Abstract
Cancer is a leading cause of death in small island nations and is forecast to increase substantially over the coming years. Governments, regional agencies, and health services of these nations face daunting challenges, including small and fragile economies, unequal distribution of resources, weak or fragmented health services, small population sizes that make sustainable workforce and service development problematic, and the unavailability of specialised cancer services to large parts of the population. Action is required to prevent large human and economic costs relating to cancer. This final Series paper highlights the challenges and opportunities for small island nations, and identifies ways in which the international community can support efforts to improve cancer control in these settings. Our recommendations focus on funding and investment opportunities to strengthen cancer-related health systems to improve sharing of technical assistance for research, surveillance, workforce, and service development, and to support small island nations with policy changes to reduce the consumption of commodities (eg, tobacco and unhealthy food products) that increase cancer risk.
Introduction
In 1992, the UN formally recognised a group of small island nations that faced “specific social, economic and environmental vulnerabilities”.1 These countries vary substantially in their development, size, cultures, languages, and history, but they also share specific features, including geographical isolation, fragile economies, ageing populations, and environments affected by global warming, which make them vulnerable to natural disasters. Most states have small populations and limited economies of scale and are therefore heavily reliant on resources from larger neighbouring countries, despite the high cost of transport, infrastructure, and communications.1 Another common feature of these countries that is that they often have underdeveloped health systems, including few workforce resources.
Although no specific criteria exists in the classification of a small island nation, more than 50 countries (not all of them islands) are recognised as such (panel 1; figure).2 Small island nations are located across three broad geographical areas: the Pacific, the Caribbean, and the Atlantic and Indian Oceans, the Mediterranean Sea, and the South China Sea (AIMS). Small island nations are represented by several regional organisations, including the Caribbean community, the Pacific community, the Indian Ocean commission, and the alliance of small island nations, which acts as a regional integration forum to address common challenges of economic, social, and sustainable human development. Some regional organisations deal specifically with health issues; for example, the Caribbean Public Health Agency3 has a focus on communicable diseases, disaster management, and the surveillance and prevention of non-communicable diseases (NCDs), whereas the Pan American Health Organization (PAHO) operates as the regional office of the Americas for WHO, and the Health Agency of the Organization of American States.
Panel 1: Small island nations2.
Caribbean
Anguilla, Antigua and Barbuda, Aruba, The Bahamas, Barbados, Belize, Bermuda, Bonaire, Sint Eustatius, Saba, British Virgin Islands, Cayman Islands, Curaçao, Cuba, Dominica, Dominican Republic, Grenada, Guadeloupe, Guyana, Haiti, Jamaica, Martinique, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago, Turks and Caicos Islands, and Virgin Islands
Pacific
American Samoa, Cook Islands, Federated States of Micronesia, Fiji, French Polynesia, Guam, Kiribati, Marshall Islands, Nauru, New Caledonia, Niue, Northern Mariana Islands, Palau, Papua New Guinea, Samoa, Solomon Islands, Timor-Leste (In this Series, Timor-Leste is considered to be a small island nation of Africa, Indian Ocean, Mediterranean and South China Seas, rather than the Pacific, because of its political and social ties with the southeast Asia region), Tonga, Tuvalu, Vanuatu, and Wallis and Futuna
Africa and Indian Ocean, Mediterranean Sea, and South China Seas
Bahrain, Cape Verde, Comoros, Guinea-Bissau, Maldives, Mauritius, São Tomé and Príncipe, Seychelles, and Singapore
Figure:
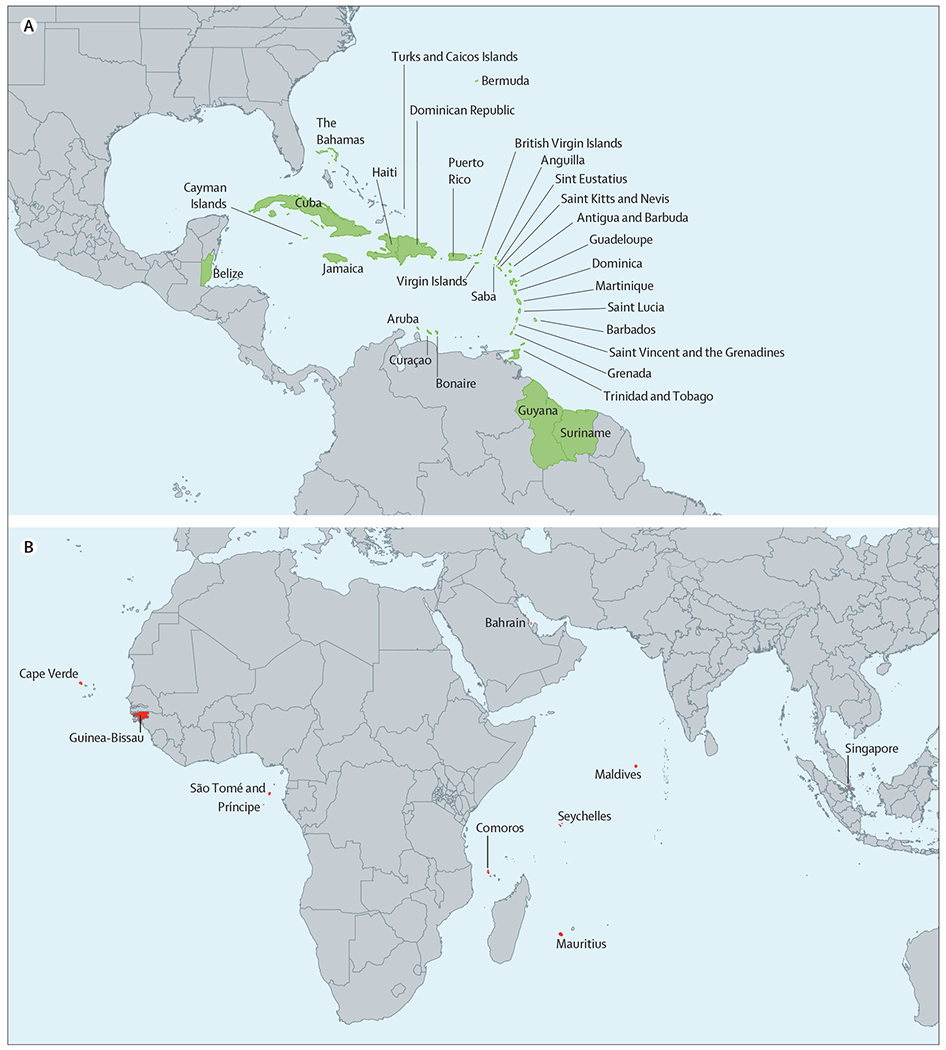
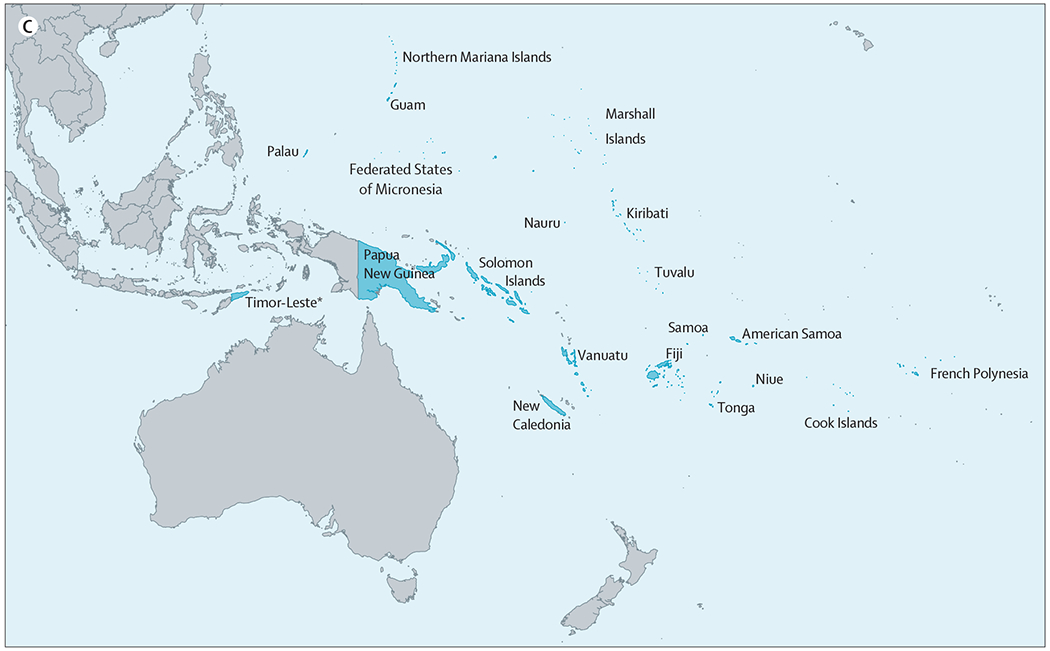
Map of the UN small island nations
This Series paper is the final of five papers examining cancer control in small island nations. The first two Series papers focus on the Pacific region, and the second two on the Caribbean. Challenges and opportunities across the cancer continuum are identified in those papers, with recommendations provided for each region. To conclude these four papers, this paper aims at providing more detailed information relating to the small island nations in the AIMS, similar to that presented for the Pacific region (papers 1 and 2 in the Series)4,5 and the Caribbean (papers 3 and 4 in the Series).6,7 We then identify key themes, issues, and barriers that arise in cancer control in the context of small island nations. Some of these factors are common to other countries and regions (eg, the need to focus on the prevention of NCDs more generally) but the focus here is to focus primarily on the factors that are particularly relevant to small island nations. Finally, we identify priority actions for small island nations and recommend actions to the global cancer control community that would facilitate and support small island nations in their efforts to improve cancer control in their own countries and regions.
Cancer control
The unique and heterogeneous nature of small island nations is often overlooked within agendas for cancer control at the global level or within low-income and middle-income country health policy. The small size of these nations is associated with capacity issues in key aspects of cancer prevention and control, from functioning registries to access to radiotherapy facilities. This Series paper aims to highlight specific challenges and opportunities for small island nations and to identify ways in which the international community can support governments, academic institutions, and civil society efforts to improve cancer control in these settings.
Pacific and Caribbean regions
The Pacific and Caribbean regions share characteristics common to (most) small island nations; that is, small, geographically dispersed populations with limited financial and health-care resources. Both regions also struggle with adequate human resources for health care and are often key sites to the effects of global warming and natural disasters, with six of the 15 countries at highest risk (globally) of being affected by the effects of global warming (Vanuatu, Tonga, Solomon Islands, Papua New Guinea, Fiji, and Kiribati) located in the Pacific.8 Countries in the Pacific and the Caribbean have gaps in policy and intervention along the continuum of cancer control, although the scope and possible solutions to these problems differ between regions. Despite these challenges, the fairly small populations and strong cohesion across the two regions could offer opportunities for flexibility and innovation in collective approaches to cancer control.9 On a global level, small island nations have frequently formed an effective lobby for advocating increased attention to climate change and the effects on their economies and environments.10 Both regions have strong links with the Commonwealth (panel 2)
Panel 2: Role of the Commonwealth in cancer control in small island nations.
Many countries in both the Caribbean and Pacific belong to the Commonwealth, which provides a sense of connection and community in a shifting global landscape. Many island populations in the Caribbean identify more closely with the Commonwealth than with Latin America, whereas the Pacific includes 11 Commonwealth member states, all discrete island nations, except Papua New Guinea. The Commonwealth’s networks and convening power means it can contribute to cancer control efforts in these regions.
The Commonwealth provides representation at international forums, such as the UN, high-level advocacy on issues relevant to member countries, and has a track record for affecting change in issues of common concern, such as climate change and antimicrobial resistance.
Consistent with the UN’s third Sustainable Development Goal and political declaration on non-communicable diseases, the Commonwealth has recognised non-communicable diseases as “a human development challenge which needs to be tackled urgently”11 and has expressed commitment to raising awareness, mobilising resources, and ensuring accessibility to the necessary prevention and treatment services.11–14 In relation to cancer, the Commonwealth has led some relevant initiatives. For example, the Cervical Cancer in the Commonwealth: Collective Action programme15 has analysed the burden of cervical cancer in low-income and middle-income countries of the Commonwealth.
However, much more needs to be done and this Series should encourage further action from the Commonwealth on cancer. New initiatives, such as the Commonwealth Innovation Hub, have the potential to enhance and coordinate efforts in cancer control in member states. There have been calls to establish a Commonwealth cancer fund to “build up capacity in cancer control in the smaller and less economically advantaged Member States through skills training and multilateral aid.”16 In relation to the Caribbean and Pacific islands, there is interest in Commonwealth support for human papillomavirus vaccination and cervical screening in its member states, and for improvements in the early detection, diagnosis, and treatment of childhood cancers.17
Heterogeneity within and between these two regions is substantial. The Caribbean has considerably more wealth, albeit distributed very unevenly both within and between countries.18 Many countries have high debtservicing pressures and fragile economies, yet countries that are categorised as upper-middle income and high-income countries (HICs) are often not eligible for financial assistance from international groups and organisations.19 Private health care plays a substantially larger role in specialised cancer care, with private–public partnerships representing a prominent approach to delivering the care needed for the region.6
In the Pacific, cancer care is less available because of the very small populations and vast geographic distances involved. In the Caribbean, treatment requiring substantial capital or infrastructure (eg, radiotherapy) is available in some countries, but is frequently met with challenges in maintaining quality and is usually accessible only to those who are able to pay. In the Pacific, specialist facilities are often absent altogether, meaning that many treatments are available only to those who can afford to seek them in neighbouring countries. Thus, both regions experience marked inequalities in access to cancer care, though the underlying mechanisms which make these inequalities possible are somewhat different.
Islands outside of the Pacific and Caribbean regions
Outside of the Pacific and Caribbean regions there are other UN-recognised small island nations, collectively referred to as the AIMS small island nations (table 1).20–24 Variation is marked between AIMS small island nations (table 1). At one end of the spectrum, Singapore and Bahrain are HICs with national population-based cancer registries, operational plans for cancer and NCDs, and comprehensive cancer services that provide specialised surgery, chemotherapy, radiotherapy, and palliative care. Conversely, advances in cancer surveillance, screening and prevention, diagnosis, and care are inadequate in almost all other AIMS small island nations. For instance, the Comoros and Guinea-Bissau are among the poorest countries in the world and struggle to meet their populations’ basic needs either in sanitation, nutrition, transportation, and basic health care. Life expectancy is low (59·8 years for Guinea-Bissau and 63·9 years for the Comoros), and fragile health systems are burdened by multiple competing priorities, including management of infectious diseases. Long periods of civil unrest in Guinea-Bissau have resulted in debilitated health systems, substantial workforce shortages, and delayed progress in health infrastructure development. The double burden of lifestyle and infection-related cancers is evident in many of these small island nations, with GLOBOCAN 201824 estimates showing that the most common cancers in AIMS small island nations are breast, cervical, and colorectum in women, and colorectum, prostate, liver, and lung in men (table 2).
Table 1:
Characteristics of small island nations in the Atlantic and Indian ocean, Mediterranean Sea, and South China seas20–24
| Estimated population (2017) | Income classification | GDP per capita (current US$, 2017) | Health expenditure as % of GDP (2015) | Life expectancy at birth (years) | Health staff per 10 000 population | Cancer registration | National cancer plan (year) | Current NCD plan | HBV vaccination coverage (BD %) | HBV vaccination coverage (B3 %) | HPV vaccination on national schedule | Organised national screening programme available | Radiology services | Pathology services | Publicly available cancer treatment services | Oral morphine available in public health sector | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bahrain | 1 492 584 | High | 23 655 | 5·2% | 79·1 | 9·3 doctors, 24·9 nurses | National high quality PBCR | Yes (2010–20) | Yes | 98% | 98% | No | Breast | x-ray, ultrasound, mammography, CT, MRI, PET | Cytology, histology, immunohistochemistry | Surgery, chemotherapy, and radiotherapy | Yes |
| Cabo Verde | 546 388 | Lower middle | 3244 | 4·8% | 73·2 | 7·7 doctors, 10 nurses | Registration activity | Yes (2015) | Yes | 96% | 96% | No | No | x-ray, ultrasound, and mammography | n/a | Surgery and chemotherapy | No |
| Comoros | 813 912 | Lower middle | 1312 | 8·0% | 63·9 | 1·7 doctors, 7 nurses | No data | No | Yes | n/a | 91% | No | No | x-ray and ultrasound | n/a | Surgery | No |
| Guinea-Bissau | 1 861 283 | Low | 724 | 6·9% | 59·8 | 0·6 doctor, 6·9 nurses | No data | No | No | n/a | 79% | No | No | x-ray, ultrasound, mammography, and CT | n/a | Surgery | No |
| Maldives | 436 330 | Upper middle | 11 151 | 11·5% | 78·4 | 10·4 doctors, 57·2 nurses | No data | No | Yes | 99% | 99% | Yes | No | x-ray, ultrasound, mammography, CT, and MRI | Cytology and histology | Surgery and chemotherapy | No |
| Mauritius | 1 264 613 | Upper middle | 10 490 | 5·5% | 74·8 | 20·2 doctors, 32·8 nurses | PBCR | Yes (2015–19) | No | n/a | 96% | Yes | No | x-ray, ultrasound, mammography, CT, MRI | Cytology, histology, and IHC | Surgery, chemotherapy, and radiotherapy | Yes |
| São Tomé and Príncipe | 204 327 | Lower middle | 1921 | 9·8% | 68.7 | 3·2 doctors | No data | No | No | 95% | 93% | Yes | No | x-ray, ultrasound, and CT | n/a | Surgery | No |
| Seychelles | 95 843 | High | 15 629 | 3·4% | 73·3 | 9·5 doctors, 44·9 nurses | PBCR | No | Yes | n/a | 97% | Yes | No | x-ray, ultrasound, mammography, CT, and MRI | Cytology, histology, and immunohistochemistry | Surgery and chemotherapy | Yes |
| Singapore | 5 612 253 | High | 57 714 | 4·3% | 82·9 | 23·1 doctors, 58·3 nurses | National high quality PBCR | Yes | No | 91% | 96% | Yes | Cervical, breast, colorectal | x-ray, ultrasound, mammography, CT, MRI, and PET | Cytology, histology, and immunohistochemistry | Surgery, chemotherapy, and radiotherapy | Yes |
| Timor-Leste* | 1 296 311 | Lower middle | 2279 | 3·1% | 68·6 | 6·7 doctors, 13·6 nurses | No data | No | Yes | 62% | 92% | No | No | x-ray, ultrasound, and CT | n/a | Surgery | No |
GDP=gross domestic product. NCD=non-communicable disease. HBV=hepatitis B virus. BD=birth dose. B3=infant doses. HPV=human papillomavirus. PRCR=population-based cancer registry.
In this Series, Timor-Leste is considered to be an Africa, Indian Ocean, Mediterranean and South China Seas small island nation (rather than Pacific) because of its political and social ties with the south-east Asia region.
Table 2:
Top five most commonly diagnosed cancers in men and women from small island nations in the Atlantic and Indian Ocean, Mediterranean Sea, and South China Sea24
| Most frequent cancers in men | Most frequent cancers in women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |
| Bahrain | Colorectum | Lung | Prostate | Bladder | NHL | Breast | Colorectum | Ovary | Uterine | Thyroid |
| Cape Verde | Prostate | Stomach | Oesophagus | Lung | Liver | Cervix | Breast | Stomach | Colorectum | Liver |
| Comoros | Prostate | Oesophagus | Liver | NHL | Colorectal | Cervix | Breast | Oesophagus | NHL | Liver |
| Guinea-Bissau | Liver | Prostate | Stomach | Colorectum | NHL | Cervix | Breast | Liver | Colorectum | Stomach |
| Maldives | Lung | Colorectum | Nasopharynx | Liver | Prostate | Breast | Cervix | Ovary | Thyroid | Colorectum |
| Mauritius | Prostate | Lung | Colorectum | Stomach | Bladder | Breast | Colorectum | Cervix | Uterine | Ovary |
| São Tomé and Príncipe | Prostate | Lung | Stomach | Liver | Bladder | Cervix | Breast | Ovary | Lung | Stomach |
| Singapore | Prostate | Lung | Colorectum | Liver | Kidney | Breast | Colorectum | Lung | Uterine | Ovary |
| Timor-Leste* | Lung | Colorectum | Nasopharynx | Liver | Prostate | Breast | Cervix | Colorectum | Lung | Ovary |
NHL=non-Hodgkin lymphoma.
In this Series, Timor-Leste is considered to be an Africa, Indian Ocean, Mediterranean and South China Seas small island nation (rather than Pacific) because of its political and social ties with the south-east Asia region. Seychelles has been excluded. The value 1 represents the most commonly diagnosed cancer whilst the value 5 represents the fifth most commonly diagnosed cancer.
Outside of Bahrain and Singapore, cancer surveillance and prevention programmes are absent or insufficient to meet the needs of the population. Mauritius and Seychelles are the only other AIMS countries (besides Bahrain and Singapore) to have population-based cancer registries, although pockets of cancer registration activity occur elsewhere (eg, Cape Verde has a hospital-based cancer registry). Despite the high burden of preventable cancers, none of these countries have established national screening programmes for cervical or breast cancers, and only two (Mauritius and Cape Verde) have operational standalone cancer plans in place. More positively, uptake of hepatitis B immunisation has been successful with >90% coverage in most of these AIMS small island nations. A growing number of small island nations are incorporating human papillomavirus vaccination into their national schedules, with the Maldives approving HPV vaccinations for 9–15 year-old girls.25 As with other small island nations, many cancer prevention and educational campaigns in these countries are led by nongovernmental organisations (NGOs) or patient groups.26
Diagnostic and treatment services are variable in all AIMS small island nations except for Bahrain and Singapore. The availability of histological and cytopathological services is scarce, and none of these nations have PET scan capability. Chemotherapy is available in four countries, and Mauritius is the only AIMS small island nation (except for Bahrain and Singapore) with radiotherapy capabilities (both in terms of adequate facilities and the availability of radiotherapists). Like other small islands globally, some AIMS small island nations have established pathways for accessing diagnostic and treatment services off-island by sending selected specimens or patients to neighbouring countries or by receiving visiting specialist services.26 For instance, patients from Cape Verde might be transferred to Portugal for radiotherapy and other oncological treatment not available in-country, whilst patients from the Seychelles might seek comprehensive care in Sri Lanka, Reunion, or India, and Mauritius has an overseas treatment scheme for brain tumours.
Like the Pacific and Caribbean small island nations, innovations in cancer control and care are emerging in the AIMS small island nations. For example, the Comoros has partnered with the Felix Guyon University Hospital, Reunion, to provide a route for cancer diagnosis by sending tissue samples offshore, and has also partnered with Mauritius and Madagascar to improve chemotherapy delivery on Comoros. Oncologists from the Portuguese-speaking small island nations (ie, Cape Verde, Sao Tome and Principe, and Guinea-Bissau) are collaborating to advance cancer control efforts through various strategies, such as improving access to cancer care, increasing cervical cancer screening and HPV vaccination, and developing educational, training, and research pathways through their connection as PALOP (países Africanos de língua oficial Portuguesa) designated countries.26
Common themes leading to recommendations
Many reports have summarised evidence on cancer control requirements for low-income countries (LICs) and middle-income countries (MICs) and developed recommendations for strengthening existing systems.27–35 These recommendations have relevance for small island nations, although the unique circumstances of remote island states create distinctive challenges for cancer control. Acknowledging the diversity of this heterogeneous group, we discuss the common themes in small island nations’ experience of addressing the burden of cancer in their populations and implications for policy.
Monetary and fiscal policy
The economic case for investing in cancer control (from specific modalities, such as radiotherapy and surgery, through to population-based measures, such as women’s health initiatives, HPV vaccination and bowel cancer screening) is equally appable to small island nations.27,29,31,32,36 Good outcomes in cancer control are also highly sensitive to equity-centred fiscal policy, requiring substantial public health expenditure (about 5–6% of gross domestic product and at least US$100 per capita) and effective governance.37 Where private investment and provision for cancer is present, it should be a minority partner that is well integrated into public care. This idea is counter to the World Bank’s historic approach to small island nations, which focuses on private sector-led growth in health and cancer care, which is predicated on stable, progressive economies. Yet, small island nations have some of the most vulnerable economies in the world, facing serious constraints due to demographic and geographic characteristics. For small island nations with smaller populations, even those that have substantial per capita investment, the absolute amount of money available is still extremely limited. Regardless, investment in public health care is crucial to maintaining economic growth even if this comes with larger budget deficits.38 Cancer is a major cause of lost productivity due to premature morbidity and mortality, and effective public investment in cancer prevention and early diagnosis (including tobacco control, vaccination, and screening) will reduce the economic burden of cancer in transitioning economies.39 Unfortunately, some small island nations are pursuing unaffordable programmes focused on costly treatment of conditions that affect only a small proportion of the population (eg, renal dialysis in many Pacific countries).40 The failure to invest and tackle the causes of cancer (eg, tobacco consumption) seriously undermines the ability of small island developing states to progress towards achieving the sustainable development goals (panel 3).
Panel 3: Small island nations, the sustainable development goals, and universal health coverage.
The Sustainable Development Goals include target 3·4; to reduce premature mortality from non-communicable diseases (NCDs) by a third through prevention and treatment by 2030. However, the potential role of non-communicable disease control in achieving the sustainable development goals extends well beyond this specific target.41 The special case of small island nations achieving and prioritising sustainable development was detailed in the small island nations accelerated modalities of action pathway, which was developed at the third International Conference of small island nations in 2013, and resulted in a resolution adopted by the general assembly of the UN in 2014.42 This pathway acknowledges the significance of health as being foundational across sustainable development goals, identifies the importance of international cooperation and partnerships in achieving them, and the central role of multisectoral strategies for both preventing and managing NCDs. This pathway also includes the strengthening of health systems and acceleration of universal health coverage implementation. Small island nations vary substantially in terms of the extent that they need to address the three interrelated elements of coverage, as defined by WHO;43 ensuring financial protection by reducing reliance on personally financed payments for patients, expanding the services covered to ensure that those selected are high priority, cost-effective, and high-quality services, and increasing the population covered. For example, in several Caribbean countries, personally financed payments of cancer care remain high, whereas a key issue in most Pacific small island nations is the relatively narrow scope of cancer treatment services available. Responding to these challenges, and the burden of cancer generally, requires integrated and coordinated policies and strategies within small island nations, with international partnerships and support to prevent and treat patients with cancer. Progress in cancer control is absolutely integral to accelerating progress towards achieving the sustainable development goals within the challenging context that is facing small island nations.
Growth in population-level drivers of cancer (eg, tobacco and obesity) are expanding the burden of cancer in small island nations beyond what can be addressed by fiscal policy. Given infection-related cancers are still high, the emergence of a so-called double disease burden creates substantial economic challenges in supplying even a basic package of cancer care, which might be beyond what individual small island nations can achieve. Joint country models need to be examined where geographically co-located small island nations create a single system. It could be feasible and cost-effective to provide only basic community services in those small island nations with good access to specialist facilities in neighbouring HICs.44 More empirical evidence is needed for the cost-effectiveness of such models and pathways. Ad-hoc support through official development assistance funding is not a long-term solution;45 rather, major official development assistance programmes need to be created that specifically address cancer control in small island nations via public health and prevention initiatives. More widely, new tariffs and excise duties on unhealthy commodities need to be built into bilateral trade agreements to reduce the drivers of cancer and generate revenue for prevention and control activities, while still retaining small island nations’ access to global markets, which are crucial to sustainable economic growth.46
Policy that supports non-communicable disease control
Small island nations face particularly difficult challenges in developing coherent and effective approaches for cancer prevention. Key drivers of the growing cancer burden in these states include their dependence on, and vulnerability to, imported goods; some of which are health-promoting, but many of which are damaging to health.47,48 In line with a broader development agenda, many small island nations have been encouraged to follow a programme of trade liberalisation to attract foreign investment and to reduce the cost of imported goods.47 The removal of trade barriers has been associated with increased consumption of tobacco, alcohol, and highly processed food and drinks, which collectively account for around 30% all cancers.49,50
Cancer prevention thus requires measures to reduce population consumption of unhealthy commodities, with the most effective strategies involving taxation, tariffs, and restrictions on marketing.28 Although small island nations have particular challenges in balancing health and trade goals, some promising examples show how efforts to protect island populations from unhealthy commodities can be successful.51 The Cook Islands, Palau, and Tonga have all introduced tobacco taxes close to the target set by WHO (70% of the sale price);52 whilst several Pacific and Caribbean countries have imposed high taxes on alcohol and sweetened beverages;53–55 and some Pacific countries have banned importation of specific unhealthy items (eg, Tokelau’s ban on the importation of sweetened fizzy drinks).47 Although work is ongoing across the Caribbean to address these issues, there is scope to do more, particularly in the case of tobacco control in the Caribbean,56 where several small island nations do not have effective advertising bans on tobacco-related products and have tax levels below 25%.52,57 Raising taxes on tobacco, alcohol, and sugar-sweetened beverages has the potential to increase government revenue whilst also reducing the burden of NCDs.28
Regionalisation of cancer planning and services
A common practice among island nations is regional collaboration with external partners to facilitate the management of health programmes, including cancer control programmes. Such programmes typically involve a combination of regionalisation (in which an external agency works in collaboration with a particular geographical region) and regionalism (in which individual countries within a geographical region come together for a common specific purpose, supported by bodies that express their collective identity and shape collective action).
WHO often works in collaboration with a geographical region in the management of specific health-care needs. In the Pacific, for example, regionalisation has allowed prompt and affordable access to technical expertise for programme development for smaller nations. The Cancer Council of the Pacific Islands, which operates in US-affiliated Pacific Islands, provides a well-established example of how locally controlled regionalism can be initiated, with the council using the University of Hawaii as a gateway to funding and support, leading to a cancer control plan and registry that are regionally recognised.58,59 A further example of regionalisation is provided by the Pacific Regional Cancer Control Partnership, which includes international partner agencies.59 Managing cancer control in small island nations at a regional level means that collaborating small island nations can share resources and gain greater leverage for funding requests and global advocacy.
A regionalisation strategy for cancer prevention and control could be an effective way forward for small island nations in other regions. Regional efforts are most likely to be effective in instances in which they link countries that share a common language, historical or political affiliations in addressing a common need or goal (eg, national comprehensive cancer planning), or the development or regulation of medicines and health technologies.60,61 Opportunities for such linkages could be found in existing government-led initiatives (eg, the Caribbean Cooperation in Health and the Ministers of Health of both the Pacific and Caribbean regions caucuses), in national and international cancer societies, in regional and local networks of NGOs (eg, the Caribbean Cooperation in Health), in academia, or via international organisations, such as the International Agency for Research on Cancer (IARC), which has established cancer registry hubs in many regions.
The motivation for specific small island nations to be involved in efforts to achieve regionalisation or regionalism will vary and depends on individual country resources, needs, and geopolitical support. High-level regionalism requires support from health leaders in relevant countries to identify the preferences, scope, and nature of the collaborations needed. For such approaches to be effective, enough political will is needed both across and within partner countries to sustain collective action and outcome, mutually agreed institutional housing, governance structures, and ongoing review processes. Equally important is that leadership and decision making occur collaboratively and reflect the needs and priorities of the constituent countries. The actions of regional agencies, academic organisations, and NGOs are crucial for providing resource planning and working to deliver key actions according to agreed regional approaches for effective cancer care and control.
Developing cancer treatment services
Workforce
Efforts to strengthen health workforces will be key to enhancing cancer control within small island nations. As with many LICs and MICs, these nations struggle with insufficient workforce training, retention, professional support, and development opportunities, which is exacerbated by a shortage of infractructure and equipment, movement of resources from public to private settings, and migration of specialised health-care workers to HICs. In addition, small population sizes limit the feasibility of specialised services, including cancer treatment centres, with models from HICs (or even larger LICs and MICs) becoming inapplicable in these settings.62 For example, one analysis63 noted that oncology stafffing is insufficient to meet the demands of the popluation. This survey, done between 2016–17 of 14 countries in the Caribbean community, showed that oncology staffing was found to be inadequate based on recommendations for specialist numbers per capita from international organisations for medical oncologists (assessed by the American Society of Clinical Oncology) and radiation oncologists (assessed by the International Atomic Energy Agency). Although the need for workforce development is recognised within the sustainable development goals (target 3c),64 small island nations are competing with other countries in a context of marked scarcity, with the global shortage of health workers estimated to reach 15 million by 2030.65
The challenges facing small island nations in developing a cancer workforce are daunting. Given their small and dispersed populations, highly specialised services are neither feasible nor affordable. For many of these nations, treating patients offshore is the only option availble to them. However, health-related travel is expensive and complex and results in poor continuity of care, high costs incurredy by patients and their families, and reduced incentive to improve local services.66
Despite these challenges, opportunities for strengthening the workforce needed for cancer control for within small island nations are plentiful. Health workforce development is a priority in both the Pacific and Caribbean regions, with efforts underway to improve workforce planning, education and training, as well as its regulation and monitoring.67,68 Regional, or subregional, approaches can enhance the efficiency and the effectiveness of health workforce planning and offer opportunities to share successful approaches. In the Pacific, for example, health workforce development has been a major agenda item in meetings of the Pacific Health Ministers,69 and several collaborative groups and programmes that work to enhance training and continuing professional development have now been established, including the Pacific Regional Clinical Services and Workforce Improvement programme.69 Large challenges persist, however, including a need for specific attention to cancer prevention and treatment in workforce development.69 Similarly, in the Caribbean, several ad hoc efforts for training and building cancer workforce capacity have taken place. However, a systematic process for cancer control workforce planning, development, and continuing education is still needed in the region.
Ensuring a reliable and affordable supply chain
A robust supply chain of essential medicines and supplies is essential for delivering effective and timely cancer diagnoses and treatment. Individually, small island nations have little purchasing power over the medicine and healthcare equipment needed and little prospect of obtaining economically sensible deals because of poor economies of scale. Centralised approaches to procurement and supply generally reduce costs and improve supply even across countries.61,70 One of the most successful examples of a cross-country supply collaboration is the organisation of the Eastern Caribbean States Pharmaceutical Procurement Scheme, which was established in 1986.71 The Organisation of Eastern Caribbean States Pharmaceutical Procurement Scheme operates as a monopsony purchaser of pharmaceuticals and medical supplies to its small island countries. This approach has resulted in increased bargaining power and improved economies of scale, resulting in substantial reductions in drug prices, as well as improved supply chain and quality assurance processes, reductions in operational costs, and better informed selection and standardisation of pharmaceuticals.72 Key success factors have previously been described in detail.71 The PAHO Strategic Fund for Essential Medicines also offers a pooled procurement mechanism for medication for participating countries in the Americas, including the Caribbean, resulting in improved pricing and purchasing of medicines, although it remains underutilised for cancer treatments.73
Innovative approaches to delivering cancer care
Innovative approaches to delivering cancer care are necessary in the context of many small island nations, where the transference of highly specialised models of cancer care from HICs are unlikely to be useful. The important role of primary care in cancer prevention, diagnosis, treatment, survivorship, and end-of-life care is increasingly being recognised.34 Arguably, this role is particularly important in the context of small island nations, where secondary care services might be insufficient, or even absent. Where available, specialised cancer care is typically restricted to regional centres and, in many cases, patients will have to leave the region to access such care. This problem highlights the importance of enhancing what type of cancer care that can be provided within specific islands. Nurses and allied health professionals are a valuable resource, potentially providing a range of cancer-related care, including prevention activites (eg, smoking cessation advice), screening, treatment, palliative, and survivorship care.74,75 Supportive and palliative oncological care is provided by generalist medical practitioners in some small island nations, care that could potentially be extended with input from colleagues in HICs. Such partnership arrangements exist for paediatric cancer in both the Pacific and Caribbean regions, and have resulted in substantially improved outcomes for affected children.5,7 These collaborations typically involve country-specific policies and procedures for communication and referral, as well as regular virtual and face-to-face meetings between clinicians based in small island nations with those based in HICs. Several factors must be in place for such models to be effective and sustainable, including a commitment from governments and relevant health-care workers who provide basic oncological services, training and professional support opportunities, and access to relevant infrastructure, policies and procedures, and equipment.
Online professional development, consultation, and mentoring programmes offer particularly useful potential for small island nations, and are already supporting care in some contexts. For example, the Pacific Open Learning Health Net was established by WHO and the Pacific Ministers of Health in 2003, and provides accredited, freely accessible learning opportunities for health workers in the region on a broad range of topics. Most of these programmes are not cancer-related, but such a platform would be ideally placed to increase training opportunities for workers in cancer care.
Other technological solutions to support local healthcare workers include the use of telemedicine and point-of-care technologies. These solutions collectively have potential for improving cancer detection, diagnosis, and treatment, particularly in settings with a shortage of infrastructure, as is the case in many small island nations.76 Telemedicine, in particular, can support local clinicians with pathological and radiological diagnoses.35 Point-of-care technologies have a range of uses, including HPV screening and treatment programmes that have been positively evaluated in small island nation settings.76–78 Telementoring programmes, such as the Extension for Community Healthcare Outcomes programme, support local clinicians to provide care for complex diseases with support and mentoring from specialists.79 The Extension for Community Healthcare Outcomes programme runs regular virtual clinics, which are held using commonly available videoconferencing technology, in which local clinicians can present and discuss cases, and specialists, based in central hubs, can provide expert knowledge and experience. This programme is increasingly being used across the cancer control continuum in low-income and middle-income country settings, including in the Caribbean, to support comprehensive cancer plan development.80 This approach could be expanded to improve access to specialist cancer care services in other small island nations.
Both telemedicine and telementoring approaches require consistent, reliable, and affordable internet access, which might be problematic in some small island nations. Other potential barriers to supporting local health-care workers include high set-up costs, particularly for telepathology (which requires high-quality imaging), regulatory and legal requirements, and quality assurance processes for experts (such as pathologists) who are based in other countries.35 However, telemedicine has a clear advantage in that small island nation health services might be able to access expertise in countries where it would not otherwise be feasible for them to maintain highly specialised services.
International referrals
For many small island nations, the delivery of comprehensive cancer treatment in-country is not feasible, which means that patients must sometimes travel internationally for treatment. Travelling to receive treatment from outside of the country can be complex and expensive, particularly in the context of time-sensitive care. Even in instances where treatment costs are covered by the government, costs to patients for travel and accommodation can be incredibly expensive, or entirely out of reach for many patients. In addition, to ensure timely treatment, processes to facilitate treatment offshore must be efficient and streamlined. Because of scarce resources and high demand, it is not always possible to ensure these criteria are fulfilled. Very little empirical research exists on the effect and costs of international referrals, nor on optimal models of such referrals. Important questions are unanswered on nearly every aspect of these referrals, including the psychosocial, economic, and health effects of international referrals on patients and their families, the effect of costs of these referrals on the referring country (including their effect on the development of local services), identification of factors that make such referrals more or less successful, and the potential role of the international community in assisting with funding or coordinating such referrals. Research in this area is urgently required.
Role of traditional healers
In most small island nations, traditional healers play an important role in health care, although almost no research has been done on either the influence of traditional healers on health or their potential to provide links between traditional and conventional medicine. Many people in small island nations will visit their traditional healer before seeking conventional medical care and will continue to do so during treatments and at the end of life. Traditional healers work with patients and families within their own communities. They use concepts and language that are familiar and congruent with the understandings of health and disease within those communities. Engaging with these healers and encouraging a complementary approach with conventional medicine is likely to lead to positive outcomes. For example, more timely diagnoses and access to treatment could be made possible by training healers to recognise common cancer symptoms and refer patients to conventional services. Furthermore, the involvement of traditional healers in conventional cancer care could improve accessibility and provide patients with ongoing spiritual and mental support. Such innovative approaches would require identifying traditional healers who are prepared to work in partnership with conventional medicine, ongoing relationship building, consideration of the need for structural changes in the clinical setting to provide space for traditional healers, consideration of training needs of those healers, and attitudinal shifts for clinicians in recognising the role that traditional healers can play in improving health care.81
Building surveillance and research infrastructure
Underpinning all the work required to strengthen cancer care within small island nations is the necessity for data systems to support cancer surveillance and inform locally relevant priorities and policies. Evidently, effective surveillance programmes, including risk factor surveys, vital registration systems, population-based cancer registries, and clinical information systems, are all esential to plan and evaluate interventions tailored to the local scale and profile of cancer. Cancer registration has a long history in small island nations, but has been historically challenged by inefficiencies in health-care infrastructure, including pathologist services. As a means to improve data quality and population-based cancer registry coverage in the Caribbean and Pacific Island regions, the I ARC, with several partner organisations, have developed specific regional hubs as part of the Global Initiative for Cancer Registry Development (GICRD). The regional hubs provide the necessary technical guidance, training, advocacy, and research capacity building to ensure sustainable development of high-quality population-based cancer registries in these regions. A sustainable expansion of high-quality registries in small island nations is thus feasible and underway, but due to small population sizes in many states, regional approaches equally apply to surveillance, including population-based cancer registries. As with other programmes of local data collection, funding is problematic for this initiative, despite the small financial costs required.
Local evidence to inform policy design and programme delivery in cancer control and prevention is badly needed in small island nations. Even though many examples of productive partnerships between HICs and small island nations exist, research systems are often underdeveloped (or non-existent) in many small island nations.82–84 The ongoing building of research capacity and infrastructure is essential for progressing small island nations’ cancer control efforts as health and cost burdens grow. These necessary requirements will be facilitated by continuing development of genuine collaborations between small island nations and HICs that address local research priorities, strengthen research infrastructure, and create a beneficial impact by interpreting and implementing research findings in a way that is appropriate to local contexts.85
Developing high-impact strategies
In seeking to manage cancer, small island nations face difficulties common to many LICs and MICs while also experiencing some unique challenges.27,36 Cancer control in these settings is often seen as prohibitively expensive, and an absence of strategic prioritisation leads to missed opportunities for its inclusion in broader health systems strengthening agendas.86 Yet, much can be done to reduce suffering and premature death from cancer, even in resource-constrained settings.27,36
WHO recommends a stepwise approach to building a national cancer programme.87 Alongside this approach, it encourages the prioritisation of effective tobacco control policies in order to reduce the largest risk factor for cancer. As noted above, taxes on tobacco can also provide much-needed revenue to support the development of health systems.
Interventions in primary and community settings offer particularly promising strategies in resource-poor settings. Such programmes can be effective even in the absence of specialist services or infrastructure and offer alignment with broader development and universal health-care goals.
Cervical cancer is a leading cause of cancer death in many small island nations and is highly preventable, even in resource-constrained settings.31 HPV vaccination and cervical screening are cost-effective interventions highlighted as priorities by the director general of WHO.88 The international community can help small island nations to strengthen their cervical cancer prevention efforts by supporting regional purchases of HPV vaccines and assisting countries in designing and implementing screening programmes tailored to their local context. For example, Papua New Guinea has introduced point-of-care screening using HPV DNA testing. This offers a promising approach for cervical cancer screening programmes for small island nations where cytological tests are not available and approaches based on visualisation of the cervix with acetic acid have had poor results.78,89
Palliative care is explicitly recognised under the human right to health.33 In low-income and middle-income countries, and even in small island nations classified as high-income countries, palliative care is an often neglected aspect of cancer care. This neglect is particularly important considering that these countries are dealing with a high proportion of patients with advanced cancer for whom palliative care and pain relief is often the only option. Palliative care can be substantially enhanced via existing primary and community-based services. Although many aspects of cancer care require costly or sophisticated treatment modalities, palliative care can be strengthened at relatively low cost by improving access, understanding, and coordination of care within existing systems.33 Key priorities include efforts to increase the accessibility of essential medicines including immediate release and injectable morphine, simple equipment, and competency-based human resources.33 The essential package of palliative care and pain relief health services has been shown to be inexpensive and is applicable in countries at all stages of palliative care development.33 Regional organisations, such as the Caribbean Palliative Care Association, play an important role in raising awareness and coordinating provision of palliative care, which is often misunderstood or neglected in existing health systems.89
Global cancer control community
Global efforts in cancer control have tended to focus on issues facing LICs and MICs, but not the particular vulnerabilities of small island nations. Smaller populations with inherent capacity issues, geographic isolation, and environments increasingly affected by the consequences of global warning result in unique challenges. Although the sovereignty of states is paramount in the development of health policy, the global community has an important role in facilitating small island nations’ own efforts to strengthen their cancer prevention and control systems. Key members of the global community include international organisations (eg, WHO and its regional offices in the Americas and the western Pacific), global alliances and networks (eg, the Commonwealth, the IARC, the EU African Caribbean Pacific Partnership,90 and the Union for International Cancer Control), and, importantly, HICs within these regions, many of which have close relationships with neighbouring small island nations. We have developed priority recommendations targeted at these groups (panel 4). These recommendations can, and should, be operationalised at both regional and global levels and developed in partnerships between organisations within the global community and small island nations themselves (either as individual countries or as collaborative groups or regions).
Panel 4: What can the global community do to help?
International agencies or neighbouring high-income countries should assist small island nations in making the economic case for investing in cancer prevention and care, both for a domestic policy audience and when applying for funding support from external sources
This first recommendation might include mapping of needs and services, evaluation of the economic costs of cancer, costs of cancer care resourcing, or cost-effectiveness evaluations of specific interventions (eg, cervical cancer prevention)
Overseas development aid should include cancer control
Too often, complex, non-communicable diseases are excluded from directly allocated expenditures for health. Official development assistance support for cancer control should be included in health system strengthening loans and grants, and should be linked to the phased development of national cancer control planning and operational plans for multicountry referrals
If possible, take steps to facilitate small island nations’ procurement of high-quality vaccines, cancer technologies for surgery, pathological tests, imaging, radiotherapy (in appropriate cases), and systemic therapies (ie, cancer medicines)
For example, the international vaccine alliance (GAVI) has been instrumental in helping resource-poor countries gain access to affordable vaccines (including human papillomavirus vaccines), but could do more to focus on the specific needs of small island nations
Support workforce development and capacity by co-developing education and training programmes, partnership arrangements, telementoring, and virtual clinics
Several effective examples of these kinds of interventions exist; for example, the Pacific island project of the Royal Australasian College of Surgeons with local Pacific universities and the Pacific Island Surgeons Association have collaborated to increase the number of locally trained surgeons5
Provide technical assistance and research support to programmes led by small island nations
Research is needed into health systems, economic evaluations, pathways and models of care to inform policy, enhance quality of care, and to improve outcomes for patients with cancer. These needs also require capacity building in local data collection, investment in the International Agency for Research on Cancer, and Caribbean and Pacific cancer registry hubs through the Global Initiative for Cancer Registry Development, will substantially improve cancer surveillance and monitoring systems in small island nations
Support the efforts of small island nations to reduce importation and consumption of commodities that increase population cancer risk (eg, tobacco, alcohol, unhealthy food products)
In particular, high-income countries that trade with small island nations should respect these countries’ efforts to protect their populations from unhealthy imported products, rather than challenging such measures under trade agreements to protect their export markets, similarly to how the USA, Australia, and New Zealand have all done in the past91,92
Provide technical and legal support for effective health governance and cancer prevention
This final recommendation includes how ministries of health and civil society organisations can strengthen public policies to reduce consumption and manage terms of engagement with commercial industries that produce unhealthy commodities (eg, tobacco, alcohol, and processed foods and beverages)
Conclusion
More than 50 heterogeneous small island nations globally are facing major challenges in cancer control. Although many of the issues facing these countries are common to other countries, the distinct features of small island nations mean that addressing these challenges requires solutions that account for the unique circumstances of small island nations. Small island nation-specific circumstances include small populations, geographic isolation, capacity constraints, environments disproportionately affected by global warming, and often fragile economies. This Series paper cannot possibly capture all the complexity and nuance of those many nations. However, we have highlighted some of the common themes that must be considered in strengthening cancer control in small island nations, particularly, ongoing fiscal constraints, considerations relating to regionalisation, the development of innovative cancer treatment services that are effective and viable in the context of small populations, and the need for specific research that is relevant to a small island nation context. The particular difficulties facing small island nations have tended not to be a focus of the international cancer control community. We have identified some key recommendations to international agents to guide them in supporting and assisting small island nations in their efforts to address the burden of cancer. These recommendations focus on reinforcing the economic case for investing in cancer control and health systems strengthening, supporting small island nations in their efforts to protect their populations from the effects of unhealthy imports (eg, tobacco and alcohol), assisting these nations in the procurement of key resources, health workforce development, and providing technical assistance across the cancer control continuum. We hope that the work presented in this paper and in all four other Series papers has highlighted the key gaps and the many opportunities needed to improve cancer outcomes in small island nations around the world.
Supplementary Material
Search strategy and selection criteria.
We identified references through searches of PubMed and grey literature with no earliest date specified and up until Dec 19th, 2018, with the search terms “Caribbean”, “Pacific”, “Small Island Developing States”, “Cancer”, “SIDS”, “regionalisation or regionalism”, “workforce”, “tobacco control”, “NCD control”, “surveillance”, “research”, and “International referrals”. Grey literature from key international agencies was searched including those from WHO, the World Bank, and the UN, as well as individual country reports (for AIMS small island nations). Additional information was obtained from agendas and reports from key regional health leaders’ meetings (such as meetings of the Heads of Health, and Ministers of Health of the Pacific and Caribbean), and government and nongovernmental websites. We systematically collected specific information on cancer control activities from Ministry of Health officials and on-the-ground experts from the countries included in this Series (see appendix for a list of key informants). Only papers and reports published in English were reviewed. References were included based on originality and relevance to the broad scope of this report.
Acknowledgments
Declaration of interests
NP was supported by the Centers for Disease Control and Prevention Cooperative Agreement, Pacific Regional Central Cancer Registry 2017–2022, American Samoa CCC 2017–2022, CNMI CCC 2017–2022, Guam CCC 2017–2022, FSM CCC 2017–2022, RMI CCC 2017–2022), Palau CCC 2017–2022, REACH 2014–2018, along with the National Cancer Institute. NP’s contribution to the contents are solely the responsibility of the author and do not necessarily represent the official views of the Centers for Disease Control and Prevention, the National Cancer Institute, or the Department of Health and Human Services. All other authors declare no competing interests. No specific funding was received for this work.
Footnotes
See Online for a French translation of the abstract of this paper
This is the fifth in a Series of five papers about cancer control in small island nations
For more on the Caribbean community (CARICOM) see http://www.caricom.org
For more on the Pacific community see http://www.spc.int
For more on the Indian Ocean Commission see http://www.commissionoceanindien.org/accueil/
For more on the alliance of small island nations see http://www.aosis.org/
For more on the Pan American Health Organization see http://www.paho.org/hq
For more on the Commonwealth Innovation Hub see http://cominnowealth.org/
For more on the Pacific Ministries of Health see https://polhn.org
For the Global Initiative for Cancer Registry Development see http://gicr.iarc.fr
See Online for appendix
For more on the Union for International Cancer Control see https://www.uicc.org
Contributor Information
Diana Sarfati, Department of Public Health, University of Otago, Wellington, Wellington, New Zealand.
Rachel Dyer, Department of Public Health, University of Otago, Wellington, Wellington, New Zealand.
Paula Vivili, Public Health Division, Pacific Community, Noumea, New Caledonia.
Josephine Herman, Ministry of Health, Rarotonga, Cook Islands.
Dingle Spence, Hope Institute Hospital, Kingston, Jamaica.
Richard Sullivan, School of Cancer and Pharmaceutical Sciences, King’s College London, London, UK.
David Weller, James Mackenzie Professor of General Practice, Usher Institute of Population Health, Sciences and Informatics, College of Medicine and Veterinary Medicine, University of Edinburgh, Edinburgh, UK.
Freddie Bray, Cancer Surveillance Section, International Agency for Research on Cancer, Lyon, France.
Sarah Hill, Global Health Policy Unit, University of Edinburgh, Edinburgh, UK.
Christopher Bates, Nossal Institute for Global Health, Melbourne School of Population and Global Health, Melbourne, VIC, Australia.
Sunia Foliaki, Centre for Public Health Research, Massey University-Wellington Campus, Wellington, New Zealand.
Neal Palafox, Pacific Regional Cancer Programs, Department of Family Medicine and Community Health, John A Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA; Population Sciences in the Pacific Program, University of Hawaii Cancer Center, Honolulu, HI, USA.
Silvana Luciani, Department of Noncommunicable Diseases and Mental Health, Pan American Health Organization, Washington, DC, USA.
Alec Ekeroma, Department of Obstetrics and Gynaecology, University of Otago, Wellington, Wellington, New Zealand; National University of Samoa, Le Papaigalagala Campus, To’omatagi, Samoa.
James Hospedales, Caribbean Public Health Agency, Kingston, Jamaica.
References
- 1.Office of the high representative for the least developed countries, landlocked developing countries and small island developing states. Small island developing states: small Islands Big(ger) Stakes. New York: UN-OHRLLS, 2011. [Google Scholar]
- 2.WHO. Small island developing states health and WHO. Country Presence Profile. Geneva: World Health Organization, 2017 [Google Scholar]
- 3.Caribbean Public Health Agency. http://carpha.org/What-We-Do/Public-Health-Activities (accessed Oct 30, 2017).
- 4.Sarfati D, Dyer R, Amosa-Lei F, et al. Cancer control in the Pacific: big challenges facing small island states. Lancet Oncol 2019; published August 5 10.1016/S1470-2045(19)30400-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ekeroma A, Dyer R, Palafox N, et al. Cancer management in the Pacific region: a report on innovation and good practice. Lancet Oncol 2019; published August 5 10.1016/S1470-2045(19)30414-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spence D, Dyer R, Andall-Brereton G, et al. Cancer control in the Caribbean island countries and territories: some progress but the journey continues. Lancet Oncol 2019; published online Aug 5 10.1016/S1470-2045(19)30512-1. [DOI] [PubMed] [Google Scholar]
- 7.Spence D, Argentieri MA, Andall-Brereton G, et al. Advancing cancer care and prevention in the Caribbean: a survey of strategies for the region. Lancet Oncol 2019; published August 5 10.1016/S1470-2045(19)30516-9. [DOI] [PubMed] [Google Scholar]
- 8.Heintze H, Kirch L, Kuppers B, et al. The world risk report 2018. Berlin: Alliance Development Works, 2018. [Google Scholar]
- 9.Mercer J, Dominey-Howes D, Kelman I, Lloyd K. The potential for combining indigenous and western knowledge in reducing vulnerability to environmental hazards in small island developing states. Environ Hazards 2007; 7: 245–56. [Google Scholar]
- 10.Lee D, Smith NJ. Small state discourses in the international political economy. Third World Q 2010; 31: 1091–105. [Google Scholar]
- 11.Commonwealth Secretariat. Health ministers to tackle non-communicable diseases. 2011. http://thecommonwealth.org/media/press-release/health-ministers-tackle-non-communicable-diseases (accessed March 3, 2019).
- 12.UN. Sustainable development goals: 17 goals to transform our world. http://www.un.org/sustainabledevelopment/sustainable-development-goals (accessed Feb 24, 2018).
- 13.UN. Political declaration of the third high-level meeting of the general assembly on the prevention and control of non-communicable diseases. A/RES/73/2. Resolution adopted by the General Assembly on 10 October 2018. 2018. http://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/73/2 (accessed March 3, 2019).
- 14.Commonwealth Secretariat. Commonwealth health ministers meeting 2018. http://thecommonwealth.org/media/event/commonwealth-health-ministers-meeting-2018 (accessed March 3, 2019).
- 15.Zubizarreta E, Lodge M, Abdel-Wahab M, Polo A. Cervical cancer in the Commonwealth: collective action. J Glob Oncol 2018; 4 (suppl 2): 153. [Google Scholar]
- 16.Lodge M Cancer in the Commonwealth. Cancer Control 2017; 12: 62–64. [Google Scholar]
- 17.Weller D, Lodge M, Eden T, et al. Open letter to Lady Scotland. Lancet Oncol 2017; 18: e194. [DOI] [PubMed] [Google Scholar]
- 18.Morley SA. The income distribution problem in Latin America and the Caribbean. Santiago: United Nations and Economic Commission for Latin America and the Caribbean, 2001. [Google Scholar]
- 19.Economic Commission for Latin America and the Caribbean. The Caribbean outlook. 2018. https://repositorio.cepal.org/bitstream/handle/11362/43581/4/S1800607_en.pdf (accessed July 10, 2018).
- 20.World Bank. World Bank open data. https://data.worldbank.org/indicator/ (accessed Feb 15, 2019).
- 21.WHO. Global health observatory data repository. 2018. http://apps.who.int/gho/data/node.main.A1444 (accessed Sept 17, 2018).
- 22.WHO. Global atlas of medical devices. Geneva: World Health Organization, 2017. [Google Scholar]
- 23.International Cancer Control Partnership. National Plans. https://www.iccp-portal.org/map (accessed March 7, 2019).
- 24.International Agency for Research on Cancer. Global cancer observatory: cancer today population fact sheets. 2018. http://gco.iarc.fr/today/fact-sheets-populations (accessed Sept 17, 2018).
- 25.WHO. Immunisation country profile 2016. http://apps.who.int/immunization_monitoring/globalsummary (accessed May 28, 2018).
- 26.Santos LL, Spencer HB, Miguel F, Tulsidás S, Rodrigues B, Lopes LV. Fight against cancer in Portuguese-speaking African countries: echoes from the last cancer meetings. Infect Agents Cancer 2019; 14: 6. [Google Scholar]
- 27.Gelband H, Jha P, Sankaranarayanan R, Horton S. Cancer. Disease Control Priorities, 3rd edn. (DCP3). Washington: World Bank, 2015. [PubMed] [Google Scholar]
- 28.WHO. Tackling NCDs: ‘best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: World Health Organization, 2017. [Google Scholar]
- 29.Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy. Lancet Oncol 2015; 16: 1153–86. [DOI] [PubMed] [Google Scholar]
- 30.Gelband H, Sankaranarayanan R, Gauvreau CL, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from disease control priorities, 3rd edition. Lancet 2016; 387: 2133–4. [DOI] [PubMed] [Google Scholar]
- 31.Ginsburg O, Badwe R, Boyle P, et al. Changing global policy to deliver safe, equitable, and affordable care for women’s cancers. Lancet 2016; 389: 871–80. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol 2015; 16: 1193–224. [DOI] [PubMed] [Google Scholar]
- 33.Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. Lancet 2018; 391: 1391–454. [DOI] [PubMed] [Google Scholar]
- 34.Rubin G, Berendsen A, Crawford SM, et al. The expanding role of primary care in cancer control. Lancet Oncol 2015; 16: 1231–72. [DOI] [PubMed] [Google Scholar]
- 35.Wilson ML, Fleming KA, Kuti MA, Looi LM, Lago N, Ru K. Access to pathology and laboratory medicine services: a crucial gap. Lancet 2018; 391: 1927–38. [DOI] [PubMed] [Google Scholar]
- 36.Knaul F, Frank J, Shulman L, for the global task force on expanded access to cancer care and control in developing countries Closing the cancer divide: a blueprint to expand access in low and middle income countries. Boston: Harvard Global Equity Initiative, 2011. [Google Scholar]
- 37.Atun R, Silva S, Knaul FM. Innovative financing instruments for global health 2002–15: a systematic analysis. Lancet Glob Health 2017; 5: e720–26. [DOI] [PubMed] [Google Scholar]
- 38.Chowdhury A, Vidyattama Y. Macroeconomic policies for growth in small Pacific island econmies. Pac Econ Bull 2008; 23: 124–44. [Google Scholar]
- 39.Pearce A, Sharp L, Hanly P, et al. Productivity losses due to premature mortality from cancer in Brazil, Russia, India, China, and South Africa (BRICS): a population-based comparison. Cancer Epidemiol 2018; 53: 27–34. [DOI] [PubMed] [Google Scholar]
- 40.World Bank. Health challenges in the small island developing countries of the Pacific and the Caribbean. https://www.worldbank.org/content/dam/Worldbank/Health%20challenges%20in%20SIDS%20of%20pacific%20and%20caribbean.pdf (accessed Feb 2, 2019).
- 41.Nugent R, Bertram MY, Jan S, et al. Investing in non-communicable disease prevention and management to advance the sustainable development goals. Lancet 2018; 391: 2029–35. [DOI] [PubMed] [Google Scholar]
- 42.UN. Resolution adopted by the General Assembly on 14 November 2014. 9/15. SIDS Accelerated Modalities of Action (SAMOA) Pathway. 2014. https://www.un.org/ga/search/view_doc.asp?symbol=A/RES/69/15&Lang=E (accessed June 4, 2019).
- 43.WHO. World health report 2010. Health systems financing: the path to universal coverage. Geneva: World Health Organization, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chalkidou K, Glassman A, Marten R, et al. Priority-setting for achieving universal health coverage. Bull World Health Organ 2016; 94: 462–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fan VY, Savedoff WD. The health financing transition: a conceptual framework and empirical evidence. Soc Sci Med 2014; 105: 112–21. [DOI] [PubMed] [Google Scholar]
- 46.Tigerstrom Von B Small island developing states and international trade: special challenges in the global partnership for development. Mel J Int Law 2005; 6: 1–35. [Google Scholar]
- 47.Legge D, Gleeson D, Snowdon W, Thow A. Trade agreements and non-communicable diseases in the Pacific Islands. Samoa: World Health Organisation Pacific NCD Forum, 2013. [Google Scholar]
- 48.Ravuvu A, Friel S, Thow A, Snowdon W, Wate J. Monitoring the impact of trade agreements on national food environments: trade imports and population nutrition risks in Fiji. Glob Health 2017; 13: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beaglehole R, Bonita R, Magnusson R. Global cancer prevention: an important pathway to global health and development. Public Health 2011; 125: 821–31. [DOI] [PubMed] [Google Scholar]
- 50.Danaei G, Vander Hoorn S, Lopez AD, Murray CJL, Ezzati M. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet 2005; 366: 1784–93. [DOI] [PubMed] [Google Scholar]
- 51.Fa’alili-Fidow J, McCool J, Percival T. Trade and health in Samoa: views from the insiders. BMC Public Health 2014; 14: 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.WHO. WHO report on the global tobacco epidemic, 2017. Geneva: World Health Organization, 2017 [Google Scholar]
- 53.Healthy Caribbean Coalition. NCDs and trade policy in the Caribbean. Bridgetown: Healthy Caribbean Coalition, 2017 [Google Scholar]
- 54.Thow AM, Quested C, Juventin L, Kun R, Khan AN, Swinburn B. Taxing soft drinks in the Pacific: implementation lessons for improving health. Health Promot Int 2010; 26: 55–64. [DOI] [PubMed] [Google Scholar]
- 55.The Pacific Monitoring Alliance for NCD Action (MANA). Status of non-communicable diseases policy and legislation in Pacific Island countries and territories, 2018. Noumea: Pacific Community, 2019. [Google Scholar]
- 56.Samuels A, Unwin N. POS Declaration Evaluation Group. Accelerating action on NCDs. Evaluation of the 2007 CARICOM Heads of Government Port of Spain NCD Summit Declaration. 2016. http://onecaribbeanhealth.org/wp-content/uploads/2018/01/POSDEVAL_The-Investigators-report_FINAL.pdf (accessed June 4, 2019).
- 57.Kirton J, Knight W, Hospedales C, Hippolyte D, Kulik J. Regional and global impacts of the 2007 Port-of-Spain Declaration on noncommunicable diseases. Rev Panam Salud Publica 2018; 42: e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Foliaki S, Bates C, Tukana I, Palafox NA. Cancer control in the Pacific: a South Pacific collaborative approach. Cancer Epidemiol 2017; 50: 193–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Palafox NA, Given L, Hohman K, et al. Comprehensive cancer control planning in the Pacific: the Cancer Council of the Pacific Islands a multi-national regional coalition. Cancer Causes Control 2018; 29: 1287–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Romero Y, Trapani D, Johnson S, et al. National cancer control plans: a global analysis. Lancet Oncol 2018; 19: e546–55. [DOI] [PubMed] [Google Scholar]
- 61.Preston C, Chahal HS, Porrás A, et al. Regionalization as an approach to regulatory systems strengthening: a case study in CARICOM member states. Rev Panam Salud Publica 2016; 39: 262–68. [PubMed] [Google Scholar]
- 62.Sirohi B, Chalkidou K, Pramesh CS, et al. Developing institutions for cancer care in low-income and middle-income countries: from cancer units to comprehensive cancer centres. Lancet Oncol 2018; 19: e395–406. [DOI] [PubMed] [Google Scholar]
- 63.Alleyne-Mike K The Caribbean community clinical oncology workforce: analyzing where we are today and projecting for tomorrow. J Oncol 2018: 7286281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.WHO. SDG 3: Ensure healthy lives and promote wellbeing for all at all ages. https://www.who.int/sdg/targets/en (accessed Jan 9, 2019).
- 65.Liu JX, Goryakin Y, Maeda A, Bruckner T, Scheffler R. Global health workforce labor market projections for 2030. Hum Resour Health 2017; 15: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Suzana M, Walls H, Smith R, Hanefeld J. Achieving universal health coverage in small island states: could importing health services provide a solution? BMJ Glob Health 2018; 3: e000612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Anonymous. Health workforce development in the Pacific. Report for Twelfth Ministers of Health Meeting. 2017. http://www.wpro.who.int/southpacific/pic_meeting/2017/documents/12thphmm_session04_03_hwf_16aug.pdf (accessed Jan 14, 2019).
- 68.Pan American Health Organization. Caribbean roadmap on human resources for universal health. https://www.paho.org/ecc/index.php?option=com_content&view=article&id=618:caribbean-roadmap-on-human-resources-for-universal-health&Itemid=332 (accessed March 8, 2019).
- 69.WHO, SPC. Health Workforce Development in the Pacific. 2017. http://www.wpro.who.int/southpacific/pic_meeting/2017/documents/12thphmm_session04_03_hwf_16aug.pdf (accessed Jan 9, 2019).
- 70.Seidman G, Atun R. Do changes to supply chains and procurement processes yield cost savings and improve availability of pharmaceuticals, vaccines or health products? A systematic review of evidence from low-income and middle-income countries. BMJ Glob Health 2017; 2: e000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Huff-Rousselle M, Burnett F. Cost containment through pharmaceutical procurement: a Caribbean case study. Int J Health Plann Manage 1996; 11: 135–57. [DOI] [PubMed] [Google Scholar]
- 72.Huff-Rousselle M The logical underpinnings and benefits of pooled pharmaceutical procurement: a pragmatic role for our public institutions? Soc Sci Med 2012; 75: 1572–80. [DOI] [PubMed] [Google Scholar]
- 73.Pan American Health Organization, WHO. PAHO strategic fund. 2018. https://www.paho.org/hq/index.php?option=com_content&view=article&id=12163:paho-strategic-fund&Itemid=1694&lang=en (accessed March 2, 2018).
- 74.Challinor JM, Galassi AL, Al-Ruzzieh MA, et al. Nursing’s potential to address the growing cancer burden in low- and middle-income countries. J Global Oncol 2016; 2: 154–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Galassi A, Challinor J. Strengthening the oncology nurse workforce in low-income and middle-income countries. Lancet Oncol 2015; 16: 887–88. [DOI] [PubMed] [Google Scholar]
- 76.Haney K, Tandon P, Divi R, Ossandon MR, Baker H, Pearlman PC. The role of affordable, point-of-care technologies for cancer care in low- and middle-income countries: a review and commentary. IEEE J Transl Eng Health Med 2017; 5: 2800514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toliman P, Badman SG, Gabuzzi J, et al. Field evaluation of xpert HPV point-of-care test for detection of human papillomavirus infection by use of self-collected vaginal and clinician-collected cervical specimens. J Clin Microbiol 2016; 54: 1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toliman PJ, Kaldor JM, Badman SG, et al. Evaluation of self-collected vaginal specimens for the detection of high-risk human papillomavirus infection and the prediction of high-grade cervical intraepithelial lesions in a high-burden, low-resource setting. Clin Microbiol Infect 25; 496–503. [DOI] [PubMed] [Google Scholar]
- 79.University of New Mexico. About ECHO. 2019. https://echo.unm.edu/about-echo-2 (accessed March 2, 2019).
- 80.Lopez MS, Baker ES, Milbourne AM, et al. Project ECHO: a telementoring program for cervical cancer prevention and treatment in low-resource settings. J Global Oncol 2016; 3: 658–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Krah E, de Kruijf J, Ragno L. Integrating traditional healers into the health care system: challenges and opportunities in rural northern Ghana. J Community Health 2018; 43: 157–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brown University. Brown, Yale researchers launch unique lab in Samoa to study obesity epidemic. 2017. https://www.brown.edu/news/2017-11-10/samoa (accessed Nov 23, 2018).
- 83.Ekeroma AJ, Pollock T, Kenealy T, et al. Pacific Island publications in the reproductive health literature 2000–2011: with New Zealand as a reference. Aust NZ J Obstet Gynaecol 2013; 53: 197–202. [DOI] [PubMed] [Google Scholar]
- 84.Tulloch-Reid MK, Saravia NG, Dennis RJ, et al. Strengthening institutional capacity for equitable health research: lessons from Latin America and the Caribbean. BMJ 2018; 362: k2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ekeroma A Collaboration as a tool for building research capacity in the Pacific Islands. Ann Human Biol 2018; 45: 295–96. [DOI] [PubMed] [Google Scholar]
- 86.Atun R, Cavalli F. The global fight against cancer: challenges and opportunities. Lancet 2018; 391: 412–13. [DOI] [PubMed] [Google Scholar]
- 87.WHO. National cancer control programmes: policies and managerial guidelines. 2nd edn. Geneva: World Health Organization, 2002. [Google Scholar]
- 88.Ghebreyesus T Cervical cancer: an NCD we can overcome. 2018. https://www.who.int/reproductivehealth/DG_Call-to-Action.pdf (accessed Feb 15, 2019).
- 89.Maharaj S, Harding R. The needs, models of care, interventions and outcomes of palliative care in the Caribbean: a systematic review of the evidence. BMC Palliat Care 2016; 15: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.European Commission. Joint communiciation to the European Parliament and the council. https://ec.europa.eu/europeaid/sites/devco/files/joint-communication-renewed-partnership-acp-20161122_en.pdf (accessed March 23, 2019).
- 91.Friel S, Hattersley L, Townsend R. Trade policy and public health. Annu Rev Public Health 2015; 36: 325–44. [DOI] [PubMed] [Google Scholar]
- 92.Thow AM, Snowdon W, Schultz JT, Leeder S, Vivili P, Swinburn BA. The role of policy in improving diets: experiences from the Pacific Obesity Prevention in Communities food policy project. Obes Rev 2011; 12: 68–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


