Abstract
Objectives
To (1) assess women’s current knowledge regarding long-term cardiovascular health after hypertensive disorders of pregnancy (2) elicit women’s preferred educational content and format regarding health after hypertensive disorders of pregnancy.
Design and setting
A custom-created online survey exploring Australian women’s knowledge about long-term health after hypertensive disorders of pregnancy, distributed through consumer groups and social media.
Participants
266 women with (n=174) or without (n=92) a history of hypertensive disorders of pregnancy.
Primary and secondary outcome measures
(1) Proportion of women identifying long-term health risks after hypertensive disorder of pregnancy using a 10-point risk knowledge score with 0–4 ‘low’, 4.1–7.0 ‘moderate’ and 7.1–10 ‘high’. (2) Exploration of preferred content, format and distribution of educational material post hypertensive disorder of pregnancy.
Results
Knowledge scores about health after hypertensive disorder of pregnancy were moderate in groups with and without a history of the disorder. Knowledge was highest regarding risk of recurrent hypertensive disorders in a subsequent pregnancy, ‘moderate’ for chronic hypertension and heart attack, ‘moderate’ and ‘low’ regarding risk of heart disease and ‘low’ for diabetes and renal disease. Only 36% of all participants were aware that risks start within 10 years after the affected pregnancy. The majority of respondents with a history of hypertensive disorder of pregnancy (76%) preferred receiving information about long-term health 0–6 months post partum from a healthcare provider (80%), key organisations (60%), social media (47%) and brochures/flyers (43%).
Conclusions
Women’s knowledge regarding health risks after hypertensive disorder of pregnancy was ‘moderate’, although with important disease-specific gaps such as increased risk of diabetes. Most women wanted to be informed about their long-term health from a healthcare provider.
Keywords: hypertension, maternal medicine, primary care
Strengths and limitations of this study.
Consumer co-created survey exploring health knowledge after hypertensive pregnancy.
For the first time survey results include findings from women with a history of gestational hypertension as well as from women without a history of hypertensive disorder of pregnancy.
Recruitment from groups with potentially greater baseline knowledge may bias results, although substantive knowledge gaps still found.
Although surveys were available in English, Arabic and Mandarin, there remains potential suboptimal coverage of culturally and linguistically diverse groups.
Introduction
Hypertensive disorders of pregnancy (HDP) include chronic hypertension (CH), pre-eclampsia (PE) and gestational hypertension (GH) and complicate 5%–10% of pregnancies.1 PE is a multi-system disorder characterised by new-onset hypertension after 20 weeks’ gestation and involvement of one or more other organ systems and/or the foetus.2 3 GH is new-onset hypertension after 20 weeks’ gestation without any other complications. Apart from GH itself being considered an adverse pregnancy outcome and it carrying an increased risk of progression to PE,2 3 is not otherwise associated with adverse pregnancy outcomes. However, both conditions are associated with long-term cardiovascular and other chronic disease sequelae.4 5 CH is defined as hypertension that is confirmed before pregnancy or before 20 completed weeks gestation, which may worsen during pregnancy and/or on which PE may be superimposed.2 Globally, cardiovascular disease (CVD) is one of the leading causes of death in women,6 and for women who have experienced an HDP, it is 2–3 times higher compared with those who did not.4 7 8 This risk of premature death is present within 10 years after the affected pregnancy7 9 10 and remains after adjusting for the presence of other cardiovascular risk factors. There is also an increasing body of recent research linking PE and GH with other major chronic diseases including chronic kidney disease, end-stage kidney disease and type 2 diabetes mellitus.11–14
Both Australian and international societies, including the Society of Obstetric Medicine of Australia and New Zealand (SOMANZ) and the International Society for the Study of Hypertension in Pregnancy (ISSHP), recommend that women and healthcare providers (HCP) are provided with information about HDP and later CVD.2 3 This includes recommending that women have a clinical review several months post partum, and regular general practitioner follow-up to monitor blood pressure, fasting lipids and blood sugar.2 Adopting a healthy lifestyle with maintenance of an ideal weight and regular aerobic exercise is emphasised.2 3 The aims of this study were to (1) explore Australian women’s current knowledge on the topic of long-term CVD health after any HDP, not just PE and (2) elicit women’s preferred educational content and format regarding health after HDP, as a basis for creating tailored information and health advice for women after HDP.
Method
A national survey of women with and without a history of HDP was conducted, using a custom-created, face-validated online survey.
Patient and public involvement
As a validated instrument to assess women’s knowledge was unavailable, a survey was custom designed. Initially, women with a history of HDP, comprising nine volunteers from the Postpartum physiology, psychology and paediatric follow-up study (P4 study)15 and Australian Action on Pre-eclampsia (AAPEC), were invited to take part in group interviews which addressed the possible content and design of the survey, tested the survey for face validity and provided feedback for improvement. The topics discussed during the interviews were sourced from findings from a scoping literature review16 and further complemented by questions specifically exploring the Australian context for women experiencing HDP. Nine women participated in the face-validation process and commented on content, language, flow, survey structure including length, whether the introduction and the risk profile proposed for the end of the survey were informative as well as using appropriate language. Following feedback and integration of suggestions from the women, the survey was modified until consensus over a final version was achieved among study investigators, including the consumer representative (LH). The survey was made available in English, Arabic and Mandarin.
Data collection
The final survey was targeted at women in Australia, 18 years and older with a history of pregnancy in the last 3 years. Women who were currently pregnant were requested to only complete the survey if they had no major issues in their current pregnancy. Women not currently pregnant with pregnancy in the preceding 3 years were eligible either if they had experienced HDP (CH, GH or PE) or a pregnancy without any serious complications. The online survey, using SurveyMonkey, was open from July to August 2019. Survey distribution occurred through the P4 study participants, organisations such as AAPEC, maternity consumer groups as well as via the project’s consumer representative and social media (Facebook and Twitter) including multicultural networks in order to reach Arabic and Mandarin speaking communities. A targeted convenience sample was selected. Prior to acknowledging their voluntary participation at the commencement of the survey, women were presented with an introductory letter outlining the details of the study (online supplemental appendix 1). Commencement of the survey was then taken as consent to participate.
bmjopen-2020-042920supp001.pdf (5.2MB, pdf)
Data collection instrument
The survey for women (online supplemental appendix 1) explored demographic details, assessed obstetric history, history of HDP and other medical history including family history. The survey was tailored to women’s self-reported HDP history (GH, PE, CH with or without worsening in pregnancy or superimposed PE, no hypertension history), with women given definitions of HDP conditions early in the survey to aid their self-report. Questions focused on knowledge of risk after pregnancy, provision of care and education following birth and what information and education women would like to receive. Women with a history of GH, PE or CH were asked to classify their perceived risk (based on their own lived HDP subtype) of experiencing various long-term health outcomes as greater, less than or equal to that of a woman with a normotensive pregnancy. Women who experienced a normotensive pregnancy were also asked to classify whether they believed women who had had HDP were at greater, lesser or equal risk. The survey included two ‘distractor’ conditions not known to have an increased risk after HDP (breast cancer and seizures) to elicit negative answers and ascertain whether women could identify what they were not at increased risk of after HDP as well as what they were at risk of. At survey completion, women were provided with a correct risk profile summary and a link to further information.
Data analysis
Quantitative survey analysis was undertaken using SPSS V.25. Demographic data and responses to individual questions were analysed descriptively. To examine difference in knowledge levels among the targeted subgroups (GH, PE, CH in pregnancy, no hypertension history) responses regarding HDP and future health risks were compared using χ2 testing or likelihood ratio for categorical data (as appropriate to subgroup sample size) and one-way analysis of variance (ANOVA) testing for continuous data. A p value of <0.05 was considered statistically significant.
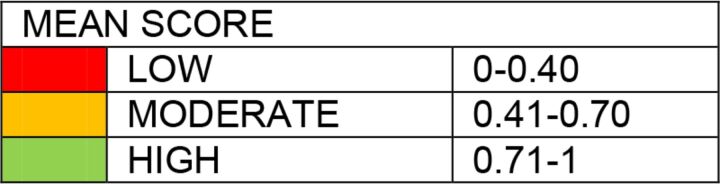
A knowledge score was created for the risk matrix whereby 1 point was allocated to the correct answer, 0 for the incorrect answer, 0 for ‘I do not know’ and 0 for no answer/left blank. A mean knowledge score for each condition/health outcome was calculated and a scale of ‘low’, ‘moderate’ and ‘high’ knowledge was established. The ranking classifications were chosen based on the data distribution and were divided into three score categories. For each individual condition/health outcome’s mean score, ‘low knowledge’ equated to a mean of 0.00–0.40, ‘moderate knowledge’ was 0.41–0.70 and ‘high knowledge’ a mean of 0.71–1.00. An overall mean score out of 10 (as there were 10 conditions) was calculated for the HDP and non-HDP groups (ie, the HDP group’s knowledge regarding their long-term health risks and the non-HDP group’s knowledge regarding the long-term health risks of HDP women). This overall score was classified as ‘low’ ‘moderate’ or ‘high’ using the same mean ranges as were used for the individual conditions. Categorical analysis for proportions of each knowledge group (‘high’, ‘moderate’ and ‘low’) was also conducted to provide a further perspective.
Results
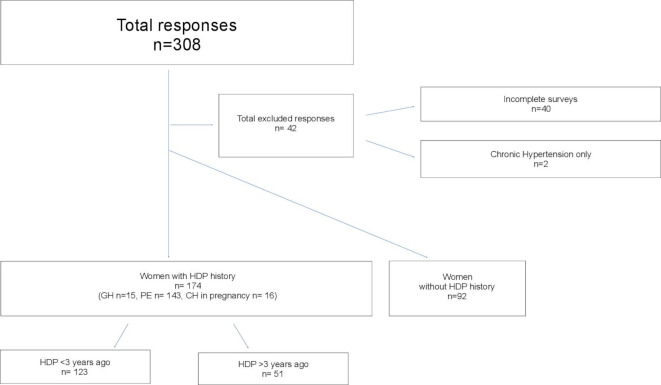
In total, 308 survey responses were received (figure 1). Forty-two were excluded: 40 for discontinuing the survey and not answering the question asking about their perception of lower/same/higher risk with regards to 10 health conditions, and two with ‘CH only’ (no worsening hypertension or superimposed PE in pregnancy) who were excluded due to small numbers. Of 266 included responses, 174 (65%) women had a lived experience of any HDP (will be known as HDP for reporting purposes) and 92 (35%) did not (will be known as non-HDP for reporting purposes). The HDP group consisted of 15 women with GH only (9%), 143 women with PE only (82%) and 16 women with CH plus superimposed pregnancy hypertension or PE (9%; will be known as CH). Of the HDP group, 123 (71%) had their most recent experience with HDP less than 3 years prior (32% <1 year prior and 39% 1–3 years prior).
Figure 1.
Survey inclusion. CH in pregnancy, chronic hypertension worsening in pregnancy and/or with superimposed PE; GH, gestational hypertension; HDP, hypertensive disorders of pregnancy; PE, pre-eclampsia.
Most respondents were in the 26–35-year or 36–45-year age groups (91%), 89% were of Caucasian ethnicity, 90% pursued education beyond secondary school and 96% were in a relationship (table 1). HDP women were more likely to be Caucasian, to have a history of diabetes, renal problems, be overweight and to have at least one additional cardiovascular risk factor than non-HDP women (online supplemental table 1), and less likely to be university-educated. Half of all participants were sourced through social media (50%), with most of the remainder (45%) recruited via the P4 study (8% of HDP women, 46% of non-HDP women) and AAPEC (35% of HDP women).
Table 1.
Respondent demographics
| Total N (%) |
GH % |
PE % |
CH % |
Total HDP N (%) |
Total non-HDP N (%) |
P value HDP vs non-HDP | |
| Total N | 266 | 15 | 143 | 16 | 174 | 92 | |
| Age | |||||||
| 18–25 | 12 (5) | 13 | 6 | – | 10 (6) | 2 (2) | 0.16 |
| 26–35 | 117 (44) | 33 | 48 | 50 | 81 (47) | 36 (39) | 0.25 |
| 36–45 | 126 (47) | 53 | 42 | 50 | 76 (44) | 50 (54) | 0.10 |
| 45+ | 10 (3) | – | 5 | – | 7 (4) | 3 (3) | 0.75 |
| Prefer not to answer | 1 (0) | – | – | – | – | 1 (1) | – |
| Ethnicity | |||||||
| Caucasian | 236 (89) | 93 | 97 | 81 | 165 (95) | 71 (77) | <0.001 |
| Asian | 23 (9) | 7 | 2 | 6 | 5 (3) | 18 (20) | <0.001 |
| Other* | 7 (3) | - | 1 | 13 | 4 (2) | 3 (8) | 0.65 |
| Highest educational attainment | |||||||
| Secondary school | 25 (9) | 7 | 14 | 13 | 23 (13) | 2 (2) | 0.003 |
| Diploma/trade† | 69 (26) | 33 | 33 | 50 | 60 (35) | 9 (10) | <0.001 |
| University degree | 171 (64) | 60 | 52 | 38 | 90 (52) | 81 (88) | <0.001 |
| Prefer not to answer | 1 (0) | – | 1 | – | 1 (1) | – | – |
| Relationship status | |||||||
| In a relationship | 254 (96) | 100 | 93 | 88 | 162 (93) | 92 (100) | 0.001 |
| Not in a relationship | 11 (4) | – | 6 | 13 | 11 (6) | 0 (1) | |
| Prefer not to answer | 1 (0) | – | 1 | – | 1 (1) | – | – |
| Recruited to survey via | |||||||
| P4 newsletter | 56 (21) | 13 | 8 | 6 | 14 (8) | 42 (46) | <0.001 |
| AAPEC | 62 (23) | 7 | 40 | 19 | 61 (35) | 1 (1) | <0.001 |
| Social media | 134 (50) | 80 | 52 | 69 | 97 (56) | 37 (40) | 0.02 |
| Other‡ | 14 (5) | – | 1 | 6 | 2 (1) | 12 (13) | <0.001 |
*Other: Indigenous Australian (n=1), Polynesian or Maori (n=2), mixed ethnicity (n=4).
†Diploma or trade certificate.
‡Other: friend (n=11), ACM (n=1), Clinic (n=1), maternity consumer group other than AAPEC (n=1).
AAPEC, Australian Action on Pre-eclampsia; ACM, Australian College of Midwives; CH, chronic hypertensionchronic hypertension worsening in pregnancy and/or with superimposed PE; GH, gestational hypertension; HDP, hypertensive disorders of pregnancy; PE, pre-eclampsia.
bmjopen-2020-042920supp002.pdf (14.9KB, pdf)
Average knowledge scores are shown in table 2 and detailed results on which these scores are based are shown in online supplemental tables 2–11. Overall knowledge of the 10 conditions in the survey was ‘moderate’ for both groups (5.6/10 among HDP and 5.2/10 among non-HDP, p=0.21), with 33% in both groups having ‘high’ overall knowledge and 32% and 40%, respectively having ‘low’ overall knowledge (online supplemental table 12). Women with a history of HDP had ‘high’ knowledge with regards to recurrence of HDP in a subsequent pregnancy (0.90) and risk of future CH (0.76). The same group had ‘moderate’ knowledge regarding increased risk of conditions such as heart attack (0.68), heart disease (0.68) and stroke (0.63). Women without HDP history had ‘high’ knowledge (0.71) for HDP recurrence in a subsequent pregnancy. The same group of women had moderate knowledge of CH (0.62) and stroke (0.53). Lowest knowledge across both groups was around the risk of future diabetes (0.25 HDP group and 0.35 for non-HDP group). Further ‘low’ scoring conditions were peripheral vascular disease (PVD) and renal disease. For most conditions HDP women had significantly higher knowledge than the non-HDP group. However, the non-HDP group were more likely to correctly identify that the risk of the two ‘distractor’ conditions, seizures or breast cancer, were equal for both groups.
Table 2.
Means of risk factor knowledge of women listed by type of HDP
| GH n=15 | PE n=143 | CH n=16 | HDP n=174 | Non-HDP n=92 | P value HDP vs non-HDP | |
| Chronic hypertension | 0.53 | 0.78 | 0.81 | 0.76 | 0.62 | 0.02 |
| Diabetes | 0.27 | 0.24 | 0.31 | 0.25 | 0.35 | 0.12 |
| Renal disease | 0.27 | 0.54 | 0.69 | 0.53 | 0.21 | <0.001 |
| Heart attack | 0.53 | 0.69 | 0.75 | 0.68 | 0.52 | 0.01 |
| Repeat HDP | 0.87 | 0.90 | 0.94 | 0.90 | 0.71 | <0.001 |
| Stroke | 0.47 | 0.62 | 0.81 | 0.63 | 0.53 | 0.14 |
| Heart disease | 0.47 | 0.69 | 0.75 | 0.68 | 0.50 | 0.005 |
| PVD | 0.33 | 0.50 | 0.50 | 0.32 | 0.45 | <0.001 |
| Breast cancer* | 0.20 | 0.52 | 0.31 | 0.47 | 0.65 | 0.004 |
| Seizures* | 0.27 | 0.29 | 0.13 | 0.27 | 0.44 | 0.01 |
| Overall mean knowledge score (out of 10) | 4.2 | 5.8 | 6.0 | 5.6 | 5.2 | 0.21 |
*Breast cancer and seizures are distractors within the survey. These were included despite being conditions that women after HDP are not at greater risk of.
CH, chronic hypertension worsening in pregnancy and/or with superimposed PE; GH, gestational hypertension; HDP, hypertensive disorders of pregnancy; PE, pre-eclampsia; PVD, peripheral vascular disease.
bmjopen-2020-042920supp003.pdf (30KB, pdf)
bmjopen-2020-042920supp012.pdf (31.2KB, pdf)
bmjopen-2020-042920supp011.pdf (31.3KB, pdf)
bmjopen-2020-042920supp010.pdf (31.3KB, pdf)
bmjopen-2020-042920supp009.pdf (31.3KB, pdf)
bmjopen-2020-042920supp008.pdf (31.3KB, pdf)
bmjopen-2020-042920supp007.pdf (31.4KB, pdf)
bmjopen-2020-042920supp006.pdf (31.4KB, pdf)
bmjopen-2020-042920supp005.pdf (31.3KB, pdf)
bmjopen-2020-042920supp004.pdf (31.3KB, pdf)
bmjopen-2020-042920supp013.pdf (31.7KB, pdf)
Online supplemental table 13 shows knowledge score breakdown by time since pregnancy. In the subgroup of HDP women who experienced PE (n=143), average knowledge was similar among women who experienced HDP within the last 3 years (5.8/10), compared with those who experienced HDP more than 3 years ago (5.7/10). Of the HDP women, only 32% were aware that the cardiovascular conditions may start manifesting within 10 years after an affected pregnancy, compared with 45% of women in the non-HDP group (p=0.036). About a third in each group (30% HDP, 36% non-HDP) were unsure about timing of risk rise/when health conditions manifest (online supplemental table 14).
bmjopen-2020-042920supp014.pdf (36.4KB, pdf)
bmjopen-2020-042920supp015.pdf (30.8KB, pdf)
Women with HDP history were asked about their personal experience of risk discussion with HCP (table 3 represents summary of collective HDP data, online supplemental table 15 provides all findings by HDP subgroup). The most frequent discussions about future health were regarding HDP in subsequent pregnancies (45%), risk of CH (43%) and ‘no discussion’ (37%). Risk discussions were no more likely to have occurred in women with HDP less than 3 years ago or over 3 years ago. There were also no statistically significant differences found between HDP subgroups about whether future risks were discussed, or what types of risk were discussed.
Table 3.
Proportion of conditions discussed when addressing future risk (multiple answers collected) within and over 3 years since last HDP (summary of collective HDP data)*
| Total n=174 N (%) | Overall total n=174 N (%) | P value <3 years vs >3 years | ||
| <3 years | >3 years | |||
| HDP next pregnancy | 55 (45) | 24 (47) | 79 (45) | 0.78 |
| Chronic hypertension | 55 (45) | 19 (37) | 74 (43) | 0.37 |
| No discussion | 45 (37) | 19 (37) | 64 (37) | 0.93 |
| Lifestyle changes | 32 (26) | 8 (16) | 40 (23) | 0.14 |
| Heart attack | 22 (18) | 7 (14) | 29 (17) | 0.50 |
| Renal disease | 23 (19) | 4 (8) | 27 (16) | 0.07 |
| Stroke | 20 (16) | 6 (12) | 26 (15) | 0.45 |
| Peripheral vascular disease | 16 (13) | 5 (10) | 21 (12) | 0.56 |
| Cannot remember | 6 (5) | 2 (4) | 8 (5) | 0.78 |
*Table represents frequency of each option; percentages add to over 100% as women were asked to select any/all that applied.
HDP, hypertensive disorder of pregnancy.
bmjopen-2020-042920supp016.pdf (71.8KB, pdf)
When asked about preferences of the timing of a future risk discussion, the majority (76%) of women wanted a discussion 0–6 months post partum. The topics most women with HDP wished to discuss (table 4) are ‘impact on my children from the pregnancy affected by HDP’ (73%), ‘signs and symptoms of the conditions’ (67%), ‘when does risk rise’ (54%) and ‘risk reduction for subsequent pregnancy’ (54%). HDP women’s preference for receiving information on long-term health after HDP is via a medical professional (80%), through key organisations such as the Australian Heart Foundation (60%) and social media (47%).
Table 4.
HDP women’s preferences for content and distribution of information/education on future risk after HDP (multiple answers collected) in order of preference
| GH % |
PE % |
CH % |
Total HDP N (%) |
|
| Total N | 15 | 143 | 16 | 174 |
| Preference of discussion topics* | ||||
| Impact on my children from the pregnancy affected by HDP | 73 | 80 | 63 | 136 (73) |
| Signs and Symptoms of the conditions | 80 | 71 | 69 | 124 (67) |
| Risk reduction for subsequent pregnancy | 40 | 62 | 44 | 101 (54) |
| When does the risk rise | 40 | 61 | 50 | 101 (54) |
| Statistics | 40 | 60 | 38 | 98 (53) |
| Reducing risk behaviours (diet, exercise, smoking cessation) | 40 | 56 | 31 | 91 (49) |
| Where to find information | 40 | 51 | 13 | 81 (44) |
| How to discuss the matter with my healthcare provider | 27 | 40 | 25 | 65 (35) |
| Preference of distribution* | ||||
| Medical professionals | 73 | 82 | 75 | 140 (80) |
| Key organisations | 53 | 61 | 63 | 105 (60) |
| Social media | 40 | 51 | 19 | 82 (47) |
| Brochures/flyers | 40 | 45 | 31 | 75 (43) |
| Online videos | 20 | 24 | 25 | 42 (24) |
| Podcast/media | 13 | 23 | 25 | 39 (22) |
*Table represents frequency of each option; percentages add to over 100% as women were asked to select any/all that applied.
CH, chronic hypertension worsening in pregnancy and/or with superimposed PE; GH, gestational hypertension; HDP, hypertensive disorders of pregnancy; PE, pre-eclampsia.
Discussion
This study found overall, ‘moderate’ knowledge of health conditions after HDP among both HDP and non-HDP women. Among women with a history of HDP, highest knowledge was identified with regards to future risk of hypertension and repeat HDP in subsequent pregnancies. Conversely, knowledge of future risk of diabetes was low, as was knowledge of the ‘distractor’ conditions among HDP women particularly. Diabetes as a future risk factor post-HDP has previously not been reported on in studies of women’s knowledge, and our findings suggest this is an important knowledge gap to address.
Other novel aspects of our study are inclusion of women who had a history of GH as well as those with a history of PE, and assessing knowledge of non-HDP women’s knowledge. Women after HDP had somewhat higher knowledge of most health risks than the non-HDP group, however non-HDP group also had better knowledge of some aspects such as timing of risk increase. However, both groups’ knowledge of the early increase in risk was low, adding further concern and reason to address the knowledge gap. When looking at the proportion of participants scoring ‘high’, these were equal between the HDP (33%) and non-HDP groups (33%), while proportions scoring ‘low’ were similar enough (32% HDP vs 40% non-HDP) to not to show statistical significance. Our scoping review in 201916 identified that post-HDP, women have insufficient knowledge of their long-term risks. By including non-HDP women we wanted to explore whether knowledge was similar between the groups, which if so would suggest HDP women are not receiving tailored, targeted information and/or any information received is not translated into knowledge of personal risk after HDP. Given women after HDP were not markedly more knowledgeable about their health risks than unaffected women, the research-to-practice translational gap is further highlighted and suggests women with a lived experience of HDP remain underinformed about their increased CVD risk.
A further important finding was that many HDP women were not made aware of future health risks, with 37% of HDP women reporting to have had ‘no discussion’ about their increased long-term risk. Women with more recent HDP were no more likely than women with HDP >3 years ago to report having risks discussed, which is concerning. This finding suggests risk discussions may not have improved in recent years despite updated guidelines emphasising long-term health,2 3 and that the extensive evidence regarding long-term implications for women after HDP continues to be lost in the translation of research to practice. We are exploring reasons for this (eg, lack of evidence base in guidelines, lack of provider knowledge of guidelines, siloed healthcare with insufficient handover from maternity care team to primary care) in our broader work.
Women’s knowledge after GH has not been previously reported as far as we are aware even though GH has similar frequency and similar future CVD risk as PE.4 17 Although only 9% of our sample were GH, this group had somewhat lower knowledge than the PE and CH groups regarding conditions after HDP (although mostly not reaching statistical significance). Over half reported receiving no discussion of health risks after GH. Despite the small number of women with a history of GH (n=15) contributing to the study, this suggests potential substantive knowledge gaps after GH to address in both women and HCP.
International studies exploring women’s knowledge have predominantly reported limited or no knowledge about the link between HDP and CVD,16 though our study found overall, ‘moderate’ knowledge of health conditions after HDP. The two conditions associated with highest knowledge were repeat HDP and risk of future hypertension. Findings were similar in Traylor et al’s18 survey conducted in the USA, where 146 women post-HDP were included (PE n=76, PE with severe features n=41, CH=29). Future hypertension and repeat HDP were correctly identified by women as risk factors; however, this knowledge was mainly reflected in the group of women who had experienced PE with severe features. In the UK, Brown et al19 (n=12 women attending postnatal follow-up clinic) also found that women are aware of repeat HDP risks; however, despite postnatal risk counselling, perception of hypertension and CVD risk was mainly associated with participants who had a family history of CVD. More recently in Australia, Hutchesson et al20 surveyed 127 women with PE in the 2 years prior, finding very high knowledge about future hypertension risk (96%, higher than our post-PE findings) and most were aware of stroke (67%) and CVD (66%) risks (similar to our findings). Over a third of women after PE had ‘no discussion’ about future risk in our study. Hutchesson et al20 reported over one third of their participants remained unaware of increased CVD risks, which is similar to our findings. Similarities may be explained by the fact that major source of PE participants for both, the Hutchesson et al20 survey and ours was the patient support/advocacy group AAPEC. Recruitment from this advocacy group may also explain a higher post-PE knowledge than other studies have reported.
Our study findings resonate with those from similarly targeted women in Canada, Portugal, UK, the USA and a previous Australian study, all conducted between 2013 and 2017.16 Therefore, from a global perspective, these findings reinforce a persistent and concerning, research to consumer gap. With international guidelines, including ISSHP,2 specifically targeted to assist HCPs providing care to women on an international scale to better manage and address health after HDP, this practice gap of knowledge transmission to women would be expected to narrow.
Education preferences
Content
Women mostly wanted educational materials to address HDP impact on their children, signs and symptoms of conditions they are at higher risk of, the timing of when their risks rise, and how to best reduce risk of recurrent HDP. Similar preferences were expressed by the women included in Seely et al’s21 focus group of 20 women after PE, with the key concern being the impact the PE pregnancy may have had on the health of their children. More recently, a UK-based study,22 involving women with a history of HDP and HCPs, identified research priorities regarding HDP. The top-ranking priority identified was the long-term physical and mental health consequences of HDP for the woman, baby and family. Other ‘uncertainties’ expressed by participants regarding their lived experience of HDP included topics such as diagnosis and management in pregnancy, prevention of future complications, short and long-term consequences of HDP for the woman and the baby, prevention of recurrent HDP as well as educational needs of HCPs and support for women and their families. Our study, with focus on women in Australia, suggests that similar uncertainties may benefit from being addressed, hence validating the importance of our findings.
Format of education and access
Our study identified that women mostly wanted to receive information about long-term health after HDP from medical professionals. Key organisations who are experts on the topic, via social media and through information brochures were other acceptable avenues of access to information. This is in contrast to Skurnik et al’s23 focus group of 14 women after PE, whose preferences for educational materials about the link between CVD and PE were via pamphlets available in doctor’s offices as well as via online communities and topical blogs. However, Hird et al’s24 participants also expressed preference for HCP as their information source, including wanting HCP to guide them towards reliable online/external information sources rather than encounter irrelevant or potentially inaccurate information due to their self-initiated search. Hutchesson et al20 report that high knowledge among participants was mainly due to the women’s own research rather than receiving all possible, relevant information from their healthcare provider. Overall, existing studies including ours would suggest that although women are very open to the use of online sources or information packs, their HCP are seen as central to closing their knowledge gaps.
Time of risk discussion
An important element to consider when communicating about risk with women who have experienced GH or PE is the timing of these discussions, as situational factors of being a new mother may alter when women are most receptive to follow-up. In our study, three-quarters of the women preferred this to occur in the first 6 months after birth. As well as being their preference, this also aligns with the potential benefits of early intervention and would allow for addressing knowledge gaps found in this study around how soon the risk rises after HDP. Addressing future risk early but not immediately is also supported by Brown et al’s study of women after PE, where participants suggested that 6 months post partum was the timeframe where they felt they had transitioned into a more comfortable stage of parenting and were able to focus more on themselves again.19
Strengths and limitations
The survey was co-created via a formalised process of seeking input and feedback on the usability, language and content from women who have previously experienced HDP. Although face-validation is a subjective process, involving consumers with a history of HDP gives added value to the survey.
Our knowledge score is both a strength, as it allows for a summary of findings across all the conditions and risks, and a limitation, as assigning cut-points for knowledge ranking is an arbitrary designation. Having included the distractor conditions (breast cancer and seizures) may also have altered the overall score. While women are more likely to experience seizures during a pregnancy complicated by HDP compared with non-HDP women, the long-term risk of seizures is similar for both groups. Similarly, the association of HDP and future increased risk of cancer (including breast cancer) has been examined in a systematic review and meta-analysis, however proven not to be associated with increased future risks after HDP.25 Distractor inclusion may well have lowered overall knowledge score, for example, women believing that after HDP they are at more risk of ongoing seizures since this is a risk during PE-affected pregnancy. However, we believe inclusion of distractors and assessment of women’s response to them is valid, as it is important for women to not incorrectly believe they are at increased risk of more conditions than they are, as well as having knowledge of their increased cardiovascular risk. The addition of women with a history of GH as well as women without any history of HDP, is also a strength to add broader perspective on this topic.
Limitations include demographic make-up of respondents, with HDP participants predominantly English speaking and Caucasian (95%) despite the survey being available in Arabic and Mandarin as well as English. The non-HDP group (20% Asian background) had similar background demographics of Australian reproductive-aged women,26 and as HDP is more prevalent among the Caucasian population,27 the sample in the context of ethnic background actually is proportionally likely close to representative of Australian HDP and non-HDP women. However, it would have been preferable to also gain insight from more culturally and linguistically diverse groups in order to understand their knowledge base and address their needs within this context.
In the survey, women were asked to select their HDP history which was then used to group them for analysis. Women’s diagnosis of HDP is by self-report is a limitation, as some bias may be introduced through inaccurate self-report of diagnosis. The broad geographical range and anonymous nature of the survey precluded any verification of diagnosis. However, women were provided with definitions of the various HDP conditions at the start of the survey to aid them in their self-report. Another limitation is where participants were recruited from, with close to half either drawn from the P4 study (an Australian post-HDP research study) or consumer group AAPEC. Therefore, there may be knowledge bias in the sample (ie, a more knowledgeable group of participants than the overall HDP or non-HDP population). The women’s level of active engagement in pursuing further information on their long-term risks as well as their level of motivation to participate in this study, further contributes to knowledge bias. The number of respondents in all included HDP subgroups are a small proportion of the total number of women experiencing HDP, which suggests volunteer bias and this affects generalisability. However, non-representative, specialised samples of women can be noted within most research addressing women’s knowledge on long-term health after HDP.16 As even this group with potentially greater baseline knowledge had substantive knowledge gaps, our study highlights the need for interventions to improve knowledge of health after HDP.
Implications
Close to two decades worth of data have been collected8 since research on the link between HDP and increased CVD risk emerged in the early 2000s, with the first systematic review published in 2007.25 It could be expected that this knowledge, by now, would have been translated into practice and shared with HDP women, however our findings suggest that this is still not the case. This study is valuable from the public health perspective, given the wider context of prevalence and importance of CVD in women. Findings from this study and the broader study it is embedded in, will contribute towards the development, application and evaluation of educational materials for women and HCP. These future projects will address persistent knowledge-to-practice-gaps regarding improving women’s cardiovascular health after HDP. Given the prevalence and impact of both HDP and CVD, this is valuable for women’s health, and public health more broadly.
Guidelines such as ISSHP2 and SOMANZ3 suggest regular follow-up after HDP as well as counselling women with regards to their individual long-term CVD risk. Although available to the public, these are not designed for women. Compiling suitable information for women would be an important step towards closing the knowledge gap. It is important to establish preferred content, presentation and timing of education for post-HDP health for women as we have in this study, to maximise the chance that women will engage with and benefit from education.
Conclusion
This Australian survey of women’s knowledge of risks after HDP, found varying knowledge from the targeted groups. Despite ‘high’ knowledge being demonstrated regarding some risks, overall significant knowledge gaps were identified for certain conditions, particularly diabetes, and for knowledge about the relatively early timing of when health risks increase after HDP. Identifying these gaps are important in planning tailored education for women, and to improve early intervention for modifiable CVD risks in women after HDP. Addressing these women’s preferences for content and to have this delivered by their healthcare provider may further lead to enhanced counselling, management and improved women’s health trajectories.
Supplementary Material
Acknowledgments
We thank all women who took the time to respond to the survey. We also thank the organisations and their social media networks who assisted with the distribution of the survey: the postpartum physiology, psychology and paediatric follow up study (P4 study) research team, Australian Action on Pre-eclampsia, maternity consumer groups, Lisa Hanley who is our volunteer consumer representative and the various shares by consumers via social media (Facebook and Twitter) including multicultural networks.
Footnotes
Twitter: @CarolineHomer, @amanda_henry_AK
Contributors: HR, AH and CSEH contributed to the conception and design of the study as well as the distribution of the survey and writing of the manuscript. HR led the analysis of the survey data, drafting and designed the tables, figures and appendixes and wrote the first draft. GL was a medical Honours student assisting with presurvey interviews as well as initial data analysis. LMR assisted in the survey development, supported the distribution, the interpretation of the findings and the discussion. MB contributed to the design of the survey and supported the interpretation of the findings and the discussion. As a maternity consumer, LH has assisted with the survey design and ensured appropriate use of language and content as well as supported the distribution. All authors contributed to drafts and revising of the paper and all approved the final version.
Funding: AH is supported by a National Health and Medical Research Council (Australia) Early Career Fellowship (APP 1141570). CSEH is supported by a NHMRC Principal Research Fellowship (APP1137745). HR is supported by an Australian Government Research Training Programme Stipend (RTPS) UTS and RTP Fees Offset (RTPFO) Scholarship: the stipend is a ‘salary’ to support HR in completing her PhD full time. The scholarship supports her enrolment fees for the PhD.
Competing interests: The article is the authors’ original work, has not received prior publication and is not under consideration for publication elsewhere. All the authors have seen and approved the manuscript being submitted. The manuscript is an honest, accurate and transparent account of the study being reported, no important aspects of the study have been omitted. We have read and understood BMJ policy on declaration of interests and declare that we have no competing interests. This manuscript presents partial results from HR’s PhD research. The project is supervised by CSEH and AH.
Patient consent for publication: Not required.
Ethics approval: Ethical approval has been provided by South-Eastern Sydney Local Health District Human Research Ethics Committee (HREC 18/POWH/326, REGIS 2019/PID05668). The ratification for the University of Technology Sydney has also been obtained under ETH18-3061.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
Author note: This manuscript presents partial results from Heike Roth’s PhD research. The project is supervised by CSEH and AH.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol 2009;33:130–7. 10.1053/j.semperi.2009.02.010 [DOI] [PubMed] [Google Scholar]
- 2.Brown MA, Magee LA, Kenny LC, et al. . Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 2018;72:24–43. 10.1161/HYPERTENSIONAHA.117.10803 [DOI] [PubMed] [Google Scholar]
- 3.Lowe SA, Bowyer L, Lust K, et al. . SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust N Z J Obstet Gynaecol 2015;55:e1–29. 10.1111/ajo.12399 [DOI] [PubMed] [Google Scholar]
- 4.Theilen LH, Fraser A, Hollingshaus MS, et al. . All-Cause and cause-specific mortality after hypertensive disease of pregnancy. Obstet Gynecol 2016;128:238–44. 10.1097/AOG.0000000000001534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riise HKR, Sulo G, Tell GS, et al. . Association Between Gestational Hypertension and Risk of Cardiovascular Disease Among 617 589 Norwegian Women. J Am Heart Assoc 2018;7. 10.1161/JAHA.117.008337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roth GA, Abate D, Abate KH, et al. . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDonald SD, Malinowski A, Zhou Q, et al. . Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J 2008;156:918–30. 10.1016/j.ahj.2008.06.042 [DOI] [PubMed] [Google Scholar]
- 8.Brown MC, Best KE, Pearce MS, et al. . Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol 2013;28:1–19. 10.1007/s10654-013-9762-6 [DOI] [PubMed] [Google Scholar]
- 9.Egeland GM, Skurtveit S, Staff AC, et al. . Pregnancy‐Related Risk Factors Are Associated With a Significant Burden of Treated Hypertension Within 10 Years of Delivery: Findings From a Population‐Based Norwegian Cohort. J Am Heart Assoc 2018;7. 10.1161/JAHA.117.008318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnott C, Nelson M, Alfaro Ramirez M, et al. . Maternal cardiovascular risk after hypertensive disorder of pregnancy. Heart 2020;106:1927–33. 10.1136/heartjnl-2020-316541 [DOI] [PubMed] [Google Scholar]
- 11.Pace R, Brazeau A-S, Meltzer S, et al. . Conjoint associations of gestational diabetes and hypertension with diabetes, hypertension, and cardiovascular disease in parents: a retrospective cohort study. Am J Epidemiol 2017;186:1115–24. 10.1093/aje/kwx263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khashan AS, Evans M, Kublickas M, et al. . Preeclampsia and risk of end stage kidney disease: a Swedish nationwide cohort study. PLoS Med 2019;16:e1002875 10.1371/journal.pmed.1002875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrett PM, McCarthy FP, Evans M, et al. . Hypertensive disorders of pregnancy and the risk of chronic kidney disease: A Swedish registry-based cohort study. PLoS Med 2020;17:e1003255. 10.1371/journal.pmed.1003255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Timpka S, Markovitz A, Schyman T, et al. . Midlife development of type 2 diabetes and hypertension in women by history of hypertensive disorders of pregnancy. Cardiovasc Diabetol 2018;17:124. 10.1186/s12933-018-0764-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis GK, Roberts L, Henry A, et al. . Postpartum physiology, psychology and paediatric study – P4 study: long term consequences for mother and child. Pregnancy Hypertension: An International Journal of Women’s Cardiovascular Health 2016;6:216–7. [DOI] [PubMed] [Google Scholar]
- 16.Roth H, LeMarquand G, Henry A, et al. . Assessing knowledge gaps of women and healthcare providers concerning cardiovascular risk after hypertensive disorders of Pregnancy—A scoping review. Front Cardiovasc Med 2019;6:178. 10.3389/fcvm.2019.00178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Theilen L, Meeks H, Fraser A, et al. . 45: long-term mortality risk and life expectancy following recurrent hypertensive disease of pregnancy. Am J Obstet Gynecol 2017;216:S32–3. 10.1016/j.ajog.2016.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Traylor J, Chandrasekaran S, Limaye M, et al. . Risk perception of future cardiovascular disease in women diagnosed with a hypertensive disorder of pregnancy. J Matern Fetal Neonatal Med 2016;29:2067–72. 10.3109/14767058.2015.1081591 [DOI] [PubMed] [Google Scholar]
- 19.Brown MC, Bell R, Collins C, et al. . Women’s perception of future risk following pregnancies complicated by preeclampsia. Hypertens 2013;32:60–73. [DOI] [PubMed] [Google Scholar]
- 20.Hutchesson M, Shrewsbury V, Park F, et al. . Are women with a recent diagnosis of pre‐eclampsia aware of their cardiovascular disease risk? A cross‐sectional survey. Aust N Z J Obstet Gynaecol 2018;58:E27–8. 10.1111/ajo.12900 [DOI] [PubMed] [Google Scholar]
- 21.Seely EW, Rich-Edwards J, Lui J, et al. . Risk of future cardiovascular disease in women with prior preeclampsia: a focus group study. BMC Pregnancy Childbirth 2013;13:240. 10.1186/1471-2393-13-240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ho A, Webster L, Bowen L, et al. . Research priorities for pregnancy hypertension: a UK priority setting partnership with the James Lind alliance. BMJ Open 2020;10:e036347. 10.1136/bmjopen-2019-036347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skurnik G, Roche AT, Stuart JJ, et al. . Improving the postpartum care of women with a recent history of preeclampsia: a focus group study. Hypertens Pregnancy 2016;35:371–81. 10.3109/10641955.2016.1154967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hird MJ, Yoshizawa RS, Robinson S, et al. . Risk for cardiovascular disease after pre-eclampsia: differences in Canadian women and healthcare provider perspectives on knowledge sharing. Health Sociology Review 2017;26:128–42. 10.1080/14461242.2016.1181981 [DOI] [Google Scholar]
- 25.Bellamy L, Casas J-P, Hingorani AD, et al. . Pre-Eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007;335:974. 10.1136/bmj.39335.385301.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Australian Bureau of Statistics 3301.0. births Australia: Commonwealth of Australia; 2018. Available: https://www.abs.gov.au/ausstats/abs@.nsf/mf/3301.0 [Accessed 13 May 2020].
- 27.Al-Rubaie ZTA, Malcolm Hudson H, Jenkins G, et al. . The association between ethnicity and pre-eclampsia in Australia: a multicentre retrospective cohort study. Aust N Z J Obstet Gynaecol 2020;60:396–404. 10.1111/ajo.13069 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-042920supp001.pdf (5.2MB, pdf)
bmjopen-2020-042920supp002.pdf (14.9KB, pdf)
bmjopen-2020-042920supp003.pdf (30KB, pdf)
bmjopen-2020-042920supp012.pdf (31.2KB, pdf)
bmjopen-2020-042920supp011.pdf (31.3KB, pdf)
bmjopen-2020-042920supp010.pdf (31.3KB, pdf)
bmjopen-2020-042920supp009.pdf (31.3KB, pdf)
bmjopen-2020-042920supp008.pdf (31.3KB, pdf)
bmjopen-2020-042920supp007.pdf (31.4KB, pdf)
bmjopen-2020-042920supp006.pdf (31.4KB, pdf)
bmjopen-2020-042920supp005.pdf (31.3KB, pdf)
bmjopen-2020-042920supp004.pdf (31.3KB, pdf)
bmjopen-2020-042920supp013.pdf (31.7KB, pdf)
bmjopen-2020-042920supp014.pdf (36.4KB, pdf)
bmjopen-2020-042920supp015.pdf (30.8KB, pdf)
bmjopen-2020-042920supp016.pdf (71.8KB, pdf)