Abstract
Context
A persistently elevated thyroid stimulating hormone (TSH) level is a common clinical problem in primary hypothyroidism patients treated with levothyroxine (LT4). “Pseudomalabsorption”, which is characterized by poor adherence,should be considered in cases of refractory hypothyroidism after excluding other causes, such as malabsorption.
Objective
We reviewed the features of the patients with persistently elevated TSH despite high-dose LT4 therapy.
Design
Symptom evaluation, medications, comorbid diseases and physical examination features of five patients who applied to our outpatient clinic between 2016-2019 and diagnosed with LT4 pseudomalabsorption were retrospectively analyzed.
Subjects and methods
The LT4 loading test was performed with an oral dose of 1,000 µg LT4. Demographic parameters, BMI, thyroid function tests, laboratory parameters for malabsorption were recorded.
Results
We observed at least two-fold increase of free thyroxine levels during the test, which was considered pseudomalabsorption. Euthyroidism was achieved in two patients by increasing the LT4 dosage and in one patient with a change in the preparation. TSH decreased significantly after being informed about compliance in one patient. Another one was given LT4 twice weekly, but TSH remained elevated because of nonadherence.
Conclusion
The LT4 loading/absorption test is a valuable tool to confirm the diagnosis of pseudomalabsorption. Informing patients, changing the preparation, increasing the dose, supervised intake of daily/weekly LT4 forms are treatment options for managing these cases.
Keywords: levothyroxine, pseudomalabsorption, refractory hypothyroidism
INTRODUCTION
A persistently elevated thyroid stimulating hormone (TSH) level is a common clinical problem in outpatient clinics treating primary hypothyroidism patients receiving levothyroxine (LT4) replacement. Recommended daily doses of LT4 replacement (1.6–1.8 µg/kg) are generally sufficient to provide euthyroid status in most hypothyroid patients (1). Although some patients require a high dose of LT4 to maintain a normal TSH level, a persistent elevation of serum TSH level under high-dose LT4 treatment needs further clinical investigation. Refractory hypothyroidism is defined as the presence of biochemical signs(serum TSH>4.5 mU/L, 6 weeks after the dose increase) or clinical hypothyroid symptoms of a LT4 dose>1.9 µg/kg/day (2). Poor compliance and persistence is the most common cause of failed LT4 therapy (3). Intestinal absorption problems or increased demand for thyroxine may cause a high-dose LT4 requirement. Common causes of LT4 malabsorption are gastrointestinal diseases, cirrhosis, nephrotic syndrome, pancreatic insufficiency, gastrointestinal malabsorptive surgical procedures, congestive heart failure, drug and dietary interactions or pregnancy (4-6).
“Pseudomalabsorption” is a contemporary term used for a very high dose requirement for LT4 in hypothyroid patients when a malabsorption cause is ruled out (7). Limited data indicate that this entity is a factitious disorder characterized by patient denial, poor adherence to therapy and is associated with psychiatric problems (8, 9). Pseudomalabsorption is a diagnosis of exclusion; therefore, a detailed examination of all causes leading to malabsorption is needed. LT4 loading test may be helpful for the diagnosis. Here we report clinical and laboratory characteristics of five consequent cases of persistently elevated serum TSH under high-dose LT4 treatment diagnosed as pseudomalabsorption.
PATIENTS AND METHODS
This study was performed with the approval of the local ethics committee and in accordance with the Helsinki declaration and written informed consent was obtained from all patients. We present the clinical and biochemical characteristics of five patients admitted to Marmara University Pendik Research Hospital Endocrinology Clinic between 2016 and 2019 that were diagnosed with LT4 pseudomalabsorption. A detailed evaluation of symptoms (may be associated with absorption disorder, such as nausea, abdominal pain, stomach cramps, diarrhea), drugs, comorbid diseases and a physical examination were performed. Gastrointestinal, liver, and pancreatic diseases were excluded through clinical and laboratory investigations. No history of previous gastrointestinal surgery, congestive heart failure, or pregnancy was observed. A detailed history of adjunctive medicine was taken and supplement use and dietary factors were ruled out. Demographic parameters (age and gender), height, weight, body mass index (calculated as: weight/height2), thyroid function tests [TSH, free thyroxine (FT4), free triiodothyronine (FT3)], thyroid auto-antibodies [thyroid peroxidase antibody (TPOAb), thyroglobulin antibody (TgAb)], laboratory parameters to exclude malabsorption [alanine aminotransferase, creatinine, calcium, albumin, hemoglobin, ferritin, vitamin B12, 25-OH Vitamin D, folic acid, anti-gliadine antibodies, anti-tissue transglutamase antibodies, anti-endomysial antibodies, parasite and Helicobacter pylori antigen (HpAg) analysis in feces] were recorded. TSH, FT3, FT4, TPOAb, TgAb, ferritin, folic acid, Vitamin B12 and 25-OH Vitamin D parameters were automatically studied by paramagnetic particle chemiluminescence immunoassay method in serum samples (DxI800, Beckman Coulter, USA). Calcium levels in serum were studied with Schwarzenbach using the o-cresolphthalein-complexsone method, albumin levels using the bromcresol green method bichromatically, creatinine levels with the kinetic Jaffe method, and ALT levels in UV wavelength kinetically using the method recommended by IFCC (AU 5800, Beckman Coulter, USA). The complete blood count was performed on EDTA samples on an automatic blood count analyzer (LH700, Beckman Coulter, USA). Celiac antibodies [Serum anti-tissue transglutaminase, anti-gliadin and anti-endomysial antibodies (IgA and IgG)] were measured by a human recombinant enzyme-linked immunosorbant assay (ELISA) method, using the commercial kits (INOVA Diagnostics Inc., San Diego, California, USA). Stool samples for parasite analysis were examined microscopically by using native lugol and formalin-ether concentration technique, and for HpAg were investigated by monoclonal antibodies with one-step colored immunochromatography technique (ImmunoCard STAT HpSA, Meridian Diagnostics Inc., Cincinnati, Ohio, USA). It was observed that albumin, creatinine, calcium, ALT and celiac antibodies levels were normal in all patients, and no parasites were detected on stool examination in any patient.
The Morisky 8-item medication adherence questionnaire (MMAS-8) consisting of 8 questions was applied to the patients to evaluate adherence to treatment. Highly adherent patients had an MMAS-8 score of 8, medium adherence 6–7, and low adherence <6 (10). The LT4 loading test was conducted with an oral dose of 1,000 µg LT4. The patient was observed by a trained nurse throughout the test. Blood samples were collected before and 1, 2, 3, and 4 hours following administration, and FT4 and TSH were measured. Pseudomalabsorption was diagnosed by revealing a two/three-fold or at least 0.4 ng/dL increase in FT4 level after 2 hours compared to baseline values (3,11,12,13).
Case 1
A 26-year-old female underwent 10 mCi radioactive iodine ablation (RAI) 2 years after being diagnosed with Graves’disease in 2016. LT4 replacement therapy was started after RAI ablation. She complained of muscle pain and decreased proximal muscle strength under LT4 (100 mcg/day) treatment;high TSH (61mU/L) and creatine kinase levels (>1,000 U) were observed. As electromyography revealed hypothyroidism-associated myopathy, LT4 dose was increased to 330 µg/day gradually. Although she stated that she used her medication properly, TSH remained elevated (53.3 mU/L). No concomitant medication or comorbid disease was detected. The H.pylori antigen HpAg test was positive in feces, eradication treatment was provided (Table 2). Iron deficiency anemia was treated with ferrous sulfate, and vitamin D deficiency was treated with cholecalciferol. Other biochemical investigations for malabsorption were unremarkable (Table 2). During LT4 loading test FT4 level increased almost three-fold at first hour with a maximal rise of 0.51 ng/dL and TSH suppressed (Figs 1A, B). A psychiatric evaluation was normal. TSH had decreased to 14 mU/L in two months under 500 µg/day LT4 daily.
Figure 1 A.
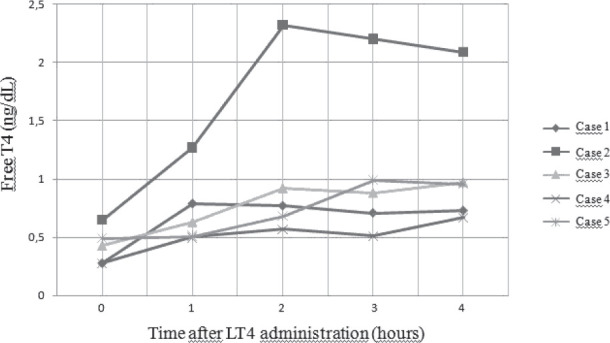
Four-hour levothyroxine loading test results.
Figure 1 B.
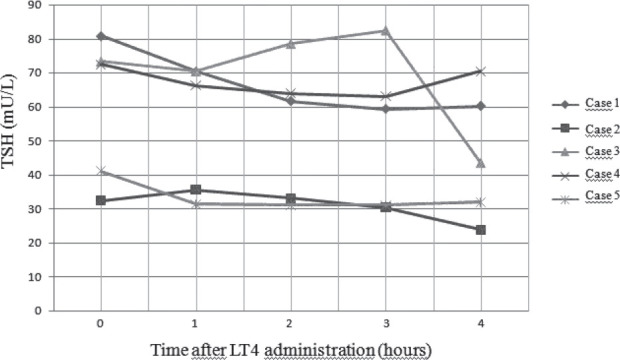
Four-hour levothyroxine loading test results.
Table 1.
Characteristics of hypothyroid patients persistant elevated TSH under high dose LT4 treatment
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age /gender | 26/female | 41/female | 57/female | 42/female | 53/female |
| BMI (kg/m2) | 28.9 | 22.9 | 31.8 | 28.3 | 67.6 |
| Etiology of hypothyroidism | Radioactive iodine ablation | Thyroidectomy | Radioactive iodine ablation | Thyroidectomy | Autoimmune thyroiditis |
| Duration of hypothyroidism (years) | 1 | 7 | 1 | 9 | 17 |
| Daily dose of LT4 (µg) | 500 | 600 | 700 | 1000 | 1000 |
| Dose of LT4 per kg per day (µg/kg) |
7.17 | 10.22 | 8.6 | 16.15 | 6.16 |
| Thyroid ultrasonography | atrophic gland 8×7×15 mm on the right, 7×6×13 mm on the left lobe No nodule was observed |
residual thyroid tissue of 10×12×16 mm on the right, 10×9×17 mm on the left No nodule was observed |
- | Thyroid gland was not monitored | The right lobe was 16×13×15 mm, the left lobe was 10×9 ×11 mm, the isthmus was 5 mm No nodule was observed |
| Diseases interfering LT4 absorption | Hp infection |
- | Hp infection |
Hp infection |
- |
| Other comorbidities | - | - | T2DM, obesity, arrhythmia, essential hypertension, asthma, panic disorder | - | T2DM, morbid obesity, hypercholesterolaemia, essential hypertension, asthma |
| Medications interference with LT4 | - | Calcium carbonate/cholecalciferol | Lansoprazole, Lactulose | Esomeprazole | Orlistat |
| Other medications | - | Vitamin D3 oral | Metformin, rivaroxaban, sotalol, verapamil hydrochloride, candesartan/hydrochlorothiazide, amlodipine, desloratadine/montelukast, trazodone, citalopram | - | metformin, exenatide, insulin glargine U300, atorvastatin, perindopril, ipratropium bromide/salbutamol |
| LT4 compliance according to MMAS-8 | High | Medium | High | Medium | Medium |
LT4:L-thyroxine; BMI: Body Mass Index; Hp:Helicobacter pylori; T2DM:Type 2 diabetes mellitus; MMAS-8:Morisky 8-item medication adherence questionnaire.
Table 2.
Laboratory findings in initial evaluation
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Normal range | |
|---|---|---|---|---|---|---|
| TSH (mU/L) At admittance |
22.68 | 36.25 | 43.62 | 63.11 | 13.95 | 0.34-5.60 |
| TSH (mU/L) 6 months before admittance |
73.7 | 39.62 | 93.8 | 72.37 | 9.36 | |
| TSH (mU/L) 12 months before admittance |
53.31 | 34.7 | 90.7 | 59.47 | 45.31 | |
| Free T4 (ng/dL) At admittance |
1.04 | 0.57 | 0.97 | 0.51 | 1.0 | 0.61-1.12 |
| Free T4 (ng/dL) 6 months before admittance |
0.34 | 0.52 | 0.25 | 0.28 | 0.88 | |
| Free T4 (ng/dL) 12 months before admittance |
0.25 | 0.5 | 0.25 | 0.31 | 0.26 | |
| Free T3 (ng/L) At admittance |
2.78 | 2.99 | 2.7 | 2.62 | 3.4 | 2.6-4.37 |
| Free T3 (ng/L) 6 months before admittance |
2.56 | 2.94 | 1.52 | 1.88 | 2.75 | |
| Free T3 (ng/L) 12 months before admittance |
1.95 | 2.57 | 1.79 | 2.74 | 2.63 | |
| TPOAb | (+) | (-) | (+) | (-) | (+) | |
| TgAb | (-) | (-) | (-) | (-) | (-) | |
| Hemoglobin (g/dL) | 11.1 | 13.7 | 12 | 8.4 | 11.4 | 12-17 |
| Ferritin (µg/L) | 5.3 | 12.5 | 17.5 | 2 | 6.6 | 12-263 |
| Vitamin B12 (ng/L) | 283 | 181 | 187 | 326 | 137 | 180-914 |
| Folic acid (µg/L) | 5.76 | 9.08 | 4.25 | 8.68 | 9.92 | 2.2-17.5 |
| 25-OH-Vitamin D (µg/L) | 5.47 | 13.03 | 19.75 | 23.23 | 30.13 | 30-100 |
| Helicobacter pylori antigen in feces | (+)* | (-) | (-) | (+)* | (-) |
TSH:Thyroid stimulating hormone; TPOAb:Thyroid peroxidase antibody; TgAb:Thyroglobulin antibody; ALT:Alanine aminotransferase, (-):Negative (+):Positive. *Eradicated.
Case 2
A 41-year-old female patient developed hypothyroidism after a subtotal thyroidectomy for multinodular goiter in 2012. She was referred to our clinic for persistant high TSH level (51.3 mU/L) under high dose of LT4 (400 µg/day). She reported adherence to all medications and LT4 pill intake was separate from oral intake of a calcium carbonate/cholecalciferol (1,000 mg/880 IU) tablet. She complained of fatigue, dry skin, muscle pain, and depressed mood. Biochemical malabsorption tests were normal (Table 2). The LT4 loading test revealed a significant increase in FT4 with a maximal rise of 1.67 ng/dL (Fig. 1A) and a decrease in TSH (Fig. 1B). The patient was informed about the adherence and LT4 dosage increased to 500 µg daily. TSH decreased to 4 mU/L during the 6 months follow-up.
Case 3
A 57-year-old female applied to our clinic due to her hypothyroidism that was diagnosed in May 2019 after 3 consequent RAI treatments of toxic adenoma. Her TSH level (93.6 mU/L) remained elevated despite gradual increasing LT4 dosage. She was under 700 µg/day LT4 at admission in November 2019. She had type 2 diabetes mellitus (T2DM), essential hypertension, asthma,panic disorder,and arrhythmia. She was using 2×1,000 mg metformin, 15 mg rivaroxaban, 80 mg sotalol, 40 mg verapamil hydrochloride, 16/12.5 mg candesartan/hydrochlorothiazide, 5 mg amlodipine, 5/10 mg desloratadine/montelukast, 50 mg trazodone, 20 mg citalopram, 30 mg lansoprazole and intermittent lactulose (Table 1). H.pylori was detected on a gastroscopic biopsy and eradication treatment was completed before presenting at our clinic (Table 2). She stated compliance of LT4 treatment appropriately. She complained of fatigue, weight gain, constipation, joint pain, and slow movements. No significant features were observed in terms of malabsorption on biochemical tests (Table 2). The LT4 loading test showed that FT4 level increased two 2.3-fold elevation of FT4 with a maximal rise of 0.54 ng/dL and TSH level decreased (Figs 1A, B), so LT4 malabsorption was ruled out. She was discharged with 100 µg L-thyroxine® tablets and euthyroidism was reached after 2 months.
Case 4
A 42-year-old female underwent a total thyroidectomy in 2010 for Graves’ disease. LT4 100 µg daily treatment was started and dosage was increased gradually to 600 µg to provide euthyroidism. However, TSH remained elevated for 3 years under the high dose of LT4. Under 1000 mg/day LT4 treatment her TSH was elevated (62 mU/L). Severe symptoms of hypothyroidism, such as weakness, effort dyspnea, constipation, dry skin, muscle pain, depressed mood, and hair loss were observed. A physical examination was normal. Ferritin and hemoglobin levels normalized within 3 months, after treating with ferrous sulfate. The H.pylori antigen HpAg was positive in the feces and eradication treatment was provided. Other tests for absorption were within normal limits (Table 2). A significant increase in FT4 with a maximal rise of 0.4ng/dL (Fig. 1A) and a decrease in TSH (Fig. 1B) was detected on the LT4 loading test (Fig. 1A). After the test, she was informed about the importance of adherence but she strictly refused the noncompliance. The LT4 preparation used by the patient was discontinued and Levotiron® 2×600 µg twice a week divided dose was started. FT4 was within normal limits after 3 months, while TSH decreased to 30 mU/L. However, TSH was found to be elevated (74 mU/L) at the last visit.
Case 5
A 53-year-old female was diagnosed with Hashimoto’s thyroiditis for 15 years. The patient was referred to our clinic 6 years ago was using 300 µg LT4. LT4 dose was increased gradually to 1,000 µg, but elevated TSH level (21.68 mU/L) persisted. Her medical history included type 2 diabetes mellitus (T2DM), morbid obesity, hypercholesterolemia, essential hypertension,and asthma. Her medications consisted of 2×1000 mg metformin, 2×5 µg exenatide, 40U insulin glargine U300, 3×120 mg Orlistat, 20 mg atorvastatin, 10 mg perindopril, and 0.5/2.5 mg ipratropium bromide/salbutamol (Table 1). The patient was given Orlistat for 6 months but the drug was discontinued due to a lack of weight loss. Iron deficiency anemia and vitamin B12 deficiency were detected (Table 2) and oral iron and vitamin B12 treatments were started. Ferritin, hemoglobin, and vitamin B12 levels normalized with replacement. She had symptoms of constipation, muscle pain, periorbital edema, and depression. During absorption test, FT4 level had increased significantly with a maximal rise of 0.5 ng/dL during LT4 absorption test (Fig. 1A) and TSH suppressed (Fig. 1B). Psychiatry consultation revealed problems with medication adherence. TSH decreased 3.9 mU/L with 1,050 µg/day LT4 dosage. However, 15 mU/L TSH level was observed after 2 months of discharge according to LT4 incompliance.
DISCUSSION
Pseudomalabsorption is a rare reason leading to a high dose levothyroxine requirement and inadequate control in hypothyroid patients. Noncompliance, which is a factitious psychiatric problem, is the major issue that causes pseudomalabsorption (13). We present 5 cases of pseudomalabsorption, major clinical problems suggested to be associated with pseudomalabsorption were poor compliance and persistence of LT4 treatment.
The diagnosis of pseudomalabsorption depends on excluding gastrointestinal malabsorption (coeliac disease, lactose intolerance, intestinal infections, H. pylori infection,or gastrointestinal surgery), nephrotic syndrome, liver or pancreatic disease, heart disease, and pregnancy (5). Medications (most common are cholestyramine, colestipol, aluminum hydroxide-containing antacids, propranolol, laxatives, ferrous salts, calcium carbonate, lovastatin, phenytoin, carbamazepine, and rifampicin) and dietary elements (soybean, prunes, walnuts, and herbal remedies) interfere with the absorption of thyroid hormones (4,5,14-16).
Poor adherence to any medical therapy is a well-known treatment problem in chronic patients (17). Noncompliance to daily administration of LT4 is the most common reason for not responding to the appropriate dose of LT4 (18). “Pseudomalabsorption” due to intentional noncompliance as part of a psychiatric disorder should be considered as illustrated in the literature (11,14,16). This term applies when the patient does not regularly take the prescribed medication, although they claim compliance to treatment (4,16). In our patients with pseudomalabsorption, we found good and moderate levels of treatment compliance according to the MMAS-8 and this was consistent with the above definition. But we observed that when LT4 dosage increased and regularly used under observation TSH levels decreased. Incompliance seems to be the main reason in chronic term.
The T4 absorption/loading test with a 1,000 μg dose of LT4 is used to assess the presence of LT4 pseudomalabsorption vs. true malabsorption (16). Pseudomalabsorption is diagnosed by demonstrating a two-three fold increase FT4 level after 2 hours compared to the initial value (3,11,12). It is known that peak serum FT4 levels are reached within 2 hours after administration. This result can vary from patient-to-patient and with the degree of hypothyroidism (5). However, there is no gold standard for the LT4 absorption test, and various protocols have been advocated in the literature. The time commitment from a patient ranges from 2 hours to 5 days Test periods ranging from 2 hours to 5 days have been reported (18). We determined our loading test method by measuring FT4 and TSH in blood samples taken before and 1, 2, 3, and 4 hours after LT4 administration, and calculated the maximum FT4 increase. A recent study conducted by Ghosh et al. indicated that a rise of FT4 value of more than 0.4 ng/dL had a high sensitivity to exclude real malabsorption (13). In accordance with the literature, in our study during the tests the maximum FT4 levels were reached at different times and with maximal rises of ≥0.4 ng/dL by the patients. In our patients maximum levels were reached at 1, 2, 4, 4, 3 hours, respectively. We did not observe any short and long term side effects of a high dose LT4, concordant with literature.
After a diagnosis of pseudomalabsorption the next step is to exclude possible psychiatric disorders. Although depression is frequent, some patients exhibit true psychopathology. This psychiatric disorder, known as factitious disorder, is characterized by a fictitious history, exaggeration, fluctuating physical symptoms, lying and multiple hospital admissions (4,11). A conservative approach is important and avoiding a confrontation with a diagnosis of noncompliance may lead to a better outcome (19). A clear discussion with the patient about how existing symptoms can be attributed to a poor disease control due to irregular administration of vital drugs often leads to a better compliance and, consequently, better symptom control. In addition, as in our patient (Case 5), noncompliance with other treatments related to comorbidities can be observed. The presence of coexisting chronic disorders may have a negative effect on treatment adherence (20). Informing the patient about the effects of poor compliance occasionally improves compliance during the follow-up (11). It is also important that the patient to believe in the efficacy of the drug and encourage the treatment. It is beneficial to change the preparation in some patients, as in our cases.
Medical treatment strategies for pseudomalabsorption are parenteral infusion of LT4 (intravenous every 3–4 days or intramuscularly every week) or supervised oral ingestion daily, once a week, and twice a week (18). The long half-life of LT4 also facilitates the possibility of once-weekly dosing in patients with compliance issues. Once-or twice weekly oral administration of LT4 is safe and efficient and could be a better strategy for some patients. Twice-weekly administration rather than once-weekly has been chosen to reduce the likelihood of fluctuations in the FT4 level in the body (21). We also recommended twice weekly LT4 in one patient and achieved euthyroidism.
This study has some limitations as the group of patients is heterogeneous with regard to hypothyroidism etiology and comorbid diseases. Two of the patients were overweight, and the other two had a diagnosis of obesity and T2DM treated with metformin. Metformin can interfere with sodium-iodide symporter and partially impede the transmembrane T4 transport in the cells (22). In cases of obesity, T2DM, metformin therapy and chronic inflammation, tissue/intracellular hypothyroidism can be observed due to disturbances in transmembrane transport or in the LT4 conversion depending on a defect of tissue deiodinases (1). Besides, circulating idiotypic T4 antibodies can be found in autoimmune thyroid diseases (Case 1, 3, 5 with TPOAb positivitiy). All the mechanisms mentioned above may contribute to persistent hypothyroidism.
In conclusion, pseudomalabsorption needs to be considered in cases of failed oral LT4 therapy for hypothyroidism despite a high dose of LT4. The LT4 loading/absorption test is a valuable tool to exclude malabsorption of LT4 with no significant side effects. Supervised oral intake of LT4 daily/twice a week/once a week or intravenous/intramuscular form of LT4 are treatment options in cases of nonadherence or a psychiatric disorder.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, Cooper DS, Kim BW, Peeters RP, Rosenthal MS, Sawka AM, American Thyroid Association Task Force on Thyroid Hormone Replacement Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670–1751. doi: 10.1089/thy.2014.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centanni M, Benvenga S, Sachmechi I. Diagnosis and management of treatment-refractory hypothyroidism: an expert consensus report. J Endocrinol Invest. 2017;40:1289–1301. doi: 10.1007/s40618-017-0706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mandel SJ, Brent GA, Larsen PR. Levothyroxine therapy in patients with thyroid disease. Ann Intern Med. 1993;119:492–502. doi: 10.7326/0003-4819-119-6-199309150-00009. [DOI] [PubMed] [Google Scholar]
- 4.Lips DJ, van Reisen MT, Voigt V, Venekamp W. Diagnosis and treatment of levothyroxine pseudomalabsorption. Neth J Med. 2004;62:114–118. [PubMed] [Google Scholar]
- 5.Benvenga S, Bartolone L, Squadrito S, Lo Giudice F, Trimarchi F. Delayed intestinal absorption of levothyroxine. Thyroid. 1995;5:249–253. doi: 10.1089/thy.1995.5.249. [DOI] [PubMed] [Google Scholar]
- 6.Skelin M, Lucijanić T, Amidžić Klarić D, Rešić A, Bakula M, Liberati-Čizmek AM, Gharib H, Rahelić D. Factors Affecting Gastrointestinal Absorption of Levothyroxine: A Review. Clin Ther. 2017;39(2):378–403. doi: 10.1016/j.clinthera.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Wilder NV, Bravenboer B, Herremans S, Vanderbruggen N, Velkeniers B. Pseudomalabsorption of Levothyroxine:A Challenge for the Endocrinologist in the Treatment of Hypothyroidism. Eur Thyroid J. 2017;6:52–56. doi: 10.1159/000452489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160:1163–1168. doi: 10.1176/appi.ajp.160.6.1163. [DOI] [PubMed] [Google Scholar]
- 9.O’Shea B. Factitious disorders: the Baron’s legacy. Intern J Psychiatry Clin Pract. 2003;7:33–39. doi: 10.1080/13651500310001040. [DOI] [PubMed] [Google Scholar]
- 10.Vezzani S, Giannetta E, Altieri B, Barbonetti A, Bellastella G, Certo R, Cignarelli A, Cinti F, D’Andrea S, Di Dalmazi G, Frara S, Garelli S, Giuffrida G, Maiorino MI, Mele C, Mezza T, Pani MG, Samà MT, Satta C, Santi D. An Italian survey of compliance with major guidelines for l-thyroxine of primary hypothyroidism. Endocr Pract. 2018;24(5):419–428. doi: 10.4158/EP-2017-0159. [DOI] [PubMed] [Google Scholar]
- 11.Ain KB, Refetoff S, Fein HG, Weintraub BD. Pseudomalabsorption of levothyroxine. JAMA. 1991;266:2118–2120. [PubMed] [Google Scholar]
- 12.Jauk B, Mikosch P, Gallowitsch HJ, Kresnik E, Molnar M, Gomez I, Lind P. Unusual malabsorption of levothyroxine. Thyroid. 2000;10:93–95. doi: 10.1089/thy.2000.10.93. [DOI] [PubMed] [Google Scholar]
- 13.Ghosh S, Pramanik S, Biswas K, Bhattacharjee K, Sarkar R, Chowdhury S, Mukhopadhyay P. Levothyroxine Absorption Test to Differentiate Pseudomalabsorption from True Malabsorption. Eur Thyroid J. 2020;9:19–24. doi: 10.1159/000504218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eledrisi MS, Szymajda A, Alshanti M, Urban RJ. Noncompliance with medical treatment: pseudomalabsorption of levothyroxine. South Med J. 2001;94:833–836. [PubMed] [Google Scholar]
- 15.Morris JC. How do you approach the problem of TSH elevation in a patient on high-dose thyroid hormone replacement? Clin Endocrinol(Oxf) 2009;70:671–673. doi: 10.1111/j.1365-2265.2009.03536.x. [DOI] [PubMed] [Google Scholar]
- 16.Ogawa D, Otsuka F, Mimura U, Ueno A, Hashimoto H, Kishida M, Ogura T, Makino H. Pseudomalabsorption of levothyroxine: a case report. Endocr J. 2000;47:45–50. doi: 10.1507/endocrj.47.45. [DOI] [PubMed] [Google Scholar]
- 17.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research; a comprehensive review. J Clin Pharm Ther. 2001;26:331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 18.Butt MI, Gupta N, Tan HL, Waheed N. Clinical application of the levothyroxine absorption test in the diagnosis of pseudo-malabsorption. Am J Case Rep. 2014;2:253–255. [Google Scholar]
- 19.Haglund LA. Challenges in the treatment of factitious disorder: a case study. Arch PsychiatrNurs. 2009;23:53–64. doi: 10.1016/j.apnu.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Rdzak GM, Whitman LM, Inzucchi SE. Levothyroxine pseudo-malabsorption: testing and treatment in the outpatient setting. Ther Adv Endocrinol Metab. 2018;9(7):217–222. doi: 10.1177/2042018818771433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rangan S, Tahrani AA, Macleod AF, Moulik PK. Once weekly thyroxine treatment as a strategy to treat non-compliance. Postgrad Med J. 2007;83:e3. doi: 10.1136/pgmj.2007.060244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sloot YJE, Janssen MJR, Herwaarden AEV, Peeters RP, Netea-Maier RT, Smit JWA. The Influence of Energy Depletion by Metformin or Hypocaloric Diet on Thyroid Iodine Uptake in Healthy Volunteers: a Randomized Trial. Sci Rep. 2019;9(1):5396. doi: 10.1038/s41598-019-41997-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


