Abstract
Introduction:
Individuals who feel discomfort about their HIV status could be reluctant to disclose to others their status; ultimately, these sentiments may lead to depression, social isolation and poor adherence to medication. This study seeks to examine the associations between discomfort with HIV status, hopelessness, and depression among adolescents in Uganda.
Methods:
We used baseline data from the Suubi+Adherence study, which recruited a total of 702 adolescents (ages 10–16 years) living with HIV in southwestern Uganda. Structural equation models were conducted separately among in-school adolescents and out-of-school adolescents to assess the hypothesized associations between discomfort level with HIV status and depressive symptoms and if this association was mediated by hopelessness.
Results:
Out-of-school adolescents had significantly higher depression scores compared with those in-school youth (M = 6.24 vs. M = 5.03, p < 0.001). Although high discomfort level with HIV status was significantly associated with higher depression scores among both in-school adolescents and out-of-school adolescent, this association among out-of-school adolescents (B = 0.49, 95%CI: 0.19, 0.79), was more substantial than for in-school adolescents (B = 0.10, 95%CI: 0.03, 0.17). Additionally, hopelessness was found to be a full mediator for this association among in-school adolescents and a partial mediator for out-of-school adolescents.
Discussion:
One’s discomfort with their HIV status and the extent to which they are hopeful about the future can contribute to the development of depressive symptoms. These factors need to be further considered in the development of assessments and interventions as they may be vital for the treatment of depression among adolescents living with HIV.
Keywords: depression, hopelessness, HIV, HIV status, adolescents, stigma
Introduction
Studies in Sub-Saharan Africa (SSA), including Uganda, have indicated that children from poverty-impacted and disadvantaged backgrounds are significantly affected by HIV and AIDS (Cohen, 2006; Pereznieto, Walker, Villar, & Alder, 2011; UNICEF, 2014). In Uganda, there were 7,500 new infections diagnosed in 2017 among children alone (UNAIDS, 2018). Of concern, HIV/AIDS is a highly stigmatized illness in Uganda; for instance, 25% of adult Ugandan men and women stated that they would not buy vegetables from a shopkeeper living with HIV (Chan et al., 2015).
The relationship between HIV status and depression has been well-documented (Kaharuza et al., 2006; Vreeman, McCoy, & Lee, 2017). However, there has been limited research on the protective factors that help to maintain the emotional and psychological well-being of HIV-positive adolescents in SSA. In response, this study seeks to extend the knowledge base by examining associations between discomfort with HIV status, depression, and hopelessness among adolescents in Uganda. Our study is guided by the Hidden Distress Model which emphasizes the idea that choosing not to disclose one’s HIV status due to fear of rejection, shame and discrimination can cause psychological distress (Steward et al., 2008). Specifically, we hypothesize that adolescents’ discomfort level with their HIV status may contribute to their potential experience of depressive symptoms, and that this relationship is mediated by feelings of hopelessness.
Methods
This paper utilized baseline data from the Suubi+Adherence study (Ssewamala et al., 2019). Participants included 702 adolescents ages 10–16 years, both in school and out of school, living with HIV in Uganda. Protocols were approved by Columbia University (Protocol AAAK3852), the Makerere University School of Public Health (Protocol 210) and the Uganda National Council for Science and Technology (Protocol SS 2969) Institutional Review Boards. All participants provided written assent and caregivers gave informed consent for their adolescents’ participation.
Measures
Outcome.
Depressive symptoms were assessed by the 14-item Children’s Depression Inventory (CDI) (Traube, Dukay, Kaaya, Reyes, & Mellins, 2010). Each CDI item has three response options that correspond to varying levels of depression symptomatology (Kovacs, 2014). The theoretical score ranged from 0–28, with higher scores indicating more depressive symptoms. There is no literature or “rule of thumb” on the specific cutoffs when one uses the 14-item scale, therefore, our team decided to use the mean as a cutoff. This scale has been used in Uganda (Kagotho, Bowen, Ssewamala, Vaughn, & Kirkbride, 2018).
Independent variable.
To measure our primary predictor of interest, in-school adolescents rated four scenarios on comfort level with talking about their HIV status to: 1) other adolescents in school, 2) close friends, 3) family members, and 4) a girlfriend/boyfriend on a 4-point Likert scale. Out-of-school adolescents did not respond to the first scenario. Higher scores indicate greater discomfort. The theoretical score ranged from 0–16 for in-school adolescents and 0–12 for out-of-school adolescents.
Mediator.
The 20-item Beck’s Hopelessness scale was used to assess the adolescents’ pessimistic outlook and negative expectations (Dozois & Covin, 2004). Higher scores represent more hopelessness. The theoretical score ranged from 20–40.
Covariates.
Sociodemographic variables considered include age, gender, primary caregiver type, and school enrollment, family assets, family cohesion, and self-concept.
Statistical analyses
Bivariate analyses were used to test for differences between in-school vs out-of-school adolescent characteristics using survey commands to adjust within-cluster correlation. Under the survey commands, we report Rao-Scott F-statistics (Rao & Scott, 1984) for categorical variables and adjusted Wald F-statistics (design-based F) for continuous variables. P-values were set a priori and considered statistically significant at <0.05 level.
SEM models were separately built for in-school vs out-of-school adolescents. In the mediation analysis, the direct effect (c’) is the effect of discomfort with HIV status on depressive symptoms in the absence of hopelessness as a mediator. The indirect effect (a×b) represented how much of the effect of discomfort with HIV status on depressive symptoms is due to mediated effects through hopelessness. Thus, the total effect (c) of discomfort with HIV status on depression is the sum of direct and indirect effects (c = c’ + a×b; Sobel, 1986). We used maximum likelihood estimation with robust (Huber-White) standard errors (MLR) to account for within-clinic correlation (White, 1980, Satorra & Bentler, 1988; Albert Satorra & Bentler, 1994). Statistical programs used were Mplus 8.3 (Muthen & Muthen, 1998–2017) and Stata SE. Version 15 (StataCorp, 2017)
Results
In total, 675 participants completed all CDI items and were included in analysis. Out-of-school adolescents had statistically significantly higher CDI (M = 6.24 vs. M = 5.03, p < 0.001) and Beck Hopelessness scores (M = 26.25 vs. M = 25.60, p < 0.045) compared with those in-school adolescents. In-school adolescents possessed more family assets than out-of-school adolescents (89.15% vs. 75.90%, p < 0.001)
SEM findings.
For in-school adolescents (Model 1, Figure 1), there was a statistically significant total effect of discomfort with HIV status on depressive symptoms. Each additional HIV status discomfort level unit was associated with a 0.10 point increase in depressive symptoms (B = 0.10, 95% CI: 0.03, 0.17). The indirect effect of HIV status discomfort level on depressive symptoms was statistically significant (B = 0.03, 95% CI: 0.004, 0.05), indicating that the HIV status discomfort level increased hopelessness which, in turn, was associated with more depressive symptoms. The direct effect of the HIV status discomfort level on depressive symptoms, however, was not statistically significant after controlling for the mediator (B = 0.07, 95% CI: −0.01, 0.14), indicating that hopelessness is a full mediator of the association between the HIV status discomfort level and depressive symptoms. The proportion of the total effect mediated by hopelessness is 26.47% (ab/c × 100%). The variation in the depressive symptoms explained by the HIV status discomfort level and the mediator together is 27.3% (R2 = 0.273).
Figure 1.
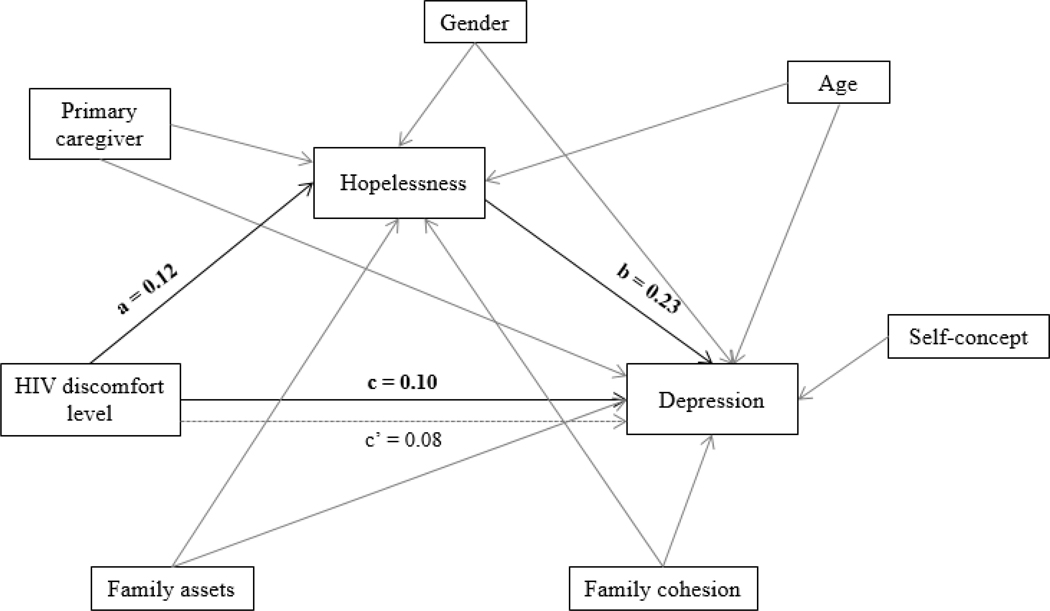
Structural equation model among adolescents enrolled in school
Note:
1. Marked bold are statistically significant unstandardized coefficient.
2. a = effect of the primary predictor on the mediator; b = effect of the mediator on the outcome; c’= the direct effect of the primary predictor on the outcome; c = the total effect of the primary predictor on the outcome.
3. The model adjusts for potential covariates: age, gender, no parents (the primary caregiver of the adolescent is not parent), family assets, and family cohesion.
4. Self-concept is a covariate only adjusted for the outcome but not for the mediator
5. This figure only presents the unstandardized coefficient for a, b, c’ and c path. All other unstandardized coefficients and standardized coefficient produced by the model are presented in the Table 2.
For out-of-school adolescents (Model 2, Figure 2), there was a statistically significant total effect of HIV status discomfort level on depressive symptoms and the effect size was stronger compared with in-school adolescents. Each additional HIV status discomfort level unit was associated with a 0.49 point increase in depressive symptoms (B = 0.49, 95%CI: 0.19, 0.79). The direct effect of the HIV status discomfort level on depressive symptoms was also statistically significant (B = 0.40, 95% CI: 0.18–0.62) but lower than the total effect. The indirect effect of the HIV status discomfort level on depressive symptoms, however, was not statistically significant (B = 0.08, 95% CI: −0.05, 0.22), indicating that hopelessness is a partial mediator for the association between the HIV status discomfort level and depressive symptoms. The proportion of the total effect mediated by hopelessness is 17.45% (ab/c × 100%). The variation in depressive symptoms explained by HIV status discomfort level and the mediator together is 31.9% (R2 = 0.319). Goodness of fit indices for the SEM were as follows: χ2 (20) = 1119.309, p < 0.001, Chi-Square contribution from each group: 120.85 for out-of-school adolescents, and 998.46 for in-school adolescents; CFI = 0.23; TLI = −0.85, RMSEA = 0.404, and SRMR = 0.18.
Figure 2.
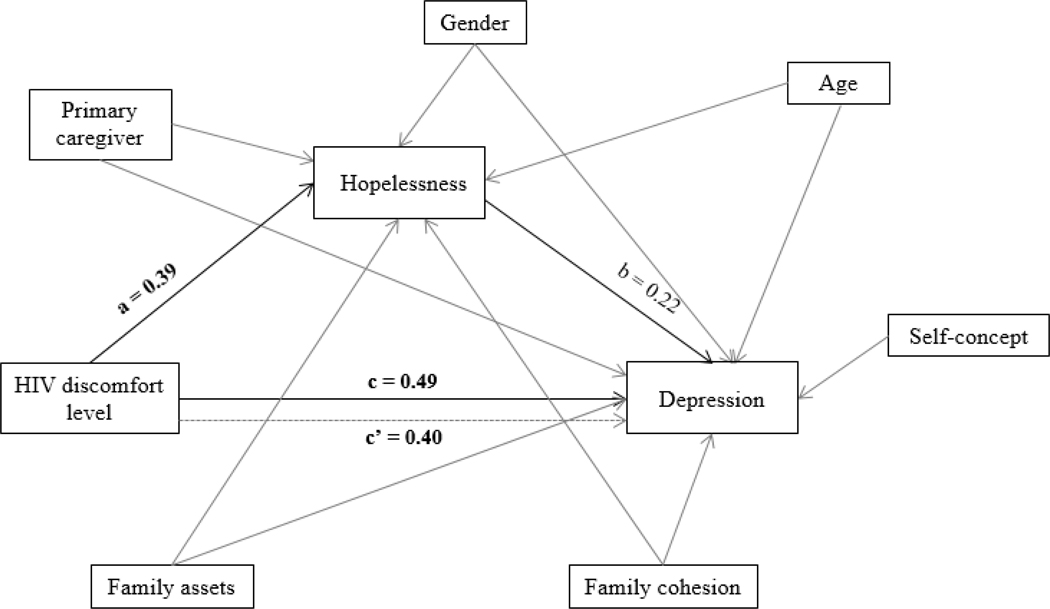
Structural equation model among adolescents who were not enrolled in school
Note:
1. Marked bold are statistically significant unstandardized coefficient.
2. a = effect of the primary predictor on the mediator; b = effect of the mediator on the outcome; c’= the direct effect of the primary predictor on the outcome; c = the total effect of the primary predictor on the outcome.
3. The model adjusts for potential covariates: age, gender, no parents (the primary caregiver of the adolescent is not parent), family assets, and family cohesion.
4. Self-concept is a covariate only adjusted for the outcome but not for the mediator
5. This figure only presents the unstandardized coefficient for a, b, c’ and c path. All other unstandardized coefficients and standardized coefficient produced by the model are presented in the Table 2.
Discussion
Our primary findings align with the Hidden Distress Model and signal a strong association between feelings of discomfort surrounding one’s HIV status and levels of depression among a particularly young, vulnerable, and ever-increasing subpopulation of the HIV/AIDS pandemic. In addition, adolescents’ discomfort with their HIV status and the extent to which they are hopeful about their future can impact subsequent depression. These are important issues to consider for adolescents in SSA living with HIV, especially for prevention and treatment of depression.
In-school adolescents reported less depression and hopelessness compared to out-of-school counterparts. This could be related to receiving social support and education about HIV within schools; both of which can reduce stigma and subsequent depression (Takada et al., 2014). Additionally, male adolescents, especially those younger in age, were more likely to report depressive symptoms compared to female adolescents. This surprising finding is counterintuitive to conventional mental health knowledge (Nolen-Hoeksema, 2001), but consistent with past SSA studies (Han, Ssewamala, & Wang, 2013; Ssewamala, Nabunya, Ilic, Mukasa, & Damulira, 2015).
Limitations include use of cross-sectional and self-report data and possible social desirability bias. Due to the young age of participants, HIV discomfort items asking about boyfriends/girlfriends could have the potential for information bias. Additionally, the small sample size of out-of-school adolescents may have reduced statistical power. Furthermore, goodness of fit indices for the SEM are limited and the models in this study were only able to capture a piece of the overall problem due to the complexity of mental health variables, illustrating the need for more comprehensive research into the mental health of this population.
Despite limitations, our findings have clinically relevant implications for targeting and tailoring interventions that address the mental health challenges of young people living with HIV. Specifically, this research helps to expand the understanding of the mechanism between hopelessness and depression among this population and highlight the importance of reducing social stigma and discrimination surrounding those who are HIV positive in SSA. Doing so can help minimize the discomfort and fear of status disclosure that HIV positive adolescents feel, and subsequently reduce feelings of hopelessness and depression.
Table 1.
Sample characteristics among the entire sample and by school enrollment (N=675)
| Total | Enrolled in school (n=592) | Did not enroll in school (n=83) | Design-based F | p | |
|---|---|---|---|---|---|
| n (%) or Mean [SD] | |||||
| Age | 65.26 | <0.001 | |||
| 10–13 | 467 (69.19) | 445 (75.17) | 22 (26.51) | ||
| 14–16 | 208 (30.81) | 147 (24.83) | 61 (73.49) | ||
| Gender | 0.034 | 0.855 | |||
| Male | 294 (43.56) | 257 (43.41) | 37 (44.58) | ||
| Female | 381 (56.44) | 335 (56.59) | 46 (55.42) | ||
| Primary caregiver | |||||
| Parent | 318 (47.11) | 294 (49.66) | 24 (28.92) | 7.17 | 0.002 |
| Grandparent | 198 (29.33) | 170 (28.72) | 28 (33.73) | ||
| Other relatives | 159 (23.56) | 128 (21.62) | 31 (37.35) | ||
| Family asset | 15.75 | <0.001 | |||
| High possession (7 or more reported assets) | 591 (87.56) | 528 (89.19) | 63 (75.90) | ||
| Low possession (6 or fewer reported assets) | 84 (12.44) | 64 (10.81) | 20 (24.10) | ||
| Family Cohesion Scale (reversed) | 16.28 (6.78) | 16.11 (6.76) | 17.48 (6.83) | 2.93 | 0.095 |
| Depression | 5.18 [3.76] | 5.03 [3.74] | 6.24 [3.74] | 11.88 | 0.001 |
| HIV status discomfort level | 12.04 [3.33] | 12.49 [3.16] | 8.86 [2.65] | -- | -- |
| Hopelessness | 25.68 [3.44] | 25.60 [3.46] | 26.25 [3.27] | 4.28 | 0.045 |
| Low self-concept | 36.32 [10.13] | 36.08 [10.03] | 38.02 [10.62] | -- | -- |
Table 2.
Structural equation model predicting depressive symptoms among adolescents currently enrolled in school and who did not enroll in school.
| Model 1: Enrolled in school (n = 592) | Model 2: Did not enroll in school (n = 83) | |||||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI | β | B | 95% CI | β | |||
| Depression on | ||||||||
| Hopelessness | 0.23 | 0.16 | 0.30 | 0.22 | 0.22 | 0.06 | 0.49 | 0.20 |
| Age a | 0.72 | 0.08 | 1.37 | 0.09 | 0.49 | –1.03 | 2.01 | 0.06 |
| Gender b | 0.73 | 0.28 | 1.18 | 0.10 | 0.88 | –0.24 | 2.01 | 0.12 |
| Primary caregiver c | 0.03 | –0.37 | 0.43 | 0.004 | –0.10 | –1.29 | 1.08 | –0.01 |
| Family assets d | 0.54 | –0.14 | 1.23 | 0.05 | –0.17 | –1.62 | 1.29 | –0.02 |
| Low family cohesion | 0.10 | 0.05 | 0.14 | 0.18 | 0.07 | –0.02 | 0.16 | 0.13 |
| Low self-concept | 0.10 | 0.07 | 0.12 | 0.26 | 0.10 | 0.03 | 0.17 | 0.29 |
| Hopelessness on | ||||||||
| HIV discomfort level | 0.12 | 0.04 | 0.20 | 0.11 | 0.39 | 0.14 | 0.64 | 0.31 |
| Age | 1.14 | 0.67 | 1.61 | 0.14 | 1.71 | 0.54 | 2.87 | 0.23 |
| Gender | 0.63 | 0.23 | 1.03 | 0.09 | 0.44 | –0.90 | 1.78 | 0.07 |
| Primary caregiver | 0.87 | 0.42 | 1.31 | 0.13 | 0.71 | –0.53 | 1.94 | 0.10 |
| Family assets | –0.22 | –0.89 | 0.46 | –0.02 | 0.29 | –1.06 | 1.65 | 0.04 |
| Low family cohesion | 0.12 | 0.09 | 0.15 | 0.24 | 0.01 | –0.08 | 0.09 | 0.01 |
| Intercepts | ||||||||
| Hopelessness | 20.65 | 19.47 | 21.83 | 5.98 | 21.48 | 18.55 | 24.42 | 6.57 |
| Depression | –7.70 | –9.07 | –6.34 | –2.11 | –8.48 | –14.61 | –2.34 | –2.32 |
| Residual variances | ||||||||
| Hopelessness | 10.53 | 9.68 | 11.38 | 0.88 | 9.15 | 7.27 | 11.03 | 0.86 |
| Depression | 9.90 | 9.01 | 10.78 | 0.74 | 9.70 | 7.49 | 11.91 | 0.72 |
| Direct effect | 0.07 | –0.01 | 0.14 | 0.07 | 0.40 | 0.18 | 0.62 | 0.29 |
| Indirect effect | 0.03 | 0.004 | 0.05 | 0.02 | 0.09 | –0.05 | 0.22 | 0.06 |
| Total effect | 0.10 | 0.03 | 0.17 | 0.09 | 0.49 | 0.19 | 0.79 | 0.35 |
| Proportion of total effect mediated | 26.47% | –- | –- | –- | 17.45% | –- | –- | –- |
Age: 10–13 vs. 14 −16 years old; reference group: 14 −16 years old
Gender: male vs. female; reference group: female
Primary caregiver: parents vs. other relatives; reference group: parents
Family assets: high possession vs. low possession; reference group: high possession
B: unstandardized regression coefficient; β : the standardized estimate
Marked bold are statistically significant unstandardized coefficient
Acknowledgments
Funding: Financial support for the Suubi + Adherence Study was provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Grant # R01HD074949 (PI: Fred M Ssewamala), National Institutes of Health (NIH), Grant #K02 DA043657 (PI: Patricia Cavazos-Rehg) and the National Institutes on Alcohol Abuse and Alcoholism (NIAAA), Grant # F32AA027941 (PI: Jacob Borodovsky). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health. We are grateful to the staff and the volunteer team at the International Center for Child Health and Development in Uganda for monitoring the study implementation process. Our special thanks go to all the children and their caregiving families who agreed to participate in the study.
Footnotes
Conflict of Interest Statement: JB is a member of the board of directors and treasurer of MySafeRx Inc., a non-profit scientific research organization. He receives no financial compensation from this organization.
References
- Bermudez LG, Jennings L, Ssewamala FM, Nabunya P, Mellins C, & McKay M (2016). Equity in adherence to antiretroviral therapy among economically vulnerable adolescents living with HIV in Uganda. AIDS Care, 28(sup2), 83–91. doi: 10.1080/09540121.2016.1176681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Weiser SD, Boum Y, Siedner MJ, Mocello AR, Haberer JE, . . . Tsai AC (2015). Persistent HIV-related stigma in rural Uganda during a period of increasing HIV incidence despite treatment expansion. AIDS (London, England), 29(1), 83–90. doi: 10.1097/QAD.0000000000000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D (2006). Poverty and HIV/AIDS in Sub-Saharan Africa Retrieved from https://www.undp.org/content/dam/aplaws/publication/en/publications/hiv-aids/poverty-and-hiv-aids-in-sub-saharan-africa/87.pdf
- Dozois DJ, & Covin R (2004). The Beck depression inventory-II (BDI-II), Beck hopelessness scale (BHS), and Beck scale for suicide ideation (BSS). Comprehensive handbook of psychological assessment, 2, 50–69. [Google Scholar]
- Fitts WH, & Warren WL (1996). Tennessee self-concept scale, TSCS 2 Manual (2nd ed.). Los Angeles: Western Psychological Services. [Google Scholar]
- Han C, Ssewamala F, & Wang J (2013). Family economic empowerment and mental health among AIDS-affected children living in AIDS-impacted communities: evidence from a randomised evaluation in southwestern Uganda. Journal of Epidemiology and Community Health, 67(3), 225. doi: 10.1136/jech-2012-201601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagotho N, Bowen NK, Ssewamala FM, Vaughn MG, & Kirkbride G (2018). Cross-national validity of the Beck Hopelessness Scale for children and adolescents: findings from the [Google Scholar]
- Kaharuza FM, Bunnell R, Moss S, Purcell DW, Bikaako-Kajura W, Wamai N, . . . Mermin J (2006). Depression and CD4 Cell Count Among Persons with HIV Infection in Uganda. AIDS and Behavior, 10(1), 105–111. doi: 10.1007/s10461-006-9142-2 [DOI] [PubMed] [Google Scholar]
- Kovacs M (2014). Children’s Depression Inventory (CDI and CDI 2) The Encyclopedia of Clinical Psychology. [Google Scholar]
- Moos R, & Moos B (1994). Family Environmental Scale Manual (3rd ed. Vol. 96). Palo Alto, CA: Consulting Psychologists Press Inc. [Google Scholar]
- Muthen L, & Muthen B (1998-2017). Mplus User’s Guide (Sixth Edition ed.). Loc Angeles, CA: Muthen & Muthen. [Google Scholar]
- Nanni MG, Caruso R, Mitchell AJ, Meggiolaro E, & Grassi L (2014). Depression in HIV Infected Patients: a Review. Current Psychiatry Reports, 17(1), 530. doi: 10.1007/s11920-014-0530-4 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (2001). Gender differences in depression. Current directions in psychological science, 10(5), 173–176. [Google Scholar]
- Pereznieto P, Walker D, Villar E, & Alder H (2011). Situation analysis of children and poverty in Uganda: Voices of children. Retrieved from https://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/7780.pdf [Google Scholar]
- Rao, & Scott. (1984). On chi-squared tests for multiway contingency tables with cell proportions estimated from survey data. Ann Stat, 12, 46–60. doi: 10.1214/aos/1176346391 [DOI] [Google Scholar]
- Satorra A, & Bentler P (1988). Scaling corrections for statistics in covariance structure analysis.: UCLA. [Google Scholar]
- Satorra A, & Bentler PM (1994). Corrections to test statistics and standard errors in covariance structure analysis Latent variables analysis: Applications for developmental research. (pp. 399–419). Thousand Oaks, CA, US: Sage Publications, Inc. [Google Scholar]
- Skinner HA, Steinhauer PD, & Santa-Barbara J (1983). The Family Assessment Measure. Canadian Journal of Community Mental Health, 2(2), 91–103. doi: 10.7870/cjcmh-1983-0018 [DOI] [Google Scholar]
- Sobel ME (1986). Some New Results on Indirect Effects and Their Standard Errors in Covariance Structure Models. Sociological Methodology, 16, 159–186. doi: 10.2307/270922 [DOI] [Google Scholar]
- Ssewamala FM, Byansi W, Bahar OS, Nabunya P, Neilands TB, Mellins C, . . . Nakigozi G (2019). Suubi+Adherence study protocol: A family economic empowerment intervention addressing HIV treatment adherence for perinatally infected adolescents. Contemporary Clinical Trials Communications, 16, 100463. doi: 10.1016/j.conctc.2019.100463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ssewamala FM, Nabunya P, Ilic V, Mukasa MN, & Damulira C (2015). Relationship Between Family Economic Resources, Psychosocial Well-being, and Educational Preferences of AIDS-Orphaned Children in Southern Uganda: Baseline Findings. Global Social Welfare, 2(2), 75–86. doi: 10.1007/s40609-015-0027-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata SE Statistical Software: Version 15. College Station, TX: StataCorp LP. [Google Scholar]
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, & Ekstrand ML (2008). HIV-related stigma: Adapting a theoretical framework for use in India. Social Science & Medicine, 67(8), 1225–1235. doi: 10.1016/j.socscimed.2008.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada S, Weiser SD, Kumbakumba E, Muzoora C, Martin JN, Hunt PW, . . . Tsai AC (2014). The Dynamic Relationship Between Social Support and HIV-Related Stigma in Rural Uganda. Annals of Behavioral Medicine, 48(1), 26–37. doi: 10.1007/s12160-013-9576-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traube D, Dukay V, Kaaya S, Reyes H, & Mellins C (2010). Cross-cultural adaptation of the Child Depression Inventory for use in Tanzania with children affected by HIV. Vulnerable Children and Youth Studies, 5(2), 174–187. doi: 10.1080/17450121003668343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2018). Uganda AIDS Country Progress Report July 2017-June 2018 Retrieved from https://www.unaids.org/sites/default/files/country/documents/UGA_2019_countryreport.pdf
- UNICEF. (2014). Situation Analysis of Child Poverty and Deprivation in Uganda. Retrieved from https://www.unicef.org/esaro/2014-UNICEF-Uganda-Child-Poverty-and-Deprivation.pdf
- Vreeman RC, McCoy BM, & Lee S (2017). Mental health challenges among adolescents living with HIV. Journal of the International AIDS Society, 20(S3), 21497. doi: 10.7448/IAS.20.4.21497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White H (1980). A Heteroskedasticity-Consistent Covariance Matrix Estimator and a Direct Test for Heteroskedasticity. Econometrica, 48(4), 817–838. doi: 10.2307/1912934 [DOI] [Google Scholar]


