Abstract
Objective:
We examined the feasibility and explored the physical, psychological, relational, and biological effects of Mindfulness-Based Stress Reduction (MBSR), an 8-week standardized mindfulness program, involving older married couples (60 years or older) with metabolic syndrome (one or both partners had metabolic syndrome). We also explored gender differences.
Methods:
A pilot randomized controlled trial (RCT) compared MBSR to a Wait List Control (WLC) arm at baseline, post-intervention, and 3-month follow-up clinic visits. Twenty-two spouses (11 couples) self-reported stress, physical and mental functioning, mindfulness, and relationship satisfaction at each time point. Fasting glucose, cholesterol, triglycerides, blood pressure, weight, and waist circumference were measured. MBSR couples answered questions about partner influences on participation, adherence, and practice at the post-intervention visit.
Results:
In terms of adherence to MBSR sessions, four of the six couples attended all 10 sessions; one couple attended 7; and one wife attended 6 and her husband attended 5 sessions. In terms of efficacy, there were no significant intervention effects; however, there were significant gender by intervention effects. Pre- to post-intervention, MBSR wives displayed greater increases in physical functioning (β = 1.18, t(36) = 3.17, p = .003) and relationship satisfaction (β = .72, t(36) = 2.81, p = .007) than WLC wives. Effects for husbands were not significant. Qualitatively, participants reported encouragement and increased relationship closeness.
Conclusions:
Engaging in MBSR as a couple to address symptoms of metabolic syndrome was well-received and feasible. Preliminary effects suggest more benefits for wives than husbands in terms of physical functioning and relational well-being.
Keywords: MBSR, couples, metabolic syndrome
Metabolic syndrome is a common multifactorial disorder that increases risk for a myriad of diseases including type 2 diabetes, cerebrovascular, and cardiovascular disease (Alexander, Landsman, Teutsch, & Haffner, 2003). In the United States between 23% and 55% of older adults meet the criteria for metabolic syndrome, which entails having any three of the following: abdominal obesity, hypertriglyceridemia, low high-density lipoprotein (HDL) cholesterol, high blood pressure, and high fasting glucose (Alexander et al., 2003; Denys, Cankurtaran, Janssens, & Petrovic, 2009). The primary treatment of metabolic syndrome as recommended by the National Heart, Lung, and Blood Institute is to make lifestyle changes, such as maintaining a heart-healthy diet, aiming for a healthy weight, managing stress, doing regular physical activity, and quitting smoking. However, few preventive behavioral interventions specifically target metabolic syndrome, and those that do predominantly focus on diet and exercise (Dunkley et al., 2012). Less is known about the effects of interventions that focus on stress reduction, despite significant positive associations between stress and each metabolic syndrome biomarker (Matthews & Kuller, 2002). Although there have been a few studies that have examined the stress buffering effects of yoga on metabolic syndrome indicators (Chu, Gotink, Yeh, Goldie, & Hunink, 2016), no studies to our knowledge have examined mindfulness interventions, which may be particularly helpful in reducing stress and attenuating the detrimental impact of metabolic syndrome among older adults (Geiger et al., 2016).
There are several reasons why mindfulness interventions may have beneficial effects on metabolic syndrome biomarkers. First, in terms of the brain, it is proposed that mindfulness trains two stress resilience pathways: (1) increasing activity and functional connectivity in stress regulatory regions of the prefrontal cortex and (2) decreasing activity and functional connectivity in regions gating the brain’s stress alarm system (Creswell & Lindsay, 2014). Stress resilience in the brain is expected to modulate the peripheral sympathetic nervous system and hypothalamic-pituitary-adrenal responses to exogenous stressors (Creswell & Lindsay, 2014). Second, it is proposed that mindfulness interventions affect stress-related health behaviors that are likely to affect biomarkers (Li, Howard, Garland, McGovern, & Lazar, 2017). Third, the following psychological mechanisms have been theorized to explain why mindfulness affects biomarkers: enhanced emotion regulation, self-awareness, attentional control, self-reported mindfulness skills, and decentering (Creswell, Lindsay, Villalba, & Chin, 2019). Another mechanism, which has received less research attention, is improved relationship quality. Mindfulness interventions have been shown to have positive consequences for close relationships (Carson, Carson, Gil, & Baucom, 2004, 2007), and a large literature shows that the heightened quality of one’s close relationships has important implications for one’s mental and physical health (Holt-Lunstad, Smith, & Layton, 2010).
It is important to consider the health effects of mindfulness interventions in the context of close relationships, especially in older adulthood. Seventy percent of older men and nearly 50% of older women are married (Aging, 2018), and spouses have significant influences on older adults’ health (Hoppmann, Michalowski, & Gerstorf, 2016). This means that lifestyle interventions should address not only older individuals’ health behaviors and psychological well-being but also that of their spouses. Indeed, prior research findings suggest that lifestyle interventions which target couples may be more effective than lifestyle interventions which target individuals. Evidence for the superiority of couple-oriented interventions over individual-oriented interventions for married couples can be found in the literature on weight control (Black, Gleser, & Kooyers, 1990; Brownell, Heckerman, Westlake, Hayes, & Monti, 1978). For example, a seminal behavioral weight loss intervention study featured three conditions: one condition in which couples attended meetings together and were trained in supportive techniques, another condition in which the spouse was willing to be involved and cooperative but did not attend any meetings or training, and a third condition in which the spouse refused to participate (Brownell et al., 1978). The results of this study revealed that participants in the shared couple involvement condition lost significantly more weight than participants in the other two conditions. Further, in the absence of shared attendance to meetings and training, participants with cooperative spouses fared no better than participants with partners who refused to cooperate. Since then, multiple meta-analyses have shown that couple-oriented interventions tend to have greater effects on health outcomes than individual-oriented psychosocial interventions for older adults with a variety of health conditions (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). These effects may be due to better adherence to recommended health behaviors among people who participate with a spouse. This may also be due to increases in individual and relational well-being among couples.
A couple-oriented mindfulness approach may be particularly helpful for older married couples dealing with chronic conditions. A few pilot studies have explored participation of couples in Mindfulness Based Stress Reduction (MBSR) for cancer patients and their spouses and for frail elders and their caregivers. One study of 21 cancer patients and their spouses found that participating in MBSR together led to significant reductions for both cancer patients and spouses in mood disturbance (McNair, 1992) and physical symptoms of stress (Carlson & Thomas, 2007) and increases in mindfulness (Birnie, Garland, & Carlson, 2010; Carlson & Brown, 2005). Although there have been promising couple-oriented mindfulness intervention studies, no study to our knowledge has examined whether unmodified, certified instructor-led MBSR is feasible for older couples who are at heightened risk for poor health. Neither have there been studies examining the impact of MBSR on older adult spouses’ physical, psychological, relational, and biological outcomes.
The aims of this study were to explore the feasibility and preliminary effectiveness of MBSR for reducing stress, improving metabolic syndrome biomarkers, and increasing mindfulness, physical and mental functioning, and relationship satisfaction for older married couples in which one or both partners had metabolic syndrome. First, to examine feasibility, we monitored and described (a) recruitment, (b) adherence, and (c) missing data for the MBSR intervention. Second, to explore effectiveness, we compared couples in the MBSR condition with couples in a waitlist control condition (WLC) on all outcomes over time, testing the primary hypothesis that spouses would have larger decreases in perceived stress and biomarkers including systolic and diastolic blood pressure (SBP, DBP), triglycerides, fasting glucose, and waist circumference and larger increases in HDL cholesterol, from baseline to post intervention and at the three months follow-up. Our secondary hypothesis was that couples in the MBSR group compared to WLC would have greater increases in mindfulness, relationship satisfaction, and physical and mental functioning and decreases in perceived stress. Finally, we hypothesized that there would be gender differences in intervention effects, with wives displaying greater changes than husbands in all outcome variables. This exploratory hypothesis about gender differences is based on findings showing that women are more affected by MBSR in terms of reduction in negative emotions and increases in mindfulness (Chen, Comerford, Shinnick, & Ziedonis, 2010; Rojiani, Santoyo, Rahrig, Roth, & Britton, 2017) and that women report more stress than men in their everyday lives (Altemus, Sarvaiya, & Neill Epperson, 2014). Third, we explored couple dynamics in the MBSR experience quantitatively assessing partner encouragement for participation and adherence. We also asked participants to describe in writing how participating with their partner influenced their experience with the MBSR intervention, and we describe these responses qualitatively.
Method
Participants
Eleven couples (22 individuals) were recruited from the greater New Haven, CT area via the Yale Center for Clinical Investigation’s Help Us Discover database, the Joint Data Analytics Team (JDAT), a unified Yale School of Medicine and Yale-New Haven Health Systems team, community flyers, and patient referrals from doctor’s offices in the area. Eligibility criteria were as follows. First, at least one partner in the couple had to have metabolic syndrome, which is determined by meeting three of the five diagnostic criteria (abdominal obesity, hypertension, hypertriglyceridemia, low HDL cholesterol, and high fasting glucose levels). Following the American Heart Association guidelines, abdominal obesity was defined as a waist circumference of more than 40 inches for men and 35 inches for women. Elevated blood pressure was 130/85 mm Hg or higher or taking blood pressure medication. Hypertriglyceridemia was 150 mg/dL or more or taking medicine for high triglycerides. Low HDL cholesterol was less than 40 mg/dL for men and less than 50 mg/dL for women or taking medication for low HDL cholesterol. High fasting glucose was 100 mg/dL or more or taking medicine for high blood glucose. Second, both couple members had to be over 60 years old, cohabiting with their partner, married or in a romantic relationship with their partner, and speak English. Couples in which either partner took psychiatric medications or practiced mind-body therapies more than once weekly were excluded. There were no restrictions regarding whether couples were heterosexual or same sex couples to be eligible for the study.
See Table 1 for participant characteristics. All couples reported having at least one partner with metabolic syndrome during the screening process, and we confirmed criteria with baseline biological and vital assessments. This revealed that in the MBSR group there were three couples in which both partners had metabolic syndrome, one couple in which only the husband had metabolic syndrome, one couple in which only the wife had metabolic syndrome, and one couple in which both partners had high waist circumference only. In the WLC group there was one couple in which both had metabolic syndrome, one couple in which only the husband met criteria, two couples which only the wife met criteria, and one couple in which both had high blood pressure only. All couples were included in our analysis.
Table 1.
Participant characteristics
| MBSR (n=12) | Waitlist (n=10) | |||
|---|---|---|---|---|
| Husbands (n=6) | Wives (n=6) | Husbands (n=5) | Wives (n=5) | |
| Age (Mean; SD) | 67 (3.35) | 67 (4.69) | 70 (7.05) | 67 (6.91) |
| At least one child together? | 2 couples | 4 couples | ||
| Ethnicity (n) | 5 White | 6 White | 4 White | 5 White |
| 1 Black | 1 Asian | |||
| Education (n) | 1 Associate’s | 1 Bachelor’s | 4 Bachelor’s | 2 Some college |
| 2 Bachelor’s | 4 Some grad school | 1 Some grad school | 1 Associate’s | |
| 1 Some grad school | 1 Some grad school | |||
| 2 Professional | 1 Professional | 1 Professional | ||
| Employment (n) | 1 Full time | 1 Part time | 2 Part time | 2 Full time |
| 3 Part time | 5 Retired | 3 Retired | 2 Part time | |
| 2 Retired | 1 Unemployed | |||
| Income (n) | 1 $40,000–49,000 | 1 $30,000–39,000 | ||
| 2 $60,000–69,000 | 1 $70,000–79,000 | |||
| 2 $70,000–79,000 | 3 >$100,000 | |||
| 1 >$100,000 | ||||
| Self-reported metabolic syndrome criteria during screening | Both: 3 | Both: 1 | ||
| Husband only: 2 | Husband only: 2 | |||
| Wife only: 1 | Wife only: 2 | |||
| Met metabolic syndrome criteria using baseline assessments | Both: 3 | Both: 1 | ||
| Husband only: 1 | Husband only: 1 | |||
| Wife only: 1 | Wife only: 2 | |||
| Neither: 1 (both partners had only high waist circumference) | Neither: 1 (both partners had only high blood pressure) | |||
Procedures
Informed consent was obtained from all individual participants included in the study. Couples participated in a baseline visit during which blood was drawn, height, weight, waist circumference, and blood pressure were measured, and questionnaires were completed to assess demographics, contextual factors, and baseline outcomes. Couples were then randomized to the MBSR (n=6) or the wait list control condition (n=5) by having the interviewer pick a card with a treatment condition on it out of an envelope of 11 cards.
The MBSR group completed the standardized program as taught at the Center for Mindfulness in Medicine, Health Care and Society (CFM) at the University of Massachusetts Medical School (Kabat-Zinn, 2013). This protocol consists of 8-weekly 2.5-hour sessions, homework consisting of 45–60 minutes of mindfulness practices six days per week, and a full-day (7.5 hours) retreat. Participants attended weekly group sessions at the first author’s lab in New Haven, CT. Sessions were taught by an experienced certified MBSR instructor (Anne Dutton, MA, LCSW). Each weekly session featured instructor-led mindfulness practices followed by a discussion of the participants’ experience and its application to participants’ everyday life. Formal practices included in the program were mindful eating, body scan, seated meditation, mindful movement and hatha yoga, and walking meditation. Informal mindfulness practices (mindfulness of daily activities) were also assigned as homework. In addition, participants were guided in bringing awareness to pleasant and unpleasant events, stress reactivity patterns and interpersonal stress. While the MBSR curriculum was not substantially altered from its validated form, to account for the simultaneous participation of couple members in the MBSR program, Ms. Dutton provided suggestions to participants about how each practice and assignment could be done in a way that acknowledged the partner’s presence. For example, participants were encouraged to do the daily formal homework practices together and to reflect in class on this experience.
Measures
Feasibility outcomes included 1) the percent of couples who screened versus enrolled, 2) the number of MBSR sessions the couple attended as recorded by the interventionist, and 3) the total minutes of home MBSR practice as reported by participants in their daily record.
Biomarkers of metabolic syndrome were assessed at baseline, post-intervention, and at the 3-month follow-up. Blood was drawn to assess triglycerides, HDL and LDL cholesterol, and fasting glucose levels. Abdominal obesity was measured according to waist circumference as per WHO protocol (2011), and systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using an automated CARESCAPE V100 cuff (GE Healthcare).
Perceived stress was measured at baseline, post-intervention, and at the 3-month follow-up using the Perceived Stress Scale (PSS-10). Participants rate how often they have had various feelings including being “overwhelmed” or “not in control of their life” in situations over the last month (Cohen, Kamarck, & Mermelstein, 1983). The Cronbach’s alpha was 0.85 across participants and time points.
Self-reported health was measured at baseline, post-intervention, and 3 months using the Short Form Health Survey (SF-12) (Ware Jr & Sherbourne, 1992). The SF-12 is a combination of items from other validated measures, many for older adults, which creates a representation of overall health. Participants are asked to think about their health over the past 4 weeks. Two subscales are calculated from the SF-12: the mental component summary and the physical component summary.
Mindfulness skills were measured at baseline, post-intervention, and 3 months using the Kentucky Inventory of Mindfulness Skills (KIMS) (Baer, Smith, & Allen, 2004), a well-validated, 39-item questionnaire that measures four dimensions of mindfulness: observing, describing, acting with awareness, and accepting without judgment. The four subscales exhibit strong expected correlations with other measures of emotional intelligence and awareness, psychological symptoms, and personality. The Cronbach’s alpha was 0.88.
Relationship satisfaction was assessed at baseline, post-intervention, and 3 months using the seven-item Relationship Assessment Scale (RAS) (Hendrick, 1988). Respondents use a five-point Likert scale (low to high) to answer questions such as “How well does your partner meet your needs?”, “How satisfied are you with your relationship”, and “How much do you love your partner?” The Cronbach’s alpha was 0.88.
Participants in the MBSR condition also answered the following questions at the post-intervention clinic visit only: (1) How was your partner involved in your decision to first participate in the intervention? (response options: encouraged you, discouraged you, or neither); (2) How was your partner involved in your decision to continue with each class? (same response options as first question); and (3) Describe how participating with your partner influenced your experience with the intervention (response: open-ended).
Data Analysis
To test the main hypotheses, changes in primary physical, psychological, relational, and biological outcomes as a function of time (i.e., baseline v. post-intervention v. follow-up), and study condition (i.e., MBSR v. Waitlist) were modeled using maximum likelihood linear mixed models on SAS/STAT 13.1 (PROC MIXED). Three-level mixed models were used where sampling occasions (level 1) were nested within individuals (level 2), and individuals were nested within dyads (level 3). Both individuals-level and dyad-level intercepts were modeled as random effects using identity matrices. Time was dummy coded and entered as a level 1 fixed effect. Given that study condition varied at the level of the dyad, study condition was dummy coded and entered as a level 3 fixed effect. Post-tests (i.e., tests contrasting intercept values or simple slopes) were conducted when omnibus tests (determining the presence of an interaction) were significant. Post-tests were significant under Bonferroni correction unless otherwise noted in the result section. For fixed effects, standardized β coefficients were computed to estimate effect size (Lorah, 2018).
The main effect of gender was examined across sampling occasion and study condition to assess global gender differences in primary outcomes of interest. Additionally, the interaction of study condition by time by biological gender was tested for all primary outcomes.
Results
Feasibility outcomes
Participant enrollment and random assignment.
Forty-six individuals responded to the study flyers and email announcements. Fourteen individuals met eligibility criteria but indicated they could not participate in the MBSR sessions which were scheduled on weekday afternoons. The majority of potential participants had work schedules that conflicted with the MBSR sessions. Other potential participants had conflicting regular appointments or were away on vacation during the late winter/early spring when the intervention occurred. The remaining 20 potential participants did not meet the eligibility criteria. In the end, 11 couples were assigned randomly to the two conditions. Thus, 24 percent of couples who were screened enrolled in the study.
Adherence to MBSR.
Four couples attended all 10 sessions (the 8 classes, the one orientation, and the one retreat day). One couple attended 7 sessions. One wife attended 6 sessions, and her husband attended 5 sessions. See Tables 2 and 3 for participants’ adherence to home practice. On average, wives did 17 (SD= 12.5) more formal practice sessions (e.g. supine yoga) and 2 (SD= 27.1) less informal practice sessions (e.g. mindful eating) than husbands did over the 8 weeks.
Table 2.
MBSR formal home practice exercises over the 8 weeks
| # Guided body scans | # Guided supine yoga | # Guided standing yoga | # Guided seated AOB | # Self-guided seated AOB | # Other selfguided practice | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Couple | wife | husband | wife | husband | wife | husband | wife | husband | wife | husband | wife | husband | wife | husband |
| 1 | 21 | 20 | 8 | 1 | 4 | 8 | 5 | 3 | 22 | 20 | 8 | 0 | 68 | 52 |
| 2 | 27 | 24 | 4 | 1 | 4 | 3 | 7 | 7 | 14 | 7 | 0 | 0 | 56 | 42 |
| 6 | 20 | 16 | 3 | 3 | 4 | 1 | 10 | 2 | 25 | 11 | 7 | 2 | 69 | 35 |
| 8 | 19 | 24 | 5 | 7 | 6 | 5 | 12 | 14 | 22 | 15 | 5 | 4 | 69 | 69 |
| 9 | 19 | 20 | 9 | 8 | 7 | 4 | 10 | 5 | 31 | 27 | 0 | 2 | 76 | 66 |
| 10 | 28 | 23 | 13 | 9 | 12 | 5 | 11 | 14 | 37 | 21 | 6 | 6 | 107 | 78 |
| Total | 134 | 127 | 42 | 29 | 27 | 27 | 65 | 45 | 151 | 101 | 26 | 14 | 445 | 342 |
Notes. All guide exercises are ~45 minutes long. AOB= awareness of breath
Table 3.
MBSR informal home practice exercises over the 8 weeks
| # Mindful eating | # Mindful walking | # Mindfulness of routine | # Other informal | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| couple | wife | husband | wife | husband | wife | husband | wife | husband | wife | husband |
| 1 | 6 | 7 | 2 | 26 | 39 | 41 | 1 | 27* | 48 | 101 |
| 2 | 4 | 5 | 7 | 7 | 28 | 14 | 0 | 0 | 39 | 26 |
| 6 | 31 | 16 | 24 | 1 | 38 | 51 | 0 | 0 | 93 | 68 |
| 8 | 3 | 8 | 11 | 9 | 43 | 31 | 0 | 0 | 57 | 48 |
| 9 | 13 | 12 | 16 | 27 | 48 | 41 | 0 | 0 | 77 | 80 |
| 10 | 12 | 14 | 9 | 2 | 16 | 27 | 2 | 0 | 39 | 43 |
| Total | 69 | 62 | 69 | 72 | 212 | 205 | 3 | 27 | 353 | 366 |
Note.
This participant indicated the activity was Tai Chi.
Missing outcome data.
All 11 couples (MBSR and WLC) completed all baseline clinic visit surveys, vital assessments, and blood draws. All WLC couples completed post-intervention and three-month clinic visit surveys, vital assessments, and blood draws, except one WLC wife could not have her blood drawn at the three-month visit due to difficulty finding her vein. Five MBSR couples completed the post-intervention and 3-month follow-up clinic surveys, vitals, and blood draws. One MBSR couple completed the surveys through the mail but did not have blood drawn or vitals taken post-intervention and at 3 months.
Preliminary Analysis
Treatment of outliers.
Outliers (± 3 SDs from the mean) were detected for LDL cholesterol (N = 1), triglycerides (N = 1), and glucose (N = 1), systolic blood pressure (N = 1), and weight (N = 1). In contrast, no outliers were detected for HDL cholesterol, physical functioning, mental functioning, mindfulness, perceived stress, or relationship satisfaction. Excluding outliers did not influence the outcome of analyses reported below, so they were retained in final analyses.
Changes in biological and vital outcomes over time.
Across study conditions, time was associated with systolic blood pressure (SBP; F(2,38) = 4.72, p = .014) and diastolic blood pressure (DBP; F(2,38) = 9.03, p > .001) such that SBP and DBP decreased from baseline follow up (SBP: β = −.71, t(38) = 3.03, p = .004; DBP: β = −.81, t(38) = 4.22, p < .001). Weight was associated with time across study conditions (F(2,38) = 4.22, p = .022) such that weight decreased from baseline to follow up (β = −.07, t(38) = 2.88, p = .006). Across conditions, time did not predict waist circumference (F(2,38) = .27, p = .76), HDL (F(2,37) = 2.43, p = .10) and LDL cholesterol (F(2,37) = 0.01, p = .99), triglycerides (F(2,37) = 1.10, p = .34), or glucose (F(2,37) = 1.17, p = .32).
Changes in physical, psychological, and relational outcomes over time.
Across conditions, time was associated with perceived stress (F(2,42) = 7.35, p = .001), such that perceived stress levels significantly decreased from baseline to post-intervention (β = −.59, t(42) = 3.34, p = .001), and from baseline to follow-up (β = −.59, t(42) = 3.29, p = .002). Mindfulness was associated with time (F(2,42) = 9.59, p < .001), such that mindfulness significantly increased from baseline to post-intervention (β = .63, t(42) = 4.02, p < .001) and from baseline to follow-up (β = .55, t(42) = 3.52, p = .001). Relationship satisfaction was associated with time (F(2,42) = 17.18, p < .001), such that relationship satisfaction significantly increased from baseline to post-intervention (β = .43, t(42) = 4.26, p < .001), and from baseline to follow-up (β = .57, t(42) = 5.62, p < .001). Time did not predict physical or mental functioning (F(2,42) = .91, p = .40; F(2,42) = .52, p = .59) across conditions.
Intervention by Time Effects
Biological and vital outcomes.
There were no significant intervention effects predicting biomarkers. The interaction of study conditions and time was non-significant when predicting LDL (F(2,35) = .27, p = .76), HDL (F(2,35) = .11, p = .89) , triglycerides (F(2,35) = .05, p = .94), glucose (F(2,35) = .04, p = .95), SBP (F(2,36) = 0.11, p = .89), DBP (F(2,36) = 1.76, p = .18), weight (F(2,36) = 1.13, p = .33), and waist circumference (F(2,36) = .24, p = .78).
Psychological, physical, and relational outcomes.
The interaction of time and study condition was not significant when predicting perceived stress (F(2,40) = 1.31, p = .28), physical functioning (F(2,40) = 2.48, p = .096), relationship satisfaction (F(2,40) = 1.04, p = .36), or mindfulness (F(2,40) = 2.17, p = .127). However, the interaction of time and study condition was significant when predicting mental functioning (F(2,40) = 4.54, p = .016). Post-tests revealed that couples assigned to the MBSR condition showed a larger decrease in mental functioning from post-intervention to the 3 month follow-up than couples assigned to the waitlist condition (β = −1.14, t(40) = 3.01, p = .004) and a non-significant change in mental functioning from baseline to post-intervention (β = .63, t(40) = 1.66, p=.10).
Gender by Intervention by Time Effects
Main effects of gender.
Across study conditions and sampling occasions, women displayed greater physical functioning (β = .55, t(10) = 2.18, p = .053), worse mental functioning (β = −.63, t(10) = 1.94, p = .080), greater LDL cholesterol (β = .43, t(9) = 2.21, p = .054), lower DBP (β = −.55, t(10) = 2.45, p = .034), lower weight (β = −.76, t(10) = 1.93, p = .082), and smaller waist circumference (β = −.73, t(10) = 2.16, p = .055) than men. However, men and women did not significantly differ (across study condition and sampling occasion) with regards to perceived stress, mindfulness, relationship satisfaction, HDL cholesterol, triglycerides, glucose, and SBP (all ps > .10).
Gender X condition X time.
The interaction of gender x condition x time was significant when predicting physical functioning (F(2,36) = 3.27, p = .049). As shown in Figure 1, follow up tests revealed that wives assigned to MBSR training displayed significantly greater increases in physical functioning from baseline to post-intervention and from baseline to follow-up relative to wives assigned to the WLC (β = 1.18, t(36) = 3.17, p = .003, and β = 1.09, t(36) = 2.95, p = .005, respectively). In contrast, husbands assigned to MBSR training and WLC displayed similar baseline to post-intervention differences and baseline to follow-up differences in physical functioning (β = −.07, t(36) = .20, p = .83, and β = .05, t(36) = .14, p = .89, respectively).
Figure 1.
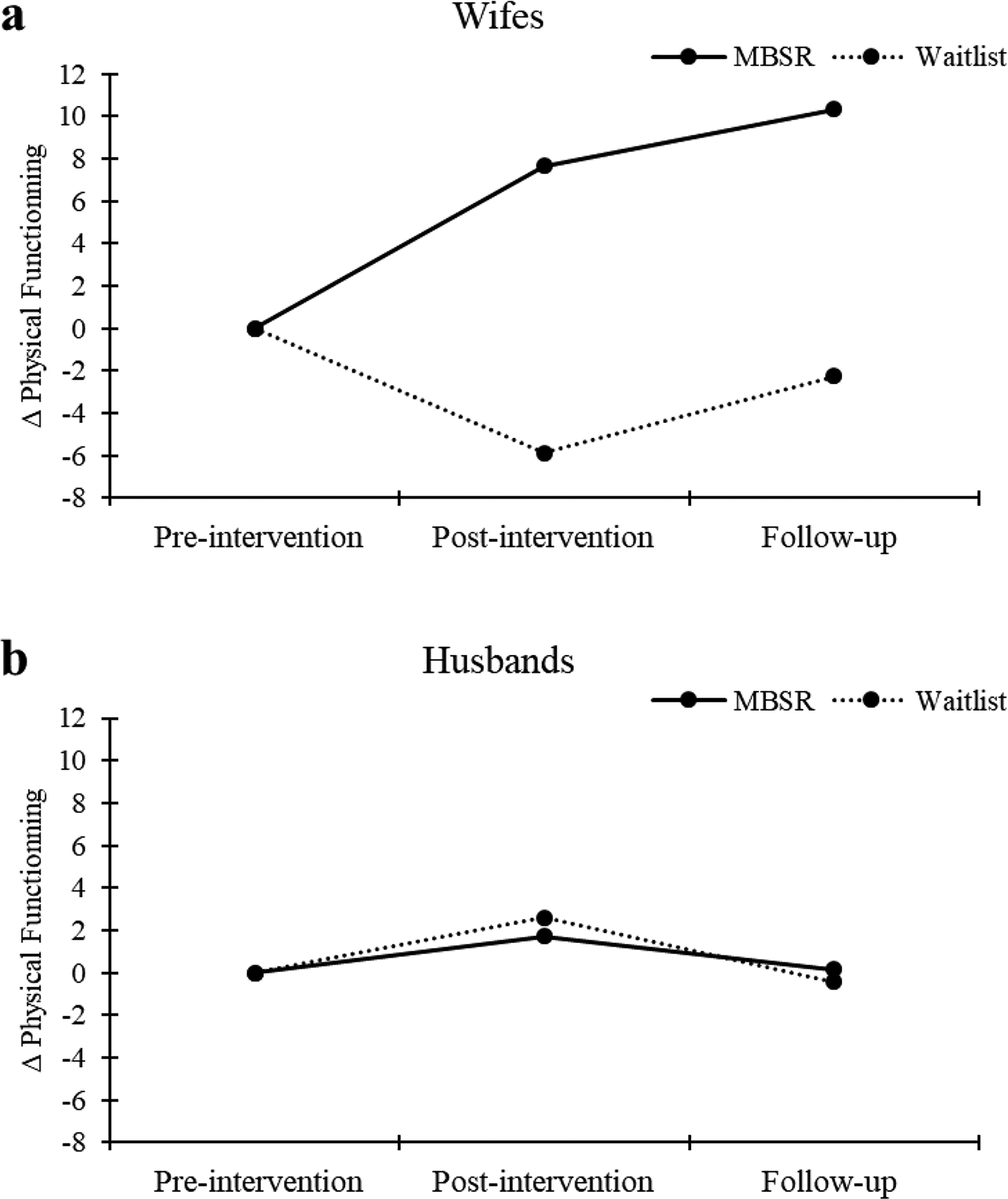
Self-reported physical functioning as function of gender, time and study conditions. Panel a illustrates the effect of study condition and time for wives. Panel b illustrates the effects of time and study condition for husbands. Means shown are unadjusted marginal means. Error bars correspond to standard error of mean estimates.
The interaction of gender x study condition x time was significant when predicting relationship satisfaction (F(2,36) = 4.45, p = .018). As shown in Figure 2, wives assigned to MBSR show a significantly larger increases in relationship satisfaction from baseline to post-intervention and from baseline to follow-up than wives assigned to the WLC (β = .72, t(36) = 2.81, p = .007, and β = .66, t(36) = 2.57, p = .014 [non-significant under Bonferroni adjustment], respectively). In contrast, husbands assigned to MBSR or the WLC displayed similar baseline to post-intervention and baseline to follow-up increases in relationship satisfaction (β = −.32, t(36) = 1.27, p = .21, and β = −.10, t(36) = .39, p = .69, respectively).
Figure 2.
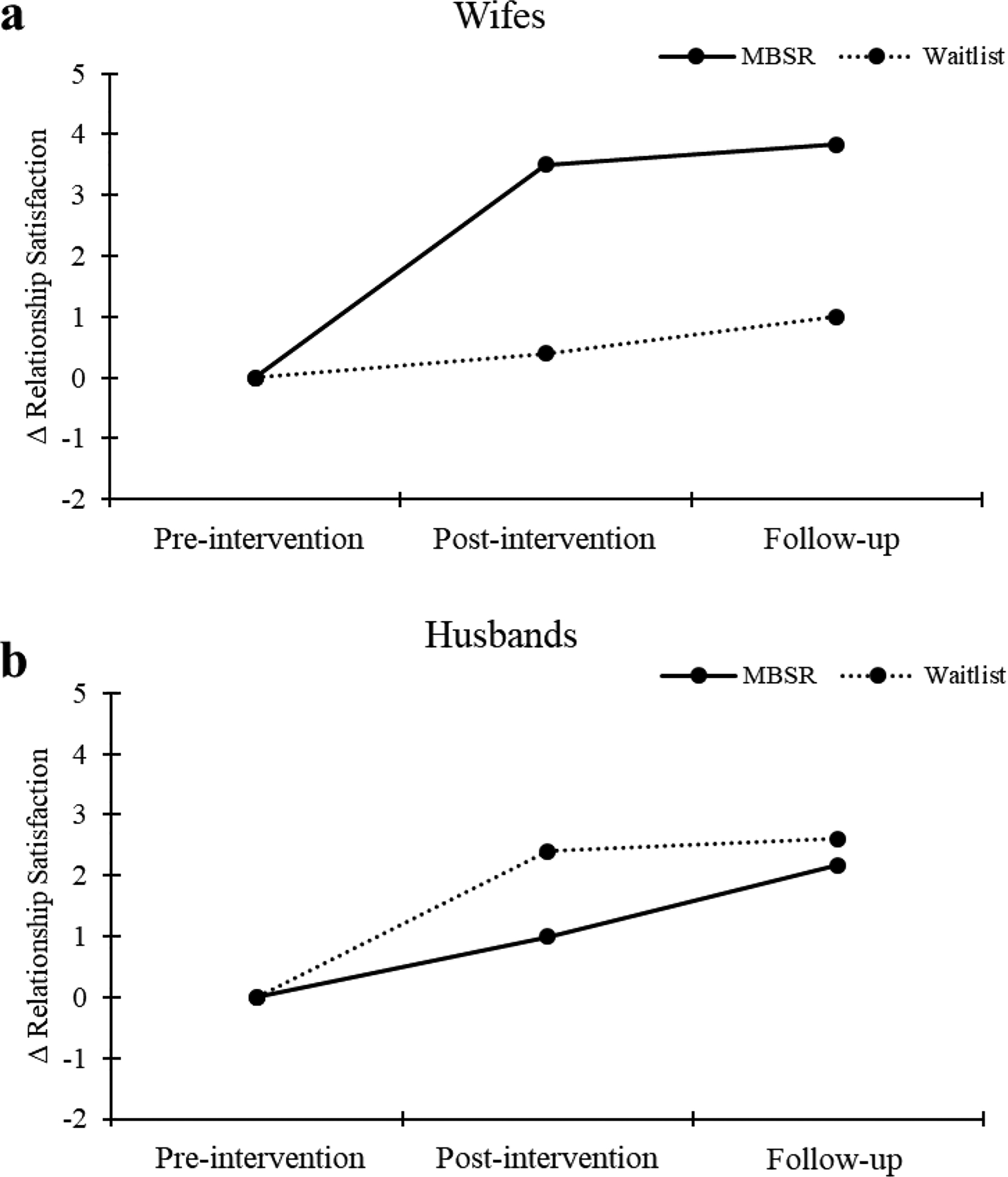
Relationship satisfaction as functioning as function of gender, time and study conditions. Panel a illustrates the effect of study condition and time for wives. Panel b illustrates the effects of time and study condition for husbands. Means shown are unadjusted marginal means. Error bars correspond to standard error of mean estimates.
Gender did not moderate the effect of study conditions and time on mental functioning, trait mindfulness, LDL cholesterol, triglycerides, glucose, SBP, DBP, weight, and waist circumference (all ps > .10). The interaction of gender x study condition x time was marginally significant when predicting perceived stress (F(2,36) = 2.59, p = .089). Wives assigned to MBSR showed a significantly larger decrease in perceived stress from baseline to post-intervention (β = −.95, t(36) = 2.22, p = .032 [non-significant under Bonferroni adjustment]) but not from baseline to follow-up (β = .22, t(36) = .51, p = .61) relative to wives assigned to the WLC. In contrast, husbands assigned to MBSR or the WLC displayed similar baseline to post-intervention and baseline to follow-up change in perceived stress (β = .06, t(36) = .15, p = .88, and β = −.07, t(36) = .18, p = .85, respectively). The interaction of gender x study condition x time was marginally significant when predicting HDL cholesterol (F(2,31) = 3.06, p = .061). Husbands assigned to MBSR displayed a larger decrease in HDL from baseline to post-treatment (β = −.87, t(36) = 2.03, p = .051 [non-significant under Bonferroni adjustment]) relative to husbands assigned to WLC. No other contrasts were significant.
Examining Couple Dynamics
Encouragement about participation and adherence.
As shown in Table 4, all husbands reported that their wives encouraged them to participate in the study, whereas, two wives felt that their partner neither encouraged or discouraged them, and one wife reported their husband discouraged them. This was the couple who discontinued the study part way through the MBSR sessions. In terms of continuing engaging in the MBSR classes, four husbands reported their wives encouraged them to continue and two husbands reported their wives neither encouraged them or discouraged them. Three wives reported their husbands encouraged them to continue engaging in MBSR, and three wives reported their husbands neither encouraged or discouraged them.
Table 4.
Partner influences on the study and MBSR intervention
| Participant | Partner’s involvement in decision to participate? | Partner’s involvement in continuing with class? | How did participating with your partner influence your experience with the intervention? |
|---|---|---|---|
| 1 H | encouraged you | neither | It was good to share the experiences and discoveries instead of trying to report on a solitary experience. We each learned something about each other as well as about ourselves. Also, each encouraged the other to do the “homework”. Gave us something to talk about in what otherwise routine lives. |
| 1 W | encouraged you | encouraged you | A great help. We were able to discuss and compare thoughts and experiences. We could encourage each other to do the homework when tired or distracted and forgive each other when we skipped or shortened the exercise on a particular day. We shared ideas and thoughts. I think for all the participating couples, it brought us closer to our partners. |
| 2H | encouraged you | encouraged you | Not applicable. Did not continue. |
| 2W | discouraged you | neither | Accountability. |
| 6 H | encouraged you | encouraged you | Participation together was a blessing and a joy. We were able to re-enforce each other’s experiences and help each other with learning and implementing the various practices. |
| 6 W | encouraged you | encouraged you | It was GREAT!! We grew even closer and felt stronger than ever in our relationship. I found myself being more “tuned in” to him and we grew from discussing our reactions/experiences with the different exercises/practices- most of which we did together. |
| 8 H | encouraged you | encouraged you | It was good. Couldn’t have done it without her. |
| 8 W | neither | neither | I often was distracted from what we were doing because I could hear my husband having difficulties with something (yoga, etc.). I also found myself constantly worrying about if he was getting tired of the study or not. However, it made it easier to do home practices when he would say “Let’s do the body scan now” or the like. |
| 9 H | encouraged you | neither | Made going to the class and doing the “homework” easier and more fun. |
| 9 W | encouraged you | encouraged you | It was fun to do the yoga and meditation with husband. Even a bit romantic. We even had a few laughs doing them together! |
| 10 H | encouraged you | encouraged you | It made sticking with the required schedule easier because we were able to do it together and if I felt like skipping some of the at home participation, she would make sure that I do what I had to. |
| 10 W | neither | neither | Really enjoyed doing it together. I felt closer to him doing the body scan and seated meditation together…and the yoga. I was so pleased to see that he likes doing yoga. We both plan to continue it…although it does sometimes cut into my gym time. |
Note. W= wife, H= husband
How participating together influenced their experience with the intervention.
Also shown in Table 4, four wives and two husbands reported feeling closer to their partners during their participation. Five husbands and two wives noted that participating with their partner helped them stay engaged with the MBSR practices. Whereas most of the participants reported benefits, one wife reported feeling distracted from her practice because of worrying that her husband was having difficulty with his practice or not wanting to participate in the study. In this couple, the husband had significant health challenges beyond metabolic syndrome.
Discussion
With this pilot randomized controlled trial we found that MBSR for older adult couples was feasible and well-accepted. We did not find that MBSR had significant main effects on any of the physical, psychological, relational, or biological outcomes compared to the wait list control; however, we did find significant gender differences in intervention effects. Specifically, we found that wives benefited more in terms of physical functioning and relationship satisfaction than husbands in response to MBSR. This is consistent with past research findings that women are more likely to experience psychological benefits in response to MBSR than are men (Chen et al., 2010). Our finding that wives engaged in more home practice than husbands may also account for the larger benefits of MBSR on physical functioning and relationship satisfaction for wives.
The present study also provides important information about how participating as a couple can impact the experience of MBSR. Qualitatively, all participants described feeling very positive about the shared experience. Spouses explained that they learned about each other, encouraged each other, were able to reinforce each other’s mindfulness experiences, grew closer to one another, and even felt more intimate when doing the mindfulness practices together. Despite that both husbands and wives enjoyed the share participation in this study, husbands reported receiving more encouragement from their partner than did the wives in engaging in the practice. This is consistent with a large literature showing that wives are responsible for health behavior work in marriage (Reczek, Gebhardt-Kram, Kissling, & Umberson, 2018; Umberson, 1992).
We did not find that MBSR had significant effects on any of the biomarkers for metabolic syndrome, and there were no trends indicating beneficial biological effects. These non-significant findings should be interpreted with caution as this was a pilot investigation that was primarily conducted to test feasibility and was not powered to fully examine efficacy. Of interest, the downward trend in cardiovascular and metabolic outcomes (i.e., SBP, DBP, and weight) observed across conditions may imply that couples in both conditions sought this study because they were willing to take action to improve their health. To the extent that this yielded more active Wait-listed participants, this may have diminished the magnitude of contrast between MBSR and the Wait-list condition.
Although we did find a significant intervention effect on mental functioning from baseline to three months, indicating that mental functioning became worse from post-intervention to the 3-month follow-up, this finding was not hypothesized and should also be interpreted with caution. However, in relation to this finding, at the 3-month follow-up interviews, multiple couples in the MBSR condition noted that they had difficulty continuing their home practice, and they missed the sense of community with the other couples. Several couples said they wished they could meet with the other couples regularly, but they had difficulty organizing and scheduling the group themselves. Future studies should consider providing guidance in how MBSR practice can be organized and continued by the participants themselves.
Limitations and Future Research
A limitation of this study is that MBSR for couples was compared to a wait list condition rather than an active comparison condition. We also did not have a comparison of older adults with metabolic syndrome participating as individuals to be able to examine the unique effects of participating as a couple. In addition, the conditions were not equally matched on the prevalence of metabolic syndrome within the couples. Importantly this study was a pilot study and had a small sample. We cannot make conclusions about the efficacy of MBSR to change each of the outcomes examined in this study. Rather, we provide important preliminary information about the feasibility of MBSR, some areas of promise in terms of how it affects couples’ outcomes, and procedural lessons learned for future, larger RCTs of MBSR for couples with metabolic syndrome. Of note, one of the important lessons we learned from recruitment for this study is that it is important to offer evening or weekend class times that accommodate couples who work full-time hours. We did not have the staff availability to offer these hours in the present study, which limited the amount and types of couples that could enroll.
Despite the exploratory nature, this study has some important strengths. It is the first study to use the full MBSR course by a certified MBSR instructor with older couples. It is also one of the few studies following participants over time to examine whether changes in outcomes were maintained or changed three months later. We measured physical, psychological, relational, and biological outcomes to get a more holistic picture of how older couples may benefit from MBSR. We also collected detailed information about home practice and couple dynamics.
Next steps will be to examine efficacy of MBSR for couples with metabolic syndrome in a fully powered RCT. It may also be useful to examine whether there are differences in the utility of engaging in MBSR as a couple for younger adults and for same sex romantic couples, friends, or adult child- older parent pairs. The homogeneity of the sample being in long-term, heterosexual, marriages meant that participants had common experiences with other couples. Furthermore, within couples the participants knew their partners very well and had no new surprises to share in their relationships. Couples reported that before the intervention, they had difficulty finding new things to talk about in their day to day lives, so sharing a new experience like MBSR and having the opportunity to talk about their emotions with each other in front of a group was novel and exciting.
In conclusion, engaging in MBSR as an older adult couple is feasible and that there are positive effects on the physical health and relational well-being of wives. Additionally, this study underscores the importance of examining interventions which may help prevent chronic diseases in older adulthood. Quite often, interventions for older adults focus on participants who already have chronic conditions when the damage has already been done. We hope our findings will inspire other researchers to consider targeting older adult pairs in addition to individuals to protect health over the lifespan.
Acknowledgements:
Funding for this study was provided by Yale’s Claude D. Pepper Older Americans Independence Center (P30 AG021342). We would like to thank Kathleen Williams for assistance with recruitment and data collection.
This study was approved by Yale University’s ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their informed consent prior to their inclusion in the study. None of the authors have a financial relationship with the organization that sponsored the research. The authors declare that they have no conflict of interest.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Data Availability Statement: Data from this study will be made available upon request from the first author.
References
- 2017 Older Americans Profile. Retrieved December, 10, 2019 from the Adminstration for Community Living website: https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf [Google Scholar]
- Alexander CM, Landsman PB, Teutsch SM, & Haffner SM (2003). NCEP-defined Metabolic Syndrome, Diabetes, and prevalence of Coronary Heart Disease among NHANES III participants age 50 years and older. Diabetes, 52 (5), 1210–1214. [DOI] [PubMed] [Google Scholar]
- Altemus M, Sarvaiya N, & Neill Epperson C (2014). Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology, 35(3), 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, & Allen KB (2004). Assessment of mindfulness by self-report the Kentucky inventory of mindfulness skills. Assessment, 11(3), 191–206. [DOI] [PubMed] [Google Scholar]
- Birnie K, Garland SN, & Carlson LE (2010). Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psycho-Oncology, 19(9), 1004–1009. [DOI] [PubMed] [Google Scholar]
- Black DR, Gleser LJ, & Kooyers KJ (1990). A meta-analytic evaluation of couples weight-loss programs. Health Psychology, 9(3), 330–347. [DOI] [PubMed] [Google Scholar]
- Brownell KD, Heckerman CL, Westlake RJ, Hayes SC, & Monti PM (1978). The effect of couples training and partner co-operativeness in the behavioral treatment of obesity. Behaviour Research and Therapy, 16(5), 323–333. [DOI] [PubMed] [Google Scholar]
- Carlson LE, & Brown KW (2005). Validation of the Mindful Attention Awareness Scale in a cancer population. Journal of Psychosomatic Research, 58(1), 29–33. [DOI] [PubMed] [Google Scholar]
- Carlson LE, & Thomas BC (2007). Development of the Calgary symptoms of stress inventory (C-SOSI). International Journal of Behavioral Medicine, 14(4), 249–256. [DOI] [PubMed] [Google Scholar]
- Carson JW, Carson KM, Gil KM, & Baucom DH (2004). Mindfulness-based relationship enhancement. Behavior Therapy, 35(3), 471–494. [Google Scholar]
- Carson JW, Carson KM, Gil KM, & Baucom DH (2007). Self-expansion as a mediator of relationship improvements in a mindfulness intervention. Journal of Marital and Family Therapy, 33(4), 517–528. [DOI] [PubMed] [Google Scholar]
- Chen KW, Comerford A, Shinnick P, & Ziedonis DM (2010). Introducing qigong meditation into residential addiction treatment: a pilot study where gender makes a difference. The Journal of Alternative and Complementary Medicine, 16(8), 875–882. [DOI] [PubMed] [Google Scholar]
- Chu P, Gotink RA, Yeh GY, Goldie SJ, & Hunink MM (2016). The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. European Journal of Preventive Cardiology, 23(3), 291–307. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396. [PubMed] [Google Scholar]
- Creswell, & Lindsay EK (2014). How does mindfulness training affect health? A mindfulness stress buffering account. Current Directions in Psychological Science, 23(6), 401–407. [Google Scholar]
- Creswell, Lindsay EK, Villalba DK, & Chin B (2019). Mindfulness training and physical health: Mechanisms and outcomes. Psychosomatic Medicine, 81 (3), 224–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denys K, Cankurtaran M, Janssens W, & Petrovic M (2009). Metabolic Syndrome in the elderly: An overview of the evidence. Acta Clinica Belgica, 64(1), 23–34. [DOI] [PubMed] [Google Scholar]
- Dunkley A, Charles K, Gray L, Camosso-Stefinovic J, Davies M, & Khunti K (2012). Effectiveness of interventions for reducing diabetes and cardiovascular disease risk in people with metabolic syndrome: Systematic review and mixed treatment comparison meta-analysis. Diabetes, Obesity and Metabolism, 14(7), 616–625. [DOI] [PubMed] [Google Scholar]
- Geiger PJ, Boggero IA, Brake CA, Caldera CA, Combs HL, Peters JR, & Baer RA (2016). Mindfulness-based interventions for older adults: a review of the effects on physical and emotional well-being. Mindfulness, 7(2), 296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrick SS (1988). A generic measure of relationship satisfaction. Journal of Marriage and the Family, 50 (1), 93–98. [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Medicine, 7(7), e1000316.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppmann CA, Michalowski V, & Gerstorf D (2016). Spousal interrelationships in health across adulthood: health behaviors and everyday stress as potential underlying mechanisms In Bookwala J(Ed.), Couple Relationships in the Middle and Late Years: Their Nature, Complexity, and Role in Health and Illness. Washington, D. C.: American Psychological Association. [Google Scholar]
- Kabat-Zinn J (2013). Full catastrophe living, revised edition: how to cope with stress, pain and illness using mindfulness meditation: Hachette UK. [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, & Saghafi EM (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40(3), 325–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, & Kuller LH (2002). The relationship between psychological risk attributes and the metabolic syndrome in healthy women: antecedent or consequence? Metabolism, 51(12), 1573–1577. [DOI] [PubMed] [Google Scholar]
- McNair DM (1992). Profile of mood states. Educational and Industrial Testing Service. [Google Scholar]
- Reczek C, Gebhardt-Kram L, Kissling A, & Umberson D (2018). Healthcare Work in Marriage: How Gay, Lesbian, and Heterosexual Spouses Encourage and Coerce Medical Care. Journal of Health and Social Behavior, 59(4), 554–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojiani R, Santoyo JF, Rahrig H, Roth HD, & Britton WB (2017). Women benefit more than men in response to college-based meditation training. Frontiers in Psychology, 8, 551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine, 34(8), 907–917. [DOI] [PubMed] [Google Scholar]
- Ware JE Jr, & Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care, 473–483. [PubMed] [Google Scholar]


