Abstract
Background:
Frontline healthcare workers (FHCWs) are at an increased risk of contracting COVID-19. We aimed to assess the stress and psychological impact of the COVID-19 pandemic among FHCWs.
Methods:
This was an exploratory hospital-based study. A semistructured e-questionnaire was developed and shared through emails, WhatsApp groups, Facebook, and Twitter. The study instruments used were stress questionnaire and the impact of event scale—revised.
Results:
We received 133 valid responses. A total of 81 (61.4%) of the respondents were single, 74 (55.6) were male, 70 (52.6%) were between 20 and 29 years of age, and 91 (68.4%) were from urban background. A total of 83 (62.4%) of respondents were doctors and 28 (21.1%) were registered nurses. A total of 36 (27.1%) were posted in emergency and 34 (25.6%) were in the in-patient department. Feeling sad and pessimistic, feeling of being avoided by others, the burden of change in the quality of work, and worrying whether the family will be cared for in their absence were significantly more in nurses as compared to the doctors. Stress due to burden in an increase in the quantity of work was seen more in FHCWs working in the swab collection center as compared to those working in the in-patient department, emergency, or theaters. Severe psychological impact was seen in 81 (60.9%) of FHCWs. The psychological impact was significantly more in males and in those who were married. It was also significantly related to the place of posting.
Conclusion:
More than half of the FHCWs had a severe psychological impact owing to COVID-19. The psychological impact was more in males and those who were married, and it was related to the place of posting of the FHCWs. Nurses had significantly higher stress as compared to doctors.
Keywords: COVID-19 pandemic, front line health care worker, stress, psychological impact
Key Messages:
Compared to prior pandemics, our results reveal a higher degree of psychological impact and stress in FHCWs in the backdrop of COVID-19. Compared to doctors, stress was more in nurses. Severe psychological impact was more in married males working in COVID clinic and swab collection center.
On December 31, 2019, China announced a group of cases of atypical community-acquired pneumonia of unknown etiology in vendors and dealers linked with seafood in the wholesale market of Wuhan, Hubei Province.1 On January 7, 2020, health authorities of China declared that this group of patients was associated with a 2019 novel coronavirus (2019-nCoV).2 Within three months, the virus had affected more than 118,000 people, caused 4,291 deaths, and spread to 114 countries. On January 30, 2020, the World Health Organization (WHO) declared COVID-19 outbreak a global pandemic and public health emergency of international concern.3
This virus is known to be transmitted through droplet infection by mildly ill or presymptomatic infected persons, which poses the greatest challenge to control, as compared to the Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) pandemics.4 The WHO reported the mortality rate in COVID-19 to be 3%–4%; however, it appeared that the mortality statistics were underreported.5, 6 Since the advent of its first case in Kashmir,7 every passing day, the government authorities and media kept on reporting an escalation in cases, as a result of which public anxieties were on the rise.8 This pandemic not only has a high case fatality rate but has also led to psychological unrest, chaos, and disturbances around the globe.9 With the advent of the COVID-19 outbreak, a worldwide shortage of personal protection equipment (PPE) was reported, which endangered the life of frontline healthcare workers (FHCWs). In a Third World country like India, it further added to the concern.10 This pandemic, with its highly contagious nature, diverse clinical presentation, unrecognized asymptomatic and presymptomatic carriers, rapid spread, nonavailability of specific antiviral treatment, and high mortality rate, has caused considerable panic around the globe.11
The FHCWs who are exposed and indirect contacts with the confirmed and suspected COVID-19 cases are vulnerable to both high risks of infection and mental health problems. The most common psychiatric issues experienced by FHCWs include anxiety, post-traumatic stress symptoms, stigma, depressive symptoms, sleep disturbances, and concern regarding contagion exposure to their friends and family.12
Therefore, it is essential to understand how FHCWs think and react when they appraise a pandemic of such magnitude. Hence, this study was undertaken to assess stress and recent-onset psychological impact in FHCWs in a government-designated COVID-19 hospital.
Materials and Methods
This was an exploratory hospital-based study conducted among the FHCWs of Kashmir’s lone government-designated COVID-19 hospital. Snowball sampling technique was used. An e-questionnaire was developed using Google Docs, to prevent transmission of infection via fomites. The e-questionnaire was shared through emails, WhatsApp groups, Facebook, and Twitter to the participants. The participants were requested to forward the survey to as many FHCWs as possible. Thus, the link was rolled out to people apart from the first point of contact and so on. On receiving and clicking on the link, the participants would get autodirected to the survey. The first page of the survey consisted of an information page about the purpose of the study and how the data would be used. Participation in the study was voluntary. Participants were asked to give consent and confirm. After they agreed to take the survey, they filled up the demographic details. Then a set of several questions appeared sequentially, which the participants were to answer.
Participants with age more than 18, able to understand the English language, and with access to the internet took part in the study. The data collection was done from April 8, 2020, to April 15, 2020, and it began three weeks after the detection and confirmation of the index case of COVID-19 in Kashmir. The sociodemographic variables, specialization, and place of posting were recorded. The online self-reported stress questionnaire and the impact of event scale—revised (IES-R) were used.
The stress questionnaire comprises 23 items contained in 4 sections: anxiety about infection, exhaustion, workload, and feeling of being protected during the pandemic of the 2019-nCoV. Each item was rated on a 5-point Likert scale (1: not at all, 2: slightly, 3: definitely, 4: markedly, 5: very severely) to describe how often the FHCWs experienced the 23 items during the pandemic. Nineteen items used in our study were based on the stress-related questionnaire used in a study on influenza pandemic (2009).13 However, four new questions were added to the questionnaire (questions 20–23]. The questionnaire was validated in the Kashmiri population, and the Cronbach’s α was found to be 0.79, meaning an acceptable consistency.
The IES-R is a 22-item Likert rating scale, with a total score ranging from 0 to 88. This self-reporting measure assesses the subjective distress in the form of post-trauma symptoms (PTS) experienced by the subjects at any time during the last month of the pandemic.14 A score of 0-23 is interpreted as normal, 24-32 as mild, 33-36 as moderate, and ˃ 37 as severe psychological impact.15 The survey was approved by the Institutional Ethics Committee and Board of Research Studies.
Statistical Analysis
Each item of the stress questionnaire was summarized as mean and standard deviation. IES-R score was treated as a categorical variable and summarized as frequency and percentage. Independent samples Kruskal–Wallis test was used to compare stress questionnaire item scores across categories of other categorical variables. In cases where Kruskal–Wallis P value was <0.05, as multiple comparisons were made, the P values were adjusted using Bonferroni correction. The association between participant characteristics and psychological impact (IES-R) was tested using Fisher’s exact test, and a two-sided exact P value was reported. All tests were two-tailed, with P < 0.05 considered statistically significant. Statistical analysis was performed using SPSS version 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, version 21.0. Armonk, NY: IBM Corp.).
Results
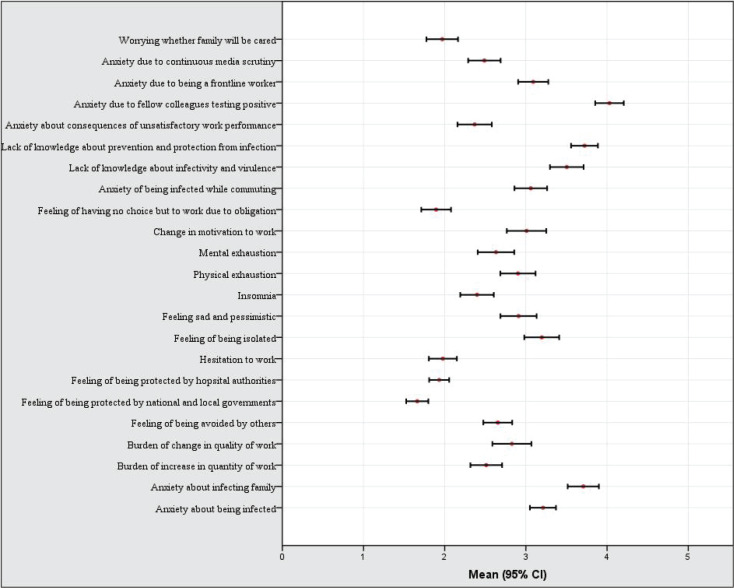
A total of 142 responses were received. Out of this, 3 were incomplete. Six respondents had a history of psychiatric illness and were therefore excluded as a result of which 133 respondents were taken. A total of 81 (61.4%) of the respondents were single, 74 (55.6%) were male, 70 (52.6%) were between 20 and 29 years of age, and 91 (68.4%) were from an urban background. 83 (62.4%) of respondents were doctors, and 28 (21.1%) were registered nurses. A total of 36 (27.1%) were posted in emergency, and 34 (25.6%) were in the in-patient department (Table 1). The mean±SD score of the stress questionnaire was 14.99±3.65. The highest stress score was seen in items like “anxiety due to colleagues testing positive” and “anxiety about infecting family.” The least stress scores were seen in items like “feeling of being protected by national and local government” and “feeling of having no choice but to work due to obligation” (Figure 1).
Table 1. Characteristics of Study Participants.
| Participant Characteristics | Frequency (%) | |
| Age (years) | 20–29 | 70 (52.6) |
| 30–39 | 43 (32.3) | |
| 40 & above | 20(15) | |
| Gender | Male | 74 (55.6) |
| Female | 59 (44.4) | |
| Residence | Urban | 91 (68.4) |
| Rural | 42 (31.6) | |
| Marital status | Single | 81 (61.4) |
| Married | 51 (38.6) | |
| Designation | Doctor | 83 (62.4) |
| Nurse | 28 (21.1) | |
| Technician | 12 (9) | |
| Others | 10 (7.5) | |
| Place of posting | Emergency | 36 (27.1) |
| IPD | 34 (25.6) | |
| Theatre | 23 (17.3) | |
| OPD | 20 (15) | |
| COVID clinic | 13 (9.8) | |
| Swab collection center | 7 (5.3) | |
IPD: in-patient department, COVID: coronavirus disease, OPD: out-patient department.
Figure 1. Mean and 95% Confidence Interval of Various Items in the Stress Questionnaire.
Feeling sad and pessimistic (P < 0.001), feeling of being avoided by others (P = 0.003), the burden of change in the quality of work (P = 0.005), worrying whether the family will be cared for in their absence (P < 0.001), and distress due to colleagues testing positive (P = 0.009) were significantly more in nurses as compared to doctors (Table 2). Stress due to the burden in an increase in the quantity of work (P = 0.014) was seen more in FHCWs working in the swab collection center as compared to those working in the in-patient department (P = 0.024), emergency (P = 0.012), or theatre (P = 0.025) (Table 3). Though not statistically significant, anxiety about being infected (P = 0.72), getting the family infected (P = 0.43), physical exhaustion (P = 0.31), and a decrease in motivation to work (P = 0.14) were more in FHCWs aged ˃ 40.
Table 2. Responses to Stress Questionnaire by the Designation of the Study Participants.
| Variables | Doctor (n = 83) |
Nurse (n = 28) |
Technician (n = 12) |
Others (n = 10) |
P Value* |
| Anxiety about being infected | 3.3 (0.9) | 3.0 (0.8) | 3.3 (1.2) | 3.2 (1.0) | 0.72 |
| Anxiety about infecting family | 3.8 (1.0) | 3.4 (1.3) | 3.6 (1.4) | 3.8 (1.1) | 0.43 |
| Burden of increase in quantity of work | 2.5 (1.1) | 2.6 (1.4) | 2.7 (1.2) | 2.3 (0.8) | 0.90 |
| Burden of change in quality of work | 2.5 (1.4) | 3.6 (1.3) | 2.8 (1.1) | 3.1 (1.7) | 0.005† |
| Feeling of being avoided by others | 2.4 (1.0) | 3.1 (1.1) | 3.0 (0.4) | 2.9 (0.7) | 0.003‡ |
| Feeling of being protected by national and local governments | 1.6 (0.7) | 2.0 (1.0) | 1.8 (0.8) | 1.6 (0.8) | 0.20 |
| Feeling of being protected by hospital authorities | 1.9 (0.6) | 2.3 (1.0) | 1.8 (0.8) | 1.8 (0.8) | 0.19 |
| Hesitation to work | 1.9 (1.0) | 1.9 (1.0) | 2.3 (1.1) | 2.2 (0.9) | 0.35 |
| Feeling of being isolated | 3.1 (1.3) | 3.6 (1.2) | 3.2 (1.5) | 2.9 (0.9) | 0.27 |
| Feeling sad and pessimistic | 2.5 (1.2) | 3.7 (1.2) | 3.6 (1.2) | 3.1 (1.1) | <0.001§ |
| Insomnia | 2.2 (1.2) | 2.9 (1.3) | 2.7 (1.1) | 2.2 (0.9) | 0.07 |
| Physical exhaustion | 2.7 (1.2) | 3.1 (1.5) | 3.4 (1.3) | 2.9 (1.0) | 0.31 |
| Mental exhaustion | 2.4 (1.3) | 2.7 (1.4) | 3.4 (1.2) | 3.0 (0.8) | 0.048¶ |
| Change in motivation to work | 2.8 (1.4) | 3.3 (1.5) | 3.6 (1.3) | 3.4 (1.4) | 0.14 |
| Feeling of having no choice but to work due to obligation | 1.8 (1.0) | 1.9 (1.2) | 2.2 (1.5) | 2.1 (0.9) | 0.66 |
| Anxiety of being infected while commuting | 2.9 (1.1) | 3.4 (1.3) | 3.0 (1.4) | 3.4 (1.5) | 0.26 |
| Lack of knowledge about infectivity and virulence | 3.3 (1.2) | 3.9 (1.1) | 3.5 (1.4) | 3.8 (1.0) | 0.15 |
| Lack of knowledge about prevention and protection from infection | 3.6 (0.9) | 3.9 (1.1) | 4.3 (0.8) | 3.8 (0.9) | 0.09 |
| Anxiety about consequences of unsatisfactory work performance | 2.3 (1.2) | 2.7 (1.3) | 2.6 (1.2) | 2.0 (0.8) | 0.30 |
| Anxiety due to fellow colleagues testing positive | 4.0 (1.0) | 4.6 (0.7) | 3.8 (1.4) | 3.5 (1.4) | 0.009# |
| Anxiety due to being a frontline worker | 3.1 (1.1) | 3.1 (1.2) | 3.3 (1.2) | 3.1 (0.9) | 0.94 |
| Anxiety due to continuous media scrutiny | 2.5 (1.2) | 2.3 (1.2) | 2.6 (1.2) | 2.6 (1.0) | 0.71 |
| Worrying whether family will be cared | 1.7 (0.9) | 2.8 (1.4) | 1.8 (0.9) | 2.7 (1.2) | <0.001** |
Figures indicate mean (standard deviation). *Independent samples Kruskal–Wallis test, followed by adjustment for multiple comparisons when P value for the Kruskal–Wallis test was < 0.05. † P value for nurses versus doctors = 0.003. ‡ P value for nurses versus doctors = 0.011. § P value for nurses versus doctors < 0.001. ¶ P value for technicians versus doctors = 0.079 (adjusted P value for multiple comparisons was not significant). # P value for nurses versus doctors = 0.016. ** P value for nurses versus doctors = 0.001, others versus doctors = 0.019.
Table 3. Responses to Stress Questionnaire by Place of Posting of the Study Participants.
| Variables | OPD (n = 20) |
IPD (n = 34) |
Emergency (n = 36) |
COVID clinic (n = 13) |
Theatre (n = 23) |
Swab Collection Center (n = 7) |
P Value* |
| Anxiety about being infected | 3.3 (1.0) | 3.2 (1.1) | 3.2 (0.8) | 3.0 (1.0) | 3.2 (0.6) | 3.7 (1.1) | 0.74 |
| Anxiety about infecting family | 3.8 (1.1) | 3.5 (1.2) | 3.9 (1.1) | 3.7 (1.3) | 3.6 (1.1) | 3.7 (1.1) | 0.78 |
| Burden of increase in quantity of work | 2.7 (1.1) | 2.4 (1.3) | 2.3 (1.1) | 2.9 (1.1) | 2.3 (0.9) | 3.9 (0.7) | 0.014† |
| Burden of change in quality of work | 2.8 (1.3) | 2.9 (1.4) | 2.6 (1.4) | 2.5 (1.4) | 3.0 (1.5) | 4.1 (1.1) | 0.12 |
| Feeling of being avoided by others | 2.7 (1.0) | 2.7 (1.0) | 2.5 (1.2) | 2.8 (1.0) | 2.4 (0.8) | 3.6 (0.5) | 0.11 |
| Feeling of being protected by national and local governments | 1.7 (0.7) | 1.7 (0.8) | 1.7 (0.9) | 1.6 (0.7) | 1.6 (0.9) | 1.1 (0.4) | 0.40 |
| Feeling of being protected by hospital authorities | 2.0 (1.0) | 2.1 (0.8) | 1.8 (0.6) | 1.8 (0.7) | 1.9 (0.6) | 2.3 (0.8) | 0.33 |
| Hesitation to work | 1.9 (1.0) | 2.2 (1.2) | 2.0 (0.9) | 1.5 (0.7) | 1.9 (0.8) | 2.6 (1.4) | 0.25 |
| Feeling of being isolated | 3.1 (1.1) | 3.3 (1.3) | 3.3 (1.3) | 3.0 (1.4) | 3.1 (1.2) | 3.7 (1.4) | 0.85 |
| Feeling sad and pessimistic | 2.9 (1.4) | 3.0 (1.4) | 2.8 (1.2) | 2.5 (1.0) | 3.0 (1.3) | 3.3 (1.6) | 0.86 |
| Insomnia | 2.6 (1.2) | 2.4 (1.5) | 2.4 (1.0) | 2.4 (1.3) | 2.1 (0.7) | 3.3 (1.6) | 0.55 |
| Physical exhaustion |
3.0 (1.2) | 2.7 (1.4) | 2.8 (1.23) | 3.2 (1.2) | 3.0 (1.2) | 3.6 (1.3) | 0.53 |
| Mental exhaustion |
2.7 (1.3) | 2.5 (1.3) | 2.6 (1.3) | 2.5 (1.3) | 2.7 (1.4) | 3.3 (1.3) | 0.74 |
| Change in motivation to work | 2.6 (1.3) | 2.9 (1.5) | 2.9 (1.5) | 3.5 (1.4) | 3.4 (1.3) | 3.0 (1.7) | 0.30 |
| Feeling of having no choice but to work due to obligation | 2.1 (1.1) | 1.9 (1.2) | 1.7 (0.8) | 1.8 (0.7) | 1.9 (1.2) | 2.4 (1.5) | 0.76 |
| Anxiety of being infected while commuting | 3.3 (1.0) | 3.1 (1.4) | 3.0 (1.1) | 2.6 (1.1) | 3.2 (1.2) | 3.1 (1.2) | 0.53 |
| Lack of knowledge about infectivity and virulence | 3.0 (1.3) | 3.3 (1.3) | 3.8 (1.1) | 3.7 (0.9) | 3.7 (0.9) | 3.4 (1.7) | 0.20 |
| Lack of knowledge about prevention and protection from infection | 3.8 (1.1) | 3.8 (1.0) | 3.4 (1.1) | 3.8 (0.6) | 3.8 (0.8) | 4.3 (0.8) | 0.33 |
| Anxiety about consequences of unsatisfactory work performance | 2.5 (1.6) | 2.3 (1.3) | 2.3 (1.1) | 2.7 (1.4) | 2.3 (1.0) | 2.4 (1.3) | 0.97 |
| Anxiety due to fellow colleagues testing positive | 4.3 (1.0) | 4.0 (1.0) | 4.1 (1.1) | 4.3 (0.9) | 3.7 (1.1) | 3.9 (0.7) | 0.38 |
| Anxiety due to being a frontline worker | 3.1 (1.1) | 3.1 (1.2) | 3.0 (1.2) | 2.9 (1.0) | 3.2 (1.0) | 3.3 (0.8) | 0.95 |
| Anxiety due to continuous media scrutiny | 2.2 (1.0) | 2.5 (1.1) | 2.5 (1.1) | 3.2 (1.4) | 2.2 (1.2) | 2.9 (1.45) | 0.29 |
| Worrying whether family will be cared | 2.1 (1.4) | 2.2 (1.1) | 2.0 (1.2) | 1.7 (1.0) | 1.9 (1.2) | 1.3 (0.5) | 0.30 |
Figures indicate mean (standard deviation).* Independent samples Kruskal–Wallis test, followed by adjustment for multiple comparisons when P value for Kruskal–Wallis test was <0.05. † P value for swab collection versus IPD = 0.024, swab collection versus emergency = 0.012, swab collection versus theatre = 0.025. IPD: in-patient department, COVID: coronavirus disease, OPD: out-patient department.
The mean total IES-R score was 45.07±25.53. Severe psychological impact was seen in 81 (60.9%) of the respondents (Table 4). The psychological impact was significantly more in males (P = 0.03) and in those who were married (P = 0.001). The psychological impact was also significantly related to the designation (P = 0.037) and the place of posting (P = 0.002) (Table 5).
Table 4. Psychological Impact of the Pandemic Among Study Participants.
| IES-R | Frequency (%) |
| Normal (0–23) | 41 (30.8) |
| Mild psychological impact (24–32) | 11 (8.3) |
| Moderate psychological impact (33–36) | 0 |
| Severe psychological impact (≥37) | 81 (60.9) |
IES-R: impact of event scale revised.
Table 5. Psychological Impact of the Pandemic by Participant Characteristics.
| Parameters Frequency (%) |
Normal (0–23) |
Mild Psychological Impact (24–32) |
Moderate Psychological Impact (33–36) |
Severe Psychological Impact ( ≥ 37) |
|||
| Frequency (%) | Frequency (%) | Frequency (%) | Total | P Value* | |||
| Age (years) | 20–29 | 24 (34.3) | 8 (11.4) | 0 (0.0) | 38 (54.3) | 70 | 0.11 |
| 30–39 | 15 (34.9) | 2 (4.7) | 0 (0.0) | 26 (60.5) | 43 | ||
| ≥40 | 2 (10.0) | 1 (5.0) | 0 (0.0) | 17 (85.0) | 20 | ||
| Gender | Male | 16 (21.6) | 8 (10.8) | 0 (0.0) | 50 (67.6) | 74 | 0.030 |
| Female | 25 (42.4) | 3 (5.1) | 0 (0.0) | 31 (52.5) | 59 | ||
| Residence | Urban | 25 (27.5) | 8 (8.8) | 0 (0.0) | 58 (63.7) | 91 | 0.46 |
| Rural | 16 (38.1) | 3 (7.1) | 0 (0.0) | 23 (54.8) | 42 | ||
| Marital status | Single | 32 (39.5) | 10 (12.3) | 0 (0.0) | 39 (48.1) | 81 | 0.001 |
| Married | 9 (17.6) | 1 (2.0) | 0 (0.0) | 41 (80.4) | 51 | ||
| designation | Doctor | 30 (36.1) | 5 (6.0) | 0 (0.0) | 48 (57.8) | 83 | 0.037 |
| Nurse | 10 (10) | 4 (14.3) | 0 (0.0) | 14 (50.0) | 28 | ||
| Technician | 0 (0.0) | 1 (8.3) | 0 (0.0) | 11 (91.7) | 12 | ||
| Others | 1 (10.0) | 1 (10.0) | 0 (0.0) | 8 (80.0) | 10 | ||
| Place of posting | OPD | 11 (55.0) | 2 (10.0) | 0 (0.0) | 7 (35.0) | 20 | 0.002 |
| IPD | 9 (26.5) | 7 (20.6) | 0 (0.0) | 18 (52.9) | 34 | ||
| Emergency | 13 (36.1) | 1 (2.8) | 0 (0.0) | 22 (61.1) | 36 | ||
| COVID clinic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 13 (100.0) | 13 | ||
| Theatre | 8 (34.8) | 1 (4.3) | 0 (0.0) | 14 (60.9) | 23 | ||
| Swab collection center | 0 (0.0) | 0 (0.0) | 0 (0.0) | 7 (100.0) | 7 | ||
IPD: in-patient department, COVID: coronavirus disease, OPD: out-patient department. *Fisher’s exact test, two-sided.
Discussion
Healthcare professionals are always at the forefront of any pandemic and risk their lives in the line of their duty.16 Since the outbreak of COVID-19 in Wuhan, many cases occurred among FHCWs who contracted the infection within the health care facilities. Many doctors and paramedics died from this infection around the world, especially in China and Italy.17, 18
During the outbreak of any pandemic, FHCWs are at risk of getting the infection, though not equally. Staff working in emergency and critical care are at a higher risk.16 For this reason, FHCWs from high-risk areas were chosen in this study. We included nurses, respiratory therapists, ancillary staff, and doctors directly in contact with COVID-19 patients. Most of the FHCWs were young (age group of 20–29 years), unmarried, males, and medical doctors posted in emergencies or in-patient department.
Stress and Profession
In comparison to doctors, the nurses experienced more stress in terms of feeling sad and pessimistic, feeling of being avoided by others, the burden of change in the quality of work, stress due to colleagues testing positive, and worrying whether the family will be cared for in case anything untoward happens to them. This could be explained by their direct and intensive involvement in patient care, close contact and proximity with the patients, insufficient and inadequate protective equipment, and lesser compensation than doctors. Further, majority of the nurses were newly recruited and had fewer years of experience.
Our results are in concordance with authors from China and Taiwan.19, 20 The reasons reported by others, in unison with our results, include anxiety about infecting family,21 inadequate staff,22 the infectivity of the disease, inadequate protective equipment,23 nosocomial spread,24 and risk to life.25
Our results also match with those of Mitchell et al. who found that26 the nursing staff experienced severe stress during the outbreak of vancomycin-resistant enterococci (VRE). Therefore, such a psychological reaction to extreme stress may be common among nurses during a highly infectious pandemic.27
A study done in nurses in the emergency department during the SARS pandemic had also revealed that nurses are more prone to develop psychological distress and behavioral disengagement than doctors, matching our results.28 Many studies done in different parts of the world have also shown that nurses working on the frontline during the SARS outbreak were affected both mentally and physically.20, 29–31
In contradiction to our results, an article from Singapore has shown that physicians and those who were single were at increased risk of developing mental health issues.32 In concordance with our results, Grace et al. have shown that FHCWs directly treating SARS-CoV positive patients experienced a high level of discrimination and mental health issues than those who were not dealing with such patients.33
The latest literature on the mental health of 1,563 health care workers concluded that over half (50.7%) of the respondents experienced depressive symptoms, approximately half of them experienced anxiety, and one-third had problems in sleep.34
The ever-increasing number of confirmed and suspected cases, overwhelming workload, stretched working hours, shortage of specialist staff, inadequate PPE, lack of FDA-approved prophylactic drugs or specific vaccine, feelings of being inadequately supported, and continuous media scrutiny and radar may all contribute to the stress in FHCWs.
Among the various stressors associated with the COVID-19 outbreak, safety was the major concern for the FHCWs. It was extremely stressful for them to see their colleagues displaying COVID-19-like symptoms, testing positive or getting intubated; patients dying in front of them from COVID-19, as well as the fear that they could transmit the disease to their families or friends. Similar concerns were also reported during the MERS-CoV outbreak.27
Other significant stressors experienced by the FHCWs, particularly nurses, were whether their family would be looked after in their absence and whether compensation will be provided to them if they died of COVID-19 infection. Our results are in unison to a MERS-CoV study wherein the expectation of extra financial compensation and recognition by the hospital helped them to reduce stress.35
Stress and Place of Posting
Stress due to the burden of an increase in the quantity of work was more in FHCWs working in swab collection center. This can be explained by a sudden and dramatic increase in the workload of microbiologists and laboratory technicians working there. To identify the asymptomatic cases and to save the region from catastrophe, they were pushed for aggressive testing. What further aggravated the stress was the continuous media scrutiny and radar, which pressurized them for a rapid increase in the testing rate,36 which was followed by a seven-fold increase in the testing rate in just two weeks.37
Stress and Age
In our study, the stress was not significantly affected by age; however, it was slightly high in the age group of 40-49 years. Anxiety about being infected and thereby infecting the family was more in the age the group of 40-49 years, which is in concordance with studies done on the influenza pandemic in the USA38 and SARS pandemic in Singapore.39 The possible reasons are that majority of the people are married and have children by this age. Thus, there is always stress about bringing the virus home and passing it on to loved ones and family members. The presence of medical comorbidities too contributes to the increased stress in this age group. However, even young people with no comorbidities can contract the disease and become critically ill or even die40; age is no bar for the virus.41 Hence, contrary to what was expected, stress was not significantly associated with age. In our study, exhaustion was also more common in the elderly people, which could further be explained by the decline in body strength with age and the comorbid medical conditions.
Psychological Impact
The psychological impact, as depicted by the IES-R score, was significantly more in males and in those who were married. The psychological impact was also significantly related to the place of posting. Severe psychological impact was reported by those working in COVID clinics or the swab collection center. The reason for the highest psychological impact in these areas seems to be a high-risk work environment experienced by the FHCWs. The most common risk was the generation of aerosols and droplets and the subsequent very high chance of illness transmission. FHCWs working in COVID clinics and swab collection center also complained of the provision of inadequate PPE such as N95 masks or face shields, splash shields, centrifuge safety cups, and sealed centrifuge rotors. The rapid escalation in cases, staggering death figures exceeding those of previous pandemics, and unprecedented nature of the COVID-19 pandemic in terms of the worldwide death toll in doctors and paramedics might have caused the heightened response in the FHCWs here in Kashmir. Unpreparedness to deal with the pandemic and lack of knowledge about the disease can be the other contributing factors.
Published data has shown that perceived risk levels related to an event are affected by unfamiliarity and perceived uncontrollability of the hazards involved and that these perceptions, in turn, affect a person’s likelihood of developing post-traumatic stress disorder.42, 43
In our study, about two-thirds of the respondents were having symptoms of PTS (mild and severe). A recent study from China has shown that 53.8% of participants rated the psychological impact of the COVID-19 outbreak as either moderate or severe during the initial phases of the outbreak; thus, these results almost match our results.44 Our results are also consistent with studies on the SARS outbreak, with psychological distress experienced at the beginning, during, and end of pandemic by 18 to 57% of FHCWs.45
Published literature about the 2003 SARS outbreak has shown severe psychological reactions among medical professionals.46–49 The commonest reasons shared by the studies include anxiety about getting the infection and carrying the contagion to their families and friends,50 uncertainty and stigmatization,50, 47 and reluctance to work. The published data has shown that FHCWs working in high-risk departments such as critical care units and isolation wards are at increased risk of developing adverse psychological reactions than those working in low-risk units.51
First medical responders including paramedics and ambulance drivers have also been found to display heightened stress, become emotionally effected and traumatized, and have higher levels of depression and anxiety.52 Review of published data on adverse effects of the disaster on the psychological health of FHCWs revealed the common risk factors for developing mental health issues, which include inadequate social support and communication, maladaptive coping, lack of knowledge, and training.51 A study in Singapore reported that more than 27% of FHCWs had a General Health Questionnaire-28 score of more than 5, and around 20% of the physicians and nurses experienced PTSD.32
Similarly, a hospital in Toronto reported about 29% of participants scoring above the normal threshold in emotional distress on GHQ-12,53 while a survey of stress reactions among FHCWs in SARS reported that 5% of participants had acute stress disorder.47
Limitations
First, convenient sampling and lack of knowledge about the nonresponders may bias the results.54 Second, a single-center study performed early in the outbreak may limit the generalizability of the findings.
Conclusion
More than half of the FHCWs had a severe psychological impact from COVID-19. The psychological impact was more in males and those who were married, and it was related to the place of posting. Nurses had significantly higher stress as compared to doctors. Early psychological interventions targeting this vulnerable group may be of help. Frequent provision of information about the pandemic and liaison psychiatric services may help to reduce the stress of on FHCWs and the psychological impact on them.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.World Health Organization. Pneumonia of unknown cause—China. 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/.
- 2.World Health Organization. Novel coronavirus—China. 2020. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/.
- 3.Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ Clin Res Ed; 2020; 368: m408. [DOI] [PubMed] [Google Scholar]
- 4.Gates B. Responding to covid-19: a once-in-a-century pandemic? N Engl J Med; 2020; 382(18): 1677–1679. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Coronavirus disease 2019 (COVID-19) situation report 46. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_2.
- 6.Baud D, Qi X, Nielsen-Saines K. et al. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis; 2020. March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.First corona virus case in Kashmir as Khanyar resident tests Positive: Govt/greater kasmir. https://www.greaterkashmir-com.cdn.ampproject.org/v/s/www.graeterkashmir.com/news/Kashmir/first-coronavirus-case-in-kashmir-as-Khanyar-resident-tests-positive-govt (accessed April 3, 2020).
- 8.Tang B, Wang X, Li Q. et al. Estimation of the transmission risk of the 2019-nCoV and its implication for public health interventions. J Clin Med; 2020; 9(2): 462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: Structured letter therapy. Psychiatr Invest; 2020; 17(2): 175–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Rolling updates on coronavirus disease (COVID-19). 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-theyhappen (accessed April 4, 2020).
- 11.Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV). BioSci Trends; 2020;14(1): 69–71. [DOI] [PubMed] [Google Scholar]
- 12.Zheng W. Mental health and a novel coronavirus (2019-nCoV) in China. J Affect Disord; 2020. Published online March 21, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuishi K, Kawazoe A, Imai H. et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci; 2012; 66(4): 353–360. [DOI] [PubMed] [Google Scholar]
- 14.Weiss D, Marmar CR. The impact of the Event Scale—Revised. In: Wilson J, Keane TM. (eds) Assessing psychological trauma and PTSD: A practitioner’s handbook. New York, NY: Guilford Press, 1997: 399–411. [Google Scholar]
- 15.Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale—revised. Behav Res Ther; 2003. Dec 1; 41(12): 1489–1496. [DOI] [PubMed] [Google Scholar]
- 16.Simonds AK, Sokol DK. Lives on the line? Ethics and practicalities of duty of care in pandemics and disasters. Eur Respir J; 2009; 34: 303–309. [DOI] [PubMed] [Google Scholar]
- 17.https://www.thehindubusinessline.com/news/world/covid-19-over-100-italian-doctors-have-died-of-treating-virus-patients/article31305687.ece (accessed April 20, 2020).
- 18.https://www.thehindubusinessline.com/news/world/covid-19-over-100-italian-doctors-have-died-of-treating-virus-patients/article31305687.ece (accessed April 20, 2020).
- 19.Li L, Cheng S, Gu J. SARS infection among health care workers in Beijing, China. JAMA; 2003; 290(20): 2662–2663. [DOI] [PubMed] [Google Scholar]
- 20.Shih FJ, Gau ML, Kao CC. et al. Dying and caring on the edge: Taiwan’s surviving nurses’ reflections on taking care of patients with severe acute respiratory syndrome. Appl Nurs Res; 2007; 20(4): 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sibbald B. Right to refuse work becomes another SARS issue. CMAJ; 2003; 169: 141. [PMC free article] [PubMed] [Google Scholar]
- 22.Taylor S, White B, Muncer S. Nurses’ cognitive structural models of work-based stress. J Adv Nurs; 1999; 29: 974–983. [DOI] [PubMed] [Google Scholar]
- 23.Farquharson C, Baguley K. Responding to the severe acute respiratory syndrome (SARS) outbreak: lessons learned in a Toronto emergency department. J Emerg Nurs; 2003; 29: 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schabas R. SARS: prudence, not panic. CMAJ; 2003; 168: 1432–1434. [PMC free article] [PubMed] [Google Scholar]
- 25.Drazen JM. SARS: looking back over the first 100 days. N Engl J Med; 2003; 349: 319–320. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell A, Cummins T, Spearing N. et al. Nurses’ experience with vancomycin-resistant enterococci (VRE). J Clin Nurs; 2002; 11: 126–133. [DOI] [PubMed] [Google Scholar]
- 27.S-H Lee, Y-Y Juang, Su YJ. et al. Facing SARS: Psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen Hosp Psychiatry; 2005; 27(5): 352–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong TW, Yau JK, Chan CL. et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur J Emerg Med; 2005; 12(1): 13–18. [DOI] [PubMed] [Google Scholar]
- 29.Chan S. Nurses fighting against severe acute respiratory syndrome (SARS) in Hong Kong. J Nurs Scholarsh; 2003; 35(3): 209. [DOI] [PubMed] [Google Scholar]
- 30.Tzeng HM. Fighting the SARS epidemic in Taiwan: a nursing perspective; J Nurs Adm; 2003; 33(11): 565–567. [DOI] [PubMed] [Google Scholar]
- 31.Mok E, Chung BP, Chung JW. et al. An exploratory study of nurses suffering from severe acute respiratory syndrome (SARS). Int J Nurs Pract; 2005; 11(4): 150–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chan AOM, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med Oxf Engl; 2004; 54: 190–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grace SL, Hershenfield K, Robertson E. et al. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics; 2005;46(5):385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu S, Yang LL, Zhang CX. et al. 2019 novel coronavirus: online mental health services. Lancet Psychiatry. 2020: In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res; 2016; 14(1): 7–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sidiq N. COVID-19 in Kashmir: “Infection seeping in community.” 2020. https://www.aa.com.tr/en/asia-pacific/covid-19-in-kashmir-infection-seeping-in-community-/1799641 (accessed May 4, 2020).
- 37.https://www.deccanherald.com/national/j-k-s-coronavirus-testing-capacity-has-increased-to-over-350-samples-per-day-jitendra-singh-825453.html (accessed on April 20, 2020).
- 38.Balicer RD, Omer SB, Barnett DJ. et al. Local public workers’ perceptions toward responding to an influenza pandemic. BMC Public Health; 2006; 6: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Hameed F, Wahla AS, Siddiqui S. et al. Characteristics and outcomes of Middle East respiratory syndrome coronavirus patients admitted to an intensive care unit in Jeddah, Saudi Arabia. J Intensive Care Med; 2016 Apr 9; 31(5): 344–348. [DOI] [PubMed] [Google Scholar]
- 40.The New Indian Express. 26-year-old becomes first Pakistani doctor to die from coronavirus. 2020. https://www.newindianexpress.com/world/2020/mar/23/26-year-old-becomes-first-pakistani-doctor-to-die-from-coronavirus-2120485.html (accessed April 11, 20).
- 41.Koh D, Lim MK, Chia SE. et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Med Care; 2005; 43: 676–682. [DOI] [PubMed] [Google Scholar]
- 42.Marshall RD, Bryant R, Amsel L. et al. The psychology of ongoing threat: Relative risk appraisal, September 11, attacks and terrorism-related fears. Am Psychol; 2007; 62(4): 304–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marshall RD, Galea S, Kilpatrick D. Psychological reactions to terrorist attacks. Findings from the National Study of Americans’ reactions to September 11: Comment. JAMA; 2002; 288(21): 2683–2684. [DOI] [PubMed] [Google Scholar]
- 44.Wang C, Pan R, Wan X. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health; 2020; 17: 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Phua DH, Tang HK, KY: Tham. Coping responses of emergency physicians and nurses to the2003 severe acute respiratory syndrome outbreak. Acad Emerg Med; 2005, 12: 322–328. [DOI] [PubMed] [Google Scholar]
- 46.Maunder R, Hunter J, Vincent L. et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ; 2003; 168(10): 1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 47.Bai Y, Lin CC, Lin CY. et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv; 2004; 55(9): 1055–1057. [DOI] [PubMed] [Google Scholar]
- 48.Lee AM, Wong JG, McAlonan GM. et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry; 2007; 52(4): 233–240. [DOI] [PubMed] [Google Scholar]
- 49.Chua SE, Cheung V, Cheung C. et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry; 2004; 49(6): 391–393. [DOI] [PubMed] [Google Scholar]
- 50.Maunder R, Hunter J, Vincent L. et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ; 2003; 168(10): 1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 51.Naushad VA, Bierens JJ, Nishan KP. et al. A systematic review of the impact of disaster on the mental health of medical responders. Prehospital Disaster Med; 2019; 34: 632–643. [DOI] [PubMed] [Google Scholar]
- 52.McAlonan GM, Lee AM, Cheung V. et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry Rev Can Psychiatr; 2007; 52: 241–247. [DOI] [PubMed] [Google Scholar]
- 53.Martinese F, Keijzers G, Grant S. et al. How would Australian hospital staff react to an avian influenza admission, or an influenza pandemic? Emerg Med Australas; 2009; 21(1): 12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ameen S, Praharaj SK. Problems in using WhatsApp groups for survey research. Indian J Psychiatry; 2020; 62: 327–328. [DOI] [PMC free article] [PubMed] [Google Scholar]