ABSTRACT
Objectives:
There are few scales that reflect the function of the stroke-affected arm as it relates to the performance of daily activities while also indicating the difficulty of scale items. In this study, we developed the Activities Specific Upper-extremity Hemiparesis Scale (ASUHS) to evaluate daily activities performable by the affected arm after stroke. We also clarified the validity, reliability, and item difficulty of the scale.
Methods:
The participants were 145 patients with stroke who were consecutively admitted to a convalescent rehabilitation ward. The unidimensionality of ASUHS was assessed by principal component analysis. Analyses of item discrimination and content validity were conducted to assess the overall validity. Reliability was evaluated by assessing internal consistency and inter-rater reliability. Item difficulties were determined by Rasch analysis.
Results:
Unidimensionality, high discrimination, and good content validity were shown for all items. ASUHS consists of a dominant hand scale and non-dominant hand scale. Both scales showed good internal consistency (Cronbach’s α coefficient = 0.99) and substantial inter-rater reliability (Cohen’s Kappa coefficient = 0.74 and 0.75, respectively). Item difficulty was determined as being in the range –8.71 to +5.18 logit.
Conclusions:
This study suggested good validity and reliability of ASUHS. Furthermore, because the item difficulties of daily activities performed by the affected arm were clarified, therapists can use ASUHS to identify the process that should be the next focus for training. Consequently, therapists may be able to train patients in daily activities that match the affected arm’s ability step by step rather than determining training activities empirically.
Keywords: daily activity, Rasch analysis, scale, stroke, upper extremity
INTRODUCTION
The major purpose of improving affected upper extremity function in stroke rehabilitation is to allow practical use of the affected arm in daily activities. Recently, many training methods, e.g., constraint-induced movement therapy,1) robot therapy,2) and mirror therapy,3) have been conducted in patients with stroke to rehabilitate the affected arm. Other strategies have also been developed to make the affected arm usable for daily living.4)
To date, the Barthel Index5) and the Functional Independence Measure (FIM)6) have been developed as measures for assessing activities of daily living (ADL); however, these scales evaluate the degree of independence of daily activities in general and not the activities performable with the affected arm after stroke. A systematic review identified the Leeds Adult Spasticity Impact Scale (LASIS), the Motor Activity Log (MAL), and ABILHAND as measures reported to evaluate real-life function or actual performance in the affected arm of stroke patients.7) LASIS evaluates the ability to hold and stabilize objects with the affected arm.8) MAL is used to evaluate the amount of use and the quality of movement of an arm in some daily activities via a self-completed form.9) ABILHAND contains several items for assessing active unilateral and bimanual function.10) Furthermore, Fugl-Meyer assessment, which is often used to evaluate arm dysfunction,11) is based on the recovery process of hemiplegia after stroke reported by Brunnstrom.12) However, these assessment scales evaluate only dysfunction or a limited set of daily activities; no scale is currently available to evaluate many of the general daily activities that are performed in real life. Although MAL and ABILHAND evaluate whether daily activities are performable, they do not allow detailed evaluation of which particular process in these activities is difficult. The difficulty level of some daily activities has been clarified in ABILHAND,10) but overall, the difficulty level and specific processes remain unclear. Training of appropriate difficulty is important in rehabilitation,13) and appropriate difficulty is also important when setting goals.14) Moreover, training differs depending on the therapist’s experience.15) These considerations also apply to training and goal setting in daily activities performed by the affected arm in stroke patients. It is difficult to determine which processes within daily activities should be the next focus for training because it is challenging for therapists to know the level of difficulty of the daily activities performed with the affected arm; consequently, they have to select practice programs and goals empirically. Therefore, we considered that developing a scale to evaluate the specific processes of daily activities performed with the stroke-affected arm and knowing their difficulty levels would contribute to effective training and goal setting for stroke patients.
The purposes of this study were to develop the Activities Specific Upper-extremity Hemiparesis Scale (ASUHS) for evaluating the activities performable by stroke-affected arms; to assess its internal consistency, inter-rater reliability, item discrimination, and content validity; and to clarify the difficulty of items in the daily activities evaluated by ASUHS.
METHODS
Item Generation
Questionnaire Construction. ASUHS was designed to measure upper extremity activity outcomes of rehabilitation services provided to inpatients with post-stroke hemiparesis. The Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) checklist provides criteria for evaluating the statistical method, internal consistency, reliability, and content validity of health status measurement instruments. These design criteria were addressed in the present study.16,17) Scale development includes four phases: (1) item generation, (2) item reduction and validity, (3) reliability, and (4) hierarchies of item difficulties.18,19)
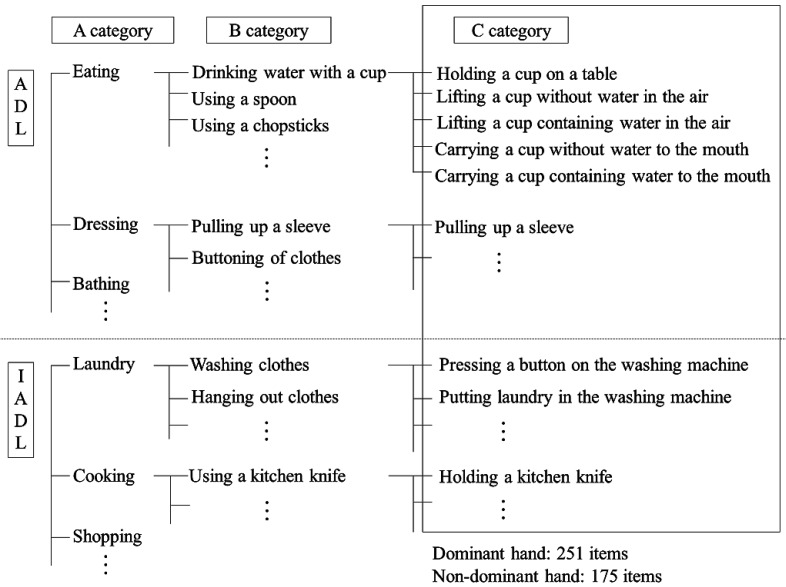
Item Generation. In creating the ASUHS items, 33 previously developed scales that focus on the measurement of motor paralysis of stroke patients, e.g., MAL and ABILHAND, and ADL and instrumental ADL scales such as the Barthel Index, FIM, and Lawton scale20) were considered. Based on these 33 scales, 46 items relating to upper extremity activities were extracted; excluded were those items not implemented because of seasonal, gender, or cultural differences. Furthermore, the preliminary items of ASUHS were created from these 46 items by combining the overlapping items and dividing all items into sub-steps. The preliminary items evaluate the activities performed by the dominant hand (251 items) or non-dominant hand (175 items) in patients with post-stroke hemiparesis. When the dominant hand is paralyzed, the actions mainly performed by the dominant hand are evaluated, and when the non-dominant hand is paralyzed, the actions performed by the non-dominant hand are evaluated. However, unlike some other measures, ASUHS includes activities requiring the use of both hands, such as manipulating buttons. Consequently, ASUHS evaluates the use of the affected arm in bilateral hand movements. The preliminary items of ASUHS were broken down into three categories with increasing levels of specificity: Category A consisted of items relating to ADL and instrumental ADL with reference to the FIM6) and Frenchay Activities Index.21) Category B consisted of the items of ADL and instrumental ADL in category A divided into units for each activity with reference to scales such as MAL; ABILHAND; and the Disabilities of the Arm, Shoulder and Hand.22) Furthermore, category C consisted of the activities of category B divided into four specific processes (Fig. 1). Although there were many items, the activities evaluated were different. Each category C item was scored by assigning points to each response according to the following four levels: 1 point (not attempted with the affected arm), 2 points (affected arm partially used for the activity), 3 points (affected arm used for the activity but is slow or inaccurate), and 4 points (arm movement appears to be normal).
Fig. 1.
The preliminary items of ASUHS. Category A consists of items relating to activities of daily living (ADL) and instrumental activities of daily living (IADL). Category B consists of Category A items subdivided into more detailed items, and category C consists of category B items subdivided into more detailed items.
Implementation of ASUHS. All ADL and instrumental ADL activities were evaluated in the occupational therapy department. Therapists scored all these activities through observation. Although not necessarily applicable to all items, actions that were clearly difficult to perform and actions that could be performed with no difficulty were not carried out, and 1 point and 4 points were respectively assigned to these tasks. For example, if it is difficult for the subject to hold a spoon for “spoon operation” in category B, then “pretending to scoop food using a spoon” and “scooping up a 1-cm block using a spoon” in category C would clearly also be difficult. Therefore, the other items under “spoon operation” would not be assessed and would be assigned 1 point. In the present study, the assessment of all ASUHS items took about 30–60 min to complete. However, in actual clinical use, the ASUHS has the advantage of it being acceptable to assess only selected category B items, in which case the time to complete the assessment is approximately 5 min. Because ASUHS includes many daily activities and processes, it is possible to know which processes are performable and how much of each process is performable with respect to overall daily activities. Further, because ASUHS indicates the difficulty level of each item, it is easier for patients and therapists to understand the daily activities that patients should be capable of doing next. Therefore, therapists can set daily activities that patients should be able to perform next as goals and can provide the activities as training tasks. As a result, ASUHS facilitates goal setting and the provision of practice programs according to the functional level of the affected arm and not to goals and practice programs empirically selected by therapists.
Item Reduction and Validity
Sample and Data Collection. The participants were 145 inpatients with stroke consecutively admitted to a convalescent rehabilitation ward between April 2015 and August 2019. The inclusion criteria were right-handed patients with their first-ever stroke who were hospitalized in a convalescent rehabilitation ward. Stroke was diagnosed according to the World Health Organization definition.23) Patients had unilateral upper extremity hemiplegia/paresis. Moreover, only right-handed people were targeted because some left-handed people sometimes mainly use their right hand, depending on the activity. The exclusion criteria were patients with severe aphasia, apraxia, and dementia (<10 of 30 on the Mini-Mental State Examination)24) who could not follow directions; patients with unilateral spatial neglect (<6 of 9 on the Behavioural Inattention Test)25); patients with balance disorder preventing them from sitting for more than 30 min; patients with intense pain caused by the affected upper extremity; and patients who could not be moved due to complex regional pain syndrome or fractures. Four occupational therapists with an average experience of 6.5 ± 1.7 years were registered as evaluators of ASUHS. Furthermore, they conducted an observational evaluation after being taught the ASUHS evaluation method.
Unidimensionality. Rasch analysis was used to develop ASUHS. Rasch analysis statistically manipulates ordinal data to create a linear measure on an interval scale, and the units of measurement have equal intervals along the scale to account for the magnitude of change.26) Because Rasch analysis requires that a single construct be measured, the unidimensionality of ASUHS was assessed a priori by principal component analysis (PCA).22,27) In PCA, selection of the number of factors is based on established rules: eigenvalues (ε) >1, the scree test, and the percentage of the common variance explained by the different components.22)
Rasch Analysis. Rasch analysis yields an infit mean square (MnSq) accompanied by a standardized Z-score (Zstd), which indicates significance.28) Fit statistics are interpreted to indicate whether an item belongs to the underlying dimension representing the construct and whether the measure obtained for a person is valid. According to previous studies, items in the present study with infit MnSq values of ≥1.4 and Zstd values of ≥2.0 were deleted as misfits.26,28,29,30) After each misfit item was deleted, Rasch analysis was reconducted until all items fitted the criteria of infit MnSq and Zstd.
Discrimination. Item discrimination describes how well items discriminate between test-takers. When a floor or ceiling effect is present, the affected ASUHS items will have poor discrimination ability. Items with discrimination parameters <0.5 were deleted as poor items.31)
Content Validity. Five stroke rehabilitation experts with a mean experience of 10.4 ± 6.1 years reviewed the items for content validity. They confirmed whether the category C items reflected the daily activities or function of the affected arm of patients with stroke by answering the following questions. Can the scale evaluate the daily activities? Does the scale reflect the function of the affected arm? Can the scale be useful in clinical assessment or practice? Is the scale easy to evaluate? Can the scale evaluate the effectiveness of rehabilitation interventions? The experts scored each item on a five-point scale: from 1 (not appropriate) to 5 (appropriate). Next, the items were revised or deleted until all items scored a perfect 5 points; finally, the items were decided with the agreement of all five experts. Furthermore, to divide ASUHS into two scales – one for dominant hand paralysis and one for non-dominant hand paralysis – when reviewing the items for content validity, the subjects were divided into two groups: those with dominant hand paralysis and those with non-dominant hand paralysis. Differences in categorical variables were analyzed by χ2 test, and differences in ordinal variables were analyzed by Mann-Whitney U test.
Reliability
Internal Consistency. The internal consistency reliability was assessed using Cronbach’s α coefficient, which summarizes the inter-item correlations among all items and category B items in a scale.
Inter-rater Reliability. In evaluating the inter-rater reliability, patients were assessed twice by two different occupational therapists within a 3-day period to minimize any change in function. The concordance between the two therapists was quantified by Cohen’s Kappa coefficients.32) Reliability was considered almost perfect if the coefficients were between 0.81 and 1.00, substantial if the values were between 0.61 and 0.80, moderate if between 0.41 and 0.60, fair if between 0.21 and 0.40, and slight if between 0 and 0.20.33)
Hierarchies of Item Difficulties. Rasch analysis was also used to determine hierarchies and ranges of item difficulties in ASUHS. In Rasch analysis, a “logit” is the natural log-odds of the difficulty level of a particular item in relation to all other items in the scale; consequently, it expresses the level of item difficulty on the scale. This analysis places both the items and the subjects into two parallel hierarchies.18)
Statistical Analysis
The statistical method, internal consistency, reliability, and content validity of the scale were evaluated according to the COSMIN checklist. Analyses of PCA results, comparisons between two groups, internal consistency, and inter-rater reliability were completed using the IBM Statistical Package for Social Science (SPSS), version 26.0. A P value <0.05 was considered statistically significant. Rasch analysis was performed using Rasch model software WINSTEPS version 3.91.0. Item discrimination was estimated using IRTPRO version 4.2, which analyzes the two-parameter model of item response theory.
Ethics
Ethical approval was obtained from Tamakyuryo Hospital, Japan (No. 29-2), prior to the start of the study, and written informed consent was obtained from all participants.
RESULTS
Item Reduction and Validity
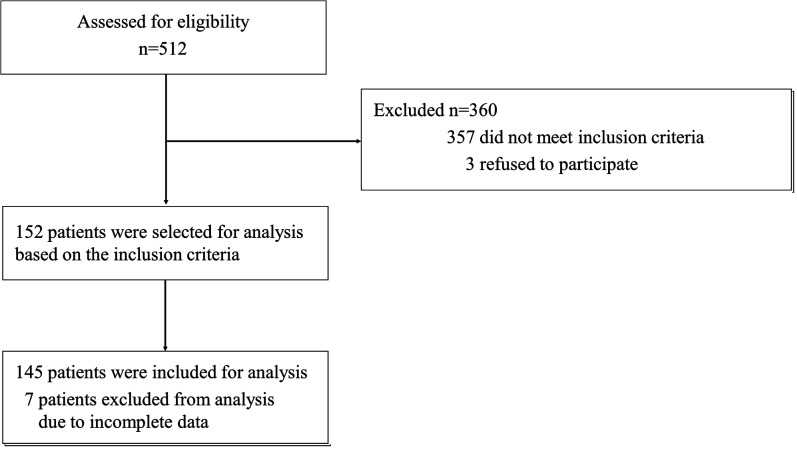
Study Participation. Of the 512 patients screened for eligibility, 145 underwent evaluation (Fig. 2). Patient characteristics are given in Table 1.
Fig. 2.
Schematic of the patient selection process. We enrolled 512 stroke patients with hemiparesis affecting either the dominant or non-dominant hand who were admitted to a convalescent rehabilitation ward. Of these 512 patients, 145 patients finally participated in the study according to the inclusion and exclusion criteria.
Table 1. Clinical characteristics of the participants.
| Characteristic | All participants (n = 145) |
Dominant hand paralysis (n = 78) |
Non-dominant hand paralysis (n = 67) | P Value |
| Age, years | 68.5±12.8 | 69.3±12.7 | 65.4±15.0 | 0.391 |
| Gender, male | 86 (59.3) | 51 (65.4) | 35 (52.2) | 0.108 |
| Time after stroke, days | 60.0±30.3 | 54.3±29.6 | 66.8±29.9 | 0.001 |
| Ischemic stroke | 94 (64.8) | 52 (66.7) | 42 (62.7) | 0.617 |
| Fugl-Meyer assessment | 40.0±22.2 | 40.8±23.2 | 39.0±21.1 | 0.285 |
| Mini-Mental State Examination | 24.7±4.1 | 25.7±4.0 | 23.9±4.1 | 0.083 |
| Functional Independence Measure | 85.1±27.1 | 84.6±27.9 | 85.9±26.2 | 0.850 |
| Activities Specific Upper-extremity Hemiparesis Scale | 2.4±1.1 | 2.5±1.2 | 2.3±1.1 | 0.319 |
Unidimensionality. PCA was conducted to confirm the unidimensionality of ASUHS. The first factor of ASUHS had an eigenvalue (amount of variation in the total sample accounted for by that factor) of 227.6, which explained 90.7% of the total variance of the score. The unidimensionality of the scale was found to be strong as a result of the substantial differences between the first and the second factors because the eigenvalue of the second factor of ASUHS was 5.9. First factor loading for each item of ASUHS was as high as 0.75–0.99. The unidimensionality of ASUHS was therefore confirmed by PCA.
Rasch Analysis. Among the 145 participants, 24 of 251 category C items did not fit the Rasch model because their infit MnSq exceeded 1.4 and their Zstd values exceeded 2.0. Examples of these items were “Holding a cup on the table,” “Holding a spoon,” “Holding a hair dryer,” “Picking up a 1.5-cm marble with chopsticks and carrying it to the mouth,” “Writing your name on 10-mm graph paper,” and “Hanging a bath towel on an overhead pole with both hands”; consequently, these items were excluded from ASUHS.
Discrimination. All 227 remaining items in ASUHS showed acceptable discrimination parameters (>0.5).
Content Validity. The ASUHS items were revised based on feedback from the five stroke rehabilitation experts. In particular, items representing activities performed less frequently in daily life and those similar to other items, e.g., “Pressing the button of the washing machine,” “Putting body soap on a towel and lathering,” “Pinching a clothespin to open and close it,” and “Wringing out a cloth,” were deleted. Each category B item in ASUHS was structured to contain four category C items. For example, category B item “using a rice bowl” was divided into four items in category C: “holding a rice bowl on the table,” “lifting a rice bowl in the air,” “holding a rice bowl at chest height,” and “carrying a rice bowl to the mouth.” After revisions, ASUHS was reduced to 168 items. Furthermore, two ASUHS scales were created: one scale consisted of 168 items performed by the affected dominant hand (ASUHS Dominant hand scale; ASUHS-D), and the other scale consisted of a subset of 116 of the overall 168 items performed by the affected non-dominant hand (ASUHS Non-Dominant hand scale; ASUHS-ND) (see Appendix). There were no significant differences between the dominant and non-dominant hand paralysis groups except for the time after stroke (Table 1). The five experts made positive comments regarding the relevance and comprehensiveness of the scale, suggesting the validity of the content.
Reliability
Internal Consistency. Cronbach’s α coefficient was 0.99 for both ASUHS-D and ASUHS-ND. Furthermore, in ASUHS-D, Cronbach’s α for each category B item (42 categories) ranged from 0.96 to 0.99, and in ASUHS-ND, Cronbach’s α for each category B item (29 categories) ranged from 0.95 to 0.99.
Inter-rater Reliability. Subjects were randomly selected, and inter-rater reliability was assessed in 8 of 78 participants for ASUHS-D and 7 of 67 participants for ASUHS-ND. Regarding assessment of the characteristics of the subjects, Fugl-Meyer assessment was 40.1 ± 21.8 and 41.3 ± 18.9 and that of ASUHS was 2.4 ± 1.0 for ASUHS-D and 2.1 ± 1.0 for ASUHS-ND. Cohen’s Kappa coefficients were 0.74 for ASUHS-D and 0.75 for ASUHS-ND, indicating good inter-rater reliability for both scales.
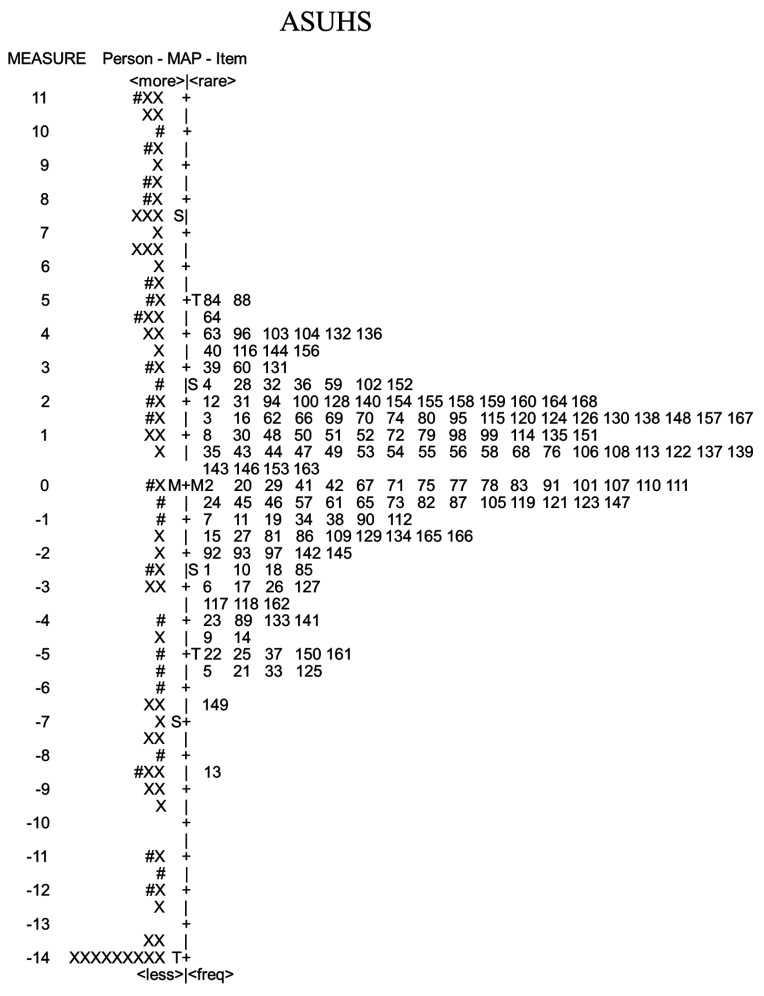
Hierarchies of Item Difficulties. The item calibrations in the Rasch analysis of ASUHS ranged from +5.18 logit for the most difficult item (brushing teeth) to –8.71 logit for the least difficult item (holding a plastic bottle). Rasch analysis places item difficulty and person ability along the linear continuum of the logit scale.34) A person–item map displaying the ASUHS item difficulty and the subjects’ ability is shown in Fig. 3. The mean value of item difficulty is located at 0 logit on the person–item map. The mean value of person ability in terms of ASUHS was located at –1.57 logit on the person–item map.
Fig. 3.
Person–item map of ASUHS. Persons are to the left of the vertical “– + – +” line, and the item difficulty map is to the right of the line. Item numbers listed here correspond to the item numbers shown in the Appendix. X, two people; #, one person; S, one standard deviation from the mean; T, two standard deviations from the mean; M, mean.
DISCUSSION
ASUHS Verification
ASUHS showed unidimensionality by PCA and high compatibility with the Rasch model by Rasch analysis. High discrimination and content validity were shown for all items, and the objectivity of the results of ASUHS-D and ASUHS-ND was sufficient. Furthermore, the 168 items of ASUHS-D and the 116 items of ASUHS-ND showed good internal consistency. The Kappa coefficients for inter-rater reliability of ASUHS-D and ASUHS-ND were 0.74 and 0.75, respectively, indicating that high reliability was obtained with “substantial agreement.”33) These results supported the clinical use of ASUHS in patients with stroke. However, the inter-rater reliability of ASUHS was lower than that obtained in patients with stroke using well-established clinical scales for the upper limb [Fugl-Meyer assessment: intraclass correlation coefficient (ICC) = 0.99,35) Action Research Arm Test: ICC = 0.9936)]. The Kappa coefficient should be increased by the provision of an instruction manual that clearly describes the evaluation criteria for each item.
ASUHS Items
In the Rasch analysis, 24 of 251 category C items that did not fit the Rasch model were excluded. Those excluded tended to be items with a very low difficulty, such as “Holding a cup on the table,” “Holding a spoon,” and “Holding a hair dryer,” or items with a very high difficulty, such as “Picking up a 1.5-cm marble with chopsticks and carrying it to the mouth,” “Writing your name on 10-mm graph paper,” and “Hanging a bath towel on an overhead pole with both hands.” According to systematic reviews, MAL is often used to evaluate daily activities performed by the affected arm of patients with stroke.7,9,10) MAL evaluates daily activities in 30 categories, whereas ASUHS evaluates daily activities in 42 categories. Although MAL evaluates the degree of performance of the daily activities themselves, therapists have difficulty in determining which process in the activities might be causing difficulty. ABILHAND indicates the difficulty of 23 daily activities by Rasch analysis and can compare the difficulties. In contrast, ASUHS divides each activity into four concrete processes and shows the difficulty of each process. With ASUHS, the concrete steps that are difficult for a patient when attempting an intended daily activity can be clarified, and therapists can identify the process that should be the next focus for training. Although ASUHS contains many items (with some not being performed, depending on the subject’s ability), it took about 30–60 min to perform all items in ASUHS. Although it is acceptable to assess only subcategories of ASUHS, further research based on item response theory is required to enable estimation of the training content according to the patient’s upper limb function and ability of activities of daily living even when selectively performing assessment items. We will conduct a future study in which the abilities of the subjects and the process of the daily activities that should be the next focus for training can be understood by performing a few selected items, rather than all items. ASUHS includes activities that differ depending on culture. For example, “holding a rice bowl in the air” is a typical task performed in Japan that may not generally be done elsewhere. Few items with such cultural specificity are evaluable with the existing scales. Therefore, one strength of ASUHS is that it includes items related to cultural differences that are difficult to evaluate with existing scales. However, differences in cultural behaviors limit the generalization of ASUHS to other cultures. Therefore, when using ASUHS, activities that are not performed in a certain culture should not be evaluated.
Item Difficulty and Person Ability
Rasch analysis places items and persons along the same linear continuum: if no items are located in the vicinity of the persons’ level of ability or if important gaps exist between the items’ difficulty levels, the ability of these patients cannot be estimated with precision.22) Item difficulty level in ASUHS ranged from –8.71 to +5.18 logit, and no important gaps existed between the items’ difficulty levels (Fig. 3). Therefore, the ability of patients can be estimated with precision using ASUHS. Furthermore, if the distribution ranges of an individual attribute and item difficulty are similar, item difficulty can be considered adequate.37)Figure 3 shows that the range of distribution of a person’s ability level was wider than that of the item difficulty distribution; the reason for this was that subjects who could not move the affected arm at all and those with little paresis were both included. Ceiling effects and floor effects were therefore found in the present study. Consequently, in the future, the functional level of affected arms that are evaluable using ASUHS must be clarified by investigating the range of Fugl-Meyer scores of subjects evaluable by ASUHS.
Item Difficulty Hierarchies
In ASUHS, the most difficult item to perform with the dominant hand was “brushing the teeth,” and the next most difficult item was “wiping the bottom with toilet paper.” In contrast, the most difficult activities for the non-dominant hand were “washing the head” and then “washing the face with water held in both hands.” Although there were differences in the activities performed between the dominant and non-dominant hands, items with a high level of difficulty were common in operations of the arm in the upper space higher than chest level and in movement using multiple joints. The items with the least difficulty were “holding a plastic bottle” followed by “holding a rice bowl on a table.” Items with less difficulty were common to the behavior of grasping something and to movement performed on a desk or in a low position. Because upward elevation of the arm and separation movement accompanied by multi-joint movement appear later in the recovery process of motor paresis after stroke,11) these actions have a high degree of difficulty. In the fingers, flexion movement often appears before extension movement, and all-finger flexion appears before separation movements of the individual fingers such as pinching.12) Therefore, grasping something with all fingers flexed is considered to be an item with less difficulty. The above findings suggested that the range of item difficulties of ASUHS was appropriate. Subjects with severe cognitive impairment who could not follow directions were excluded, but subjects with mild and moderate cognitive impairments, such as inattention, aphasia, and apraxia, were not excluded. In addition to motor function, mild and moderate cognitive impairment, aphasia, and apraxia may affect the performance of the daily activities performed with the affected arm. Because these effects were not completely eliminated in this study, additional research is required.
The existing scales used to evaluate affected arm function in stroke patients have difficulty in indicating the process of a daily activity that should be targeted next. However, with ASUHS, the specific process of a daily activity that should be able to be performed next is clarified for both patients and therapists because ASUHS clarifies the difficulty level of the daily activities performed by the affected arm. For example, if a patient performs “Lifting a plastic bottle without water in the air (–4.58 logit),” the next step should be to perform “Lifting a cup without water in the air (–4.58 logit),” with the same difficulty level or to begin training for the next goal at the next highest difficulty level, e.g., “Wetting hands with running water (–3.99 logit)” or “Holding the handle of a kettle (–3.92 logit).”
Clinical Implications of the ASUHS Scale
In rehabilitation, using an appropriate difficulty level is important when selecting a training program and setting goals.13,14) However, it is difficult to determine which processes within daily activities should be the next focus for training because it is challenging for therapists to know the difficulty of the daily activities performed with an affected arm; consequently, practice programs are usually selected empirically. Moreover, it is difficult for patients to know what daily activities can be performed with the affected hand or what process they will be able to perform next. Consequently, these issues make shared decision making38) between the therapist and the patient even more difficult. We therefore developed ASUHS, in which many daily activities are divided into small concrete steps, to objectively evaluate in detail how well these steps are performed with the affected arm. ASUHS has several advantages: (1) many daily activities and their specific processes can be evaluated in detail; (2) the difficulty levels of these activities are known, and it is therefore easy to determine which processes within daily activities should be the next focus for training; (3) even inexperienced therapists can recognize the functional level of the affected arm and the daily activities that can be performed with it; (4) patients can know the process they will be able to perform next; (5) sharing the results of ASUHS with patients encourages them to become conscious of using their hands in daily activities; and (6) patients are more motivated to perform rehabilitation because they know exactly which daily activities can be achieved. ASUHS allows the therapist to directly assess the patient’s desired daily activities and can support decision making between the therapist and the patient regarding the program. In the next stage of ASUHS research, instead of reducing the items of ASUHS, we will develop a shortened version that will make it possible to estimate the items of the entire ASUHS so that it can be applied clinically.
Limitations
This study has a noteworthy limitation. Of the 512 patients evaluated for eligibility, only 145 participated. Although ASUHS can be applied to patients meeting the criteria of this study, it may be difficult to apply ASUHS to patients not meeting these criteria.
CONCLUSIONS
Few scales currently available to evaluate in detail the affected arm in stroke patients can be used both in performing many daily activities and to indicate the difficulty of the daily activities. We therefore developed ASUHS to objectively evaluate in detail the daily activities performable by an affected arm. The reliability and validity of ASUHS were preliminarily supported. ASUHS clarifies the difficulty level of the daily activities performed by the affected arm and indicates to therapists the specific processes of daily activities that the patient should be able to perform next. This study suggested that ASUHS may be a potentially useful clinical scale.
ACKNOWLEDGMENTS
We would like to thank Prof. Makoto Suzuki for providing us with thoughtful suggestions and ample support to complete this study. This study was supported by JSPS KAKENHI Grant Number JP18K17765 and a grant from Kitasato University School of Allied Health Sciences (Grant-in-Aid for Research Project, No. 2017-1061).
Footnotes
CONFLICTS OF INTEREST: The authors declare that there are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
APPENDIX. THE 168 ITEMS IN ASUHS-D AND THE 116 ITEMS IN ASUHS-ND
The 168 items (Table A1, A2, A3) are the items of ASUHS-D. The category B items indicated with an asterisk are excluded when the non-dominant hand is assessed. ASUHS-D, Activities Specific Upper-extremity Hemiparesis Scale-Dominant hand scale; ASUHS-ND, Activities Specific Upper-extremity Hemiparesis Scale-Non-Dominant hand scale; ADL, activities of daily living; IADL, instrumental activities of daily living.
Table A1. The 168 Items in ASUHS-D and 116 Items in ASUHS-ND: Items 1–56.
| Category A | Category B | Category C | Category A | Category B | Category C | ||
| ADL | Eating | Using a rice bowl | 1. Holding a rice bowl on a table | 32. Putting head through the shirt | |||
| 2. Lifting a rice bowl in the air | Taking off a pullover shirt | 33. Taking off the sleeve on the affected side | |||||
| 3. Holding a rice bowl at chest height | 34. Taking off the sleeve on the non-affected side | ||||||
| 4. Carrying a rice bowl to the mouth | 35. Grabbing the shirt from behind the neck | ||||||
| Drinking water from a plastic bottle | 5. Holding a plastic bottle | 36. Pulling off the shirt over the head | |||||
| 6. Lifting a plastic bottle without water in the air | Putting on pants | 37. Raising pants to the knees with both hands | |||||
| 7. Carrying a plastic bottle without water to the mouth | 38. Raising pants to the waist with both hands (help with standing position is acceptable) | ||||||
| 8. Carrying a plastic bottle containing water to the mouth | |||||||
| Drinking water with a cup | 9. Lifting a cup without water in the air | 39. Inserting the affected foot into the hem area with both hands (help with posture maintenance is acceptable) | |||||
| 10. Lifting a cup containing water in the air | |||||||
| 11. Carrying a cup without water to the mouth | 40. Inserting the non-affected foot into the hem area with both hands | ||||||
| 12. Carrying a cup containing water to the mouth | Taking off pants | 41. Pulling down pants to the thigh with both hands (help with standing position is acceptable) | |||||
| *Using a spoon | 13. Pretending to scoop food using a spoon | ||||||
| 14. Scooping up a 1-cm block using a spoon | 42. Pulling down pants to below the knee with both hands (help with standing position is acceptable) | ||||||
| 15. Carrying a spoon with 1-cm block to the mouth | |||||||
| 16. Carrying a spoon with 1.5-cm marble to the mouth | 43. Taking off pants over the non-affected foot with both hands | ||||||
| Dressing | Pulling up sleeve | 17. Pulling up sleeve until just below the elbow | 44. Taking off pants over the affected foot with both hands | ||||
| 18. Returning the pulled-up sleeve from just below the elbow | Putting on socks | 45. Pulling a sock to the non-affected heel with both hands | |||||
| 19. Pulling up sleeve to the upper arm | 46. Putting the non-affected toes into a sock with both hands | ||||||
| 20. Returning the pulled-up sleeve from the upper arm | 47. Pulling a sock to the affected heel with both hands | ||||||
| Putting on a front-opening shirt | 21. Passing affected arm through the sleeve | 48. Putting the affected toes into a sock with both hands | |||||
| 22. Passing affected arm through the sleeve to the shoulder | Taking off socks | 49. Taking a sock off the heel of the non-affected side with both hands | |||||
| 23. Moving clothes to the non-affected side from the back | 50. Taking a sock off the toes of the non-affected side with both hands | ||||||
| 24. Passing non-affected arm through the sleeve | 51. Taking a sock off the heel of affected side with both hands (help with posture maintenance is acceptable) | ||||||
| Taking off a front-opening shirt | 25. Taking off the sleeve on the affected side | ||||||
| 26. Pinching sleeve on the non-affected side with affected hand | 52. Taking a sock off the toes of the affected side with both hands (help with posture maintenance is acceptable) | ||||||
| 27. Taking off the sleeve on the non-affected side | |||||||
| 28. Moving clothes to the affected side from the back | Manipulating a zipper and buttons | 53. Unzipping a jacket | |||||
| Putting on a pullover shirt | 29. Putting the affected arm in the sleeve | 54. Zipping up a jacket | |||||
| 30. Putting the non-affected arm in the sleeve | 55. Unbuttoning a shirt | ||||||
| 31. Pulling down the hem | 56. Buttoning the shirt |
Table A2. The 168 Items in ASUHS-D and 116 Items in ASUHS-ND: Items 57–117.
| Category A | Category B | Category C | Category A | Category B | Category C | ||
| Tying a string | 57. Tying a string lightly on a desk | 88. Washing hands | |||||
| 58. Tying a string tightly on a desk | *Brushing the teeth | 89. Opening lid of toothpaste | |||||
| 59. Tying a string into a bowknot on a desk | 90. Squeezing toothpaste from the tube onto a toothbrush | ||||||
| 60. Tying a bowknot in a shoestring | 91. Putting the toothbrush into the mouth | ||||||
| Bathing | Handling a shower nozzle | 61. Taking a shower nozzle from the shower rack | 92. Brushing the teeth | ||||
| 62. Hanging the shower nozzle on the shower rack | Washing the face | 93. Holding water in both hands | |||||
| 63. Handling the shower nozzle and spraying the entire body | 94. Wiping the face with a towel | ||||||
| 64. Handling the shower nozzle and spraying the entire head | 95. Putting water on the face with both hands | ||||||
| Wiping the body with a towel | 65. Wiping both legs with a towel | 96. Washing the face with water held in both hands | |||||
| 66. Wiping the non-affected arm with a towel | Doing the laundry | *Doing the laundry | 97. Holding a basket containing laundry | ||||
| 67. Wiping the front of the trunk with a towel | 98. Putting the laundry in the washing machine | ||||||
| 68. Wiping the back with a towel using both hands | 99. Putting detergent into the washing machine after scooping the detergent with a measuring cup | ||||||
| Washing the body | 69. Rubbing both legs with a towel | ||||||
| 70. Rubbing the non-affected arm with a towel | 100. Taking the laundry out of the washing machine | ||||||
| 71. Rubbing the front of the trunk with a towel | *Ironing | 101. Ironing out wrinkles in a handkerchief with an iron | |||||
| 72. Rubbing the back with a towel using both hands | 102. Placing clothes on the ironing board | ||||||
| Washing and drying the hair | 73. Squeezing the contents out of a shampoo bottle | 103. Ironing out wrinkles in clothes with an iron | |||||
| 74. Drying the hair with a hair dryer | 104. Operating an iron’s temperature control switch | ||||||
| 75. Wiping the entire head with a towel | Folding the laundry | 105. Folding a towel | |||||
| 76. Washing the entire head | 106. Folding a pullover shirt | ||||||
| Toileting | Opening and closing a door | 77. Pulling a hinged door | 107. Folding pants | ||||
| 78. Pushing a hinged door | 108. Folding a front-opening shirt | ||||||
| 79. Pulling a sliding door | Hanging out the laundry | 109. Hanging the laundry on a hanger | |||||
| 80. Turning a key | 110. Hanging laundry on a hanger on a pole at face height | ||||||
| *Wiping the buttocks | 81. Pulling out toilet paper | 111. Pinning laundry with a clothespin at face height | |||||
| 82. Tearing toilet paper | 112. Hanging a bath towel on a pole at face height | ||||||
| 83. Folding up toilet paper | Communicating | *Operating a PC | 113. Moving the mouse | ||||
| 84. Wiping the buttocks (help in raising the buttocks is acceptable) | 114. Clicking the mouse | ||||||
| Grooming | Washing hands | 85. Wetting hands with running water | 115. Pressing one character key | ||||
| 86. Opening and closing a lever-type faucet | 116. Entering your name | ||||||
| 87. Turning the faucet | *Calling | 117. Picking up the handset |
Table A3. The 168 Items in ASUHS-D and 116 Items in ASUHS-ND: Items 118–168.
| Category A | Category B | Category C | Category A | Category B | Category C | ||
| 118. Pressing the buttons to enter a phone number | *Handling a kitchen knife | 145. Moving a kitchen knife back and forth to imitate cutting | |||||
| 119. Holding the handset to the ear | 146. Cutting clay in two with a kitchen knife | ||||||
| 120. Talking while holding the handset to the ear | 147. Cutting clay at 3-cm intervals with a kitchen knife | ||||||
| Reading | 121. Holding a book open on a desk | 148. Cutting clay at 5-mm intervals with a kitchen knife | |||||
| 122. Turning a page of a book on a desk | Shopping | Handling shopping baskets and carts | 149. Holding a shopping cart handle with both hands | ||||
| 123. Opening and holding a book with both hands in the air | 150. Holding an empty shopping basket | ||||||
| 124. Turning a page while holding a book with both hands | 151. Placing a shopping basket containing a 1-kg weight on a desk | ||||||
| *Writing | 125. Picking up a pen on a desk and holding it properly | 152. Placing a shopping basket containing a 3-kg weight on a desk | |||||
| 126. Drawing horizontal and vertical lines | *Dealing with money | 153. Picking up coins and bills on a desk | |||||
| 127. Drawing a circle | 154. Putting coins and bills in and taking them out of a wallet | ||||||
| 128. Writing your name | 155. Taking the change from a vending machine | ||||||
| Cooking | *Opening and closing a lid | 129. Opening and closing an opened jam bottle lid (5 cm in diameter) | 156. Inserting coins into a vending machine | ||||
| 130. Opening and closing an opened plastic bottle lid | Cleaning | Wiping things clean | 157. Moving a cloth back and forth to wipe a desk | ||||
| 131. Opening the seal of a freezer bag | 158. Moving a cloth to the left and right to wipe a desk | ||||||
| 132. Peeling off the wrapping on a container | 159. Wiping a window lower than the face | ||||||
| Handling a pot | 133. Holding an empty two-handed pot with both hands | 160. Wiping a window higher than the face | |||||
| 134. Holding a two-handed pot containing water with both hands | Putting things in and taking them out | 161. Opening a drawer | |||||
| 135. Holding a one-handed pot filled with water | 162. Closing a drawer | ||||||
| 136. Pouring water from a one-handed pot into a dish | 163. Taking a note out of a drawer | ||||||
| Handling a kettle | 137. Holding the handle of a kettle | 164. Putting a book on a bookshelf | |||||
| 138. Lifting the kettle | *Cleaning | 165. Wiping the floor with a floor wiper | |||||
| 139. Moving the kettle to the cup | 166. Sweeping the floor with a broom | ||||||
| 140. Tilting the kettle over the cup to pour water | 167. Handling a stick-type vacuum cleaner | ||||||
| *Washing the dishes | 141. Holding detergent container and applying detergent to the sponge | 168. Handling a standard vacuum cleaner | |||||
| 142. Washing dishes with a sponge | |||||||
| 143. Rinsing the dishwashing detergent with water | |||||||
| 144. Washing a pot and pan with a sponge |
REFERENCES
- 1.Wolf SL,Thompson PA,Winstein CJ,Miller JP,Blanton SR,Nichols-Larsen DS,Morris DM,Uswatte G,Taub E,Light KE,Sawaki L: The EXCITE stroke trial: comparing early and delayed constraint-induced movement therapy. Stroke 2010;41:2309–2315. 10.1161/STROKEAHA.110.588723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Takahashi K,Domen K,Sakamoto T,Toshima M,Otaka Y,Seto M,Irie K,Haga B,Takebayashi T,Hachisuka K: Efficacy of upper extremity robotic therapy in subacute poststroke hemiplegia an exploratory randomized trial. Stroke 2016;47:1385–1388. 10.1161/STROKEAHA.115.012520 [DOI] [PubMed] [Google Scholar]
- 3.Yavuzer G,Selles R,Sezer N,Sütbeyaz S,Bussmann JB,Köseoğlu F,Atay MB,Stam HJ: Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 2008;89:393–398. 10.1016/j.apmr.2007.08.162 [DOI] [PubMed] [Google Scholar]
- 4.Morris DM,Taub E,Mark VW: Constraint-induced movement therapy: characterizing the intervention protocol. Eura Medicophys 2006;42:257–268. [PubMed] [Google Scholar]
- 5.Wade DT,Collin C: The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud 1988;10:64–67. 10.3109/09638288809164105 [DOI] [PubMed] [Google Scholar]
- 6.Granger CV,Hamilton BB,Linacre JM,Heinemann AW,Wright BD: Performance profiles of the functional independence measure. Am J Phys Med Rehabil 1993;72:84–89. 10.1097/00002060-199304000-00005 [DOI] [PubMed] [Google Scholar]
- 7.Ashford S,Slade M,Malaprade F,Turner-Stokes L: Evaluation of functional outcome measures for the hemiparetic upper limb: a systematic review. J Rehabil Med 2008;40:787–795. 10.2340/16501977-0276 [DOI] [PubMed] [Google Scholar]
- 8.Bhakta BB,Cozens JA,Chamberlain MA,Bamford JM: Impact of botulinum toxin type A on disability and carer burden due to arm spasticity after stroke: a randomised double blind placebo controlled trial. J Neurol Neurosurg Psychiatry 2000;69:217–221. 10.1136/jnnp.69.2.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taub E,Miller NE,Novack TA,Cook EW 3rd,Fleming WC,Nepomuceno CS,Connell JS,Crago JE: Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil 1993;74:347–354. [PubMed] [Google Scholar]
- 10.Penta M,Tesio L,Arnould C,Zancan A,Thonnard JL: The ABILHAND questionnaire as a measure of manual ability in chronic stroke patients: Rasch-based validation and relationship to upper limb impairment. Stroke 2001;32:1627–1634. 10.1161/01.STR.32.7.1627 [DOI] [PubMed] [Google Scholar]
- 11.Fugl-Meyer AR,Jääskö L,Leyman I,Olsson S,Steglind S: The post-stroke hemiplegic patient. 1. A method for evaluation of physical performance. Scand J Rehabil Med 1975;7:13–31. [PubMed] [Google Scholar]
- 12.Brunnstrom S: Movement Therapy in Hemiplegia. Harper and Row, New York, 1970. [Google Scholar]
- 13.Medical Advisory Secretariat, Health Quality Ontario: Constraint-induced movement therapy for rehabilitation of arm dysfunction after stroke in adults: an evidence-based analysis. Ont Health Technol Assess Ser 2011;11:1–58. www.hqontario.ca/en/mas/tech/pdfs/2011/rev_CIMT_November.pdf Accessed 18Nov2020 [Internet] [PMC free article] [PubMed] [Google Scholar]
- 14.Locke EA,Latham GP: The development of goal setting theory: a half century retrospective. Motiv Sci 2019;5:93–105. 10.1037/mot0000127 [DOI] [Google Scholar]
- 15.Kooijman MK,Swinkels IC,Veenhof C,Spreeuwenberg P,Leemrijse CJ: Physiotherapists’ compliance with ankle injury guidelines is different for patients with acute injuries and patients with functional instability: an observational study. J Physiother 2011;57:41–46. 10.1016/S1836-9553(11)70006-6 [DOI] [PubMed] [Google Scholar]
- 16.Mokkink LB,Terwee CB,Patrick DL,Alonso J,Stratford PW,Knol DL,Bouter LM,de Vet HC: The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 2010;19:539–549. 10.1007/s11136-010-9606-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mokkink LB,Terwee CB,Patrick DL,Alonso J,Stratford PW,Knol DL,Bouter LM,de Vet HC: COSMIN Checklist Manual. Executive Board of VU University Amsterdam, Amsterdam, 2010. [Google Scholar]
- 18.Suzuki M,Yamada S,Shimizu Y,Kono Y,Hirashiki A,Izawa H,Murohara T: Development of the participation scale for patients with congestive heart failure. Am J Phys Med Rehabil 2012;91:501–510. 10.1097/PHM.0b013e31824ad653 [DOI] [PubMed] [Google Scholar]
- 19.Jackson A,Rogerson M,Le Grande M,Thompson D,Ski C,Alvarenga M,Amerena J,Higgins R,Raciti M,Murphy BM: Protocol for the development and validation of a measure of persistent psychological and emotional distress in cardiac patients: the Cardiac Distress Inventory. BMJ Open 2020;10:e034946. 10.1136/bmjopen-2019-034946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawton MP,Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–186. 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- 21.Holbrook M,Skilbeck C: An activities index for use with stroke patients. Age Ageing 1983;12:166–170. 10.1093/ageing/12.2.166 [DOI] [PubMed] [Google Scholar]
- 22.Forget NJ,Jerosch-Herold C,Shepstone L,Higgins J: Psychometric evaluation of the Disabilities of the Arm, Shoulder and Hand (DASH) with Dupuytren’s contracture: validity evidence using Rasch modeling. BMC Musculoskelet Disord 2014;15:361–372. 10.1186/1471-2474-15-361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stroke – 1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989;20:1407–1431. 10.1161/01.STR.20.10.1407 [DOI] [PubMed] [Google Scholar]
- 24.Vellas B,Gauthier S,Allain H,Andrieu S,Aquino JP,Berrut G,Berthel M,Blanchard F,Camus V,Dartigues JF,Dubois B,Forette F,Franco A,Gonthier R,Grand A,Hervy MP,Jeandel C,Joel ME,Jouanny P,Lebert F,Michot P,Montastruc JL,Nourhashemi F,Ousset PJ,Pariente J,Rigaud AS,Robert P,Ruault G,Strubel D,Touchon J,Verny M,Vetel JM: Consensus statement on dementia of Alzheimer type in the severe stage. J Nutr Health Aging 2005;9:330–338. [PubMed] [Google Scholar]
- 25.Halligan PW,Cockburn J,Wilson BA: The behavioural assessment of visual neglect. Neuropsychol Rehabil 1991;1:5–32. 10.1080/09602019108401377 [DOI] [Google Scholar]
- 26.Chang WC,Chan C: Rasch analysis for outcomes measures: some methodological considerations. Arch Phys Med Rehabil 1995;76:934–939. 10.1016/S0003-9993(95)80070-0 [DOI] [PubMed] [Google Scholar]
- 27.Franchignoni F,Godi M,Guglielmetti S,Nardone A,Giordano A: Enhancing the usefulness of the Mini-BESTest for measuring dynamic balance: a Rasch validation study. Eur J Phys Rehabil Med 2015;51:429–437. [PubMed] [Google Scholar]
- 28.Kielhofner G,Forsyth K,Kramer J,Iyenger A: Developing the Occupational Self Assessment: the use of Rasch analysis to assure internal validity, sensitivity and reliability. Br J Occup Ther 2009;72:94–104. 10.1177/030802260907200302 [DOI] [Google Scholar]
- 29.Linacre JM: A User’s Guide to Winsteps Ministep: Rasch-model Computer Programs. Winsteps, Chicago, 2009. [Google Scholar]
- 30.Yazdani K,Nedjat S,Karimlou M,Zeraati H,Mohammad K,Fotouhi A: Developing a Shortened Quality of Life Scale from Persian Version of the WHOQOL-100 using the Rasch analysis. Iran J Public Health 2015;44:522–534. [PMC free article] [PubMed] [Google Scholar]
- 31.Shen M,Hu M,Sun Z: Development and validation of brief scales to measure emotional and behavioural problems among Chinese adolescents. BMJ Open 2017;7:e012961. 10.1136/bmjopen-2016-012961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen JA: Coefficient of Agreement, a Psychological and Statistical Study Based upon the Block-design Tests. Macmillan, New York, 1923. [Google Scholar]
- 33.Landis JR,Koch GG: The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 34.Ardolino EM,Hutchinson KJ,Pinto Zipp G,Clark M,Harkema SJ: The ABLE scale: the development and psychometric properties of an outcome measure for the spinal cord injury population. Phys Ther 2012;92:1046–1054. 10.2522/ptj.20110257 [DOI] [PubMed] [Google Scholar]
- 35.See J,Dodakian L,Chou C,Chan V,McKenzie A,Reinkensmeyer DJ,Cramer SC: A standardized approach to the Fugl-Meyer assessment and its implications for clinical trials. Neurorehabil Neural Repair 2013;27:732–741. 10.1177/1545968313491000 [DOI] [PubMed] [Google Scholar]
- 36.Platz T,Pinkowski C,van Wijck F,Kim IH,di Bella P,Johnson G: Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil 2005;19:404–411. 10.1191/0269215505cr832oa [DOI] [PubMed] [Google Scholar]
- 37.Park EY,Choi YI: Rasch analysis of the London Handicap Scale in stroke patients: a cross-sectional study. J Neuroeng Rehabil 2014;11:114. 10.1186/1743-0003-11-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Charles C,Gafni A,Whelan T: Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Soc Sci Med 1997;44:681–692. 10.1016/S0277-9536(96)00221-3 [DOI] [PubMed] [Google Scholar]