Abstract
Background:
Medial patellofemoral ligament (MPFL) injuries are common in patients with acute lateral patellar dislocations, but the pattern of MPFL injuries is unclear, especially with respect to patient age.
Purpose:
The primary aim was to determine the prevalence of MPFL injuries according to the site of injury in patients with acute lateral patellar dislocations. The secondary aim was to compare the site of MPFL injuries in patients aged ≤16 versus >16 years.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic literature search was performed with PubMed, Embase, and CINAHL to identify articles published from January 1, 1999, to May 31, 2019, that examined the site of MPFL injuries in patients with acute patellar dislocations. The study design, sample size, age at injury, technique used for diagnosing MPFL injuries (magnetic resonance imaging, ultrasound, and/or surgery), and prevalence and site of MPFL injuries were extracted from each study. The pooled estimate of the proportion of MPFL injuries at each site was calculated (femur, patella, midsubstance, and combined sites of injury) as well as proportions stratified by age group (≤16 and >16 years).
Results:
The literature search yielded 420 unique articles, of which 52 were screened for eligibility; of these, 17 were excluded. Thus, a total of 35 articles (2558 patients) were included in the final analysis. The overall prevalence of MPFL injuries was 94.7% (95% CI, 91.2%-96.8%). Most MPFL injuries occurred at the patella (37.1% [95% CI, 30.8%-43.9%]), followed by the femur (36.8% [95% CI, 31.0%-43.0%]), combined sites (25.1% [95% CI, 20.7%-30.1%]), and the midsubstance (15.6% [95% CI, 13.2%-18.4%]). In patients aged ≤16 years, most MPFL injuries occurred at the patella (39.3% [95% CI, 27.9%-51.9%]), and in patients aged >16 years, most MPFL injuries occurred at the femur (47.2% [95% CI, 40.6%-54.0%]).
Conclusion:
The prevalence of MPFL injuries in patients with acute patellar dislocations varied by site of injury and by age. MPFL injuries at the patella were most prevalent overall and in children and adolescents, and MPFL injuries at the femur were more prevalent in adults.
Keywords: medial patellofemoral ligament, acute injury, patellar dislocation, meta-analysis
The annual incidence of acute lateral patellar dislocations ranges from 5.8 to 7.0 cases per 100,000 person-years in the general population and is as high as 29 cases per 100,000 person-years among those aged 10 to 17 years.13 The majority of first-time patellar dislocations occur during sports or physical activity (60%), often resulting from a direct blow to the knee or from a noncontact injury involving external rotation of the leg while the foot is planted.22,26,33 Other risk factors for acute patellar dislocations include female sex, family history, and patellofemoral dysplasia.17 Alterations in osseous or soft tissue structures, such as patella alta, trochlear dysplasia, and abnormalities of the medial patellofemoral ligament (MPFL), can lead to patellar dislocations.26 The MPFL is the primary ligamentous restraint of the patella and aids in preventing lateral patellar subluxation by providing 50% to 60% of lateral patellar translation control.2,10 Magnetic resonance imaging (MRI) has been found to be 85% sensitive and 70% accurate for diagnosing MPFL ruptures.32 As many as 78% to 100% of MPFLs are partially or completely ruptured on MRI after acute lateral patellar dislocations.11 MPFL repair or reconstruction is indicated for cases with recurrent instability, native soft tissue laxity, deficient bony stabilizers, and more severe MPFL tears.26 Repair should only be considered for patients with an initial patellar dislocation who are undergoing a concomitant procedure (eg, osteochondral repair) because MPFL repair has been shown to result in just as many recurrent dislocations as nonoperative management and more recurrent dislocations than MPFL reconstruction.31,35 MPFL injuries can occur at the femoral insertion, midsubstance, patellar attachment, or more than 1 of these sites.11,15
MPFL injuries at the femoral attachment tend to be more common in adults, while MPFL injuries at the patellar attachment tend to be more common in children and adolescents.10,14,26 However, most studies that have examined the prevalence of MPFL injuries by site of injury have done so using small samples of fewer than 100 patients, and only 1 small study compared the rate of MPFL injuries in children versus adults.6 Determining the site(s) of MPFL injuries in patients with acute lateral patellar dislocations can aid in treatment planning, especially for patients deemed surgical candidates.19
The primary aim of this systematic review was to determine the prevalence of MPFL injuries according to the site of injury in patients with acute lateral patellar dislocations. The secondary aim was to compare the site of MPFL injuries in skeletally immature (aged ≤16 years) versus skeletally mature (aged >16 years) patients. The primary hypothesis was that the site of MPFL injuries would vary among patients with an acute lateral patellar dislocation. The secondary hypothesis was that there would be more MPFL injuries at the patella in patients aged ≤16 years and more MPFL injuries at the femur in patients aged >16 years.
Methods
Literature Search and Selection Criteria
A systematic review of the literature pertaining to the site of MPFL injuries in patients with acute lateral patellar dislocations was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. An electronic search was performed on June 27, 2019, with PubMed, Embase, and CINAHL to identify articles published from January 1, 1999, through May 31, 2019. The search terms were the following: (“medial patellofemoral ligament” OR “MPFL”) AND (“tear” OR “rupture” OR “avulsion”) AND/OR (“acute” OR “first” OR “initial”) AND “patellar dislocation.” We included articles that were written in English and reported the site of MPFL injuries in patients with a primary acute lateral patellar dislocation. We excluded articles not published in English and studies of chronic patellar dislocations, secondary patellar dislocations, insufficient MPFL injury data for extraction, and studies whose data were published previously. There were 2 authors (M.A.K. and L.M.) who independently reviewed the results of the literature search to identify articles for inclusion and exclusion. In the event of discrepancies, the advice of the senior author (J.M.M.) was sought.
Level of Evidence and Quality Assessment
The level of evidence was determined based on criteria established by the Oxford Centre for Evidence-Based Medicine.29 The Downs and Black study quality assessment tool was used to score the methodological quality and risk of bias for each study.12 The maximum Downs and Black score (indicating good quality/low risk of bias) was 9 for case series, 15 for observational studies, and 32 for randomized controlled trials.
Data Extraction
The same 2 reviewers independently extracted the following data from each article into a standardized spreadsheet: study design, sample size, age at injury, method for diagnosing MPFL injuries (MRI, ultrasound, and/or surgery), overall prevalence of MPFL injuries, and site of MPFL injuries. The site of MPFL injuries included the (1) femur, (2) patella, (3) midsubstance, or (4) combined sites that involved the femur, patella, and/or midsubstance.
Statistical Analysis
The pooled estimate of the proportion of MPFL injuries at each site was calculated (femur, patella, midsubstance, and combined sites of injury) as well as the overall proportion of MPFL injuries. The proportion of MPFL injuries was also stratified by age group (≤16 and >16 years). To assess heterogeneity, the I 2 (significance level of I 2 > 50%) and Cochran Q statistic (significance level of P < .05) were calculated. Tests of heterogeneity were found to be significant, and thus, random-effects models were used. Forest plots with proportions and 95% CIs are reported. Meta-analyses were performed with Comprehensive Meta-Analysis Software (Version 3; Biostat).
Results
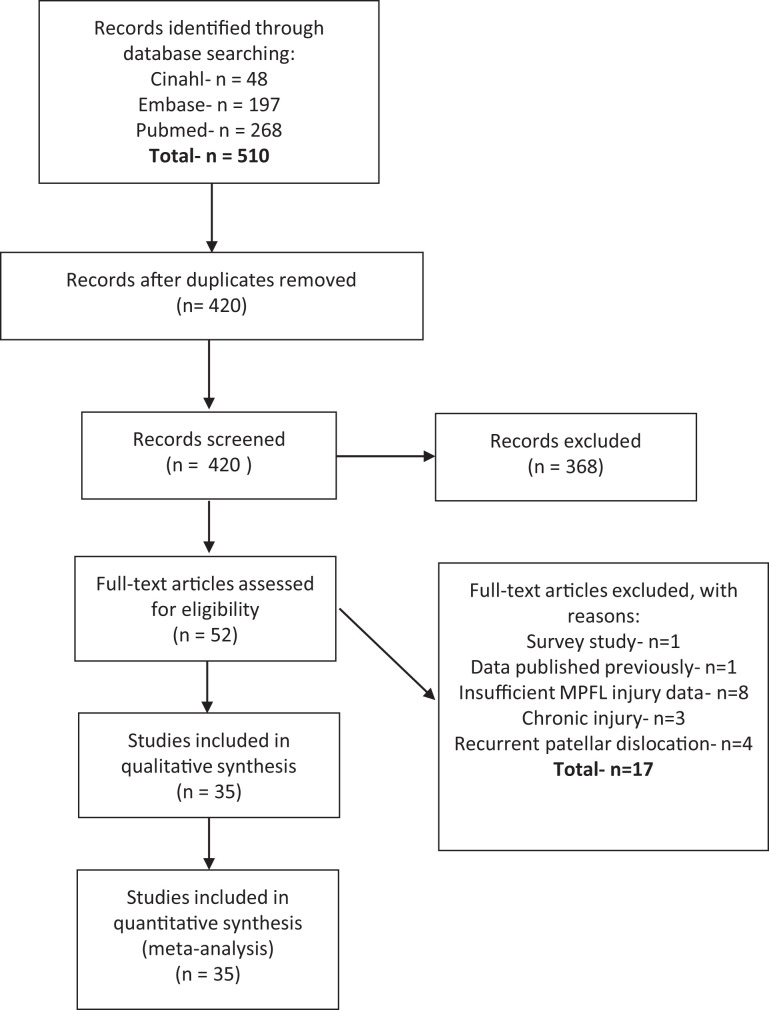
The initial search yielded 420 unique articles, of which 52 were screened for eligibility. Of the 52 full-text articles, 17 were excluded because they involved survey research, data were previously published, there was insufficient reporting of MPFL injury data, they included chronic injuries, or they included recurrent patellar dislocations. The final analysis included 35 articles with a total of 2558 patients (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flowchart.
As demonstrated in Appendix Table A1, the majority of included studies were level 4 evidence (n = 28; 80.0%), followed by level 2 (n = 3; 8.6%), level 3 (n = 3; 8.6%), and level 1 (n = 1; 2.8%). Most case series (n = 27) and observational studies (n = 5) were of good quality and had a low risk of bias based on Downs and Black scores; however, the randomized controlled trials (n = 3) were of lower quality, mainly because of lack of blinding, loss to follow-up, and lack of power analysis. The mean patient age was ≤16 years in 10 studies (28.6%) and >16 years in 23 studies (65.7%); age was not reported in 2 studies (5.7%). Most studies diagnosed MPFL injuries on preoperative MRI (n = 25; 71.4%), followed by surgical confirmation in 9 studies (25.7%) and a diagnosis on ultrasound in 1 study (2.9%).
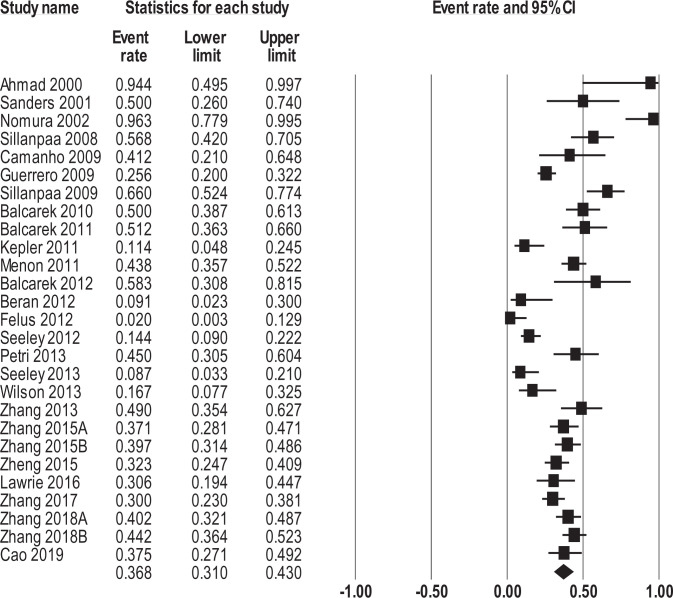
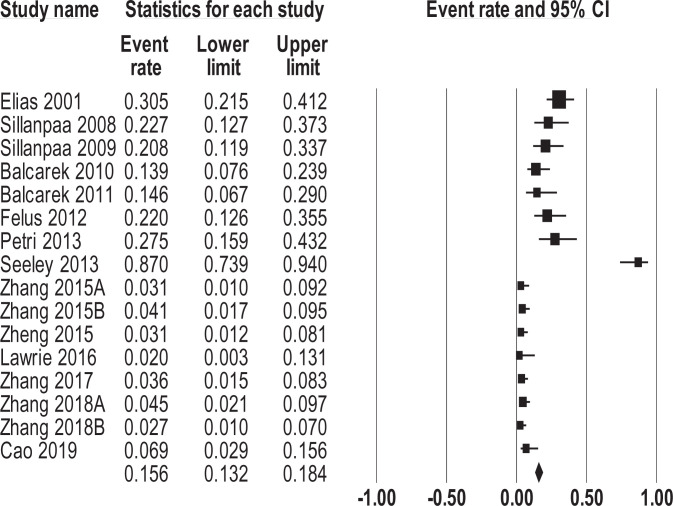
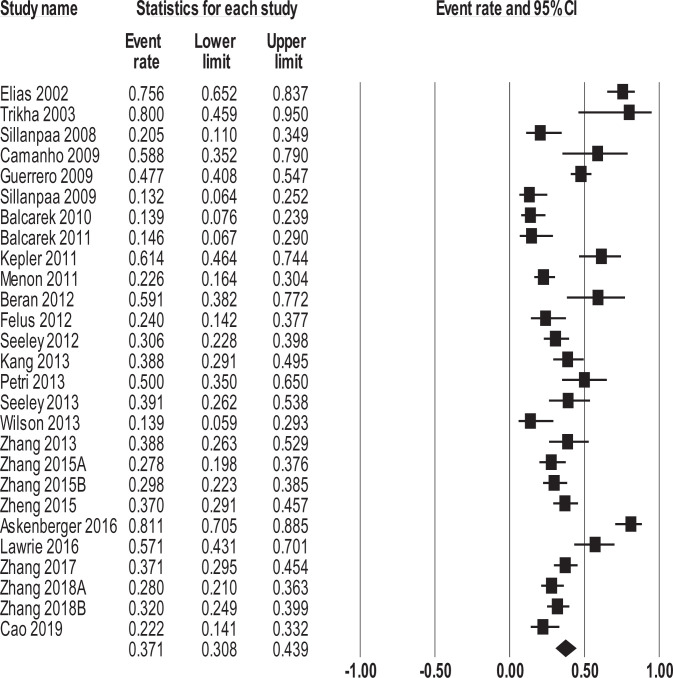
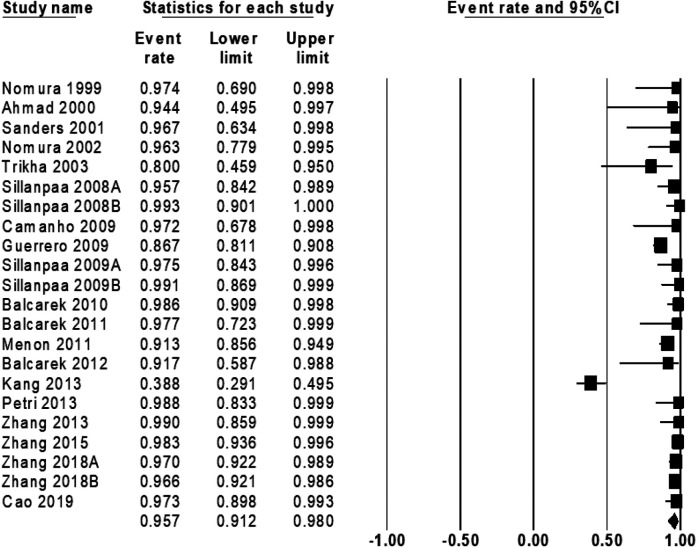
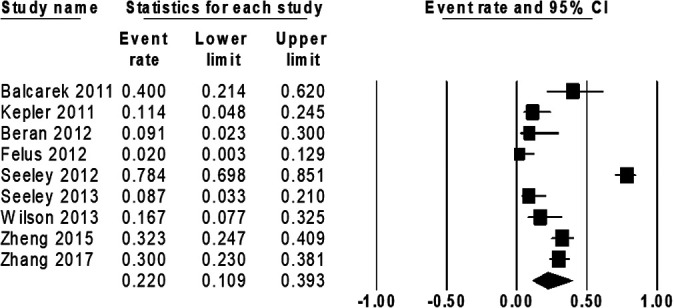
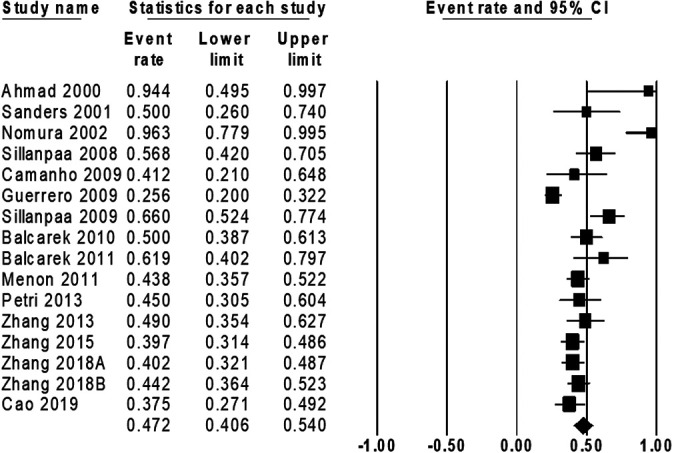
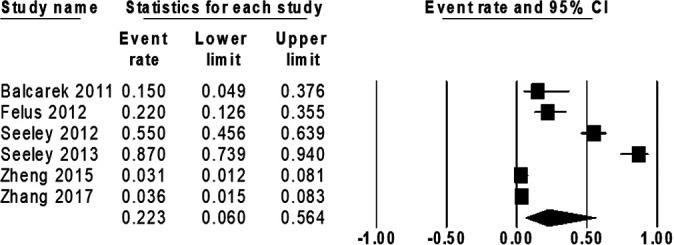
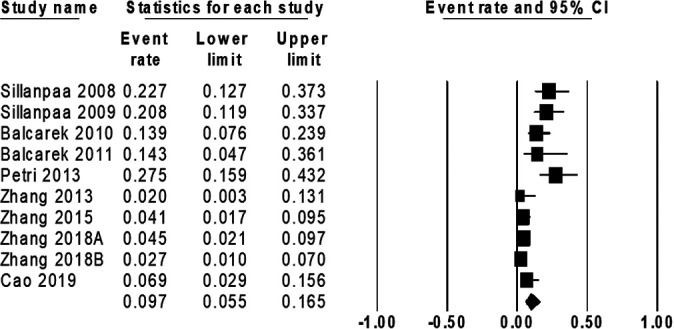
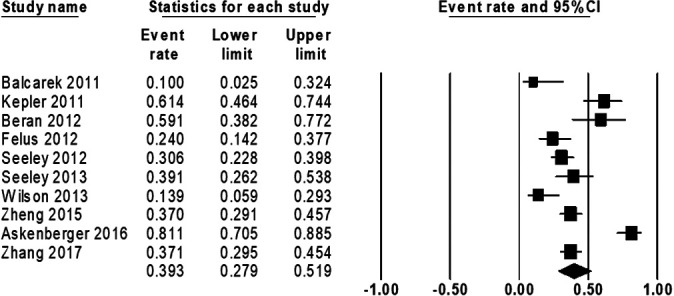
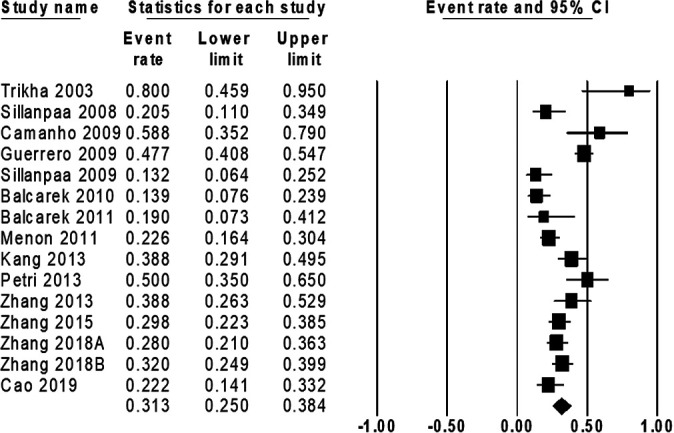
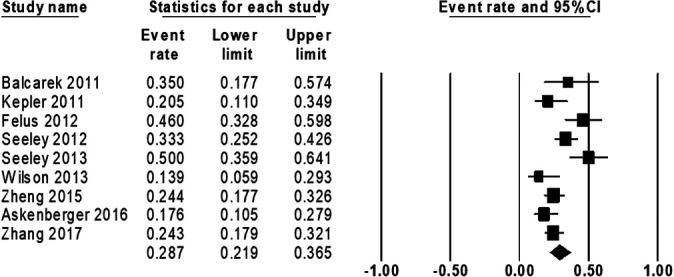
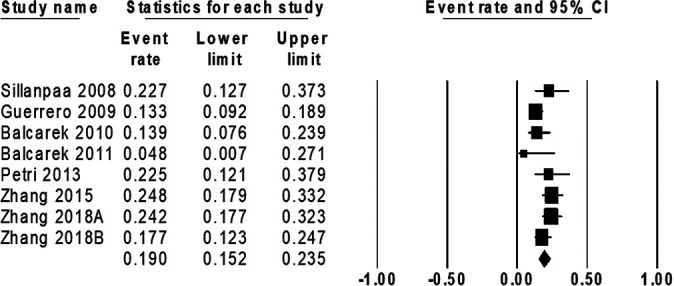
The overall pooled prevalence of MPFL injuries was 94.7% (95% CI, 91.2%-96.8%) and was slightly lower in studies with a mean patient age ≤16 years (90.8% [95% CI, 81.8%-95.6%]) compared with studies with a mean patient age >16 years (95.7% [95% CI, 91.2%-98.0%]) (Appendix Figures A1 -A4). The site of MPFL injuries varied (Figures 2 -5). Most MPFL injuries occurred at the patella (37.1% [95% CI, 30.8%-43.9%]), followed by the femur (36.8% [95% CI, 31.0%-43.0%]), combined sites (25.1% [95% CI, 20.7%-30.1%]), and the midsubstance (15.6% [95% CI, 13.2%-18.4%]).
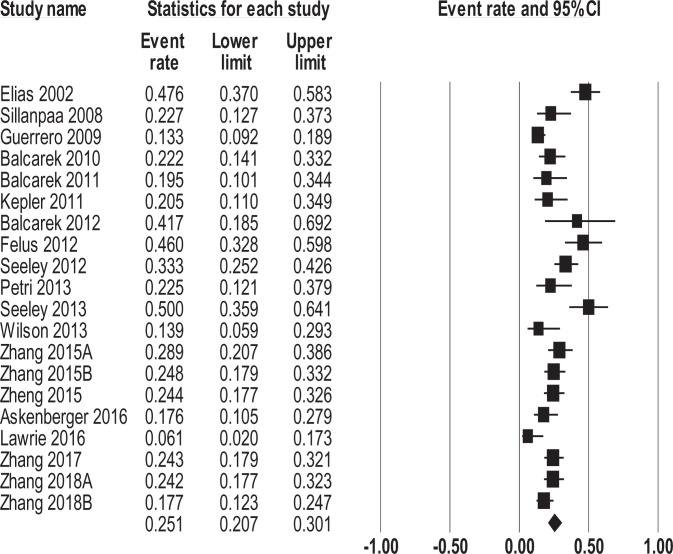
Figure 2.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the femur. Tests of heterogeneity: Q = 147.8 (P < .001); I 2 = 82%.
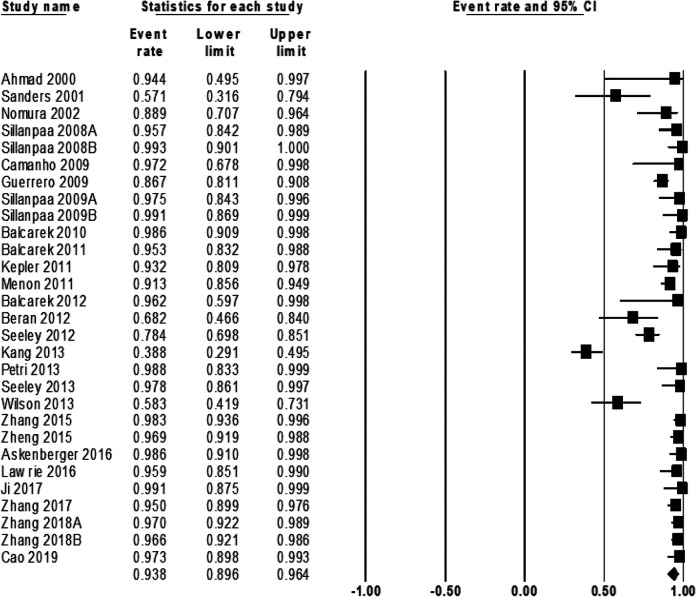
Figure 3.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the midsubstance. Tests of heterogeneity: Q = 164.8 (P < .001); I 2 = 91%.
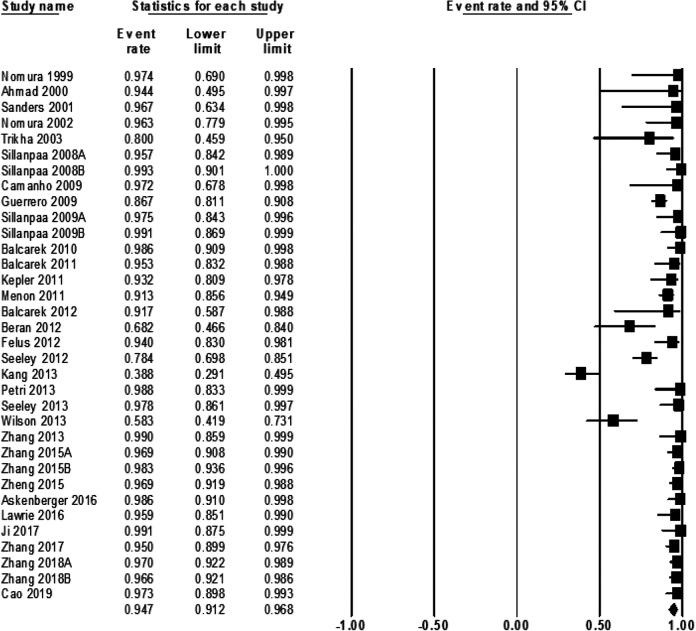
Figure 4.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the patella. Tests of heterogeneity: Q = 212.1 (P < .001); I 2 = 88%.
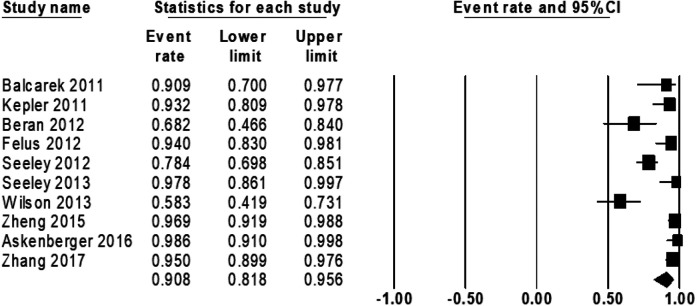
Figure 5.
Forest plot illustrating the prevalence of combined sites of medial patellofemoral ligament (MPFL) injuries. Combined MPFL injuries involved the femur, midsubstance, and/or patella. Tests of heterogeneity: Q = 82.7 (P < .001); I 2 = 77%.
Among studies with a mean patient age ≤16 years, most MPFL injuries occurred at the patella (39.3% [95% CI, 27.9%-51.9%]), followed by combined sites (28.7% [95% CI, 21.9%-36.5%]), the midsubstance (22.3% [95% CI, 6.0%-56.4%]), and the femur (22.0% [95% CI, 10.9%-39.3%]) (Appendix Figures A5, A7, A9, and A11). Among studies with a mean patient age >16 years, most MPFL injuries occurred at the femur (47.2% [95% CI, 40.6%-54.0%]), followed by the patella (31.3% [95% CI, 25.0%-38.4%]), combined sites (19.0% [95% CI, 15.2%-23.5%]), and the midsubstance (9.7% [95% CI, 5.5%-16.5%]) (Appendix Figures A6, A8, A10, and A12).
Discussion
We found that the overall prevalence of MPFL injuries was 94.7% and conclude that disruption of the MPFL can be considered the “essential lesion” of acute lateral patellar dislocations. MPFL injuries occurred most commonly at the patellar attachment (37.1%) and femoral insertion (36.8%), followed by combined sites (25.1%) and the midsubstance (15.6%). As hypothesized, most MPFL injuries occurred at the patella in patients aged ≤16 years (39.3%) and at the femur in patients aged >16 years (47.2%).
We found that the prevalence for both femoral insertion and patellar attachment MPFL injuries were approximately 37%, with slightly more injuries at the patellar attachment. There has been conflicting evidence regarding the localization of MPFL injuries in patients with acute patellar dislocations. Historically, the femoral insertion has been thought to be the most common site of MPFL injuries. Of the 35 articles included in our systematic review, the most common site of MPFL injuries was the femoral insertion in 15 studies,‡ the patellar attachment in 12 studies,§ the midsubstance in 2 studies,33,34 combined sites in 1 study,16 and was not reported in 5 studies.20,27,28,36,38 There are a number of factors that may account for the discrepancies in data regarding the localization of MPFL injuries, including (1) the lack of an accurate definition of a complete MPFL rupture on MRI, (2) not being able to discern the dynamic status of the ligament on MRI after a patellar dislocation, and (3) difficulty in visualizing the oblique course of the fibers of the MPFL in relation to standard planes used for MRI.16 It has also been shown that the pattern of MPFL injuries is associated with predisposing anatomic factors for an acute patellar dislocation.4 For instance, an injury at the patellar insertion is more likely to occur when the tibial tubercle–trochlear groove distance is increased and the values of trochlear dysplasia vary for patellar and femoral MPFL injuries. Also, variation in the diagnostic method (ie, MRI, ultrasound, surgical visualization) and small sample sizes make it difficult to compare the localization of MPFL injuries between studies.
Similar to previous research,10,14,26 we observed an age difference in the localization of MPFL injuries, with patellar-sided injuries being more common in patients aged ≤16 years and femoral-sided injuries being more common in patients aged >16 years. To our knowledge, only 1 study directly compared the localization of MPFL injuries between children and adults with acute patellar dislocations, finding no age-based difference in MPFL injury patterns.6 Femoral-sided injuries were most common in both children and adults in that study; however, the sample size was small (N = 43) and may not be representative of all acute patellar dislocations. On the other hand, a number of studies restricted to the recruitment of children and adolescents found patellar-sided MPFL injuries to be most common among this age group.3,16,23,33,34,45,49 Felus and Kowalczyk16 found that the patellar attachment was the most common site of MPFL injuries in children and adolescents, and all but 2 of the patients with patellar-sided MPFL injuries also had an avulsion fracture of the medial patellar border. The authors speculated that younger persons may be more susceptible to patellar-sided injuries because the medial patellar border stays cartilaginous until age 16 to 18 years, unlike the distal femoral epiphysis, which ossifies around age 13 to 15 years. This chondro-osseous boundary is susceptible to tension forces, resulting in marginal avulsion fractures of the patella or detachment injuries of the MPFL at the patella in children and adolescents.49 Seeley et al33 found that the articular cartilage sulcus angle may be associated with the pattern of MPFL injuries in children and adolescents, such that patellar-sided injures were associated with a steeper articular sulcus angle and femoral-sided injuries were associated with a flattened articular sulcus angle. Zheng et al49 found that 37% of 127 children and adolescents with acute patellar dislocations had a patellar-sided MPFL injury. The authors speculated that the patellar attachment of the MPFL in younger patients may be weaker and more easily injured because the fibers of the MPFL and the vastus medialis obliquus may not be fully combined yet on the patellar side; however, no anatomic studies have confirmed this hypothesis.
The operative management of MPFL ruptures is considered the gold standard for addressing recurrent instability; however, choosing between MPFL repair and reconstruction remains controversial. Similar subjective outcome scores have been demonstrated for MPFL repair and MPFL reconstruction, although MPFL repair tends to result in more recurrent dislocations.35,41 Therefore, properly diagnosing the location and severity of MPFL injuries is essential for treatment planning and avoids a one-size-fits-all approach to surgical correction when the injury site varies significantly. According to our review, most practitioners used MRI as the diagnostic tool of choice, and this study encourages our radiology colleagues to describe specifically the site of MPFL injuries to enhance reading accuracy. We support performing MRI on patients with a patellar instability event to identify the location of MPFL injuries and to evaluate for intra-articular abnormalities. In this way, both acute and delayed surgery can be indicated appropriately.
To our knowledge, this study is the only systematic review that has examined the localization of MPFL injuries in patients with acute lateral patellar dislocations and, to date, is the largest study on this topic (N = 2558). However, this study is not without limitations. The method used for diagnosing MPFL injuries varied between studies and may have led to confounding. However, the risk of confounding is likely low because the majority of studies confirmed MPFL injuries using MRI. Patellar medial margin fractures and articular cartilage status may be associated with the MPFL injury pattern and could also be potential confounders, but this information was not reported in most studies, which precluded any further analysis. Our analyses stratified by age should be interpreted cautiously. We were unable to conduct a direct statistical comparison of injury rates between age groups. Although there were more patellar-sided injuries in patients aged ≤16 years, for instance, the 95% CI did overlap with patients aged >16 years, which suggests that this difference is not statistically significant. Most studies were level 4 case series, although we found a low risk of bias in the majority of studies, and case series are appropriate for determining prevalence rates. Finally, this study may be at risk for publication and language bias because we only included peer-reviewed articles published in English.
In conclusion, the prevalence of MPFL injuries in patients with an acute patellar dislocation varied by site of injury and by age. MPFL injuries at the patella were most prevalent overall and in children and adolescents, and MPFL injuries at the femur were more prevalent in adults.
Appendix
Table A1.
Study Characteristics and MPFL Dataa
| First Author (Year) | Study Design (LOE) | DB Scoreb | Sample Size, | Age at Injury,c y | Diagnosis Method | Prevalence of MPFL Injuries, n (%) | Location of MPFL Injuries, n (%) |
|---|---|---|---|---|---|---|---|
| Nomura27 (1999) | Case series (4) | 9 | 18 | 19.6 (12-38) | Surgery | 7/18 (38.9) avulsions, 10/18 (55.6) ruptures, 17/18 (94.4) total injuries | NR |
| Ahmad1 (2000) | Case series (4) | 9 | 8 | 32 (16-56) | MRI | 8/8 (100.0) | 8/8 (100.0) at FEM |
| Sanders32 (2001) | Case series (4) | 9 | 14 | 29.6 (12-60) | MRI (mean, 11 d from injury) and arthroscopic surgery (mean, 21 d from imaging) | 8/14 (57.1) with complete disruption on MRI, 14/14 (100.0) with some degree of MPFL injury during arthroscopic surgery | On MRI: 4/14 (28.6) with edema isolated to FEM, 1/14 (7.1) with focal edema isolated to PAT, 5/14 (35.7) with diffuse edema beginning at FEM and extending into MID, 4/14 (28.6) with diffuse edema extending entire length of MPFL from FEM to PAT During arthroscopic surgery: 7/14 (50.0) with complete disruption near FEM or avulsion of femur, 7/14 (50.0) with stretching or partial tear of MPFL and adjacent soft tissue edema |
| Elias15 (2002) | Case-control (3) | 13 | 179 (82 knees [81 patients] with acute lateral patellar dislocations, 98 controls) | Cases: 20 (9-57) Controls: 29 (13-49) |
MRI (mean, 21 d after injury) | NR | 62/82 (75.6) at PAT, 25/82 (30.5) at MID, 39/82 (47.6) with COM injuries |
| Nomura28 (2002) | Case series (4) | 8 | 27 | 18 (13-29) | MRI (mean, 6 d after injury) and open exploration | 24/27 (88.9) on MRI, 26/27 (96.3) during open exploration | 13/27 (48.1) with substantial-type tears on MRI, 10/27 (37.0) with avulsion tears, 16/27 (59.3) with substantial-type tears during open explorationd |
| Trikha40 (2003) | Case series (4) | 9 | 10 | Median = 20.5 (13-37) | US | 8/10 (80.0) | 8/10 (80.0) at PAT |
| Sillanpää37 (2008) | Cohort (2) | 12 | 76 (30 operative, 46 nonoperative)e | Median = 20 (19-22) | MRI (mean, 4 d after injury) | 44/46 (95.7) | 25/46 (54.3) at FEM, 9/46 (19.6) at PAT, 10/46 (21.7) at MID, 10/46 (21.7) with COM injuries (MID and PAT injuries also had signs of partial disruption at femur) |
| Sillanpää36 (2008) | Case series (4) | 9 | 73 | Median = 20 (18-23) | MRI (mean, 4 d after injury) and open surgery | 73/73 (100.0) both on MRI and during open surgeryf | NR |
| Camanho8 (2009) | RCT (2) | 21 | 33 (17 operative, 16 nonoperative) | Operative: 24.6 (15-33) Nonoperative: 26.8 (12-74) |
MRIg | 17/17 (100.0) | 10/17 (58.8) at PAT, 7/17 (41.2) at FEM |
| Guerrero18 (2009) | Case series (4) | 9 | 195 | 23 (10-56) | MRI | 169/195 (86.7) with ruptures, 26/195 (13.3) with attenuation of MPFL without rupture | 93/195 (47.7) at PAT, 50/195 (25.6) at FEM, 26/195 (13.3) with COM injuries at PAT + FEM |
| Sillanpää38 (2009) | RCT (1) | 23 | 40 (18 operative, 22 nonoperative) | Median = 20 (19-22) | MRI (median, 3 d after injury) | 17/18 (94.4) injuries in operative group, 22/22 (100.0) injuries in nonoperative group, 39/40 (97.5) total injuries | NR |
| Sillanpää39 (2009) | Cohort (3) | 13 | 53 | 20 (19-23) | MRI (mean, 3 d after injury) | 53/53 (100.0) | 35/53 (66.0) at FEM, 7/53 (13.2) at PAT, 11/53 (20.8) at MID |
| Balcarek4 (2010) | Case-control (4) | 13 | 146 (73 patients with acute lateral patellar dislocations, 73 controls) | 23.6 | MRI (within 7 wk of injury) | 35/73 (47.9) partial tears, 37/73 (50.7) complete tears, 72/73 (98.6) total tears | 36/73 (49.3) at FEM, 10/73 (13.7) at MID, 10/73 (13.7) at PAT, 16/73 (21.9) with COM injuries (13 at PAT + FEM and 3 at FEM + MID) |
| Balcarek6 (2011) | Case-control (3) | 13 | 43 (22 children and adolescents with acute patellar dislocations, 21 adults with acute patellar dislocations) | Children: 14.2 (11-15) Adults: 25.7 (18-38) |
MRI (within 13 d of injury) | Children: 12/22 (54.5) partial tears, 8/22 (36.4) complete tears, 20/22 (90.9) total tears Adults: 11/21 (52.4) partial tears, 10/21 (47.6) complete tears, 21/21 (100.0) total tears |
Children: 8/22 (36.4) at FEM, 7/22 (31.8) with COM injuries at FEM + PAT, 3/22 (13.6) at MID, 2/22 (9.1) at PAT Adults: 13/21 (61.9) at FEM, 1/21 (4.8) with COM injuries at FEM + PAT, 3/21 (14.3) at MID, 4/21 (19.0) at PAT |
| Kepler23 (2011) | Case series (4) | 8 | 44 | 14.3 (9.8-17.8) | MRI | 41/44 (93.2) | 27/44 (61.4) at PAT, 5/44 (11.4) at FEM, 9/44 (20.5) with COM injuries (5 at PAT + FEM and 4 at MID + FEM or PAT) |
| Menon25 (2011) | Case series (4) | 8 | 150 | 28 (10-72) | MRI | 137/150 (91.3) | 60/150 (40.0) at FEM, 31/150 (20.7) at PAT, 46/150 (30.7) with diffuse pattern of injury |
| Balcarek5 (2012) | Case series (4) | 9 | 12 patients with acute patellar dislocationsh | Median = 18 (13-42) | MRI (mean, 3 d after injury) and arthroscopic surgery | On MRI: 7/12 (58.3) partial tears, 5/12 (41.7) complete tears, 12/12 (100.0) total tears During arthroscopic surgery: 11/12 (91.7) |
On MRI: 7/12 (58.3) at FEM, 5/12 (41.7) with COM injuries at PAT + FEM, 7/12 (58.3) with osteochondral flake fractures Arthroscopic surgery failed to show direct injuries of femoral MPFL in all patients with MPFL tears at FEM and COM injuries. After transection of synovial membrane, hematoma became obvious during arthroscopic surgery and could be confirmed as injury of MPFL by mini-open exploration in 11/12 patients. |
| Beran7 (2012) | Case series (4) | 9 | 21 patients (22 knees) with weightbearing lesions of LFC | 13.8 | MRI | 15/22 (68.2) | 13/22 (59.1) at PAT with combined osteochondral fractures or bone bruises of midlateral weightbearing region of LFC, 2/22 (9.1) at FEM |
| Felus16 (2012) | Case series (4) | 8 | 50 | 14.75 (10.5-17.5) | US and surgery | 26/50 (52.0) partial ruptures, 21/50 (42.0) complete ruptures, 47/50 (94.0) total ruptures | 12/50 (24.0) at PAT, 11/50 (22.0) at MID, 1/50 (2.0) at FEM, 23/50 (46.0) with COM injuries (10 at PAT + MID, 8 at PAT + FEM, 4 at PAT + FEM + MID, and 1 at MID + FEM) |
| Seeley33 (2012) | Case series (4) | 8 | 111 | 14.9 (11-18) | MRI (mean, 17 d after injury) | 87/111 (78.4) | 16/111 (14.4) at FEM, 34/111 (30.6) at PAT, 37/111 (33.3) with COM injuries at PAT and FEM, 61/111 (55.0) with MID attenuation |
| Kang21 (2013) | Case series (4) | 9 | 85 patients (33 in overlap region of MPFL, 52 in nonoverlap region of MPFL)i | 19.7 | MRI | 33/85 (38.8) | 33/85 (38.8) at PAT |
| Petri30 (2013) | Case series (4) | 8 | 40 | 24.6 (16-40) | MRI (within 3 mo of injury) | 17/40 (42.5) partial tears, 23/40 (57.5) complete tears, 40/40 (100.0) total tears | 20/40 (50.0) at PAT, 11/40 (27.5) at MID, 18/40 (45.0) at FEM, 9/40 (22.5) with COM injuries |
| Seeley34 (2013) | Case series (4) | 9 | 46 | 14.6 (11-18) | MRI (mean, 12 d after injury) | 45/46 (97.8) | 4/46 (8.7) at FEM, 18/46 (39.1) at PAT, 23/46 (50.0) with COM injuries at PAT + FEM, 40/46 (87.0) with MID attenuation |
| Wilson42 (2013) | Case series (4) | 9 | 36 | 14.5 (8-17) | MRI (mean, 35 d [range, 5-135 d] after injury) | 5/36 (13.9) sprains, 16/36 (44.4) tears, 21/36 (58.3) total injuries | 5/36 (13.9) at PAT, 6/36 (16.7) at FEM, 5/36 (13.9) with COM injuries at PAT + FEM |
| Zhang47 (2013) | Case series (4) | 9 | 49 | Median = 24.5 (16-41) | US (within 14 d of injury) and surgery | 21/49 (42.9) partial tears, 28/49 (57.1) complete tears, 49/49 (100.0) total tears | 9 partial tears at FEM, 8 at PAT, and 1 at MID were diagnosed on US and confirmed during surgery. 15 complete tears at FEM and 11 at PAT were confirmed during surgery. 1 partial tear at PAT and 2 partial tears at FEM were misinterpreted as complete tears on US, and 1 complete tear at FEM and another at PAT were misinterpreted as partial tears on US. |
| Zhang43 (2015) | Case series (4) | 8 | 97 | 22 (9-44) | MRI, US, and surgery | Partial tears: 69/97 (71.1 ) on US, 62/97 (63.9) on MRI, 41/97 (42.3) during surgery Complete tears: 44/97 (45.4) on US, 41/97 (42.3) on MRI, 53/97 (54.6) during surgery Total tears: 94/97 (96.9) during surgery |
During surgery: 36/97 (37.1) at FEM, 27/97 (27.8) at PAT, 3/97 (3.1) at MID, 28/97 (28.9) with COM injuries (5 at PAT + FEM, 10 at MID + PAT, 8 at FEM + MID, and 5 at MID + PAT + FEM) |
| Zhang44 (2015) | Case series (4) | 8 | 121 | 25 (18-44) | MRI | 48/121 (39.7) partial tears, 71/121 (58.7) complete tears, 119/121 (98.3) total tears | 48/121 (39.7) at FEM, 36/121 (29.8) at PAT, 5/121 (4.1) at MID, 30/121 (24.8) with COM injuries (16 at FEM + PAT, 8 at FEM + MID, 4 at PAT + MID, and 2 at FEM + MID + PAT) |
| Zheng49 (2015) | Case series (4) | 8 | 127 | 14.1 (9-14) | MRI | 54/127 (42.5) partial tears, 69/127 (54.3) complete tears, 123/127 (96.9) total tears | 47/127 (37.0) at PAT, 41/127 (32.3) at FEM, 4/127 (3.1) at MID, 31/127 (24.4) with COM injuries (14 at PAT + FEM, 8 at PAT + MID, 5 at FEM + MID, and 4 at MID + PAT + FEM) |
| Askenberger3 (2016) | Case series (4) | 9 | 74 | 13.1 (9-14) | MRI and arthroscopic surgery | 73/74 (98.6) | On MRI: 44/74 (59.5) at PAT, 26/74 (35.1) with COM injuries (18 at PAT + FEM, 7 at PAT + MID, and 1 at PAT + FEM + MID), 3/74 (4.1) at FEM During arthroscopic surgery: 60/74 (81.1) at PAT (49/60 were complete tears), 13/74 (17.6) with COM injuries (PAT + blood-tinged synovium toward femoral insertion) |
| Lawrie24 (2016) | Case series (4) | 8 | 47 patients (49 MPFL repairs) | NR | MRI | 47/49 (95.9) | 28/49 (57.1) at PAT, 15/49 (30.6) at FEM, 3/49 (6.1) with COM injuries at PAT + FEM, 1/49 (2.0) at MID |
| Ji20 (2017) | RCT (2) | 24 | 56 (30 operative, 26 nonoperative) | NR | MRI (within 3 wk of injury) | 56/56 (100.0) | NR |
| Zhang45 (2017) | Case series (4) | 8 | 140 | 14.3 (9-17) | MRI | 58/140 (41.4) partial tears, 75/140 (53.6) complete tears, 133/140 (95.0) total tears | 52/140 (37.1) at PAT, 42/140 (30.0) at FEM, 5/140 (3.6) at MID, 34/140 (24.3) with COM injuries (17 at FEM + PAT, 8 at PAT + MID, 5 at FEM + MID, and 4 at FEM + MID + PAT) |
| Zhang46 (2018) | Case series (4) | 8 | 132 | 24 (18-44) | MRI | 52/132 (39.4) partial tears, 76/132 (57.6) complete tears, 128/132 (97.0) total tears | 53/132 (40.2) at FEM, 37/132 (28.0) at PAT, 6/132 (4.5) at MID, 32/132 (24.2) with COM injuries |
| Zhang48 (2018) | Case series (4) | 8 | 147 | 20 (8-42) | MRI | 62/147 (42.2) partial tears, 80/147 (54.4) complete tears, 142/147 (96.6) total tears | 47/147 (32.0) at PAT, 65/147 (44.2) at FEM, 4/147 (2.7) at MID, 26/147 (17.7) with COM injuries |
| Cao9 (2019) | Case series (4) | 8 | 74 | 21.1 (9-42) | MRI | 19/74 (25.7) partial tears, 53/74 (71.6) complete tears, 72/74 (97.3) total tears | 16/74 (21.6) at PAT (type 2a: complete tear and osteochondral avulsion fracture without articular cartilage), 5/74 (6.8) at MID (type 2b: complete tear), 27/74 (36.5) at FEM (type 2c: complete tear and osteochondral avulsion fracture without articular cartilage), 5/74 (6.8) with type 3 MPFL injuries (fracture of patella’s medial facet affecting articular surface) |
aCOM, combined site involving more than 1 location; DB, Downs and Black; FEM, femoral attachment; LFC, lateral femoral condyle; LOE, level of evidence; MID, midsubstance; MPFL, medial patellofemoral ligament; MRI, magnetic resonance imaging; NR, not reported; PAT, patellar insertion; RCT, randomized controlled trial; US, ultrasound.
bThe maximum scores (indicating good quality/low risk of bias) were 9 for case series, 15 for observational studies, and 32 for RCTs.
cValues are presented as mean or mean (range) unless otherwise indicated.
dNomura et al28 defined substantial-type tears as ruptures in the substance of the ligament itself, especially near the femoral attachment. An avulsion tear was defined as a detachment-type injury of the femoral attachment of the MPFL. For analysis, we considered both substantial-type and avulsion tears as MPFL injuries at the femur.
ePreoperative MRI data were only available for the 46 patients who underwent nonoperative management.
fA total of 28 of 73 patients had an MRI scan available, and only 3 patients underwent open surgery.
gMRI scans were only available for 17 patients in the operative group.
hThere were 10 patients excluded with recurrent patellar dislocations.
iKang et al21 defined the overlap region as an injury from the dividing point to the medial patellar margin and the nonoverlap region as an injury from the dividing point to the femoral origin. We only included data from cases with MPFL injuries in the overlap region in our analysis.
Figure A1.
Forest plot illustrating the overall prevalence of medial patellofemoral ligament (MPFL) injuries. All diagnostic methods for MPFL injuries were included. For studies that reported the prevalence of MPFL injuries based on both imaging and surgical findings, surgical findings were included in the analysis. Q = 261.8 (P < .001); I 2 = 87%.
Figure A2.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries confirmed by magnetic resonance imaging. Q = 251.2 (P < .001); I 2 = 89%.
Figure A3.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries in studies with a mean patient age ≤16 years. Q = 62.5 (P < .0001); I 2 = 86%.
Figure A4.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries in studies with a mean patient age >16 years. Q = 183.4 (P < .001); I 2 = 89%.
Figure A5.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the femur in studies with a mean patient age ≤16 years. Q = 111.1 (P < .0001); I 2 = 93%.
Figure A6.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the femur in studies with a mean patient age >16 years. Q = 60.8 (P < .001); I 2 = 75%.
Figure A7.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the midsubstance in studies with a mean patient age ≤16 years. Q = 123.0 (P < .0001); I 2 = 96%.
Figure A8.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the midsubstance in studies with a mean patient age >16 years. Q = 44.6 (P < .001); I 2 = 80%.
Figure A9.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the patella in studies with a mean patient age ≤16 years. Q = 74.9 (P < .0001); I 2 = 88%.
Figure A10.
Forest plot illustrating the prevalence of medial patellofemoral ligament injuries at the patella in studies with a mean patient age >16 years. Q = 73.4 (P < .0001); I 2 = 81%.
Figure A11.
Forest plot illustrating the prevalence of combined sites of medial patellofemoral ligament (MPFL) injuries in studies with a mean patient age ≤16 years. Combined MPFL injuries involved the femur, midsubstance, and/or patella. Q = 29.9 (P < .0001); I 2 = 73%.
Figure A12.
Forest plot illustrating the prevalence of combined sites of medial patellofemoral ligament (MPFL) injuries in studies with a mean patient age >16 years. Combined MPFL injuries involved the femur, midsubstance, and/or patella. Q = 13.3 (P < .0001); I 2 = 47%.
Footnotes
Final revision submitted May 28, 2020; accepted June 19, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson Jr. Foundation. J.M.M. has received research support from Carestream Health, educational support from Arthrex, and hospitality payments from Linvatec. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahmad CS, Stein BE, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation: a review of eight cases. Am J Sports Med. 2000;28(6):804–810. [DOI] [PubMed] [Google Scholar]
- 2. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10(3):215–220. [DOI] [PubMed] [Google Scholar]
- 3. Askenberger M, Arendt EA, Ekstrom W, Voss U, Finnbogason T, Janarv PM. Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. Am J Sports Med. 2016;44(1):152–158. [DOI] [PubMed] [Google Scholar]
- 4. Balcarek P, Ammon J, Frosch S, et al. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy. 2010;26(7):926–935. [DOI] [PubMed] [Google Scholar]
- 5. Balcarek P, Walde TA, Frosch S, Schuttrumpf JP, Wachowski MM, Sturmer KM. MRI but not arthroscopy accurately diagnoses femoral MPFL injury in first-time patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1575–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Balcarek P, Walde TA, Frosch S, et al. Patellar dislocations in children, adolescents and adults: a comparative MRI study of medial patellofemoral ligament injury patterns and trochlear groove anatomy. Eur J Radiol. 2011;79(3):415–420. [DOI] [PubMed] [Google Scholar]
- 7. Beran MC, Samora WP, Klingele KE. Weight-bearing osteochondral lesions of the lateral femoral condyle following patellar dislocation in adolescent athletes. Orthopedics. 2012;35(7):e1033–e1037. [DOI] [PubMed] [Google Scholar]
- 8. Camanho GL, Viegas Ade C, Bitar AC, Demange MK, Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–625. [DOI] [PubMed] [Google Scholar]
- 9. Cao H, An Q, Gou B, et al. A new classification of injury patterns of the medial patellofemoral ligament after acute lateral patella dislocation detected using magnetic resonance imaging studies. Injury. 2019;50(2):534–540. [DOI] [PubMed] [Google Scholar]
- 10. Chotel F, Berard J, Raux S. Patellar instability in children and adolescents. Orthop Traumatol Surg Res. 2014;100(1_suppl):S125–S137. [DOI] [PubMed] [Google Scholar]
- 11. Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of individual anatomical risk factors for patellar instability. Semin Musculoskelet Radiol. 2016;20(1):65–73. [DOI] [PubMed] [Google Scholar]
- 12. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res. 2015;101(1_suppl):S59–S67. [DOI] [PubMed] [Google Scholar]
- 14. Earhart C, Patel DB, White EA, Gottsegen CJ, Forrester DM, Matcuk GR., Jr Transient lateral patellar dislocation: review of imaging findings, patellofemoral anatomy, and treatment options. Emerg Radiol. 2013;20(1):11–23. [DOI] [PubMed] [Google Scholar]
- 15. Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225(3):736–743. [DOI] [PubMed] [Google Scholar]
- 16. Felus J, Kowalczyk B. Age-related differences in medial patellofemoral ligament injury patterns in traumatic patellar dislocation: case series of 50 surgically treated children and adolescents. Am J Sports Med. 2012;40(10):2357–2364. [DOI] [PubMed] [Google Scholar]
- 17. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 18. Guerrero P, Li X, Patel K, Brown M, Busconi B. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports Med Arthrosc Rehabil Ther Technol. 2009;1(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34(3):385–396. [DOI] [PubMed] [Google Scholar]
- 20. Ji G, Wang S, Wang X, Liu J, Niu J, Wang F. Surgical versus nonsurgical treatments of acute primary patellar dislocation with special emphasis on the MPFL injury patterns. J Knee Surg. 2017;30(4):378–384. [DOI] [PubMed] [Google Scholar]
- 21. Kang HJ, Wang F, Chen BC, Zhang YZ, Ma L. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):325–331. [DOI] [PubMed] [Google Scholar]
- 22. Kapur S, Wissman RD, Robertson M, Verma S, Kreeger MC, Oostveen RJ. Acute knee dislocation: review of an elusive entity. Curr Probl Diagn Radiol. 2009;38(6):237–250. [DOI] [PubMed] [Google Scholar]
- 23. Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39(7):1444–1449. [DOI] [PubMed] [Google Scholar]
- 24. Lawrie S, Welsh J. MPFL repair for acute patella dislocation. Orthop J Sports Med. 2016;4(2_suppl):2325967116S00017. [Google Scholar]
- 25. Menon S, Rapaport H, Al-Tawil O, Math K, Scuderi G, Katz D. Acute lateral patellar dislocation: incidence and patterns of osseous, cartilaginous, and medial patellofemoral ligament injury in 150 patients on MRI. Emerg Radiol. 2011;18:453–481. [Google Scholar]
- 26. Meyers AB, Laor T, Sharafinski M, Zbojniewicz AM. Imaging assessment of patellar instability and its treatment in children and adolescents. Pediatr Radiol. 2016;46(5):618–636. [DOI] [PubMed] [Google Scholar]
- 27. Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9(2):139–143. [DOI] [PubMed] [Google Scholar]
- 29. OCEBM Levels of Evidence Working Group. The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine. Accessed September 29, 2020. http://www.cebm.net/index.aspx?o=5653
- 30. Petri M, von Falck C, Broese M, et al. Influence of rupture patterns of the medial patellofemoral ligament (MPFL) on the outcome after operative treatment of traumatic patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):683–689. [DOI] [PubMed] [Google Scholar]
- 31. Redler LH, Wright ML. Surgical management of patellofemoral instability in the skeletally immature patient. J Am Acad Orthop Surg. 2018;26(19):e405–e415. [DOI] [PubMed] [Google Scholar]
- 32. Sanders TG, Morrison WB, Singleton BA, Miller MD, Cornum KG. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25(6):957–962. [DOI] [PubMed] [Google Scholar]
- 33. Seeley M, Bowman KF, Walsh C, Sabb BJ, Vanderhave KL. Magnetic resonance imaging of acute patellar dislocation in children: patterns of injury and risk factors for recurrence. J Pediatr Orthop. 2012;32(2):145–155. [DOI] [PubMed] [Google Scholar]
- 34. Seeley MA, Knesek M, Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop. 2013;33(5):511–518. [DOI] [PubMed] [Google Scholar]
- 35. Sherman SL, Geeslin DW, Hogan DW, et al. Comparison of MPFL repair versus MPFL reconstruction for refractory patella instability in patients under 18 years old. Orthop J Sports Med. 2020;8(4_suppl_3):2325967120S00189. [Google Scholar]
- 36. Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. [DOI] [PubMed] [Google Scholar]
- 37. Sillanpää PJ, Mäenpää HM, Mattila VM, Visuri T, Pihlajamäki H. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med. 2008;36(12):2301–2309. [DOI] [PubMed] [Google Scholar]
- 38. Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263–273. [DOI] [PubMed] [Google Scholar]
- 39. Sillanpää PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamäki H. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am J Sports Med. 2009;37(8):1513–1521. [DOI] [PubMed] [Google Scholar]
- 40. Trikha SP, Acton D, O’Reilly M, Curtis MJ, Bell J. Acute lateral dislocation of the patella: correlation of ultrasound scanning with operative findings. Injury. 2003;34(8):568–571. [DOI] [PubMed] [Google Scholar]
- 41. Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 42. Wilson A, Afarin A, Shaw C, Shirley E, Pierce J, Slakey JB. Magnetic resonance imaging findings after acute patellar dislocation in children. Orthop J Sports Med. 2013;1(6):2325967113512460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zhang GY, Zheng L, Ding HY, Li EM, Sun BS, Shi H. Evaluation of medial patellofemoral ligament tears after acute lateral patellar dislocation: comparison of high-frequency ultrasound and MR. Eur Radiol. 2015;25(1):274–281. [DOI] [PubMed] [Google Scholar]
- 44. Zhang GY, Zheng L, Feng Y, et al. Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in adults: an MRI evaluation. Injury. 2015;46(12):2413–2421. [DOI] [PubMed] [Google Scholar]
- 45. Zhang GY, Zheng L, Shi H, Ji BJ, Feng Y, Ding HY. Injury patterns of medial patellofemoral ligament after acute lateral patellar dislocation in children: correlation analysis with anatomical variants and articular cartilage lesion of the patella. Eur Radiol. 2017;27(3):1322–1330. [DOI] [PubMed] [Google Scholar]
- 46. Zhang GY, Zheng L, Shi H, et al. Correlation analysis between injury patterns of medial patellofemoral ligament and vastus medialis obliquus after acute first-time lateral patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):719–726. [DOI] [PubMed] [Google Scholar]
- 47. Zhang GY, Zheng L, Shi H, Qu SH, Ding HY. Sonography on injury of the medial patellofemoral ligament after acute traumatic lateral patellar dislocation: injury patterns and correlation analysis with injury of articular cartilage of the inferomedial patella. Injury. 2013;44(12):1892–1898. [DOI] [PubMed] [Google Scholar]
- 48. Zhang GY, Zhu HX, Li EM, et al. The correlation between the injury patterns of the medial patellofemoral ligament in an acute first-time lateral patellar dislocation on MR imaging and the incidence of a second-time lateral patellar dislocation. Korean J Radiol. 2018;19(2):292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zheng L, Shi H, Feng Y, Sun BS, Ding HY, Zhang GY. Injury patterns of medial patellofemoral ligament and correlation analysis with articular cartilage lesions of the lateral femoral condyle after acute lateral patellar dislocation in children and adolescents: an MRI evaluation. Injury. 2015;46(6):1137–1144. [DOI] [PubMed] [Google Scholar]