Abstract
Background
The association of pulmonary embolism (PE) with deep vein thrombosis (DVT) in patients with coronavirus disease 2019 (COVID-19) remains unclear, and the diagnostic accuracy of D-dimer tests for PE is unknown.
Purpose
To conduct meta-analysis of the study-level incidence of PE and DVT and to evaluate the diagnostic accuracy of D-dimer tests for PE from multicenter individual patient data.
Materials and Methods
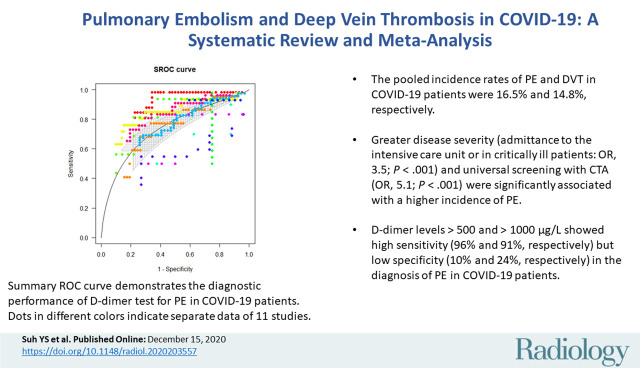
A systematic literature search identified studies evaluating the incidence of PE or DVT in patients with COVID-19 from January 1, 2020, to June 15, 2020. These outcomes were pooled using a random-effects model and were further evaluated using metaregression analysis. The diagnostic accuracy of D-dimer tests for PE was estimated on the basis of individual patient data using the summary receiver operating characteristic curve.
Results
Twenty-seven studies with 3342 patients with COVID-19 were included in the analysis. The pooled incidence rates of PE and DVT were 16.5% (95% CI: 11.6, 22.9; I2 = 0.93) and 14.8% (95% CI: 8.5, 24.5; I2 = 0.94), respectively. PE was more frequently found in patients who were admitted to the intensive care unit (ICU) (24.7% [95% CI: 18.6, 32.1] vs 10.5% [95% CI: 5.1, 20.2] in those not admitted to the ICU) and in studies with universal screening using CT pulmonary angiography. DVT was present in 42.4% of patients with PE. D-dimer tests had an area under the receiver operating characteristic curve of 0.737 for PE, and D-dimer levels of 500 and 1000 μg/L showed high sensitivity (96% and 91%, respectively) but low specificity (10% and 24%, respectively).
Conclusion
Pulmonary embolism (PE) and deep vein thrombosis (DVT) occurred in 16.5% and 14.8% of patients with coronavirus disease 2019 (COVID-19), respectively, and more than half of patients with PE lacked DVT. The cutoffs of D-dimer levels used to exclude PE in preexisting guidelines seem applicable to patients with COVID-19.
© RSNA, 2020
Supplemental material is available for this article.
See also the editorial by Woodard in this issue.
Summary
Pulmonary embolism (PE) and deep vein thrombosis (DVT) occurred in 16.5% and 14.8% of patients with coronavirus disease 2019, respectively, and more than half of patients with PE lacked DVT.
Key Results
■ The pooled incidence rates of pulmonary embolism (PE) and deep vein thrombosis in patients with coronavirus disease 2019 (COVID-19) were 16.5% and 14.8%, respectively.
■ Greater disease severity (necessitating admittance to the intensive care unit or in critically ill patients: odds ratio, 3.5; 95% CI: 1.9, 6.3; P < .001) and universal screening with CT pulmonary angiography (odds ratio, 5.1; 95% CI: 2.3, 11.5; P < .001) were significantly associated with a higher incidence of PE.
■ D-dimer levels greater than 500 and greater than 1000 μg/L showed high sensitivity (96% and 91%, respectively) but low specificity (10% and 24%, respectively) in the diagnosis of PE in patients with COVID-19.
Introduction
Coronavirus disease 2019 (COVID-19) is an ongoing global public threat, resulting in more than 10 million cumulative cases and more than 500 000 deaths worldwide as of June 30, 2020 (1). Older age and comorbidities are major risk factors for morbidity and mortality in patients with COVID-19 (2). Prothrombotic coagulation abnormalities and thromboembolism are emerging as frequent complications in critically ill patients with COVID-19, and these complications may contribute to morbidity and mortality (3). In particular, pulmonary embolism (PE) accounts for a majority of thromboembolic events in COVID-19 (4), but the association between PE and deep vein thrombosis (DVT) in patients with COVID-19 remains unclear (5). Furthermore, D-dimer levels are recognized as an independent predictor for survival (6) and thromboembolic events in COVID-19 (7), but the diagnostic accuracy of D-dimer tests for PE in patients with COVID-19 is unknown.
Therefore, we conducted a meta-analysis of the study-level incidence and characteristics of PE and DVT in patients with COVID-19 in the current literature and evaluated the diagnostic accuracy of D-dimer tests for PE from multicenter individual patient data.
Materials and Methods
Literature Search and Study Selection
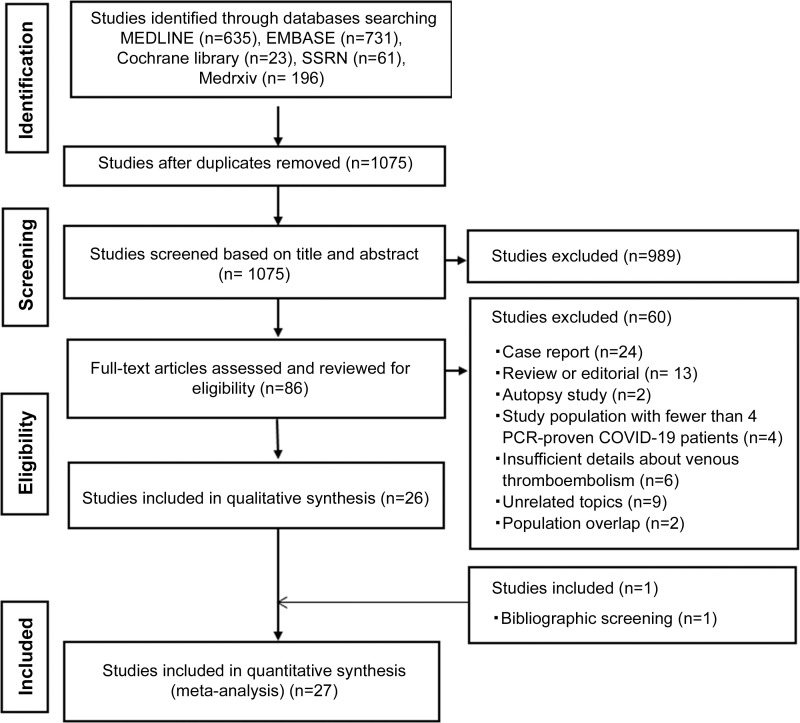
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses reporting guidelines, and the study protocol was registered in the International Prospective Register of Systematic Reviews database (registration number: CRD42020196777).
On June 15, 2020, we searched MEDLINE, Embase, the Cochrane Library, MedRxiv, and BioRxiv SSRN for studies on COVID-19 that reported the incidence of PE, venous thromboembolism including DVT, or both, and were published in English in 2020 (Appendix E1 [online]). The search strategy was designed by two experienced investigators in consensus (Y.J.S., S.H.Y.; thoracic radiologists with 4 and 8 years of experience with meta-analysis, respectively) and was followed by the literature search. The search was further supplemented by screening the bibliographies of the retrieved articles.
First, both reviewers independently screened all the publications on the basis of their titles and abstracts. The studies that satisfied the inclusion criteria were then retrieved for full-text assessments. The following inclusion criteria were applied to determine eligibility: study populations consisting of four or more patients with polymerase chain reaction–proven COVID-19, studies primarily investigating PE or venous thromboembolic events in patients with COVID-19 in vivo, and data described in sufficient detail to extract outcomes. We excluded studies with postmortem evaluations of PE or venous thromboembolic events in COVID-19.
Data Extraction
The two independent reviewers extracted the data from the articles, and any disagreements were resolved by consensus. Extracted data included study characteristics; demographic characteristics, including age and sex; severity of COVID-19 infection (critically ill patients or those admitted to the intensive care unit [ICU] vs noncritically ill patients or those admitted to the general ward); use of anticoagulation at the diagnosis of PE or DVT; the number of CT pulmonary angiographic examinations performed for the diagnosis of PE; and results, including the number of patients with PE and DVT, as well as the location of PE.
To evaluate the diagnostic accuracy of D-dimer tests for PE, we contacted the corresponding authors of the included articles for three items (D-dimer levels, whether CT pulmonary angiography was performed, and the presence of PE) in the individual anonymized patient data that the authors had already collected and presented in their study.
Definition of Outcomes
The primary outcome of this meta-analysis was the incidence of PE and DVT in patients with COVID-19. DVT events were confined to lower-extremity DVT. The secondary outcomes were the location of PE (the most proximal luminal filling defect in a patient; central [main or lobar pulmonary artery branch] vs peripheral [segmental or subsegmental branch]) (7) and the diagnostic accuracy of D-dimer test for the diagnosis of PE in patients with COVID-19.
Quality Assessment
The Newcastle-Ottawa Quality Scale for cohort studies was applied to assess the quality of the included studies (8). The scale assigns a maximum of four points for selection (representativeness of the exposed cohort, selection of the nonexposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at the start of the study), two points for comparability (comparability of cohorts on the basis of the design or analysis controlled for confounders), and three points for exposure or outcome (appropriate assessment of outcome, sufficient period, and adequacy of follow-up period). Studies were independently reviewed by two reviewers (Y.J.S., S.H.Y.), and any discrepancy was resolved through discussion and consensus. A score of six or higher indicated high quality.
Statistical Analysis
Extracted outcomes were pooled by weighted averages using a DerSimonian-Laird random‐effects model. We assessed the extent of statistical heterogeneity between studies using the Cochran Q test and I2 statistics (9,10), and P values less than .1 or I2 statistics greater than 50% were considered to indicate the presence of substantial heterogeneity. To investigate the cause of heterogeneity between studies, a subgroup analysis of the following study characteristics was performed: study design, the severity of COVID-19 infection, and the proportion of patients who underwent CT pulmonary angiography within the study population and use of prophylactic or therapeutic anticoagulation. Meta-regression was performed using a random-effects model to assess the effect of study characteristics on PE incidence, and the cluster robust estimator was used to account for correlations among multiple effect sizes within a study.
To analyze the diagnostic performance of D-dimer tests for PE, a summary receiver operating characteristic curve was estimated with a multiple-threshold model, a multilevel random-effects model that considers sensitivity and specificity as functions of the thresholds and accounts for heterogeneity across studies, and the correlation of sensitivity with specificity (11). We used data from patients who underwent CT pulmonary angiography, as the presence or absence of PE could not be certain without CT pulmonary angiography. The optimal cutoffs were estimated by maximizing the Youden index under varying weights for sensitivity.
Statistical analysis was performed using software (Comprehensive Meta-Analysis, version 3; Biostat and R, version 3.6.; R Foundation for Statistical Computing). The potential for publication bias was assessed using the Egger test and was drawn as funnel plots (12).
Results
Literature Search
Of the 1646 references identified in the initial database search, 27 studies with 3342 patients with COVID-19 were included in the analysis of the overall incidence of PE and DVT (7,13–38) (Fig 1). Thirteen studies (1896 patients) reported the incidence of both PE and DVT (13,14,20,22,25,27–30,32,33,37,38), whereas nine studies (1022 patients) and five studies (424 patients) reported the incidence of PE only (7,15,19,21,23,24,31,34,36) and DVT only (16–18,26,35), respectively.
Figure 1:
Flowchart of the literature review process. COVID-19 = coronavirus disease 2019, PCR = polymerase chain reaction.
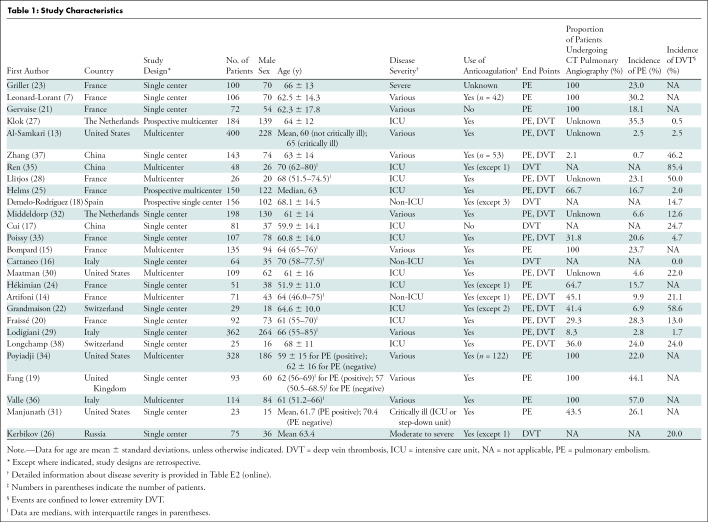
Study Characteristics and Quality Assessment
The characteristics of the included studies are summarized in Table 1. Three of the 27 studies were prospective, and the other 24 were retrospective. The study population comprised patients not in the ICU in four studies, patients in the ICU (or critically ill patients) in 12 studies, and patients with various levels of disease severity in 11 studies. In eight of those 11 studies, data could be separately extracted for patients in the ICU (or critically ill patients) and those not in the ICU (or noncritically ill patients). The use of prophylactic or therapeutic anticoagulation was reported in 24 studies, and no or unknown use of anticoagulation was described in three studies. Among 22 studies that reported the incidence of PE, CT pulmonary angiography was performed to ascertain the presence of PE in the entire study population in seven studies and in only part or an unknown proportion of the study population in 15 studies.
Table 1:
Study Characteristics
With the Newcastle-Ottawa scale, 14 studies (52%) were classified as being of high quality, and the other 13 (48%) were of low quality. The results of the quality assessment are presented in Table E1 (online).
Incidence of PE and DVT in Patients with COVID-19
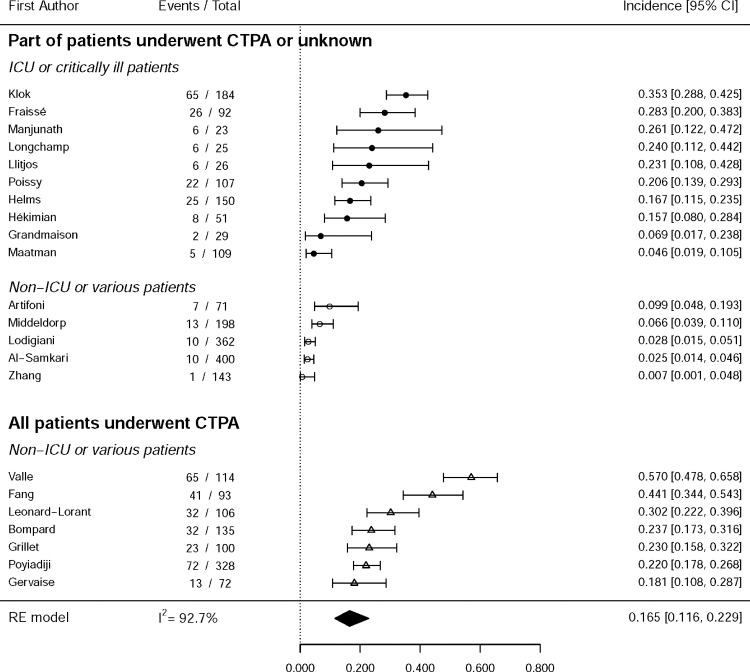
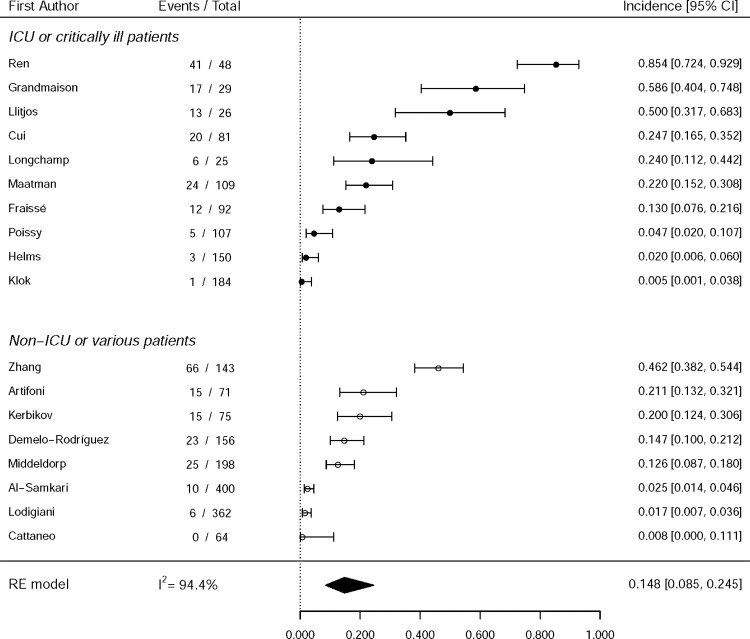
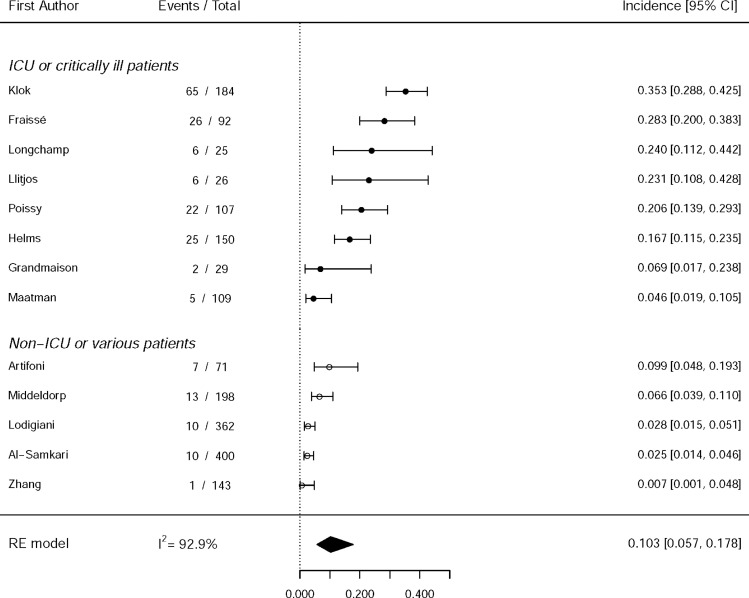
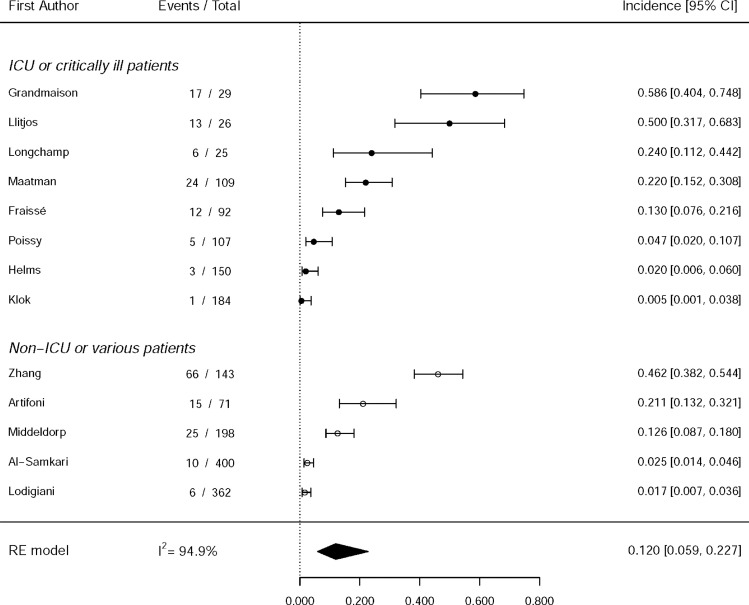
The pooled incidence rates of overall PE and DVT were 16.5% (95% CI: 11.6, 22.9) and 14.8% (95% CI: 8.5, 24.5), respectively (Fig 2). Significant interstudy heterogeneity was observed (I2 = 0.93, P < .001 for PE; I2 = 0.94, P < .001 for DVT). In 13 studies (1896 patients) that investigated the incidence of both PE and DVT, the incidence rates were 10.3% (95% CI: 5.7, 17.8; I2 = 0.93; P < .001) and 12.0% (95% CI: 5.9, 22.7; I2 = 0.95; P < .001), respectively. The pooled proportion of positive DVT results in patients with PE was 42% among 88 PE lesions in eight studies (95% CI: 23, 65; I2 = 0.63; P = .008) (Fig E1 [online]). Information on PE location was available for 318 patients in 14 studies (Table E3 [online]): 39.0% (95% CI: 30.0, 48.9; I2 = 0.56; P = .005) were central, and 60.4% (95% CI: 50.3, 69.7; I2 = 0.58; P = .003) were peripheral.
Figure 2a:
Forest plots show pooled incidence rates of (a) pulmonary embolism (PE) (n = 22) and (b) deep vein thrombosis (DVT) (n = 18) in patients with coronavirus disease 2019. The estimated overall incidence rates of PE and DVT were 16.5% (95% CI: 11.6, 22.9) and 14.8% (95% CI: 8.5, 24.5), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects. Forest plots show pooled incidence rates of (c, d) both pulmonary embolism (PE) and deep vein thrombosis (DVT) (n = 13) in patients with coronavirus disease 2019. In the 13 studies that reported both PE and DVT, the incidence rates were 10.3% (95% CI: 5.7, 17.8) and 12.0% (95% CI: 5.9, 22.7), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects.
Figure 2b:
Forest plots show pooled incidence rates of (a) pulmonary embolism (PE) (n = 22) and (b) deep vein thrombosis (DVT) (n = 18) in patients with coronavirus disease 2019. The estimated overall incidence rates of PE and DVT were 16.5% (95% CI: 11.6, 22.9) and 14.8% (95% CI: 8.5, 24.5), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects. Forest plots show pooled incidence rates of (c, d) both pulmonary embolism (PE) and deep vein thrombosis (DVT) (n = 13) in patients with coronavirus disease 2019. In the 13 studies that reported both PE and DVT, the incidence rates were 10.3% (95% CI: 5.7, 17.8) and 12.0% (95% CI: 5.9, 22.7), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects.
Figure 2c:
Forest plots show pooled incidence rates of (a) pulmonary embolism (PE) (n = 22) and (b) deep vein thrombosis (DVT) (n = 18) in patients with coronavirus disease 2019. The estimated overall incidence rates of PE and DVT were 16.5% (95% CI: 11.6, 22.9) and 14.8% (95% CI: 8.5, 24.5), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects. Forest plots show pooled incidence rates of (c, d) both pulmonary embolism (PE) and deep vein thrombosis (DVT) (n = 13) in patients with coronavirus disease 2019. In the 13 studies that reported both PE and DVT, the incidence rates were 10.3% (95% CI: 5.7, 17.8) and 12.0% (95% CI: 5.9, 22.7), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects.
Figure 2d:
Forest plots show pooled incidence rates of (a) pulmonary embolism (PE) (n = 22) and (b) deep vein thrombosis (DVT) (n = 18) in patients with coronavirus disease 2019. The estimated overall incidence rates of PE and DVT were 16.5% (95% CI: 11.6, 22.9) and 14.8% (95% CI: 8.5, 24.5), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects. Forest plots show pooled incidence rates of (c, d) both pulmonary embolism (PE) and deep vein thrombosis (DVT) (n = 13) in patients with coronavirus disease 2019. In the 13 studies that reported both PE and DVT, the incidence rates were 10.3% (95% CI: 5.7, 17.8) and 12.0% (95% CI: 5.9, 22.7), respectively. Significant interstudy heterogeneity was seen in all groups. CTPA = CT pulmonary angiography, ICU = intensive care unit, RE = random effects.
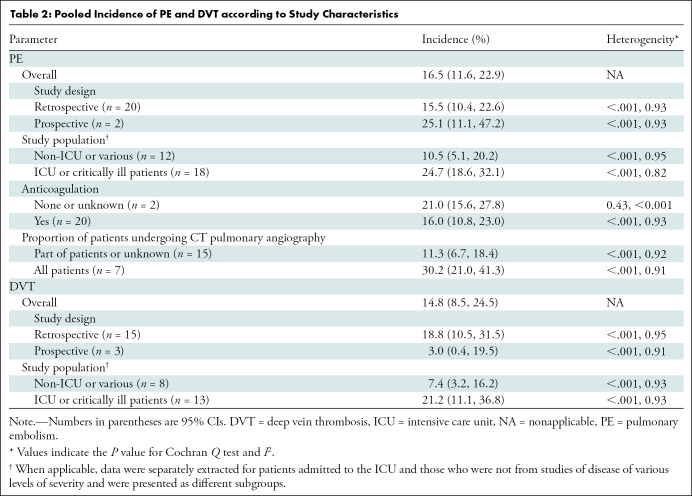
The incidence rates of PE and DVT according to study characteristics are presented in Table 2. Prospective studies reported a higher incidence of PE but a lower incidence of DVT than did retrospective studies. Studies with anticoagulation had a lower incidence of PE than did those with no or unknown anticoagulation. Studies of patients admitted to the ICU or critically ill patients reported higher incidence rates of PE and DVT than did those of patients who were not admitted to the ICU or those of patients with various levels of disease severity (PE: 24.7% [95% CI: 18.6, 32.1] vs 10.5% [95% CI: 5.1, 20.2]; DVT: 21.2% [95% CI: 11.1, 36.8] vs 7.4% [95% CI: 3.2, 16.2]). Studies in which CT pulmonary angiography was performed in all patients showed a higher incidence of PE than did those in which CT pulmonary angiography was performed in only some of the patients or in an unknown proportion (30.2% [95% CI: 21.0, 41.3] vs 11.3% [95% CI: 6.7, 18.4]).
Table 2:
Pooled Incidence of PE and DVT according to Study Characteristics
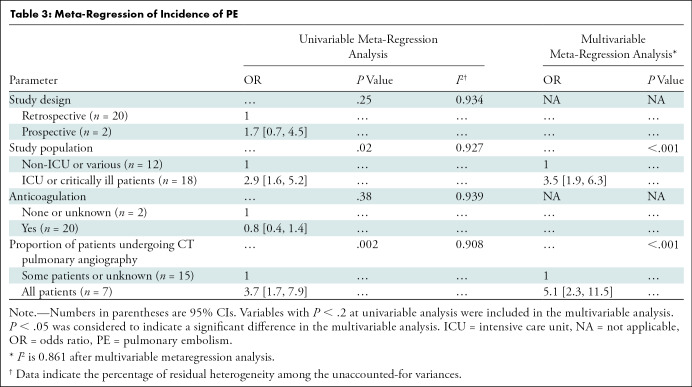
In a univariable meta-regression analysis, study design and use of anticoagulation were not associated with an increased incidence of PE (P = .25 and P = .38, respectively) (Table 3). However, greater disease severity (P = .0016) and a higher proportion of patients undergoing CT pulmonary angiography (P = .002) were significantly associated with the higher incidence of PE. When multiple study-level characteristics were adjusted, a higher incidence of PE was associated with a study population of patients admitted to the ICU or who were critically ill (odds ratio, 3.5; 95% CI: 1.9, 6.3; P < .001) and universal CT pulmonary angiography screening in the study population (odds ratio, 5.1; 95% CI: 2.3, 11.5; P < .001).
Table 3:
Meta-Regression of Incidence of PE
Diagnostic Performance of D-dimer for PE in Patients with COVID-19
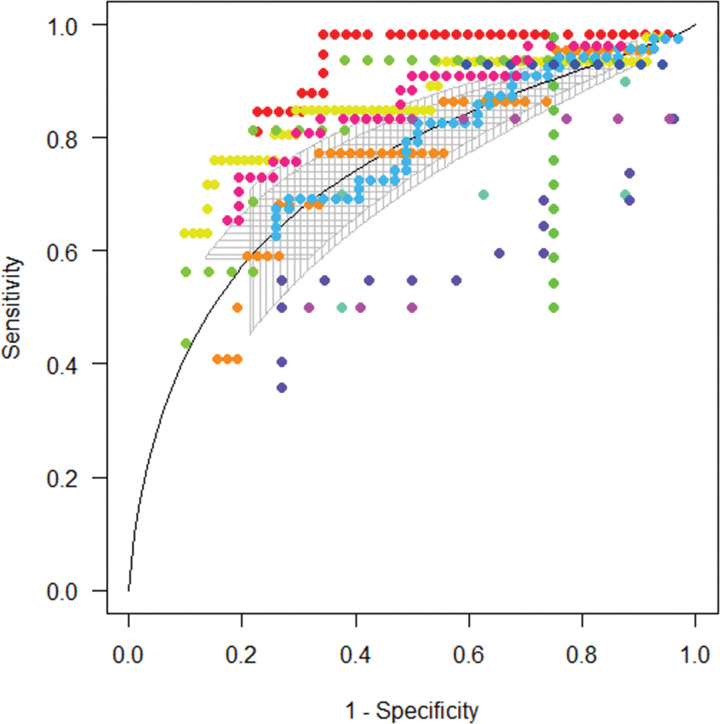
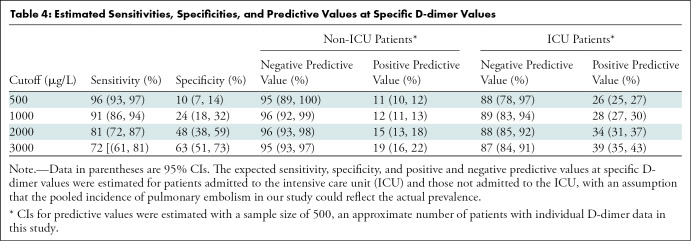
In total, 11 studies provided data regarding D-dimer levels and the presence of PE as assessed with CT pulmonary angiography in their study population (567 patients) (7,14,15,19–22,24,33,36,38). D-dimer levels were higher in patients with PE (median, 7625 μg/L; n = 218) than in those without PE (median, 1750 μg/L; n = 349). The summary receiver operating characteristic curve yielded an area under the receiver operating characteristic curve of 0.737 (Fig 3), suggesting cutoffs of D-dimer levels for PE diagnosis under varying weights for sensitivity and specificity. For example, the cutoff was 4453.2 μg/L using the same weight for sensitivity and specificity (sensitivity, 62% [95% CI: 49, 73]; specificity, 76% [95% CI: 65, 84]) (Table E4 [online]). With cutoff values of 500 and 1000 μg/L, the sensitivity of D-dimer tests for PE was 96% (95% CI: 93, 97) and 91% (95% CI: 86, 94), respectively, and its specificity was 10% (95% CI: 7, 14) and 24% (95% CI: 18, 32) (Table 4). The negative predicted value of the D-dimer level was estimated as 95% (95% CI: 89, 100) in patients not in the ICU and as 88% (95% CI: 78, 97) in patients in the ICU by using a cutoff value of 500 μg/L, and it was predicted as 96% (95% CI: 92, 99) in patients not in the ICU and as 89% (95% CI: 83, 94) in patients admitted to the ICU by using a cutoff of 1000 μg/L.
Figure 3:
Summary receiver operating characteristic curve shows the diagnostic performance of D-dimer tests for pulmonary embolism in patients with coronavirus disease 2019. Dots of different colors indicate separate data of 11 studies.
Table 4:
Estimated Sensitivities, Specificities, and Predictive Values at Specific D-dimer Values
Publication Bias
The funnel plots did not show significant publication bias for the incidence of PE and DVT (P = .22 and P = .36) (Fig 4).
Figure 4a:
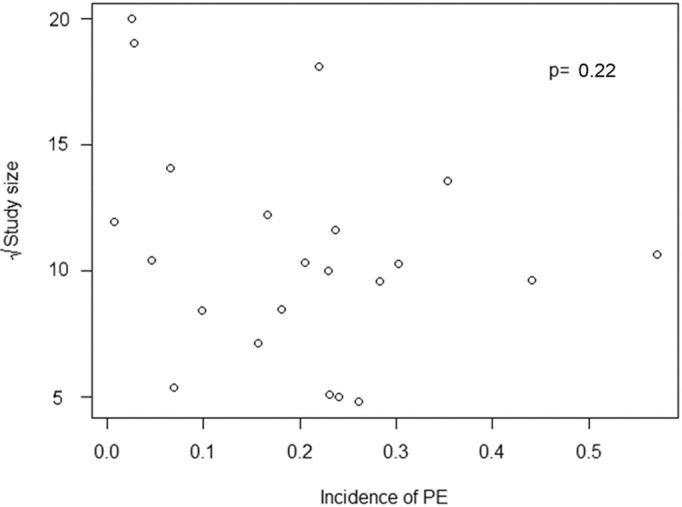
Funnel plots used to detect publication bias. Each circle represents a study included in the analysis. Probability values of asymmetry from the Egger test are shown. (a) Incidence of pulmonary embolism (PE). (b) Incidence of deep vein thrombosis (DVT).
Figure 4b:
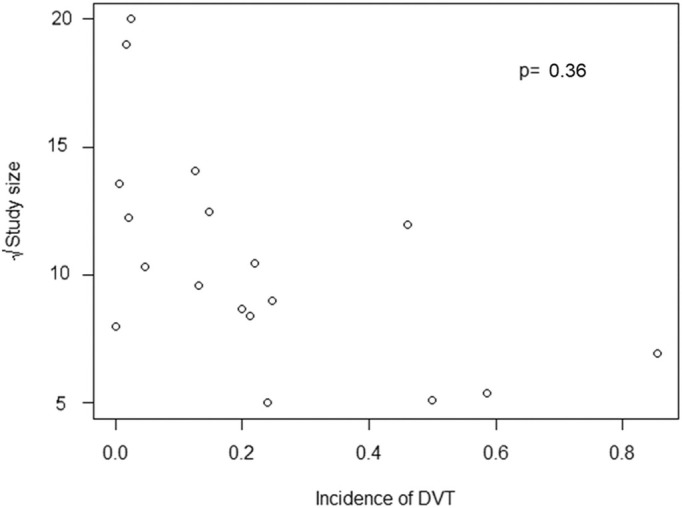
Funnel plots used to detect publication bias. Each circle represents a study included in the analysis. Probability values of asymmetry from the Egger test are shown. (a) Incidence of pulmonary embolism (PE). (b) Incidence of deep vein thrombosis (DVT).
Discussion
This meta-analysis demonstrated that the pooled incidence rates of pulmonary embolism (PE) and deep vein thrombosis (DVT) in patients with coronavirus disease 2019 (COVID-19) were 16.5% and 14.8%, respectively, and substantial interstudy heterogeneity was present. The multivariable meta-regression analysis demonstrated that greater disease severity and universal screening with CT pulmonary angiography were significantly associated with a higher incidence of PE (P < .001 for both). Furthermore, 42.4% of patients with PE had DVT, and PE was more frequently located in the peripheral portion of the pulmonary arteries than in the central portion (60.4% vs 39.0%). D-dimer levels greater than 500 μg/L and greater than 1000 μg/L showed high sensitivity (96% and 91%, respectively) but low specificity (10% and 24%, respectively) for the diagnosis of PE in patients with COVID-19.
Although PE has been reported to occur frequently in patients with COVID-19 and to be associated with a poor prognosis (27), its actual incidence is unknown. The reported incidence of PE ranged from 0.7% to 57.0% in the studies included in this meta-analysis. This variation in the reported incidence can be assumed to reflect differences across studies in the disease severity of the study population and the frequency of performing diagnostic imaging studies, such as CT pulmonary angiography. Accordingly, the multivariable meta-analysis revealed that greater disease severity and universal screening with CT pulmonary angiography were significantly associated with a higher incidence of PE (P < .001 for both).
In this meta-analysis, the pooled incidence of PE was 24.7% in patients admitted to the ICU, although it was high (10.5%) even in patients not admitted to the ICU. The PE incidence was higher than the reported value in patients with non–COVID-19 viral pneumonia who were admitted to the ICU or who had acute respiratory distress syndrome (range, 1.3%–7.5%) (25,33). Besides the increased risk of venous thromboembolism in acutely ill patients, another hypothesis—in situ immunothrombosis—has been proposed to explain the high incidence of PE in patients with COVID-19 (39), as previous autopsy studies found multiple thrombi in small to medium pulmonary arteries (40–43). In a recent systematic review, microthrombosis was frequently observed in lung histopathologic analysis of the population with COVID-19 (57%), which was higher than that in the population with H1N1 influenza (24%) (44). This hypothesis is supported by the results of a previous study, which reported that the PE phenotype in patients with COVID-19 was different from the PE phenotype in patients without COVID-19 pneumonia; specifically, in patients with COVID-19, the thrombotic lesions were more distributed in the peripheral arteries of the lung, and the total clot burden was lower (5). Similarly, the results of our meta-analysis support the hypothesis that in situ thrombosis partly contributes to prothrombotic events in COVID-19 because DVT was present in only 42.4% of patients with PE, which was lower than the usual prevalence (60%) of DVT in patients with PE (45), and more than half of PEs were located in the distal pulmonary arteries.
Because most CT pulmonary angiographic examinations are performed based on clinical suspicion rather than systematic screening, the incidence of PE may be somewhat underestimated, especially in cases of small segmental or subsegmental PE (27). Therefore, D-dimer levels play a crucial role in screening and the ultimate diagnosis of PE (14). The elevation of D-dimer levels in the COVID-19 population may stem from prothrombotic coagulopathy or pulmonary microvascular thrombosis beyond the resolution of CT pulmonary angiography.
Because D-dimer levels tend to be elevated even in patients with COVID-19 without PE, D-dimer cutoffs for PE screening can be a substantial concern in the care of patients with COVID-19. In our study, the conventional cutoff values (500 or 1000 μg/L) showed high sensitivity (96% and 91, respectively), which is comparable to the sensitivity of D-dimer levels in patients without COVID-19 (46). In fact, higher cutoff values than those conventionally used (>1000 μg/L) reduced the sensitivity, limiting the clinical application of D-dimer levels as a screening examination to rule out PE. Our results suggest that the conventional cutoffs of D-dimer levels in preexisting guidelines can be applicable to the COVID-19 population for PE screening that serves as a basis for subsequent CT pulmonary angiographic examinations (46,47). However, considering the low diagnostic performance (area under the curve, 0.737) of D-dimer tests and the relatively lower negative predictive value in patients admitted to the ICU, a combination of pretest clinical probability assessment and age-adjusted D-dimer cutoff values could improve the diagnostic yield of D-dimer levels (48,49).
In all but three of the included studies, patients received anticoagulation with a prophylactic or therapeutic dose. Generally, it is recommended that critically ill patients who require ICU care receive prophylactic anticoagulation because they are considered to be at high thrombotic risk as a result of extended periods of immobilization, mechanical ventilation, and vascular injury or surgery (50). In consideration of the high frequency of venous thromboembolism and the positive effect of heparin for reducing mortality in patients with COVID-19, systematic pharmacologic thromboprophylaxis is recommended for all patients who require hospital admission for COVID-19, even if they do not receive care in the ICU (51). However, the high incidence of PE or DVT despite prophylactic anticoagulation may suggest that a more reinforced thromboprophylaxis regimen could reduce venous thromboembolism and improve the prognosis of patients with COVID-19 (22).
Our study had several limitations. First, a substantial proportion (48%) of the included studies were of low quality, probably because they intended to promptly report the significance of PE in COVID-19, a rapidly spreading condition with substantial public health implications. Nevertheless, to our knowledge, our meta-analysis was the largest one to investigate the incidence of PE and DVT in the COVID-19 population. Second, the incidence of PE and DVT reported herein could be an overestimate relative to the entire COVID-19 population, as the included studies preferentially analyzed patients with severe disease and our literature search based on the search term thrombosis/embolism might have resulted in a low likelihood of including studies with zero incidence. Third, the effect of the dose or regimen of anticoagulation was not investigated because this information was often unavailable or insufficient in the included studies. Fourth, we analyzed baseline D-dimer levels at admission, and changes in D-dimer levels could not be considered in the analysis. Fourth, the prognostic impact of PE was not assessed in this meta-analysis because we focused on the incidence of PE or DVT and the diagnostic accuracy and cutoff of D-dimer levels for PE diagnosis.
In conclusion, the pooled incidence rates of pulmonary embolism (PE) and deep vein thrombosis (DVT) in patients with coronavirus disease 2019 (COVID-19) were high, at 16.5% and 14.8%, respectively, and exceeded 20% in patients admitted to the intensive care unit. PE was confined to the peripheral pulmonary arteries in more than half of patients with PE, and DVT was found in less than half of the patients with PE. The D-dimer cutoffs used to exclude PE (500 and 1000 μg/L) in the preexisting guidelines seem to be applicable to patients with COVID-19.
APPENDIX
SUPPLEMENTAL FIGURE
Disclosures of Conflicts of Interest: Y.J.S. disclosed no relevant relationships. H.H. disclosed no relevant relationships. M.O. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: is a consultant for Canon Medical Systems Europe. Other relationships: disclosed no relevant relationships. F.B. disclosed no relevant relationships. M.P.R. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: gave lectures for MSD France, was compensated for travel by Guerbet France. Other relationships: disclosed no relevant relationships. C.V. disclosed no relevant relationships. A.G. disclosed no relevant relationships. J.P. disclosed no relevant relationships. S.S. disclosed no relevant relationships. G.H. disclosed no relevant relationships. M.A. disclosed no relevant relationships. D.P. disclosed no relevant relationships. D.C. disclosed no relevant relationships. J.D. disclosed no relevant relationships. B.S. disclosed no relevant relationships. C.F. disclosed no relevant relationships. G.G. disclosed no relevant relationships. H.R. disclosed no relevant relationships. S.H.Y. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: is Chief Medical Officer of Medical IP. Other relationships: disclosed no relevant relationships.
Abbreviations:
- COVID-19
- coronavirus disease 2019
- DVT
- deep vein thrombosis
- ICU
- intensive care unit
- PE
- pulmonary embolism
References
- 1.World Health Organization . Coronavirus disease (COVID-19): situation report, 162. Geneva, Switzerland: World Health Organization, 2020. [Google Scholar]
- 2.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8(5):475–481 [Published correction appears in Lancet Respir Med 2020;8(4):e26.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Lancet Haematology . COVID-19 coagulopathy: an evolving story. Lancet Haematol 2020;7(6):e425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Dam LF, Kroft LJM, van der Wal LI, et al. Clinical and computed tomography characteristics of COVID-19 associated acute pulmonary embolism: a different phenotype of thrombotic disease? Thromb Res 2020;193:86–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;180(7):934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Léonard-Lorant I, Delabranche X, Séverac F, et al. Acute pulmonary embolism in patients with COVID-19 at CT angiography and relationship to D-dimer levels. Radiology 2020;296(3):E189–E191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, Canada: Ottawa Hospital Research Institute, 2011. [Google Scholar]
- 9.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 10.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7(3):177–188. [DOI] [PubMed] [Google Scholar]
- 11.Steinhauser S, Schumacher M, Rücker G. Modelling multiple thresholds in meta-analysis of diagnostic test accuracy studies. BMC Med Res Methodol 2016;16(1):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Samkari H, Karp Leaf RS, Dzik WH, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 2020;136(4):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Artifoni M, Danic G, Gautier G, et al. Systematic assessment of venous thromboembolism in COVID-19 patients receiving thromboprophylaxis: incidence and role of D-dimer as predictive factors. J Thromb Thrombolysis 2020;50(1):211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bompard F, Monnier H, Saab I, et al. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J 2020;56(1):2001365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cattaneo M, Bertinato EM, Birocchi S, et al. Pulmonary embolism or pulmonary thrombosis in COVID-19? Is the recommendation to use high-dose heparin for thromboprophylaxis justified? Thromb Haemost 2020;120(8):1230–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 2020;18(6):1421–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res 2020;192:23–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang C, Garzillo G, Batohi B, et al. Extent of pulmonary thromboembolic disease in patients with COVID-19 on CT: relationship with pulmonary parenchymal disease. Clin Radiol 2020;75(10):780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fraissé M, Logre E, Pajot O, Mentec H, Plantefève G, Contou D. Thrombotic and hemorrhagic events in critically ill COVID-19 patients: a French monocenter retrospective study. Crit Care 2020;24(1):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gervaise A, Bouzad C, Peroux E, Helissey C. Acute pulmonary embolism in non-hospitalized COVID-19 patients referred to CTPA by emergency department. Eur Radiol 2020;30(11):6170–6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grandmaison G, Andrey A, Périard D, et al. Systematic screening for venous thromboembolic events in COVID-19 pneumonia. TH Open 2020;4(2):e113–e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grillet F, Behr J, Calame P, Aubry S, Delabrousse E. Acute pulmonary embolism associated with COVID-19 pneumonia detected with pulmonary CT angiography. Radiology 2020;296(3):E186–E188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hékimian G, Lebreton G, Bréchot N, Luyt CE, Schmidt M, Combes A. Severe pulmonary embolism in COVID-19 patients: a call for increased awareness. Crit Care 2020;24(1):274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med 2020;46(6):1089–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerbikov OB, Orekhov PY, Borskaya EN, Nosenko NS. High incidence of venous thrombosis in patients with moderate to severe COVID-19. MedRxiv 2020.06.12.20129536v1 [preprint] 10.1101/2020.06.12.20129536. Posted June 14, 2020. Accessed June 17, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klok FA, Kruip MJHA, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res 2020;191:148–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost 2020;18(7):1743–1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020;191:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maatman TK, Jalali F, Feizpour C, et al. Routine venous thromboembolism prophylaxis may be inadequate in the hypercoagulable state of severe coronavirus disease 2019. Crit Care Med 2020;48(9):e783–e790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manjunath M, Miranda J, Fraenkel L, et al. Acute pulmonary embolism in critically ill patients with COVID-19. medRxiv 2020. [Google Scholar]
- 32.Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18(8):1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in patients with COVID-19: awareness of an increased prevalence. Circulation 2020;142(2):184–186. [DOI] [PubMed] [Google Scholar]
- 34.Poyiadji N, Cormier P, Patel PY, et al. Acute pulmonary embolism and COVID-19. Radiology 2020;297(3):E335–E338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ren B, Yan F, Deng Z, et al. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation 2020;142(2):181–183. [DOI] [PubMed] [Google Scholar]
- 36.Valle C, Bonaffini PA, Dal Corso M, et al. Pulmonary embolism and COVID-19, an unexpected association: experience from two centers in the core of the infection Italian peak. SSRN 3588533 [preprint] 10.2139/ssrn.3588533. Posted June 2, 2020. Accessed June 15, 2020. [DOI] [PMC free article] [PubMed]
- 37.Zhang L, Feng X, Zhang D, et al. Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China: prevalence, risk factors, and outcome. Circulation 2020;142(2):114–128. [DOI] [PubMed] [Google Scholar]
- 38.Longchamp A, Longchamp J, Manzocchi-Besson S, et al. Venous thromboembolism in critically Ill patients with COVID-19: results of a screening study for deep vein thrombosis. Res Pract Thromb Haemost 2020;4(5):842–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McFadyen JD, Stevens H, Peter K. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res 2020;127(4):571–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lax SF, Skok K, Zechner P, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med 2020;173(5):350–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med 2020;383(2):120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med 2020;8(7):681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carsana L, Sonzogni A, Nasr A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis 2020;20(10):1135–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hariri LP, North CM, Shih AR, et al. Lung histopathology in COVID-19 as compared to SARS and H1N1 influenza: a systematic review. Chest doi:10.1016/j.chest.2020.09.259. Published online October 7, 2020. Accessed October 7, 2020. [DOI] [PMC free article] [PubMed]
- 45.Girard P, Sanchez O, Leroyer C, et al. Deep venous thrombosis in patients with acute pulmonary embolism: prevalence, risk factors, and clinical significance. Chest 2005;128(3):1593–1600. [DOI] [PubMed] [Google Scholar]
- 46.Lim W, Le Gal G, Bates SM, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: diagnosis of venous thromboembolism. Blood Adv 2018;2(22):3226–3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2020;41(4):543–603. [DOI] [PubMed] [Google Scholar]
- 48.Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA 2014;311(11):1117–1124 [Published correction appears in JAMA 2014;311(16):1694.]. [DOI] [PubMed] [Google Scholar]
- 49.Kearon C, de Wit K, Parpia S, et al. Diagnosis of pulmonary embolism with D-dimer adjusted to clinical probability. N Engl J Med 2019;381(22):2125–2134. [DOI] [PubMed] [Google Scholar]
- 50.Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141(2 Suppl):7S–47S [Published corrections appear in Chest 2012;141(4):1129 and Chest 2012;142(6):1698. Dosage error in article text.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020;18(5):1023–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.