Abstract
This Series paper describes the current state of cancer control in Pacific island countries and territories (PICTs). PICTs are diverse but face common challenges of having small, geographically dispersed, isolated populations, with restricted resources, fragile ecological and economic systems, and overburdened health services. PICTs face a triple burden of infection-related cancers, rapid transition to lifestyle-related diseases, and ageing populations; additionally, PICTs are increasingly having to respond to natural disasters associated with climate change. In the Pacific region, cancer surveillance systems are generally weaker than those in high-income countries, and patients often present at advanced cancer stage. Many PICTs are unable to provide comprehensive cancer services, with some patients receiving cancer care in other countries where resources allow. Many PICTs do not have, or have poorly developed, cancer screening, pathology, oncology, surgical, and palliative care services, although some examples of innovative cancer planning, prevention, and treatment approaches have been developed in the region. To improve cancer outcomes, we recommend prioritising regional collaborative approaches, enhancing cervical cancer prevention, improving cancer surveillance and palliative care services, and developing targeted treatment capacity in the region.
Introduction
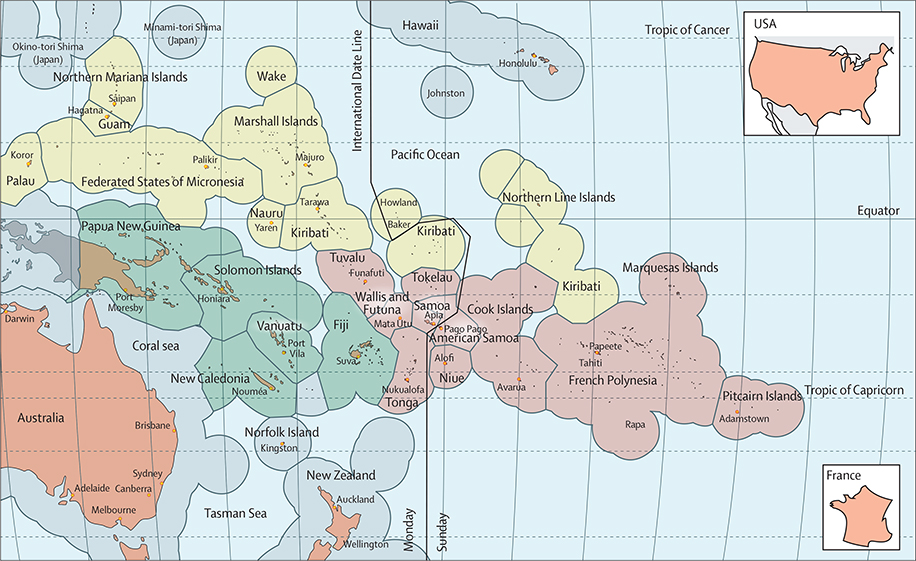
The region of the Pacific island countries and territories (PICTs) consists of 22 countries and territories surrounded by 165 million km2 of ocean (figure 1). PICTs are highly diverse in geography, social and economic development, population size, culture, language, and history (table 1).1–3 For example, Papua New Guinea has a larger population than Sweden, estimated to be more than 8 million people in 2012, but, at the other end of the spectrum, Niue has a resident population of around 1500 people.1 Despite these differences, PICTs share common features; these include, fragile economies, with a narrow export base; geographical isolation; and insufficiently resourced health systems, which remain vulnerable to the effects of climate change and extreme weather threats such as tropical cyclones and floods.4–6 In addition to frequent minor climatic events (such as local flooding and minor cyclones), natural disasters occur regularly in the region. For example, in 2014 there were flash floods in Honiara, Solomon Islands, which left tens of thousands of people homeless and 22 dead. Cyclones are also a regular occurrence in the region; in 2015, cyclone Pam hit the island of Vanuatu, which caused 15 deaths and massive damage to infrastructure in the region.7 The following year, cyclone Winston resulted in the deaths of 44 people and caused more than US$1.4 billon in damage, with Fiji primarily affected; and in 2018, cyclone Gita hit Tonga, which damaged more than a thousand homes and killed two people.7
Figure 1: Map of the Pacific region.
Green islands are part of Melanesia, red islands are part of Polynesia, and yellow islands are part of Micronesia.
Table 1:
Socioeconomic characteristics of 20 Pacific island countries and territories
| Estimated population (2018) | Income classification (according to World Bank classifications) | Year of independence or political affiliations | GDP per capita (current US$, 2017) | Current health expenditure as % GDP (2015) | Out-of-pocket expenditure (% of current health expenditure) | Life expectancy at birth (years), total | Mortality rate (crude, per 1000 population) | Number of physicians per 10 000 population | Number of nurses per 10 000 population | |
|---|---|---|---|---|---|---|---|---|---|---|
| Papua New Guinea | 8558800 | Lower middle | 1949 | 2555·90 | 3·8 | 5·8 | 54·2 | 7·1 | 0·5 | 5 |
| Fiji | 888400 | Upper middle | 1970 | 5589·40 | 3·6 | 21·4 | 67·5 | 7·1 | 8 | 29 |
| Solomon Islands | 682500 | Lower middle | 1978 | 2132·10 | 5·3 | 3·3 | 70·2 | 4·8 | 2 | 18 |
| Vanuatu | 304500 | Lower middle | 1980 | 3123·60 | 3·5 | 8·9 | 71·7 | 4·8 | 2 | 22 |
| NewCaledonia | 285500 | High | Overseas collectivity of France | NA | NA | NA | 77·1 | 5·7 | 25 | 60 |
| French Polynesia | 277100 | High | Overseas collectivity of France | NA | NA | NA | 75·8 | 5·4 | 19 | 47 |
| Samoa | 196700 | Upper middle | 1962 | 4360·80 | 5·6 | 11·5 | 74·2 | 5·0 | 5 | 15 |
| Guam | 172400 | High | Unincorporatedterritory of USA | 35562·60 | NA | NA | 78·7 | 5·1 | NA | NA |
| Kiribati | 120100 | Lower middle | 1979 | 1685·20 | 7·6 | 0·2 | 62·2 | 7·0 | 2 | 46 |
| Federated States of Micronesia | 105300 | Lower middle | 1986 (in compact of free association with USA) | 3187·60 | 13·1 | 2·5 | 70·0 | 6·2 | 2 | 36 |
| Tonga | 100300 | Upper middle | 1970 | 3944·20 | 5·9 | 10·2 | 70·6 | 6·0 | 5 | 30 |
| American Samoa | 56700 | Upper middle | Unincorporatedterritory of USA | 11834·70 | NA | NA | 74·0 | 4·2 | NA | NA |
| Northern Mariana Islands | 56200 | High | Self-governing Commonwealth of the USA | 22572·40 | NA | NA | 76·4 | NA | 4 | 19 |
| Marshall Islands | 55500 | Upper middle | 1986 (in compact of free association with USA) | 3753·30 | 22·1 | 9·7 | 71·8 | 3·7 | 5 | 36 |
| Palau | 17900 | High | 1994 (in compact of free association with USA) | 13417·30 | 10·6 | 21·8 | 73·0 | 10·0 | 12 | 53 |
| Cook Islands | 15200 | Not available | Self-governing state in free association with New Zealand | NA | 2·7 | 8·0 | 75·3 | NA | 12 | 65 |
| Nauru | 11000 | Upper middle | 1968 | 8343·80 | 4·8 | 1·3 | 61·2 | NA | 14 | 70 |
| Tuvalu | 10200 | Upper middle | 1979 | 3550·00 | 14·1 | 0·7 | 69·6 | NA | 9 | 38 |
| Niue | 1520 | Not available | Self-governing state in free association with New Zealand | NA | 6·3 | 1·9 | 73·2 | NA | 18 | 98 |
| Tokelau | 1400 | Not available | Territory of New Zealand | NA | NA | NA | 69·1 | NA | 27 | 82 |
Pitcairn Islands and Wallis and Futuna have been exduded from this analysis because no key informants were located to provide data. GDP=gross domestic product. NA=not applicable.
Migration (permanent and temporary) to high-income countries for education or increased earning opportunities is common among PICT populations.8 With an increasing cancer burden, PICTs are facing the triple burden of infection-related cancers, a rapid transition to cancers relating to reproductive, dietary, and hormonal factors, and growing ageing populations.9,10 In most PICTs, cancer surveillance systems are insufficient and patients tend to present late with advanced cancers. Many PICTs are unable to provide cancer care to those affected, with patients not receiving care at all, receiving restricted treatment only, or being treated abroad when health-care resources allow.10–12 Treatment abroad poses a substantial economic burden on the patient and their family, but many PICTs do not have any, or have restricted access to, cancer screening, pathology, oncology, surgical, and palliation services. In this Series paper, we describe these challenges in more detail. The second paper in the Series, by Ekeroma and colleagues,13 highlights examples of innovative practice that can begin to provide sustainable solutions to cancer control in the Pacific region.
Political and health system structures of the Pacific region
The Pacific region is divided along the old colonial boundaries (figure 1) according to the subregions of Melanesia (Fiji, Papua New Guinea, New Caledonia, Solomon Islands, and Vanuatu), Polynesia (American Samoa, Cook Islands, French Polynesia, Niue, Pitcairn Islands, Samoa, Tokelau, Tonga, Tuvalu, and Wallis and Futuna), and Micronesia (Federated States of Micronesia, Guam, Kiribati, Marshall Islands, Nauru, Northern Mariana Islands, and Palau).14,15 These 22 Pacific states are a combination of both independent nations and territories historically and politically affiliated with larger high-income countries (HICs; table 1). French Polynesia, New Caledonia, and Wallis and Futuna are self-governing overseas collectivities of France. The populations of Cook Islands, Niue, and Tokelau are New Zealand citizens with the right to access the publicly funded health services in New Zealand. The inhabitants of the US-affiliated Pacific islands (USAPIs) are naturalised US citizens (Guam and Northern Mariana Islands), US nationals (American Samoa), or freely associated sovereign states (Federated States of Micronesia, Marshall Islands, and Palau) all of which benefit from economic assistance from the USA.16 Furthermore, the political systems of PICTs vary, often reflecting HICs with which they have the closest ties.16 The varying political and economic ties with HICs have substantial implications for both the resourcing of health services and the local economy.
With some minor exceptions (such as private specialist clinics), health services are largely publicly funded and delivered free of charge or heavily subsidised by PICT governments, which has led to health-care financing becoming a major challenge for many PICT governments.6,17 The Pacific region receives external financial and technical support for health-care delivery, and various multilateral and bilateral partnerships assist public, private, and non-governmental organisations (NGOs) health-related entities in a bid to improve health outcomes.18 The World Bank estimates that, in 2016, 20·5% of current health expenditure for PICTs was funded from external sources (including the USA, France, and other neighbouring HICs; compared with 1·3% for low to middle income countries [LMICs] in general).1
All PICT health systems are organised around one or more central referral hospitals, and several lower level facilities of varying size and capacity.6 The structure and delivery of primary care services varies between and within the PICTs, but for most countries and territories the majority of primary care services are provided by the government, with a smaller number provided by NGOs, such as faith-based organisations, and private practices.19–23 In smaller PICTs, primary care might be the highest level of care available on the island or it might only be provided at the single hospital on the island alongside curative services.6 In some large towns and cities in Fiji, Papua New Guinea, New Caledonia, French Polynesia, and Guam, access to primary care includes private practices, with services similar to those seen in HICs. However, in the outer islands and rural areas of many PICTs the primary care services most readily accessible are nurse, nurse aid, or community health worker run clinics, with varying capacities to manage acute and chronic conditions. In many PICTs, doctors are only located at central hospitals, and some patients will bypass their local clinic to seek primary care at the hospital.19–23 Traditional healers are also an integral part of the health services in many PICTs.24
The Pacific Community (SPC) and WHO-Western Pacific Region (WHO-WPR) are the two major regional bodies providing strategic coordination and technical support for health-related activities.15,25 The Pacific island territories are predominantly funded by France, the USA, and New Zealand; the southern PICTs have longstanding relationships with Australia and New Zealand. Australia is the largest donor in the region to the southern PICTs and over half of New Zealand’s international development assistance budget is directed toward the Pacific region.26,27 Japan, Cuba, and, to some extent, South Korea and China are also actors in health services in many Pacific islands, as are development partners, such as the World Bank, Asian Development Bank, the European Union, and a number of UN agencies.27,28
Most PICT governments have difficulty maintaining an adequate health workforce, with shortages in the number of health-care professionals in several of the countries and territories.29,30 Nursing training, at varying levels, is provided in most PICTs, while medical training is available regionally at academic institutions located in Fiji, Papua New Guinea, and Samoa, and pharmacy and postgraduate training are available in Fiji and Papua New Guinea. To address workforce shortages, and lower medical training costs, at least six PICT governments have participated in Cuba’s bilateral health assistance programme since 2008, in which Cuban medical doctors are deployed in a country, and students from abroad receive medical scholarships to study in Cuba.31 PICTs that host visiting medical and surgical specialists from New Zealand, China, Taiwan, Australia, the USA, France, and other countries can deliver health-care services funded by donor countries and NGOs.32
Non-communicable disease (NCD) policy, globalisation, and risk factors
Increasing trade links and the effects of globalisation have contributed to a heavy dependence of PICTs on imported foods, which has been compounded by the effects of climate change and variable weather patterns.33–35 The widespread availability of heavily processed foods rich in carbohydrate, free sugars, trans fats, and salt at relatively low prices is a causative factor in the NCD epidemic,36,37 obesity,38,39 and the increasing number of obesity-related cancers in the Pacific region. In 2007, Samoa banned the importation of cheap high-fat turkey tails as part of its efforts to combat NCDs; however, in 2011, the ban was reversed to meet conditions of international trade agreements.40 Other low-quality foods continue to be imported into the Pacific region, such as mutton flaps, which are cheap, low-quality cuts of meat that are extremely high in saturated fat.35
Another potential driver of the NCD pandemic across the Pacific is climate change.4 Climate change, resulting in higher temperatures, altered rainfall, increasing storm frequency, and rising sea levels, threaten the production of locally grown foods and access to drinking water, increasing the dependence of the PICT populations on imported food, elevating the risk of obesity and decreasing the amount of physical activity done by the population.4 The effects of climate change in combination with disruptions to health-care services and environmental infrastructure and population displacement increase both the drivers for and effects of NCDs.4 Nuclear testing by the USA, in the Marshall Islands (1946–62), and France, in French Polynesia (1966–96), has contaminated food sources and exposed local population to ionising radiation.45,46 The testing by the USA in the Marshall Islands in 1954 was described as: “the most serious episode of radioactive contamination in the history of nuclear weapons testing”,46 resulting in an ongoing excess of thyroid cancer, a number of other cancers, and extensive pollution of the marine ecosystem.47
NCDs are a serious and growing problem in the Pacific. The Pacific region has some of the highest obesity prevalences in the world, with more than half of all adults in many PICTs categorised as obese (table 2). This prevalence is reflected in the high prevalence of diabetes and an increase in the number of complications associated with the disease, including chronic kidney disease. For example, nearly half of all adults aged 18–64 years in American Samoa have raised blood glucose concentrations,48 and, in neighbouring Samoa, 11·5% of the adult population is estimated to have chronic kidney disease.49 Smoking prevalence in the region is variable, but typically higher in men than in women, with over half of all men smoking in four of 20 PICTs (Wallis and Futuna, and Pitcairn Islands were excluded from this analysis because no key informants were located to provide data; table 2).48 Additionally, betel (or Areca) nut chewing, a common practice in some Melanesian and Micronesian PICTs, is associated with an increased risk of oral cancer.
Table 2:
Health characteristics in 20 Pacific island countries and territories and their cancer surveillance and prevention status41–44
| Cancer registration* | National cancer plan (year) | Current NCD plan | Prevalence of adult smokers by gender† (%) |
Number of tobacco control measures in place‡ | Prevalence of obese adults by gender† (%) |
Number of obesity prevention measures in place§ | HBV vaccination coverage |
HPV vaccination coverage |
Organised screening programmes |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Birth dose | B3 | HPV vaccination availability (year introduced) | HPV vaccination target age group (estimated coverage, %) | Cervical cancer | Breast cancer | Bowel cancer | ||||||
| Papua New Guinea | Registration activity | Yes (2015, 2017–21) | Yes | 60·3 | 27·0 | 5 | 5·1 | 8·7 | 1–2 | 31 | 50 | Pilot | 9-year-old girls | No | No | No |
| Fiji | PBCR | Draft (2016) | Yes | 47·0 | 14·3 | 5 | 22·4 | 42·0 | 5 | 93 | 93 | National (2013) | 12-year-old girls (>90%) | No | No | No |
| Solom on Islands | Registration activity | No¶ | Yes | 54·5 | 21·0 | 5 | 18·4 | 27·0 | 3–4 | 48 | 80 | Pilot | 9-year-old girls | No | No | No |
| Vanuatu | No data | No | Yes | 45·8 | 4·0 | 5 | 13·9 | 23·3 | 3–4 | 86 | 86 | National | 10-year-old girls | No | No | No |
| New Caledonia | High-quality national PBCR | No¶ | No | NA | NA | 5 | NA | NA | 3–4 | 99 | 98 | National (2011) | 11–12-year-old girls (42%) | Yes(Pap) | Yes (MMG) | Under consideration |
| French Polynesia | High-quality national PBCR | Yes (2018–22) | Yes | 38·5 | 43·6 | 3–4 | 38·9 | 41·9 | 5 | 98 | 98 | NA | NA | Partial (Pap) | Partial (MMG) | No |
| Samoa | Registration activity | No | No | 36·5 | 13·7 | 5 | 44·8 | 68·6 | 3–4 | 95 | 90 | NA | NA | No | No | No |
| Guam | High-quality regional PBCR | Yes (2018–22) | No | NA | NA | 5 | NA | NA | 3–4 | 83 | 83 | National | 11–13-year-old girls (75–95%) | Yes(Pap) | Yes (MMG) | Under consideration |
| Kiribati | No data | No | No | 64·7 | 33·4 | 5 | 32·4 | 55·6 | 1–2 | 79 | 81 | NA | NA | No | No | No |
| Federated States of Micronesia | High-quality regional PBCR | Yes (2019–24) | No | 42·0 | 21·0 | 1–2 | 30·0 | 55·8 | 3–4 | 75 | 80 | National | 11–13-year-old girls (75–95%) | Yes, variable in States (Pap and VIA) | Yes(CBE) | No |
| Tonga | Registration activity | No | Yes | 46·4 | 13·4 | 5 | 57·2 | 77·6 | 3–4 | 91 | 96 | NA | NA | No | No | No |
| American Samoa | High-quality regional PBCR | Yes (2012–17) | No | 49·0 | 29·7 | 3–4 | 69·3 | 80·4 | 1–2 | 100 | 78 | National | 11–13-year-old girls (75–95%) | Yes(Pap) | Yes (MMG) | No |
| Northern Mariana Islands | High-quality regional PBCR | Yes (2007–12) | No | 33·3 | 17·2 | 3–4 | 65·7 | 62·6 | 1–2 | 98 | 62 | National | 11–13-year-old girls (75–95%) | Yes(Pap) | Yes (MMG) | No |
| Marshall Islands | High-quality regional PBCR | Yes (2017–22) | Yes | 39·5 | 6·0 | 3–4 | 18·4 | 54·2 | 1–2 | 86 | 82 | National | 11–13-year-old girls (75–95%) | Yes, partial (Pap and VIA) | Yes, partial (MMG and CBE) | No |
| Palau | High-quality regional PBCR | Yes (2017–22) | Yes | 24·0 | 8·4 | 3–4 | 45·2 | 47·7 | 1–2 | 99 | 98 | National | 11–13-year-old girls (75–95%) | Yes(Pap) | Yes (MMG) | No |
| Cook Islands | Registration actlvlty | No¶ | Yes | 37·9 | 27·7 | 5 | 68·7 | 70·7 | 5 | 99 | 99 | National (2011) | 9-year-old girls | Yes(Pap) | Yes(MMG) | No |
| Nauru | No data | No | Yes | 47·4 | 45·3 | 5 | 71–0 | 69·4 | 3–4 | 99 | 97 | NA | NA | Yes(Pap) | No | No |
| Tuvalu | No data | No | Yes | 48·6 | 22·4 | 5 | 55·2 | 70·7 | 1–2 | 99 | 94 | NA | NA | No | No | No |
| Niue | No data | No | No | 22·6 | 13·0 | 1–2 | 59·2 | 62·7 | 5 | 84 | 99 | NA | NA | No | No | No |
| Tokelau | No data | No | No | 58·6 | ·· | 5 | 59·2 | 62·7 | 5 | 100 | 100 | NA | NA | No | No | No |
Pitcairn Islands and Wallis and Futuna have been excluded from the analysis because no key informants were located to provide data. NCD=non-communicable disease. HBV=hepatitis B virus. HPV=human papilloma virus. PBCR=population-based cancer registry. NA=not applicable. Pap=papanicolaou. MMG=mammography. VIA=visual inspection with acetic acid. CBE=clinical breast examination.
Status of cancer registration was high-quality national PBCR, regional high-quality PBCR, registration activity, or no data.
From STEPS Country Reports (year, age group): Papua New Guinea (2007–08, 15–64 years), Fiji (2011, 25–64 years), Solomon Islands (2015, 18–69 years), Vanuatu (2011, 25–64 years), French Polynesia (2010,18–64 years), Samoa (2013, 18–64 years), Kiribati (2015–16, 18–69 years), Federated States of Micronesia (2008, 25–64 years), Tonga (2012, 25–64 years), American Samoa (2006, 25–64 years), Northern Mariana Islands (2016, 18 years and older),Marshall Islands (2012, 15–64 years), Palau (2011–13, 25–64 years), Cook Islands (2013–15, 18–64 years), Nauru (2015–16, 18–69 years), Tuvalu (2015, 18–69 years), Niue (2011, 15 years and older), and Tokelau (2014, 18–69 years).
Tobacco control measures (indicators: excise tax, smoke-free environments, health warnings, and restriction of advertising, promotions, sponsorships, sales, and licensing).
Obesity prevention measures (five indicators: food fiscal policies, healthy food policies in schools, food-based dietary guidelines, salt consumption policies, and compulsory physical education in schools).
Includes anticancer plans in non-NCD policy documents (eg, sexual or reproductive health).
In 2010, the USAPI health leadership team developed an emergency regional NCD declaration, and, in 2014, PICT health and finance ministers declared an NCD crisis and endorsed the Roadmap Report,50 a promising regional strategy for implementing NCD prevention and control.51 Country-specific NCD roadmaps across the Pacific region were developed and included commitments to increase tobacco excise to at least 70% of the retail price, increase alcohol taxation, and to develop policies that reduce consumption of unhealthy food and beverages.52 The ministers of health of the Pacific committed to a goal of a tobacco-free Pacific (reducing the number of adults that smoke to <5%) by 2025.53 The Pacific Monitoring Alliance for NCD Action (MANA)—an alliance of PICTs and agencies interested and involved in NCD monitoring—was established in 2016. In 2018, the work of the Pacific MANA was assessed and its progress endorsed by 14 PICTs.54,55 With the support of a coordinating team (including the Pacific Research Center for the Prevention of Obesity and Non-Communicable Diseases, Pacific Island Health Officers’ Association, SPC, and WHO), a Pacific MANA dashboard has been agreed to monitor progress on NCD actions by all PICTs with annual reporting to Heads of Health. Evidence of improvements emerging from some PICTs is beginning to be reported. One example is the percentage of the population that smokes has decreased among those aged 13–15 years in Guam in 2001–13 from 39% to 24% in men and 35% to 31% in women.56 Similarly, in Samoa, the percentage of the population that smokes has decreased from 64% to 40% in men, and 21% to 17% in women, from 1991 to 2013.57 Some islands have taken particularly innovative measures. For example, the New Zealand territory, Tokelau was awarded the WHO Healthy Islands Best Practice Recognition for its policy of preventing the importation of fizzy drinks, and for its tobacco control policies, which include substantial increases in tobacco tax and reductions in importation.58
Cancer epidemiology and surveillance
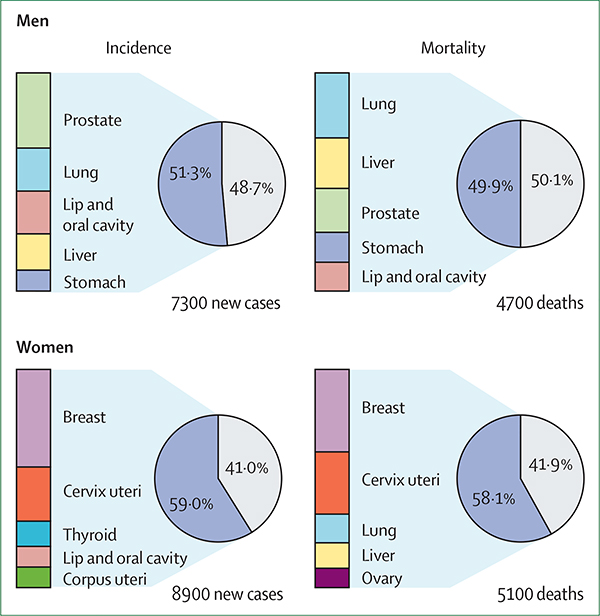
Approximately 16 200 new cancer cases and 9800 cancer deaths are reported in PICTs annually (figure 2). According to GLOBOCAN 2018 estimates,59 the cancer profile of the PICTs tells a story of ongoing transition from cancers associated with infection to those associated with high-income lifestyles. Around half of the cancer cases and deaths in men are due to cancers of the lung, liver, lip and oral cavity, prostate, or stomach (figure 2). In women, breast and cervical cancers are the major contributors in terms of both incidence and mortality and were responsible for around two-fifths of the total cancer burden in 2018. Thyroid, uterine, and oral cavity cancer are among the top five most common cancers; lung and liver cancers are still prominent causes of death in women (table 3). A high and increasing incidence of obesity-related cancers, particularly breast and uterine disease, has been noted in the region.48 A double burden emerges in the Pacific, with a profile that includes cancers linked to poverty and infection coinciding with those cancers that are more associated with a changing diet, physical inactivity, obesity, and exposure to tobacco, such as lung, breast and uterine cancers. As indicated, specific populations have a higher incidence of certain cancers, such as oral cancers among tobacco chewers and smokers and betel quid chewers in Papua New Guinea and Solomon Islands, and thyroid cancer in women of French Polynesia and New Caledonia (table 3).60,61 Evidence exists that suggests that over-diagnosis of thyriod cancer is a major problem globally, but the extent to which this is an issue in the Pacific is unknown.62
Figure 2:
Estimated proportion of total cancer incidence and mortality for the top five cancers by gender in selected Pacific island countries and territories (GLOBOCAN 2018)
Table 3:
Cancer incidence, mortality, and ranking of the top five most frequent cancers by gender for selected Pacific island countries and territories data based on GLOBOCAN 20l859
| Cancer incidence (age standardised rate per 100 000 people)* |
Cancer mortality (age standardised rate per 100 000 people)† |
Most frequent cancers in men |
Most frequent cancers in women |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | First | Second | Third | Fourth | Fifth | First | Second | Third | Fourth | Fifth | |
| Fiji | 141·1 | 189·2 | 78·6 | 108·1 | Prostate | Liver | Colorectum | Lung | Leukaemia | Breast | Cervix | Uterus | Thyroid | Ovary |
| French Polynesia | 272·2 | 211·6 | 157·2 | 102·2 | Prostate | Lung | Colorectum | Liver | Stomach | Breast | Thyroid | Lung | Colorectum | Uterus |
| Guam | 198·9 | 161·4 | 141·9 | 92·0 | Lung | Prostate | Liver | Colorectum | Stomach | Breast | Lung | Cervix | Colorectum | Uterus |
| New Caledonia | 357·1 | 297·3 | 151·6 | 86·5 | Prostate | Lung | Colorectum | Bladder | Stomach | Breast | Lung | Thyroid | Colorectum | Uterus |
| Papua New Guinea | 205·2 | 207·3 | 147·2 | 128·9 | Lip and oral | Prostate | Colorectum | Liver | Lung | Breast | Cervix | Lip and oral | Thyroid | Liver |
| Samoa | 202·3 | 217·1 | 126·2 | 112·4 | Prostate | Lung | Colorectum | Liver | Non-Hodgkin lymphoma | Breast | Lung | Uterus | Colorectum | Thyroid |
| Solomon Islands | 100·5 | 135·4 | 81·2 | 76·5 | Prostate | Liver | Lung | Leukaemia | Colorectum | Breast | Cervix | Thyroid | Uterus | Ovary |
| Vanuatu | 103·8 | 105·5 | 82·2 | 57·8 | Liver | Prostate | Lung | Leukaemia | Colorectum | Breast | Cervix | Thyroid | Uterus | Colorectum |
When data were not directly available from countries, cancer incidence was estimated on the basis of methods used by GLOBOCAN 2018.
When data were not available from countries, cancer mortality was estimated on the basis of methods used by GLOBOCAN 2018.
Future projections of the annual number of cancer cases and deaths in PICTs in 2040 relative to 2018 anticipate major increases in disease burden over the coming decades, given the effect of population ageing and growth. Assuming that no change in the overall cancer incidence occurs, demographic projections suggest that 84% more cancer cases and 92% more deaths will occur between 2018 and 2040. If cancer cases decline by 2% per annum, the number of cases and deaths is projected to increase by around 20% by 2040, but a 2% increase in the number of cases per annum would lead to an almost doubling of the current incidence and mortality estimates in the region (appendix p 1). These estimates translate to approximately 20 000–45 000 new cases and 12 000–28 000 additional deaths by 2040.63
Cancer surveillance in the Pacific region faces challenges that are common to most small nations worldwide. GLOBOCAN 2018 estimates (excluding New Caledonia and French Polynesia) of cancer incidence in the PICTs appear low (table 3), which might, in part, be due to an under assessment of cancer cases in the region as a result of a small number of robust cancer surveillance systems across the PICTs.9,59 The USAPI have a regional central cancer registry, which has nurtured country-specific registries;64 however, in the PICTs outside of the USAPI the quality and availability of diagnostic information and death certificates are inadequate, possibly resulting in underestimates of the region’s cancer burden.9,10 The International Agency for Research on Cancer estimates cancer incidence in countries that do not have cancer registries, with the use of data from similar, neighbouring countries.60 For example, in Papua New Guinea, a weighted average of the census data combined with the mean cancer incidence in Fiji, Vanuatu, and New Caledonia was used; likewise, the mean cancer incidence in Vanuatu and Fiji was used to calculate incidence for the Solomon Islands. To develop health-care capacity and support decision making, a Pacific Cancer Registry Hub is being established through the Global Initiative for Cancer Registry Development facilitated by the International Agency for Research on Cancer and supported by partners including Australia, New Zealand, SPC, and WHO. The Hub proposal was approved by the Pacific Heads of Health in 2018 and options are now being considered as to how to leverage necessary investments for implementation.
Cancer control planning in the region
Despite the challenges and complexities in which cancer prevention, care, and control exist in the Pacific, only a few PICTs have standalone comprehensive cancer control plans (table 2). The USAPI have the most comprehensive examples of cancer control plans, with an overarching regional plan that supports country-specific strategies. French Polynesia also has a specific cancer control plan, with Fiji finalising a draft plan. Other countries incorporate elements of cancer control within their NCD control strategies and reproductive health plans. Papua New Guinea, in particular, has incorporated a substantial amount of cancer control planning within the country’s NCD plan,65 and has developed local guidelines for the management of various types of cancer.66 Papua New Guinea has included a specified objective to reduce the incidence of cancers through immunisation, screening, early detection, treatment, and management, with plans to address risk factors, including the reduction of tobacco use, betel nut consumption, and harmful alcohol use, unhealthy diet, and physical inactivity. There are a number of other cancer-specific activities within this plan focusing on hepatitis B and human papillomavirus (HPV) vaccination delivery and coverage, the feasibility of preventing cervical cancer through visual inspection with acetic acid, developing a population-based cancer registry and improving palliative care services. Limitations in resource infrastructure and expertise might hinder the ability of some small Pacific nations to develop plans such as those of Papua New Guinea. Regional planning might be a more realistic way to combat the increasing number of cancer cases in the region,11 but, clearly, the existence of a PICT-specific plan alone is insufficient to ensure progress, even assuming that the plan is comprehensive. Sustained resources for specific activities and an ongoing evaluation of progress are key elements to any cancer control plan, but the extent to which these elements are being achieved in most PICTs is unclear.
Immunisation and screening
Chronic hepatitis B is endemic in most PICTs (prevalence of up to 27%).67 However, estimated coverage of hepatitis B vaccination is greater than 85% for most PICTs (table 2), and the region is seeing a decline in hepatitis B surface antigen seroprevalence.68 Nevertheless, vaccine coverage remains suboptimal in some Pacific nations, particularly those with large isolated rural populations (eg, vaccine coverage for hepatitis B is estimated to be 35% in Papua New Guinea).46 Pilot studies delivering vaccines outside the cold chain (ie, delivering vaccines in a manner which is less dependent on the products being kept below a certain temperature), educating pregnant women, and improving linkages between communities and health facilities have resulted in substantially higher vaccine coverage in a number of settings including the Solomon Islands69 and Kiribati compared with coverage before the initiation of these initiatives.70
Although cervical cancer has been recognised as a priority for cancer control in most PICTs,71 both HPV vaccination and cervical screening remain under developed in much of the Pacific region (table 2). National breast cancer screening programmes are available only in some countries of the USAPI, the two French territories, and the Cook Islands, but coverage in all three countries tends to be low (eg, 30–33% in French Polynesia)72 and essential quality elements are missing from the screening strategies (eg, French Polynesia’s programme does not have a recall system, and Federated States of Micronesia’s breast screening programme includes clinical breast examination only). No organised screening for bowel cancer occurs in any PICT, although opportunistic screening exists in some of the USAPIs. Oral screening through visual inspection for premalignant lesions related to betel nut chewing might be of value in high-risk individuals,73 but screening is only used in some clinics in Guam and the Northern Mariana Islands.
Establishing and sustaining population-based screening is challenging because of poor access to necessary infrastructure, such as information and laboratory systems, and personnel and competing priorities. Visual inspection with acetic acid and point-of-care HPV systems have changed the horizon for cervical screening by offering a single episode option for early detection and treatment.74 With resource constraints and competing health priorities, population-based breast screening with mammography or bowel screening might not be feasible in many PICTs, and caution must be exercised with opportunistic screening, which can strain health system resources and exacerbate inequalities across a country, particularly if lower risk people are more likely to be screened.
Cancer diagnosis and treatment
Early diagnosis and clear referral guidelines are important to optimise cancer outcomes. PICTs face numerous challenges in enhancing these processes, and few, if any, examples of documented cancer-specific pathways for diagnosis and referral exist. Overall, data on disease-related characteristics, treatment outcomes, and cancer survival are scarce or absent for most PICTs. Data from the Pacific Regional Central Cancer Registry, recorded from 2007 to 2015, showed that more than 70% of adult cancers are diagnosed at stage 3 or worse in all USAPIs. In addition, more than 50% of adult patients with cancer died within 5 years of diagnosis in most USAPIs, apart from American Samoa, Northern Mariana Islands, and Guam, with up to 80–90% of patients dying within 5 years of diagnosis on the Micronesian islands of Kosrae and Yap.75,76
Pathology, laboratory, and radiological services
The availability and accessibility of cancer diagnostics services, including pathology, are grossly disproportional to the current burden of the disease in the Pacific region (table 4). Less than a third of the 22 PICTs have a full-time pathologist or radiologist. The remainder of PICTs send specimens and patients overseas for diagnostic tests, which is expensive and can result in considerable delays.
Table 4:
Capacity for cancer care and numbers of specialists in 20 Pacific Island countries and territories as of mid-2018
| Publicly available pathology Services | Publicly available radiology Services | Number of specialist diagnostic staff | Publicly available cancer units that are operational | Publicly available chemotherapy Services | Number of medical oncologists | Publicly available radiotherapy Services | Number of publicly available radiotherapy centres | Number of radiation oncologists | Publicly available cancer surgery Services | Formal palliative care Services | Oral morphine available in primary care centres or public health sector | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Papua New Guinea | Histology, IHC, and cytology | MRI (private), CT, MMG, USS, and x-ray | 8 pathologistsand 8 radiologists | No | Yes | 0 | No (previously available) | 0 (previo us ly available) | 0 | Yes | No | Yes, but com mon ly out of stock outside urban areas |
| Fiji | Histology, IHC, and cytology | MRI, CT, MMG, USS, and x-ray | 1 pathologist and 3 radiologists | Yes | Yes | 1 | No | 0 | 0 | Yes | No | Yes, but commonly out of stock outside urban areas |
| Sol om on Islands | Non-gynaecological cytology only | MMG, USS, and x-ray | 1 pathologistand 1 radiologist | No | Few agents available | 0 | No | 0 | 0 | Yes | No | Yes, but commonly out of stock outside urban areas |
| Vanuatu | Some cytology and histology techniques | USS and x-ray | 1 pathologist and no radiologists | No | Paediatric cases only | 0 | No | 0 | 0 | Yes | No | Yes, but commonly out of stock outside urban areas |
| NewCaledonia | Histology, IHC, and cytology | MRI, CT, MMG, USS, and x-ray | 2 pathologists and 13 radiologists | Yes | Yes | 2 | Yes | 1 | 2 | Yes | Yes | Yes |
| French Polynesia | Histology, IHC, and cytology | Nuclear medicine, MRI, CT, MMG, USS, and x-ray | 2 patholog ists and 8 radiologists | Yes | Yes | 3 | Yes | 1 | 2 | Yes | Yes | Yes |
| Samoa | Histology, cytology | CT, MMG, USS, and x-ray | pathologistand radiologists | No | Paediatric cases only | 0 | No | 0 | 0 | Yes | No | Yes, but commonly out of stock outside urban areas |
| Guam | Histology | Nuclear medicine, MRI, CT, MMG, USS, and x-ray | 2 pathologistsand 20 radiologists | Yes | Yes | 5 | Yes | 1 | 2 | Yes | Yes | Yes |
| Kiribati | Gynaecological cytology | USS and x-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | No | Yes, but commonly out of stock outside urban areas |
| Federated States of Micronesia | Some cytology and histology techniques | USS and x-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | No | Yes, but commonly out of stock outside urban areas |
| Tonga | Histology, cytology | CT, MMG, USS, and x-ray | lpathologist and 2 radiologists | No | Mai ntenance only | 0 | No | 0 | 0 | Yes | No | Yes, but commonly out of stock outside urban areas |
| American Samoa | Histology | CT, MMG, USS, and x-ray | 1 pathologist and 1 radiologist | No | No | 0 | No | 0 | 0 | Limited | No | Yes |
| Northern Mariana Islands | Histology | USS and x-ray | lpathologist and no radiologists | No | Maintenance only | 0 | No | 0 | 0 | Limited | No | Yes |
| Marshall Islands | None available | USS and x-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | No | Yes |
| Palau | None available | CT, MMG, USS, and x-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | No | Yes |
| Cook Islands | None available | USS andx-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | Yes | Yes |
| Nauru | None available | CT, MMG, USS, and x-ray | No pathologists 1 radiologist | No | No | 0 | No | 0 | 0 | Limited | No | Yes |
| Tuvalu | None available | USS andx-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | Limited | No | Yes |
| Niue | None available | USS and x-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | No | No | Yes |
| Tokelau | None available | X-ray | No pathologists or radiologists | No | No | 0 | No | 0 | 0 | No | No | Yes |
Pitcairn Islands and Wallis and Futuna have been exduded from the analysis because no key informants were located to provide data. Limited surgery services means that only a few procedures for a few cancers can be performed, for example removal of obvious tumours. IHC=immunohistochemistry. MMG=mammography. USS=ultrasound screening.
In terms of infrastructure, most countries have basic radiological equipment, such as plain x-ray and ultrasound. However, only a few countries have functional mammograms, CT, or MRI scans, or capacity for fluoroscopy studies; a PET scan cannot be found across any of the 22 PICTs. Similarly, for pathology and laboratory diagnostic services, only Papua New Guinea, Fiji, Solomon Islands, Vanuatu, New Caledonia, Guam, French Polynesia, Tonga, and Samoa have access to histological and cytological methods of diagnosing cancers on the basis of haematoxylin and eosin and Papanicolaou stains. A small number of countries can test for biochemical tumour markers in the blood, but only New Caledonia, Papua New Guinea, Guam, French Polynesia, and Fiji have selective panels of immunohistochemistry stains for accurate diagnosis and treatment.77 Other techniques, such as molecular testing, flow cytometry, cytogenetics, and fluorescence in-situ hybridisation, are not available in all PICTs. Equipment breakdown is common, often with long delays for repair, resulting in delayed management of patients or requiring patients to travel overseas for diagnostic services. In many countries, diagnosis is largely done by clinical investigations.78 Previously reliant on off-island referrals for pathology services, the Federated States of Micronesia is currently using telepathology (including cytology and histology) with Japan. Laboratory technicians in all Federated States of Micronesia state hospitals have been trained to prepare the specimens, and the images are then digitally projected from the national telepathology lab in Pohnpei, Federated States of Micronesia, to a pathologist based in Japan for interpretation, reducing delays.79
Further barriers to establishing appropriate cancer diagnostics include underdeveloped quality management systems and the absence of national and regional quality standards for diagnostic services in the Pacific.80 To address these issues, the inaugural technical meeting for pathologists and registrars in the Pacific was held in 2018, with the aim of identifying approaches to improve standards and quality of pathology services in the region.
Efforts to improve the delivery of endoscopy training and service provision have been undertaken in the Solomon Islands, Fiji, Samoa, and Kiribati, aiming to improve diagnosis, and hopefully result in earlier detection of gastric and colorectal cancers.
Cancer surgery
Surgery is a central component in cancer control, required in more than 80% of cancers,81 and is responsible for approximately 65% of all sucessful treatments.82 In many Pacific countries, surgical services for cancer remain underdeveloped (table 4). Compared with HICs, the PICTs have relatively few surgeons, a high proportion of advanced stage cancers, and poor surgical infrastructure support, meaning that the provision of surgical services is extremely challenging compared with the ability to provide surgical treatment in neighbouring HICs. Most PICTs have a combination of surgical services, which range from in-country management options with or without the support of visiting specialist teams, to overseas referral depending on the infrastructure and support required for the condition. Niue is an example of a PICT with a small population and limited surgical capabilities (providing only basic surgery, such as appendectomy), where in comparison Fiji has the capacity for specialised cancer surgery, including neurosurgery and paediatric surgery.
There are a number of initiatives to increase the surgical capacity in the Pacific region, outlined by Ekeroma and colleagues.13 For example, the Pacific Islands Project, delivered by the Royal Australasian College of Surgeons, and the New Zealand Medical Treatment Scheme, have both engaged in service delivery and capacity improvement through the training of nursing, anaesthetic, surgical, and other core non-surgical specialist staff since 1995.83 At the end of 2018, approximately 150 Pacific surgeons had received their training in Papua New Guinea and Fiji, with the majority working in the region.84 In 2017, Nauru and Cook Islands were the only PICTs (outside the French territories, Niue, Tokelau, and USAPIs), that surpassed The Lancet’s Commission on Global Surgery85 target of 20 specialist surgeons, anaesthetists, and obstetricians per 100 000 population, with the remaining PICTs ranging from 1·6 (Samoa) to 18·5 (Tuvalu) specialists per 100 000 population.
Medical oncology
Adult oncology services are minimal in the Pacific region. There is only one medical oncologist in Fiji and no radiation oncologists outside of New Caledonia, French Polynesia, and Guam (table 4) within these three territories, medical oncology services are well developed. There are also some chemotherapeutic options available in Fiji, Papua New Guinea, and the Solomon Islands, but otherwise, little or no chemotherapy options are available for adult patients living with cancer in the other 16 PICTs.
Barriers to developing these services are common across the region: small, dispersed populations, poor medical infrastructure and resources, and competing service priorities. Some of the small islands might not have the population sizes large enough to justify a specialised oncology workforce, and there are only a few examples of strong links between hospital doctors working in the Pacific islands and oncologists in neighbouring HICs outside of paediatric oncology. Complex treatment protocols used in HICs are unlikely to be feasible in the Pacific islands and supportive care services might not be consistently available. Additionally, lack of rescue treatments for potential complications associated with neutropenia can be a barrier to clinicians providing chemotherapy even when it is available. The Caribbean region has developed beneficial procurement processes such as those developed by the Organisation of the Eastern Caribbean States and the Pan-American Health Organisation,86 but no such pan-Pacific processes exist.87 For those countries that do provide chemotherapy, procurement of drugs can be problematic, with the drugs mainly provided by other countries and continents, largely Australia, New Zealand, Asia, and the USA. The Solomon Islands is currently building a small oncology unit with at least one full-time oncology trainee, with the aim of centralising and improving cancer care. Treatment and outcomes for childhood cancer are improving because of the combined efforts of clinicians and policy makers through partnerships with neighbouring HICs. These initiatives are described in more detail by Ekeroma and colleagues.13
Radiotherapy
Radiotherapy is an essential part of cancer care.88,89 On the basis of the model developed by Barton and colleagues,88 and with data from GLOBOCAN estimates for cancer incidence in each country, we estimate that between 42% and 55% of patients with cancer in the Pacific islands will need radiotherapy at least once, totalling roughly 6500 patients every year. Access to radiotherapy would improve local disease control from 17% to 29%, increase survival from 4% to 8%, prevent more than 1400 cancer recurrences, and save about 400 lives per year.88 However, only three functioning radiotherapy facilities are available in the Pacific region (table 4).
Major barriers to the development of radiotherapy services are the low caseloads due to the low population sizes with a small number of people requiring radiotherapy and the difficulties of recruiting and retaining trained staff in a health environment that enables the delivery of a quality service. There are additional barriers relating to the cost of the facilities, equipment maintenance costs, and expertise and the need for diagnostic, surgical, and engineering supports. Only Fiji and Papua New Guinea have a sufficient caseload (over 400 new radiotherapy cases per year) to make use of a single megavoltage machine like a Cobalt-60 or a linear accelerator.90 Cobalt has been favoured because of its robustness, but safety and technical limitations have meant that linear accelerators are more prevalent in low-income and middle-income countries.91 Papua New Guinea had a single cobalt machine for many years that broke down in 2000.89 In 2010 it was replaced with another Cobalt machine, but the machine has not been used since the country’s only radiation oncologist died in 2017. Fiji has plans for a radiotherapy service and modelling suggests that it could be cost-effective.92
For now, improved access to radiotherapy services for those living in the Pacific islands will require innovative methods of delivering the treatment, which substantially reduces the cost of standalone units and enables the remote operation of some functions, with quality assurance and planning and perhaps teleconsultations being important options to consider.93
Palliative care
Palliative care is underdeveloped in the Pacific region.94–96 Much of the work of palliative care is undertaken by the patient’s extended family, with often insufficient support from health-care professionals. Ad-hoc services within existing health-care structures, including NGOs such as local Cancer Societies and faith-based organisations, have begun to lead work to strengthen the provision of palliative care. However, these services tend to be unfunded, and not well supported by senior health-care staff or by associated policies, strategies, and guidelines. Correct use of analgesics, such as morphine, in patients requiring palliative care is a major ongoing issue, and access to morphine is extremely poor in many parts of the Pacific, especially in rural areas and in the outer islands. Opioid utilisation is extremely low in the Pacific.97,98
Given the growing burden of cancer (and other NCDs), and the small range of treatment options, the need for high-quality palliative care is likely to increase. However, service development efforts, in particular financial aid, have often been directed towards projects focused on saving and improving lives, rather than supporting the development of palliative care services.99
Nevertheless, some progress in building capacity to support palliative care has been made. The Essential Pain Management initiative is endorsed by the Faculty of Pain Medicine, Australian and New Zealand College of Anaesthetists.100 Essential Pain Management workshops have been held in the Pacific since 2011, teaching a simple framework of recognition, assessment, and management of all types of pain, including cancer pain. A shortened version of Essential Pain Management for undergraduates is now embedded into the medical undergraduate curriculums in Fiji and Samoa. In the USAPI, efforts to improve palliative care with telehealth training, curriculum development, and inclusion of traditional methods for end of life and palliative care have been made.101
Traditional and alternative medicine
Traditional healers are often the first point of contact for people seeking health care. Many cultural and spiritual beliefs surround illness in PICTs, and for many people living in the Pacific the use of various traditional customs and alternative medicines has been common practice for many centuries. There are strong traditional beliefs around the origin of sickness, which can include the belief that sickness is punishment for a cultural or spiritual transgression.
In a setting with scarce treatment options and often poor outcomes associated with conventional cancer treatment, traditional medicine might be first-line health care; however, traditional medicine is generally practised outside of the formal health system. Patients commonly consult a traditional or religious healer before or during conventional medical treatment, which can result in delays in accessing or completing medical diagnosis and treatment. Traditional healers in these settings are often highly regarded and respected in their communities, and they are able to offer treatment to a patient usually in the home setting surrounded by family, with language and concepts that the patient understands.
Traditional medicines are typically not catalogued or recorded, and research into their use is minimal. However, some PICTs have recognised traditional healers under aspects of their health policy. For example, in 2007, the Papua New Guinea Government approved a National Policy on Traditional Medicine, recommending the integration of traditional medicine into the national primary health-care system. A traditional medicine database containing a repository of medicinal plant usage in Papua New Guinea has been operational since the early 2000s to promote the safe and effective use of traditional medicine, and to promote further research into these practices. Additionally, work is being done to identify, document, and support indigenous approaches to survivorship, end of life, and palliative care across a number of PICTs, including Federated States of Micronesia.102
Travel for cancer services
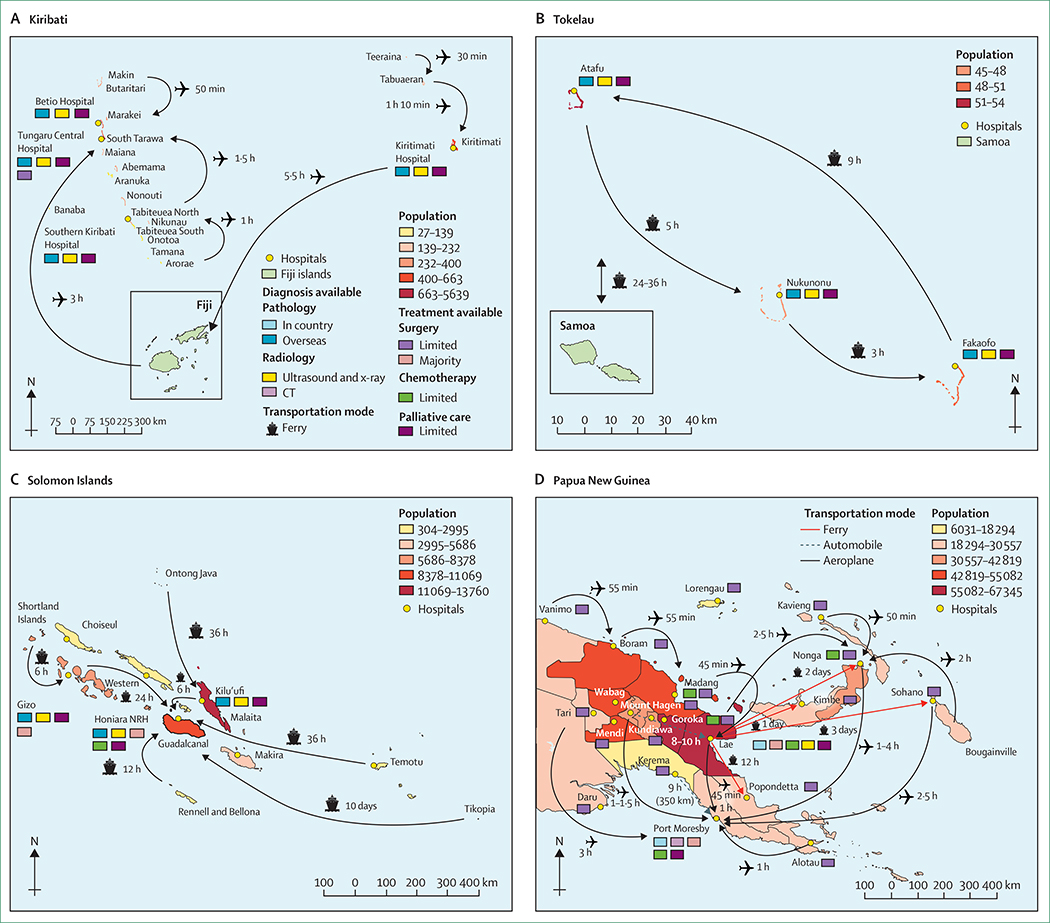
In six PICTs, more than three-quarters of the population live rurally;1 as a result, substantial additional logistical challenges exist for rural and outer island populations when accessing cancer care in the Pacific (panel 1). Adequate road networks connecting health-care centres to the population exist in many PICTs, but remote outer islands can have less developed or poor access to transport links. Access to cancer treatment can often require travel by boat, plane, and car (figure 3). Sea and land transport options in some PICTs can be dangerous, absent, or poorly maintained, and if available, air travel is costly. Furthermore, frequent natural disasters can disrupt travel plans. For these reasons, many will not seek medical treatment, present late, or not return for follow-up.
Panel 1: Case study illustrating the barriers relating to travel in the Solomon Islands.
Mrs A is a 40-year-old married woman with five children living in rural Solomon Islands. Her family has a subsistence-based lifestyle (fishing, gardening, and producing copra) and household annual income is approximately 7800 Solomon Islands dollars (SBD; around US$960). The nearest nurse aid clinic is 1 h away by canoe (SB$30 for fuel, return trip). She notices a breast lump that gradually increases in size over 3 years. She presents to the provincial hospital 9 h away by passenger boat where she is diagnosed clinically with breast cancer. She is referred to the central hospital in Honiara for a biopsy. To access this service, the patient and her sister travel by passenger boat for 24 h, costing $500 per person per trip (approximately US$60). A biopsy of the breast lump is done and the tissue sent to a lab in Australia. Mrs A stays with family members for a few days following her biopsy and then returns to her home village by boat. After 1 month, the central hospital receives a result confirming locally advanced breast cancer. A few months later, after not hearing back from the hospital and concerned about the breast lump, Mrs A undertakes the journey from her village once again with her sister to the central hospital. This time she undergoes a total mastectomy and receives some chemotherapy under the surgical team. On discharge she remains with her family for a few days and then returns to her home village, where she undergoes no further follow-up.
Figure 3: Required travel routes and times taken by patients within selected Pacific Island countries and territories to access cancer care.
Transportation methods and time taken for patients from Kiribati (A), Tokelau (B), Solomon Islands (C), and Papua New Guinea (D) to reach cancer care. NRH=National Referral Hospital of Honiara.
Kiribati’s three island groups are spread over a distance of 3·5 million km2, with no direct air travel from the outer Line Islands (Kiritimati Island [Northern Line Islands] in the east, Arorae in the south, and Makin in the north; figure 3A) to the capital, Tarawa. Similarly, the smallest PICT, Tokelau (figure 3B), does not have an airport or port, and all off-island travel must go via Samoa, a 24–30 h boat journey available fortnightly. In the Solomon Islands (figure 3C), Vanuatu, and Federated States of Micronesia, travel between the outer islands is predominantly by sea. Ships can come weeks to months apart and often have little to no safety equipment on board. Elsewhere, more than 80% of Papua New Guinea’s population is located in rural areas and no road link exists between the capital, Port Moresby, and the former radiotherapy services in Lae (figure 3D). Rugged mountainous terrain, swamp lands, and large rivers make over half the country inaccessible by road.
Overseas referrals
Some patients with cancer in the Pacific might travel to treatment centres in other countries, either neighbouring PICTs with a comparatively higher level of care, or to Australia, New Zealand, France, or the USA. Referrals are absolutely necessary for the patient to gain access to more complex or specialised care in smaller PICTs. However, for many individuals accessing care overseas is very challenging and often an option only available to those that are well connected or have a high income. Increasingly, PICTs are negotiating with hospitals in the Philippines, India, and China to access cancer care because the cost of care is lower in these countries. Residents of the three New Zealand territories (Cook Islands, Niue, and Tokelau) are eligible for free cancer treatment in New Zealand hospitals, and in some instances, respective governments cover the costs of airfares for the patient (and occasionally an escort); however, the costs of accommodation and other expenses for those patients travelling to New Zealand are borne by the patient and their family.103
Most paediatric oncology cases in French Polynesia are referred to mainland France and cases from New Caledonia are sent to Australia for treatment. Patients from the USAPIs are predominantly referred to the Philippines, Taiwan, or the US mainland.
Most PICTs have state-funded international referral processes and procedures.104 Governments are challenged to meet a growing demand for specialised treatments only available offshore with a restricted budget. Referral committees or clinicians are faced with making judgments about the potential benefits for patients, often on the basis of poor diagnostic ability and inadequate information regarding prognosis available to them. This process can take weeks or months, reducing the likelihood of successful treatment. In addition, patients are often expected to pay for their own travel and accommodation, which is beyond the financial means of many. In 2017, 1929 patients from 11 PICTs were referred overseas, with the highest number of referrals to New Zealand (n=594), France (n=535), Taiwan (n=212), Philippines (n=189), and India (n=117). Other destinations included: Hawaii (n=84), Malaysia (n=62), Fiji (n=53), Samoa (n=51), the USA (n=23), and Australia (n=9). In 2017, at least 7% of overseas medical referrals from five PICTs were oncology referrals.105 For some PICTs, overseas referrals are a prominent portion of their health budget, up to half of the current health expenditure for some countries.105 For most PICTS, the estimation of the proportion of patients who would be likely to benefit from referral and who actually receive it is difficult to determine, but, in Fiji where some cancer treatment is available, 10–15% of patients with cervical cancer requiring curative or palliative radio therapy received their treatment overseas, which was funded by the Fijian Government.92
Research
In addition to the poor health systems in most PICTs, health research systems in those countries are either fragile or non-existent.106,107 Improving national health research systems from the top down will need considerable political leadership and financial commitment as seen in the success of the Papua New Guinea Institute of Medical Research, which is part-funded by the Government of Papua New Guinea.108 The Institute has had great success at attracting funding and has formed multiple collaborations with international researchers and academic institutions, leading to high research output.109 In the small island states, sharing and using research systems of larger countries within the region is a more viable option, such as the Cook Islands requiring researchers to have ethical approval from a New Zealand institution.109 Because most researchers will be clinicians, building research capacity in the Pacific islands where objectives are aligned to national health goals and the projects are implementational or operational in nature is needed.110 Bottom-up research capacity building approaches are also needed, where overseas collaborators engage and build the skills of local people; this type of collaboration has occurred between Yale University, New Haven, CT, USA, and Brown University, Providence, RI, USA, and Samoa.111 Genuine research collaborations are a vital key to research capacity building in the Pacific,112 and, with the incidence of cancer predicted to increase as a result of increasing levels of obesity, the region is ripe for research into cancer prevention.
Conclusion and recommendations
The Pacific region, with its geographically dispersed countries and territories, faces tremendous challenges in providing adequate cancer prevention and control services. Many of these challenges are common to other LMICs, but others are specific to small island states. In particular, the small populations of these geographically isolated islands, which are regularly exposed to natural disasters, means that few financial or personnel resources are available for cancer care. Additionally, this region has been largely neglected in global cancer control agendas. Addressing the problems of cancer control inevitably intersects with a more general strengthening of the entire health-care system; improving out comes from cancer requires integration and action from all sectors of the health system and governments, health workforce development, and a focus on health-care financing, prioritisation, and procurement. We acknowledge this broader agenda and the context in which cancer control strategies need to be developed.
There are a number of possible actions to address the challenges of cancer control in the Pacific region. We have outlined the actions that we believe should be prioritised (panel 2). These recommendations were tabled at the Pacific Heads of Health meeting, April 3, 2019, Nadi, Fiji, and will be tabled at the Ministers of Health meeting scheduled for Aug 6–9, 2019, Tahiti. These include considering a regional collaborative approach to cancer control, ensuring cancer control is made integral to the broader NCD agenda, strengthening palliative care provision in the region, increasing HPV vaccination and cervical cancer screening, improving cancer surveillance, and developing cancer treatment capacity. Importantly, the focus of development should not shift to expensive low-value therapies as has been seen in some other LMICs.113
Panel 2: Recommendations for cancer control for the Pacific region
Regional collaborative approach to cancer control
In environments of constrained resource, in particular for regions with low numbers of health-care professionals, which is inherent in countries with small population numbers, sharing expertise, experience, and resources (such as educational and technical resources) is likely to be almost an inevitable prerequisite for success. The close relationships that exist across and beyond countries in the Pacific region provide an excellent foundation to move the cancer agenda forward. We recommend that countries and regional organisations consider regional or subregional collaborative approaches to control cancer, including cancer control planning and surveillance, cancer screening, and cancer treatment services such as drug and equipment procurement.
Ensure cancer control is integral to the broader non-communicable disease (NCD) agenda
Strengthening tobacco control strategies is a focus for the region, yet many countries have very high numbers of smokers, particularly among men. Ensuring that evidence-based policies, such as tobacco taxation (including the increase of excise duties to at least 70% of the retail price of cigarettes, as outlined in the NCD Roadmap);114 smoke-free environments; bans on advertising, promotion, and sponsorship; warning labels of tobacco; and cessation support, are fully implemented remains a priority. The role of obesity in driving the NCD epidemic in the Pacific is indisputable and the burden associated with the high number of obesity-related cancers in the region is expected to increase over time. Strategies to address disease burden should prioritise cost-effectiveness plans, such as taxes and subsidies on food and drinks, including the increase of sugar-sweetened beverage excise taxes114 to 20% of the retail price; mandatory healthy food policies in schools (eg, banning sugary drinks and ensuring healthy food and beverages are available, such as water and fruit); and restricted marketing of unhealthy food to children.114 The Pacific Monitoring Alliance for NCD Action115 is monitoring progress towards these goals. We strongly support continued action to meet the goals of the Pacific NCD Roadmap, particularly those relating to tobacco use, and lowering the prevalence of excess bodyweight.
Strengthened palliative care provision in the region
Improved palliative care is imperative in the region, particularly access to immediate-release morphine for those with moderate-to-severe pain or dyspnoea. Improvements are likely to require a review of potential legal and regulatory barriers, awareness building campaigns, workforce development, and the development of palliative care guidelines and service delivery plans in collaboration with health-care providers (including nurses, doctors, and pharmacists), patients and their families, communities, including traditional healers, and non-government organisations. The Lancet Commission97 on palliative care developed an Essential Package of Palliative Care, which includes essential medications, equipment, and human resources to provide basic palliative care in resource-constrained environments. We recommend that all Pacific countries have a palliative care plan or ensure the full integration of palliative care in relevant health sector plans by 2030.
Increasing human papillomavirus (HPV) vaccination and cervical cancer screening
Cervical cancer is a major burden in the region; it is the second biggest cause of cancer death among women. It was identified as a priority for action by Pacific health leaders in 2014. Prevention and control of cervical cancer through HPV vaccination of girls aged 9–13 years and cervical screening of women aged 30–49 years are recommended as part of the WHO “Best Buys” for low-income and middle-income countries.116 Recent research based in Samoa has suggested that cervical screening with HPV screening would be highly cost-effective, feasible, and acceptable to the population under a range of scenario assumptions.117 We recommend that by 2030, 70% of girls aged 9–13 years are immunised against HPV and that at least 70% of women aged between 30 years and 49 years have undergone at least one cervical cancer screen with timely, safe, and effective treatment of precancerous lesions in all Pacific countries and territories.
Improving cancer surveillance
Effective cancer control planning and monitoring requires up-to-date, accurate data on the current and emerging patterns of cancer incidence and survival. Functional high-quality cancer registers provide these data. The Global Initiative of Cancer Registers is working with a number of Pacific nations to develop a cancer registry hub in the region. We support this initiative, and recommend that ongoing, sustainable resources are identified to ensure the successful implementation and continuing viability of this initiative in at least five Pacific countries that do not have high-quality cancer registers by 2025.
Developing cancer diagnostic and treatment capacity across the region
Pan-Pacific improvements to cancer diagnostic and treatment capacity requires longer-term investment and must be balanced with competing health and welfare priorities. The extent to which timely diagnosis and treatment can be provided within countries will depend on their capacity and access to resources (within and outside the country). Effective networks need to be established and maintained to ensure access for small populations. Some services will inevitably need to be provided outside of some of the Pacific island nations and territories. At a minimum, there should be a focus on ensuring safe, effective, and accessible diagnosis and treatment for cancers with good prognosis, such as early-stage breast, cervical and colorectal cancers, lymphoma, and curable childhood cancer. We recommend that Pacific countries set targets and work towards ensuring that all stage 1 and 2 breast, cervical and colorectal cancers, and curable childhood cancers are treated with curative intent in a timely and effective manner.
Search strategy and selection criteria
We identified all published reports and grey literature written in English (with one exception) through searches of PubMed The initial search was completed by Dec 30, 2018, with key sources checked until April 1, 2019, using the search terms “Pacific”, “cancer”, “oncology” “small island developing states”, “sids”, “palliative care”, “traditional medicine”, “alternative medicine”, “tobacco control”, “NCD control”, “surveillance”, “prevention”, “screening”, and “International referrals”. We searched grey literature from key international agencies including WHO, the World Bank, the UN, and a number of regional governmental and non-governmental sources (such as The Pacific Community, Pacific Cancer Programs), individual country reports, and from reports from Heads of Health and Ministers of Health meetings in the Pacific. We also obtained specific data on cancer control activities from Ministries of Health and clinicians within each country included in this Series. References were included on the basis of originality and relevance to the broad scope of this Series paper.
Despite the challenges involved, PICTs are developing innovative and practical solutions. There are some indicators of success; reduction in the number of smokers in some countries, improved monitoring of NCDs, increasing focus on prevention of cervical cancer, and improved survival of children with cancer.
Supplementary Material
Acknowledgments
Declaration of interests
NP is supported by current Centers for Disease Control and Prevention cooperative agreement numbers 17NU58DP006312 (Pacific Regional Central Cancer Registry 2017–222), NU58DP006335 (American Samoa CCC 2017–222), NU58DP006348 (CNMI CCC 2017–222), NU58DP006269 (Guam CCC 2017–222), NU58DP006303 (FSM CCC 2017–222), NU58DP006336 (RMI CCC 2017–222), NU58DP006289 (Palau CCC 2017–222), and NU58DP005810 (REACH 2014–218), and the National Cancer Institute 2U54CA143727. NP’s contribution to the contents are solely the responsibility of the author and do not necessarily represent the official views of the Centers for Disease Control and Prevention, the National Cancer Institute, or the Department of Health and Human Services. All other authors declared no competing interests. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Footnotes
For more on the Global Initiative for Cancer Registry Development see http://gicr.iarc.fr
See Online for appendix
Contributor Information
Diana Sarfati, Department of Public Health, University of Otago Wellington, Wellington, New Zealand.
Rachel Dyer, Department of Public Health, University of Otago Wellington, Wellington, New Zealand.
Filipina Amosa-Lei Sam, Pathology Department, Tupua Tamasese Meaole Hospital, Private Bag National Health Services, Apia, Samoa.
Michael Barton, Collaboration for Cancer Outcomes Research and Evaluation, Ingham Institute for Applied Medical Research, University of New South Wales, Liverpool, NSW, Australia.
Freddie Bray, Cancer Surveillance Section, International Agency for Research on Cancer, Lyon, France.
Eka Buadromo, Pathology Department, Vaiola Hospital, Nuku’alofa, Tonga.
Alec Ekeroma, Department of Obstetrics and Gynaecology, National University of Samoa, Apia, Samoa; Department of Obstetrics and Gynaecology, University of Otago, Wellington, New Zealand.
Sunia Foliaki, Centre for Public Health Research, Massey University-Wellington Campus, Wellington, New Zealand.
James Fong, Obstetrics and Gynaecology Unit, Colonial War Memorial Hospital, Ministry of Health, Suva, Fiji; Department of Obstetrics and Gynaecology, Fiji National University, Suva, Fiji.
Josephine Herman, Ministry of Health, Rarotonga, Cook Islands.
Linda Huggins, Palliative Care Services, Middlemore Hospital, Counties Manukau Health, Auckland, New Zealand.
Kiki Maoate, Department of Paediatric Surgery, Christchurch Public Hospital, Christchurch, New Zealand.
Ineke Meredith, Department of Surgery, Capital; Coast District Health Board, Wellington Regional Hospital, Wellington, New Zealand.
Glen Mola, Department of Obstetrics, Gynaecology and Reproductive Health, Port Moresby General Hospital, Port Moresby, Papua New Guinea; School of Medicine and Health Sciences, University of Papua New Guinea, Boroko, Papua New Guinea.
Neal Palafox, Pacific Regional Cancer Programs, Department of Family Medicine and Community Health, John A Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA; Population Sciences in the Pacific Program, University of Hawaii Cancer Center, Honolulu, HI, USA.
Viliami Puloka, Department of Public Health, University of Otago Wellington, Wellington, New Zealand; Health Promotion Forum of New Zealand, Auckland, New Zealand.
Hai-Rim Shin, Non-communicable Disease and Health Promotion, Western Pacific Regional Office, World Health Organization, Manila, Philippines.
Jane Skeen, Starship Blood and Cancer Centre, Starship Children’s Health, Auckland, New Zealand.
Wendy Snowdon, Division of Pacific Technical Support, World Health Organization, Suva, Fiji.
Malama Tafuna’i, Department of Obstetrics and Gynaecology, National University of Samoa, Apia, Samoa.
Andrea Teng, Department of Public Health, University of Otago Wellington, Wellington, New Zealand.
David Watters, Deakin University and Barwon Health, University Hospital Geelong, Geelong, VIC, Australia.
Paula Vivili, Public Health Division, Pacific Community, Noumea, New Caledonia.
References
- 1.Statistics for Development Division. 2018 pocket statistical summary. 2018. https://prism.spc.int/ (accessed Oct 30, 2018). [Google Scholar]
- 2.SPC-SDD. National minimum development indicators. 2018. http://www.spc.int/nmdi/ (accessed May 18, 2018). [Google Scholar]
- 3.World Bank. World Bank open data. 2018. https://data.worldbank.org/ (accessed July 8, 2018).
- 4.McIver L, Kim R, Woodward A, et al. Health impacts of climate change in Pacific island countries: a regional assessment of vulnerabilities and adaptation priorities. Environ Health Perspect 2016; 124: 1707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of the High Representative for the Least Developed Countries, Landlocked Developing Countries and Small Island Developing States (UN-OHRLLS) Small island developing states in numbers: climate change. Edition 2015. https://sustainabledevelopment.un.org/content/documents/2189SIDS-IN-NUMBERS-CLIMATECHANGE-EDITION_2015.pdf (accessed Jul 8, 2019) [Google Scholar]
- 6.WHO. Health systems development in the Pacific http://www.wpro.who.int/southpacific/programmes/health_sector/health_systems/page/en/ (accessed Nov 2, 2018).
- 7.Wikipedia. South Pacific tropical cyclone. https://en.wikipedia.org/wiki/South_Pacific_tropical_cyclone (accessed May 31, 2019).
- 8.Connell J The two cultures of health worker migration: a Pacific perspective. Soc Sci Med 2014; 116: 73–81. [DOI] [PubMed] [Google Scholar]
- 9.Tervonen H, Foliaki S, Bray F, Roder D. Cancer epidemiology in the small nations of Pacific islands. Cancer Epidemiol 2017; 50 (Pt B): 184–92. [DOI] [PubMed] [Google Scholar]
- 10.Tervonen HE, Bray F, Foliaki S, Roder D. Cancer registration challenges in low- and middle-income countries—the case of the Pacific islands. Eur J Cancer Care 2017; 26: 1–5. [DOI] [PubMed] [Google Scholar]
- 11.Foliaki S, Bates C, Tukana I, Palafox NA. Cancer control in the Pacific: a South Pacific collaborative approach. Cancer Epidemiol 2017; 50: 193–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martiniuk A, Jagilli R, Natuzzi E, et al. Cancer in the Solomon Islands. Cancer Epidemiol 2017; 50: 176–83. [DOI] [PubMed] [Google Scholar]
- 13.Ekeroma A, Dyer R, Palafox N, et al. Cancer management in the Pacific region: a report on innovation and good practice. Lancet Oncol 2019; published online Aug 5. 10.1016/S1470-2045(19)30414-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin HR, Carlos MC, Varghese C. Cancer control in the Asia Pacific region: current status and concerns. Jpn J Clin Oncol 2012; 42: 867–81. [DOI] [PubMed] [Google Scholar]
- 15.SPC. The Pacific Community. https://www.spc.int/our-members (accessed Oct 30, 2017).
- 16.Firth S Instability in the Pacific Islands: A status report. Sydney, NSW: Lowy Institute, 2018. [Google Scholar]
- 17.Anderson I, Irava W. The implications of aging on the health systems of the Pacific islands: challenges and opportunities. Health Syst Reform 2017; 3: 191–202. [DOI] [PubMed] [Google Scholar]
- 18.Negin J, Robinson H. Funding for HIV and non-communicable diseases: implications for priority setting in the Pacific region. Health Policy Plan 2010; 24: 72–81. [Google Scholar]
- 19.Hodge N, Slatyer B, Skiller L. Solomon Islands health systems review. Manila: World Health Organization, Regional Office for the Western Pacific, 2015. [Google Scholar]
- 20.Grundy J, Dakulaia P, Wai K, Maaisen A, Whittaker M. Papua New Guinea Health Systems Review. New Delhi: World Health Organization, Regional Office for South-East Asia, 2019. [Google Scholar]
- 21.Roberts G, Irava W, Tuiketei T, et al. The Fiji Islands health systems review. Manila: World Health Organization, Regional Office for the Western Pacific, 2011. [Google Scholar]
- 22.Hort K, Nachtnebel M, Mahony A, Pillai N. Purchasing arrangements with the private sector to provide primary health care in underserved areas. Manila: World Health Organization, Regional Office for the Western Pacific, 2014. [Google Scholar]
- 23.Rodny A, Huana S, Ika V, et al. The Kingdom of Tonga health systems review. Manila: World Health Organization, Regional Office for the Western Pacific, 2015. [Google Scholar]
- 24.WHO. Apia action plan on traditional medicine in the Pacific island countries (Apia Action Plan 2000). Manila: World Health Organization, 2000. [Google Scholar]
- 25.WHO. World Health Organization: Western Pacific. https://www.who.int/westernpacific (accessed June 2, 2018).
- 26.New Zealand Foreign Affairs and Trade. Aid & development. 2018. https://www.mfat.govt.nz/en/aid-and-development/our-approach-to-aid/where-our-funding-goes/ (accessed June 17, 2018).
- 27.OECD. Aid at a glance charts. 2017. http://www.oecd.org/dac/financing-sustainable-development/development-finance-data/aid-at-a-glance.htm (accessed June 17, 2018).
- 28.Lowy Institute. Pacific Aid Map. 2018. https://pacificaidmap.lowyinstitute.org/ (accessed Jan 7, 2018).
- 29.WHO. Global Health Observatory data repository. 2018. http://apps.who.int/gho/data/node.main.A1444 (accessed Sept 17, 2018). [DOI] [PubMed] [Google Scholar]
- 30.WHO. Health Information and Intelligence Platform (HIIP): country profiles. 2015–16 http://hiip.wpro.who.int/portal/Countryprofiles.aspx (accessed September 17, 2018).
- 31.Asante AD, Negin J, Hall J, Dewdney J, Zwi AB. Analysis of policy implications and challenges of the Cuban health assistance program related to human resources for health in the Pacific. Human Resource Health 2012; 10: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WHO, Pacific Community. Health workforce development in the Pacific. 2017. http://www.wpro.who.int/southpacific/pic_meeting/2017/documents/12thphmm_session04_03_hwf_16aug.pdf (accessed Jan 9, 2019).
- 33.Legge D, Gleeson D, Snowdon W, Thow AM. Trade agreements and non-communicable diseases in the Pacific islands. Samoa: World Health Organisation Pacific NCD Forum, 2013. [Google Scholar]
- 34.Snowdon W, Moodie M, Schultz J, Swinburn B. Modelling of potential food policy interventions in Fiji and Tonga and their impacts on noncommunicable disease mortality. Food Policy 2011; 36: 597–605. [Google Scholar]
- 35.Thow AM. Trade liberalisation and the nutrition transition: mapping the pathways for public health nutritionists. Public Health Nutr 2009; 12: 2150–58. [DOI] [PubMed] [Google Scholar]
- 36.Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med 2012; 9: e1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Snowdon W, Thow AM. Trade policy and obesity prevention: challenges and innovation in the Pacific islands. Obes Rev 2013; 14 (suppl 2): 150–58. [DOI] [PubMed] [Google Scholar]
- 38.Sahal Estimé M, Lutz B, Strobel F. Trade as a structural driver of dietary risk factors for noncommunicable diseases in the Pacific: an analysis of household income and expenditure survey data. Global Health 2014; 10: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lin TK, Teymourian Y, Tursini MS. The effect of sugar and processed food imports on the prevalence of overweight and obesity in 172 countries. Global Health 2018; 14: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thow AM, Reeve E, Naseri T, Martyn T, Bollars C. Food supply, nutrition and trade policy: reversal of an import ban on turkey tails. Bull World Health Organ 2017; 95: 723–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.WHO. Noncommunicable diseases and their risk factors . STEPS country reports. 2019. https://www.who.int/ncds/surveillance/steps/reports/en/ (accessed April 8, 2019). [Google Scholar]
- 42.Secretariat of the Pacific Community. Agenda item 3·1: pacific non communicable diseases roadmap—progress update, 2017. 5th Meeting of the Heads of Health; April 25–27, 2017, Suva, Fiji. [Google Scholar]
- 43.WHO. WHO vaccine-preventable diseases: monitoring system. 2018 global summary. 2018. http://apps.who.int/immunization_monitoring/globalsummary/ (accessed April 7, 2019). [Google Scholar]
- 44.Sung H, Siegel RL, Torre LA, et al. Global patterns in excess body weight and the associated cancer burden. CA Cancer J Clin 2018; 69: 88–112. [DOI] [PubMed] [Google Scholar]
- 45.Land CE, Bouville A, Apostoaei I, Simon SL. Projected lifetime cancer risks from exposure to regional radioactive fallout in the Marshall Islands. Health Phys 2010; 99: 201–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prăvălie R Nuclear weapons tests and environmental consequences: a global perspective. Ambio 2014; 43: 729–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Simon S, Bouville A, Land C. Fallout from nuclear weapons tests and cancer risks. Am Sci 2006; 94: 48–56. [Google Scholar]
- 48.Kessaram T, McKenzie J, Girin N, et al. Noncommunicable diseases and risk factors in adult populations of several Pacific islands: results from the WHO STEPwise approach to surveillance. Aust NZ J Public Health 2015; 39: 336–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Kidney Foundation of Samoa. Annual report July 2015—June 2016. 2016. http://www.palemene.ws/new/wpcontent/uploads//05.Annual%20Reports/NKF/NKF-2016-AnnualReport-Final-English-Jan-2017.pdf (accessed Oct 30, 2018).
- 50.Forum Economic Finance Ministers Meeting. Non-Commicable Disease (NCD) Roadmap report. Washington, DC: World Bank, 2014. [Google Scholar]
- 51.Magnusson RS, Patterson D. How can we strengthen governance of non-communicable diseases in Pacific island countries and territories? Asia Pac Policy Stud 2015; 2: 293–309. [Google Scholar]
- 52.Joint Forum of Economic and Pacific Health Ministers. Joint Forum Economic and Pacific Health Ministers meeting outcomes statement Honiara, Solomon Islands 2014. https://cooperation-regionale.gouv.nc/sites/default/files/atoms/files/outcomes.pdf (accessed Sept 30, 2018). [Google Scholar]
- 53.WHO Western Pacific Region. Tobacco-free Pacific 2025. http://www.wpro.who.int/southpacific/programmes/healthy_communities/tobacco/page/en/ (accessed May 15, 2019).
- 54.Secretariat for Pacific Heads of Health Meeting. Agenda item: pacific monitoring alliance for nci action—update, 2018. 6th Meeting of the Heads of Health; April 25–27, 2017, Denarau, Fiji. [Google Scholar]
- 55.Tolley H, Snowdon W, Wate J, et al. Monitoring and accountability for the Pacific response to the non-communicable diseases crisis. BMC Public Health 2016; 16: 958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kessaram T, McKenzie J, Girin N, et al. Tobacco smoking in islands of the Pacific region, 2001–2013. Prev Chronic Dis 2015; 12: E212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Linhart C, Naseri T, Lin S, et al. Tobacco smoking trends in Samoa over four decades: can continued globalization rectify that which it has wrought? Global Health 2017; 13: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tauafiafi LAF. Tokelau wins prestigious 2017 WHO Tobacco Free global award. https://www.tokelau.org.nz/Bulletin/Sept+2017/Tokelau+wins+prestigious+2017+WHO+Tobacco+Free+global+award.html (accessed Feb 2, 2019).
- 59.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 69: 394–42. [DOI] [PubMed] [Google Scholar]
- 60.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019; 144: 1941–53. [DOI] [PubMed] [Google Scholar]
- 61.International Agency for Research on Cancer. Global Cancer Observatory: cancer today population fact sheets. 2018. http://gco.iarc.fr/today/fact-sheets-populations (accessed Sep 17, 2018). [Google Scholar]
- 62.Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med 2016; 375: 614–17. [DOI] [PubMed] [Google Scholar]
- 63.WHO. Global Cancer Observatory: cancer tomorrow. 2018. https://gco.iarc.fr/tomorrow (accessed Nov 13, 2018).
- 64.Hernandez BY, Bordallo RA, Green MD, Haddock RL. Cancer in Guam and Hawaii: a comparison of two U.S. island populations. Cancer Epidemiol 2017; 50: 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.National Department of Health. National multisectoral strategic plan for the prevention and control of non-communicable diseases 2015–2020. Port Moresby: Ministry of Health, 2015. [Google Scholar]
- 66.Watters D, Niblett J. Guidelines for the treatment of cancer in Papua New Guinea. 3rd edn. Sydney NSW: MJA Books, 2007. [Google Scholar]
- 67.Howell J, Van Gemert C, Lemoine M, Thursz M, Hellard M. An overview of hepatitis B prevalence, prevention, and management in the Pacific Islands and Territories. J Gastroenterol Hepatol 2014; 29: 1854–66. [DOI] [PubMed] [Google Scholar]
- 68.Patel MK, Wannemuehler K, Tairi R, et al. Progress towards achieving hepatitis B control in the Cook Islands, Niue, Tokelau, and Kiribati. Vaccine 2016; 34: 4298–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Breakwell L, Anga J, Dadari I, Sadr-Azodi N, Ogaoga D, Patel M. Evaluation of storing hepatitis B vaccine outside the cold chain in the Solomon Islands: Identifying opportunities and barriers to implementation. Vaccine 2017; 35: 2770–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Li X, Heffelfinger J, Wiesen E, et al. Improving hepatitis B birth dose coverage through village health volunteer training and pregnant women education. Vaccine 2017; 35: 4396–401. [DOI] [PubMed] [Google Scholar]
- 71.Obel J, McKenzie J, Buenconsejo-Lum LE, et al. Mapping HPV vaccination and cervical cancer screening practice in the Pacific region-strengthening national and regional cervical cancer prevention. Asia Pac J Cancer Prev 2015; 16: 3435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Direction De La Santé. Stratégie polynésienne de lutte contre le cancer. Polynésie française: Ministre des solidarités et de la santé, 2017. [Google Scholar]
- 73.Paulino YC, Hurwitz EL, Warnakulasuriya S, et al. Screening for oral potentially malignant disorders among areca (betel) nut chewers in Guam and Saipan. BMC Oral Health 2014; 14: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Toliman P, Badman SG, Gabuzzi J, et al. Field evaluation of xpert HPV point-of-care test for detection of human papillomavirus infection by use of self-collected vaginal and clinician-collected cervical specimens. J Clin Microbiol 2016; 54: 1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Palafox NA, Given L, Hohman K, et al. Comprehensive cancer control planning in the Pacific: the Cancer Council of the Pacific Islands a multi-national regional coalition. Cancer Causes Control 2018; 29: 1287–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pacific Regional Central Cancer Registry. Cancer in the US Affiliated Pacific Islands 2007–2015. 2015. http://www.pihoa.org/fullsite/newsroom/wp-content/uploads/downloads/2015/06/PIJCancer-FactsFigures.pdf (accessed July 16, 2019).
- 77.Yip C-H, Cazap E, Anderson BO, et al. Breast cancer management in middle-resource countries (MRCs): consensus statement from the breast health global initiative. Breast 2011; 20: S12–19. [DOI] [PubMed] [Google Scholar]
- 78.Foliaki S, Best D, Akauola S, Cheng S, Borman B, Pearce N. Cancer incidence in four Pacific countries: Tonga, Fiji Islands, Cook Islands and Niue. Pacific Health Dialog 2011; 17: 21–32. [PubMed] [Google Scholar]
- 79.Jaynes B Improving diagnostic capability in the FSM through tele-pathology application. Kasekehlie Press (PahnPei), February 15, 2018. http://www.kpress.info/index.php?option=com_content&view=article&id=873:improving-diagnostic-capability-in-the-fsm-through-telepathology-application&catid=8&Itemid=103 (accessed Nov 13, 2018). [Google Scholar]
- 80.Nkengasong JN, Yao K, Onyebujoh P. Laboratory medicine in low-income and middle-income countries: progress and challenges. Lancet 2018; 391: 1873–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol 2015; 16: 1193–224. [DOI] [PubMed] [Google Scholar]
- 82.Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386: 569–624. [DOI] [PubMed] [Google Scholar]
- 83.Watters DA, Ewing H, McCaig E. Three phases of the Pacific Islands Project (1995–2010). ANZ J Surg 2012; 82: 318–24. [DOI] [PubMed] [Google Scholar]
- 84.Watters DA, McCaig E, Nagra S, Kevau I. Surgical training programmes in the South Pacific, Papua New Guinea and Timor Leste. Br J Surg 2019; 106: e53–61. [DOI] [PubMed] [Google Scholar]
- 85.Guest GD, McLeod E, Perry WRG, et al. Collecting data for global surgical indicators: a collaborative approach in the Pacific Region. BMJ Glob Health 2017; 2: e000376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Spence D, Dyer R, Andall-Brereton G, et al. Cancer control in the Caribbean island countries and territories: some progress but the journey continues. Lancet Oncol 2019; published online Aug 5. 10.1016/S1470-2045(19)30512-1. [DOI] [PubMed] [Google Scholar]
- 87.Huff-Rousselle M The logical underpinnings and benefits of pooled pharmaceutical procurement: a pragmatic role for our public institutions? Soc Sci Med 2012; 75: 1572–80. [DOI] [PubMed] [Google Scholar]
- 88.Barton MB, Jacob S, Shafiq J, et al. Estimating the demand for radiotherapy from the evidence: A review of changes from 2003 to 2012. Radiother Oncol 2014; 112: 140–44. [DOI] [PubMed] [Google Scholar]
- 89.Barton MB, Frommer M, Shafiq J. Role of radiotherapy in cancer control in low-income and middle-income countries. Lancet Oncol 2006; 7: 584–95. [DOI] [PubMed] [Google Scholar]
- 90.International Atomic Energy Agency. Planning national radiotherapy services: a practical tool. Vienna: International Atomic Energy Agency, 2010. [Google Scholar]
- 91.Healy B, van der Merwe D, Christaki K, Meghzifene A. Cobalt-60 machines and medical linear accelerators: competing technologies for external beam radiotherapy. Clin Oncol 2017; 29: 110–15. [DOI] [PubMed] [Google Scholar]
- 92.Kim E, Cho Y-M, Kwon S, Park K. Cost-benefit analysis of establishing and operating radiation oncology services in Fiji. Cancer Epidemiol 2017; 50: 247–56. [DOI] [PubMed] [Google Scholar]
- 93.Feain I, Court L, Palta J, Beddar S, Keall P. Innovations in radiotherapy technology. Clin Oncol 2017; 29: 120–28. [DOI] [PubMed] [Google Scholar]
- 94.Lynch T, Connor S, Clark D. Mapping levels of palliative care development: a global update. J Pain Symptom Manag 2013; 45: 1094–106. [DOI] [PubMed] [Google Scholar]
- 95.WHO. Global atlas of palliative care at the end of life. London: Worldwide Palliative Care Alliance, 2014. [Google Scholar]
- 96.Muirden N Palliative care in Papua New Guinea: report of the International Association of Hospice and Palliative Care Traveling Fellowship. J Pain Palliat Care Pharmacother 2003; 17: 191–200. [PubMed] [Google Scholar]
- 97.Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. Lancet 2018; 391: 1391–454. [DOI] [PubMed] [Google Scholar]
- 98.Duthey B, Scholten W. Adequacy of opioid analgesic consumption at country, global, and regional levels in 2010, its relationship with development level, and changes compared with 2006. J Pain Symptom Manage 2014; 47: 283–97. [DOI] [PubMed] [Google Scholar]
- 99.Spratt J. Death and development in the Pacific In: Development Policy Centre, editor. Devpolicy blog; 2014. http://www.devpolicy.org/death-and-development-in-the-pacific-20140505/?print=pdf (accessed Sept 9, 2018). [Google Scholar]
- 100.Goucke CR, Jackson T, Morriss W, Royle J. Essential pain management: an educational program for health care workers. World J Surg 2015; 39: 865–70. [DOI] [PubMed] [Google Scholar]
- 101.Mau Kōkua. USAPI palliative care curriculum. https://kokuamau.org/usapi-palliative-care-curriculum/ (accessed Oct 30, 2018).
- 102.Maskarinec GG, Yalmadau K, Maluchmai MR, Tun P, Yinnifel C, Hancock WT. Palliative care and traditional practices of death and dying in Wa’ab (Yap Proper) and in the Outer Islands of Yap. Hawaii Med J 2011; 70 (suppl 2): 27–30. [PMC free article] [PubMed] [Google Scholar]
- 103.Cook Islands Ministry of Health. Patient referral policy 2015. Rarotonga: Te Marae Ora, Ministry of Health, 2015. [Google Scholar]
- 104.Easterbrook-Smith S, Wichman V. Report of the Evaluation of the Cook Islands medical health specialists visits schemes. Wellington: New Zealand Ministry of Foreign Affairs and Trade, 2011. [Google Scholar]
- 105.Fusimalohi S, Irava W, Kim S, Pellny M. Mapping of OMR and VSMT in Pacific islands countries—a pathway for regional cooperation towards UHC. Suva, Fiji: Division of Pacific Technical Support, World Health Organization, 2019. [Google Scholar]
- 106.Ekeroma AJ, Biribo S, Herman J, Hill A, Kenealy T. Health research systems in six pacific island countries and territories. J Res Devel 2016; 4: 1–9. [Google Scholar]
- 107.WHO. Consultation on strengthening health research capacity in the pacific. Nadi: World Health Organization Western Pacific Region, 2007. [Google Scholar]
- 108.Vallely A, Betuela I, Greenhill A, et al. Papua New Guinea Institute of Medical Research: Scientific Report 2006–2011. 2012https://www.researchgate.net/publication/234014682_Papua_New_Guinea_Institute_of_Medical_Research_Scientific_Report_2006_-2011 (accessed March 15,2019).
- 109.Ekeroma AJ, Pollock T, Kenealy T, et al. Pacific Island publications in the reproductive health literature 2000–2011: with New Zealand as a reference. Aust NZ J Obstet Gynaecol 2013; 53: 197–202. [DOI] [PubMed] [Google Scholar]
- 110.Bissell K, Viney K, Brostrom R, et al. Building operational research capacity in the Pacific. Public Health Action 2014; 4 (suppl 1): S2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Brown University. Brown, Yale researchers launch unique lab in Samoa to study obesity epidemic. News from Brown; 2017. https://www.brown.edu/news/2017-11-10/samoa (accessed Jan 30, 2019). [Google Scholar]
- 112.Ekeroma A Collaboration as a tool for building research capacity in the Pacific Islands. Ann Human Biol 2018; 45: 295–96. [DOI] [PubMed] [Google Scholar]
- 113.Gyawali B Cancer drugs in LMICs: cheap but unaffordable. Oncotarget 2017; 8: 89425–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.World Bank. NCD roadmap report: a background document on preventing and controlling non-communicable disease in the Pacific. Washington, DC: World Bank Group, 2014. [Google Scholar]
- 115.Pacific MANA Coordination Team. Status of NCD policy and legislation in Pacific island countries and territories, 2018. http://www.forumsec.org/wp-content/uploads/2019/02/WP-9-Item7.2-Annex-MANA-Dashboard-Report-2018.pdf (accessed Aug 9, 2018).
- 116.WHO. Tackling NCDs: ‘best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: World Health Organization, 2017. [Google Scholar]
- 117.Rijnberg V, Hansen P, Ekeroma A, Stanton J-AL. Is cervical cancer screening cost-effective for Samoa? A cost-utility analysis based on a cohort Markov model. Pacific Journal Reproductive Health 2019; 1: 423–39. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.