Abstract
Background:
There is significant global variation in the prevalence of DKA at diagnosis among youth with T1D. However, data for youth with T2D are limited, even in developed countries. We compared the prevalence of DKA at diagnosis among individuals with T1D and T2D from the SEARCH for Diabetes in Youth (SEARCH) and the Registry of people with diabetes in India with young age at onset (YDR) registries.
Methods:
We harmonized the SEARCH and YDR data sets to the structure and terminology in the OMOP Common Data Model (v5). Data used in the analysis were from youth with T1D and T2D diagnosed before 20 years and newly diagnosed between 2006 and 2012 in YDR and between 2009 and 2012 in SEARCH.
Results:
There were 5,366 U.S. youth (4,078 with T1D, 1,288 with T2D) and 2335 Indian youth (2108 with T1D, 227 with T2D). More than one third of T1D youth enrolled in SEARCH had DKA at diagnosis which was significantly higher than in YDR (35.3% vs 28.7%, p<0.0001). The burden of DKA in youth with T1D was significantly higher among younger age groups; this relationship was similar across registries (p=0.4). The prevalence of DKA among T2D in SEARCH and YDR were 5.5% and 6.6% respectively (p=0.4).
Conclusions:
There is significant burden of DKA at diagnosis with T1D among youth from U.S. and India, especially among the younger age groups. The reasons for this high prevalence are largely unknown but are critical to developing interventions to prevent DKA at diagnosis.
Keywords: Diabetic ketoacidois, Type 1 diabetes, Type 2 diabetes, SEARCH for Diabetes in Youth registry, YDR registry
Introduction
An absolute or relative lack of insulin and the consequent unrestricted flux of carbohydrate, amino acid and lipid nutrients to the blood results in diabetic ketoacidosis (DKA) in individuals with diabetes mellitus1. DKA is characterized by hyperglycemia, ketonemia and metabolic acidosis. DKA is a potentially life-threatening acute complication and a common presentation of type 1 diabetes (T1D) at diagnosis. Children and adolescents with type 2 diabetes (T2D) may present with some degree of metabolic de-compensation at diagnosis including ketosis, symptomatic hyperglycemia, and DKA2.
DKA and subsequent cerebral edema continues to be a leading cause of morbidity and mortality among children and adolescents with diabetes3,4. One in four survivors of DKA with cerebral edema also suffer from residual morbidity5. Previous reports suggest that DKA at diagnosis is associated with adverse neuro-cognitive outcomes and is an independent predictor of poor longer-term glycemic control among individuals with T1D6–8.
Recent studies suggests that DKA at diagnosis is more common in populations with lower socioeconomic status and a lower background prevalence of T1D9. There are limited data comparing the prevalence and trends in prevalence of DKA among children and adolescents with either T1D or T2D, even in countries with high prevalence of youth onset diabetes. An earlier analysis from the SEARCH registry reported a high but stable trend in the prevalence of DKA among T1D and a 10% yearly decline in DKA among United States (U.S.) youth with T2D at diagnosis10. However, such data are limited in countries like India, where the absolute number of individuals with youth onset diabetes is quite high. Exploring similarities or variations in DKA burden at diagnosis between countries could provide insights in to developing context specific preventive strategies to reduce mortality and morbidity associated with DKA at diagnosis of diabetes.
Methods
Data for this analysis were obtained from the collaborative partnership between SEARCH for Diabetes in Youth (SEARCH) registry in the U.S. and the Registry of People with Diabetes with Youth Age at Onset (YDR) in India.
SEARCH for Diabetes in Youth
The SEARCH registry is a multi-ethnic, population-based registry with five sites across the U.S. ascertaining physician-diagnosed non-gestational incident diabetes cases among individuals aged 19 years or younger. Detailed information about SEARCH is published elsewhere11,12. Each site conducts active surveillance under the Health Insurance Portability and Accountability Act (HIPAA) waivers of consent using networks of endocrinologists, healthcare providers, hospitals and community health centers, and clinical and administrative data systems along with electronic medical records. Cases are confirmed as valid after review of medical records or by the referring physician. All registered participants are asked to complete an Initial Participant Survey (IPS) and medical record abstractions are conducted within 6 months from diagnosis for all registered cases to validate the diagnosis of diabetes and obtain information about DKA. DKA at diagnosis with diabetes at was considered to be present if, in the context of hyperglycemia, any of the following were present: blood bicarbonate level <15 mmol/L, pH <7.25 (venous) or <7.30 (arterial or capillary), and/or a DKA diagnosis mentioned in the medical records10.
Registry of People with Diabetes with Youth Age at Onset (YDR)
The YDR registry is an observational multicenter clinic-based registry enlisting all cases of physician-diagnosed diabetes, diagnosed at the age of 25 years or younger, who were registered at a designated registry reporting center on or after January 1, 2000, residing within assigned geographical areas. More detailed information about YDR is published elsewhere11,12. Individuals are classified into various diabetes categories based on the assessment of the principal investigator at the reporting center using symptom-based clinical criteria agreed upon by the registry expert group prior to initiation of data collection in 2006. YDR data collection is coordinated by the ICMR through regional collaborating centers and their interacting reporting centers. All individuals have a proforma (registration and clinical extract) completed by the participant and physician to obtain information on socio-demographics, clinical profile, anthropometrics and laboratory measurements of the individual. Data from the period 2000–2006 were collected retrospectively in a structured format from medical records; while data from 2006–2012 were collected prospectively and completed by both the participant and physician at the time of registration, which is referred to here as the baseline visit. There are eight regional collaborating centers across India who provide cases to YDR. For this project, data from three of the eight regional collaborating centers (one in Chennai (Madras Diabetes Research Foundation) and two in New Delhi (All India Institute of Medical Sciences (AIIMS) and the University College of Medical Sciences, Delhi) were used. DKA information was obtained from self-report or documented DKA from medical records at the time of registration10. Since the average duration of diabetes at registration was 6.2 months for T1D and 7.0 months for T2D, DKA data was obtained within approximately 6 months from diagnosis.
Selected data from SEARCH and YDR were harmonized to the structure and terminology in the Observational Medical Outcomes Partnership (OMOP) Common Data Model (v5). We assigned common concept IDs for DKA and other variables in both registries. Uniform programs were run on the databases to generate the result tables. The analysis was conducted at each site without the physical transfer of data between sites. Hence, we were restricted from performing any multivariable adjusted analysis across the data sets. Additional details of data harmonization are provided in a previous article by Hockett et al. within this special edition.
Statistical Analysis
Data used in the analyses were from youth with T1D and T2D, aged less than 20 years and newly diagnosed between 2006 and 2012 in YDR and between 2009 and 2012 in SEARCH. The period prevalence of DKA at diagnosis (per 100 youth with type 1 or type 2 diabetes) was calculated as the proportion presenting with DKA at the time of diagnosis. The prevalence was also calculated by age group and gender. We compared the prevalence of DKA at diagnosis across registries using chi-square test. The linear trend in prevalence of DKA in both the registries was tested using chi square test for linear trend. All of the tests were 2-sided and a p-value of 0.05 was considered statistically significant.
Results
Characteristics of individuals with diabetes
Data from 5,366 SEARCH (4,078 with T1D, 1,288 with T2D) and 2,335 YDR (2,108 with T1D, 227 with T2D) youth were analyzed. The demographic characteristics of the study population in both SEARCH and YDR according to diabetes type are shown in Table 1. Both T1D and T2D individuals from YDR were older at diagnosis compared to SEARCH. The proportion of females with T2D was significantly higher in SEARCH. However, there was no difference in gender distribution between the registries for individuals with T1D.
Table 1:
Demographic characteristics of SEARCH (2009–2012) and YDR (2006–2012) youth by diabetes type.
| T1D | T2D | |||||
|---|---|---|---|---|---|---|
| SEARCH (2009–2012*) n=4,078 |
YDR (2006–2012*) n=2,108 |
p-value | SEARCH (2009–2012*) n=1,288 |
YDR (2006–2012*) n=227 |
p-value | |
| Age at diagnosis, mean ± SD | 10.0 ± 4.5 | 10.4 ± 5.0 | <0.001 | 14.8 ± 2.8 | 16.1 ± 2.8 | <0.001 |
| Age at diagnosis, n (%) | ||||||
| 0–4 yrs | 652 (16.0) | 332 (15.7) | <0.001 | 1 (<0.01) | 0 (0) | <0.001 |
| 5–9 yrs | 1,315 (32.2) | 646 (30.6) | 59 (4.6) | 10 (4.4) | ||
| 10–14 yrs | 1,482 (36.3) | 688 (32.6) | 595 (46.2) | 59 (26.0) | ||
| 15–19 yrs | 629 (15.4) | 442 (20.9) | 633 (49.1) | 158 (69.6) | ||
| Gender | ||||||
| Female, n (%) | 1,882 (46.1) | 993 (47.1) | 829 (64.3) | 111 (48.9) | ||
| Male, n (%) | 2,196 (53.9) | 1115 (52.9) | 0.3 | 459 (35.6) | 116 (51.1) | <0.001 |
year of diagnosis
Period Prevalence of DKA in SEARCH and YDR, by Diabetes Type
The prevalence of DKA at diagnosis by diabetes type and demographic characteristics are shown in the Table 2. More than one third of T1D youth enrolled in SEARCH had DKA at diagnosis which was significantly higher than YDR (overall 35.3% vs 28.7%, p<0.0001), in each age-group and among both boys and girls. The burden of DKA among individuals with T1D was significantly higher among younger age groups in both SEARCH and YDR and this relationship was similar across registries (p=0.4). For T2D, the numbers were much smaller; however, there were no statistically significant differences in the prevalence of DKA between SEARCH and YDR overall (5.5% vs 6.6%, p=0.4), by age-group or gender. None of the individuals with T2D diagnosed below 10 years had history of DKA at diagnosis.
Table 2.
Prevalence of DKA at diagnosis in SEARCH (2009–2012) and YDR (2006–2012) youth, by diabetes type.
| T1D | T2D | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SEARCH (2009–2012*) |
YDR (2006–2012*) |
p-value | SEARCH (2009–2012*) |
YDR (2006–2012*) |
p-value | |||||
| n | % | n | % | n | % | n | % | |||
| Crude Prevalence (per 100) | 4,078 | 35.3 | 2,108 | 28.7 | <0.0001 | 1,288 | 5.5 | 227 | 6.6 | 0.4 |
| Prevalence by age at diagnosis | ||||||||||
| 0–4 yrs^ | 652 | 43.7 | 332 | 36.7 | <0.0001 | - | - | - | - | |
| 5–9 yrs^ | 1,315 | 35.2 | 646 | 30.0 | <0.0001 | - | - | - | - | |
| 10–14 yrs | 1,482 | 35.4 | 688 | 30.5 | <0.0001 | 595 | 6.9 | 59 | 8.4 | 0.5 |
| 15–19 yrs | 629 | 26.6 | 442 | 18.1 | <0.0001 | 633 | 4.6 | 158 | 6.3 | 0.2 |
| Prevalence by gender | ||||||||||
| Female | 1,882 | 35.1 | 993 | 28.7 | <0.0001 | 829 | 4.2 | 111 | 7.2 | 0.2 |
| Male | 2,196 | 35.4 | 1,115 | 28.8 | <0.0001 | 459 | 7.8 | 116 | 6.0 | 0.9 |
year of diagnosis
None of the individuals with T2D diagnosed below 10 years had history of DKA at diagnosis
Temporal Trends in the Prevalence of DKA in SEARCH and YDR, by Diabetes Type
In SEARCH, the prevalence of DKA significantly increased from 2009 to 2012 (p<0.001). In YDR the DKA prevalence was relatively stable at high levels all the years (2006 to 2012) with no statistically significant linear trend (Figure 1).
Figure 1:
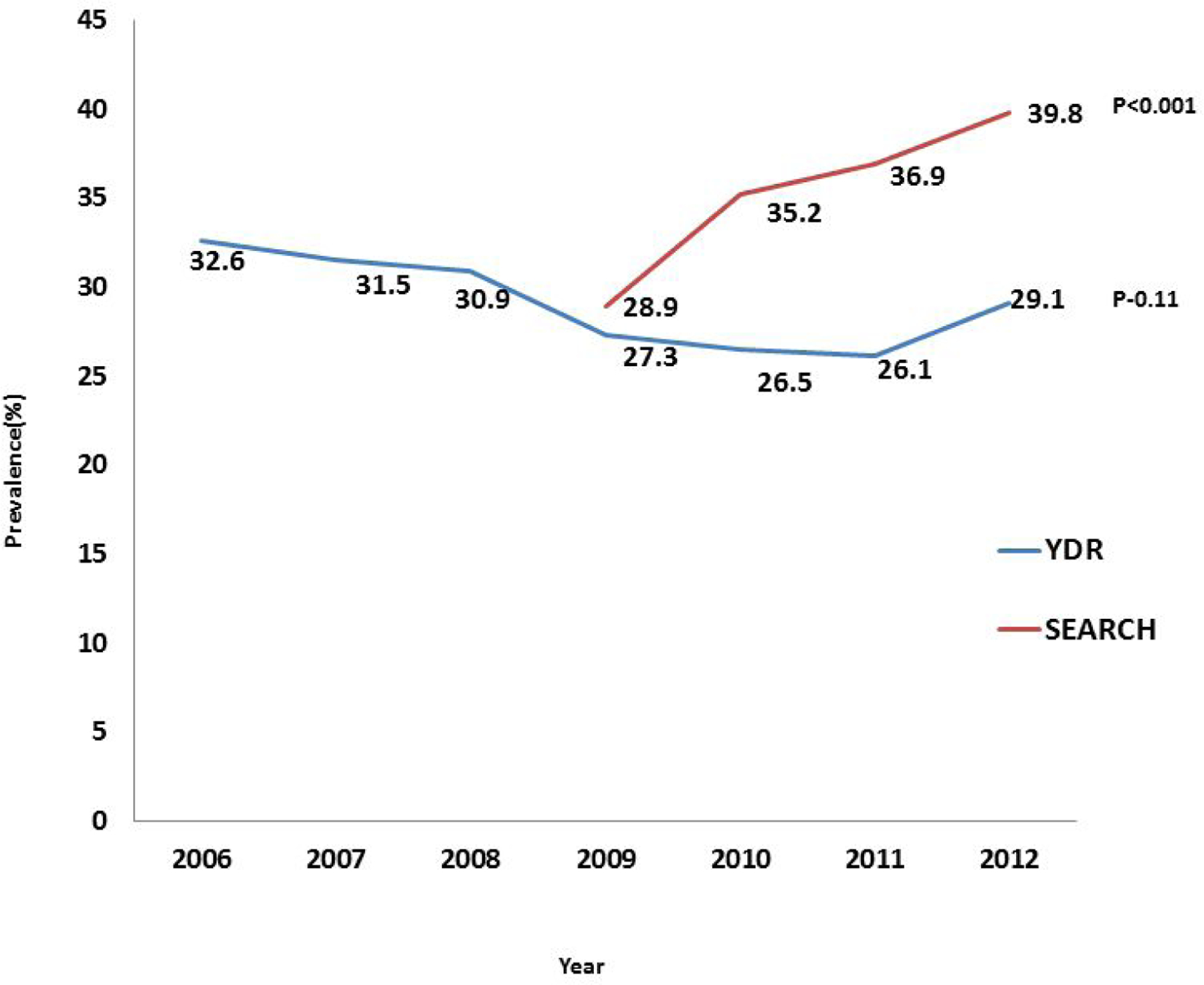
Trend in DKA prevalence at diagnosis among individuals with T1D in SEARCH (2009–2012) and YDR (2006–2012).
Discussion
Our study revealed a significant burden of DKA at diagnosis among individuals with youth-onset T1D from both India and the U.S., especially among those in the younger age groups. The burden of DKA at diagnosis among individuals with T2D was similar in both the registries. The prevalence of DKA at diagnosis with T1D increased over time in SEARCH but remained relatively stable (at high levels) in YDR.
Our current prevalence estimates of DKA at diagnosis with T1D for SEARCH are higher than the estimates from other U.S. studies and the earlier reports from SEARCH itself10. There are no such data from India to compare the findings from YDR reported here. For T2D, the current study estimates that 5.5% of individuals with youth-onset T2D in SEARCH present in DKA at diagnosis, which is lower than earlier published estimates from SEARCH (11.7% in 2002–03 to 5.7% in 2008–10)10. In both SEARCH and YDR the prevalence of DKA among individuals with T2D was more pronounced in the 10–14 age group compared to youth in 15–19 age group. This is consistent with earlier reports from SEARCH10.
DKA prevalence estimates among individuals with T1D for both SEARCH and YDR reported in the current analysis, are much higher than those from UK, Canada and Finland, reported a decade ago13,14. The EURODIAB project (2001) reported DKA prevalence at diagnosis ranging from 11% to 67% in 11 centers across Europe15. A recent systematic review summarizing data from 65 studies comprising over 29,000 children in 31 countries concluded that the frequency of DKA at diagnosis ranged from 12.8% to 80%, with highest frequencies in the United Arab Emirates (80%), Saudi Arabia (59%) and Romania (67%), and the lowest in Sweden(14%) and Canada (19 %)9. Further, the prevalence of DKA at diagnosis was inversely associated with gross domestic product (GDP) of the countries9. There is large heterogeneity in the published literature on DKA at onset/diagnosis, in terms of sample size, period of study, design and method of case identification. Hence, comparisons of our estimate with other studies should be done with caution16.
The prevalence of DKA at diagnosis seems to be inversely associated with the background prevalence of T1D in the countries9. Given the lower incidence of T1D in India, we expected a higher prevalence of DKA among the Indian population compared to U.S.. However, the results were contrary to our expectations, with higher prevalence of DKA in all the age groups in SEARCH compared to YDR. This could be due to several reasons with the distinct possibility of recall or recording bias and underreporting of DKA events in YDR. A principal reason for this could be the difference in methods used to ascertain and confirm the diagnosis of DKA in the two registries. Given the process flow in YDR, the information on DKA was captured from self-report or hospitalization records at the time of registration at a reporting center. Further, there could be a time lag between the date of diagnosis and registration of participants at the reporting centers. In contrast, SEARCH not only had direct access to medical records but was able to confirm the diagnosis of DKA through lab data including serum bicarbonate levels. Since YDR is a clinic-based registry, there could also be referral bias with likely impact on the estimated frequency of DKA.
There is a global variation in mortality associated with DKA at diagnosis among children and adolescents with diabetes. In developed countries, the overall mortality varies from 0.15% to 0.35% while in countries like India and Bangladesh, clinic-based studies report rates ranging from 3.4% to 13.4%17. Cerebral edema, sepsis and renal failure are the major precipitating factors of DKA-related mortality in the developing world17. These differential mortality rates may explain the differences seen in the estimated prevalence of DKA across countries. Therefore, the lower prevalence of DKA at diagnosis reported by YDR compared to SEARCH likely reflects a worrisome higher DKA-associated mortality, before T1D is diagnosed, which we were unfortunately unable to study. More efforts are needed to quantify the population level mortality associated with DKA at diabetes diagnosis in India.
The high burden of DKA among younger age groups in both the registries is concerning. Delayed diagnosis, relatively aggressive metabolic deterioration and difficulty in early diagnosis of symptoms in toddlers with T1D make them vulnerable to develop DKA15. Increasing parental awareness and improving health system preparedness to closely monitor children with genetic risk of T1D have shown promising results in the past18. However, it remains unclear whether the high propensity for DKA in younger children is a consequence of a particularly aggressive form of diabetes.
Data on temporal changes in DKA prevalence vary between reports from different parts of the globe with some studies reporting a declining trend14,19, while others finding no change13,20. Our analysis showed a statistically significant upward trend in the prevalence of DKA among U.S. children and adolescents with T1D after 2009–2010. This is different from earlier reports from SEARCH that showed a high but stable trend between 2002 and 200910. The reasons for this increasing trend in DKA at diagnosis of T1D among SEARCH youth in recent years need to be further explored. In YDR, the burden of DKA remained relatively stable during the study period (p=0.1); however, this should be interpreted with caution given the limitations mentioned above. Nevertheless, in both countries, the burden of DKA at diagnosis among individuals with T1D remains unacceptably high.
This report is the one of the first studies to systematically harmonize and compare data on DKA at diagnosis from Asian Indian and U.S. populations. To the best of our knowledge, this is the first study to compare DKA at diagnosis among youth with T2D between U.S. and Indian populations. For both registries, data were collected independent of the present study and over a similar time period. However, the study has several important limitations. As mentioned earlier, there were significant differences in the method of DKA ascertainment between the registries. Moreover, we were unable to study the effect of a potentially high burden of DKA-associated mortality before diagnosis of T1D in India. The sample sizes for T2D in both registries were small and not adequately powered for trend analyses. Further, SEARCH did not have DKA information for years 2006–2008. We were only able to conduct a descriptive analysis of the harmonized data, as there was no physical transfer of data between the registries. However, this comparison is an important first step in our understanding of DKA burden at diagnosis with diabetes in youth, which should lead to further research on potential explanations for observed differences.
Our data show a significant burden of DKA at diagnosis among a racially/ethnically diverse U.S. and an Asian Indian cohort of youth with T1D, especially among the younger age groups. These findings have serious public health implications as the DKA associated hospitalizations and subsequent morbidities dramatically increase the cost of diabetes care. Effective interventions to increase awareness and improve access to health care are required in both countries to prevent DKA at diagnosis among youth onset diabetes.
Acknowledgments:
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families and their health care providers, whose participation made this study possible. YDR acknowledges the patients enrolled and the participation of the reporting centers contributing data to YDR. SEARCH for Diabetes in Youth (SEARCH) registry in the U.S. is funded by the Centers for Disease Control and Prevention (CDC) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The Registry of People with Diabetes with Youth Age at Onset (YDR) in India is funded by the Indian Council of Medical Research (ICMR).
Grant support: Study supported by the National Institutes of Health (R21DK105869–02) and the Indian Council of Medical Research.
SEARCH 3/4: The authors wish to acknowledge the involvement of the Kaiser Permanente Southern California’s Clinical Research Center (funded by Kaiser Foundation Health Plan and supported in part by the Southern California Permanente Medical Group); the South Carolina Clinical & Translational Research Institute, at the Medical University of South Carolina, NIH/National Center for Advancing Translational Sciences (NCATS) grant number UL1 TR000062, UL1 Tr001450; Seattle Children’s Hospital and the University of Washington, NIH/NCATS grant number UL1 TR00423; University of Colorado Pediatric Clinical and Translational Research Center, NIH/NCATS grant Number UL1 TR000154; the Barbara Davis Center at the University of Colorado at Denver (DERC NIH grant number P30 DK57516); the University of Cincinnati, NIH/NCATS grant number UL1 TR000077, UL1 TR001425; and the Children with Medical Handicaps program managed by the Ohio Department of Health. This study includes data provided by the Ohio Department of Health, which should not be considered an endorsement of this study or its conclusions.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Grant Support (SEARCH 3): SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05–069, and DP-10–001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases.
Grant Support (SEARCH 4): The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, U18DP006139) is funded by the Centers for Disease Control and Prevention and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Sites (SEARCH 3/4): Kaiser Permanente Southern California (U18DP006133, U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U18DP006139, U48/CCU819241–3, U01 DP000247, and U18DP000247–06A1), Cincinnati’s Children’s Hospital Medical Center (U18DP006134, U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U18DP006138, U48/CCU419249, U01 DP000254, and U18DP002708), Seattle Children’s Hospital (U18DP006136, U58/CCU019235–4, U01 DP000244, and U18DP002710–01), Wake Forest University School of Medicine (U18DP006131, U48/CCU919219, U01 DP000250, and 200–2010-35171)
Abbreviations:
- DKA
Diabetic Ketoacidosis
- T1D
Type 1 Diabetes Mellitus
- T2D
Type 2 Diabetes Mellitus
- OMOP
Observational Medical Outcomes Partnership
- YDR
Registry of People with Diabetes with Youth Age at Onset
- U.S.
United States
Footnotes
Disclosures: None of the authors have any potential conflicts of interest relevant to the manuscript.
References
- 1.Eledrisi MS, Alshanti MS, Shah MF, Brolosy B, Jaha N. Overview of the diagnosis and management of diabetic ketoacidosis. Am J Med Sci. 2006;331(5):243–251. http://www.ncbi.nlm.nih.gov/pubmed/16702793. Accessed May 19, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Arslanian S, Bacha F, Grey M, Marcus MD, White NH, Zeitler P. Evaluation and Management of Youth-Onset Type 2 Diabetes: A Position Statement by the American Diabetes Association. Diabetes Care. 2018;41(12):2648–2668. doi: 10.2337/dci18-0052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edge JA, Hawkins MM, Winter DL, Dunger DB. The risk and outcome of cerebral oedema developing during diabetic ketoacidosis. Arch Dis Child. 2001;85(1):16–22. http://www.ncbi.nlm.nih.gov/pubmed/11420189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glaser N, Barnett P, McCaslin I, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264–269. doi: 10.1056/NEJM200101253440404 [DOI] [PubMed] [Google Scholar]
- 5.Lawrence SE, Cummings EA, Gaboury I, Daneman D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J Pediatr. 2005;146(5):688–692. doi: 10.1016/j.jpeds.2004.12.041 [DOI] [PubMed] [Google Scholar]
- 6.Duca LM, Wang B, Rewers M, Rewers A. Diabetic Ketoacidosis at Diagnosis of Type 1 Diabetes Predicts Poor Long-term Glycemic Control. Diabetes Care. 2017;40(9):1249–1255. doi: 10.2337/dc17-0558 [DOI] [PubMed] [Google Scholar]
- 7.Shalitin S, Fisher S, Yackbovitch-Gavan M, et al. Ketoacidosis at onset of type 1 diabetes is a predictor of long-term glycemic control. Pediatr Diabetes. 2018;19(2):320–328. doi: 10.1111/pedi.12546 [DOI] [PubMed] [Google Scholar]
- 8.Duca LM, Reboussin BA, Pihoker C, et al. Diabetic ketoacidosis at diagnosis of type 1 diabetes and glycemic control over time: The SEARCH for diabetes in youth study. Pediatr Diabetes. 2019;20(2):172–179. doi: 10.1111/pedi.12809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Usher-Smith JA, Thompson M, Ercole A, Walter FM. Variation between countries in the frequency of diabetic ketoacidosis at first presentation of type 1 diabetes in children: a systematic review. Diabetologia. 2012;55(11):2878–2894. doi: 10.1007/s00125-012-2690-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dabelea D, Rewers A, Stafford JM, et al. Trends in the Prevalence of Ketoacidosis at Diabetes Diagnosis: The SEARCH for Diabetes in Youth Study. Pediatrics. 2014;133(4):e938–e945. doi: 10.1542/peds.2013-2795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamman RF, Bell RA, Dabelea D, et al. The SEARCH for Diabetes in Youth study: rationale, findings, and future directions. Diabetes Care. 2014;37(12):3336–3344. doi: 10.2337/dc14-0574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Praveen PA, Madhu SV, Mohan V, et al. Registry of Youth Onset Diabetes in India (YDR): Rationale, Recruitment, and Current Status. J Diabetes Sci Technol. May 2016. doi: 10.1177/1932296816645121 [DOI] [PMC free article] [PubMed]
- 13.Bui TP, Werther GA, Cameron FJ. Trends in diabetic ketoacidosis in childhood and adolescence: a 15-yr experience. Pediatr Diabetes. 2002;3(2):82–88. doi: 10.1034/j.1399-5448.2002.30204.x [DOI] [PubMed] [Google Scholar]
- 14.Hekkala A, Knip M, Veijola R. Ketoacidosis at Diagnosis of Type 1 Diabetes in Children in Northern Finland: Temporal changes over 20 years. Diabetes Care. 2007;30(4):861–866. doi: 10.2337/dc06-2281 [DOI] [PubMed] [Google Scholar]
- 15.Lévy-Marchal C, Patterson CC, Green A, EURODIAB ACE Study Group. Europe and Diabetes. Geographical variation of presentation at diagnosis of type I diabetes in children: the EURODIAB study. European and Dibetes. Diabetologia. 2001;44 Suppl 3:B75–80. http://www.ncbi.nlm.nih.gov/pubmed/11724421. [DOI] [PubMed] [Google Scholar]
- 16.VanderWeele J, Pollack T, Oakes DJ, et al. Validation of data from electronic data warehouse in diabetic ketoacidosis: Caution is needed. J Diabetes Complications. 2018;32(7):650–654. doi: 10.1016/j.jdiacomp.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 17.Varadarajan P Risk factors for mortality in children with diabetic keto acidosis from developing countries. World J Diabetes. 2014;5(6):932. doi: 10.4239/wjd.v5.i6.932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Environmental Determinants of Diabetes in the Young (TEDDY) Study. Ann N Y Acad Sci. 2008;1150(1):1–13. doi: 10.1196/annals.1447.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdul-Rasoul M, Al-Mahdi M, Al-Qattan H, et al. Ketoacidosis at presentation of type 1 diabetes in children in Kuwait: frequency and clinical characteristics. Pediatr Diabetes. 2010;11(5):351–356. doi: 10.1111/j.1399-5448.2009.00600.x [DOI] [PubMed] [Google Scholar]
- 20.Jefferies C, Cutfield SW, Derraik JGB, et al. 15-year incidence of diabetic ketoacidosis at onset of type 1 diabetes in children from a regional setting (Auckland, New Zealand). Sci Rep. 2015;5(1):10358. doi: 10.1038/srep10358 [DOI] [PMC free article] [PubMed] [Google Scholar]


