Abstract
BACKGROUND
There is recently a concern regarding the reinfection and reactivation of previously reCoVered coronavirus disease 2019 (CoVID-19) patients.
AIM
To summarize the recent findings and reports of CoVID-19 reinfection in patients previously reCoVered from the disease.
METHODS
This study was a systematic review of current evidence conducted in August 2020. The authors studied the probable reinfection risk of novel coronavirus (CoVID-19). We performed a systematic search using the keywords in online databases. The investigation adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to ensure the reliability and validity of this study and results.
RESULTS
We reviewed 31 studies. Eight studies described reCoVered patients with reinfection. Only one study reported reinfected patients who died. In 26 studies, there was no information about the status of the patients. Several studies indicated that reinfection is not probable and that post-infection immunity is at least temporary and short.
CONCLUSION
Based on our review, we concluded that a positive polymerase chain reaction retest could be due to several reasons and should not always be considered as reinfection or reactivation of the disease. Most relevant studies in positive retest patients have shown relative and probably temporary immunity after the reCoVery of the disease.
Keywords: Reactivation, Reinfection, Postinfection, Coronavirus, CoVID-19, SARS-CoV-2
Core Tip: The reinfection in patients reCoVered from coronavirus disease 2019 (CoVID-19) could create a serious challenge in tackling the CoVID-19 pandemic as the reCoVered patients could be a source of virus spread in society. Previous studies have found a positive viral ribonucleic acid test in some of the discharged CoVID-19 patients 10 to 27 d after reCoVery. Recurrence of CoVID-19 after reCoVery should be differentiated from secondary medical conditions such as super infection, pulmonary embolism, or persistent ribonucleic acid virus that can be disCoVered in respiratory specimens in clinically cured CoVID-19 patients. This review aims to assist a systematic compilation of severe acute respiratory syndrome coronavirus 2 reactivation in reCoVered CoVID-19 patients.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a new strain of coronavirus, causes coronavirus disease 2019 (CoVID-19), which was first reported in China in late 2019 and then spread rapidly worldwide[1-5]. The symptoms of CoVID-19 are high temperature, dry cough, shortness of breath, headache, tiredness, loss of taste or smell, and gastrointestinal symptoms such as diarrhea, anorexia, nausea, and abdominal pain[6-8]. Increased liver enzyme and low counts of lymphocytes (lymphocytopenia) along with increased C-reactive protein (CRP) levels are often present in CoVD-19 patients[9]. It could eventually lead to acute respiratory distress syndrome (ARDS) and death[1,10,11]. Although there is currently no certainty in virus biological behavior and risk of recurrence in the human body, recent studies reported evidence of the virus reactivation following an asymptomatic CoVID-19 infection in a small group of patients[1,12,13].
The risk factors of SARS-CoV-2 reactivation are related to the type of immuno-suppressive therapies, factors in the host such as older age, gender, underlying diseases such as diabetes, heart disease, obesity, cancer, and virologic factors[1,14]. Some viruses such as varicella-zoster can remain dormant in host cells for some time, not causing any illness and then reactivate and cause the disease. Recent evidence indicates that SARS-CoV-2 could present similar behavior and reactivate in patients with previously confirmed CoVID-19 infection and cause illness and person-to-person transmission[15].
Recent studies reported that some reCoVered CoVID-19 patients tested positive for virus nucleic acid again[16,17]. Elderly people with comorbidities are more likely to present with CoVID-19 reinfection[18]. Studies suggested that there are three major mechanisms for the reinfection of CoVID-19, including short-lived, ineffective, and strain-specific immune response[19,20].
The gold standard test for diagnosing SARS-CoV-2 infection is nasopharyngeal swab. Swabs from patients who reCoVered from CoVID-19 infection are negative, indicating full reCoVery from CoVID-19 infection. However, a certain number of individuals could be a false negative[17,18], because the samples for identifying SARS-CoV-2 viral load depend on the result of reverse transcription polymerase chain reaction (RT-PCR). SARS-CoV-2 uses angiotensin-converting enzyme-2 (ACE-2) as the receptor for cellular entry. The expression of ACE2 protein in the lungs is more than that in the upper respiratory tract. Therefore, it is important from which site the sample was taken in a patient with CoVID-19, as it may cause false-negative RT-PCR results[21].
In recent studies, SARS-CoV-2 was detected in fecal and sputum specimens of patients who were discharged from the hospital with a negative pharyngeal swab after a couple of weeks[17,22]. In other coronavirus pandemics such as Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), immunoglobulin levels in patients lasted for a minimum of 2 years, indicating that patients could be vulnerable to reinfection after 3 years[23,24]. The tests that detect SARS-CoV-2 genetic material are very sensitive; however, in patients who have reCoVered from CoVID-19, virus fragments can persist in the body and can be detected by the test. This should not be considered as a new infection[23].
The reinfection in patients reCoVered from CoVID-19 could create a serious challenge in tackling the CoVID-19 pandemic as the reCoVered patients could be a source of virus spread in society[19]. Previous studies have found a positive viral ribonucleic acid (RNA) test in some discharged CoVID-19 patients 10 to 27 d after reCoVery[1,19]. Recurrence of CoVID-19 after reCoVery should be differentiated from secondary medical conditions such as super infection, pulmonary embolism, or persistent RNA virus that can be disCoVered in respiratory specimens in clinically cured CoVID-19 patients[25]. This review aims to provide a systematic compilation of SARS-CoV-2 reactivation in reCoVered CoVID-19 patients.
MATERIALS AND METHODS
This study was a systematic literature review of current evidence conducted in August 2020. The authors studied the probable reinfection risk of novel coronavirus (CoVID-19). Our study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to ensure the reliability and validity of this study and results.
Data sources
By application of a systematic search and using the keywords in the online databases including PubMed, Scopus, Web of Science, and Science Direct, we extracted all the relevant papers and reports published in English from December 2019 through August 2020. We included several combinations of keywords in the following orders to conduct the search strategy: (1) “Coronavirus” or “CoVID-19” or “SARS-CoV-2” or “Novel Coronavirus” or “2019-nCoV” [Title/Abstract]; (2) “Reactivation” or “Reinfection” or “Postinfection” [Title/Abstract]; and (1) and (2).
Study selection
Three independent investigators retrieved the studies that were the most relevant by titles and abstracts. Subsequently, the full text of the retrieved papers was reviewed and the most relevant papers were chosen according to the eligibility criteria. Then, we extracted the relevant data and organized them in Tables. The original papers that were peer-reviewed and published in English and fulfilled the eligibility criteria were included in the final report.
We considered the exclusion criteria for this study as follows: (1) Papers conveying non-human studies including in vitro observations or articles focusing on animal experiments, or discussing CoVID-19 as a whole subject, without citation of the keywords of this study; (2) Papers in which their full text were out of access; and (3) Any suspicious and duplicated results in the databases.
Data extraction
After summarizing, we transferred the information of the authors, type of article (e.g., case reports), publication date, country of origin, sample size, age, gender, and clinical symptoms to a data extraction sheet. Two independent investigators collected this information and subsequently organized them in the Tables. Finally, to ensure no duplications or overlap exist in the content, all the selected articles were cross-checked by other authors.
Quality assessment
As aforementioned, we applied the PRISMA checklist to ensure the quality and reliability of selected articles. Two independent researchers evaluated the consistency and quality of the articles and the bias risk. In either case of discrepancy in viewpoints, a third independent researcher resolved the issue. The full text of selected articles was fully read, and the key findings were extracted.
RESULTS
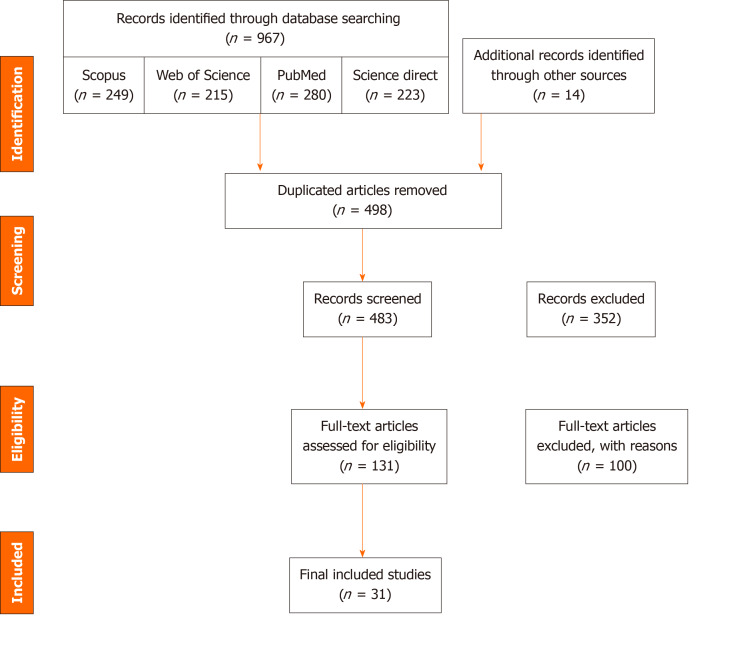
In this study, 981 documents were identified using a systematic search strategy. After a primary review of retrieved articles, 498 duplicates were removed, and the title and abstract of the remaining 483 resources were reviewed. After applying the selection criteria, 552 articles were excluded, and only 31 articles met the inclusion criteria and were included in the final review (Figure 1).
Figure 1.
Flow diagram for the selection process of identified articles.
We have reviewed 35 studies. Eight studies described reCoVered patients with reinfection. Only one study reported reinfected patients who died. In 26 studies, there was no information about the status of the patients (Table 1)[2,10,16,17,20,25-28,30-53].
Table 1.
Identified reinfection risk of novel coronavirus
| ID | Ref. | Type of study | Country | Study population |
Reinfection outcome
|
|||
|
ReCoVery
|
Death
|
Unknown
|
Other findings
|
|||||
| 1 | Alizargar et al[16] | Letter to the editor | South Korea | CoVID-19 patients | No | No | Yes | South Korea reported that 116 reCoVered cases of CoVID-19 were found positive again |
| 2 | Gousseff et al[25] | Letter to the editor | France | CoVID-19 patients | Yes | Yes | No | Between April 6 and May 14, 2020, 11 patients were identified (sex ratio M/F 1.2, median age 55, range 19-91 yr). The median duration of symptoms was 18 (13-41) d for the first episode and 10 d for the second one for the 7 patients who eventually reCoVered |
| 3 | Chaturvedi et al[20] | Review | South Korea | CoVID-19 patients | No | No | Yes | Concerning reports released from the Korea Centers for Disease Control and Prevention (KCDC) have noted that up to 163 patients who were presumed to have reCoVered from SARS-CoV-2 infection ended up testing positive with PCR testing yet again |
| 4 | Gomez-Mayordomo et al[30] | Short communication | Spain | A case study in a patient with relapsing-remitting MS treated with fingolimod | No | No | Yes | This case suggests that discontinuation of fingolimod during CoVID-19 could imply a worsening of SARS-CoV-2 infection. No information about reinfection |
| 5 | Hageman et al[31] | Editorial | United States | CoVID-19 in children | Yes | No | No | Limited data suggest that reCoVery might confer immunity |
| 6 | Hoang et al[32] | Letter to the editor | France | Patients reCoVered from CoVID-19 | No | No | Yes | Recurrence of SARS-CoV-2 in patients who had reCoVered from CoVID-19 has been described. However, it is possible that recurrences could actually be persistent infections in which the PCR resulted falsely negative at discharge |
| 7 | Inamo et al[33] | Letter of biomedical and clinical research | Japan | CoVID-19 patients | No | No | Yes | - |
| 8 | Islam et al[34] | Review article | Bangladesh | CoVID-19 patients | No | No | Yes | There is a possibility of reinfection as the humoral immunity weakens over time |
| 9 | Kang et al[26] | Commentary | China | CoVID-19 patients | No | No | Yes | ReCoVered patients become retest positive due to false-negative PCR or patients did not completely meet discharge criteria or due to dead viruses |
| 10 | Kannan et al[35] | Review article | India | Gene study between SARS-CoV-2 and SARS-CoV-1 and batCoV and MERS-CoV | No | No | Yes | Many researchers observed that there is SARS-CoV-2 reinfection in the same treated patients |
| 11 | Karimi et al[36] | Letter to the editor | Iran | CoVID-19 patients | Yes | No | No | - |
| 12 | Kassa et al[37] | Analytic article | Botswana | CoVID-19 patients | No | No | Yes | Not related to our topic but it is said “reinfection” by the family of coronavirus is possible |
| 13 | Kellam et al[38] | Review article | United Kingdom | Patients with coronavirus infection | No | No | Yes | Immediate reinfection is not possible but reinfection of previously mild SARS-CoV-2 cases is a realistic possibility |
| 14 | Kirkcaldy et al[39] | Viewpoint | United States | CoVID-19 Patients | No | No | Yes | ReCoVery from CoVID-19 might confer immunity against reinfection, at least temporarily |
| 15 | Koks et al[40] | Commentary | Australia | CoVID-19 patients | No | No | Yes | No information related to our study except “the testing needs to be repeated several times as persons with negative tests could become positive the next day as a result of a new infection or there plication of the virus” |
| 16 | Law et al[27] | Letter to the editor | China/Hong Kong | Patients reCoVered from CoVID-19 | No | No | Yes | There is currently no supporting evidence for CoVID-19 reinfection after reCoVery but retest can be positive due to several reasons |
| 17 | Laxminarayan et al[41] | Perspective | India | CoVID-19 in children | No | No | Yes | Reinfection is not probable |
| 18 | Leslie et al[42] | Letter | United States | SARS-CoV-2 patients | No | No | Yes | Patients with past infection with other coronaviruses that cause common cold may have some immunity to SARS-CoV-2 |
| 19 | Luo et al[43] | Case report | China | Woman with CoVID-19 | Yes | No | No | - |
| 20 | Meca-Lallana et al[44] | Correspondence | Spain | CoVID-19 patients with MS | No | No | Yes | - |
| 21 | Okhuese et al[45] | Statistical | Nigeria | CoVID-19 patients | No | No | Yes | There is no secondary reinfection in reCoVered patients. However, some reports have shown there have been a few rare cases of reinfection |
| 22 | Omer et al[46] | Viewpoint | United States | CoVID-19 patients in the United States | No | No | Yes | True reinfection is unlikely |
| 23 | Ota et al[47] | In brief | United States | Rhesus monkeys | No | No | Yes | - |
| 24 | Ozdinc et al[48] | Statistical | Turkey | Turkish people infected with CoVID-19 | No | No | Yes | There is short term immunity |
| 25 | Roy et al[17] | Review | India | CoVID-19 patients | No | No | Yes | Reinfection with SARS-CoV-2 seems unlikely taking into consideration our knowledge. We must maintain vigilance during the convalescence period and must take into consideration the probability of genetic mutations, as observed, rather than reinfection by the same strain |
| 26 | Steinchen et al[49] | Case report | Germany | A case of rheumatoid arthritis and CoVID-19 patient | Yes | No | No | A case of rheumatoid arthritis and insufficient compensation is reported under long-term combination therapy with methotrexate and leflunomide. After going through CoVID-19 infection, a new adjustment was made to a tumor necrosis factor (TNF) blocker. No reactivation of the infection has occurred in the short period of time initiated by the initiated bDMARD (biologic disease-modifying antirheumatic drug) therapy after surviving CoVID-19 infection with positive antibody status. Biologic therapy without mandatory medical indication should not be performed to protect against SARS-CoV-2 infection |
| 27 | Ueffing et al[50] | Review | Germany | CoVID-19 patients | No | No | Yes | Seven human pathogenic coronaviruses have already been detected in humans, most of which can cause respiratory diseases, but occasionally also conjunctivitis and middle ear infections. Four of the previously known coronaviruses (229E, NL63, OC43, and HKU1) typically cause relatively minor symptoms in the context of human infection of the upper respiratory tract. SARS-CoV and the 2012 MERS-CoV lead to severe respiratory diseases and have a significant mortality rate. Experiences with other coronavirus infections (SARS and MERS) indicate that the immunity could persist for several years. Based on animal experiments, already acquired data on other coronavirus types and plausibility, it can be assumed that seroconverted patients have the immunity of limited duration and only a very low risk of reinfection |
| 28 | Verhagen et al[51] | Research study | England and Wales | CoVID-19 patients | No | No | Yes | Areas face disproportionate risks for CoVID-19 hospitalization pressures due to their socioeconomic differences and the demographic composition of their populations. Our flexible online dashboard allows policymakers and health officials to monitor and evaluate potential health care demand at a granular level as the infection rate and hospital capacity changes throughout the course of this pandemic. This agile knowledge is invaluable to tackle the enormous logistical challenges to re-allocate resources and target susceptible areas for aggressive testing and tracing to mitigate transmission |
| 29 | Waltuch et al[52] | Case reports | United States | Children with CoVID-19 infection | No | No | Yes | Patients presenting with CoVID-19 associated post-infectious cytokine release syndrome appear to present with prolonged fever (5 d or greater) and GI symptoms with or without rash. This syndrome may overlap with features of Kawasaki Disease and Toxic Shock Syndrome. Patients who present with this clinical picture should have frequent vital signs and will require admission due to the potential for rapid deterioration |
| 30 | Tao et al[28] | Research study | China | CoVID-19 patients | Yes | No | No | These results implied that the positive result is unlikely caused by the reinfection from others or the remained virus. Rather, it may derive from the remained virus transferred from the lower respiratory tract to the throat or nose with coughing. Accordingly, it is suggested that the specimen detection of bronchoalveolar lavage fluid from the lower respiratory tract should be used as the discharge criteria |
| 31 | Zhou et al[53] | Review | China | CoVID-19 patients | No | No | Yes | Re-fever and positive nucleic acid test after discharge from the hospital might be due to the biological characteristics of 2019-nCoV, and might also be related to the basic disease, clinical status, glucocorticoid use, sampling, processing, and detecting of patients, and some even related to the reinfection or secondary bacterial virus infection |
CoVID-19: Coronavirus disease 2019; F: Female; GI: Gastrointestinal; HBV: Hepatitis B virus; M: Male; MERS-CoV: Middle East respiratory syndrome-coronavirus; MS: Multiple sclerosis; PCR: Polymerase chain reaction; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2.
Several studies indicated that reinfection is not probable and that postinfection immunity is at least temporarily and short; however, other studies, particularly from South Korea and China, reported some reinfection cases. South Korea reported that 116 reCoVered cases of CoVID-19 were found to be positive again[16]. Another study from South Korea reported that up to 163 patients who were presumed to have reCoVered from SARS-CoV-2 ended up testing positive again[20]. Several studies from China do not support reinfection[26-29]. There is only one study from China that reported five cases of reactivation[5].
The results of the present study showed that there are many factors that we need to take into account about reinfection. Some cases may have resulted in a false negative at discharge or patients did not completely meet discharge criteria. Although we should not forget that reinfection could be possible, because some studies have shown humoral immunity weakens over time.
DISCUSSION
Due to the widespread expansion of the CoVID-19 epidemic around the world, there are more and more infected cases, and of course, many people have reCoVered from this viral infection. However, there is recently a concern regarding the reinfection in previously reCoVered SARS-CoV-2 patients. In the present review, we summarized the recent findings and reports of CoVID-19 reinfection in patients previously reCoVered from the disease. This is important to inform the public regarding the possible risk of reinfection to restrain the transmission of SARS-CoV-2 and control the current epidemic[25].
The findings from the current review of existing evidence suggest two possible scenarios for new infection in patients who were previously reCoVered from CoVD-19, including reinfection and reactivation. Studies have shown some cases of symptom recurrence such as fever, malaise, myalgia, and cough after discharge. The positive PCR test confirmed the infection and suggested reinfection. Although this has been attributed to the biological characteristics of CoVID-19 and other factors, such as underlying diseases, clinical status, glucocorticoid use, sample collection, patient detection, follow-up, and even secondary bacterial infection, it could be due to reinfection with CoVID-19[53,54]. Positive follow-up tests may also derive from the remained virus transferred from the lower respiratory tract to the throat and nose with coughing. Therefore, it is suggested that the fluid collected in the bronchoalveolar lavage of the lower respiratory tract should be tested and used as the discharge criteria in SARS-CoV-2 patients[28]. In fact, a retest can be positive due to several reasons; thus, it is difficult to distinguish between reinfection, reactivation, or other causes.
Among the reviewed studies, six studies emphasized short-term immunity following reCoVery[18,19,25,26,33,35]. One study indicated that the antibodies and the immunity could last about 40 d and that there is a possibility of reinfection or reactivation of latent infection after this period. Therefore, reCoVery from CoVID-19 might not confer immunity against reinfection forever[38,39]. Furthermore, previous studies related to other human coronavirus types suggested the possibility of reinfection by other members of the coronavirus family following reCoVery from a particular type[24]. Although there are previous studies that suggest the reinfection with SARS-CoV-2 is unlikely, we must maintain vigilance during the convalescence period and consider the probability of genetic mutations as observed rather than reinfection by the same strain[6,29,33,34].
The results of the present study showed that there are many factors that we need to take into account about reinfection. Some cases may have resulted in false negative at discharge or patients did not completely meet discharge criteria. We should not forget, however, that reinfection could be possible because some studies have shown humoral immunity weakens over time. The certainty regarding the reinfection in CoVID-19 patients is limited, and we strongly recommend further studies to explore the virological, immunological, and epidemiologic characteristics of SARS-CoV-2 to determine the biological behavior of the virus and describe the potential mechanisms of disease recurrences.
CONCLUSION
In conclusion, positive PCR retest results could be due to several reasons such as the type of specimen collection and technical errors associated with each component of swab testing, the methods used before discharging patients, prolonged viral shedding, and infection by mutated SARS-CoV-2. Thus, it should not always be considered as a reinfection or reactivation of the disease. Furthermore, most relevant studies on symptomatic and positive retest patients have shown relative and probably temporary immunity after the reCoVery of the disease, which means that immunity acquired following primary infection with SARS-CoV-2 may protect from subsequent exposure to the virus at least for a limited period.
ARTICLE HIGHLIGHTS
Research background
Due to the high rate of transmission of coronavirus disease 2019 (CoVID-19), a large number of people around the world became infected with the virus. There is evidence of reinfection with this virus. Therefore, people who get the disease once may be reinfected after reCoVery. Further investigation of reinfection by CoVID-19 is one of the necessities for better management of current conditions.
Research motivation
There have been reports of reCoVered individuals who have a second positive coronary test. This has raised concerns that there is no guarantee that the body will be safe after corona disease, even in the short term.
Research objectives
The aim of the present study was to investigate the available evidence of reinfection in patients with CoVID-19 who have reCoVered.
Research methods
This is a review study of different research types. Since there are myriads of publications released each and every day, with each trying to shed light on this pandemic from different perspectives, we aimed to summarize the very recent and of course the most trustworthy studies regarding the possibility of reinfection of CoVID-19 in this review in order to provide health care professionals and researchers imminent access to a multitude of these studies via a concise resource to save their invaluable time for other yet to do tasks.
Research results
The results have shown that there is a slight chance of reinfection. Though the duration of immunity is still unknown and needs to be determined; there is no guarantee that infected patients will not be infected again according to our results. These reinfections can be related to immunity system problems in cases of immunosuppressive disease or drugs that can misdirect our results, but there were many cases that got reinfected without any sign of the problems mentioned above.
Research conclusions
Based on the available evidence, reinfection in improved patients has been proven. Still, there is not enough data to definitely distinguish reinfection, reactivation, or infection with a new mutated severe acute respiratory syndrome coronavirus 2. So, further studies are necessary to understand if a CoVID-19 recurrence is possible and whether it could be considered a real threat.
Research perspectives
We strongly suggest further studies to follow up discharged CoVID-19 patients, check their course of symptoms periodically, and analyze related antibody levels; widespread virological studies are necessary to understand better this new global predicament.
ACKNOWLEDGEMENTS
The present study was conducted in collaboration with Khalkhal University of Medical Sciences, Iranian Institute for Reduction of High Risk Behaviors, Tehran University of Medical Sciences and Department of Global Health and Socio-epidemiology, Kyoto University.
Footnotes
Conflict-of-interest statement: The authors confirm that they have no conflict of interest.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Unsolicited manuscript
Peer-review started: September 2, 2020
First decision: September 21, 2020
Article in press: November 19, 2020
Specialty type: Virology
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Bendary M, Jahromi R S-Editor: Gao CC L-Editor: Filipodia P-Editor: Xing YX
Contributor Information
SeyedAhmad SeyedAlinaghi, Iranian Research Center for HIV/AIDS, Iranian Institute for Reduction of High Risk Behaviors, Tehran University of Medical Sciences, Tehran 1586489615, Iran.
Shahram Oliaei, HBOT Research Center, Golestan Hospital, Islamic Republic of Iran, Navy and AJA Medical University, Tehran 7134845794, Iran.
Shaghayegh Kianzad, School of Medicine, Iran University of Medical Sciences, Tehran 7134845794, Iran.
Amir Masoud Afsahi, Department of Radiology, School of Medicine, University of California, San Diego (UCSD), California, CA 587652458, United States.
Mehrzad MohsseniPour, Iranian Research Center for HIV/AIDS, Iranian Institute for Reduction of High Risk Behaviors, Tehran University of Medical Sciences, Tehran 1586489615, Iran.
Alireza Barzegary, School of Medicine, Islamic Azad University, Tehran 7134845794, Iran.
Pegah Mirzapour, Iranian Research Center for HIV/AIDS, Iranian Institute for Reduction of High Risk Behaviors, Tehran University of Medical Sciences, Tehran 1586489615, Iran.
Farzane Behnezhad, Department of Virology, School of Public Health, Tehran University of Medical Sciences, Tehran 7134845794, Iran.
Tayebeh Noori, Department of Health Information Technology, Zabol University of Medical Sciences, Zabol 5486952364, Iran.
Esmaeil Mehraeen, Department of Health Information Technology, Khalkhal University of Medical Sciences, Khalkhal 1419733141, Iran. es.mehraeen@gmail.com.
Omid Dadras, Department of Global Health and Socioepidemiology, Graduate School of Medicine, Kyoto University, Kyoto 215789652, Japan.
Fabricio Voltarelli, Graduation Program of Health Sciences, Faculty of Medicine, Federal University of Mato Grosso, Cuiabá 458796523, Brazil.
Jean-Marc Sabatier, Université Aix-Marseille, Institutde Neuro-physiopathologie (INP), UMR 7051, Faculté de Pharmacie, 27 Bd Jean Moulin, Marseille 546789235, France.
References
- 1.Sekhavati E, Jafari F, SeyedAlinaghi S, Jamalimoghadamsiahkali S, Sadr S, Tabarestani M, Pirhayati M, Zendehdel A, Manafi N, Hajiabdolbaghi M, Ahmadinejad Z, Kouchak HE, Jafari S, Khalili H, Salehi M, Seifi A, Golestan FS, Ghiasvand F. Safety and effectiveness of azithromycin in patients with CoVID-19: An open-label randomised trial. Int J Antimicrob Agents. 2020;56:106143. doi: 10.1016/j.ijantimicag.2020.106143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ye G, Pan Z, Pan Y, Deng Q, Chen L, Li J, Li Y, Wang X. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J Infect. 2020;80:e14–e17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehraeen E, Behnezhad F, Salehi MA, Noori T, Harandi H, SeyedAlinaghi S. Olfactory and gustatory dysfunctions due to the coronavirus disease (CoVID-19): a review of current evidence. Eur Arch Otorhinolaryngol. 2020;17:1–6. doi: 10.1007/s00405-020-06120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SeyedAlinaghi S, Ghadimi M, Hajiabdolbaghi M, Rasoolinejad M, Abbasian L, Nezhad MH, Manshadi SD, Ghadimi F, Ahmadinejad Z. Prevalence of CoVID-19-like Symptoms among People Living with HIV, and Using Antiretroviral Therapy for Prevention and Treatment. Curr HIV Res. 2020;18:373–380. doi: 10.2174/1570162X18666200712175535. [DOI] [PubMed] [Google Scholar]
- 5. Zhao W, Wang Y, Tang Y, Zhao W, Fan Y, Liu G, Chen R, Song R, Zhou W, Liu Y, Zhang F. Characteristics of Children With Reactivation of SARS-CoV-2 Infection After Hospital Discharge. Clin Pediatr (Phila) 2020;59:929–932. doi: 10.1177/0009922820928057. [DOI] [PubMed] [Google Scholar]
- 6.Sadr S, SeyedAlinaghi S, Ghiasvand F, Hassan Nezhad M, Javadian N, Hossienzade R, Jafari F. Isolated severe thrombocytopenia in a patient with CoVID-19: A case report. IDCases. 2020;21:e00820. doi: 10.1016/j.idcr.2020.e00820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghiasvand F, SeyedAlinaghi S. Isolated Anosmia as a Presentation of CoVID-19: An Experience in a Referral Hospital. Infect Disord Drug Targets. 2020;20:350. doi: 10.2174/1871526520999200520173216. [DOI] [PubMed] [Google Scholar]
- 8.Ghiasvand F, Miandoab SZ, Harandi H, Golestan FS, Alinaghi SAS. A Patient with CoVID-19 Disease in a Referral Hospital in Iran: A Typical Case. Infect Disord Drug Targets. 2020;20:559–562. doi: 10.2174/1871526520666200429115535. [DOI] [PubMed] [Google Scholar]
- 9.Mahmoudi S, Mehdizadeh M, Shervin Badv R, Navaeian A, Pourakbari B, Rostamyan M, Sharifzadeh Ekbatani M, Eshaghi H, Abdolsalehi MR, Alimadadi H, Movahedi Z, Mamishi S. The Coronavirus Disease 2019 (CoVID-19) in Children: A Study in an Iranian Children's Referral Hospital. Infect Drug Resist. 2020;13:2649–2655. doi: 10.2147/IDR.S259064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aldhaleei WA, Alnuaimi A, Bhagavathula AS. CoVID-19 Induced Hepatitis B Virus Reactivation: A Novel Case From the United Arab Emirates. Cureus. 2020;12:e8645. doi: 10.7759/cureus.8645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghiasvand F, Ghadimi M, Ghadimi F, Safarpour S, Hosseinzadeh R, SeyedAlinaghi S. Symmetrical polyneuropathy in coronavirus disease 2019 (CoVID-19) IDCases. 2020;21:e00815. doi: 10.1016/j.idcr.2020.e00815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ravioli S, Ochsner H, Lindner G. Reactivation of CoVID-19 pneumonia: A report of two cases. J Infect. 2020;81:e72–e73. doi: 10.1016/j.jinf.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asadollahi-Amin A, Hasibi M, Ghadimi F, Rezaei H, SeyedAlinaghi S. Lung Involvement Found on Chest CT Scan in a Pre-Symptomatic Person with SARS-CoV-2 Infection: A Case Report. Trop Med Infect Dis. 2020;5 doi: 10.3390/tropicalmed5020056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehraeen E, Hayati B, Saeidi S, Heydari M, Seyed Alinaghi S. Self-Care Instructions for People Not Requiring Hospitalization for Coronavirus Disease 2019 (CoVID-19) Arch Clin Infect Dis. 2020;15 [Google Scholar]
- 15.Shah VK, Firmal P, Alam A, Ganguly D, Chattopadhyay S. Overview of Immune Response During SARS-CoV-2 Infection: Lessons From the Past. Front Immunol. 2020;11:1949. doi: 10.3389/fimmu.2020.01949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alizargar J. Risk of reactivation or reinfection of novel coronavirus (CoVID-19) J Formos Med Assoc. 2020;119:1123. doi: 10.1016/j.jfma.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roy S. CoVID-19 Reinfection: Myth or Truth? SN Compr Clin Med. 2020:1–4. doi: 10.1007/s42399-020-00335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bongiovanni M, Basile F. Re-infection by CoVID-19: a real threat for the future management of pandemia? Infect Dis (Lond) 2020;52:581–582. doi: 10.1080/23744235.2020.1769177. [DOI] [PubMed] [Google Scholar]
- 19.Elrashdy F, Aljaddawi AA, Redwan EM, Uversky VN. On the potential role of exosomes in the CoVID-19 reinfection/reactivation opportunity. J Biomol Struct Dyn. 2020:1–12. doi: 10.1080/07391102.2020.1790426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaturvedi R, Naidu R, Sheth S, Chakravarthy K. Efficacy of Serology Testing in Predicting Reinfection in Patients With SARS-CoV-2. Disaster Med Public Health Prep. 2020:1–3. doi: 10.1017/dmp.2020.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jahromi R, Avazpour A, Jahromi M, Alavi JJIJoCR. CoVID-19 with positive bronchoalveolar lavage fluid but negative nasopharyngeal and oropharyngeal swabs: A case report and insights. Indian J Case Rep. 2020:380–382. [Google Scholar]
- 22.Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, Yin H, Xiao Q, Tang Y, Qu X, Kuang L, Fang X, Mishra N, Lu J, Shan H, Jiang G, Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Villamil JFP, Olivera MJ. CoVID-19: Is Reinfection a Threat or Not? Iran J Public Health. 2020;49:112–3. doi: 10.18502/ijph.v49iS1.3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu LP, Wang NC, Chang YH, Tian XY, Na DY, Zhang LY, Zheng L, Lan T, Wang LF, Liang GD. Duration of antibody responses after severe acute respiratory syndrome. Emerg Infect Dis. 2007;13:1562–1564. doi: 10.3201/eid1310.070576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gousseff M, Penot P, Gallay L, Batisse D, Benech N, Bouiller K, Collarino R, Conrad A, Slama D, Joseph C, Lemaignen A, Lescure FX, Levy B, Mahevas M, Pozzetto B, Vignier N, Wyplosz B, Salmon D, Goehringer F, Botelho-Nevers E in behalf of the COCOREC study group. Clinical recurrences of CoVID-19 symptoms after reCoVery: Viral relapse, reinfection or inflammatory rebound? J Infect. 2020;81:816–846. doi: 10.1016/j.jinf.2020.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kang H, Wang Y, Tong Z, Liu X. Retest positive for SARS-CoV-2 RNA of "reCoVered" patients with CoVID-19: Persistence, sampling issues, or re-infection? J Med Virol. :2020. doi: 10.1002/jmv.26114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Law SK, Leung AWN, Xu C. Is reinfection possible after reCoVery from CoVID-19? Hong Kong Med J. 2020;26:264–265. doi: 10.12809/hkmj208601. [DOI] [PubMed] [Google Scholar]
- 28.Tao JJ, Hu Z, Liu J, Pang P, Fu G, Qian A, Chen S, Lin L, Cao G, Sun H, Yang Y, Wang M. Positive RT-PCR Test Results in Discharged CoVID-19 Patients: Reinfection or Residual? 2020. [Google Scholar]
- 29.Zhang L, Liu Y. Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gomez-Mayordomo V, Montero-Escribano P, Matías-Guiu JA, González-García N, Porta-Etessam J, Matías-Guiu J. Clinical exacerbation of SARS-CoV-2 infection after fingolimod withdrawal. J Med Virol. 2020 doi: 10.1002/jmv.26279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hageman JR. What Are the Newest Effects of CoVID-19 in Children? Pediatr Ann. 2020;49:e242–e243. doi: 10.3928/19382359-20200520-02. [DOI] [PubMed] [Google Scholar]
- 32.Hoang VT, Dao TL, Gautret P. Recurrence of positive SARS-CoV-2 in patients reCoVered from CoVID-19. J Med Virol. 2020 doi: 10.1002/jmv.26056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Inamo J. How should we overcome the threat by the pandemic of 2019-nCoV? Clin Rheumatol. 2020;39:2471–2473. doi: 10.1007/s10067-020-05083-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Islam H, Rahman A, Masud J, Shweta DS, Araf Y, Ullah MA, Sium SM, Sarkar B. A Generalized Overview of SARS-CoV-2: Where Does the Current Knowledge Stand? Electron J Gen Med. 2020;17:em251. [Google Scholar]
- 35.Kannan S, Subbaram K, Ali S, Kannan H. Molecular characterization and amino acid homology of nucleocapsid (N) Protein in SARS-CoV-1, SARS-CoV-2, MERS-CoV, and bat coronavirus. J Pure Appl Microbio. 2020;23:14. [Google Scholar]
- 36.Karimi A, Shirvani F, Seifi K. Reinfection or relapse in sars-CoV-2-infected patients; does it occur? Arch Pediatr Infecti Dis. 2020;8:e103466. [Google Scholar]
- 37.Kassa SM, Njagarah JBH, Terefe YA. Analysis of the mitigation strategies for COVID-19: From mathematical modelling perspective. Chaos Solitons Fractals. 2020;138:109968. doi: 10.1016/j.chaos.2020.109968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kellam P, Barclay W. The dynamics of humoral immune responses following SARS-CoV-2 infection and the potential for reinfection. J Gen Virol. 2020;101:791–797. doi: 10.1099/jgv.0.001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kirkcaldy RD, King BA, Brooks JT. CoVID-19 and Postinfection Immunity: Limited Evidence, Many Remaining Questions. JAMA . 2020;323:2245–2246. doi: 10.1001/jama.2020.7869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Koks S, Williams RW, Quinn J, Farzaneh F, Conran N, Tsai SJ, Awandare G, Goodman SR. CoVID-19: Time for precision epidemiology. Exp Biol Med (Maywood) 2020;245:677–679. doi: 10.1177/1535370220919349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Laxminarayan R, John TJ. Is Gradual and Controlled Approach to Herd Protection a Valid Strategy to Curb the CoVID-19 Pandemic? Indian Pediatr. 2020;57:505–507. doi: 10.1007/s13312-020-1844-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leslie M. T cells found in coronavirus patients 'bode well' for long-term immunity. Science. 2020;368:809–810. doi: 10.1126/science.368.6493.809. [DOI] [PubMed] [Google Scholar]
- 43.Luo A. Positive SARS-CoV-2 test in a woman with CoVID-19 at 22 days after hospital discharge: A case report. Zhongyi Kexue Zazhi (English) 2020:1–5. [Google Scholar]
- 44.Meca-Lallana V, Aguirre C, Cardeñoso L, Alarcon T, Figuerola-Tejerina A, Del Río B, Álvarez MR, Vivancos J. Establishment of a safety protocol for the administration of treatments in multiple sclerosis during the SARS-CoV-2 pandemic. Mult Scler Relat Disord. 2020;44:102244. doi: 10.1016/j.msard.2020.102244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okhuese AV. Estimation of the Probability of Reinfection With CoVID-19 by the Susceptible-Exposed-Infectious-Removed-Undetectable-Susceptible Model. JMIR Public Health Surveill . 2020; 6:e19097. doi: 10.2196/19097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Omer SB, Malani P, Del Rio C. The CoVID-19 Pandemic in the US: A Clinical Update. JAMA. 2020;323:1767–1768. doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- 47.Ota M. Will we see protection or reinfection in CoVID-19? Nat Rev Immunol. 2020;20:351. doi: 10.1038/s41577-020-0316-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ozdinc M, Senel K, Ozturkcan S, Akgul A. Predicting the progress of CoVID-19: the case for Turkey. Turkiye Klinikleri J Med Sci. 2020 [Google Scholar]
- 49.Steinchen N, Müller-Ladner U, Lange U. [Biological therapy after CoVID-19 infection : No reactivation of a CoVID-19 infection with positive SARS-CoV-2 antibody status under biological therapy] Z Rheumatol. 2020;79:574–577. doi: 10.1007/s00393-020-00824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ueffing M, Bayyoud T, Schindler M, Ziemssen F. [Basic principles of replication and immunology of SARS-CoV-2] Ophthalmologe. 2020;117:609–614. doi: 10.1007/s00347-020-01155-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Verhagen MD, Brazel DM, Dowd JB, Kashnitsky I, Mills MC. Forecasting spatial, socioeconomic and demographic variation in CoVID-19 health care demand in England and Wales. BMC Med. 2020;18:203. doi: 10.1186/s12916-020-01646-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Waltuch T, Gill P, Zinns LE, Whitney R, Tokarski J, Tsung JW, Sanders JE. Features of CoVID-19 post-infectious cytokine release syndrome in children presenting to the emergency department. Am J Emerg Med 2020; 38: 2246.e3-2246. :e6. doi: 10.1016/j.ajem.2020.05.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhou L, Liu K, Liu HG. [Cause analysis and treatment strategies of "recurrence" with novel coronavirus pneumonia (CoVID-19) patients after discharge from hospital] Zhonghua Jiehe He Huxi Zazhi. 2020; 43:281–284. doi: 10.3760/cma.j.cn112147-20200229-00219. [DOI] [PubMed] [Google Scholar]
- 54. Arafkas M, Khosrawipour T, Kocbach P, Zielinski K, Schubert J, Mikolajczyk A, Celinska M, Khosrawipour V. Current meta-analysis does not support the possibility of CoVID-19 reinfections. J Med Virol. 2020 doi: 10.1002/jmv.26496. [DOI] [PubMed] [Google Scholar]