ABSTRACT
Background: Children and adolescents in foster care often experience many co-occurring subtypes of maltreatment. However, little is known about different combinations of maltreatment subtypes, referred to as maltreatment classes. Furthermore, the association between those maltreatment classes and ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD) has not been investigated in children and adolescents. In previous studies, classes characterized by cumulative maltreatment were associated with severe psychopathological symptoms. So far, no study investigated ICD-11 PTSD and CPTSD.
Objective: The first aim of this study was the detection of distinct maltreatment classes by examining frequently co-occurring maltreatment subtypes. The second aim was the examination of the association between those maltreatment classes and ICD-11 PTSD and CPTSD.
Method: Participants were 147 children and adolescents currently living in foster care institutions in Lower Austria. Maltreatment history, ICD-11 PTSD and CPTSD were assessed using standardized self-report questionnaires. Latent class analysis was applied to examine maltreatment subtypes. χ2 difference testing was used to examine class associations with PTSD and CPTSD.
Results: Three latent classes that comprised different subtypes of maltreatment were identified (limited maltreatment, n = 49; high neglect, n = 53; cumulative maltreatment, n = 45). Cumulative maltreatment was associated with higher symptom severity of PTSD and CPTSD than the limited maltreatment and the high neglect class, with effect sizes ranging from 0.62 to 0.93.
Conclusions: The association of the cumulative maltreatment class with the highest symptom severity of PTSD and CPTSD highlights the detrimental effect of cumulative maltreatment. The detection of a high neglect class identifies children and adolescents, who are at high-risk of experiencing future maltreatment because of their previous experiences of neglect and the associated lack of protection. The examination of the association of distinct maltreatment classes with ICD-11 PTSD and CPTSD might provide implications for targeted prevention, assessment and treatment.
KEYWORDS: Children, adolescents, foster care, ICD-11, posttraumatic stress disorder (PTSD), complex PTSD, neglect, abuse, childhood maltreatment, latent class analysis
HIGHLIGHTS
• Three classes of childhood maltreatment were detected (limited maltreatment, high neglect, cumulative maltreatment).• Class membership was associated with ICD-11 PTSD and CPTSD.• Based on the findings, tailored prevention and intervention is possible for high-risk individuals.
Antecedentes: Los niños y adolescentes bajo cuidados alternativos a menudo experimentan muchos subtipos de maltrato concurrentes. Sin embargo, se sabe poco sobre las diferentes combinaciones de subtipos de maltrato, denominadas clases de maltrato. Además, la asociación entre esas clases de maltrato y el trastorno de estrés postraumático (TEPT) y el trastorno de estrés postraumático complejo (TEPTC) de la CIE-11 no se ha investigado en niños y adolescentes. En estudios anteriores, las clases caracterizadas por maltrato acumulativo se asociaron con síntomas psicopatológicos graves. Hasta ahora, ningún estudio investigó el TEPT y el TEPT-C de la CIE-11.
Objetivo: El primer objetivo de este estudio fue la detección de distintas clases de maltrato mediante el examen de subtipos de maltrato que concurren con frecuencia. El segundo objetivo fue el examen de la asociación entre esas clases de maltrato y CIE-11 TEPT y TEPTC.
Método: Los participantes fueron 147 niños y adolescentes que actualmente viven en instituciones de acogida en Baja Austria. Se evaluaron los antecedentes de maltrato, TEPT y TEPT-C de la CIE-11 mediante cuestionarios de auto-reporte estandarizados.
Se aplicó un análisis de clases latentes para examinar los subtipos de maltrato. Se utilizó la prueba de diferencia de χ2 para examinar las asociaciones de clases con TEPT y TEPTC.
Resultados: Se identificaron tres clases latentes que comprendían diferentes subtipos de maltrato (maltrato limitado, n = 49; alto nivel de negligencia, n = 53; maltrato acumulativo, n = 45). El maltrato acumulado se asoció con una mayor gravedad de los síntomas de TEPT y TEPTC que el maltrato limitado y la clase de alto nivel de negligencia, con tamaños de efecto que van de 0,62 a 0,93.
Conclusiones: La asociación de la clase de maltrato acumulativo con la mayor gravedad de los síntomas de TEPT y TEPTC destaca el efecto perjudicial del maltrato acumulativo. La detección de una clase de alto nivel de negligencia identifica a los niños y adolescentes, que tienen un alto riesgo de sufrir maltrato en el futuro debido a sus experiencias anteriores de negligencia y la falta de protección asociada. El examen de la asociación de distintas clases de maltrato con TEPT y TEPTC de la CIE-11 podría proporcionar implicaciones para la prevención, evaluación y tratamiento específicos.
PALABRAS CLAVE: Niños, adolescentes, cuidados alternativos, CIE-11, trastorno de estrés postraumático (TEPT), TEPT Complejo, negligencia, abuso, maltrato infantil, análisis de clases latente
背景: 寄养的儿童和青少年经常会遭受多种并发的虐待。但是, 关于虐待亚型的不同组合 (称为虐待类别) 知之甚少。此外, 尚未在儿童和青少年中研究这些虐待类别与ICD-11创伤后应激障碍 (PTSD) 和复杂性PTSD (CPTSD) 之间的关联。在先前的研究中, 以累积虐待为特征的类别与严重的心理病理症状相关。到目前为止, 尚无研究考查ICD-11 PTSD和CPTSD。
目的: 本研究的第一个目标是通过考查经常并发的虐待亚型来检测不同的虐待类别。第二个目标是考查这些虐待类别与ICD-11 PTSD和CPTSD之间的关联。
方法: 参与者为目前居住在下奥地利州寄养机构中的147名儿童和青少年。使用标准化自我报告问卷评估了虐待史, ICD-11 PTSD和CPTSD。潜在类别分析用于考查虐待亚型。 χ2差异检验用于考查类别与PTSD和CPTSD的关联。
结果: 识别出3种包含不同虐待亚型的潜在类别 (有限虐待类, n= 49; 高度忽视类, n= 53; 累积虐待类, n= 45) 。与有限虐待类和高度忽视类相比, 累积虐待类与更高的PTSD和CPTSD症状严重程度相关, 其效应量范围为0.62至0.93。
结论: 累积虐待类与最高的PTSD和CPTSD症状严重程度的关联突显了累积虐待类的有害影响。发现高度忽视类识别出的儿童和青少年, 由于先前的被忽视经历和相关保护的缺乏, 具有未来遭受虐待的高风险。对不同虐待类别与ICD-11 PTSD和CPTSD关联的考查可能对于针对性预防, 评估和治疗有所启发.
关键词: 儿童, 青少年, 寄养, ICD-11, 创伤后应激障碍 (PTSD), 复杂性PTSD, 忽视虐待, 童年期虐待, 潜在类别分析
1. Background
1.1. Childhood maltreatment
Worldwide, many children and adolescents suffer from the mental and physical consequences of childhood maltreatment (Cicchetti, 2016), commonly defined as sexual, physical and emotional abuse and physical and emotional neglect (Krug, Dahlberg, Mercy, Zwi, & Lozano, 2002). Different subtypes of childhood maltreatment seldom occur in isolation. Rather, they are characterized by their tendency to co-occur (Masten & Barnes, 2018). This is described by the term cumulative maltreatment (Briere, Agee, & Dietrich, 2016; Hodges et al., 2013).
1.2. Foster care
Children and adolescents living in foster care often have suffered from a variety of early experiences of maltreatment prior to their foster care placement such as neglect and abuse (Bronsard et al., 2016; Greeson et al., 2011; Oswald, Heil, & Goldbeck, 2010). Data from several studies suggest that foster children are especially at risk of experiencing cumulative maltreatment (Lawrence, Carlson, & Egeland, 2006). They often report many co-occurring types of maltreatment, with rates of experiencing more than one subtype ranging from 35% (Greger, Myhre, Lydersen, & Jozefiak, 2015) to 81.2% (Collin-Vézina, Coleman, Milne, Sell, & Daigneault, 2011). A crucial factor for the well-being of children and adolescents in foster care is the stability of placement, which subsequently has an impact on other relevant psychopathological outcomes (Moore, McDonald, & Cronbaugh-Auld, 2016). Therefore, frequent changes in foster care placement can be a risk factor for healthy development (Lewis, Dozier, Ackerman, & Sepulveda-Kozakowski, 2007; Newton, Litrownik, & Landsverk, 2000; Rubin, O’Reilly, Luan, & Localio, 2007). Furthermore, the duration of foster care stay was also associated with physical and mental well-being in prior studies (Fallesen, 2013; Frenkel et al., 2020; Navarro-Soria, Servera, & Burns, 2020).
1.3. Classes of childhood maltreatment
Despite the known risk of cumulative maltreatment, little is known about different combinations of maltreatment subtypes, referred to as maltreatment classes, and their association with psychopathological symptoms (Lotzin, Grundmann, Hiller, Pawils, & Schäfer, 2019; Rebbe, Nurius, Ahrens, & Courtney, 2017). One reason for this is that traditional, variable-centred methods are not able to take different combinations of experiences of maltreatment into account (Debowska, Willmott, Boduszek, & Jones, 2017). However, the person-centred approach latent class analysis (LCA) is well suited to depict heterogeneity and account for the complexity in the processing of maltreatment, because it is capable of making statements about an individual (Warmingham, Handley, Rogosch, Manly, & Cicchetti, 2019).
So far, only two studies have dealt with maltreatment and trauma classes in foster children and adolescents, which have found a diverging number of classes (Pears, Kim, & Fisher, 2008; Rebbe et al., 2017). In those studies, different types of abuse, neglect and other potentially traumatic experiences were assessed in preschool children and adolescents. The studies found four (Pears et al., 2008) and three (Rebbe et al., 2017) classes of maltreatment and trauma, respectively. In both studies, the class characterized by cumulative maltreatment and trauma was associated with the most severe mental health problems. In other studies assessing different types of childhood maltreatment (sexual abuse, physical abuse, emotional abuse and neglect), three (Charak, Tromp, & Koot, 2018) and four (Charak & Koot, 2015; Warmingham et al., 2019) distinct classes of childhood maltreatment were found, respectively. Within the investigation of adolescents involved in the justice system, three studies examining polyvictimization found three (Charak, Ford, Modrowski, & Kerig, 2019) six (Ford, Elhai, Connor, & Frueh, 2010) and five classes (Adams et al., 2016), respectively. In all studies, individuals in the subgroups characterized by cumulative maltreatment and polyvictimization had an elevated risk of showing psychopathological symptoms.
Since children and adolescents in foster care usually experience several subtypes of maltreatment (Bronsard et al., 2016; Greeson et al., 2011; Oswald et al., 2010), it is important to examine different combinations of co-occurring maltreatment subtypes in this population thoroughly. To date, only two studies examined maltreatment classes in children or adolescents in foster care (Pears et al., 2008; Rebbe et al., 2017). However, only one study assessed childhood maltreatment comprehensively (Pears et al., 2008). Up to date, there is no study examining maltreatment classes in foster children in Austria.
1.4. Post-traumatic sequelae: ICD-11 PTSD and CPTSD
The experience of childhood maltreatment is associated with an increased risk for developing a wide range of post-traumatic symptoms such as posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD; Brewin et al., 2017; Maercker et al., 2013). In this context, both types of maltreatment, namely abuse and neglect, can result in post-traumatic symptoms (Gilbert et al., 2009; Nikulina, Widom, & Czaja, 2011; Widom, 1999). The World Health Organization (WHO) included the two disorders PTSD and CPTSD in the 11th version of the International Classification of Diseases (ICD-11; WHO, 2018). In the ICD-11, the PTSD diagnosis was reduced to three symptom clusters and a complex form of PTSD, namely CPTSD, was introduced (Brewin et al., 2017; Maercker et al., 2013). While PTSD is characterized by the symptom clusters re-experiencing, avoidance and sense of threat, CPTSD is characterized by the symptom clusters of PTSD and three symptom clusters related to disturbances in self-organization (DSO). The DSO symptom clusters include negative self-concept, affective dysregulation and disturbances in relationships (Bisson, 2013; Hyland et al., 2017).
Although the construct validity of PTSD and CPTSD has been largely confirmed in adults (Cloitre et al., 2018; Hyland et al., 2017; Karatzias et al., 2016) and also in children and adolescents (Haselgruber, Sölva, & Lueger-Schuster, 2019; Kazlauskas et al., 2020; Sachser, Keller, & Goldbeck, 2017), there are still uncertainties regarding the specific risk factors that are associated with the two diagnoses PTSD and CPTSD, especially in children and adolescents (Cloitre et al., 2020; Hecker, Huber, Maier, & Maercker, 2018). The experience of cumulative maltreatment was found to be associated with symptom complexity in children (Cloitre et al., 2009). In addition, it was often reported that both gender and age were associated with differences in the severity and frequency of posttraumatic symptoms (Bokszczanin, 2007; Ditlevsen & Elklit, 2010; Steinberg et al., 2013).
1.5. The current study
The first objective of this study was the examination of frequently occurring combinations of subtypes of childhood maltreatment to detect latent classes of childhood maltreatment in foster children and adolescents in Austria. The second objective was the examination of the association of those maltreatment classes with ICD-11 PTSD and CPTSD. Covariates age, gender, number of placements and duration of foster care placement were included.
Based on prior findings, it was hypothesized that
three or four classes of maltreatment will be found, which can be characterized by different combinations of abuse and neglect;
at least one class depicting cumulative maltreatment will be found;
classes characterized by cumulative maltreatment will be associated with greater symptom severity in PTSD and CPTSD;
2. Methods
2.1. Participants
Recruitment of participants was conducted in cooperation with the commissioning authorities of the government of Lower Austria. Eligibility criteria required individuals to be aged 10 to 18 at the beginning of the study, accommodated for at least 12 more months in care, and speak German sufficiently. Individuals were excluded if they were in an acute and severe psychiatric crisis, had a substance dependency, showed suicidal tendencies or were intellectually disabled to the extent that they were unlikely to understand the questions.
An initial sample of 161 children and adolescents were included in the study. Seven participants were excluded because of severe cognitive problems. The data from another seven participants had to be excluded from the analysis because they did not fill out any of the questionnaires included in the analysis. The exclusion of these cases resulted in a sample of 147 children and adolescents for the analysis. Of this sample, 69.4% of the participants were male and 30.6% were female. The mean age was M = 14.36 (SD = 2.48). The length of stay in the foster care was an average of M = 2.76 years (SD = 1.99). Excluded participants did not differ from included participants in terms of age (t(152) = 1.834, p = .069). However, the two groups showed differences in terms of gender (χ2 (1) = 26.597, p < .001), with only boys being excluded.
2.2. Measures
2.2.1. Childhood maltreatment
Five types of childhood maltreatment were assessed using the Childhood Trauma Questionnaire (CTQ, Bernstein et al., 2003). The CTQ is a screening instrument that enquires physical, sexual and emotional abuse as well as physical and emotional neglect with five items each on a five-point Likert scale (ranging from ‘Never true’ to ‘Very often true’). The CTQ is widely used to assess maltreatment experiences in childhood. The psychometric properties for the present study were mostly good with a Cronbach’s α of .89 (sexual abuse), .87 (emotional abuse), .87 (emotional neglect) and .86 (physical abuse). One exception was physical neglect with a poor Cronbach’s α of .40. However, this is in line with validation studies in German (Karos, Niederstrasser, Abidi, Bernstein, & Bader, 2014), Swedish (Gerdner & Allgulander, 2009), and Canadian populations (Paivio & Cramer, 2004). For the latent class analysis, the dichotomous values of the individual scales were used. These were calculated based on the cut-offs of the manual (Bernstein & Fink, 1998).
2.2.2. PTSD and CPTSD
The two disorders PTSD and CPTSD were assessed using the International Trauma Questionnaire- Child and Adolescent Version (ITQ- CA, Cloitre et al., 2018). This questionnaire is based on the recently released ICD-11 (WHO, 2018). It is composed of 12 items, which are rated on a five-point Likert scale (ranging from ‘Never’ to ‘Almost always’) measuring PTSD and CPTSD and 10 items which are rated dichotomously (‘Yes’/‘No’) measuring functional impairment for each disorder. The different scales each consist of two items and Cronbach’s α may therefore be inaccurate. Because of this, composite reliability (CR) was applied in order to calculate internal consistency. The CR is acceptable for a score > .60 (Raykov, 1997). In this study, the scales showed acceptable through good internal consistencies of a CR of .73 (PTSD) and .88 (CPTSD).
2.3. Missing data
When considering the individual subscales of the CTQ, the following percentages of missing values were found: Emotional abuse: 2%, physical abuse: 3.4%, sexual abuse: 0%; emotional neglect: 4.1%, physical neglect: 1.4%. For the ITQ, 2% of missing values were found for both diagnoses. Full information maximum likelihood was used to handle all missing data. This method does not depend on the number of missing values (Enders & Bandalos, 2001) and is state-of-the-art to manage missing data (Schafer & Graham, 2002). To test the missing data mechanisms, Little’s MCAR Test was conducted. It yielded a non-significant result (χ2(180) = 183.31, p = .417). Therefore, it can be assumed that the data are missing completely at random (MCAR).
2.4. Procedure
The data were obtained within the data collection of a large-scale longitudinal research project, which was initiated by the government of Lower Austria. The data for this study was assessed in two measurement maves (1: May – October 2018; 2: March- September 2019). Data concerning family maltreatment history prior to foster care placement were collected during the first measurement wave. The data on ICD-11 PTSD and CPTSD were drawn from the second wave when the ITQ- CA was used for the first time. The Ethics Committee of the University of Vienna (#00328) approved an ethic proposal in advance.
The participants and their respective caregivers provided written consent after the procedure was explained to the children and adolescents in detail. Clinical psychologists in training and master students under supervision visited the foster care institutions to administer self-report questionnaires to collect the data. The assessment was mainly conducted within group settings with two participants being closely supervised by one psychologist. Where any kind of difficulties (e.g. reading or attention deficits) were known, an individual setting was implemented.
2.5. Data analysis
Data analysis was conducted with IBM SPSS Statistics 25 and Mplus 7.0 (Muthén & Muthén, 1998-2017). Descriptive statistics and ANCOVA were obtained with IBM SPSS Statistics 25. LCA and χ2 group comparisons were conducted with Mplus 7.0. LCA was used to examine the best fitting number of classes of childhood maltreatment. For the estimation of latent classes, different dichotomous indicators are examined. To establish the optimal number of latent classes, an iterative estimation of different class solutions identifies the model solution that shows the best fit-indices (Nylund, Asparouhov, & Muthén, 2007). In the present study, the five different subtypes of maltreatment assessed dichotomously with the CTQ were included as indicators for the classes. To avoid solutions based on local maxima, 5000 random starts and 1000 iterations have been specified for each model (Hipp & Bauer, 2006). In order to determine the most appropriate number of classes, models with different number of classes (2–5) were calculated consecutively and the fit indices of the classes were compared. Smaller scores on the AIC (Akaike, 1974), BIC (Schwarz, 1978) and SABIC (Sclove, 1987) point to a higher fit. A value > .80 for entropy points towards a reliable classification of participants. Non- significant values of the bootstrap likelihood ratio test (BLRT) point towards k-1 classes. Since model fit indices often do not clearly indicate a single outcome, it is proposed to consider all fit indices. The interpretability and practical applicability of a solution is also an important criterion on which the decision should be based (Nylund-Gibson & Choi, 2018).
Follow up comparisons were conducted with the three-step approach using the DE3STEP command in Mplus (Vermunt, 2010). χ2 group comparisons were conducted to test the differences between the classes concerning symptoms of PTSD, DSO, and CPTSD. An ANCOVA was conducted to include the covariates age gender, number of placements, and duration of placement.
3. Results
3.1. Descriptive statistics
Regarding the co-occurrence of different subtypes of childhood maltreatment, 23.1% reported no maltreatment, 20.1% reported having experienced one subtype of maltreatment, 23.1% reported two different types of maltreatment, 12.7% reported the experience of three subtypes, 12.7% reported having experienced four subtypes and 8.2% reported the experience of all five subtypes of childhood maltreatment. In total, 56.7% of children and adolescents reported having experienced more than one experience of maltreatment according to the CTQ. The screening for ICD-11 post-traumatic symptoms showed that 8.7% of the participants fulfilled the criteria for PTSD and 8.2% fulfilled the criteria for CPTSD. For descriptive statistics of sociodemographic variables, see Table 1. For descriptive statistics of the CTQ subscales, PTSD/CPTSD and functional impairment sum score for the sample, see Table 2. variables included in the analysis, see Supplement 1, online supplementary data.
Table 1.
Descriptive statistics of sociodemographic variables
| N (%) | M (SD) | |
|---|---|---|
| Nationality | ||
| Austria | 105 (89.0) | |
| Germany | 3 (2.5) | |
| Other | 10 (8.5) | |
| Education | ||
| Special needs school | 55 (47.8) | |
| Elementary school | 1 (0.9) | |
| Secondary school | 34 (29.6) | |
| Vocational school | 23 (20.0) | |
| Higher educational school | 2 (1.7) | |
| Contact with parents | ||
| No | 5 (3.6) | |
| Yes | 132 (95.7) | |
| Once a week or more often | 110 (85.9) | |
| Once a month or more often | 16 (12.5) | |
| Once in six months or more often | 2 (1.6) | |
| Age of first placement | 10.92 (3.36) | |
| Number of placements | 1.17 (0.40) |
N = number of participants, % = percent, M = mean, SD = standard deviation.
Table 2.
Descriptive statistics of the CTQ subscales, PTSD/CPTSD and functional impairment sum score for the sample (N = 147)
| M | SD | Range | |
|---|---|---|---|
| Maltreatment | |||
| Emotional abuse | 8.99 | 4.93 | 1–25 |
| Physical abuse | 7.57 | 4.45 | 1–25 |
| Sexual abuse | 6.05 | 2.98 | 1–25 |
| Emotional neglect | 9.86 | 4.68 | 1–25 |
| Physical neglect | 8.07 | 3.07 | 1–25 |
| Post-traumatic symptoms | |||
| PTSD | 5.99 | 4.89 | 0–30 |
| DSO | 6.25 | 5.82 | 0–30 |
| CPTSD | 12.21 | 9.82 | 0–60 |
| Functional impairment | |||
| PTSD | 1.64 | 1.70 | 0–5 |
| DSO | 1.57 | 1.77 | 0–5 |
M = mean; SD = standard deviation; Range = possible range of the scale.
3.2. Latent class analysis
For the comparison of the model fit indices for the LCA, see Table 3. Based on the lowest levels on the AIC and the SABIC, the highest levels on Entropy and a significant BLRT, the three-class solution was chosen as the best fitting model. This solution showed appropriate classification of individuals with average latent class probabilities ranging from .921 to .954. According to the characteristics of each class, the classes were labelled as follows: Class 1, which comprised 32.1% of the participants (n = 49; 6.1% female and 27.2% male), exhibited low rates on all subtypes of maltreatment, therefore it was termed ‘limited maltreatment’. Class 2 exhibited low rates on the three abuse subtypes and high rates on the two neglect subtypes, therefore it was termed ‘high neglect’. This class comprised 36.1% of the participants (n = 53; 15.6% female and 15% male). Class 3, which comprised 31.7% of the participants (n = 45; 27.2% female and 8.8% male) exhibited high rates on all maltreatment subtypes, therefore it was termed ‘cumulative maltreatment’. For the visual presentation of the three classes, see Figure 1.
Table 3.
Model fit indices of latent classes of childhood trauma subtypes (N = 147)
| C | LL | AIC | BIC | SABIC | Entropy | BLRT p |
|---|---|---|---|---|---|---|
| 2 | −410.550 | 843.101 | 875.995 | 841.185 | 0.768 | −458.066 <.001 |
| 3 | −403.105 | 840.209 | 891.047 | 837.249 | 0.861 |
−410.550 <.001 |
| 4 | −399.175 | 844.350 | 913.130 | 840.345 | 0.815 | −403.105.375 |
| 5 | −397.340 | 852.680 | 939.402 | 847.630 | 0.793 | −399.175 0.667 |
C = number of classes; LL = log-likelihood; AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; SABIC = Sample-size adjusted Bayesian Information Criterion; BLRT = bootstrapped likelihood ratio test; p = p-value.
Bold values indicate the best fitting parameter for each model.
Figure 1.
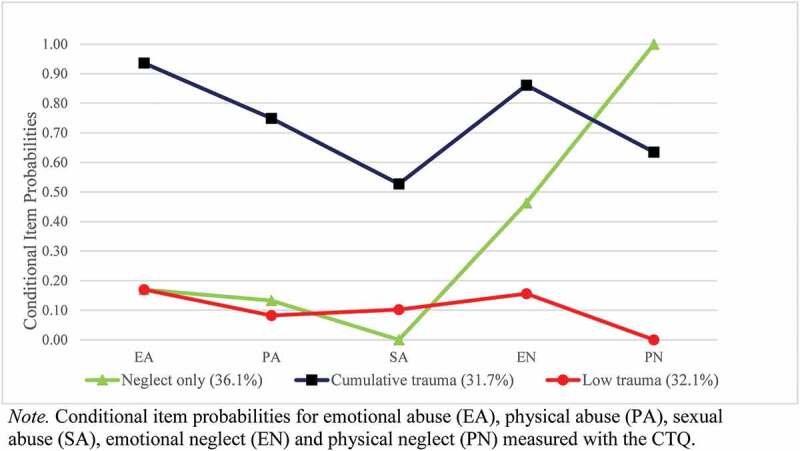
Graphic representation of the distinct classes
3.3. Class comparison
The cumulative maltreatment class showed the highest PTSD, DSO, and CPTSD symptom severity and functional impairment. The high neglect class showed the lowest post-traumatic symptom severity in PTSD, DSO, and CPTSD. The limited maltreatment class showed medium symptom severity in PTSD, DSO, and CPTSD and the lowest values for functional impairment. For a descriptive comparison of the means and standard deviations between the three maltreatment classes for age, PTSD, DSO, CPTSD, and functional impairment, see Table 4.
Table 4.
Descriptive comparison of trauma classes according to age, PTSD, DSO and CPTSD symptom severity and functional impairment (FI) for the distinct symptom clusters PTSD and DSO
| Class 1 ‘limited maltreatment’ |
Class 2 ‘high neglect’ |
Class 3 ‘cumulative maltreatment’ |
|
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| Age | 14.72 (0.36) | 13.97 (0.39) | 14.85 (0.38) |
| PTSD | 5.25 (0.70) | 4.25 (0.73) | 8.65 (0.81) |
| DSO | 3.60 (0.73) | 2.46 (1.17) | 11.68 (0.91) |
| CPTSD | 9.40 (1.31) | 7.57 (1.80) | 19.69 (1.66) |
| FI PTSD | 1.26 (0.23) | 1.81 (0.67) | 2.22 (0.33) |
| FI DSO | 1.04 (0.23) | 1.67 (0.76) | 2.50 (0.40) |
M = mean, SD = standard deviation.
Bolded values indicate the highest scores for each variable.
Regarding the differences in post-traumatic symptoms between the individual classes, both limited maltreatment and high neglect differed significantly from cumulative maltreatment. The high neglect class showed lower symptom severity in PTSD (χ2 = 14.08 (2), p < .001, d = .62), DSO (χ2 = 43.5 (2), p < .001, d = .90) and CPTSD (χ2 = 20.18 (2), p < .001, d = .91) than the cumulative maltreatment class. Likewise, the limited maltreatment class showed significantly lower symptom severity in PTSD (χ2 = 9.02 (2), p = .003, d = .81), DSO (χ2 = 41.39 (2), p < .001, d = .89) and CPTSD (χ2 = 20.80 (2), p < .001, d = .93) than the cumulative maltreatment class. However, the limited maltreatment class did not differ significantly from the high neglect class regarding symptom severity for PTSD, DSO, and CPTSD. Regarding functional impairment, only the limited maltreatment class differed significantly from the cumulative maltreatment class in functional impairment for the PTSD cluster (χ2 = 4.93 (2), p = .026, d = .33) and for the DSO cluster (χ2 = 8.62 (2), p = .003, d = .45). Table 5 shows the χ2 differences in PTSD, DSO, CPTSD, and functional impairment. For a descriptive comparison of maltreatment classes regarding the CTQ subscales, see Table 6.
Table 5.
χ2 differences for PTSD, DSO, CPTSD and functional impairment (FI) for both clusters depending on trauma classes
| ‘high neglect’ vs. ‘cumulative maltreatment’ |
‘high neglect’ vs. ‘limited maltreatment’ |
‘cumulative maltreatment’ vs. ‘limited maltreatment’ |
|
|---|---|---|---|
| χ2 | χ2 | χ2 | |
| PTSD | 14.08** | 0.97 | 9.02* |
| DSO | 43.50** | 0.64 | 41.39** |
| CPTSD | 20.18** | 0.67 | 20.80** |
| FI PTSD | 0.27 | 0.47 | 4.93* |
| FI DSO | 0.78 | 0.54 | 8.62* |
*Significant values p < .05; **significant values p < .001.
Table 6.
Descriptive comparison of maltreatment classes according to mean and standard deviation for the CTQ subscales
| Class 1 ‘limited maltreatment’ |
Class 2 ‘high neglect’ |
Class 3 ‘cumulative maltreatment’ |
|
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| Emotional abuse | 7.00 (0.29) | 6.35 (0.24) | 14.21 (0.91) |
| Physical abuse | 4.94 (0.20) | 6.64 (0.86) | 12.41 (0.96) |
| Sexual abuse | 5.13 (0.10) | 4.87 (0.11) | 8.55 (0.81) |
| Emotional neglect | 7.01 (0.26) | 11.46 (1.46) | 14.63 (0.77) |
| Physical neglect | 6.56 (0.21) | 9.55 (0.49) | 10.43 (0.69) |
M = mean, SD = standard deviation.
Bolded values indicate the highest scores for each variable.
Regarding the ANCOVA for PTSD symptom severity, gender was a significant covariate (F(1) = 16.71, p < .001). However, age (F(1) = 0.42, p = .516), number of placements (F(1) = 0.02, p = .895), and duration of placement (F(1) = 0.97, p = .328) were not significant. Class membership was still a significant predictor after including the covariates (F(2) = 4.24, p = .16). For CPTSD symptom severity, gender was a significant covariate (F(1) = 19.85, p < .001). Age (F(1) = 0.33, p = .565), number of placements (F(1) = 0.53, p = .470), and duration of placement (F(1) = 1.85, p = .178) were not significant. However, class membership was still a significant predictor after including the covariates (F(2) = 7.86, p = .001).
4. Discussion
Based on the present data on maltreatment subtypes, three latent classes were found. Previous studies examining co-occurring subtypes of maltreatment found inconsistent results regarding the number of classes. In accordance with the present findings, three classes were found within adolescents in foster care (Rebbe et al., 2017) and adolescents referred to mental health services (Charak et al., 2018). Other studies found four maltreatment classes (Charak & Koot, 2015; Pears et al., 2008; Warmingham et al., 2019). Within the examination of polyvictimization, three (Charak et al., 2019), five (Adams et al., 2016), and six classes were found (Ford et al., 2010), respectively. However, those inconsistencies may be due to the inclusion of different types of maltreatment and potentially traumatic experiences in the various studies. In some of the studies, a wide range of different experiences of maltreatment, trauma and other environmental risk factors were included. The findings from prior studies support the conclusion that the number of classes increases with the number of potentially traumatic experiences included in the analysis. Furthermore, differences in the populations under examination might have influenced the results.
The three classes found in the current study are characterized by different combinations of subtypes of maltreatment (high neglect, cumulative maltreatment, limited maltreatment). In accordance with a study based on a sample of adolescents in foster care (Rebbe et al., 2017), a low maltreatment class and a cumulative maltreatment class were found in the present study. This finding was also reported by studies examining other populations (Adams et al., 2016; Charak et al., 2018; Ford et al., 2010; Warmingham et al., 2019).
Surprisingly, a high neglect class was found in the present study. Only two other studies have found similar results with regard to a high neglect class (Charak & Koot, 2015; Warmingham et al., 2019). Those results are likely to be related to the assessment of neglect. In the present study, emotional and physical neglect were assessed with five items each, similar as maltreatment was assessed in the study by Charak and Koot (2015). In the study by Warmingham et al. (2019), four types of neglect were included. In contrast, other comparable studies often did not assess neglect (Ford et al., 2010) or just one form of neglect (Adams et al., 2016). However, another study assessing childhood maltreatment with the CTQ did not find a neglect only class (Charak et al., 2018). One possible explanation might be that although the children and adolescents in the present study are at very high risk of experiencing maltreatment and associated psychopathology, they do not necessarily show symptoms of a particular disorder. In the study by Charak et al., almost all participants had a diagnosed mental disorder (Charak et al., 2018) and the likelihood for a mental disorder increases with the experience of both, abuse and neglect (Pears et al., 2008). This may highlight the differences between the populations under investigation and the resulting need for individual examination of different populations to implement targetet prevention.
Neglect is considered as harmful and debilitating as abuse (Stoltenborgh, Bakermans-Kranenburg, & van IJzendoorn, 2013); however, it has often been insufficiently addressed in the investigation of child well-being. The experience of neglect in childhood could increase the risk of falling victim to another potentially traumatic experience, since failure to meet basic needs can create a lack of safety (Dubowitz et al., 2016). Neglected children and adolescents often show a range of different negative developmental outcomes including behavioural problems, delays in cognitive development and socio-emotional difficulties (Hildyard & Wolfe, 2002). Those factors in turn can be risk factors for further unfavourable developmental outcomes (Kobulsky, Dubowitz, & Xu, 2019). Furthermore, childhood neglect may have a profound impact on a person’s lifestyle, e.g. various (risky) behaviours increase the likelihood of experiencing a traumatic situation and subsequently developing PTSD (Widom, 1999).
Another important finding was that the cumulative maltreatment class was associated with a significantly higher ICD-11 CPTSD symptom severity than the limited maltreatment class and the high neglect class. These findings are in line with prior research, indicating that ICD-11 CPTSD symptom severity is associated with multiple experiences of different subtypes of childhood maltreatment (Hyland et al., 2017; Karatzias et al., 2019). In line with this, it was shown that cumulative maltreatment was associated with complex psychopathological symptoms in children (Cloitre et al., 2009; Hodges et al., 2013). Prior studies regarding maltreatment classes found associations between the cumulative maltreatment classes and a wide range of psychopathological problems (Adams et al., 2016; Ford et al., 2010; Warmingham et al., 2019).
Furthermore, the cumulative maltreatment class was associated with significantly higher ICD-11 PTSD symptom severity than the other two classes in the present study. This result corroborates the findings of two studies, who found that the class characterized by polyvictimization showed the highest PTSD symptom severity (Adams et al., 2016; Charak et al., 2019). However, as PTSD was assessed according to DSM-IV in the study by Adams et al. (2016), and according to DSM-5 in the study by Charak et al. (2019), it is not fully comparable to the present findings.
The cumulative maltreatment class did not differ significantly from the high neglect class in functional impairment for both post-traumatic clusters PTSD and DSO, indicating that neglect is as debilitating as abuse when concerning functional impairment in different domains of life. This is in line with frequently reported results from previous studies (Hildyard & Wolfe, 2002).
Contrary to expectations, a tendency was found that the high neglect class showed lower ICD-11 PTSD and CPTSD symptom severity than the limited maltreatment class. However, this tendency was not significant. This is possibly explained by the fact that PTSD and CPTSD are per definition related to a specific traumatic experience (Bisson, 2013; Hyland et al., 2017), however, neglect is not necessarily associated with one specific and distinct traumatic experience (Dubowitz et al., 2016), but is characterized by a persistent negligence of the needs and safety of a child (Stoltenborgh et al., 2013). Furthermore, individuals in the high neglect class may be more self-reflective and are therefore able to report and understand that they have been neglected. This self-reflection might also have contributed to a healthy self-management of their experiences (Ensink et al., 2015). Although, contrary to expectations, neglect was not associated with PTSD/CPTSD in this study, it may be associated with various other unfavourable developmental outcomes (Hildyard & Wolfe, 2002) and therefore an in-depth investigation is necessary.
Within the examination of covariates, only gender showed significant effects, with females being more likely to belong to the cumulative maltreatment class. This is in line with previous studies (Bokszczanin, 2007; Kaplow, Dodge, Amaya-Jackson, & Saxe, 2005).
4.1. Limitations
Some limitations are to be considered. Primarily, the assessment of the variables at two different time points may have led to the omission of experiences of maltreatment that occurred in the meantime. However, since maltreatment experiences within the family were assessed and children and adolescents were accommodated in foster care for the duration of the entire project, it may be assumed that no additional instances of maltreatment by parents have to be accounted for. Since self-assessment questionnaires were administered, it is possible that bias occurred because of the retrospective reporting. In addition, both experiences of maltreatment and psychopathological symptoms may not have been reported accurately (over-or underreporting). This may be due to several reasons, including feelings of shame or an inability to remember individual experiences of the participants. Regarding the assessment of post-traumatic symptoms, it should be considered that the ITQ is a screening instrument and is therefore to be interpreted with caution. Emotional neglect may be relatively receptive to individual interpretations (Stoltenborgh et al., 2013). Therefore, the questions concerning emotional neglect may have been difficult to answer for some participants, as this involves a certain ability of self-reflection. Furthermore, cronbach’s alpha for physical neglect is low and this scale may therefore be less reliable.
Another limitation was related to the representativeness of the sample. The population under examination is not representative for foster children and adolescents in the German-speaking area. Moreover, the sample was rather small for the implementation of an LCA. However, since the model estimations terminated normally and the fit indices were clearly interpretable, it can be assumed that the sample size was sufficient.
4.2. Implications
Knowledge about classes of childhood maltreatment and their association with ICD-11 post-traumatic symptoms is important to implement appropriate assessment, prevention, and treatment strategies. As there are very few instruments to assess ICD-11 PTSD and CPTSD in children and adolescents, data on this topic is sparse. Therefore, the examination of maltreatment classes as specific risk factors for PTSD and CPTSD provides relevant information for clinicians (Hyland et al., 2017) and also child protective services. Individuals who experienced different combinations of maltreatment subtypes need targeted support. As PTSD and CPTSD are two distinct disorders, prevention, intervention and treatment should include different strategies than current programmes treating PTSD (Karatzias et al., 2017).
As the experience of neglect can have a strong negative impact on the overall mental health of an individual (Stoltenborgh et al., 2013), the detection of a high neglect class in the present study should have implications for assessment of maltreatment experiences in children and adolescents in foster care. Furthermore, it is important to examine other problems associated with neglect reported in prior studies such as behavioural problems, depressive symptoms, anxiety and personality pathology (Charak & Koot, 2015; Ford et al., 2010; Rebbe et al., 2017; Warmingham et al., 2019). Overall, it is vital to identify distinct classes of subtypes of childhood maltreatment to identify individuals who are at a high risk for an unfavourable futher development.
Furthermore, the examination of the association between specific risk factors and the development of distinct post-traumatic symptoms, as early as in childhood and adolescence is important to understand the needs of survivors of early maltreatment and neglect. Thereby, appropriate strategies for prevention, intervention and treatment can be informed and prevention from a chronic psychopathological development can be achieved.
Supplementary Material
Funding Statement
This work was funded by the Lower Austrian Government [grant number FA472021].
Disclosure statement
The authors declare that they have no competing financial or personal interests.
Data availability statement
The present data were assessed in the course of a research project commissioned and funded by the government of Lower Austria. Therefore, data cannot be shared due to legal reasons.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Adams, Z. W., Moreland, A., Cohen, J. R., Lee, R. C., Hanson, R. F., Danielson, C. K., … Briggs, E. C. (2016). Polyvictimization: Latent profiles and mental health outcomes in a clinical sample of adolescents. Psychology of Violence, 6(1), 145–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akaike, H. (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19(6), 716–723. [Google Scholar]
- Bernstein, D. P., & Fink, L. (1998). Childhood trauma questionnaire: A retrospective self-report: Manual. San Antonio, TX: Harcourt Brace & Co. [Google Scholar]
- Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., … Zule, W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. [DOI] [PubMed] [Google Scholar]
- Bisson, J. I. (2013). What happened to harmonization of the PTSD diagnosis? The divergence of ICD11 and DSM5. Epidemiology and Psychiatric Sciences, 22(3), 205–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokszczanin, A. (2007). PTSD symptoms in children and adolescents 28 months after a flood: Age and gender differences. Journal of Traumatic Stress, 20(3), 347–351. [DOI] [PubMed] [Google Scholar]
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., … Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. [DOI] [PubMed] [Google Scholar]
- Briere, J., Agee, E., & Dietrich, A. (2016). Cumulative trauma and current posttraumatic stress disorder status in general population and inmate samples. Psychological Trauma: Theory, Research, Practice and Policy, 8(4), 439–446. [DOI] [PubMed] [Google Scholar]
- Bronsard, G., Alessandrini, M., Fond, G., Loundou, A., Auquier, P., Tordjman, S., & Boyer, L. (2016). The prevalence of mental disorders among children and adolescents in the child welfare system: A systematic review and meta-analysis. Medicine, 95(7), 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charak, R., Ford, J. D., Modrowski, C. A., & Kerig, P. K. (2019). Polyvictimization, emotion dysregulation, symptoms of posttraumatic stress disorder, and behavioral health problems among justice-involved youth: A latent class analysis. Journal of Abnormal Child Psychology, 47(2), 287–298. [DOI] [PubMed] [Google Scholar]
- Charak, R., & Koot, H. M. (2015). Severity of maltreatment and personality pathology in adolescents of Jammu, India: A latent class approach. Child Abuse & Neglect, 50, 56–66. [DOI] [PubMed] [Google Scholar]
- Charak, R., Tromp, N. B., & Koot, H. M. (2018). Associations of specific and multiple types of childhood abuse and neglect with personality pathology among adolescents referred for mental health services. Psychiatry Research, 270, 906–914. [DOI] [PubMed] [Google Scholar]
- Cicchetti (Ed.). (2016). Developmental psychopathology. Hoboken, NJ, USA: John Wiley & Sons, Inc. doi: 10.1002/9781119125556 [DOI] [Google Scholar]
- Cloitre, M., Brewin, C. R., Bisson, J. I., Hyland, P., Karatzias, T., Lueger-Schuster, B., … Shevlin, M. (2020). Evidence for the coherence and integrity of the complex PTSD (CPTSD) diagnosis: Response to Achterhof et al., (2019) and Ford (2020). European Journal of Psychotraumatology, 11(1), 1739873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta psychiatrica Scandinavica, 138(6), 536–546. [DOI] [PubMed] [Google Scholar]
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B. A, Pynoos, R. S., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. [DOI] [PubMed] [Google Scholar]
- Collin-Vézina, D., Coleman, K., Milne, L., Sell, J., & Daigneault, I. (2011). Trauma experiences, maltreatment-related impairments, and resilience among child welfare youth in residential care. International Journal of Mental Health and Addiction, 9(5), 577–589. [Google Scholar]
- Debowska, A., Willmott, D., Boduszek, D., & Jones, A. D. (2017). What do we know about child abuse and neglect patterns of co-occurrence? A systematic review of profiling studies and recommendations for future research. Child Abuse & Neglect, 70, 100–111. [DOI] [PubMed] [Google Scholar]
- Ditlevsen, D. N., & Elklit, A. (2010). The combined effect of gender and age on post traumatic stress disorder: Do men and women show differences in the lifespan distribution of the disorder? Annals of General Psychiatry, 9(1), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz, H., Thompson, R., Proctor, L., Metzger, R., Black, M. M., English, D., … Magder, L. (2016). Adversity, maltreatment, and resilience in young children. Academic Pediatrics, 16(3), 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders, C. K., & Bandalos, D. L. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Retrieved from https://works.bepress.com/deborah_bandalos/17/ [PubMed]
- Ensink, K., Normandin, L., Target, M., Fonagy, P., Sabourin, S., & Berthelot, N. (2015). Mentalization in children and mothers in the context of trauma: An initial study of the validity of the Child Reflective Functioning Scale. The British Journal of Developmental Psychology, 33(2), 203–217. [DOI] [PubMed] [Google Scholar]
- Fallesen, P. (2013). Time well spent: The duration of foster care and early adult labor market, educational, and health outcomes. Journal of Adolescence, 36(6), 1003–1011. [DOI] [PubMed] [Google Scholar]
- Ford, J. D., Elhai, J. D., Connor, D. F., & Frueh, B. C. (2010). Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 46(6), 545–552. [DOI] [PubMed] [Google Scholar]
- Frenkel, T. I., Donzella, B., Frenn, K. A., Rousseau, S., Fox, N. A., & Gunnar, M. R. (2020). Moderating the risk for attention deficits in children with pre-adoptive adversity: The protective role of shorter duration of out of home placement and children’s enhanced error monitoring. Journal of Abnormal Child Psychology, 1–14. doi: 10.1007/s10802-020-00671-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerdner, A., & Allgulander, C. (2009). Psychometric properties of the Swedish version of the Childhood Trauma Questionnaire-Short Form (CTQ-SF). Nordic Journal of Psychiatry, 63(2), 160–170. [DOI] [PubMed] [Google Scholar]
- Gilbert, R., Widom, C. S., Browne, K., Fergusson, D., Webb, E., & Janson, S. (2009). Burden and consequences of child maltreatment in high-income countries. The Lancet, 373(9657), 68–81. [DOI] [PubMed] [Google Scholar]
- Greeson, J. K. P., Ake, G. S., Howard, M. S., Briggs, E. C., Ko, S. J., & Pynoos, R. S. (2011). Complex trauma and mental health in children and adolescents placed in foster care: Findings from the National Child Traumatic Stress Network. Child Welfare, 90(6), 91–108. [PubMed] [Google Scholar]
- Greger, H. K., Myhre, A. K., Lydersen, S., & Jozefiak, T. (2015). Previous maltreatment and present mental health in a high-risk adolescent population. Child Abuse & Neglect, 45, 122–134. [DOI] [PubMed] [Google Scholar]
- Haselgruber, A., Sölva, K., & Lueger-Schuster, B. (2019). Validation of ICD-11 PTSD and complex PTSD in foster children using the International Trauma Questionnaire. Acta psychiatrica Scandinavica. Advance online publication. doi: 10.1111/acps.13100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecker, T., Huber, S., Maier, T., & Maercker, A. (2018). Differential associations among pTSD and complex PTSD symptoms and traumatic experiences and postmigration difficulties in a culturally diverse refugee sample. Journal of Traumatic Stress, 31(6), 795–804. [DOI] [PubMed] [Google Scholar]
- Hildyard, K. L., & Wolfe, D. A. (2002). Child neglect: Developmental issues and outcomes. Child Abuse & Neglect, 26(6–7), 679–695. [DOI] [PubMed] [Google Scholar]
- Hipp, J. R., & Bauer, D. J. (2006). Local solutions in the estimation of growth mixture models. Psychological Methods, 11(1), 36–53. [DOI] [PubMed] [Google Scholar]
- Hodges, M., Godbout, N., Briere, J., Lanktree, C., Gilbert, A., & Kletzka, N. T. (2013). Cumulative trauma and symptom complexity in children: A path analysis. Child Abuse & Neglect, 37(11), 891–898. [DOI] [PubMed] [Google Scholar]
- Hyland, P., Murphy, J., Shevlin, M., Vallières, F., McElroy, E., Elklit, A., … Cloitre, M. (2017). Variation in post-traumatic response: The role of trauma type in predicting ICD-11 PTSD and CPTSD symptoms. Social Psychiatry and Psychiatric Epidemiology, 52(6), 727–736. [DOI] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M., Brewin, C. R., Cloitre, M., Downes, A. J., Jumbe, S., … Roberts, N. P. (2017). Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Acta psychiatrica Scandinavica, 136(3), 313–322. [DOI] [PubMed] [Google Scholar]
- Kaplow, J. B., Dodge, K. A., Amaya-Jackson, L., & Saxe, G. N. (2005). Pathways to PTSD, part II: Sexually abused children. The American Journal of Psychiatry, 162(7), 1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T., Hyland, P., Bradley, A., Cloitre, M., Roberts, N. P., Bisson, J. I., & Shevlin, M. (2019). Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: Findings from a trauma-exposed population-based sample of adults in the UK. Depression and Anxiety, 36(9), 887–894. [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2016). An initial psychometric assessment of an ICD-11 based measure of PTSD and complex PTSD (ICD-TQ): Evidence of construct validity. Journal of Anxiety Disorders, 44, 73–79. [DOI] [PubMed] [Google Scholar]
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., … Cloitre, M. (2017). Evidence of distinct profiles of Posttraumatic Stress Disorder (PTSD) and Complex Posttraumatic Stress Disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. [DOI] [PubMed] [Google Scholar]
- Karos, K., Niederstrasser, N., Abidi, L., Bernstein, D. P., & Bader, K. (2014). Factor structure, reliability, and known groups validity of the German version of the Childhood Trauma Questionnaire (Short-form) in Swiss patients and nonpatients. Journal of Child Sexual Abuse, 23(4), 418–430. [DOI] [PubMed] [Google Scholar]
- Kazlauskas, E., Zelviene, P., Daniunaite, I., Hyland, P., Kvedaraite, M., Shevlin, M., & Cloitre, M. (2020). The structure of ICD-11 PTSD and Complex PTSD in adolescents exposed to potentially traumatic experiences. Journal of Affective Disorders, 265, 169–174. [DOI] [PubMed] [Google Scholar]
- Kobulsky, J. M., Dubowitz, H., & Xu, Y. (2019). The global challenge of the neglect of children. Child Abuse & Neglect, 104296. doi: 10.1016/j.chiabu.2019.104296 [DOI] [PubMed] [Google Scholar]
- Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., & Lozano, R. (2002). World report on violence and health: Child abuse and neglect by parents and other caregivers. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Lawrence, C. R., Carlson, E. A., & Egeland, B. (2006). The impact of foster care on development. Development and Psychopathology, 18(1), 57–76. [DOI] [PubMed] [Google Scholar]
- Lewis, E. E., Dozier, M., Ackerman, J., & Sepulveda-Kozakowski, S. (2007). The effect of placement instability on adopted children’s inhibitory control abilities and oppositional behavior. Developmental Psychology, 43(6), 1415–1427. [DOI] [PubMed] [Google Scholar]
- Lotzin, A., Grundmann, J., Hiller, P., Pawils, S., & Schäfer, I. (2019). Profiles of childhood trauma in women with substance use disorders and comorbid Posttraumatic Stress Disorders. Frontiers in Psychiatry, 10, 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., van Ommeren, M., Jones, L. M., … Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 12(3), 198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten, A. S., & Barnes, A. J. (2018). Resilience in children: Developmental perspectives. Children, 5(7). doi: 10.3390/children5070098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, T. D., McDonald, T. P., & Cronbaugh-Auld, K. (2016). Assessing risk of placement instability to aid foster care placement decision making. Journal of Public Child Welfare, 10(2), 117–131. [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998-2017). Mplus user’s guide (Version Eight) [Computer software]. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Navarro-Soria, I., Servera, M., & Burns, G. L. (2020). Association of foster care and its duration with clinical symptoms and impairment: Foster care versus non-foster care comparisons with Spanish children. Journal of Child and Family Studies, 29(2), 526–533. [Google Scholar]
- Newton, R. R., Litrownik, A. J., & Landsverk, J. A. (2000). Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse & Neglect, 24(10), 1363–1374. [DOI] [PubMed] [Google Scholar]
- Nikulina, V., Widom, C. S., & Czaja, S. (2011). The role of childhood neglect and childhood poverty in predicting mental health, academic achievement and crime in adulthood. American Journal of Community Psychology, 48(3–4), 309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Nylund-Gibson, K., & Choi, A. Y. (2018). Ten frequently asked questions about latent class analysis. Translational Issues in Psychological Science, 4(4), 440–461. [Google Scholar]
- Oswald, S. H., Heil, K., & Goldbeck, L. (2010). History of maltreatment and mental health problems in foster children: A review of the literature. Journal of Pediatric Psychology, 35(5), 462–472. [DOI] [PubMed] [Google Scholar]
- Paivio, S. C., & Cramer, K. M. (2004). Factor structure and reliability of the Childhood Trauma Questionnaire in a Canadian undergraduate student sample. Child Abuse & Neglect, 28(8), 889–904. [DOI] [PubMed] [Google Scholar]
- Pears, K. C., Kim, H. K., & Fisher, P. A. (2008). Psychosocial and cognitive functioning of children with specific profiles of maltreatment. Child Abuse & Neglect, 32(10), 958–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov, T. (1997). Estimation of composite reliability for congeneric measures. Applied Psychological Measurement, 21(2), 173–184. [Google Scholar]
- Rebbe, R., Nurius, P. S., Ahrens, K. R., & Courtney, M. E. (2017). Adverse childhood experiences among youth aging out of foster care: A latent class analysis. Children and Youth Services Review, 74, 108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, D. M., O’Reilly, A. L. R., Luan, X., & Localio, A. R. (2007). The impact of placement stability on behavioral well-being for children in foster care. Pediatrics, 119(2), 336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(2), 160–168. [DOI] [PubMed] [Google Scholar]
- Schafer, J. L., & Graham, J. W. (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. [PubMed] [Google Scholar]
- Schwarz, G. (1978). Estimating the dimension of a model. The Annals of Statistics, 6(2), 461–464. [Google Scholar]
- Sclove, S. L. (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52(3), 333–343. [Google Scholar]
- Steinberg, A. M., Brymer, M. J., Kim, S., Briggs, E. C., Ippen, C. G., Ostrowski, S. A., … Pynoos, R. S. (2013). Psychometric properties of the UCLA PTSD reaction index: Part I. Journal of Traumatic Stress, 26(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Stoltenborgh, M., Bakermans-Kranenburg, M. J., & van IJzendoorn, M. H. (2013). The neglect of child neglect: A meta-analytic review of the prevalence of neglect. Social Psychiatry and Psychiatric Epidemiology, 48(3), 345–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt, J. K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18(4), 450–469. [Google Scholar]
- Warmingham, J. M., Handley, E. D., Rogosch, F. A., Manly, J. T., & Cicchetti, D. (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse & Neglect, 87, 28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2018). The ICD-11 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines [Online]. Geneva: Author. Retrieved from https://icd.who.int/ [Google Scholar]
- Widom, C. S. (1999). Posttraumatic stress disorder in abused and neglected children grown up. The American Journal of Psychiatry, 156(8), 1223–1229. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The present data were assessed in the course of a research project commissioned and funded by the government of Lower Austria. Therefore, data cannot be shared due to legal reasons.


