Abstract
The present systematic review and meta-analysis provides a comprehensive assessment of the sciatic nerve (SN) variants relative to the piriformis muscle (PM) and compares those variants’ prevalence among different geographical populations with respect to gender and laterality. A database search was conducted to identify cadaveric studies pertinent to SN variants relative to the PM. A total of 44 articles were included. The typical morphological pattern (type A, with the SN passing undivided below the PM) was found to be the most common variant, with 90% pooled prevalence. SN variants were more common among East Asians, with a 31% pooled prevalence of total variants. No significant differences were established with respect to gender and laterality. In greater than 10% of the population, the SN coursed through or above piriformis. Patients’ epidemiological characteristics may predispose them to certain variants. The common peroneal nerve (CPN) is more susceptible to injury during a total hip arthroplasty or a hip arthroscopy where anomalies are encountered. As anatomical variants are commonly associated with piriformis syndrome, they should always be considered during diagnosis and treatment.
Keywords: sciatic nerve, variation, abnormality, piriformis muscle, anatomy, anomaly
Introduction and background
The sciatic nerve (SN), the longest and widest nerve of the human body, is formed from the L4-S3 ventral roots and normally exits the pelvis, via a single trunk, through the great sciatic foramen below the piriformis muscle (PM). The SN courses in the posterior thigh compartment and divides into the tibial and the common peroneal trunk at the popliteal fossa. The tibial and common peroneal nerves (TN and CPN) are surrounded by a common epineural sheath into the SN main trunk. However, tibial and peroneal fascicular groups are separated by a connective tissue, known as the Compton-Cruveilheir septum [1]. The SN innervates the muscles of the posterior thigh compartment and all the lower leg and foot compartments.
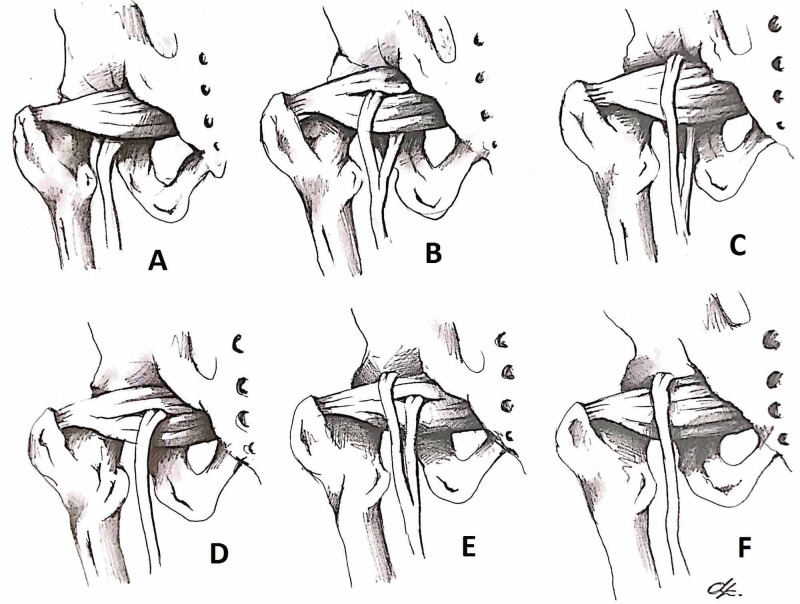
The separate (autonomous) development of the SN tibial and peroneal divisions could explain the source of SN variants during embryonic development [2]. The possible relationships between the SN and PM were first categorized by Beaton and Anson [3] into the following six morphological types (Figure 1):
Figure 1. The Beaton and Anson classification system (1937)*.
*[3]
Type A: typical morphological pattern, the SN passes below the PM undivided. Type B: the CPN exits through the PM and the TN exits below the PM. Type C: the CPN exits above the PM and the TN and below the PM. Type D: the SN exits through the PM, as a single trunk. Type E: the CPN exits above the PM and the TN through the PM. Type F: the SN passes undivided above the PM
SN: sciatic nerve; PM: piriformis muscle; CPN: common peroneal nerve; TN: tibial nerve
Type A: typical pattern with the SN passing below the PM, undivided
Type B: the CPN exits through the PM and TN exits below the PM
Type C: the CPN exits above the PM and TN and below the PM
Type D: the SN exits through the PM, as a single trunk
Type E: the CPN exits above the PM and TN through the PM, and
Type F: the SN passes undivided above the PM
Clinical awareness of SN variants is of high importance, as they constitute a common etiology of piriformis syndrome (a condition characterized by the SN entrapment from PM). Common symptoms include buttock pain and sciatica, which are aggravated by sitting [4]. An awareness of SN variants is crucial when performing a total hip arthroplasty, particularly via a posterior approach, SN blockade, or PM imaging-guided injections. Accurate knowledge of the typical SN anatomy and its variants could prevent a plethora of complications during procedures in the area and could aid in the diagnosis of various pathologies.
The current systematic review and meta-analysis of the literature provides an evidence-based assessment of SN variants in relation to the PM, by highlighting the variants’ prevalence among different populations, taking into account gender and laterality as well.
Review
Methods
Search Strategy
The current systematic review and meta-analysis was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines [5]. A literature search of the databases PubMed, Scopus, SciELO, and Web of Science was conducted from their inception up to May 2020 to find studies about SN variants relative to the PM. The search terms used were as follows: “sciatic nerve”, “nervus ischiadicus”, “Ischiadic Nerve”, “Ischiatic Nerve”, “anatomy”, “variation” and “anomalies” with “AND” and “OR” as Boolean terms.
Inclusion Criteria and Study Selection
Only cadaveric studies were included. Case reports, letters to the editors, conference abstracts, and articles involving clinical or imaging studies were excluded. In compliance with the search strategy, two independent investigators screened and assessed the retrieved articles for eligibility. Any duplicates or obviously irrelevant studies were excluded. If eligibility could not be confirmed by the title or the abstract, the full text was retrieved. Reference lists of the related articles were hand-searched for any additional eligible studies in a further effort not to miss out on any relevant publications. Any disagreement regarding eligibility was resolved by a discussion between the two investigators and, if necessary, a third investigator was consulted.
Data Extraction
A dedicated data extraction form was developed for recording all relevant details, involving publication details [author(s) and year of publication], sample size, SN variants relative to the PM, gender, and laterality when recorded. In cases of nonexisting data, the authors were contacted for further clarification if possible. The classification system used was the one introduced by Beaton and Anson [3]. We exclusively analyzed our data according to types A-D, as E and F types were described as hypothetical by Beaton and Anson and most of the subsequent studies did not subcategorize their groups according to them.
Statistical Analysis
Collected data were statistically analyzed using MetaXL version 5.3 (EpiGear International, Queensland, Australia). Heterogeneity assessment was performed by using the I2 statistic and x2 test. I2 statistic of >50% and/or a p-value of <0.1 for Cochran’s Q were deemed indicators of significant heterogeneity among studies. Using the random-effects model, the weighted average and confidence intervals (95% CI) were calculated.
Results and discussion
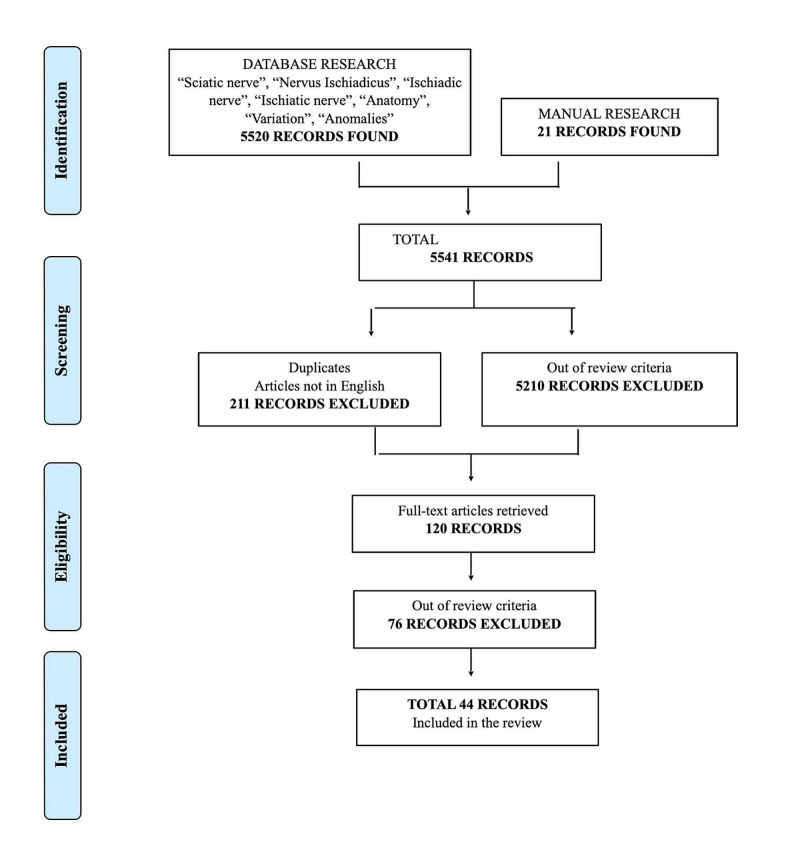
From the initial search, a total of 5,520 records were retrieved. Manual searching of reference lists yielded 21 additional articles. After exclusion of duplicates (211), articles not in English, and those irrelevant to the objectives of the present systematic review (5,210), 120 publications were retrieved in full text. Forty-four articles were deemed suitable for inclusion. The literature review selection process is summarized in Figure 2.
Figure 2. PRISMA flowchart summarizing the selection process.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Study Characteristics
Study characteristics of the included articles are summarized in Table 1. A total of 44 studies (8,257 samples) were included in the systematic review and meta-analysis [3,6-48]. Included studies were published from 1893 up to 2016, were written in the English language (or at least included an abstract written in English), and involved a population origin of wide geographical distribution. Geographic subgroup analysis was based on population characteristics, the geographic location, and the number of studies derived from each country.
Table 1. Characteristics of the cadaveric studies included in the systematic review.
aNo data reported with respect to geographic region. bData missing from one specimen. c1 additional variant not described in Beaton and Anson classification. d4 additional variants not described in Beaton and Anson classification: a variant with a PM with three muscle bellies and a CPN passing between superficial and intermediate muscle belly and the deep muscle belly passing through the TN; a variant in which the CPN passed between the two bellies of a double-headed PM and the TN passed below the PM; and two variants in which the SN passed below the PM and a supernumerary muscle located just superior to the PM (in the suprapiriform foramen)
Note: types E and F were excluded from the meta-analysis due to the limited number of studies that included them
SN: sciatic nerve; PM: piriformis muscle; CPN: common peroneal nerve; TN: tibial nerve
| Author | Year of publication | Country of population origin | Sample size | Type A, n (%) | Type B, n (%) | Type C, n (%) | Type D, n (%) | Type E, n (%) | Type F, n (%) | Total variations, n (%) |
| Paterson [6] | 1893 | Scotland (Europe) | 23 | 20 (87%) | 3 (13%) | - | - | - | - | 3 (13%) |
| Parsons and Keith [7] | 1897 | England (Europe) | 138 | 118 (85.5%) | 17 (12.3%) | 3 (2.1%) | - | - | - | 20 (14.4%) |
| Bardeen [8] | 1901 | USA | 246 | 220 (89.4%) | 25 (10.2%) | 1 (0,4%) | - | - | - | 26 (10.6%) |
| Trotter [9] | 1932 | USA | 464 | 400 (86.2%) | - | - | - | - | - | 64 (13.8%) |
| Beaton and Anson [3] | 1937 | USA | 240 | 216 (90%) | 17 (7%) | 5 (2%) | 2 (0.8%) | - | - | 24 (10%) |
| Ming-Tzu [10] | 1941 | China (East Asia) | 140 | 92 (65.7%) | 46 (32.9%) | - | 2 (1.4%) | - | - | 48 (34.3%) |
| Misra [11] | 1954 | India | 300 | 262 (87.3%) | 18 (6%) | 12 (4%) | 8 (2.7%) | - | - | 38 (12.6%) |
| Kubota et al. [12] | 1960 | Japan (East Asia) | 38 | 33 (86.8%) | - | 5 (13.2%) | - | - | - | 5 (13.2%) |
| Anson and McVay [13] | 1971 | USA | 2,008 | 1,789 (89.1%) | 201 (10%) | 13 (0.6%) | 5 (0.2%) | - | - | 219 (10.9%) |
| Nizankowski et al. [14] | 1972 | Poland (Europe) | 200 | 181 (90.5%) | 8 (4%) | 3 (1.5%) | 5 (2.5%) | 3 (1.5%) | - | 19 (9.5%) |
| Lee and Tsai [15] | 1974 | Taiwan (East Asia) | 168 | 118 (70.2%) | 33 (19.6%) | 7 (4.2%) | 3 (1.8%) | 1 (1.5%) | 2 (2.9%) | 50 (29.8%) |
| Pećina [16] | 1979 | Croatia (Europe) | 130 | 102 (78.5%) | 27 (20.8%) | 1 (0.7%) | - | - | - | 28 (21.5%) |
| Chiba [17] | 1992 | Japan (East Asia) | 511 | 328 (64.2%) | 173 (33.9%) | 10 (2%) | - | - | - | 183 (35.8%) |
| Chiba et al. [18] | 1994 | Japan (East Asia) | 442 | 285 (64.5%) | 148 (33.5%) | 9 (2%) | - | - | - | 157 (35.5%) |
| Georgiadis et al. [19] | 1996 | USA | 42 | 40 (95.2%) | 2 (4.8%) | - | - | - | - | 2 (4.8%) |
| Gabrielli et al. [20] | 1997 | Brazil | 80 | 69 (86.2%) | 9 (11.3%) | 2 (2.5%) | - | - | - | 11 (13.7%) |
| Pokorný et al. [21] | 1998 | Czech Republic (Europe) | 51 | 41 (80.4%) | 7 (13.7%) | 2 (3.9%) | 1 (2%) | - | - | 10 (19.6%) |
| Uluutku and Kurtoğlu [22] | 1999 | Turkey | 50 | 37 (74%) | 8 (16%) | 5 (10%) | - | - | - | 13 (26%) |
| Okraszewska et al. [23] | 2002 | Poland (Europe) | 36 | 29 (80.6%) | 2 (5.6%) | 2 (5.6%) | 3 (8.3%) | - | - | 7 (19.4%) |
| Fishman et al. [24] | 2002 | USA | 76 | 65 (85.5%) | - | - | - | - | - | 11 (14.5%) |
| Indrekvam et al. [25] | 2002 | Norway (Europe) | 19 | 15 (78.9%) | - | - | - | - | - | 4 (21.1%) |
| Benzon et al. [26] | 2003 | USA | 66 | 65 (98.4%) | 1 | - | - | - | - | 1 (1.6%) |
| Ndiaye et al. [27] | 2004 | Senegal (Africa) | 20 | 19 (95%) | - | - | - | - | 1 (5%) | 1 (5%) |
| Agur and Dalleya [28] | 2005 | 640 | 557 (87%) | 78 (12.2%) | 3 (0.5%) | - | - | - | 81 (12.7%) | |
| Ugrenović et al. [29] | 2005 | Serbia-Montenegro (Europe) | 200 | 192 (96%) | 5 (2.5%) | 3 (1.5%) | - | - | - | 8 (4%) |
| Pokorný et al. [30] | 2006 | Czech Republic (Europe) | 91 | 72 (79.1%) | 13 (14.3%) | 4 (4.4%) | 2 (2.2%) | - | - | 19 (20.9%) |
| Chukwuanukwu et al. [31] | 2007 | Nigeria (Africa) | 52 | 50 (96.2%) | 2 (3.8%) | - | - | - | - | 2 (3.8%) |
| Vincente et al. [32] | 2007 | Brazil | 40 | 34 (85%) | 6 (15%) | - | - | - | - | 6 (15%) |
| Pecina et al. [33] | 2008 | Croatia (Europe) | 10 | 7 (70%) | 3 (30%) | - | - | - | - | 3 (30%) |
| Güvençer et al. [34] | 2008 | Turkey | 50 | 38 (76%) | 7 (14%) | 4 (8%) | - | - | 11 (24%)b | |
| Kukiriza et al. [35] | 2010 | Uganda (Africa) | 80 | 62 (77.5%) | - | - | 18 (22,5%) | |||
| Brooks et al. [36] | 2011 | Brazil | 40 | 36 (90%) | - | - | 4 (10%) | - | - | 4 (10%) |
| Muthu Kumar et al. [37] | 2011 | India | 50 | 50 (100%) | - | - | - | - | - | 0 (0%) |
| Ogeng'o et al. [38] | 2011 | Kenya (Africa) | 164 | 147 (89.6%) | 13 (7.9%) | 4 (2.4%) | - | - | - | 17 (10.4%) |
| Patel et al. [39] | 2011 | India | 86 | 81 (94.2%) | 5 (5.8%) | - | - | - | - | 5 (5.8%) |
| Sabnis [40] | 2012 | India | 140 | 139 (99.3%) | - | 1 (0.7%) | - | - | - | 1 (0.7%) |
| Delabie et al. [41] | 2013 | France (Europe) | 104 | 94 (90.4%) | 10 (9.6%) | - | - | - | - | 10 (9.6%) |
| Prathiba et al. [42] | 2013 | India | 100 | 92 (92%) | 3 (3%) | 1 (1%) | - | - | 4 (4%) | |
| Adibatti and Sangeetha [43] | 2014 | India | 50 | 47 (94%) | - | - | - | - | - | 3 (6%) |
| Desalegn and Tesfay [44] | 2014 | Ethiopia (Africa) | 36 | 33 (91.7%) | 2 (5.6%) | - | - | - | - | 2 (5.6%)c |
| Gomes et al. [45] | 2014 | Brazil | 40 | 35 (87.5%) | 5 (12.5%) | - | - | - | - | 5 (12.5%) |
| Natsis et al. [46] | 2014 | Greece (Europe) | 294 | 275 (93.5%) | 12 (4.1%) | 1 (0.3%) | 1 (0.3%) | - | 1 (0.3%) | 14 (4.7%)d |
| Sulak et al. [47] | 2014 | Turkey | 400 | 392 (98%) | 5 (1.3%) | 3 (0.8%) | - | - | - | 8 (1.9%) |
| Lewis et al. [48] | 2016 | USA | 102 | 90 (88.2%) | 9 (8.8%) | 3 (2.9%) | - | - | - | 12 (11.8%) |
| Total | 8,257 | 7,067 | 923 | 106 | 37 | 4 | 4 | 1,177 | ||
| Total prevalence (confidence interval) | 90% (83-90%) | 8% (5-10%) | 2% (0-3%) | 1% (0-2%) | 13% (10-16%) | |||||
| I2 | 95% | 93% | ||||||||
| Cochrane’s Q, p-value | 0.00 | 0.00 | ||||||||
Prevalence of Sciatic Nerve Variants Relative to the Piriformis Muscle
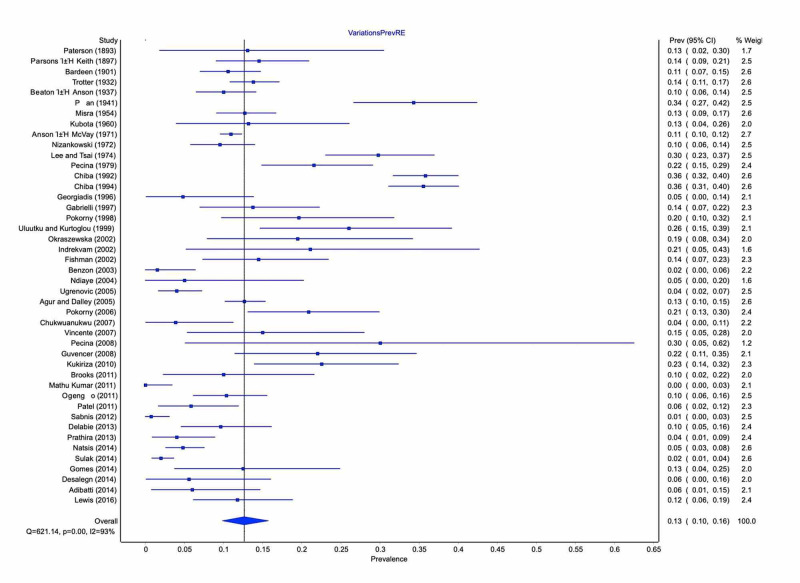
Type A was the most common morphological pattern with 90% pooled prevalence (95% CI: 83-90%) and represented the typical pattern. Total variants' pooled prevalence, including the unclassified type by Beaton and Anson [3], was 13% (95% CI: 10-16%) (Figure 3). Type B variant occurred in 8% (95% CI: 5-10%), followed by types C in 2% (95% CI: 0-3%) and D in 1% (95% CI: 0-2%).
Figure 3. Prevalence of anatomic variations of the SN relative to the PM.
SN: sciatic nerve; PM: piriformis muscle
Geographic subgroup analysis, summarized in Table 2, showed significant differences among populations. Turkey, Brazil, India, and the USA were independently analyzed since more than three studies originated from these regions, while studies derived from European, African, and East Asian countries were classified accordingly. East Asia presented the highest pooled prevalence [31% (95% CI: 26-37%)] of SN variants, followed by Turkey [14% (95% CI: 0-38%)]. In all the other regions, the upper CI limit of the variant patterns’ prevalence was less than 19%. SN variants’ distribution with respect to laterality was documented in nine studies (2,572 specimens) (Table 3). They were observed in the left side in 23% (95% CI: 16-31%), in the right side in 22% (95% CI: 13-32%), and bilaterally in 16% (95% CI: 7-26%). Only three studies (290 specimens) stated the gender of the included specimens (Table 4). Gender analysis showed a higher, but not significant, prevalence of variations in females [18% pooled prevalence (95% CI: 5-35%)] compared to males [11% (95% CI: 4-21%)].
Table 2. Subgroup analysis by geographic region.
| Geographic region | Type Α | Type Β | Type C | Type D | Total variations |
| Turkey | 85% (CI: 60-100%) | 9% (CI: 0-31%) | 2% (CI: 0-3%) | 0% (CI 0-9%) | 14% (CI: 0-38%) |
| Europe | 88% (CI: 81-91%) | 9% (CI: 6-14%) | 2% (CI: 0-4%) | 1% (CI 0-3%) | 14% (CI: 9-19%) |
| USA | 95% (CI: 84-96%) | 4% (CI: 1-9%) | 1% (CI: 0-3%) | 0% (CI: 0-2%) | 11% (CI: 9-13%) |
| Brazil | 89% (CI: 76-95%) | 8% (CI: 2-18%) | 1% (CI: 0-5%) | 2% (CI: 0-6%) | 13% (CI: 9-19%) |
| India | 97% (CI: 90-99%) | 2% (CI: 0-6%) | 1% (CI: 0-3%) | 1% (CI: 0-3%) | 4% (CI: 1-9%) |
| East Asia | 73% (CI: 59-79%) | 24% (CI: 14-33%) | 3% (CI: 0-7%) | 1% (CI: 0-3%) | 31% (CI: 26-37%) |
| Africa | 95% (CI: 82-95%) | 3% (CI: 0-8%) | 1% (CI: 0-4%) | 0% (CI: 0-2%) | 10% (CI: 5-17%) |
| Total | 90% (CI: 83-90%) | 8% (CI: 5-10%) | 2% (CI: 0-3%) | 1% (CI: 0-2%) | 13% (CI: 10-16%) |
Table 3. Sciatic nerve variants relative to piriformis muscle with respect to laterality.
L: left; R: right; B: bilateral
a3 of the specimens (1 left, 2 right) had unclassified variants in Beaton and Anson classification. bData missing from 3 specimens
| Author(s) (publication year) | Side (left, right) | Type A | Type Β | Type C | TypeD | Total | |||||||||||
| L | R | B | L | R | B | L | R | B | L | R | B | L | R | B | Total | ||
| Parsons and Keith [7] (1897) | 138 (69L, 69R) | 58 | 60 | - | 9 | 8 | - | - | - | - | 2 | 1 | - | 11, 15.9% | 9, 13% | - | 20, 14.5% |
| Ming-Tzu (1941) [10] | 140 (70L, 70R) | 45 | 47 | 36 | 24 | 22 | 13 | - | - | - | 1 | 1 | - | 25, 35.7% | 23, 32.9% | 13 | 48, 34.2% |
| Nizankowski et al.α (1972) [14] | 200 (99L, 101R) | 88 | 93 | - | 5 | 3 | - | - | 3 | - | 4 | 1 | - | 11, 11.1% | 8, 7.9% | - | 19, 9.5% |
| Chiba (1992) [17] | 511 (254L, 254R)b | 170 | 157 | 126 | 78 | 93 | 37 | 6 | 4 | 2 | - | - | - | 84 | 100 | 39 | 183 |
| Chiba et al. (1994) [18] | 442 (221L, 221R) | 148 | 137 | 113 | 68 | 80 | 35 | 5 | 4 | 2 | - | - | - | 73, 33% | 84, 38% | 37 | 157, 35.5% |
| Pokorný et al. (1998) [21] | 51 (28L, 23R) | 21 | 20 | - | 4 | 3 | - | 2 | - | - | 1 | - | - | 7, 25% | 3, 13% | - | 10, 19.6% |
| Uluutku and Kurtoğlu (1999) [22] | 50 (25L, 25R) | 18 | 19 | - | 4 | 4 | - | 3 | 2 | - | - | - | - | 7, 28% | 6, 24% | - | 13, 26% |
| Vincente et al. (2007) [32] | 40 (20L, 20R) | 17 | 17 | 17 | 3 | 3 | 3 | - | - | - | - | - | - | 3, 15% | 3, 15% | 3 | 6, 15% |
| Gomes et al. (2014) [45] | 40 (20L, 20R) | 18 | 17 | 17 | 2 | 3 | 2 | - | - | - | - | - | - | 2, 10% | 3, 15% | 2 | 5, 12.5% |
| Total | 2,572 | 583 | 567 | 309 | 214 | 224 | 100 | 16 | 14 | 4 | 7 | 3 | - | 283 | 290 | 124 | 573 |
| Total prevalence (confidence interval) | 77% (67-85) | 78% (67-88) | 62% (48-74) | 19% (12-28) | 19% (10-30) | 15% (7-26) | 2% (0-6) | 2% (0-6) | 1% (0-4) | 2% (0-5) | 1% (0-4) | 0% (0-3) | 23% (16-31) | 22% (13-32) | 16% (7-26) | ||
| I2 | 85% | 91% | 87% | 85% | 91% | 87% | 85% | 91% | 87% | 85% | 91% | 87% | 81% | 89% | 87% | ||
| Cochrane’s Q, p-value | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | ||
Table 4. Sciatic nerve variants relative to piriformis muscle with respect to gender.
M: males; F: females
a3 of the specimens (1 male, 2 females) had unclassified variants in Beaton and Anson classification
| Author (year of publication) | Number of samples (male, female) | Type A | Type Β | Type C | Type D | Total | ||||||
| M | F | M | F | M | F | M | F | M | F | Total | ||
| Nizankowski et al.α (1972) [14] | 200 (109M, 91F) | 99, 90% | 82, 91.1% | 4, 3.63% | 4, 4.4% | 2, 1.81% | 1, 1.1% | 2, 1.81% | 3, 3.33% | 8, 7.3% | 8, 8.8% | 19, 9.5% |
| Uluutku and Kurtoğlu (1999) [22] | 50 (14M, 36F) | 8, 57.14% | 29, 80.55% | 5, 35.71% | 3, 8.33% | 1, 7.14% | 4, 11.1% | - | - | 6, 42.8% | 7, 19.4% | 13, 26% |
| Gomes et al. (2014) [45] | 40 (34M, 6F) | 29, 85.29% | 6, 100% | - | 5, 83.3% | - | - | - | - | 5, 14.7% | 0, 0% | 5, 12.5% |
| Total | 290 (157M, 133F) | 136, 86.62% | 117, 88.96% | 9, 5.73% | 12, 9.02% | 3, 1.91% | 5, 3.76% | 2, 1.27% | 3, 2.25% | 14, 8.91% | 20, 15.3% | 37, 12.75% |
| Total prevalence (confidence interval) | 87% (76-98%) | 82% (59-97%) | 6% (0-16%) | 13% (0-34%) | 3% (0-14%) | 5% (0-14%) | 2% (0-10%) | 2% (0-9%) | 11% (4-21%) | 18% (5-35%) | ||
| I2 | 63% | 84% | 63% | 84% | 84% | 63% | 84% | 63% | 37% | 75% | ||
| Cochrane’s Q, p-value | 0.07 | 0.00 | 0.07 | 0.00 | 0.00 | 0.07 | 0.00 | 0.07 | 0.2 | 0.02 | ||
Discussion
The present systematic review and meta-analysis provides a comprehensive and evidence-based assessment of SN variants in relation to PM. Although typical (type A) morphological pattern was the most common one (90% prevalence), its presence widely varied (64.5-100%) among the selected studies. The variant type B had 8% prevalence, followed by types C and D with 2% and 1% prevalence, respectively. Type B had a significantly higher prevalence in East Asia (24% prevalence) compared to Europe (9%), the USA (4%), and Africa (3%). Concerning gender impact, females appeared to have a higher, but not significant, prevalence of SN variants compared to males. Type B variant was twice as prevalent in females (13% prevalence) compared to males (6%). This finding could be explained by the SN's close proximity to female reproductive organs. Thus, patients’ epidemiological characteristics may predispose them to certain variants. Analysis based on laterality revealed symmetry in typical SN anatomy (62% prevalence), as well as in variant patterns' occurrence (16% prevalence).
An awareness of SN variants is essential to avoid iatrogenic nerve injury [41-44,48]. The two most common mechanisms of nerve injury, intraoperatively, are stretching and direct injury (compression or laceration) [41-43]. The SN is subject to traction forces during total hip arthroplasty, especially when performed via a posterior approach [29,30]. Therefore, SN variants relative to the PM increase the intraoperative risk of injury, either due to improper Hohmann retractor placement or by direct injury when a PM tenotomy is required [45]. The CPN is more susceptible to injury by traction when the variant types B and C are encountered, either during hip dislocation or when the lengthening of the extremity occurs [45]. The SN may also be injured after traumatic posterior hip dislocation [45], and in such cases, the coexistence of variants in the area increases the risk of injury.
Hip arthroscopy and specifically the posterolateral portal placement (as close as 11 mm to the SN) may injure the SN due to its close proximity. Type B variant may put the SN at an increased risk of injury during hip arthroscopy. Moreover, knowledge of SN variants is necessary when the SN blockade is conducted. There is a high probability of anesthetizing only the CPN or the TN when an SN high bifurcation is present, as in types B and C [39].
The piriformis syndrome is characterized by sciatic clinical manifestations caused by extrapelvic SN compression at the hip. An incidence of 6% of piriformis syndrome has been reported in patients suffering from sciatica [23,34]. Typical clinical manifestations include buttock pain with or without radiation to the ipsilateral posterior thigh and the occasional extension below the knee [4]. Pain is exacerbated by flexion, adduction, and internal rotation of the hip. Aberrations of the SN course may contribute to its compression. Pećina has suggested that type B variant (CPN course through the PM) is more commonly associated with piriformis syndrome, and especially when the CPN passes between PM tendinous parts [16]. The clinician should consider the SN variants when treating a patient with sciatica and especially when dealing intraoperatively with a piriformis syndrome [24,26].
Multiple imaging modalities are available for SN variant identification. Among them, MRI remains the gold standard. Magnetic resonance neurography can reliably and effectively identify the presence of an SN variant or even SN compression in piriformis syndrome [32,33].
Study limitations
This study has some limitations. Many studies we looked into had modified the classification system proposed by Beaton and Anson or had included variants that were stated as “non-classified”. High heterogeneity was observed among the studies, which could not be explained by geographic or gender differences alone.
Conclusions
Based on our findings, type A (a single SN trunk coursing below the PM) is the most common morphological type and is considered as the typical pattern. SN variants are fairly common, particularly among East Asians. Clinicians should always bear in mind those variants when performing hip interventions, nerve blockade in the area, and during diagnosis and treatment of piriformis syndrome. Future clinical investigations are necessary to further evaluate SN atypical course clinical implications in relation to the PM.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Microanatomical structure of the human sciatic nerve. Sladjana UZ, Ivan JD, Bratislav SD. Surg Radiol Anat. 2008;30:619–626. doi: 10.1007/s00276-008-0386-6. [DOI] [PubMed] [Google Scholar]
- 2.Keibel F, Mall FP. Philadelphia, PA: J. B. Lippincott Company; 1910. Manual of Human Embryology. [Google Scholar]
- 3.The relation of the sciatic nerve and of its subdivisions to the piriformis muscle. Beaton LE, Anson BJ. Anat Rec. 2005;70:1–5. [Google Scholar]
- 4.Piriformis syndrome and low back pain: a new classification and review of the literature. Papadopoulos EC, Khan SN. Orthop Clin North Am. 2004;35:65–71. doi: 10.1016/S0030-5898(03)00105-6. [DOI] [PubMed] [Google Scholar]
- 5.Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. PLoS Med. 2009;6:0. [PMC free article] [PubMed] [Google Scholar]
- 6.The origin and distribution of the nerves to the lower limb. Paterson AM. https://pubmed.ncbi.nlm.nih.gov/17232071/ J Anat Physiol. 1893;28:84–95. [PMC free article] [PubMed] [Google Scholar]
- 7.Sixth Annual Report of the Committee of Collective Investigation of the Anatomical Society of Great Britain and Ireland, 1895-96. Parsons FG, Keith A. https://pubmed.ncbi.nlm.nih.gov/17232229/ J Anat Physiol. 1896;31:31–44. [PMC free article] [PubMed] [Google Scholar]
- 8.Development and variation of the musculature of the inferior extremity and the neighboring regions of the trunk in man. Bardeen CR. Am J Anat. 1906;6:259–390. [Google Scholar]
- 9.The relation of the sciatic nerve to the piriformis muscle in American whites and negroes. Trotter M. Anat Rec. 1932;52:321–323. [Google Scholar]
- 10.The relation of the sciatic nerve to the piriformis muscle in the Chinese. Ming-Tzu P. Am J Phys Anthropol. 1941;28:375–380. [Google Scholar]
- 11.The relations of the sciatic nerve to the piriformis in Indian cadavers. Misra BD. J Anat Soc India. 1954;3:28–33. [Google Scholar]
- 12.Rare types of relation between the sciatic nerve and the piriformis muscle. Kubota K, Noguchi I, Nakano T. Okajimas Folia Anat Jap. 1960;36:329–343. [Google Scholar]
- 13.Anson B, McVay CB. Philadelphia, PA: Saunders; 1971. Surgical Anatomy. [Google Scholar]
- 14.Variations in the anatomy of the sciatic nerve in man (Article in Polish) Nizankowski C, Slociak J, Szybejko J. https://pubmed.ncbi.nlm.nih.gov/4539117/ Folia Morphol (Warsz) 1972;31:507–513. [PubMed] [Google Scholar]
- 15.The relation of the sciatic nerve to the piriformis muscle (Article in Chinese) Lee CS, Tsai TL. https://pubmed.ncbi.nlm.nih.gov/4527572/ Taiwan Yi Xue Hui Za Zhi. 1974;73:75–80. [PubMed] [Google Scholar]
- 16.Contribution to the etiological explanation of the piriformis syndrome. Pećina M. https://pubmed.ncbi.nlm.nih.gov/532546/ Acta Anat (Basel) 1979;105:181–187. [PubMed] [Google Scholar]
- 17.Multiple positional relationships of nerves arising from the sacral plexus to the piriformis muscle in humans (Article in Japanese) Chiba S. https://pubmed.ncbi.nlm.nih.gov/1296428/ Kaibogaku Zasshi. 1992;67:691–724. [PubMed] [Google Scholar]
- 18.Perforation of dorsal branches of the sacral nerve plexus through the piriformis muscle and its relation to changes of segmental arrangements of the vertebral column and others (Article in Japanese) Chiba S, Ishibashi Y, Kasai T. https://pubmed.ncbi.nlm.nih.gov/8091946/ Kaibogaku Zasshi. 1994;69:281–305. [PubMed] [Google Scholar]
- 19.Entry sites for antegrade femoral nailing. Georgiadis GM, Olexa TA, Ebraheim NA. Clin Orthop Relat Res. 1996;330:281–287. doi: 10.1097/00003086-199609000-00036. [DOI] [PubMed] [Google Scholar]
- 20.Inferior gluteal nerve course associated to the high division of the sciatic nerve. Gabrielli C, Olave E, Mandiola E, et al. https://www.biologyonline.com/articles/inferior-gluteal-nerve-course Rev Chil Anat. 1997;15:79–83. [Google Scholar]
- 21.Anatomic variability of the relation of pelvitrochanteric muscles and sciatic nerve (Article in Czech) Pokorný D, Sosna A, Veigl P, Jahoda D. https://pubmed.ncbi.nlm.nih.gov/20492810/ Acta Chir Orthop Traumatol Cech. 1998;65:336–339. [PubMed] [Google Scholar]
- 22.Variations of nerves located in deep gluteal region. Uluutku MH, Kurtoğlu Z. Okajimas Folia Anat Jpn. 1999;76:273–276. doi: 10.2535/ofaj1936.76.5_273. [DOI] [PubMed] [Google Scholar]
- 23.Sciatic nerve variations in some studies on the Polish population and its statistical significance. Okraszewska E, Migdalski L, Jedrzejewski KS, Bolanowski W. https://pubmed.ncbi.nlm.nih.gov/12725497/ Folia Morphol (Warsz) 2002;61:277–282. [PubMed] [Google Scholar]
- 24.Piriformis syndrome: diagnosis, treatment, and outcome--a 10-year study. Fishman LM, Dombi GW, Michaelsen C, Ringel S, Rozbruch J, Rosner B, Weber C. Arch Phys Med Rehabil. 2002;83:295–301. doi: 10.1053/apmr.2002.30622. [DOI] [PubMed] [Google Scholar]
- 25.Piriformis muscle syndrome in 19 patients treated by tenotomy--a 1- to 16-year follow-up study. Indrekvam K, Sudmann E. Int Orthop. 2002;26:101–103. doi: 10.1007/s00264-001-0319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Benzon HT, Katz JA, Benzon HA, Iqbal MS. Anesthesiology. 2003;98:1442–1448. doi: 10.1097/00000542-200306000-00022. [DOI] [PubMed] [Google Scholar]
- 27.Sciatic nerve in gluteal portion: application of sciatic nerve post injection lesion (Article in French) Ndiaye A, Sakho Y, Fall F, Dia A, Sow ML. Morphologie. 2004;88:135–138. doi: 10.1016/s1286-0115(04)98136-2. [DOI] [PubMed] [Google Scholar]
- 28.Agur AM, Dalley AF. Philadelphia, PA: Lippincott Williams and Wilkins; 2015. Grant’s Atlas of Anatomy. [Google Scholar]
- 29.The level of the sciatic nerve division and its relations to the piriform muscle (Article in Serbian) Ugrenović S, Jovanović I, Krstić V, Stojanović V, Vasović L, Antić S, Pavlović S. Vojnosanit Pregl. 2005;62:45–49. doi: 10.2298/vsp0501045u. [DOI] [PubMed] [Google Scholar]
- 30.Topographic variations of the relationship of the sciatic nerve and the piriformis muscle and its relevance to palsy after total hip arthroplasty. Pokorný D, Jahoda D, Veigl D, Pinskerová V, Sosna A. Surg Radiol Anat. 2006;28:88–91. doi: 10.1007/s00276-005-0056-x. [DOI] [PubMed] [Google Scholar]
- 31.Bilateral high division of the sciatic nerve: incidence and clinical implications in Nigeria. Chukwuanukwu T, Ukoha UU, Chukqujekwu IE, et al. Trop J Med Res. 2007;11:12–13. [Google Scholar]
- 32.Study on anatomical relationships and variations between the sciatic nerve and piriform muscle. Vincente EJD, Viotto MJS, Barbosa CAA, Vincente PC. Rev Bras Fisioter. 2007;11:227–232. [Google Scholar]
- 33.Surgical evaluation of magnetic resonance imaging findings in piriformis muscle syndrome. Pecina HI, Boric I, Smoljanovic T, Duvancic D, Pecina M. Skeletal Radiol. 2008;37:1019–1023. doi: 10.1007/s00256-008-0538-0. [DOI] [PubMed] [Google Scholar]
- 34.Variations in the high division of the sciatic nerve and relationship between the sciatic nerve and the piriformis. Güvençer M, Iyem C, Akyer P, Tetik S, Naderi S. https://pubmed.ncbi.nlm.nih.gov/19431123/ Turk Neurosurg. 2009;19:139–144. [PubMed] [Google Scholar]
- 35.Levels of bifurcation of the sciatic nerve among Ugandans at School of Biomedical Sciences Makerere and Mulago Hospital Uganda. Kukiriza J, Kiryowa H, Turyabahika J, Ochieng J, Ibingira CB. https://www.semanticscholar.org/paper/Levels-of-Bifurcation-of-the-Sciatic-Nerve-among-at-Kukiriza-Kiryowa/732391864ae7d48c31bc31415001e392e2ee6bdf East Cent African J Surg. 2010;15:69–75. [Google Scholar]
- 36.Anatomical variations of the sciatic nerve in a group of Brazilian cadavers (Article in Portuguese) Brooks JBB, Silva CAC, Soares SA, Kai MR, Cabral RH, Fragoso YD. Revista Dor Sao Paulo. 2011;12:332–336. [Google Scholar]
- 37.A cadaveric study of sciatic nerve and its level of bifurcation. Muthu Kumar T, Srimathi Srimathi, Rani A, Latha S. https://www.researchgate.net/publication/288227500_A_cadaveric_study_of_sciatic_nerve_and_it's_level_of_bifurcation J Clin Diag Res. 2011;5:1502–1504. [Google Scholar]
- 38.Variant anatomy of sciatic nerve in a black Kenyan population. Ogeng'o JA, El-Busaidy H, Mwika PM, Khanbhai MM, Munguti J. https://pubmed.ncbi.nlm.nih.gov/21866528/ Folia Morphol (Warsz) 2011;70:175–179. [PubMed] [Google Scholar]
- 39.A variation in the high division of the sciatic nerve and its relation with piriformis muscle. Patel SV, Shah M, Vora R, Zalawadia A, Rathod SP. https://www.researchgate.net/publication/303223379_A_variation_in_the_high_division_of_the_sciatic_nerve_and_its_relation_with_piriformis_muscle Natl J Med Res. 2011;1:27–30. [Google Scholar]
- 40.Anatomical variations of sciatic nerve bifurcation in human cadavers. Sabnis AS. https://bioinfopublication.org/files/articles/3_2_4_JCRL.pdf J Clin Res Lett. 2012;3:46–48. [Google Scholar]
- 41.Relationships between piriformis muscle and sciatic nerve: radioanatomical study with 104 buttocks (Article in French) Delabie A, Peltier J, Havet E, Page C, Foulon P, Le Gars D. Morphologie. 2013;97:12–18. doi: 10.1016/j.morpho.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 42.A cadaveric study on anatomical variations of sciatic nerve in relation to pyriformis muscle in Andhra Pradesh region. Prathiba K, Madan S, Udaya Kumar P, Dharmendar P, Nisha Nisha. https://www.ijcrr.com/article_html.php?did=1044 Int J Curr Res Rev. 2013;5:56–60. [Google Scholar]
- 43.Study on variant anatomy of sciatic nerve. Adibatti M, Sangeetha V. J Clin Diagn Res. 2014;8:0. doi: 10.7860/JCDR/2014/9116.4725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Variations of sciatic nerve its exit in relation to piriformis muscle in the Northern Ethiopia. Desalegn M, Tesfay A. https://www.semanticscholar.org/paper/Variations-of-Sciatic-Nerve-Its-Exit-in-Relation-to-Desalegn-Tesfay/ef65c286a838b3e7463cdbaa5128777e5bfb614e Int J Pharma Sci Res. 2014;5:953–956. [Google Scholar]
- 45.Topographic anatomical study of the sciatic nerve relationship to the posterior portal in hip arthroscopy. Gomes BA, Ramos MR, Fiorelli RK, Almeida CR, Fiorelli SK. Rev Col Bras Cir. 2014;41:440–444. doi: 10.1590/0100-69912014006010. [DOI] [PubMed] [Google Scholar]
- 46.Anatomical variations between the sciatic nerve and the piriformis muscle: a contribution to surgical anatomy in piriformis syndrome. Natsis K, Totlis T, Konstantinidis GA, Paraskevas G, Piagkou M, Koebke J. Surg Radiol Anat. 2014;36:273–280. doi: 10.1007/s00276-013-1180-7. [DOI] [PubMed] [Google Scholar]
- 47.Anatomical relation between sciatic nerve and piriformis muscle and its bifurcation level during fetal period in human. Sulak O, Sakalli B, Ozguner G, Kastamoni Y. Surg Radiol Anat. 2014;36:265–272. doi: 10.1007/s00276-013-1179-0. [DOI] [PubMed] [Google Scholar]
- 48.Anatomical variations of the sciatic nerve, in relation to the piriformis muscle. Lewis S, Jurak J, Lee C, Lewis R, Gest T. Transl Res Anat. 2016;5:15–19. [Google Scholar]