Summary
Objective
Commercial online weight management programmes are popular and easily accessible but often lack training in empirically validated behaviour change strategies and produce suboptimal outcomes. This study evaluated the effects of a Web‐based virtual reality (VR) programme for enhancing behavioural skills training and weight loss when offered as an adjunct to a commercial online weight management programme.
Methods
N = 146 adults with overweight/obesity (body mass index [BMI] 27‐40 kg/m2) were randomized to 6 months of no‐cost access to the Weight Watchers (WW) online platform alone or enhanced with the Experience Success (WW + ES) programme, consisting of four Web‐based VR sessions for training in behavioural weight‐loss skills related to the home environment, the workplace, physical activity and social situations (i.e., a party at a friend's house). Weight was measured at the research centre at baseline, 3 and 6 months.
Results
Both groups achieved statistically significant weight loss across the trial, with no difference in mean ± standard error (SE) weight loss between WW and WW + ES at 3 months (2.7 ± 1.1 kg vs. 4.2 ± 1.1 kg, respectively; P = .086) but greater weight loss in WW + ES at 6 months (2.6 ± 1.3 kg vs. 4.9 ± 1.3 kg, respectively; P = .042).
Conclusions
This study demonstrates the potential of Web‐based VR skills training to enhance outcomes of commercial online weight management programmes that are widely accessible. Compared with traditional didactic methods for online skills training, VR simulation provides opportunities to learn behavioural skills via modelling and experiment with skills in real‐world situations. More research is needed to identify specific behavioural mechanisms by which ES may improve outcomes.
Keywords: obesity, virtual reality, weight loss
1. INTRODUCTION
Gold‐standard empirically validated behavioural weight‐loss programmes 1 (BWLs) have failed to reach most individuals with overweight and obesity due to the high cost and limited accessibility of the frequent in‐person treatment sessions they require. 2 Commercial online programmes have emerged as a potentially cost‐effective alternative; however, they vary widely in the degree to which they incorporate evidence‐based strategies and skills for weight loss. 3 Furthermore, their online format limits the degree to which patients can benefit from important experiential components of in‐person treatment. In particular, the behaviour change theories that serve as the foundation for most BWLs, such as Social Cognitive Theory (SCT), emphasize the importance of modelling (i.e., observing a treatment provider or peer demonstrate appropriate skills use) and practice (i.e., attempting and refining loss skills during treatment sessions before implementing them in real‐world settings) that are rarely replicated online. 4 This limited integration of empirically validated skills training, and the lack of experiential learning, likely contribute to the historically modest weight losses produced by online weight management programmes. 1 There is thus a need for adjunctive resources to provide experiential training in empirically validated weight management strategies in commercial online programmes.
Virtual reality (VR) technology has the potential to address the aforementioned gaps in commercial online weight management programmes by facilitating simulated learning experiences. 5 , 6 The hallmark of VR is ‘a three‐dimensional image or environment that can be interacted with in a seemingly real or physical way.’ 7 VR can be highly ‘immersive’ when implemented via specialized equipment, such as stereoscopic VR goggles, headphones and tactile gloves. Alternatively, VR can be implemented in the form of a three‐dimensional environment that is viewed and navigated using a personal computer (PC) with online connectivity, which is available to most US adults. Using VR, individuals can be presented with realistic situations involving common challenges to weight management. They can see others model effective use of skills to overcome these challenges (one of the most fundamental forms of human learning), practice implementing skills in a realistic way and virtually experience the consequences of their choices, both positive and negative. Experiential learning methods have been shown to result in deeper and more persistent learning compared with more didactic methods often implemented in online weight management programmes, such as skills training videos or informational Web pages. 8 , 9 , 10 , 11
Several previous studies have demonstrated the potential of VR for weight management, but none have specifically aimed to improve outcomes of commercial online programmes. 5 , 12 , 13 , 14 , 15 , 16 For example, a PC‐based weight‐loss intervention delivered in the virtual world Second Life that included the opportunity to practice weight‐loss skills and interact with peers produced statistically significant 12‐week weight losses that did not differ from those achieved via in‐person treatment (3.9 vs. 2.8 kg, respectively; P = .29). 17 In addition, the Second Life condition produced superior improvements in weight‐related self‐efficacy. Another study with N = 20 found that participants who received 9 months of weight‐loss treatment in Second Life achieved larger mean weight losses compared with participants who received 3 months of face‐to‐face treatment followed by 6 months of Second Life (14.0% versus 9.5% of initial body weight, respectively; P < .05). 18
In a previous study, our research team developed the standalone ‘Experience Success’ (ES) platform to deliver PC‐based VR scenarios targeting (1) knowledge of barriers that interfere with eating control, (2) behavioural skills to cope with these barriers, (3) confidence for using these skills and (4) commitment to using these skills in real‐world situations. 19 A single scenario was developed that focused on eating in social situations, which involved attending a virtual house party populated with virtual guests. In navigating the party, users were faced with social challenges such as peer pressure to overeat and intrusive/negative comments about their weight‐loss efforts. They also faced practical challenges, including building a healthy plate of food from a potluck buffet. Users were able to observe certain guests demonstrating skills for coping with these challenges (modelling) and experiment with various skills themselves (practice). In testing at a research centre with N = 37 adults with overweight/obesity, participants described the scenario as highly realistic, and participants reported increased ability to cope with the types of challenges presented in the scenario. The average of acceptability and feasibility ratings was 6.5 out of 7, which encompassed comprehensibility, credibility, relevance, usefulness, applicability, ease of use, liking and likelihood of recommending the VR scenario to others.
The purpose of the current study is to describe a more fully developed ES system that includes three additional scenarios focused on behavioural weight‐loss skills related to the home environment, the workplace and physical activity and to evaluate its effects on 3‐ and 6‐month weight losses when provided as an adjunct to a popular commercial online weight management programme in a small randomized trial. Change in weight control behaviours, many of which were targeted by ES, were measured and tested as potential contributors to change weight loss. Participant engagement was also measured and tested as a potential contributor to change in weight control behaviours and weight loss. Lastly, participant satisfaction with ES was evaluated.
2. METHODS
2.1. Participants
Eligibility requirements included English language fluency, age 18 to 70 years, body mass index (BMI) 25 to 45 kg/m2, ability to walk two blocks unassisted without stopping and access to an Internet‐connected PC. Exclusion criteria included: report of a heart condition, chest pain during periods of activity or rest or loss of consciousness on the Physical Activity Readiness Questionnaire; 20 report of a medical condition that would affect the safety and/or efficacy of a weight management programme involving diet and physical activity; report of a condition that would render the participant potentially unlikely to be able to follow the study protocol for 6 months, including terminal illness, substance abuse, eating disorder, dementia or other significant uncontrolled psychiatric problem; current pregnancy, within 6‐month postpartum, or intention to become pregnant within 6 months; plan to move out of the local geographic area within 6 months; previous participation in a weight‐loss study at the research centre within 2 years; and current use of weight‐loss medication, and current participation in another behavioural weight management programme. Individuals endorsing joint problems, medical conditions or use of prescription medication that could limit physical activity were required to provide documentation of physician approval prior to participation.
2.2. Study design
This 6‐month randomized controlled trial was conducted at the Weight Control and Diabetes Research Center of The Miriam Hospital and Brown University. Recruitment was conducted via ads in local print media and announcements sent electronically to employees of a large regional healthcare system. Initial eligibility screening was conducted by phone. Individuals who screened eligible were invited to attend an orientation session at the research centre where the study procedures were explained in detail, informed consent procedures were completed and height and weight were measured to confirm their BMI was in the eligible range. During the following week, participants were required to demonstrate Internet access and ability to follow basic study procedures. They were first asked to visit a study website to view an online lesson that reviewed the study protocol. They were instructed to return to the study website approximately 3 days later to answer five simple questions to confirm their comprehension of study procedures. Participants who completed these tasks successfully were then allowed to attend a randomization visit at the research centre where they received printed instructions for the treatment condition to which they were assigned. Participants were randomized to condition using randomly permuted blocks of two, four and six stratified by sex. Study procedures were approved by The Miriam Hospital IRB.
2.3. The Weight Watchers online programme
All participants received 6 months of no‐cost access to the online weight management programme offered by WW (formerly Weight Watchers), accessible via website and mobile app. The WW programme focused on the use of a points system to track dietary intake relative to a daily goal in order to produce an energy deficit and increase dietary quality. The daily points goal was personalized based on sex, age, starting weight and activity level. Foods with high energy density and/or little nutritional value (e.g., sweets and snack foods) were assigned a high point value, while foods with better nutritional quality with low energy density (e.g., fruit, vegetables, whole grains, lean meats and other proteins) were assigned a low or zero‐point value. The WW programme also contained basic diet and physical activity education, and while some online WW resources provided information on theory‐based behavioural weight‐loss strategies, these strategies were not the focus of the WW programme.
2.4. The ES programme
Half of the participants were randomized to receive the ES programme (WW + ES) in addition to the WW programme. ES consisted of four separate ‘scenarios’ focused on challenges at home, the workplace, the gym and social gatherings that were made available to participants at weeks 2, 4, 6 and 8, respectively. In addition to capturing locations in which adult weight losers reported facing most of their behaviour challenges in our previous study, 19 these locations are applicable across a wide range of participant demographics and backgrounds and provided opportunities for a variety of different types of weight‐loss challenges. While our previous work on the ES system involved fully 3D‐modelled environments and avatars, development was costly and more difficult to deliver via the Web due to their graphically intensive nature. As such, the scenarios for this study were developed using static 3D‐modelled backgrounds that were blended with live‐action video recordings of human actors, which reduced development costs and enabled Web‐based delivery to most PCs and mobile devices. This approach also had the added benefit of improved emotional realism.
The scenarios followed the weight‐loss journey of a character, ‘Alex,’ portrayed by a middle‐aged White woman with obesity. This demographic was chosen for the main character given that it represents the background most common for individuals presenting for obesity treatment, and the resources available for this project only allowed for one version of Alex to be created. The scenarios were presented in an order that depicted one full day in Alex's life (starting at home, going to work, going to the gym and then ending the day at a party at a friend's house). Each scenario allowed participants to guide Alex's actions through several challenges unique to each respective environment by choosing from a list of predetermined options at key decision points, as described below. Consistent with SCT, emphasis was placed on presenting participants with opportunities to observe Alex and other actors within the scenarios successfully implement empirically validated behavioural weight‐loss strategies. The strategies emphasized were drawn from two theories, SCT and Self‐Regulation Theory, which serve as the foundation for BWL. These strategies included goal setting, planning, self‐monitoring, self‐administered rewards for meeting goals, stimulus control and capitalizing on social support. To facilitate practice of key skills, the scenarios included ‘mini‐games’ in which participants were tasked with completing a specific behavioural challenge requiring a multistep problem‐solving process (Figure 1).
FIGURE 1.
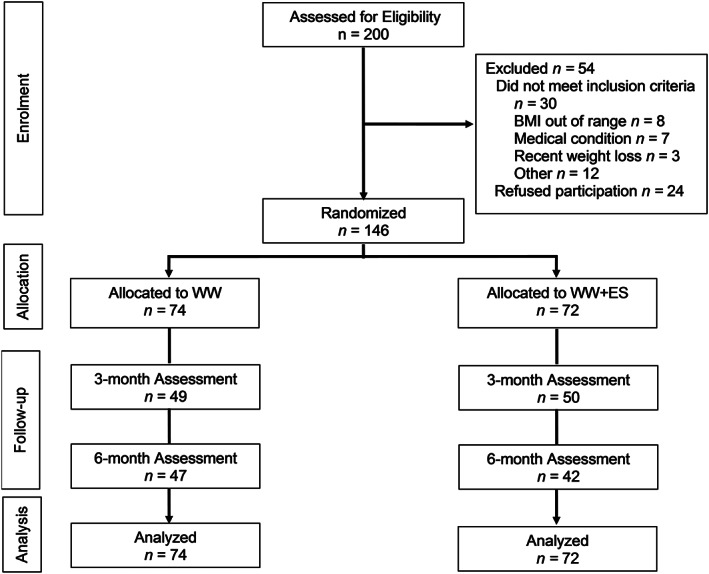
The CONSORT flow diagram includes data on assessment of eligibility, patient enrolment, allocation to condition, follow‐up and primary analysis
The narratives of each scenario were linked, such that taken together, they depicted a single day in Alex's life. The Web‐based dashboard that housed the ES programme used a ‘map of the neighbourhood’ to organize the scenarios and allow participants to navigate between them. Each time a new scenario was made available, it unlocked a new point of interest on the map. Once a scenario was unlocked, participants had access to it for the remainder of their participation in the study. Participants were encouraged to complete each scenario more than once to experiment with applying a diverse set of strategies to overcome behavioural challenges and to experience different narrative outcomes related to their decisions. No single approach was depicted as superior to the others. Rather, the goal was to depict realistic outcomes of various solutions, both positive and negative. For example, when faced with peer pressure to eat birthday cake at a social gathering, deciding to be forthright about Alex's weight‐loss efforts quickly stopped the cake from being offered but caused Alex to become the focus of sensitive personal questions about why and how she is losing weight. Using an indirect communication strategy to deflect the offer of cake helped Alex to avoid such questions, but it resulted in more sustained pressure to consume high‐calorie foods.
The first scenario focused on the morning routine and challenges in the workplace. Key decisions points included: whether to wake up early and exercise or prioritize sleep; whether to self‐weigh, and, if so, how to react to only achieving modest progress; how to react to her house guest who ate her healthy breakfast and baked her cinnamon rolls as a substitute (see Figure 2); whether and how to pack a lunch for work; what to order at the drive‐thru during her commute; whether or not to take the stairs or elevator; coping with being offered doughnuts at work; reacting to a friend suggesting public weigh‐ins for a workplace weight‐loss competition; how to handle an impromptu lunch time celebration with high‐calorie foods; and how to respond to a coworker who is infringing on Alex's privacy regarding her weight‐loss efforts. This scenario predominantly emphasized behavioural strategies related to planning, coping with feeling disappointed and upset, stimulus control, capitalizing on positive social support and assertive communication. The mini‐game involved packing a healthy lunch without being late for work. It indirectly taught principles of food energy density and strategies for food preparation by requiring participants to assemble a meal that is highly satiating, without exceeding an upper calorie threshold or a time limit for preparation.
FIGURE 2.
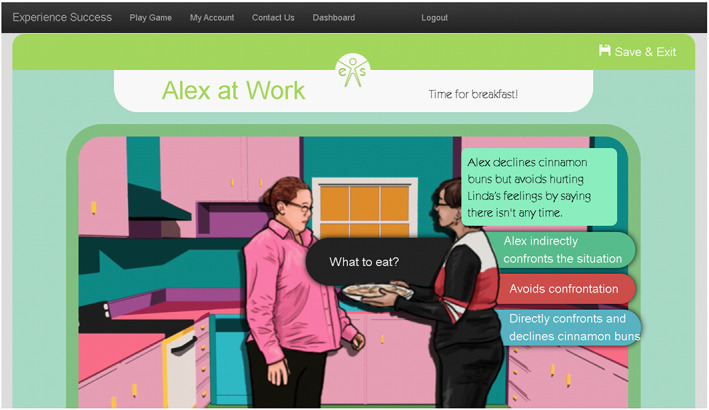
After Alex's friend eats Alex's healthy prepared breakfast, the user chooses Alex's response to her friend's offer of cinnamon buns for breakfast before going to work
The second scenario focused on challenges in the home after work. Key decision points included how to handle temptation caused by palatable high‐calorie food in plain view in the kitchen, eating from restaurants and coping with stress and weight‐loss setbacks. This scenario predominantly emphasized behavioural strategies related to social support, stimulus control and emotional coping. The first mini‐game asked participants to plan ahead and problem solve to stay under a calorie goal while ordering food from a takeout menu or cooking at home. A second mini‐game asked participants to create a frozen yoghurt dessert from a self‐serve establishment without going over an upper calorie limit in a timed challenge. This mini‐game was timed to simulate the pressured experience of putting together a dessert without holding up the line in a typical frozen yoghurt retail setting to maximize self‐efficacy in real‐life time‐limited situations. It also emphasized hidden sources of calories in what may appear at first to be healthy food choices.
The third scenario focused on exercising at a gym. Key challenges and decision points included deciding on the most important features when joining a gym, whether and how to exercise alone or with others, coping with real and perceived weight stigma and how to navigate a gym and relevant interpersonal interactions. This scenario emphasized behavioural strategies including planning, establishing social support, communication and emotional coping (particularly related to weight stigma). The mini‐game focused on how to create a workout schedule based on one's current physical fitness (see Figure 3). This challenged participants to evaluate their current activity levels and develop a reasonable plan to help them reach their goals without causing excessive discomfort (and thereby reducing the chances of future exercise) or injury. This game reinforced planning, self‐monitoring, goal setting and emotional coping.
FIGURE 3.
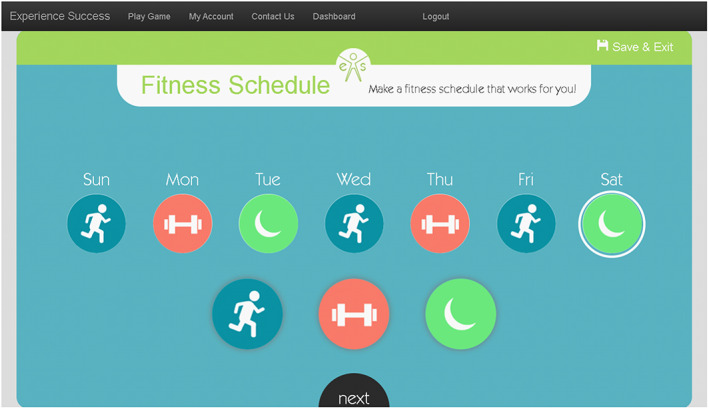
When Alex is in the gym, the user is guided through creating a fitness plan and selecting appropriate exercises, frequency, intensity and duration consistent with programme recommendations and their activity preferences
The fourth scenario focused on attending a social gathering at a friend's house. Key challenges and decisions points included whether and how to disclose weight‐loss efforts to friends, coping with peer pressure to overeat, how to handle friends who espouse misinformation and weight‐loss myths and identification of personal life values and goals that motivate weight‐loss efforts. This scenario emphasized behavioural strategies related to emotional coping, values, interpersonal effectiveness and motivation. The mini‐game focused on estimating the number of calories expended in various forms and durations of exercise and estimating how long one would need to exercise to ‘burn off’ various snack foods. Achieving a better score in this mini‐game allowed Alex to consume healthier snacks after her workout before the party, while worse scores led Alex to consume a high‐calorie snack. The game also addressed strategies for self‐reinforcement that facilitate continued weight‐loss progress. A second mini‐game required users to match items from a buffet to the virtual party goers' dietary requirements within a time limit. This mini‐game provided education about various healthy dietary approaches (e.g., Mediterranean and vegetarian) and simulated the challenge of selecting healthy foods in a time‐limited situation, such as walking along a buffet line.
2.5. Measures
The primary outcome, objective body weight, was measured at the research centre at baseline, 3 and 6 months using a calibrated Tanita® BWB‐800 scale. Weight loss from baseline was calculated in kilogrammes and percent of initial body weight. The proportion of participants achieving a weight loss of greater than or equal to 5% of initial body weight was also calculated.
Engagement with ES was measured in two ways. The first involved tracking completion of ‘scenes’ within a scenario. Each scene involved a few minutes of interaction to address a specific behavioural challenge. Each scenario involved multiple scenes. The second involved tracking completion of full scenarios.
The Weight Control Strategies Scale 21 (WCSS) was used to measure self‐reported adoption of behaviours commonly taught in BWLs to facilitate weight loss. Many of the behaviours captured by the WCSS were also emphasized in ES, as described above. In addition to producing a total score, the WCSS produces subscale scores for several domains well‐aligned with areas of emphasis in the ES programme including Dietary Choices (WCSS‐DC), Self‐monitoring Strategies (WCSS‐SM), Physical Activity (WCSS‐PA) and Psychological Coping (WCSS‐PC). The WCSS total score and subscale scores ranged from a possible 0 (never) to 4 (always) with a midpoint of 2 (about half the time). The WCSS total score and subscales have demonstrated good internal consistency and reliability (Cronbach's alpha .79 to .89), improve during BWL and are correlated with key BWL outcomes including weight, energy intake and energy expenditure.
At 3 and 6 months, participants in both treatment conditions were asked to rate their overall satisfaction with the weight‐loss programme that they received on a 7‐point Likert scale ranging from 1 (very dissatisfied) to 7 (very satisfied). Participants were also asked whether they would recommend the weight‐loss programme to their friends, family or coworkers on a scale of 1 (definitely would not recommend) to 7 (definitely would recommend).
2.6. Statistical analysis
All analyses were performed using IBM SPSS Statistics® for Windows, Version 25.0 (IBM Corp., Armonk, New York). Descriptive statistics for baseline characteristics and ES engagement were generated for each treatment condition and the sample as a whole using the mean, standard deviation, frequency and proportions, as appropriate.
The primary outcomes analysis testing overall and between‐groups change in weight was conducted via generalized linear mixed models (GLMMs) using maximum likelihood estimation. 22 Predictors included treatment condition (WW and WW + ES), time (3‐ and 6‐month assessment points), baseline BMI and covariates selected a priori because of their known association with weight change during BWL and routine inclusion in BWL outcome analyses (i.e., self‐reported age, sex and race/ethnicity represented as non‐Hispanic White versus all others). A random effect of subject was included in the analysis. This approach followed intent‐to‐treat principles by incorporating all available data and using a likelihood function to estimate treatment effects without requiring explicit imputation of missing data. Least‐squares means were calculated via the GLMMs for each condition and compared at 3 and 6 months.
GLMMs were also used to analyse change in WCSS scores, test ES engagement as a predictor of WCSS change and weight loss and test WCSS as a predictor of weight loss. Separate models were used to test for overall change and between groups differences in the WCSS total score and subscale scores. ES engagement was then tested as a predictor of WCSS change in the WW + ES condition, only. Change in WCSS scores and ES engagement were added separately to the model of weight change, described above, to test for associations. An interaction term between WCSS change and group assignment was tested to determine whether the association between change in WCSS and weight loss varied by group.
Participant retention and the proportion of participants achieving a weight loss of greater than or equal to 5% were compared between conditions at 3 and 6 months using a chi‐square test. The 3‐ and 6‐month between‐groups difference in self‐reported satisfaction with treatment, and the likelihood that they would recommend the treatment programme to others, were compared for completers only using independent‐samples t‐tests.
All statistical tests were two‐tailed with alpha = .05. A target sample size of N = 125 was selected to be able to detect a minimum clinically significant between‐groups difference in weight loss of 1.6 kg as statistically significant. This sample size was increased to N = 145 during the conduct of the trial in order to preserve statistical power given observed rates of attrition.
3. RESULTS
Participant flow through the trial is depicted using a CONSORT diagram in Figure 1. Of 200 individuals screened for eligibility, 24 chose not to participate and 30 were excluded, most often because of a BMI outside of the eligible range or medical condition. Characteristics of the 74 participants randomized to WW and the 72 participants randomized to WW + ES are reported in Table 1; the sample was primarily female, middle‐aged and White. Retention was 68% (N = 99) at 3 months and 61% (N = 89) at 6 months and did not differ by treatment condition (Ps > .520).
TABLE 1.
Participant characteristics at baseline
| WW (n = 74) | WW + ES (n = 72) | Total (n = 146) | |
|---|---|---|---|
| Sex, No. (%) | |||
| Men | 17 (23.0) | 15 (20.8) | 32 (21.9) |
| Women | 57 (77.0) | 57 (79.2) | 114 (78.1) |
| Age, mean (SD), years | 59.6 (9.2) | 57.0 (11.2) | 58.3 (10.3) |
| Race, No. (%) | |||
| Asian | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| Black | 2 (2.7) | 1 (1.4) | 3 (2.1) |
| White | 70 (94.6) | 68 (94.4) | 138 (94.5) |
| Other | 2 (2.7) | 2 (2.8) | 4 (2.7) |
| Ethnicity, No. (%) | |||
| Hispanic or Latino | 1 (1.4) | 1 (1.4) | 2 (1.4) |
| Education, No. | |||
| High school or less | 5 (6.8) | 5 (6.9) | 10 (6.8) |
| Some college | 28 (37.8) | 15 (20.8) | 43 (29.5) |
| College or university degree | 16 (21.6) | 25 (34.7) | 41 (28.1) |
| Graduate degree | 25 (33.8) | 27 (37.5) | 52 (35.6) |
| Weight, mean (SD), kg | 92.3 (21.0) | 90.5 (18.1) | 91.4 (15.6) |
| Body mass index, mean (SD), kg/m2 | 33.2 (5.1) | 33.0 (4.6) | 33.1 (4.9) |
Abbreviations: ES, Experience Success; WW, Weight Watchers.
Results of the primary outcomes analysis are reported in Table 2; both treatment conditions achieved statistically significant weight loss at 3 and 6 months (Ps < .001). While there were no statistically significant between‐groups differences in weight loss at 3 months (Ps > .085), WW + ES produced mean ± standard error (SE) weight losses of 4.7 ± 1.1 kg and 4.9 ± 1.3% at 6 months, nearly twice the 2.6 ± 1.1 kg and 2.5 ± 1.3% produced by WW alone (ps<.047). There were no between‐groups difference in the proportion of participants achieving a weight loss of greater than or equal to 5% at 3 and 6 months (Ps>.210).
TABLE 2.
Weight‐loss outcomes
| WW (n = 74) | WW + ES (n = 72) | |
|---|---|---|
| Weight loss, mean (SE), kg | ||
| 3 months | 2.7 (1.1) | 4.2 (1.1) |
| 6 months | 2.6 (1.1) | 4.7 (1.1) |
| Weight loss, mean (SE), % | ||
| 3 months | 2.8 (1.3) | 4.6 (1.3) |
| 6 months | 2.5 (1.3) | 4.9 (1.3) |
| Proportion achieving weight loss of ≥5% of initial weight, No. (%) | ||
| 3 months | 15 (20.0) | 21 (29.2) |
| 6 months | 15 (20.0) | 17 (23.6) |
Note. Statistically significant weight loss was observed in both conditions at 3 and 6 months (P < .001). Bolded values indicate a significant difference between groups (P < .05).
Abbreviations: ES, Experience Success; WW, Weight Watchers.
Participants assigned to WW + ES completed a mean ± SD of 31.3 ± 23.2 ES scenes (range 1‐119) and 1.5 ± 1.3 full ES scenarios (range 0‐4). Greater weight loss (kilogrammes) was associated with a greater number of scenes completed (coefficient = .08; SE = .02; P = .001) but not full scenarios completed (coefficient = .7; SE = .4; P = .105).
WCSS scores were analysed as a secondary outcome and are reported for each condition, and the sample as a whole, in Table 3. Both conditions exhibited statistically significant increases on the WCSS total score and subscales (Ps < .001), but there were no between‐groups differences (Ps > .175). Greater improvements in WCSS scores were associated with greater weight loss (kilogrammes) across the sample (Ps < .033), and there were no between‐groups differences in the strength of the associations. ES engagement was not associated with change in WCSS (Ps > .133) with two exceptions; a greater number of ES scenes completed was associated with greater improvements in WCSS‐SM (coefficient = .009; SE = .005; P = .0044) and WCSS‐PC (coefficient = .007; SE = .003; P = .044).
TABLE 3.
WCSS scores
| WW (n = 74) | WW + ES (n = 72) | Total (n = 146) | P value for WW vs. WW + ES | |
|---|---|---|---|---|
| WCSS total score, mean (SE) | ||||
| Baseline | 1.27 ± .06 | 1.33 ± .06 | 1.30 ± .04 | .482 |
| 3 months | 1.55 ± .05 | 1.62 ± .05 | 1.59 ± .04 | .329 |
| 6 months | 1.91 ± .07 | 1.91 ± .08 | 1.87 ± .05 | .425 |
| WCSS ‐ dietary choices, mean (SE) | ||||
| Baseline | 2.32 ± .07 | 2.39 ± .08 | 2.36 ± .05 | .495 |
| 3 months | 2.61 ± .06 | 2.73 ± .07 | 2.67 ± .05 | .184 |
| 6 months | 2.90 ± .09 | 3.08 ± .09 | 2.99 ± .06 | .175 |
| WCSS ‐ self‐monitoring, mean (SE) | ||||
| Baseline | .78 ± .09 | .86 ± .09 | .82 ± .07 | .557 |
| 3 months | 1.13 ± .08 | 1.32 ± .08 | 1.27 ± .06 | .414 |
| 6 months | 1.68 ± .11 | 1.78 ± .12 | 1.73 ± 08 | .532 |
| WCSS ‐ physical activity, mean (SE) | ||||
| Baseline | 1.16 ± .11 | 1.25 ± .11 | 1.21 ± .08 | .578 |
| 3 months | 1.36 ± .10 | 1.39 ± .10 | 1.37 ± .07 | .789 |
| 6 months | 1.55 ± .13 | 1.54 ± .14 | 1.54 ± .09 | .944 |
| WCSS ‐ psychological coping, mean (SE) | ||||
| Baseline | 1.08 ± .09 | 1.15 ± .09 | 1.11 ± .06 | .583 |
| 3 months | 1.49 ± .08 | 1.57 ± .08 | 1.53 ± .05 | .487 |
| 6 months | 1.90 ± .10 | 1.99 ± .11 | 1.94 ± .07 | .578 |
Note. Statistically significant improvement in all WCSS scores was observed in both conditions (P < .001).
Abbreviations: ES, Experience Success; WW, Weight Watchers; WCSS, Weight Control Strategy Scale.
Treatment satisfaction was higher in WW + ES than WW alone at 3 months (mean ± SE: 5.3 ± .2 vs. 4.6 ± .2; P = .033) but not at 6 months (4.9 ± .3 vs. 4.5 ± .2; P = .285). Participants assigned to WW + ES were no more likely than those assigned to WW alone to recommend the treatment programme to others at 3 months (5.6 ± .2 vs. 5.2 ± .2; P = .248) or 6 months (5.3 ± .3 vs. 5.0 ± .2; P = .77).
4. DISCUSSION
In this randomized controlled trial, provision of a Web‐based VR programme for training in BWL skills in combination with a popular commercial online weight management programme produced significantly better weight losses than provision of the commercial online programme alone at 6 months. The lack of a difference in weight loss at 3 months suggests either that statistical power was inadequate to detect the effect or that the total effect of the ES programme was somewhat delayed. The former appears more likely given that the magnitude of the between‐groups difference was similar at 3‐ and 6‐month timepoints. The weight losses overall were modest, but on average, WW + ES exceeded the recommended minimum clinically significant weight loss of 3% of initial body weight. In contrast, WW alone approached, but did not reach, this important threshold. On average, only 20% to 30% of participants reached the more common threshold of 5% weight loss evaluated in clinical trials, and there was no difference between groups. Taken together, these results provide preliminary support for Web‐based VR technology as a tool to improve weight‐loss outcomes of popular weight management programmes delivered online. However, the large amount of missing data in this study is a major limitation that limits confidence in any conclusions that can be drawn about the efficacy of the ES programme, and as such, the results of this study should be viewed as preliminary.
Greater completion of ES scenes was associated with larger weight losses, suggesting that ES may have been a driver of weight‐loss outcomes. Alternatively, completion of ES scenes may be a proxy for overall intervention engagement or motivation. Completion of full ES scenarios was not associated with weight loss, likely because it is a less sensitive measure of engagement that does not capture partial completion of a scenario, or a participant returning to an already completed scenario to experiment with a wider range of behavioural strategies.
Given the superior mean weight losses in WW + ES, it is surprising that superior increases in self‐reported use of weight control strategies were not also observed. While WCSS scores increased in both treatment conditions, the lack of a between‐groups differences suggest that either participants were not able to accurately evaluate and report on their own behaviour, the WCSS did not measure the constructs that explain the between‐groups difference in weight loss or the sample size was inadequate to provide sufficient statistical power to detect what were potentially clinically significance between‐groups differences. The latter does not appear likely, given the small average between‐groups standardized effect size of Cohen's d = .11 (range .01 to .22.), which are unlikely to represent a clinically significant difference. Despite no evidence of meaningful between‐groups differences on WCSS scores, greater engagement with ES was found to be associated with greater improvements in two WCSS subscales related to self‐monitoring and psychological coping, again demonstrating a positive effect of ES, and pointing to ways in which ES may contribute to positive weight‐loss outcomes. In sum, these findings highlight the need for further research to explore the mechanistic pathways by which programmes such as ES exert their effects. Real‐time measurement methods that avoid reliance on retrospective self‐report, such as ecological momentary assessment, may be especially well suited for this purpose.
The low cost, reach and scalability of commercial online weight management programmes such as WW, and adjunctive interventions such as ES, make them promising tools for addressing the obesity epidemic. Improving access to effective weight‐loss strategies for individuals who cannot or will not seek in‐person services is a public heath priority. However, to date, these tools have demonstrated clear limitations and shortcomings. In particular, they appear to appeal to a limited demographic that is overrepresented by well‐educated, middle‐aged, White women, which has been demonstrated in a range of prior studies in addition to this one. 1 , 23 Further efforts are required to tailor treatment and recruitment strategies to other populations. High rates of disengagement are another critical problem of online programmes. Again, many studies have illustrated this phenomenon, 24 which is further reinforced by the relatively high rate of attrition in this study compared with programmes delivered face‐to‐face. While ES was not explicitly designed to address this problem, it did not reduce attrition despite indications that it improved satisfaction with treatment. Strategies such as incorporating minimal human contact to facilitate accountability and support appear to improve engagement and treatment outcomes but tend to increase cost, highlighting the need for additional work to promote engagement in fully automated programmes.
5. CONCLUSIONS
A Web‐based VR programme for training in empirically validated behavioural weight management skills produced modest improvements in the average weight losses produced by a popular commercial online programme. The improvements in weight control behaviours produced by the VR programme were not significantly better than those produced by the commercial online programme, alone. However, greater engagement with the VR programme was associated with better behavioural and weight‐loss outcomes. While VR technology is advantageous in terms of cost, scalability and reach, better strategies are needed to motivate and sustain engagement among a wider range of individuals.
FUNDING
This project was funded by a research grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R42 DK103537). Dr Goldstein is funded by a research grant from the National Heart, Lung, and Blood Institute (K23 HL136845).
CONFLICTS OF INTEREST
Dr Tuerk received research consultant fees from Virtually Better, Inc. Drs Thomas and Bond received research support (i.e., partial salary paid through their academic institutions and funds to conduct the research) from Weight Watchers International, Inc. for other research projects during the execution of this study. Weight Watchers International, Inc. was not involved in the funding or execution of this study. Drs Goldstein and Hadley have no disclosures to report.
TRIAL REGISTRATION
clinicaltrials.gov Identifier: NCT02836132.
ACKNOWLEDGEMENTS
J.G.T. conceived and helped develop the ES programme, conceived and carried out the study procedures and analysed data. C.M.G. helped develop the ES programme and carry out the study procedures. D.S.B., W.H. and P.W.T. helped develop the ES programme. All authors were involved in writing the paper and had final approval of the submitted and published versions. The authors would like to thank the study participants for their contributions to this project.
Thomas JG, Goldstein CM, Bond DS, Hadley W, Tuerk PW. Web‐based virtual reality to enhance behavioural skills training and weight loss in a commercial online weight management programme: The Experience Success randomized trial. Obes Sci Pract. 2020;6:587–595. 10.1002/osp4.451
REFERENCES
- 1. Sorgente A, Pietrabissa G, Manzoni GM, et al. Web‐based interventions for weight loss or weight loss maintenance in overweight and obese people: a systematic review of systematic reviews. J Med Internet Res. 2017;19:e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wadden TA, Tronieri JS, Butryn ML. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol. 2020;75(2):235–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bardus M, van Beurden SB, Smith JR, Abraham C. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int J Behav Nutr Phys Act. 2016;13:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623‐649. [Google Scholar]
- 5. Ferrer‐Garcia M, Gutiérrez‐Maldonado J, Riva G. Virtual reality based treatments in eating disorders and obesity: a review. J Contep Psychother. 2013;43:207‐221. [Google Scholar]
- 6. Ershow AG, Peterson CM, Riley WT, Rizzo AS, Wansink B. Virtual reality technologies for research and education in obesity and diabetes: research needs and opportunities. J Diabetes Sci Technol. 2011;5:212‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. "virtual realty." lexico.com. 2020. https://www.lexico.com/en/definition/virtual_reality (12 April 2020).
- 8. Illeris K. What do we actually mean by experiential learning? Hum Resour Dev Rev. 2007;6:84‐95. [Google Scholar]
- 9. Beckem JM. Bringing life to learning: immersive experiential learning simulations for online and blended courses. JALN. 2012;16:61‐70. [Google Scholar]
- 10. Lee EA‐L, Wong KW. A review of using virtual reality for learning In: Transactions on edutainment I. Springer; 2008:231‐241. [Google Scholar]
- 11. Lee EA‐L, Wong KW, Fung CC. How does desktop virtual reality enhance learning outcomes? A structural equation modeling approach. Comput Educ. 2010;55:1424‐1442. [Google Scholar]
- 12. Behm‐Morawitz E, Lewallen J, Choi G. A second chsance at health: how a 3D virtual world can improve health self‐efficacy for weight loss management among adults. Cyberpsychol Behav Soc Netw. 2016;19:74‐79. [DOI] [PubMed] [Google Scholar]
- 13. Sullivan D, Goetz J, Gibson C, et al. A virtual reality intervention (Second Life) to improve weight maintenance: rationale and design for an 18‐month randomized trial. Contemp Clin Trials. 2016;46:77‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Riva G, Gaggioli A, Dakanalis A. From body dissatisfaction to obesity: how virtual reality may improve obesity prevention and treatment in adolescents. Paper presented at: MMVR2013. [PubMed]
- 15. Williams LM, Pines A, Goldstein‐Piekarski AN, et al. The ENGAGE study: integrating neuroimaging, virtual reality and smartphone sensing to understand self‐regulation for managing depression and obesity in a precision medicine model. Behav Res Ther. 2018;101:58‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lafond E, Riva G, Gutierrez‐Maldonado J, Wiederhold BK. Eating disorders and obesity in virtual reality: a comprehensive research chart. Cyberpsychol Behav Soc Netw. 2016;19:141‐147. [DOI] [PubMed] [Google Scholar]
- 17. Johnston JD, Massey AP, Devaneaux CA. Innovation in weight loss programs: a 3‐dimensional virtual‐world approach. J Med Internet Res. 2012;14:e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sullivan DK, Goetz JR, Gibson CA, et al. Improving weight maintenance using virtual reality (Second Life). J Nutr Educ Behav. 2013;45:264‐268. [DOI] [PubMed] [Google Scholar]
- 19. Thomas JG, Spitalnick JS, Hadley W, Bond DS, Wing RR. Development of and feedback on a fully automated virtual reality system for online training in weight management skills. J Diabetes Sci Technol. 2015;9:145‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adams R. Revised physical activity readiness questionnaire. Can Fam Physician. 1999;45:992, 995:1004‐1005. [PMC free article] [PubMed] [Google Scholar]
- 21. Pinto AM, Fava JL, Raynor HA, LaRose JG, Wing RR. Development and validation of the weight control strategies scale. Obesity. 2013;21:2429‐2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McCulloch CE, Neuhaus JM. Generalized linear mixed models. Wiley StatsRef: Statistics Reference Online. 2014. [Google Scholar]
- 23. Bennett GG, Steinberg DM, Stoute C, et al. Electronic health (eHealth) interventions for weight management among racial/ethnic minority adults: a systematic review. Obes Rev. 2014;15:146‐158. [DOI] [PubMed] [Google Scholar]
- 24. Arem H, Irwin M. A review of web‐based weight loss interventions in adults. Obes Rev. 2011;12:e236‐e243. [DOI] [PMC free article] [PubMed] [Google Scholar]


