoming | 223 | 102 (46) | 86 (39) | 3 (1) | 0 (—) | 8 (4) | 0 (—) | 6 (3) | 18 (8) |
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease 2019; NH = non-Hispanic; NH/PI = Native Hawaiian/Other Pacific Islander.
* SARS-CoV-2 viral tests include polymerase chain reaction and antigen tests.
† The Health Resources Services Administration funds health centers in all 50 states, the District of Columbia, and the following U.S. territories and freely associated states: American Samoa, Federated States of Micronesia, Guam, Northern Mariana Islands, Marshall Islands, Puerto Rico, and U.S. Virgin Islands.
§ Data for the number of persons receiving testing or who had positive test results are aggregated by health center before submission and cannot be deduplicated, which might inflate or misrepresent the number of patients who received testing or who had positive test results.
Discussion
Health centers’ efforts to increase testing for SARS-CoV-2 are an important mitigation strategy to reach racial and ethnic minority groups at increased risk for COVID-19. Published state and national data indicate that racial and ethnic minority groups might be more likely to become infected with SARS-CoV-2, experience more severe COVID-19–associated illness, and have higher risk for death from COVID-19 (2–7). This study contributes to understanding current health center testing patterns and areas for improvement. Long-standing social inequalities and health disparities among racial and ethnic minority groups likely result from a multitude of factors that lead to increased risk for getting ill and dying of COVID-19, including discrimination,**** limited health care access and utilization, occupation, housing, and educational and income gaps.†††† Further, these factors might contribute to other risk factors for severe disease and death, including limited health care access, underlying medical conditions, and higher levels of environmental exposure. The factors contributing to disparities likely vary widely within and among groups, depending on geographic location and other contextual factors.
Health centers have a long-standing commitment to meeting the primary care needs of their communities (8). HRSA has awarded funding§§§§ to support health centers to purchase, administer, and expand capacity for COVID-19 testing and response-related activities, which has enabled health centers to maintain or increase their staffing levels, conduct training, purchase personal protective equipment, and administer tests. Health center services, including testing, contact tracing, isolation, providing health care, and aiding recovery from the impact of unintended negative consequences¶¶¶¶ of mitigation strategies, have increased the capacity of health centers to reach populations at increased risk for COVID-19 as well as access to testing and care.*****
A recent analysis of SARS-CoV-2 testing in a multistate network of health centers during the first weeks of the COVID-19 pandemic reported small racial differences in testing and positivity rates; however, larger differences were identified by ethnicity, preferred language, and insurance status, underscoring health centers’ unique position for serving racial and ethnic minority groups and addressing the ongoing need for targeted, language-concordant testing strategies (9). The results of this analysis indicate that health centers have afforded racial and ethnic minority populations access to SARS-CoV-2 testing during the COVID-19 pandemic and that these populations were at increased risk for COVID-19, given the large percentage of positive test results. White and Hispanic patients each accounted for 29% of tests performed; however, only 19% of positive test results were among White persons who received testing, whereas 61% were among racial and ethnic minority groups, with the largest percentage of positive test results (45%) among Hispanic patients. Twenty-six states and Puerto Rico reported >40% of positive tests among persons of Hispanic ethnicity with 1.5% of all Hispanic patients receiving testing at Puerto Rican health centers.
The findings in this report are subject to at least five limitations. First, the data used in this analysis are based on responses from health centers that voluntarily reported data to the Health Center COVID-19 Survey and might not be representative of all health centers in the United States, its territories, and freely associated states. Second, data represent a date range of information provided by health centers specified by weekly reporting date. Summary information across report dates is not comparable because of differences in health center responses for a given report date. Third, race and ethnicity data were missing for approximately 22% of patients who received testing and 19% of patients who had positive test results. Fourth, the reported number of patients tested each week does not fully represent the same patients included in the reported number with positive test results that week because of a lag between the date the specimen is collected and the availability of test results. Therefore, positivity cannot be inferred by dividing the number of patients who received positive test results by the number receiving testing. Finally, data for the number of persons with testing or positive results are aggregated by health centers before submission and cannot be deduplicated, which might inflate or misrepresent the number of patients receiving testing or positive test results.
Health centers are an integral component of health systems designed to address structural inequities (10). During the COVID-19 public health emergency, health centers have played an important role in providing access to testing in communities disproportionately affected by COVID-19. Health centers’ ability to reach populations at higher risk for SARS-CoV-2 infection might reduce COVID-19 transmission by identifying cases and supporting public health contact tracing and isolation among populations they serve.
Summary.
What is already known about this topic?
Long-standing social inequities and health disparities have resulted in increased risk for COVID-19 infection, severe illness, and death among racial and ethnic minority populations.
What is added by this report?
Health centers have provided racial and ethnic minority populations access to SARS-CoV-2 testing. Improving health centers’ ability to reach groups at increased risk for COVID-19 might reduce transmission by identifying cases and supporting contact tracing and isolation.
What are the implications for public health practice?
Efforts to improve coordination of COVID-19 response-related activities between state and local public health departments and HRSA-funded health centers can increase access to testing and follow-up care for populations at increased risk for COVID-19.
Acknowledgments
All Health Resources and Services Administration–funded health centers that completed the weekly Health Center COVID-19 Survey.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
Footnotes
Based on community needs, health centers offer medical, dental, vision, behavioral health, and enabling services.
Follow up services could include support for public health contact tracing, case investigation, case management, reporting, and isolation/quarantine.
The term “health center” is used to include both Federally Qualified Health Centers (FQHCs) and Health Center Program Look-Alikes (i.e., a health center that meets all Health Center Program requirements but does not receive federal award funding). During COVID-19, HRSA provided one-time COVID-19 funding to FQHCs and Health Center Look-Alikes to purchase, administer, and expand capacity for testing to monitor and support COVID-19 testing and response related activities. Data from FQHCs are included for this analysis.
Areas where economic, geographic, or cultural barriers limit access to affordable health care services.
In June 2020, there were 1,382 HRSA-funded health centers; by September 2020, there were 1,376.
In April 2020, HRSA began administering the voluntary weekly Health Center COVID-19 Survey. On June 5, 2020, survey questions related to testing were modified to disaggregate between virus detection (polymerase chain reaction, antigen) and antibody detection (serology). Before June 5, 2020, data from survey questions related to testing might be reflective of COVID-19 tests for both virus and antibody detection.
HRSA funds health centers in DC and the following U.S. territories and freely associated states: American Samoa, Federated States of Micronesia, Guam, Northern Mariana Islands, Marshall Islands, Puerto Rico, and U.S. Virgin Islands.
Patients who reported Hispanic/Latino ethnicity were classified as Hispanic/Latino, regardless of race.
Discrimination, which includes racism, can lead to chronic and toxic stress and shapes social and economic factors that put some people from racial and ethnic minority groups at increased risk for COVID-19.
To date, in 2020, HRSA has awarded approximately $2 billion through three rounds of funding to health centers: 1) March 24: $100 million (https://www.hhs.gov/about/news/2020/03/24/hhs-awards-100-million-to-health-centers-for-covid-19-response.html); 2) April 8:$1.3 billion (https://www.hhs.gov/about/news/2020/04/08/hhs-awards-billion-to-health-centers-in-historic-covid19-response.html); and 3) May 7: $583 million (https://www.hhs.gov/about/news/2020/05/07/hhs-awards-more-than-half-billion-across-the-nation-to-expand-covid19-testing.html).
Potential unintended negative consequences include loss of health insurance; food, housing, and income insecurity; mental health concerns; substance use; and violence resulting from social isolation, financial stress, and anxiety.
References
- 1.Health Resources and Services Administration. 2019 Uniform Data System—National Health Center data. Rockville, MD: US Department of Health and human Services; 2020. https://data.hrsa.gov/tools/data-reporting/program-data/national
- 2.Killerby ME, Link-Gelles R, Haight SC, et al. ; CDC COVID-19 Response Clinical Team. Characteristics associated with hospitalization among patients with COVID-19—metropolitan Atlanta, Georgia, March–April 2020. MMWR Morb Mortal Wkly Rep 2020;69:790–4. 10.15585/mmwr.mm6925e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:759–65. 10.15585/mmwr.mm6924e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gold JAW, Wong KK, Szablewski CM, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19—Georgia, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:545–50. 10.15585/mmwr.mm6918e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wortham JM, Lee JT, Althomsons S, et al. Characteristics of persons who died with COVID-19—United States, February 12–May 18, 2020. MMWR Morb Mortal Wkly Rep 2020;69:923–9. 10.15585/mmwr.mm6928e1 [DOI] [PubMed] [Google Scholar]
- 6.Center KE, Da Silva J, Hernandez AL, et al. Multidisciplinary community-based investigation of a COVID-19 outbreak among Marshallese and Hispanic/Latino communities—Benton and Washington Counties, Arkansas, March–June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1807–11. 10.15585/mmwr.mm6948a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Podewils LJ, Burket TL, Mettenbrink C, et al. Disproportionate incidence of COVID-19 infection, hospitalizations, and deaths among persons identifying as Hispanic or Latino—Denver, Colorado March–October 2020. MMWR Morb Mortal Wkly Rep 2020;69:1812–6. 10.15585/mmwr.mm6948a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine. Integrating social care into the delivery of health care: moving upstream to improve the nation's health. Washington, DC: National Academies Press; 2019. [PubMed] [Google Scholar]
- 9.Heintzman J, O’Malley J, Marino M, et al. SARS-CoV-2 testing and changes in primary care services in a multistate network of community health centers during the COVID-19 pandemic. JAMA 2020;324:1459–62. 10.1001/jama.2020.15891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lavoie JG, Varcoe C, Wathen CN, Ford-Gilboe M, Browne AJ; EQUIP Research Team. Sentinels of inequity: examining policy requirements for equity-oriented primary healthcare. BMC Health Serv Res 2018;18:705–17. 10.1186/s12913-018-3501-3 [DOI] [PMC free article] [PubMed] [Google Scholar]