Abstract
Background:
Physeal injuries of the coracoid process are rare but may be increasing because of increased participation of youth in year-round sports.
Purpose:
To analyze reported physeal and apophyseal injuries of the coracoid process.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
PubMed and Scopus were searched using the terms scapula fracture and coracoid fracture. The inclusion criteria were English full-text articles describing coracoid fracture as well as articles that described patient characteristics and presented appropriate images. The exclusion criteria were descriptive cases without images as well as those lacking appropriate images. Citation tracking was conducted to find additional articles and full-text articles written in other languages. Articles were included if they reported physeal injury or judged to involve physeal injury based on the provided images.
Results:
Overall, 22 studies including 32 patients (29 males, 3 females) were identified. All but 2 patients were younger than 18 years of age, and 66% (21/32) had sustained injuries during or as a result of participation in sporting activities. The affected site was the physis at the base in 18 patients, an intra-articular fracture in the primary coracoid ossification center combined with the subcoracoid ossification center to form an intra-articular fracture in 5, the apophysis of the tip in 3, the apophysis of the angle in 5, and uncertain in 1. Eleven patients had concurrent acromioclavicular injuries. The injury was acute in 23 patients, chronic in 6, and traumatic nonunion in 3. Among 21 cases in which treatment methods and outcomes were described, 21% of the acute cases (4/19), and 2 of the 3 nonunions were surgically treated. Only 1 study used a widely accepted evaluation method. Follow-up periods ranged from 6 weeks to 2 years. Outcomes were generally excellent for nonoperative and operative treatment and without any serious complications.
Conclusion:
Coracoid physeal injuries occurred most commonly in patients aged 13 to 15 years of age (71%) and were usually sustained during or as a result of sports activities (66%). The most common injury site was the physis at its base. The cause of these injuries is probably severe or repeated traction of the attached muscles and ligaments. The majority of these injuries can be successfully treated nonoperatively.
Keywords: shoulder, scapula, physeal injury, sports trauma, adolescent
The shoulder is a complex joint comprising multiple anatomic joints and jointlike structures and 3 bones (clavicle, scapula, and humerus) ranging from the sternoclavicular joint to the glenohumeral joint. In this complex joint, the coracoid process plays an important role as (1) an attachment site of the coracoclavicular ligaments that firmly connect the clavicle and scapula, (2) a part of the coracoacromial arch, and (3) the origin and insertion sites of 3 muscles. Although the coracoid process is a small bony projection, fractures of the coracoid process have numerous effects on the function of neighboring joints and musculoskeletal systems.
In patients aged <18 years, scapular fractures account for 0.33% of all fractures, with a peak incidence at the age of 14 years in males and 11 years in females.12 Although fractures represent 7% to 26% of all reported injuries sustained during sports activities in children and adolescents, approximately 15% of all fractures in children involve a physis.43 The incidence of acute physeal injuries ranges from 1% to 12% of all sporting injuries, depending on the sport.8 However, the rate of coracoid physeal injuries among all patients with physeal injuries and coracoid fractures remains unknown.
The purpose of this review was to systematically evaluate the available literature to clarify the current concept of physeal and apophyseal injuries of the coracoid process. We briefly introduce the anatomy and development of the coracoid process because knowledge of these topics is required to understand physeal and apophyseal injuries of the coracoid process, including chronic stress injuries.
Coracoid Anatomy and Development
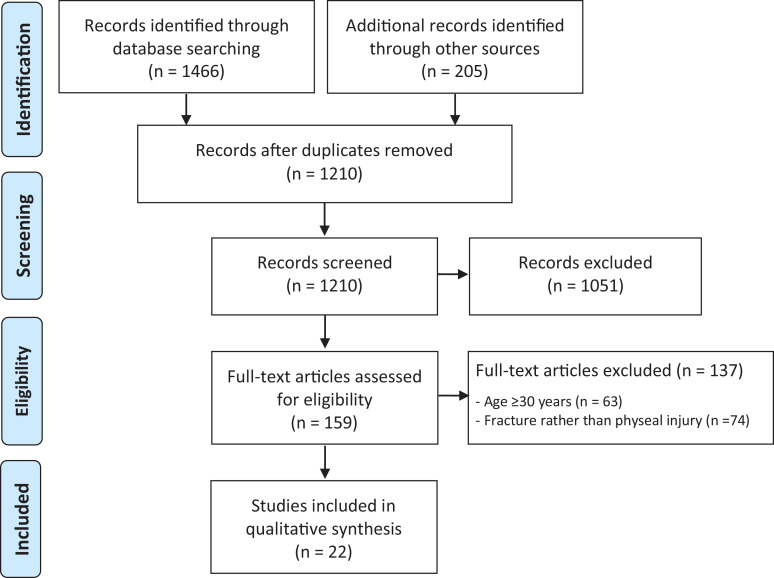
The coracoid process arises from the upper border of the neck of the scapula. The junction of the vertical and horizontal parts of the coracoid process is called the “elbow” or “angle.” Numerous ligaments and 3 muscles are anchored to the coracoid process (Figure 1).
Figure 1.
Muscles and ligaments attached to the coracoid process: pectoralis minor muscle (1), conjoint tendon of the coracobrachialis muscle and short head of the biceps brachii muscle (2), superior scapular transverse ligament (a), coracoclavicular ligaments (b), coracoacromial ligament (c), coracohumeral ligament (hidden behind the coracoacromial ligament) (d).
The most important ligaments are the coracoclavicular ligaments that attach to the angle of the coracoid process.27 The pectoralis minor inserts at the superior and medial aspect of the proximal horizontal part of the coracoid process. The coracobrachialis and short head of the biceps, forming the conjoint tendon, insert at the tip.
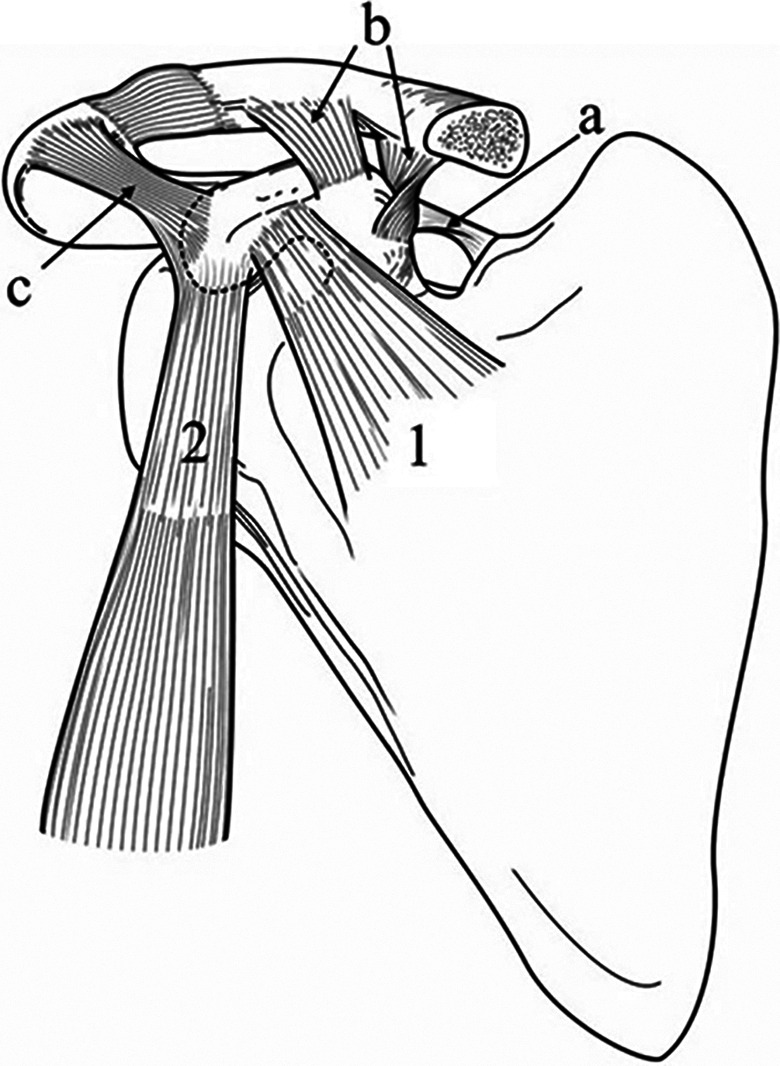
Ossification of the coracoid process begins with the development of a primary center 3 to 4 months after birth,49 although it can be present before birth.20,26,50 At 2 years of age, the coracoid ossification center expands, establishing a true bipolar growth region (bipolar physis) between the main portion of the scapula and the coracoid process; this region permits growth at the scapula and coracoid surfaces, away from a central reserve zone.42,49
The subcoracoid (or infracoracoid) ossification center is the first scapular secondary ossification center to ossify, and it forms the upper one-third of the glenoid articular surface.49 This ossification center develops at 8 to 10 years of age and extends toward the bipolar growth plate between the base of the coracoid and scapula.54 The subcoracoid ossification center then has a double epiphyseal surface for articulation with the coracoid process anteriorly and the remainder of the scapula inferiorly (Figure 2).49
Figure 2.
Development of the coracoid process at age 12 to 13 years of age. The subcoracoid ossification center is the first scapular secondary ossification center to ossify, and it forms the upper one-third of the glenoid.
Both epiphyseal surfaces of the subcoracoid ossification center commence fusion simultaneously around 11 to 16 years of age.9,49 Complete fusion between the coracoid and subcoracoid ossification centers occurs before complete fusion of the subcoracoid to the remainder of the scapula.49 The coracoid and subcoracoid ossification centers are completely fused by 16 to 17 years of age in both sexes.9,49,54 Sex-related differences in maturity are less noticeable in the scapular girdle.9
After fusion of the coracoid process to the scapula, the thin and scale-like apophysis (accessory ossification center, tension epiphysis) that passes forward and laterally across the angle appears at around 14 to 15 years of age.9,39 The apophysis of the tip is flakelike in appearance and reportedly appears between 13 to 16 years and merges until 17 to 20 years of age.49 The appearance and fusion of the ossification centers vary widely and are significantly influenced by observation method, race, and socioeconomic status.9,24
Methods
This systematic review was conducted per the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using a checklist for systematic reviews.32 The literature search was performed from January 2018 to December 2019, and the publication years of the included articles ranged from 1900 to 2018. The PubMed and Scopus databases were searched using the terms “scapula fracture” and “coracoid fracture” to identify relevant studies. Two reviewers (K.O., N.M.) independently conducted the search and review. The inclusion criteria were as follows: English full-text articles concerning coracoid fracture that described the patients’ characteristics and presented the appropriate images (radiography, computed tomography, or magnetic resonance imaging [MRI]) to confirm the details of coracoid fracture. The exclusion criteria were descriptive articles or cases in which radiography was not used and articles or cases without appropriate images to enable evaluation of the injury details. Citation tracking was conducted to find additional related English-language articles and notable full-text articles written in other languages, which were selected and added to the qualitative synthesis.
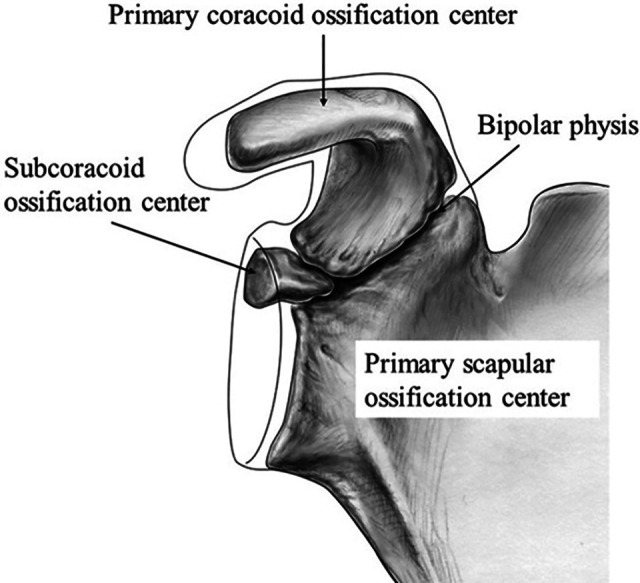
The article-selection process is shown in Figure 3. Ultimately, 22 studies were included in the analysis. All were case reports with the exception of 3 small case series. Each patient was analyzed regarding age, sex, cause of injury, injured site, associated injuries, injury type (acute or chronic), type of treatment, and outcome.
Figure 3.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart of the study.
Results
Patient Characteristics
The 22 articles included 32 reported cases of physeal injury of the coracoid process (Table 1). §
Table 1.
Characteristics of Patients Included in the Present Reviewa
| Year | Authors | Age (y), Sex, Side | Cause | Injury Type | Injured Site | AC injuries | Treatment, Outcome |
|---|---|---|---|---|---|---|---|
| 1951 | Schaefer48 | 15, M, left | ? | Acute | Base | Nonop, excellent | |
| 1971 | Benton and Nelson6 | 19, M, right | Tennis? | Nonunion | Tip | Surg, good | |
| 1975 | Protass et al46 | 17, M, left | Football | Acute | Base | Dislocation | Nonop |
| 1975 | Protass et al46 | 22, F, left | Car accident | Acute | Base | Dislocation | Surg |
| 1975 | Protass et al46 | 14, M, left | Bicycling | Acute | Base | Dislocation | Nonop |
| 1977 | Montgomery and Loyd33 | 15, M, left | Football | Acute | Angle | Dislocation | Surg, excellent |
| 1977 | Montgomery and Loyd33 | 15, M, right | MVA | Acute | Angle | Dislocation | Nonop, good |
| 1983 | Bernard et al7 | 13, M, left | Football | Acute | Base? | Dislocation | Nonop, excellent |
| 1986 | Taga et al52 | 9, F, right | ? | Acute | IA | Grade I | Nonop, excellent |
| 1995 | Combalía et al11 | 12, M, left | Soccer | Acute | Base | Dislocation | Nonop, excellent |
| 1996 | Cottalorda et al13 | 15, M, right | Judo | Acute | Base | Nonop, excellent | |
| 1998 | Holst and Christiansen22 | 13, M, right | Fall | Acute | IA | Grade I | Nonop, excellent |
| 2007 | Nakagawa et al36 | 17, M, left | Judo | Acute | Angle | Dislocation | Nonop |
| 2009 | Mwaturura and Bourne35 | 14, M, left | Football | Acute | Base | Nonop, excellent | |
| 2009 | Leijnen et al29 | 16, M, right | MCA | Acute | Angle | Maximum tenderness | Nonop |
| 2010 | Davis15 | 15, M, right | Wrestling | Acute | Base | ||
| 2011 | Nakama et al37 | 16, M, right | Flying rings | Acute?b | Tip | Surg, excellent | |
| 2012 | Chitre et al10 | 13, M, right | Skiing | Acute | Base | Nonop, excellent | |
| 2014 | Pedersen et al44 | 14, M, left | Ice hockey | Acute | IA | Subluxation | Nonop, excellent |
| 2016 | Archik et al3 | 15, M, right | Cricket | Acute?b | Tip | Surg, excellent | |
| 2016 | Mohammed et al31 | 14, M, right | Football | Acute | Angle | Dislocation | |
| 2016 | Delgado et al16 | 13, M, left | Football | Acute | Base | ||
| 2017 | Stone and Freehill51 | 14, M, left | MCA | Nonunion | IA | Surg, excellent | |
| 2017 | Alaia et al2 | 13-22,c 7 M:1 F | 5 sports,d 2 NMD, 1 fall | 6 chronic, 1 nonunion, 1 acutee | All base | ||
| 2018 | Cross et al14 | 15, M, right | Rugby | Acute | IA | Subluxation | Nonop, excellent |
aAC, acromioclavicular joint; F, female; IA, intra-articular; M, male; MCA, motorcycle accident; MVA, motor vehicle accident; NMD, neuromuscular disorders; Nonop, nonoperative; Surg, surgery.
bIt is possible that acute injury superimposes on chronic physeal injury secondary to repetitive stress.
cPatients aged <18 y: n = 7.
dFootball, archery, basketball, swimming, rugby.
eNonunion, rugby player; acute, fall.
Although some reports did not clearly describe whether the injury was physeal or apophyseal, this detail was determined from the presented images.3,6,7,10,48 The patients comprised 29 males and 3 females with an age range of 9 to 22 years of age. All patients were younger than 18 years with the exception of 2 patients aged 22 years of age.2,46 Notably, 1 article described the injury of a 19-year-old male who had experienced shoulder pain for 4 years and therefore seemed to have been injured at the age of 15 years.6 Among the articles that precisely described the age at which symptoms occurred, 71% (17/24) of patients were 13 to 15 years old.
The injuries were sustained during or due to sports activities in 66% (21/32) of patients: American football in 7, judo in 2, and rugby in 2, as well as tennis, soccer, wrestling, flying ring, ski, ice hockey, cricket, archery, basketball, and swimming in 1 each.∥ Five injuries were caused as the result of a traffic accident, 2 by a fall, and 2 by neuromuscular disorders.2,22,29,33,46,51 The cause of the remaining 2 injuries was uncertain.48,52
Injured Sites and Associated Injuries
The site of physeal or apophyseal injuries was the physis at the coracoid base in 18 patients aged 12 to 22 years. The primary coracoid ossification center combined with the subcoracoid ossification center was affected in 5 patients aged 9 to 15 years (mean, 12.8 years), forming an intra-articular fracture.14,22,44,51,52 Apophyseal injuries of the tip occurred in 3 patients aged 15 and 16 years.3,6,37 Apophyseal injuries of the angle occurred in 5 patients with associated acromioclavicular dislocation in 4 of these 5 patients, whose ages ranged from 14 to 17 years (mean, 15.4 years).29,31,33,36 The specific affected site was uncertain in the remaining 13-year-old boy.7
Acromioclavicular joint injury was the most common associated musculoskeletal injury around the shoulder. Its dislocation occurred in 9 patients; subluxation was sustained by 2 patients.7,11,14,31,33,36,44,46 In these patients, the injured sites of the coracoid process were the base in 5 patients, intra-articular in 2, and apophysis at the angle in 4. A proximal humeral fracture was observed in 1 patient. The patient had sustained this fracture as well as an intra-articular physeal injury of the coracoid 1 year prior; the latter had been overlooked, resulting in nonunion.51
Injury Type (Acute or Chronic)
The injury type was acute in 23 patients. Six patients had chronic injury caused by repetitive stress.2 Three patients were initially diagnosed with a nonunion of the base or tip.2,6,51
Treatment Methods, Outcomes, and Complications
Treatment methods and outcomes were described in 21 cases. The other 11 cases were retrospectively reported by radiologists and lacked clinical data. Among the 21 cases in which the treatment methods and outcomes were described, 79% (15/19) of acute injuries were nonoperatively treated using an arm sling or other type of support. Of the 4 patients who underwent surgery, fixation of the avulsed apophysis of the angle using nonabsorbable sutures was performed in 1 case33; fixation of the associated acromioclavicular dislocation using Steinman pins with no procedure for the coracoid was performed in 1 case46; and fixation of the avulsed apophysis of the tip using a cannulated screw and washer was performed in 2 cases.3,37 Two cases of nonunion were surgically treated: 1 patient underwent resection of the tip fragment and reattachment of the conjoint tendon to the remaining coracoid, while the other underwent fixation using a cannulated screw.6,51 Although the evaluation methods varied among the studies and only 1 study used the widely accepted evaluation method, the treatment outcomes were generally excellent without any residual symptoms or limitation of range of motion in 14 of 16 patients who were followed up for >6 weeks (mean ± SD, 22 ± 27 weeks), regardless of whether the treatment was nonoperative or operative. However, 1 patient showed reduced abduction strength and persistent vague posterior discomfort after surgical treatment for nonunion of the tip,6 and 1 patient experienced aching at the acromioclavicular joint with activity and cosmetic deformity after nonoperative treatment for acute apophyseal injury of the angle.33 The outcomes were unknown in the other 4 patients.36,46
Except for the 2 aforementioned cases, there were no reports of intraoperative, early postoperative, or late postoperative complications, including injury- or treatment-related growth disturbance.
Discussion
Scapular fractures occur relatively infrequently, accounting for 0.4% to 1.0% of all fractures.5,38,47 Coracoid fractures have been reported to account for 0% to 7% of all scapular fractures, based on studies using plain radiography.1,4,17,18,23,30,34,53 However, this incidence is likely to be underestimated because coracoid fractures are easily overlooked unless appropriate plain radiography designed to reveal the coracoid process is performed. As only 32 reported cases in 22 studies were identified in this review, physeal or apophyseal injury of the coracoid process appears to be much rarer than its fracture. Most patients with coracoid physeal injuries (71%) were 13 to 15 years old when their symptoms occurred. This coincides with the most common age at which most physeal fractures occur.45 The male:female ratio of the reported physeal injuries in this review was 29:3, whereas this ratio among children with any acute physeal fractures was reported to be 2:1.45 Thus, physeal injury of the coracoid process is overwhelmingly more common in male than female patients.
In the present review, the most commonly injured site of the developing coracoid was the physis at the coracoid base. The primary coracoid ossification center, combined with the subcoracoid ossification center, was sometimes injured, forming an intra-articular fracture.14,22,44,51,52 Although all the authors of these cases reported a physeal injury at the base, detailed examination of the provided images revealed that the subcoracoid ossification center was displaced with the primary coracoid ossification center. The age of these patients corresponds to the age immediately prior to the start of physeal closure of the subcoracoid ossification center.9,49 Because apophyseal injuries of the tip occurred in 3 patients aged 15 and 16 years of age,3,6,37 the most common age for this injury appeared to be between 15 and 16 years. As apophyseal injuries of the angle occurred in 5 patients aged 14 to 17 years (mean, 15.4 years), the most common age for this injury appears to be approximately 15 years. Differences in the prevalence of epiphyseal and apophyseal injury at different sites could be caused by differences in the appearance and fusion times of each ossification center.
Several clinical factors can be used to deduce the mechanism of epiphyseal injury and fracture of the coracoid process.40 Because the coracoid process is deeply situated under the clavicle and protected from direct trauma, direct trauma is unlikely to be the mechanism of coracoid physeal injury. This review identified no cases in which the physeal injury appeared to result from direct trauma to the coracoid process, with the exception of 1 case reported by Pedersen et al.44 Of the concurrent musculoskeletal injuries, acromioclavicular joint injury was the most frequent, occurring in 48% (11/23) of patients with acute physeal injuries. Before physeal closure, the coracoclavicular ligaments are often stronger than the physis. Therefore, an injury that would result in ligamentous disruption in an adult may injure only the physis of the coracoid process in a child.8,43 The physeal or apophyseal injuries combined with acromioclavicular injuries thus may have occurred via traction of the coracoclavicular ligaments. In a case of apophyseal separation at the angle without obvious acromioclavicular injury,29 we assumed that the acromioclavicular joint or distal clavicular epiphysis had been damaged because of marked tenderness around the acromioclavicular joint.
For the remaining 12 acute injuries, 6 chronic injuries, and 2 nonunions (which were not associated with acromioclavicular injuries), we presume that the cause of injury was violent or repeated traction of muscles attached to the coracoid process. Based on the current findings, we agree with Alaia et al2 that increased muscular pull of the short head of the biceps, coracobrachialis, and/or pectoralis minor on the coracoid process leads to physeal stress injury in athletes. We speculate that this hypothesis is also valid in cases of acute injury. Therefore, we consider that the main cause of physeal injury of the coracoid process is violent or repeated traction of the attached muscles and ligaments.
The incidence of acute physeal injuries reportedly ranges from 1% to 12% of injuries, depending on the sport.8 However, there are no available data regarding the incidence of coracoid physeal injuries among all physeal injuries related to sports activity. In this review, 66% (21/32) of coracoid physeal injuries occurred during or as a result of sports activities. The acute injuries most commonly occurred in association with contact sports such as American football, judo, ice hockey, rugby, and soccer. All 3 patients with apophyseal separation at the tip were repeatedly subjected to traction stress by the conjoint tendon during sports activities. Among them, 2 patients with acute apophyseal injuries may have had a chronic physeal injury secondary to repetitive stress superimposed on an acute injury.2,3,37 Three patients in this review had symptomatic nonunion, 2 of which were considered the result of additional continuous stress attributed to continuing sports activity after physeal injury secondary to repetitive stress.2,6 Additionally, 4 cases with symptomatic chronic injury based on sports activity were reported.2 Because the incidence of physeal injuries of the coracoid process may increase in the future because of widespread participation in youth sports, physicians or coaches encountering children who subject their shoulders to high levels of repetitive stress and who develop shoulder pain should consider the possibility of chronic physeal injury of the coracoid process.
Acute cases are frequently associated with acromioclavicular injury, of which local symptoms overlap those of coracoid physeal or apophyseal injury, which complicates diagnosis of the latter. However, in isolated physeal injury and apophyseal injury at the tip, the presence of characteristic symptoms, such as tenderness confined to the coracoid and induction of anterior shoulder pain on resistive elbow flexion or forearm supination or on deep breathing, provides substantial evidence for accurate diagnosis.41 Imaging exploration is indispensable for making a definitive diagnosis of physeal or apophyseal coracoid injury and for distinguishing between fracture and physeal or apophyseal injury, but the coracoid process is not easily visualized by routine radiographic projections. Although radiographic projection in the arm-elevated position that permits observation of the entire coracoid was applied in earlier studies,28,48 it caused pain for a patient with acute injury. Subsequently, various types of the angle-up view, anterior oblique view, or scapular Y view now are recommended.19,21,46 Computed tomography and MRI are also useful for this purpose.2,25 Alaia et al2 reported 6 chronic physeal injuries that were not clinically suspected before MRI examination, which revealed chronic physeal injury. Therefore, physicians encountering children who subject their shoulders to high levels of repetitive stress and develop shoulder pain should examine these children using MRI. In any event, most of the aforementioned imaging measures are applied only when the presence of coracoid injury is suspected by the physician.
The treatment outcomes were generally excellent regardless of whether the injury was treated nonoperatively or surgically, and no serious complications occurred. Regarding the indications for surgery in acute cases, it is inappropriate to determine the indication by the distance of displacement because of variation in a patient’s physique. Reduction and fixation of the acromioclavicular joint for apophyseal separation at the angle accompanied by acromioclavicular dislocation and open reduction and fixation for apophyseal separation at the tip with ≥5-mm displacement that is continuously pulled by the conjoint tendon may be indicated. However, with the exception of symptomatic nonunions, the treatment of most physeal injuries is principally nonoperative, with excellent outcomes usually being reported.
The main limitation of the current review is that the number of cases that met the inclusion criteria was extremely small. Additionally, because some cases were retrospectively reported by radiologists and lacked details regarding medical history and treatment method, the number of cases that could be analyzed differed for each analysis item. Many studies did not employ widely used evaluation methods; therefore, the results of different treatment methods could not be compared. Finally, because the patients were adolescents, the follow-up period was generally short, and the occurrence of late complications could not be confirmed.
Conclusion
Coracoid physeal injuries occurred in patients aged 13 to 15 years (71%) and were usually sustained during or due to various sports activities (66%). The most common injury site was the physis at the base. The primary coracoid ossification center combined with the subcoracoid ossification center was notably injured in 5 cases, forming an intra-articular fracture. The cause of these injuries is probably violent or repeated traction of the attached muscles and ligaments. The majority of these injuries can be successfully treated nonoperatively.
Acknowledgment
The authors thank Edanz Editing for editing a draft of this manuscript.
Footnotes
Final revision submitted June 10, 2020; accepted June 24, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ada JR, Miller ME. Scapular fractures: analysis of 113 cases. Clin Orthop Relat Res. 1991;269:174–180. [PubMed] [Google Scholar]
- 2. Alaia EF, Rosenberg ZS, Rossi I, et al. Growth plate injury at the base of the coracoid: MRI features. Skeletal Radiol. 2017;46:1507–1512. [DOI] [PubMed] [Google Scholar]
- 3. Archik S, Nanda SN, Tripathi S, et al. An isolated displaced fracture of the coracoid process treated with open reduction and internal fixation—a case report and review of literature. J Orthop Case Rep. 2016;6:37–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Armstrong CP, Van der Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury. 1984;15:324–329. [DOI] [PubMed] [Google Scholar]
- 5. Bartoníček J. Scapular fractures In: Court-Brown CM, ed. Rockwood and Green’s Fractures in Adults. 8th ed. Wolters Kluwer Health; 2015:1475–1501. [Google Scholar]
- 6. Benton J, Nelson C. Avulsion of the coracoid process in an athlete: report of a case. J Bone Joint Surg Am. 1971;53:356–358. [PubMed] [Google Scholar]
- 7. Bernard TN, Jr, Brunet ME, Haddad RJ., Jr Fractured coracoid process in acromioclavicular dislocations: report of four cases and review of the literature. Clin Orthop Relat Res. 1983;175:227–232. [PubMed] [Google Scholar]
- 8. Caine D, DiFiori J, Maffulli N. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40:749–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cardoso HFV, Spake L, Humphrey LT. Age estimation of immature human skeletal remains from the dimensions of the girdle bones in the postnatal period. Am J Phys Anthropol. 2017;163:772–783. [DOI] [PubMed] [Google Scholar]
- 10. Chitre AR, Divecha HM, Hakimi M, et al. Traumatic isolated coracoid fractures in the adolescent. Case Rep Orthop. 2012;2012:371627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Combalía A, Arandes JM, Alemany X, et al. Acromioclavicular dislocation with epiphyseal separation of the coracoid process: report of a case and review of the literature. J Trauma. 1995;38:812–815. [DOI] [PubMed] [Google Scholar]
- 12. Cooper C, Dennison EM, Leufkens HG, et al. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19:1976–1981. [DOI] [PubMed] [Google Scholar]
- 13. Cottalorda J, Allard D, Dutour N, et al. Fracture of the coracoid process in an adolescent. Injury. 1996;27:436–437. [DOI] [PubMed] [Google Scholar]
- 14. Cross GWV, Reilly P, Khanna M. Salter-Harris type 1 coracoid process fracture in a rugby playing adolescent. BJR Case Rep. 2018;4(3):20180011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davis KW. Imaging pediatric sports injuries: upper extremity. Radiol Clin North Am. 2010;48:1199–1211. [DOI] [PubMed] [Google Scholar]
- 16. Delgado J, Jaramillo D, Chauvin NA. Imaging the injured pediatric athlete: upper extremity. Radiographics. 2016;36:1672–1687. [DOI] [PubMed] [Google Scholar]
- 17. Féry A, Sommelet J. Fracture of the coracoid process [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1979;65:403–407. [PubMed] [Google Scholar]
- 18. Findlay RT. Fractures of the scapula and ribs. Am J Surg. 1937;38:489–494. [Google Scholar]
- 19. Froimson AI. Fracture of the coracoid process of the scapula. J Bone Joint Surg Am. 1978;60:710–711. [PubMed] [Google Scholar]
- 20. Gardner E, Gray DJ. Prenatal development of the human shoulder and acromioclavicular joints. Am J Anat. 1953;92:219–276. [DOI] [PubMed] [Google Scholar]
- 21. Goldberg RP, Vicks B. Oblique angled view for coracoid fractures. Skeletal Radiol. 1983;9:195–197. [DOI] [PubMed] [Google Scholar]
- 22. Holst AK, Christiansen JV. Epiphyseal separation of the coracoid process without acromioclavicular dislocation. Skeletal Radiol. 1998;27:461–462. [DOI] [PubMed] [Google Scholar]
- 23. Imatani RJ. Fractures of the scapula: a review of 53 fractures. J Trauma. 1975;15:473–478. [DOI] [PubMed] [Google Scholar]
- 24. Kan JH, Strouse PJ. Embryology, anatomy, and normal findings In: Coley BD, ed. Caffey’s Pediatric Diagnostic Imaging. 12th ed. Elsevier Saunders; 2013:1329–1346. [Google Scholar]
- 25. Kopecky KK, Bies JR, Ellis JH. CT diagnosis of fracture of the coracoid process of the scapula. Comput Radiol. 1984;8(5):325–327. [DOI] [PubMed] [Google Scholar]
- 26. Kuhns LR, Sherman MP, Poznanski AK, Holt JF. Humeral-head and coracoid ossification in the newborn. Radiology. 1973;107:145–149. [DOI] [PubMed] [Google Scholar]
- 27. Lambert SM. Shoulder girdle and arm In Standring S, ed. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41th ed. Elsevier; 2016:797–836. [Google Scholar]
- 28. Landoff GA. Eine bischer nicht beschriebene Schädigung am Processuscoracoideus. Acta Chir Scand. 1943;89:401–406. [Google Scholar]
- 29. Leijnen M, Steenvoorde P, Da Costa A, et al. Isolated apophyseal avulsion of the coracoid process: case report and review of literature. Acta Orthop Belg. 2009;75:262–264. [PubMed] [Google Scholar]
- 30. McGahan JP, Rab GT, Dublin A. Fractures of the scapula. J Trauma. 1980;20:880–883. [DOI] [PubMed] [Google Scholar]
- 31. Mohammed H, Skalski MR, Patel DB, et al. Coracoid process: the lighthouse of the shoulder. Radiographics. 2016;36:2084–2101. [DOI] [PubMed] [Google Scholar]
- 32. Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Montgomery SP, Loyd RD. Avulsion fracture of the coracoid epiphysis with acromioclavicular separation: report of two cases in adolescents and review of the literature. J Bone Joint Surg Am. 1977;59:963–965. [PubMed] [Google Scholar]
- 34. Mourgues G, Machenaud A, Fischer L, et al. Fractures de l’omoplate. Lyon Chir. 1973;69:47–50. [Google Scholar]
- 35. Mwaturura T, Bourne R. An unusual cause of shoulder pain: undisplaced Salter-Harris type I fracture of the coracoid process. Am J Orthop (Belle Mead NJ). 2009;38:e101–e103. [PubMed] [Google Scholar]
- 36. Nakagawa Y, Okumoto H, Sakamoto Y. Fractures of the coracoid process of the scapula: complex injury of the shoulder girdle [in Japanese]. Katakansetsu. 2007;31:323–327. [Google Scholar]
- 37. Nakama K, Gotoh M, Mitsui Y, et al. Epiphyseal fracture of the coracoid process occurring at the conjoined tendon origin. Case Rep Orthop. 2011;2011:329745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Newell ED. Review of over two thousand fractures in the past seven years. South Med J. 1927;20:644–647. [Google Scholar]
- 39. Nougarolis F, Mokrane FZ, Sans N, et al. Bone age estimation based on multislice computed tomography study of the scapula. Int J Legal Med. 2017;131:547–558. [DOI] [PubMed] [Google Scholar]
- 40. Ogawa K, Toyama Y, Ishige S, et al. Fracture of the coracoid process: its classification and pathomechanism [in Japanese]. Nihon Seikeigeka Gakkai Zasshi. 1990;64:909–919. [PubMed] [Google Scholar]
- 41. Ogawa K, Ikegami H, Takeda T, et al. Defining impairment and treatment of subacute and chronic fractures of the coracoid process. J Trauma. 2009;67:1040–1045. [DOI] [PubMed] [Google Scholar]
- 42. Ogden JA, Phillips SB. Radiology of postnatal skeletal development: VII. The scapula. Skeletal Radiol. 1983;9:157–169. [DOI] [PubMed] [Google Scholar]
- 43. Ogden JA. Skeletal Injury in the Child. 3rd ed Springer-Verlag, 2000. [Google Scholar]
- 44. Pedersen V, Prall WC, Ockert B, et al. Non-operative treatment of a fracture to the coracoid process with acromioclavicular dislocation in an adolescent. Orthop Rev (Pavia). 2014;6(3):5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Peterson HA, Madhok R, Benson JT, et al. Physeal fractures: part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14:423–430. [DOI] [PubMed] [Google Scholar]
- 46. Protass JJ, Stampfli FV, Osmer JC. Coracoid process fracture diagnosis in acromioclavicular separation. Radiology. 1975;116:61–64. [DOI] [PubMed] [Google Scholar]
- 47. Rowe CR. Fractures of the scapula. Surg Clin North Am. 1963;43:1565–1571. [DOI] [PubMed] [Google Scholar]
- 48. Schaefer HG. Clinical aspect of coracoid fractures [in German]. Chirurg. 1951;22:172–173. [PubMed] [Google Scholar]
- 49. Scheuer L, Black S. The pectoral girdle In: Developmental Juvenile Osteology. Academic Press; 2000:244–271. [Google Scholar]
- 50. Smith S. Note on the ossification of the scapula. J Anat. 1925;59(pt 4):387. [PMC free article] [PubMed] [Google Scholar]
- 51. Stone AV, Freehill MT. A 14-year-old male patient with chronic shoulder pain. “Rush Grand Rounds.” Orthopedics Today. March 2017. [Google Scholar]
- 52. Taga I, Yoneda M, Ono K. Epiphyseal separation of the coracoid process associated with acromioclavicular sprain: a case report and review of the literature. Clin Orthop Relat Res. 1986;207:138–141. [PubMed] [Google Scholar]
- 53. Wilber MC, Evans EB. Fractures of the scapula: an analysis of forty cases and a review of the literature. J Bone Joint Surg Am. 1977;59:358–362. [PubMed] [Google Scholar]
- 54. Zember JS, Rosenberg ZS, Kwong S, et al. Normal skeletal maturation and imaging pitfalls in the pediatric shoulder. Radiographics. 2015;35:1108–1122. [DOI] [PubMed] [Google Scholar]