Abstract
Co-administration of tobacco/nicotine and marijuana (e.g., using both products on the same occasion by mixing them in the same delivery device) is a risky, yet common form of co-use among young adults. Understanding motivations for co-administration co-use, and how these are associated with subsequent use and related problems, is needed to inform policy, prevention, and intervention efforts. We conducted a latent class analysis on 342 young adults with past year co-administration of tobacco/nicotine and marijuana to determine how emergent classes of 16 co-use motives were associated with use and co-administration co-use of tobacco/nicotine and marijuana one year later. Four classes emerged: (1) a high all class that reported high endorsement of all motives, (2) a high coping class that reported high endorsement of co-use due to coping with stress and bad moods, (3) a high social/physiological reinforcement class that reported low endorsement of coping but high probability of social and relaxation motives and motives to even out effects of each substance, and (4) a low all class that reported low endorsement of all motives. The high all and high coping classes reported greater frequency and quantity of single substance use and co-administration. The high coping class reported more marijuana consequences than the low all class. The high all and high coping classes reported younger age of initiation of each individual substance and co-administration. Considering co-use motives may be useful in identifying those at highest risk for future use and consequences and tailoring interventions to the distinct needs of co-use subgroups.
Keywords: tobacco, nicotine, cannabis, reasons, motives
Co-use of tobacco/nicotine and marijuana, where both substances are used within a specific time period or used together on the same occasion, is prevalent among young people (Goodwin et al., 2018; Schauer, Berg, Kegler, Donovan, & Windle, 2015; Schauer, Rosenberry, & Peters, 2017; Tucker et al., 2019b). Recent findings from 2,429 young adults based primarily in California reveal that over one-third reported use of both tobacco/nicotine and marijuana at some point in the past year (Tucker et al., 2019a). Specifically, over 80% who used tobacco in the past year also reported marijuana use during the same period, and nearly three quarters (72%) of youths who used marijuana in the past year also reported tobacco/nicotine use. Co-use of tobacco/nicotine and marijuana has been linked to a number of negative outcomes in both cross-sectional and longitudinal work, including greater frequency and heavier quantities of use of both drugs, poor grades, physical and mental health problems, and trouble with cessation efforts of either drug (Cobb, Soule, Rudy, Sutter, & Cohn, 2018; Moore & Budney, 2001; Peters et al., 2014; Ramo, Liu, & Prochaska, 2012; Strong et al., 2018; Tucker et al., 2019a; 2019b).
This literature can become confusing, however, as studies have not typically differentiated between types of co-use (with a few exceptions; e.g., (Hernández-Serrano, Font-Mayolas, & Gras, 2015; Tucker et al., 2019a)). Yet the type of co-use one engages in is important as it has implications for the extent of use and the riskiness associated with use. For example, in most studies, co-use refers to what is now commonly defined as concurrent use, which involves using both substances during a specified period, but only on separate occasions such that their effects do not overlap (e.g., smoking a joint on Tuesday and a cigarette on Saturday, but both occurred in the past month). Such use does not account for potentiation where effects of one substance used on an occasion enhance or attenuate the effects of the other (Kohut, 2017). Simultaneous or sequential use is defined as using both substances on the same occasion, one right after the other, but not mixing them together in the same delivery device (e.g., smoking a cigarette immediately after smoking a joint). A third type of co-use is co-administration, which involves using both substances at the same time, within the same device, such as smoking a spliff that contains both tobacco and marijuana. Understanding these differentiations is essential to understanding patterns, predictors, and consequences of co-use that can inform policies around the co-use of these two substances.
Research studies find that co-administration is among the most hazardous form of co-use, as individuals who engage in this type of co-use are at increased risk for heavier tobacco/nicotine and marijuana use, greater marijuana-related consequences and cannabis use disorder symptoms, greater delinquency, and poorer physical and mental health functioning compared to those who engage in concurrent co-use (Ream, Benoit, Johnson, & Dunlap, 2008; Tucker et al., 2019a). Typical forms of co-administration include bongs, bowls, hand pipes, blunts, and cigarettes that contain both tobacco and marijuana. The emergence of vaping products in recent years has led to novel methods of co-administration, such as electronic nicotine delivery systems (ENDS) that contain both nicotine e-liquid and a marijuana product such as hash oil, delta-9tetrahydrocannabinol (d-9-THC) wax, or dried buds. Concerns about the safety of ENDS has emerged in the media lately, given several deaths that have been linked to ENDS use, and in particular, the use of ENDS and other ‘vaping’ products to consume marijuana (Centers for Disease Control and Prevention, 2019). In addition, the co-administration of tobacco/nicotine and marijuana can lead to significantly increased amounts of inhaled THC, the psychoactive component of marijuana that creates the “high” from marijuana (Van der Kooy, Pomahacova, & Verpoorte, 2009). Importantly, the most prominent forms of co-administration involve inhalation of combustible products, such as smoking joints, blunts, and bongs that contain both drugs (Richardson, Pearson, Xiao, Stalgaitis, & Vallone, 2014; Schauer et al., 2016; Tucker et al., 2019a), and inhalation from smoke has been clearly linked to short- and long-term health problems (Meier & Hatsukami, 2016). Despite evidence of harms, the co-administration of tobacco/nicotine and marijuana is perceived by young people to be less harmful than use of either of these substances alone (Haines-Saah, Moffat, Jenkins, & Johnson, 2014).
International studies indicate that co-administration of tobacco/nicotine and marijuana is more prevalent in Europe than in the United States (Hazekamp, Ware, Muller-Vahl, Abrams, & Grotenhermen, 2013; Hindocha, Freeman, Ferris, Lynskey, & Winstock, 2016). However, rates of co-administration among young adults in the United States are high – for example, we found in a diverse sample of over 2,400 young adults around age 20 and 21 that 14% of the full sample engaged in past year co-administration (Tucker et al., 2019a). Given the prevalence and risks of co-administration, it is important to examine reasons, or motives, that young adults have for engaging in this form of substance use. A better understanding of motives for co-use can help to inform intervention and prevention efforts to reduce prevalence of co-use by youths and young adults. Moreover, recognizing the reasons why young people engage in co-use can help policymakers develop policies around co-use, such as those related to advertising products, requiring warning labels on devices, and establishing age restrictions on both tobacco/nicotine and marijuana in legalized states. Yet, only a handful of studies have begun to explore motives for co-use among young people, and although none have specifically examined motives among those who engage in co-administration, motives for co-use more generally likely relate to co-administration forms of use. In one qualitative study, 22 youths aged 15 to 21 reported combining tobacco/nicotine with marijuana (e.g., in joints, blunts) primarily because pure marijuana joints could be too strong, too expensive, or not able to burn correctly without the added tobacco (Akre, Michaud, Berchtold, & Suris, 2009). In another qualitative study of 77 youths aged 13 to 18, several individuals reported mixing tobacco and marijuana because combined use creates a head rush or “body buzz,” and it extended the amount of marijuana smoked in a joint, pipe, or bong when a limited amount of the drug was available (Haines-Saah et al., 2014). In a third qualitative study, young adults aged 18 to 34 reported the main reasons for co-administration of tobacco/nicotine and marijuana were to adjust the dose of either substance, save money, and modulate the high/flavor, such as to achieve a desired flavor or because nicotine enhances the high from marijuana ( Schauer et al., 2016). This latter reason is consistent with a study of 30 African American young adults aged 18 to 29, where participants reported using blunts (i.e., cigar wrappers that contain nicotine) to smoke marijuana to enhance the high of marijuana alone (Mead et al., 2018).
A recent two-phased study sought to create a measure of co-use motives among 18 to 25 year-olds who engaged in any form of co-use (Berg et al., 2018). Researchers conducted phone interviews with 46 young adults and found that the primary reasons for using both substances together were to enhance effects of the other (e.g., smoking a cigarette after a joint enhanced the effect of the marijuana) and due to social influences (e.g., using at a party but not when alone). They then queried 328 young adults and found that after controlling for tobacco use and marijuana use motives, co-use motives most strongly associated with substance use related to enhancing the drugs’ effects, experimentation, and social reasons. In another recent study of 182 adults (mean age of 34), higher scores on co-use motives to enhance the effects of either substance were associated with more frequent concurrent co-use of tobacco/nicotine and marijuana, greater number of cigarettes smoked per day, and greater nicotine dependence severity (Akbar, Tomko, Salazar, Squeglia, & McClure, 2019).
There are still important gaps to address in the emerging research on tobacco/nicotine and marijuana co-use motives. First, the co-use motives literature thus far has primarily been qualitative. Qualitative work is critically important at the initial stages of understanding co-use motives among young people; however, larger quantitative studies are needed to understand how these motives may influence the substance use behavior of young people over time. Second, the co-use motive research to date has not differentiated between types of co-use. As mentioned earlier, this differentiation is essential in that motives (and their potential effects on behavior) may differ for concurrent co-use, sequential co-use, and co-administration co-use. Third, many studies of co-use focus on combustible smoking methods, and although these methods are most common (e.g., Richardson et al., 2014; Schauer et al., 2016; Tucker et al., 2019a), the emergence of novel and unique ways to consume tobacco/nicotine and marijuana have made it important to ask participants about alternate product types and methods of use (Russell, Rueda, Room, Tyndall, & Fischer, 2018). Lastly, there are no studies that examine how co-use motives may be associated with substance use behavior over time. Such work is imperative to inform prevention, intervention, and policy efforts.
The present study overcomes limitations of prior work by examining co-use motives among a large sample of young adults who reported co-administration of tobacco/nicotine and marijuana in the past year, using a variety of forms and devices. We conducted latent class analyses to explore classes of co-use motives. We then examined if there were differences between these classes on demographics and age of substance initiation. Finally, we assessed substance use outcomes one year later across emergent classes to understand how these classes of co-use motives associated with subsequent use of each individual substance, consequences, and co-administration of tobacco/nicotine and marijuana. Alcohol outcomes (age of initiation, frequency, quantity, consequences) were also included as exploratory given the associations between alcohol use and tobacco/nicotine use among young adults (Bluestein et al., 2019; Cohn et al., 2015; Gubner et al., 2016).
Method
Participants and Procedures
Participants were initially recruited in grades 6th and 7th (ages 11 to 13) in 2008 for an alcohol and other drug prevention program, CHOICE, which was conducted in 16 middle schools in southern California (D’Amico et al., 2012). The large cohort study included 11 waves of surveys, first in classrooms during waves 1 to 5, and then completed online from waves 6 to 11. We have discussed the larger study in detail elsewhere, including participation and retention rates across survey waves (D’Amico, Tucker, Miles, Ewing, Shih, & Pedersen, 2016; Dunbar et al., 2018). In brief, parents gave consent for students until the participants turned 18 years old, at which point participants were reconsented. Retention rates across waves ranged from 61% to 92%, with 92% retention from wave 10 to 11 (i.e., the waves analyzed in this paper). If a participant did not complete a wave of data collection, they were still eligible to complete all subsequent waves. That is, they did not “dropout” of the study once they missed a survey wave; rather we fielded the full sample at every wave so that all participants had an opportunity to participate in each individual survey. Substance use at wave 10 did not significantly predict retention at wave 11, similar to previous waves (D’Amico et al., 2016; Dunbar et al., 2018); however, slightly more women (94%) then men (91%) were retained at wave 11, and those who were slightly younger at wave 10 were more likely to be retained (mean age of 20.6 retained versus mean age of 20.9 not retained). We did not find a significant difference in retention by race/ethnicity. The study has a Certificate of Confidentiality, and all procedures were approved by the local institutional review board.
For the current study, we utilized (a) wave 10 (Time 1) when participants were between the ages of 20 and 22 and (b) wave 11 (Time 2) when participants were between the ages of 21 and 23. Accounting for missingness and skip patterns of variables needed for analyses, our final analytic sample was N=342. That is, some individuals either did not have data due to missing the follow up assessment (i.e., attrition) or did not have data for specific measures due to preprogrammed skip patterns (i.e., individuals with no lifetime substance use would not answer questions on co-use motives). The analytic sample for this study consists of participants who reported co-administration of tobacco/nicotine and marijuana in the past year on the wave 10 survey. Co-administration was defined for participants as mixing tobacco/nicotine and marijuana in a number of different ways (e.g., a “spliff” that contains both tobacco and marijuana, or a vape pen that contains both nicotine e-liquid and marijuana) (Tucker et al., 2019a). We selected young adults who reported co-administration as the target group given their unique pattern of co-use, which varies considerably from other types of co-use where the two substances are not mixed within the same delivery device.
Measures
Demographics.
Participants responded to items regarding age, sex, race/ethnicity, mother’s education (i.e., a proxy for socioeconomic status), whether or not they were attending college part- or full-time, and sexual orientation.
Age of Initiation for Substances.
Participants were asked at what age they had first used tobacco/nicotine, marijuana, and co-use of both tobacco/nicotine and marijuana. Age at first use of tobacco/nicotine was assessed via seven different products (i.e., cigarette, e-cigarette, personal vaporizer, hand pipe, hookah, smokeless tobacco, and cigar/little cigars/cigarillos). It was specified that all products contained tobacco/nicotine only. We took the earliest age of use of any of these products as the age of tobacco/nicotine initiation. Age at first use of marijuana was assessed via eight different products (i.e., joint, blunt, hand pipe, bongs, dabs, edibles, e-cigarette filled with marijuana, personal vaporizer filled with marijuana). It was specified that all products assessed contained marijuana only. We again took the earliest age of use of any of these products as the age of marijuana initiation. Age of first co-use of tobacco/nicotine and marijuana (i.e., first co-administration use) was assessed via nine different products (i.e., cigarettes that contained both tobacco and marijuana; cigarettes dipped in hash oil; joints containing both tobacco and marijuana (spliff); blunts, bongs, hookahs, hand pipes/bowls, e-cigarettes, or personal vaporizers that contained both drugs; and any other way of using tobacco/nicotine and marijuana through the same delivery device). We took the earliest age when youths reported mixing any of these tobacco/nicotine and marijuana products as the age of co-administration initiation. We also assessed age of first “full drink of alcohol, such as a can of beer, glass of wine, wine cooler, or shot of liquor” and used the response from the item initiation of alcohol use.
Co-Use Motives at Time 1.
Based on a review of the co-use literature, review of literature on both tobacco/nicotine and marijuana motives, and discussions with co-use content experts, we created 16 items to assess motivations for co-use of tobacco/nicotine and marijuana (Akbar et al., 2019; Akre et al., 2009; Berg et al., 2018; Haines-Saah et al., 2014; Lee, Neighbors, & Woods, 2007; Schauer et al., 2016; Simons, Correia, & Carey, 2000). Items reflected motives related to social facilitation, experimentation, coping and relaxation, cutting down, peer pressure, and enhancement. Wording of individual items can be found in Figure 1. Respondents were asked: “Using the five-point scale from 1 = never to 5 = always, decide how frequently your own use of tobacco and marijuana at the same time is motivated by each of the reasons listed.” Response options were based on established scales of alcohol and marijuana use motives (Cooper, 1994; Lee et al., 2007). Reliability of the 16 items was adequate (α = 0.94).
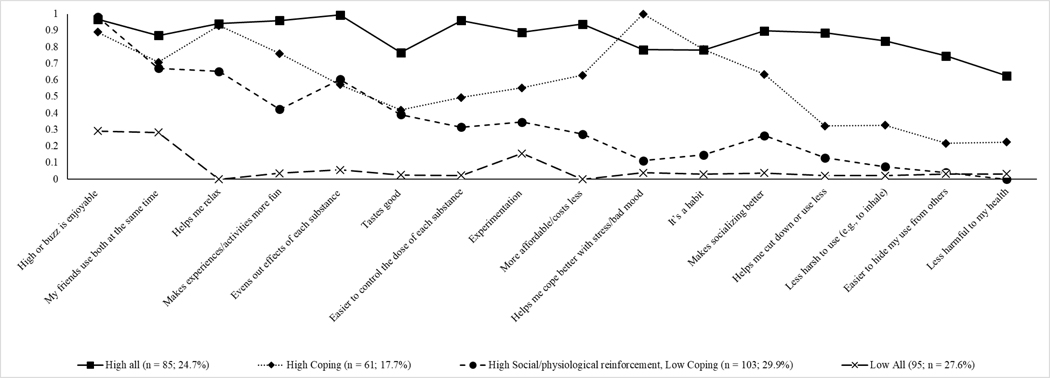
Figure 1. Item probability plot for final four class solution of co-use motives.
Note: Slight changes to wording in the figure were made for space. In the survey, “Makes experiences/activities more fun” was presented as “Makes experiences/activities more fun or interesting,” “Experimentation” was presented as “Experimentation (e.g., new experience, curiosity),” “Helps me cut down or use less” was presented as “Helps me cut down or use less of one or both substances” and “Easier to hide my use from others” was presented as “Easier to hide my use from others (use discretely).”
Substance Use Outcomes at Time 2.
Targeted substance use outcomes one year later were for tobacco/nicotine use, tobacco/nicotine dependence, marijuana use, consequences from marijuana use, and co-administration of both tobacco/nicotine and marijuana.
Tobacco/nicotine outcomes.
Frequency of cigarettes and e-cigarettes were assessed using items from Monitoring the Future asking how often participants had used each of these in the past year (1=none to 6=20 or more times). Quantity was assessed for both cigarette and e-cigarettes. For cigarettes, participants were first asked if they had ever used cigarettes in their lifetime. Those participants who reported using cigarettes at least once in their lifetime were then asked to indicate how many cigarettes they typically smoked on the days they smoked cigarettes, with response options ranging from “less than 1 cigarette a day” (re-coded to 0.5) to “20 or more cigarettes a day” (re-coded to 20). For e-cigarettes, participants were first asked about lifetime use and those who reported e-cigarette use in their lifetime were then similarly asked how many times per day they used their e-cigarette, assuming that one “time” consisted of around 15 puffs or lasting around 10 minutes. Those who reported never smoking cigarettes or never using e-cigarettes were assigned values of zero for quantity items.
Tobacco/nicotine dependence was assessed with two indicators of time to first cigarette and time to first e-cigarette (Baker et al., 2007). Both items asked participants to indicate how soon after waking they used their first cigarette/e-cigarette, with response options of “within 5 minutes (1),” “6–30 minutes (2),” “31–60 minutes (3),” and “after 60 minutes (4).” Lower values represent greater dependence.
Marijuana outcomes.
We assessed frequency of marijuana use using items from Monitoring the Future. First participants were asked about lifetime use. Participants who reported lifetime use were then asked how many times they had used marijuana in the past year (1=none to 6=20 or more times). Responses were recoded to reflect none (coded as 0) to more than 20 times (coded as 20); thus, the frequency of use items have a range of 0–20 that represents the number of times used in the past year. We asked about flower/bud as it is a predominant form of marijuana among young adults (Schauer, King, Bunnell, Promoff, & McAfee, 2016). For marijuana quantity, participants who reported past year use were first asked how many times they used marijuana on the days they used. Those who reported at least one time, reported “on a typical use day, how much marijuana flower/bud do you personally consume (don’t include amount you may have shared)?” (Kilmer et al., 2013). Response options ranged from 1=< 0.25 grams to 10=more than 5 grams. Prior to this item, participants were provided with pictures of 0.5 gram, 1.0 gram, and 3.5 grams (eighth ounce) of marijuana flower/bud (compared to the size of a bottle cap). Response options were recoded to reflect the mid-point number of grams to yield a continuous score ranging from 0.25–5.0 grams. Those who reported never using marijuana were given zero values for the quantity item.
Consequences from marijuana use were assessed with two measures. One of these was the 3-item Cannabis Use Disorder Identification Test Short-Form (CUDIT-SF; Bonn-Miller, Heinz, Smith, Bruno, & Adamson, 2016), which is an indicator of problem cannabis use. Participants who reported past month marijuana use rated how often during the past six months they found that they were not able to stop using marijuana/cannabis once they had started, devoted a great deal of their time to getting; using; or recovering from marijuana/cannabis, and had problems with their memory or concentration after using marijuana/cannabis. Items were rated on a scale from 0=never to 4=daily or almost daily and then summed to yield a continuous score (α = .75). The other consequence scale was a 10-item measure based on items from the RAND Adolescent/Young Adult Panel Study (Ellickson, D’Amico, Collins, & Klein, 2005) and the Marijuana Consequences Questionnaire (Simons, Dvorak, Merrill, & Read, 2012). Respondents were asked how many times various things had happened to them in the past year because of using marijuana (such as missing school, work, or other obligations; getting into trouble; doing something you later felt sorry for). Each item was rated from 1=none to 7=20 or more times, with responses to individual items summed to create a composite score (α = .92).
Co-administration co-use outcomes.
Co-administration co-use in the past year was assessed via 10 items: cigarettes that contained both tobacco and marijuana; cigarettes dipped in hash oil; joints containing both tobacco and marijuana (spliff); blunts, bongs, hookahs, hand pipes/bowls, e-cigarettes, or personal vaporizers that contained both drugs; and any other way of using tobacco/nicotine and marijuana through the same delivery device. Frequency of each of these types of co-administration was assessed separately on a scale from 0=0 times to 7=7 or more times. Note that these response options for co-use do not allow for direct comparison with the other substance use frequency outcomes. We created a single outcome for overall co-administration by calculating the mean response across the 10 items.
Exploratory alcohol outcomes.
We assessed both frequency and quantity of alcohol use using items from Monitoring the Future. Participants who reported lifetime use were then asked how many times they had used alcohol in the past year (1=none to 6=20 or more times); responses were coded to reflect none (coded as 0) to more than 20 times (coded as 20). Quantity was assessed with a single item for those who reported lifetime use, asking about typical number of drinks consumed per drinking occasion (“a few sips” [coded as 0.25]; “about ½ a drink” [coded as 0.5], and the remaining options of 1 to 15 drinks coded to represent the typical number of drinks consumed). Alcohol-related consequences were assessed with nine items (e.g., “You got into a fight or argument because of drinking alcohol,” “You passed out from drinking”) obtained from the Project ALERT Youth Survey (Tucker, Orlando, & Ellickson, 2003) and the Brief Young Adult Alcohol Consequences Questionnaire (Kahler, Strong, & Read, 2005). Each item was rated from 1=none to 7=20 or more times, with responses to individual items summed to create a composite score (α = .91).
Analytic Plan
We conducted a latent class analysis (LCA) using data from Time 1 on reports of tobacco/nicotine and marijuana co-use motives. We used the manual three-step approach (Nylund-Gibson, Grimm, Quirk, & Furlong, 2014) using Mplus version 8.0 (Muthén & Muthén, 2010) to extract classes. To determine the best fitting solution, we estimated separate models that fit one to six latent class solutions. To assess which model best fit the data, we considered several indicators including reductions in negative two log likelihood (−2LL), Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), and the sample size adjusted Bayesian Information Criteria (aBIC), as well as non-significant Lo-Mendell-Rubin adjusted likelihood ratio test (LMRT), and the bootstrapped likelihood ratio test (BLRT). The −2LL, AIC, BIC, and aBIC are all log likelihood measures for which lower values indicate better fit; non-significant LMRT and BLRT indicate a k-1 solution fit the data best (Nylund et al., 2007).
We first examined if there were differences between classes on demographics and age of substance initiation. We then assessed how aspects of various substance use outcomes and problems at Time 2 varied across emergent classes of co-use motives from Time 1. We used the manual three-step auxiliary BCH approach, which uses a pseudo-class Wald chi-square test, to assess mean differences between classes on outcomes. The BCH approach uses weights which reflect the measurement error of the latent class variable. This approach ensures that measurement of latent classes is not influenced by inclusion of covariates by fixing parameters of the latent classes. Using the manual BCH approach estimates weighted mean differences across distal outcomes and outputs all pairwise comparisons using a pseudo-class Wald chi square test. All models controlled for whether participants had received the CHOICE intervention a decade earlier in middle school as part of the parent study, as well as for factors that have been linked to heavier substance use in prior work: sex (female reference; Dario & O’Neal, 2018), race/ethnicity (non-Hispanic white reference; Kalof, 2000), age (centered on grand mean; Felson & Cundiff, 2014), and mother’s education (e.g., proxy for socio-economic status; Mellins et al., 2017). Across both waves of data, missing data never exceeded 10.1%. Mplus adjusts for missing data using a maximum likelihood estimator under the assumption that data are missing at random and uses all data that are available for each participant.
Results
Sample Description
Table 1 contains demographic information for participants, as well as means for outcomes. Participants (N = 342) were approximately 21 years old and less than half female (40%). The majority of participants were White (35%), Hispanic (32%), or Asian (16%). Most participants were currently enrolled in college (82%), had a mother who completed at least a high school education (91%), and reported straight sexual orientation (85%). Participants reported a mean age of 15.9 for initiation of both tobacco/nicotine and marijuana. They reported initiation of co-administration of these two substances about a year later at age 17.2.
Table 1.
Descriptive Characteristics of the Sample
| Variable | M(SD) or n% |
|---|---|
| Demographics at Time 1 | |
| Age | 20.7 (0.6) |
| Female n(%) | 135 (39.5%) |
| African-American n(%) | 11 (3.2%) |
| White n(%) | 121 (35.4%) |
| Multi-race/Other n(%) | 47 (13.7%) |
| Hispanic n(%) | 109 (31.9%) |
| Asian/Pacific Islander n(%) | 54 (15.8%) |
| Mother’s education – Did not finish high school n(%)a | 20 (5.9%) |
| Mother’s education – Finished high school or some college n(%)a | 87 (25.4%) |
| Mother’s education – Finished college or higher n(%)a | 225 (65.8%) |
| Currently attending college part- or full-time n(%) b | 280 (81.9%) |
| Straight sexual orientation n(%) | 289 (84.8%) |
| Age of initiation | |
| Age of marijuana initiation | 15.9 (2.1) |
| Age of tobacco/nicotine initiation | 15.9 (2.4) |
| Age of co-use initiation | 17.2 (2.2) |
| Marijuana Outcomes at Time 2 | |
| Frequency of marijuana use (past year) | 14.3 (7.9) |
| Quantity of marijuana use | 0.8 (1.0) |
| Marijuana consequences (past year) | 19.5 (11.2) |
| Cannabis use disorder screen | 2.6 (2.9) |
| Tobacco/nicotine Outcomes at Time 2 | |
| Frequency of cigarette use (past year) | 6.6 (7.8) |
| Quantity of cigarette use | 1.0 (2.5) |
| Frequency of e-cigarette use (past year) | 7.7 (8.7) |
| Quantity of e-cigarette use | 4.0 (8.5) |
| Cigarette dependence (time to first cigarette) | 3.6 (0.8) |
| E-cigarette dependence (time to first e-cigarette) | 3.0 (1.3) |
| Tobacco/nicotine and Marijuana Co-use Outcome at Time 2 | |
| Frequency of co-use (past year) | 0.7 (1.2) |
Note:
There were 10 participants (2.9%) who reported “Don’t Know” group for mother’s education
2 participants reported being currently enrolled in high school
Latent Class Analysis from Time 1 variables
We present model fit indices for the LCA up to six classes in Table 2. Based on model fit indices and substantive analysis of the plotted profiles, we chose the four-class solution. Figure 1 presents the item probability plot of endorsing co-use motive items. Each of the four classes are described below.
Table 2.
Model Fit Statistics for Latent Class Analysis at Time 1
| Model | −2 Log-likelihood | AIC | BIC | aBIC | Entropy | VLRT | p-value | LMRT | p-value | BLRT | p-value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 class | 7058.682 | 7090.682 | 7152.133 | 7101.377 | |||||||
| 2 class | 5411.07 | 5477.071 | 5603.812 | 5499.127 | 0.915 | 1647.612 | 0.00 | 1631.183 | 0.00 | 1647.612 | 0.00 |
| 3 class | 5069.34 | 5169.339 | 5361.371 | 5202.758 | 0.895 | 341.732 | 0.01 | 338.324 | 0.01 | 341.732 | 0.00 |
| 4 class | 4964.97 | 5098.971 | 5356.294 | 5143.753 | 0.901 | 104.368 | 0.01 | 103.328 | 0.01 | 104.368 | 0.00 |
| 5 class | 4904.968 | 5072.968 | 5395.582 | 5129.113 | 0.856 | 60.003 | 0.69 | 59.404 | 0.69 | 60.003 | 0.00 |
| 6 class | 4852.056 | 5054.056 | 5441.96 | 5121.562 | 0.88 | 52.913 | 0.11 | 52.385 | 0.12 | 52.913 | 0.00 |
Note. AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; aBIC = Sample size-adjusted BIC; BLRT = Parametric Bootstrapped Likelihood Ratio Test; LMRT = Lo-Mendell-Rubin Likelihood Ratio Test. The −2LL, AIC, BIC, and aBIC are all log likelihood measures for which lower values indicate better fit. Non-significant LMRT and BLRT indicate a k-1 solution fit the data best.
Class 1: High endorsement of all motives (“high all”).
This class represented 24.7% (n = 85) of the sample. Participants in this class had high endorsement of all co-use motive items which ranged in endorsement from 0.62 (“less harmful to my health”) to 0.99 (“evens out the effects of each substance”).
Class 2: High endorsement of coping motives (“high coping”).
This class represented 17.7% (n = 61) of the sample. Participants in this class had the highest endorsement of “coping with stress/bad mood” (probability 1.00), using because it’s a habit (0.79 probability), and makes socializing better (0.64 probability). They had relatively low endorsement of items related to health or cutting down on use, and relatively moderate endorsement of items associated with social reasons for co-use.
Class 3: High endorsement of social and physiological reinforcement motives and low endorsement of coping motives (“high social/physiological reinforcement”).
Individuals in this class represented the largest proportion of the sample (29.9%; n = 103). In general, these individuals had the highest probability of endorsing social (e.g., “my friends use both at the same time” [probability 0.67]), relaxation (e.g., “helps me relax” [probability 0.65], and instrumentality (e.g., “evens out effects of each substance” [probability 0.61]) items, and relatively low endorsement surrounding coping or health related items (e.g., “coping with stress/bad mood” [probability 0.11]).
Class 4: Low endorsement of all motives (“low all”).
This class represented 27.6% (n = 95) of the sample. Participants in this class had the lowest endorsement of all co-use motive items, with a range from 0.00 (“more affordable/costs less”) to 0.29 (“high or buzz is enjoyable”).
Demographics and Age of Initiation at Time 1
Demographics.
There were no significant differences in age, gender, race/ethnicity, mother’s education, or sexual orientation across classes. Using an indicator of whether participants were currently enrolled in college or not, there were overall differences across classes, X2 (3, N = 342) = 8.26, p = 0.041, with differences between the high all class (Class 1; 71.3% in college) and the high social/physiological reinforcement class (Class 3; 88.6% in college; X2 = 8.08, p = 0.004), and the low all class (Class 4; 84.0% in college; X2 = 3.95, p = 0.047).
Age of Initiation.
There were significant differences between classes for age of initiation for all three substance categories (tobacco/nicotine, marijuana, co-administration of tobacco/nicotine and marijuana). For initiation of tobacco/nicotine, there were overall differences across classes, X2 (3, N = 342) = 8.66, p = 0.034, with the high coping class (Class 2) reporting a lower age of initiation (age of 15.3) than the high social/physiological reinforcement class (Class 3; age of 16.2; X2 = 4.01, p = 0.045) and the low all class (Class 4; age of 16.3; X2 = 3.91, p = 0.048). The high all class (Class 1; age of 15.5) reported a lower age of initiation for tobacco/nicotine than the high social/physiological reinforcement class (Class 3; X2 = 4.29, p = 0.038).
For initiation of marijuana, there were overall differences across classes, X2 (3, N = 342) = 10.89, p = 0.012, with the high coping class (Class 2) reporting a lower age of initiation (age of 15.3) than the high social/physiological reinforcement class (Class 3; age of 16.1; X2 = 4.86, p = 0.028) and the low all class (Class 4; age of 16.3; X2 = 7.10, p = 0.008). The high all class (Class 1; age of 15.5) reported a lower age of marijuana initiation than the low all class (Class 4; X2 = 4.97, p = 0.026).
For initiation of co-administration of tobacco/nicotine and marijuana, there were overall differences across classes, X2 (3, N = 342) = 18.26, p < 0.001, with the high all class (Class 1) reporting a lower age of initiation (age of 16.6) than the high social/physiological reinforcement class (Class 3; age of 17.4; X2 = 6.97, p = 0.008) and the low all class (Class 4; age of 17.9; X2 = 11.98, p = 0.001). The high coping class (Class 2) also reported a lower age of initiation (age of 16.6) than the high social/physiological reinforcement class (Class 3; age of 17.4; X2 = 4.92, p = 0.027) and the low all class (Class 4; age of 17.9; X2 = 9.26, p = 0.002).
For the exploratory analysis of age of alcohol initiation, no differences occurred across emergent classes. The mean age of alcohol initiation for all participants was 15.39 (SD = 2.35).
Substance Use Outcomes at Time 2
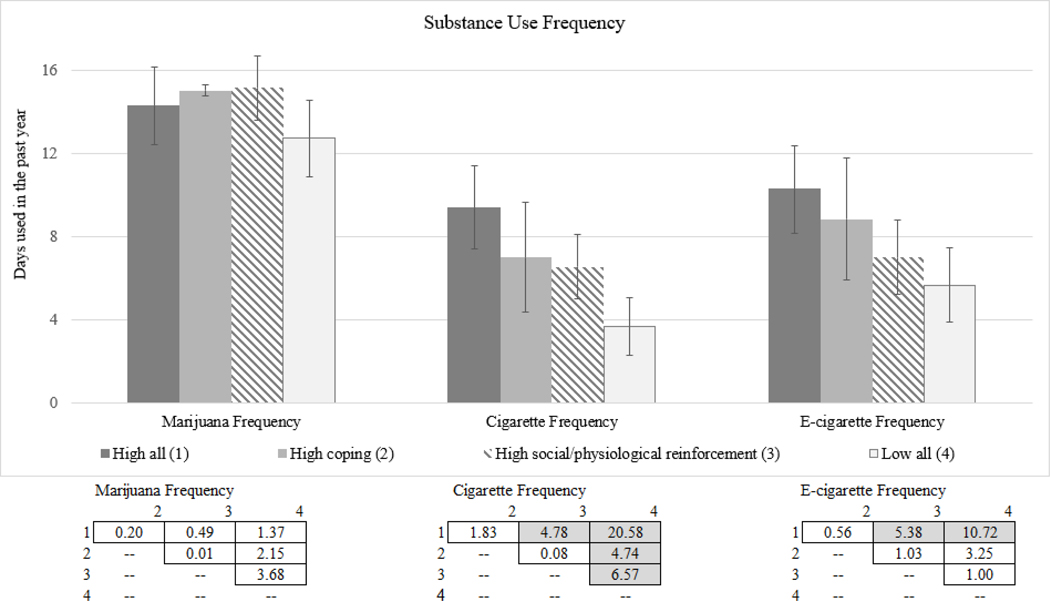
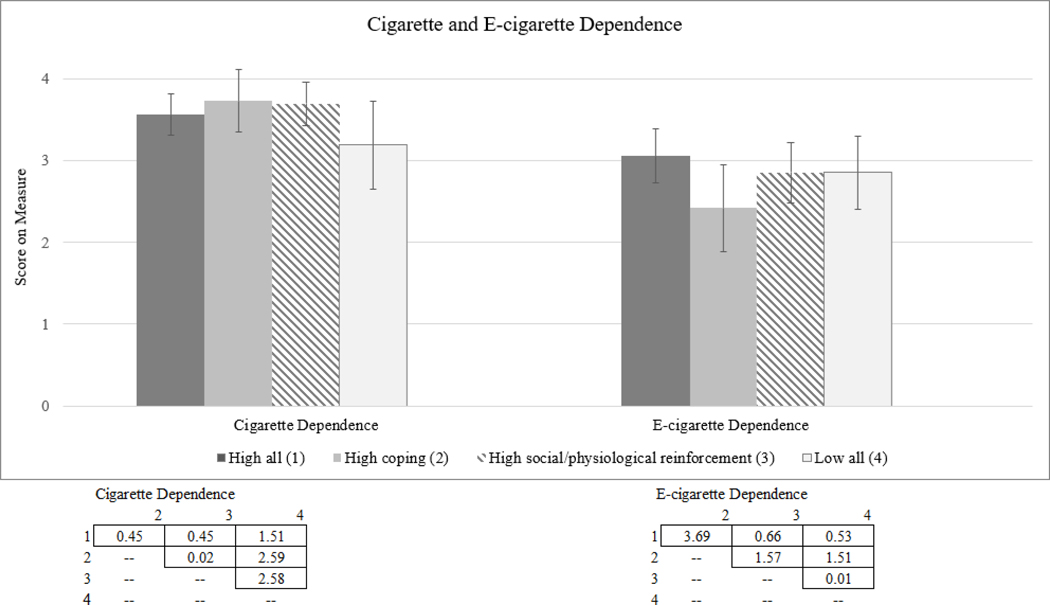
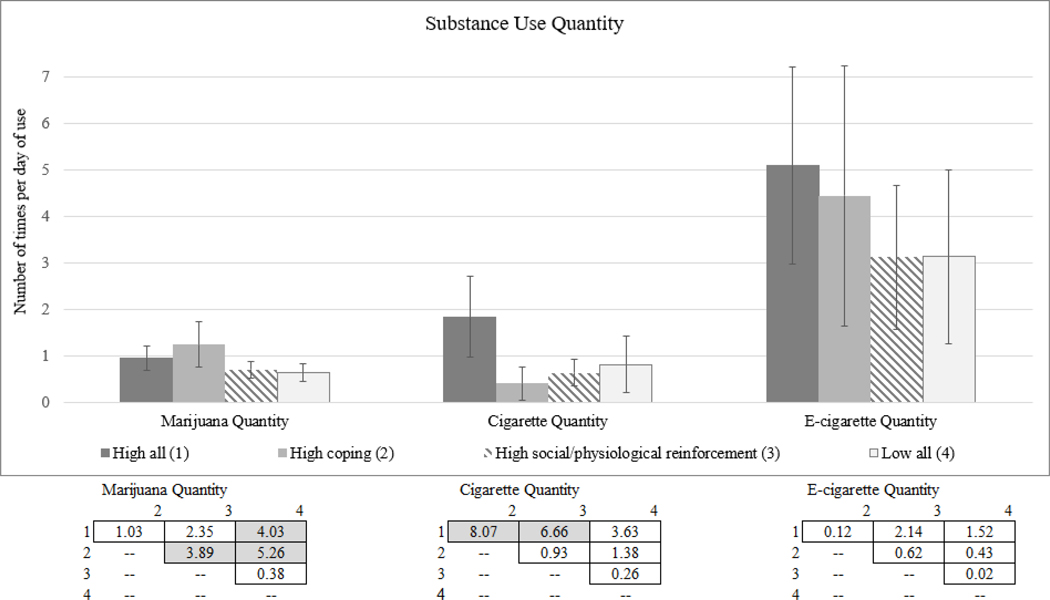
We next assessed how emergent classes of co-use motives were related to substance use and problems one year later. Because of the large number of comparisons across classes, we plotted means and confidence intervals of each outcome by class membership and a table to denote significant differences between classes (see Figures 2 through Figure 6). Figure 2 contains frequency outcomes for marijuana, tobacco, and e-cigarettes. Figure 3 presents results for quantity of marijuana, tobacco, and e-cigarettes. Figure 4 contains the marijuana consequence outcome. Figure 5 contains the CUD outcome and frequency for co-administration co-use in the past year for tobacco/nicotine and marijuana. Lastly, Figure 6 contains cigarette and e-cigarette dependence outcomes.
Figure 2. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for Substance Use Frequency at Time 2.
Note. Figure vertical bars represent mean values on the past year frequency measure for each substance and by the indicated groups. Values in boxes indicate chi-square values between indicated groups (e.g., chi-square difference between class 1 and class 2 for marijuana frequency is 0.20). Shaded values are significant at p < .05.
Figure 6. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for Cigarette and E-cigarette Dependence at Time 2.
Note. Figure vertical bars represent mean value scores for the cigarette and e-cigarette dependence measure by the indicated groups. Values in boxes indicate chi-square values between indicated groups. There were no significant differences between groups at p < .05.
Figure 3. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for Substance Use Quantity at Time 2.
Note. Figure vertical bars represent mean values on the past year quantity measure for each substance and by the indicated groups. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05.
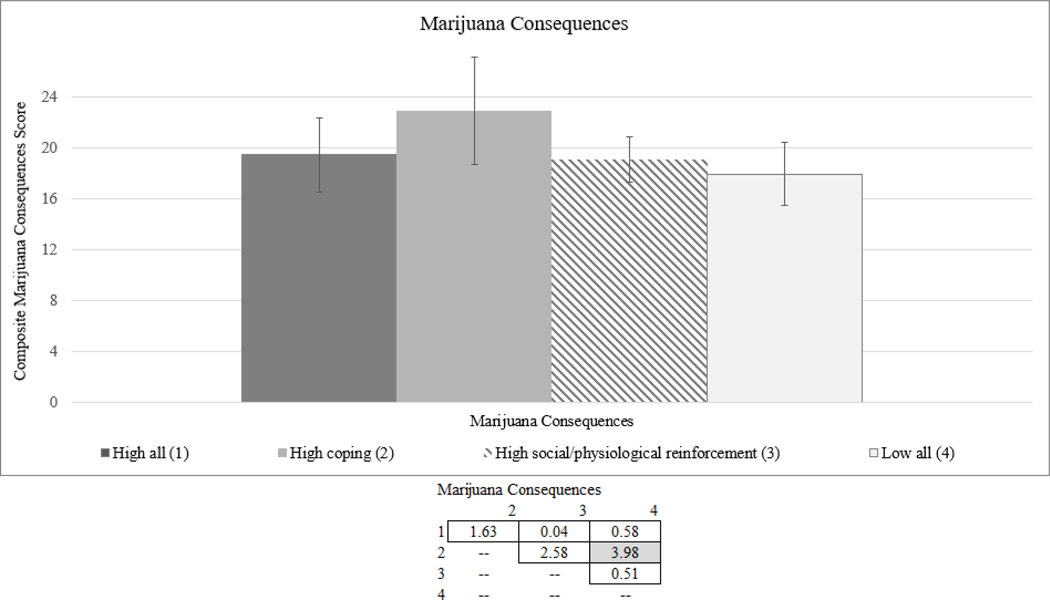
Figure 4. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for Marijuana Consequences at Time 2.
Note. Figure vertical bars represent mean values on the marijuana consequences measures by the indicated groups. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05.
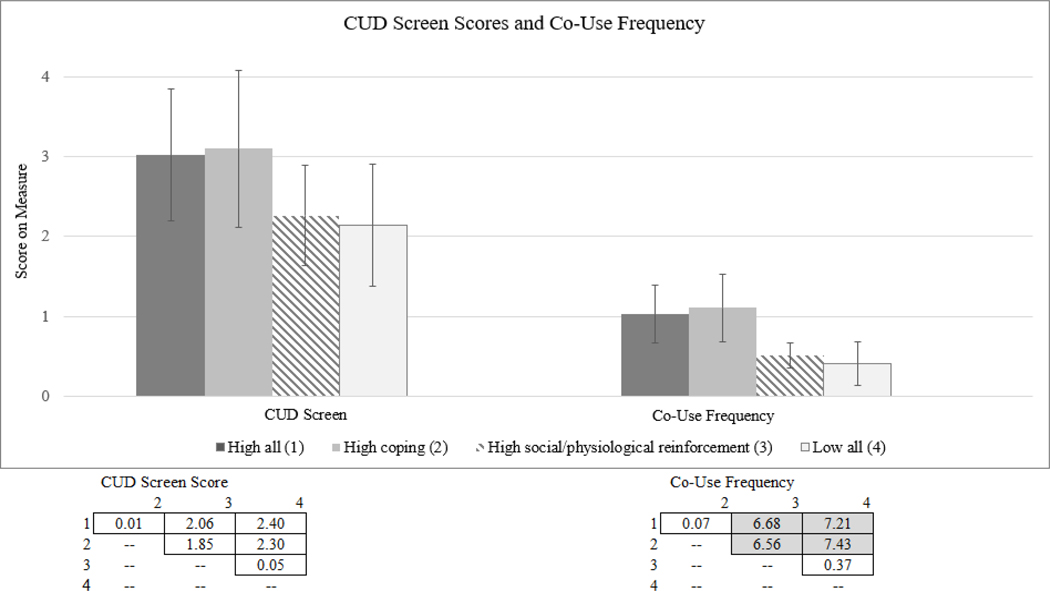
Figure 5. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for CUDIT Scores and Co-Use Frequency at Time 2.
Note. CUD = Cannabis Use Disorder. CUDIT = Cannabis Use Disorder Identification Test, Figure vertical bars represent mean value scores for the CUDIT and the co-use frequency measure by the indicated groups. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05.
Frequency, quantity, and dependence of tobacco/nicotine use.
In terms of frequency of combustible cigarette smoking, we found that the low all class (Class 4) reported less frequent cigarette use than the other three classes. Further, individuals in the high all class (Class 1) reported more frequent cigarette use compared to the high social/physiological class (Class 3).
Only one difference emerged for quantity of cigarette use, with individuals in the high all class (Class 1) reporting greater quantity of cigarette use than individuals in the high social/physiological class (Class 3). For e-cigarette use, individuals in the high all class (Class 1) reported higher frequency of e-cigarette use than youths in the high social/psychological (Class 3) and low all (Class 4) classes. However, no class differences were found for quantity of e-cigarette use. There were also no significant differences between classes on tobacco/nicotine dependence, as specified by time to first cigarette or e-cigarette outcomes.
Frequency, quantity, and consequences of marijuana use.
There were no significant differences between classes in terms of past year marijuana use frequency or CUD screen scores. However, individuals in the high coping class (Class 2) reported greater quantity of marijuana use than the high social/physiological class (Class 3). Individuals in both the high all (Class 1) and high coping classes reported greater quantity of marijuana use than the low all class (Class 4). We also found that individuals in the high coping class (Class 2) reported significantly more marijuana consequences compared to individuals in the low all class (Class 4).
Frequency of co-administration of tobacco/nicotine and marijuana.
Individuals in the high all (Class 1) and high coping (Class 2) classes reported more frequent co-administration co-use than individuals in the high social/physiological (Class 3) and low all (Class 4) classes.
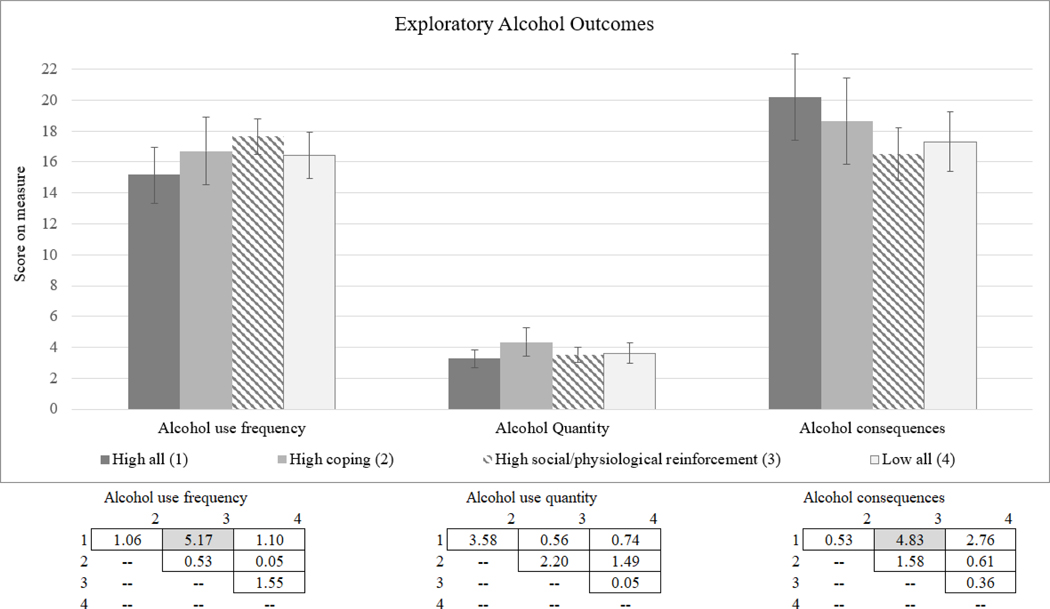
Frequency and quantity of alcohol use.
For exploratory alcohol outcomes, there were few significant differences across classes for alcohol use (see Appendix). The only difference that emerged for alcohol use frequency and quantity was that individuals in the high social/physiological class (Class 3) reported significantly higher past year alcohol frequency than individuals in the high all class (Class 1). For alcohol consequences, only one difference emerged, with individuals in the high all (Class 1) reporting a greater number of alcohol consequences compared to individuals in the high social/physiological (Class 3).
Discussion
This study represents the first examination of motives for co-use of tobacco/nicotine and marijuana by young adults aged 19 to 22 using two time points spanning a year between assessments. In a sample of 342 young adults who reported past year co-administration of these substances, we found four emergent classes of co-use motives, with classes defined by high endorsement of all motives, high endorsement of coping motives, high endorsement of social/physiological reinforcement motives, and low endorsement of all motives. We found no significant differences between classes on demographics, with the exception of current college enrollment, where those in the high all class were less likely to be enrolled in college than those in the low all class or those who primarily used for social/physiological reinforcement. Results also highlighted a generally lower age of initiation of tobacco/nicotine, marijuana, and co-use of these substances for those in the high all class and those who used primarily for coping motives.
Findings indicated important differences between these classes in terms of subsequent substance use and related problems one year later. In general, young adults who endorsed high levels of all motives, or primarily coping-related motives at Time 1, generally reported more frequent and heavier use of tobacco/nicotine and marijuana at Time 2, whereas those with low endorsement across motives reported less frequent and less heavy use. For frequency of use, those who endorsed primarily coping motives or were high on all motives reported more frequent past year tobacco/nicotine use, as well as more frequent co-administration of tobacco/nicotine with marijuana one year later compared to young adults who primarily endorsed social/physiological reinforcement motives or reported low levels of all motives. Those who endorsed high levels of all motives also reported more frequent e-cigarette use than those who primarily endorsed social/physiological reinforcement motives or reported low levels of all motives. For quantity of use, young adults who endorsed high levels of all motives at Time 1 reported a greater quantity of marijuana use than those who reported low levels of all motives one year later, as well as greater quantity of cigarette use than those who primarily endorsed high coping or high social/physiological reinforcement motives. Further, young adults who primarily endorsed coping motives reported greater quantities of marijuana use than those who primarily endorsed social/physiological motives or reported low levels of all motives. Few differences were found for marijuana problems or cannabis dependence, with only the high coping class reporting greater marijuana consequences than the low all class and no differences between classes on CUD screens. There were no significant findings across classes for tobacco/nicotine dependence. There were also very limited findings for the exploratory alcohol outcomes of frequency, quantity, and consequences. It is important to note that the study only included a one-year follow-up. Future longitudinal research spanning longer time periods is critical for understanding whether and how co-use motives may influence trajectories of use and outcomes over the long term.
Findings have implications for prevention and intervention efforts with young adults who co-administer tobacco/nicotine and marijuana. Specifically, two co-use motive classes (high coping and high all) emerged as being at high risk for heavier and more frequent substance use one year later. First, both classes reported earlier age of initiation of tobacco/nicotine, marijuana, and co-administration of tobacco/nicotine and marijuana, and much research has shown that earlier age of substance initiation predicts heavier use, consequences, and substance use disorders in young adulthood (Buchmann et al., 2013; Dawson et al., 2008; King & Chassin, 2007; Rioux et al., 2018). The high coping class had higher risk for subsequent heavier and more frequent use for both substances and co-administration of these substances. Interestingly, co-use motives focused on coping (e.g., helps me cope better with stress/bad mood) have not been examined in prior co-use motive work (e.g., Akbar et al., 2019; Berg et al., 2018). However, research has shown that young people who use marijuana alone to cope with negative affect are at risk for greater marijuana use and negative outcomes over time (Blevins, Banes, Stephens, Walker, & Roffman, 2016; Lee, Neighbors, Hendershot, & Grossbard, 2009; Lee et al., 2007) and young people who use tobacco (e.g., cigarettes) alone to cope with negative affect are also at risk for concurrent tobacco use and associated negative outcomes (McEwen, West, & McRobbie, 2008; Piko, Varga, & Wills, 2015; Wong, Haardorfer, Windle, & Berg, 2017). We found that coping-related motives for co-use mirror findings for single-drug motives, which highlights the importance of prevention and intervention efforts continuing to focus on helping young adults find alternate ways of managing stress and negative affect.
The high all class included young adults who did not have a specific set of reasons for co-use, but endorsed most reasons at relatively high levels. These individuals may be physically or psychologically dependent on one or both substance(s), given their particularly strong endorsement of motives related to enjoying the high, evening out the effects of each of the substances, ease of controlling dose (e.g., smoking a spliff to limit the amount of marijuana consumed), and desire to control costs. Thus, prevention and intervention efforts may need to focus on young adults who report high levels of co-use, independent of their specific motives for use, as these individuals may use whenever or for whatever reason, which could make efforts targeting specific motives less effective than for other classes of co-use. State-level and national policy efforts are also underway to curtail underage use of tobacco/nicotine and to place restrictions on purchasing particular vaping products that have recently been linked to lung injuries.
A strength of this study is the inclusion of alternate forms of consuming nicotine; mainly, the use of ENDS. Though commonly promoted as a tool for smokers to transition off of combustible cigarettes (Collins, Glasser, Abudayyeh, Pearson, & Villanti, 2018), multiple studies show that use of ENDS is a risk factor for subsequent initiation and escalation of cigarette smoking in adolescents and young adults (Berry et al., 2019; Dai, Catley, Richter, Goggin, & Ellerbeck, 2018; Dunbar et al., 2019; National Academies of Sciences & Medicine, 2018; Soneji et al., 2017). ENDS are also used to consume forms of marijuana (e.g., cannabis oil) (Morean, Kong, Camenga, Cavallo, & Krishnan-Sarin, 2015). ENDS and other ‘vaping’ products have come under recent government attention in relation to an outbreak of potentially fatal severe lung injury cases (1,479 lung injury cases and 33 deaths as of October 2019) that have been linked to use of these products, and use of THC products are believed to “play a major role in the outbreak” (Centers for Disease Control and Prevention, 2019). Interestingly, motives related to perceived reduced harmfulness to health (e.g., using ENDS to vape nicotine e-juice and cannabis oil instead of inhaling a combustible spliff) and ease of hiding use (e.g., using a flavored ENDS device that limits the potent smell of or marijuana) were endorsed at relatively low levels in all groups. This indicates that even though vaping products are widely available to young people, and use of these devices to consume nicotine and/or marijuana has increased dramatically in recent years (Miech, Johnston, O’Malley, Bachman, & Patrick, 2019), young people may still prefer to consume marijuana and tobacco together in combustible formats (Richardson et al., 2014; Schauer et al., 2016; Tucker et al., 2019a). However, the product landscape and regulatory environment for both tobacco/nicotine and marijuana are rapidly evolving; for example, an increasing number of states are legalizing marijuana for recreational sale and possession, which dramatically expands access to a range of different product types for co-use consumption (Borodovsky, Crosier, Lee, Sargent, & Budney, 2016). As such, ongoing surveillance is needed to better understand emerging trends in product co-use, as well as motives for engaging in use and co-use of specific types of tobacco/nicotine and marijuana products.
Limitations should be noted. First, we did not use an established measure of tobacco/nicotine and marijuana co-use motives because at the time of our study there were no measures published (and since then there is only one published scale (Berg et al., 2018)), and no measures or qualitative discussion of items focused solely on the problematic co-administration form of co-use. Although our co-use motives items asked about use “at the same time,” participants could have considered sequential use in their responses, as we did not specify that the two substances needed to be used in the same delivery device (which is exclusive to co-administration). We also attempted to measure co-administration of tobacco/nicotine and marijuana with a wide array of products; however, the types of products are constantly evolving. For example, although such devices were not available or widely known yet in the United States when our survey was conducted, we did not include JUUL (Morean et al., 2019) or heated tobacco products (Auer, Concha-Lozano, Jacot-Sadowski, Cornuz, & Berthet, 2017) in our assessment of e-cigarette outcomes. In addition, we relied on retrospective self-report regarding age of initiation, which is subject to recall bias, especially since participants were remembering back an average of four to five years. We focused solely on co-administration use due to the potential for greater use and consequences with this type of co-use, but sequential use is also associated with problematic use and problems (Tucker et al., 2019a). Lastly, generalizability of results is limited by the use of a predominantly California sample.
Conclusions
Taken together, findings suggest that young adults’ motives for co-using tobacco/nicotine and marijuana predict future patterns of both single product use and co-use. There is particular concern for those young people who report high coping-related co-use motives, as such individuals may be co-using tobacco/nicotine and marijuana as a strategy to cope with stress, mental health problems, or other emotional difficulties. A more in depth examination of how these co-use motives relate to mental health could inform the development of prevention and intervention programs focused on helping individuals learn alternative ways of coping. There is also concern for youths who report high endorsement of all co-use motives, which could make these individuals difficult to target with intervention and prevention efforts given that they do not have specific reasons for use. Efforts may need to focus on other aspects to motivate youths to reduce or discontinue co-use, such as increasing resistance self-efficacy to limit use in high-risk situations or targeting social influences of co-use such as correcting misperceived peer norms. Such efforts would need to be evaluated in further work that includes co-use motives in models to determine if such motives are modifiable, and if so, whether reductions in strength of specific co-use motives are associated with changes in patterns of use.
Acknowledgments
Funding Source: Work on this article was supported by funds from the California Tobacco-Related Disease Research Grants Program of the University of California, Grant Number 26IR-0011 (PI: Joan Tucker) and by three grants from the National Institute of Alcohol Abuse and Alcoholism (R01AA016577; R01AA020883; R01AA025848; PI: Elizabeth D’Amico). The authors wish to thank Kirsten Becker and Jennifer Parker for overseeing the data collection.
Appendix: Exploratory Alcohol Outcomes
Figure. Means, Confidence Intervals, and Chi-Square Values by Time 1 Class for Alcohol Outcomes at Time 2.
Note. Figure vertical bars represent mean value scores for the alcohol use frequency and quantity measures by the indicated groups. Values in boxes indicate chi-square values between indicated groups. Shaded values are significant at p < .05.
References
- Akbar SA, Tomko RL, Salazar CA, Squeglia LM, & McClure EA (2019). Tobacco and cannabis co-use and interrelatedness among adults. Addictive Behaviors, 90, 354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akre C, Michaud P-A, Berchtold A, & Suris J-C (2009). Cannabis and tobacco use: where are the boundaries? A qualitative study on cannabis consumption modes among adolescents. Health Education Research, 25(1), 74–82. [DOI] [PubMed] [Google Scholar]
- Auer R, Concha-Lozano N, Jacot-Sadowski I, Cornuz J, & Berthet A. (2017). Heat-Not-Burn tobacco cigarettes: Smoke by any other name. JAMA Internal Medicine, 177(7), 1050–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, et al. (2007). Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine & Tobacco Research, 9 (Suppl 4), S555–S570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Payne J, Henriksen L, Cavazos-Rehg P, Getachew B, Schauer GL, & Haardörfer R. (2018). Reasons for marijuana and tobacco co-use among young adults: A mixed methods scale development study. Substance Use and Misuse, 53(3), 357–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry KM, Fetterman JL, Benjamin EJ, Bhatnagar A, Barrington-Trimis JL, Leventhal AM, & Stokes A. (2019). Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in US youths. JAMA Network Open, 2(2), e187794-e187794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CE, Banes KE, Stephens RS, Walker DD, & Roffman RA (2016). Motives for marijuana use among heavy-using high school students: An analysis of structure and utility of the Comprehensive Marijuana Motives Questionnaire. Addictive Behaviors, 57, 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluestein M, Kelder S, Perry CL, & Pérez A. (2019). Exploring associations between the use of alcohol and marijuana with e-cigarette use in a USA nationally representative sample of young adults. International Journal of Health Sciences, 13(1), 30. [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Heinz AJ, Smith EV, Bruno R, & Adamson S. (2016). Preliminary development of a brief cannabis use disorder screening tool: The Cannabis Use Disorder Identification Test Short-Form. Cannabis and Cannabinoid Research, 1(1), 252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Crosier BS, Lee DC, Sargent JD, & Budney AJ (2016). Smoking, vaping, eating: Is legalization impacting the way people use cannabis? International Journal of Drug Policy, 36, 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann AF, Blomeyer D, Jennen C, Schmidt MH, Esser G, Banaschewski T, & Laucht M. J. A. b. (2013). Early smoking onset may promise initial pleasurable sensations and later addiction. 18(6), 947–954. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Outbreak of Lung Injury Associated with E-Cigarette Use, or Vaping. Atlanta, GA: Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion. Retrieved October 21, 2019 and archived at https://web.archive.org/web/20191021030452/https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. [Google Scholar]
- Cobb CO, Soule EK, Rudy AK, Sutter ME, & Cohn AM (2018). Patterns and correlates of tobacco and cannabis co-use by tobacco product type: Findings from the Virginia Youth Survey. Substance Use and Misuse, 53(14), 2310–2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, & Mermelstein R. (2015). The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addictive Behaviors, 48, 79–88. [DOI] [PubMed] [Google Scholar]
- Collins L, Glasser AM, Abudayyeh H, Pearson JL, & Villanti AC (2018). E-Cigarette marketing and communication: How e-cigarette companies market e-cigarettes and the public engages with e-cigarette information. Nicotine & Tobacco Research, 21(1), 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6(2), 117–128. [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Zhou AJ, Shih RA, & Green HD Jr. (2012). Preventing alcohol use with a voluntary after school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prevention Science, 13(4), 415–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, & Pedersen ER (2016). Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17. Addiction, 111, 1825–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, & Ellerbeck EFJP (2018). Electronic cigarettes and future marijuana use: a longitudinal study. 141(5), e20173787. [DOI] [PubMed] [Google Scholar]
- Dario LM, & O’Neal EN (2018). Do the mental health consequences of sexual victimization differ between males and females? A general strain theory approach. Women & Criminal Justice, 28(1), 19–42. [Google Scholar]
- Dawson DA, Goldstein RB, Patricia Chou S, June Ruan W, Grant BFJAC, & Research E. (2008). Age at first drink and the first incidence of adult onset DSM IV alcohol use disorders. 32(12), 2149–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar MS, Davis JP, Rodriguez A, Tucker JS, Seelam R, & D’Amico EJ (2019). Disentangling within- and between-person effects of shared risk factors on e-cigarette and cigarette use trajectories from adolescence to young adulthood. Nicotine & Tobacco Research, 21(10), 1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar MS, Tucker JS, Ewing BA, Parast L, Pedersen ER, Rodriguez A, & D’Amico EJ (2018). Ethnic differences in cigarette use trajectories and health, psychosocial, and academic Outcomes. Journal of Adolescent Health, 62, 327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, D’Amico EJ, Collins RL, & Klein DJ (2005). Marijuana use and later problems: When frequency of recent use explains age of initiation effects (and when it does not). Substance Use and Misuse, 40(3), 343–359. [DOI] [PubMed] [Google Scholar]
- Felson RB, & Cundiff PR (2014). Sexual assault as a crime against young people. Archives of Sexual Behavior, 43(2), 273–284. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Pacek LR, Copeland J, Moeller SJ, Dierker L, Weinberger A, . . . Hasin D. S. J. A. j. o. p. h. (2018). Trends in daily cannabis use among cigarette smokers: United States, 2002–2014. 108(1), 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubner NR, Delucchi KL, & Ramo DE (2016). Associations between binge drinking frequency and tobacco use among young adults. Addictive Behaviors, 60, 191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines-Saah RJ, Moffat B, Jenkins EK, & Johnson JL (2014). The Influences of Health Beliefs and Identity on Adolescent Marijuana and Tobacco Co-Use. Qualitative Health Research, 24(7), 946–956. [DOI] [PubMed] [Google Scholar]
- Hazekamp A, Ware MA, Muller-Vahl KR, Abrams D, & Grotenhermen F. (2013). The medicinal use of cannabis and cannabinoids: An international cross-sectional survey on administration forms. Journal of Psychoactive Drugs, 45(3), 199–210. [DOI] [PubMed] [Google Scholar]
- Hernández-Serrano O, Font-Mayolas S, & Gras ME (2015). Polydrug use and its relationship with the familiar and social context amongst young college students. Addiction Biology, 27(3), 205–213. [PubMed] [Google Scholar]
- Hindocha C, Freeman TP, Ferris JA, Lynskey MT, & Winstock AR (2016). No smoke without tobacco: a global overview of cannabis and tobacco routes of administration and their association with intention to quit. Frontiers in Psychiatry, 7, 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, & Read JP (2005). Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research, 29(7), 1180–1189. [DOI] [PubMed] [Google Scholar]
- Kalof L. (2000). Ethnic differences in female sexual victimization. Sexuality and Culture, 4(4), 75–98. [Google Scholar]
- Kilmer B, Caulkins J, Midgette G, Dahlkemper L, MacCoun R, & Pacula RL (2013). Before the grand opening: Measuring Washington State’s marijuana market in the last year before legalized commercial sales. Santa Monica, CA: RAND Corporation. Available at https://www.rand.org/pubs/research_reports/RR466.html. [Google Scholar]
- King KM, & Chassin L. (2007). A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. Journal of Studies on Alcohol and Drugs, 68(2), 256–265. [DOI] [PubMed] [Google Scholar]
- Kohut SJ (2017). Interactions between nicotine and drugs of abuse: a review of preclinical findings. The American Journal of Drug and Alcohol Abuse, 43(2), 155–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, & Grossbard JR (2009). Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs, 70(2), 279–287. doi: 10.15288/jsad.2009.70.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, & Woods BA (2007). Marijuana motives: young adults’ reasons for using marijuana. Addictive Behaviors, 32(7), 1384–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen A, West R, & McRobbie H. (2008). Motives for smoking and their correlates in clients attending Stop Smoking treatment services. Nicotine and Tobacco Research, 10(5), 843–850. [DOI] [PubMed] [Google Scholar]
- Mead EL, Johnson SL, Siddiqui J, Butler J 3rd, Kirchner T, & Feldman RH (2018). Beyond blunts: Reasons for cigarette and cigar use among African American young adult dual users. Addiction research & theory, 26(5), 349–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier E, & Hatsukami DK (2016). A review of the additive health risk of cannabis and tobacco co-use. Drug and Alcohol Dependence, 166, 6–12. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Walsh K, Sarvet AL, Wall M, Gilbert L, Santelli JS, et al. (2017). Sexual assault incidents among college undergraduates: Prevalence and factors associated with risk. PloS One, 12(11), e0186471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Johnston L, O’Malley PM, Bachman JG, & Patrick ME (2019). Adolescent vaping and nicotine use in 2017–2018—US national estimates. New England Journal of Medicine, 380(2), 192–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BA, & Budney AJ (2001). Tobacco smoking in marijuana-dependent outpatients. Journal of Substance Abuse, 13(4), 583–596. [DOI] [PubMed] [Google Scholar]
- Morean ME, Bold KW, Kong G, Gueorguieva R, Camenga D, Simon P, et al. (2019). Adolescents’ awareness of the nicotine strength and e-cigarette status of JUUL e-cigarettes. Drug and Alcohol Dependence, 204, 107512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, & Krishnan-Sarin S. (2015). High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics, 136(4), 611–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus: Statistical analysis with latent variables: User’s guide: Muthén & Muthén Los Angeles. [Google Scholar]
- National Academies of Sciences, E., & Medicine. (2018). Public health consequences of e-cigarettes: National Academies Press. [PubMed] [Google Scholar]
- Nylund-Gibson K, Grimm R, Quirk M, & Furlong M. (2014). A latent transition mixture model using the three-step specification. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 439–454. [Google Scholar]
- Peters EN, Schwartz RP, Wang S, O’Grady KE, Blanco CJD, & dependence, a. (2014). Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence. 134, 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piko BF, Varga S, & Wills TA (2015). A study of motives for tobacco and alcohol use among high school students in Hungary. Journal of Community Health, 40(4), 744–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Liu H, & Prochaska JJ (2012). Tobacco and marijuana use among adolescents and young adults: A systematic review of their co-use. Clinical Psychology Review, 32(2), 105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ream GL, Benoit E, Johnson BD, & Dunlap E. (2008). Smoking tobacco along with marijuana increases symptoms of cannabis dependence. Drug and Alcohol Dependence, 95(3), 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson A, Pearson J, Xiao H, Stalgaitis C, & Vallone D. (2014). Prevalence, harm perceptions, and reasons for using noncombustible tobacco products among current and former smokers. American Journal of Public Health, 104(8), 1437–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rioux C, Castellanos-Ryan N, Parent S, Vitaro F, Tremblay RE, & Seguin JR (2018). Age of cannabis use onset and adult drug abuse symptoms: a prospective study of common risk factors and indirect effects. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 63(7), 457–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell C, Rueda S, Room R, Tyndall M, & Fischer B. (2018). Routes of administration for cannabis use–basic prevalence and related health outcomes: A scoping review and synthesis. International Journal of Drug Policy, 52, 87–96. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, & Windle M. (2015). Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addictive Behaviors, 49, 26–32. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Hall CD, Berg CJ, Donovan DM, Windle M, & Kegler MC (2016). Differences in the relationship of marijuana and tobacco by frequency of use: A qualitative study with adults aged 18–34 years. Psychology of Addictive Behaviors, 30(3), 406–414. [DOI] [PubMed] [Google Scholar]
- Schauer GL, King BA, Bunnell RE, Promoff G, & McAfee TA (2016). Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. American Journal of Preventive Medicine, 50(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, & Peters EN (2017). Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addictive Behaviors, 64, 200–211. [DOI] [PubMed] [Google Scholar]
- Simons J, Correia CJ, & Carey KB (2000). A comparison of motives for marijuana and alcohol use among experienced users. Addictive Behaviors, 25(1), 153–160. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Merrill JE, & Read JP (2012). Dimensions and severity of marijuana consequences: Development and validation of the Marijuana Consequences Questionnaire (MACQ). Addictive Behaviors, 37(5), 613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. (2017). Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: A systematic review and meta-analysis. JAMA Pediatrics, 171(8), 788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Myers MG, Pulvers K, Noble M, Brikmanis K, & Doran N. (2018). Marijuana use among US tobacco users: Findings from wave 1 of the population assessment of tobacco health (PATH) study. Drug and Alcohol Dependence, 186, 16–22. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Orlando M, & Ellickson PL (2003). Patterns and correlates of binge drinking trajectories from early adolescence to young adulthood. Health Psychology, 22(1), 79. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Pedersen ER, Seelam R, Dunbar MS, Shih RA, & D’Amico EJ (2019a). Types of cannabis and tobacco/nicotine co-use and associated outcomes in young adulthood. Psychology of Addictive Behaviors, 33(4), 401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Rodriguez A, Dunbar MS, Pedersen ER, Davis JP, Shih RA, & D’Amico EJ (2019b). Cannabis and tobacco use and co-use: Trajectories and correlates from early adolescence to emerging adulthood. Drug and Alcohol Dependence, 204, 107499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Kooy F, Pomahacova B, & Verpoorte R. (2009). Cannabis smoke condensate II: influence of tobacco on tetrahydrocannabinol levels. Inhalation Toxicology, 21(2), 87–90. [DOI] [PubMed] [Google Scholar]
- Wong EC, Haardorfer R, Windle M, & Berg CJ (2017). Distinct motives for use among polytobacco versus cigarette only users and among single tobacco product users. Nicotine and Tobacco Research, 20(1), 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]