Abstract
Background
Based on the status of the COVID-19 global pandemic, there is an urgent need to systematically evaluate the effectiveness of wearing masks to protect public health from COVID-19 infection.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement was consulted to report this systematic review. We conducted a systematic review and meta-analysis to evaluate the effectiveness of using face masks to prevent the spread of SARS-CoV-2. Relevant articles were retrieved from PubMed, Web of Science, ScienceDirect, Cochrane Library, and Chinese National Knowledge Infrastructure, VIP (Chinese) database. There were no language restrictions. This study was registered with PROSPERO under the number CRD42020211862.
Results
A total of 6 studies were included, involving 4 countries, after a total of 5,178 eligible articles were searched in databases and references. In general, wearing a mask was associated with a significantly reduced risk of COVID-19 infection (OR = 0.38, 95% CI: 0.21-0.69, I2 = 54.1%). For the healthcare workers group, masks were shown to have a reduced risk of infection by nearly 70%. Sensitivity analysis showed that the results were robust.
Conclusions
The results of this systematic review and meta-analysis support the conclusion that wearing a mask could reduce the risk of COVID-19 infection. Robust randomized trials are needed in the future to better provide evidence for these interventions.
Key Words: Personal protection equipment, Respiratory virus, SARS-CoV-2, Prevention, Healthcare worker
Coronavirus disease 2019 (COVID-19) is a global pandemic that has become a major public health burden worldwide. It has many potential long-term effects due to already fragile healthcare systems.1 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is transmitted through close contact and person-to-person transmission and causes COVID-19. To date, viral RNA has been found in air sampling in several studies.2 , 3 For the current foreseeable future, until a safe and effective vaccine or treatment is available, COVID-19 prevention will continue to rely on nonpharmacological interventions, including mitigation of pandemics in community settings. Therefore, evaluation of personal protective equipment (PPE), such as masks or respirators, is critical to prevent the spread of SARS-CoV-2.
There are different standards of masks, and qualified masks can help to protect users from a large number of respiratory droplets.4 , 5 They vary in thickness and permeability. N95 respirators are specifically designed to protect users from small airborne particles, including aerosols. Asadi et al. found that surgical masks and unventilated KN95 respirators reduced the emission rate of outward particles by an average of 90% and 74% during talking and coughing, respectively.6 In the prevention and control of COVID-19, the correct use of PPE is one of the most important measures to effectively interrupt the spread of the SARS-CoV-2, and to protect the safety of healthcare workers and other nonhealthcare populations.
Recommendations regarding the effect of wearing a mask on the prevention of respiratory virus transmission (RVI) have been confirmed by many studies. A meta-analysis found reduced spread of Severe Acute Respiratory Syndrome (SARS; OR = 0.32; 95% CI: 0.25–0.40).7 Another meta-analysis recently found that mask use by healthcare and nonhealthcare workers reduced the risk of laboratory-confirmed respiratory viral infection by 80% (95% CI: 0.11-0.37) and 47% (95% CI: 0.36-0.79), respectively.8
Compared with other respiratory virus infections, the protective effect of masks on COVID-19 still lacks relevant comprehensive evidence. Therefore, we performed a systematic review and meta-analysis to evaluate the effectiveness of the use of masks to prevent SARS-CoV-2 transmission.
METHODS
Identification and selection of studies
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement was consulted to report this systematic review. We prospectively submitted the systematic review protocol for registration on PROSPERO (CRD42020211862).
Regarding this meta-analysis, a comprehensive searching strategy was carefully designed to select eligible studies from multiple electronic databases, including PubMed, Web of Science, Cochrane Library, and Chinese National Knowledge Infrastructure, VIP (Chinese) database, from 10 November 2019 to 10 October 2020. The following combined search terms were used in the search: (“mask” OR “face mask” OR “respirators” OR “N95” OR “*mask”) AND (“severe acute respiratory syndrome coronavirus 2” OR “2019-nCoV” OR “COVID-19” OR “SARS-CoV-2”). Relevant Chinese technical terms for the Chinese databases were used to search for published articles.
Furthermore, references of all relevant articles and reviews were retrieved to search for additional eligible studies. Articles providing abstracts only were excluded. After deleting duplicates, all abstracts and titles were filtered independently by two reviewers to remove the irrelevant articles. We downloaded and read the full text of the potential research related to the selection criteria to incorporate systematic reviews. Reviewers compared and discussed the results. If a discussion by the two reviewers did not result in an agreement, then the third party was called upon to create consensus.
Inclusion and exclusion criteria
The studies meeting the following criteria were included: (1) concerning the relationship between the face mask and preventing COVID-19; (2) diagnosis of SARS-CoV-2 must have laboratory evidence; (3) providing complete data of cases and controls for calculating an odds ratio (OR) with 95% confidence interval (CI); (4) study design is correct and appropriate; (5) no language restrictions applied. The exclusive criteria were as follows: (1) insufficient data to ascertain the adjusted ORs; (2) conferences/meetings abstracts, case reports, editorials, and review articles; (3) duplicate publication or overlapping studies.
Data extraction and assessment of study quality
The following information was abstracted according to predesigned data extraction form by two independent reviewers (MM L & YN L): first author, year of publication, country, number of mask group and COVID-19 infection, number of the control group and COVID-19 infection, mask type, study design, whether healthcare workers or not, and main findings of the study. Another reviewer (L G) checked the extracted data for completeness and accuracy.
The Newcastle-Ottawa Scale was used to evaluate the quality of the case-control study: study ratings of 7-9 stars corresponded to high-quality, 5-6 stars to moderate quality, and 4 stars or less to low quality.9 Three members of the review team completed assessments independently. The disagreements were resolved by discussion.
Statistical analysis
The association of mask use with subsequent COVID-19 was assessed with ORs with a 95% CI. Adjusted and unadjusted pooled estimates were calculated separately. P values less than .05 were considered statistically significant. Considering the potential for between-study heterogeneity, subgroup analyzes were carried out based on stratification by HCWs, countries, and types of masks. Sensitivity analysis was performed by omitting individual studies to assess the stability of the meta-analysis. The heterogeneity was assessed using the I2 statistic. The heterogeneity was considered insignificance when P > .10 and I2 < 50%. Under any interpretation, a fixed-effect meta-analysis ignores heterogeneity. When heterogeneity is present, a confidence interval around the random-effects summary estimate is wider than a confidence interval around a fixed-effect summary estimate.10, 11, 12 Borenstein et al. argued that the random-effects model is more suitable for meta-analyses in which the effects of interventions differ between studies.10 Since it is generally considered to be implausible that intervention effects across studies are identical (unless the intervention has no effect at all), therefore in this study a random-effects model was used. Begg's and Egger's test were performed to quantitatively analyze the potential publication bias. The P values of Begg's and Egger's test more than .05 implied no obvious publication bias in this meta-analysis.13 , 14 The meta-analysis was performed using Stata (version 16.0; Stata Corp, College Station, TX) software.
RESULTS
Characteristics of eligible studies
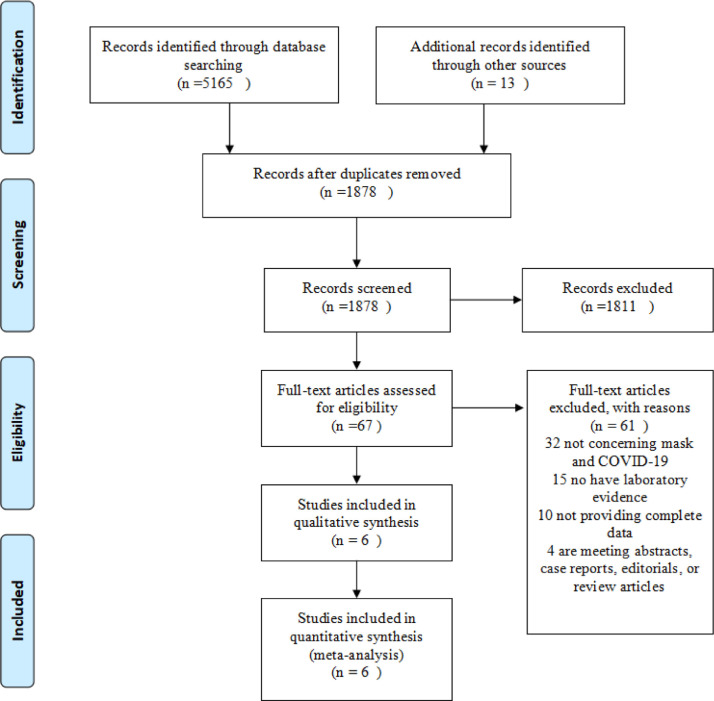
A flow diagram of the literature search and related screening process is shown in Figure 1 . A total of 6 studies met our inclusion criteria,15, 16, 17, 18, 19, 20 all studies included were case-control studies (Table 1 ). Among them, studies were conducted in China, the USA, Thailand, and Bangladesh. All patients had laboratory evidence. The study by Doung-ngern et al. investigated non-professional populations, and other studies focused on healthcare workers.
Fig 1.
Flow diagram of the study search and selection process.
Table 1.
Characteristics of eligible studies
| Study | Year | Country | Virus | Mask group |
Control group |
Mask type | Type of Study | Healthcare workers | Main findings & comments | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infections⁎ | Mask† | Infections‡ | Control§ | |||||||||
| 1 | Chen et al. | 2021 | China | 2019-nCoV | 10 | 78 | 8 | 27 | Mask¶ | Case-control study | Healthcare workers | Risk analysis revealed that wearing face masks could reduce infection risk. |
| 2 | Doung-ngern et al. | 2020 | Thailand | 2019-nCoV | 29 | 227 | 102 | 602 | Mask¶ | Case-control study | Non-healthcare workers | The consistent wearing of masks, handwashing, and social distancing to protect against COVID-19. |
| 3 | Guo et al. | 2020 | China | 2019-nCoV | 7 | 40 | 17 | 32 | Mask¶ | Case-control study | Healthcare workers | Wearing respirators or masks all of the time was found to be protective. |
| 4 | Heinzerling et al. | 2020 | USA | 2019-nCoV | 0 | 3 | 3 | 34 | Mask¶ | Case-control study | Healthcare workers | PPE use can help minimize unprotected, high-risk HCP exposures, and protect the health care workforce. |
| 5 | Khalil et al. | 2020 | Bangladesh | 2019-nCoV | 36 | 92 | 62 | 98 | N95 | Case-control study | Healthcare workers | The use of masks and decontamination of the patient's surroundings may give protection against COVID-19. |
| 6 | Wang et al. | 2020 | China | 2019-nCoV | 0 | 278 | 10 | 215 | N95 | Case-control study | Healthcare workers | The 2019-nCoV infection rate for medical staff was significantly increased in the no-mask group compared with the N95 respirator group (adjusted odds ratio (OR): 464.82, [95% CI: 97.73-infinite]). |
⁎Infections in the mask group.
†Total sample in the mask group.
‡Infections in the control group.
§Total sample in the control group.
¶Specific type of mask was not reported.
Quality of studies
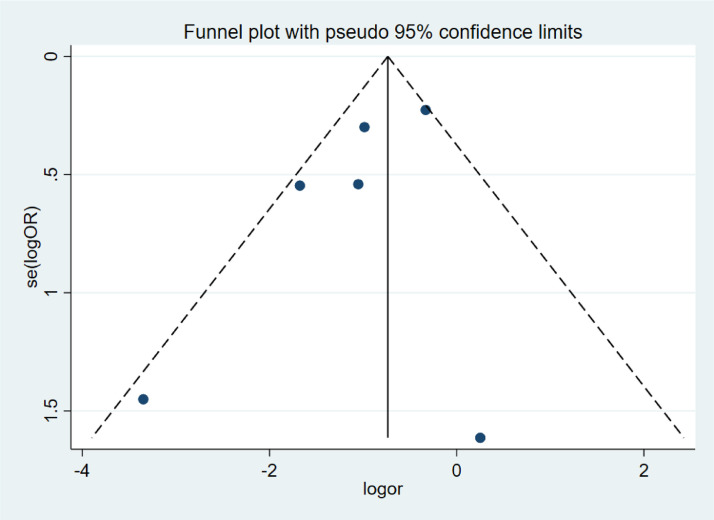
Inter-rater agreement of the quality of included studies was strong. Table 2 summarizes the quality evaluations of the included studies. Funnel plots assessing the risk of publication bias are included in Figure 2 . Neither Begg's test (z = 0.75, P= .452) nor Egger's test (t = −1.44, P= .224) manifested any distinct evidence of the publication bias. The sensitivity analyses did not substantially alter the pooled ORs by excluding one-by-one study, indicating that the meta-analysis was generally robust.
Table 2.
The quality of the case-control studies and cohort studies
| Study | Year | Selection | Comparability | Outcome | Stars* | |
|---|---|---|---|---|---|---|
| 1 | Chen et al. | 2020 | 3 | 2 | 2 | 7 |
| 2 | Doung-ngern et al. | 2020 | 4 | 2 | 3 | 9 |
| 3 | Guo et al. | 2020 | 3 | 2 | 2 | 7 |
| 4 | Heinzerling et al. | 2020 | 2 | 2 | 2 | 6 |
| 5 | Khalil et al. | 2020 | 3 | 2 | 2 | 7 |
| 6 | Wang et al. | 2020 | 3 | 1 | 1 | 5 |
Scoring by Newcastle-Ottawa Scale.
Fig 2.
Funnel plots of face masks and COVID-19.
Masks and risk of SARS-CoV-2 infection
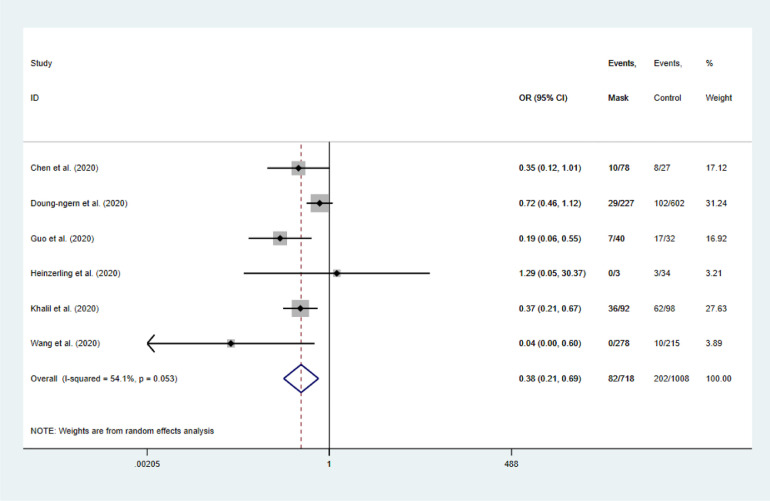
The 6 studies reporting on the effectiveness of wearing masks included 1,233 participants. In general, face masks were effective in preventing the spread of SARS-CoV-2. After wearing a mask, the risk of contracting COVID-19 was significantly reduced, with the pooled OR of 0.38 and 95% CI: 0.21-0.69 (I2 = 54.1%, M-H Random-effect model; Fig 3 ).
Fig 3.
Forest plot for the random-effect meta-analysis.
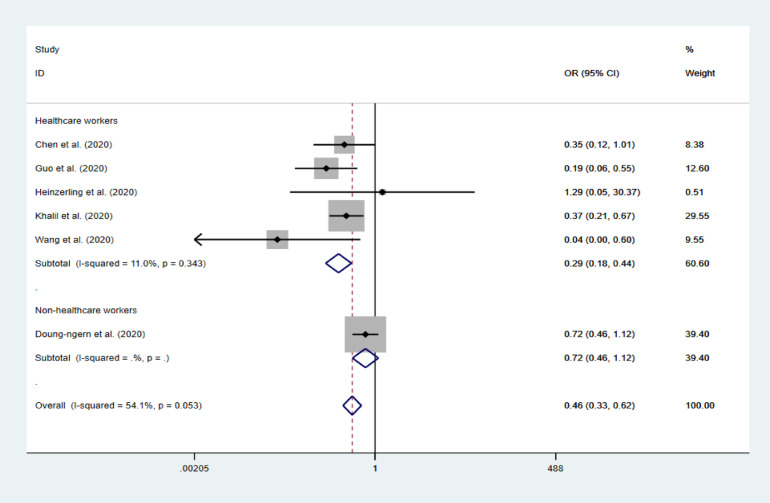
In the subgroup of HCWs only, the protective effect was more obvious, with the pooled OR of 0.29 (95% CI: 0.18-0.44, I2 = 11%; Fig 4 ).
Fig 4.
Forest plots of the fixed-effect of masks on COVID-19 between HCW and non-HCW.
Only Doung-ngern et al.16 investigating non-HCW, and no protective effect was found in the subgroup analysis (OR = 0.72, 95% CI: 0.46-1.12). It should be noted that the estimate after adjusted possible confounding variables was 0.23 (95% CI: 0.09-0.59) in this study, and the protection of masks was still statistically significant (adjustment variables including sex, age, contact place, the shortest distance of contact, duration of contact, sharing dishes, or cigarettes and handwashing; Table 3 ).
Table 3.
Meta-analysis results of the effect of masks on COVID-19 infection among different subgroups
| Subgroup | Study numbers | OR | 95%CI | Heterogeneity | |
|---|---|---|---|---|---|
| Unadjusted estimates | Overall | 6 | 0.38 | 0.21-0.69 | 54.1% |
| HCWs | 5 | 0.29 | 0.18-0.44 | 11.0% | |
| Non-HCWs | 1 | 0.72 | 0.46-1.12 | N/A | |
| China | 3 | 0.21 | 0.09-0.53 | 26.1% | |
| Other countries | 3 | 0.55 | 0.32-0.95 | 39.3% | |
| Mask group* | 4 | 0.44 | 0.21-0.93 | 52.0% | |
| N95 group | 2 | 0.17 | 0.02-1.69 | 64.6% | |
| Adjusted estimates | Overall | 5 | 0.19 | 0.11-0.33 | 77.6% |
| HCWs | 4 | 0.18 | 0.09-0.34 | 83.0% | |
| Non-HCWs | 1 | 0.23 | 0.09-0.59 | N/A | |
| China | 3 | 0.06 | 0.02-0.17 | 81.4% | |
| Other countries | 2 | 0.3 | 0.16-0.57 | 0.0% | |
| Mask group* | 3 | 0.19 | 0.09-0.38 | 0.0% | |
| N95 group | 2 | 0.2 | 0.09-0.44 | 94.3% |
HCW, Healthcare workers; Non-HCWs, Nonhealthcare workers; N/A, Not applicable
Specific type of mask was not reported.
By subgroup analysis of geographic locations, beneficial protective effects of wearing masks were found in China (OR = 0.21, 95% CI: 0.09-0.53, I2 = 26.1%), and other countries (OR = 0.55, 95% CI: 0.32-0.95, I2 = 39.3%). Face mask could significantly reduce the risk of SARS-CoV-2 infection (OR = 0.44, 95% CI: 0.21-0.93, I2 = 52.0%). And no significant protective effect was shown in the N95 respirator group (OR = 0.17, 95% CI: 0.02-1.69, I2 = 94.6%) in subgroup analysis. However, the significant protective effect of N95 respirator was shown in the adjusted estimation subgroup analysis (OR = 0.19, 95% CI: 0.09-0.38, I2 = 0.0%; Table 3).
DISCUSSION
This meta-analysis of all available articles provides the most current evidence to date on the efficacy of face masks in preventing the transmission of SARS-CoV-2, which causes COVID-19 in 2019. It spread quickly after being discovered from Wuhan, China at the end of 2019, eventually leading to a global pandemic.21 Experimental studies have grown live viruses from aerosols and surfaces several hours after implantation.22 A large amount of pathological evidence shows that aerosol transmission is the predominant route of transmission.23 Proximity and ventilation are also determinants of transmission risk.24
Wearing a mask can prevent the inhalation of large droplets and sprays.25 Research evidence shows that masks can filter sub-micron dust particles.26 The previous meta-analysis concluded that after wearing a mask, the risk of respiratory viral infections including influenza, SARS, and H1N1 was significantly reduced with the pooled OR was of 0.35. This result is similar to the result of our meta-analysis that wearing a mask is also very effective in preventing the spread of COVID-19 (OR = 0.38, 95% CI: 0.21-0.69).
It should be noted that this meta-analysis was not the only study investigating the association between the facemask and the risk of COVID-19. Chu et al. found that the face mask use reduced the risk of COVID-19, SARS, and MERS.1 Wang et al. implemented a protocol for systematic review and meta-analysis and plan to collect randomized controlled trials on the efficacy of community masks against influenza. Although the relevant results have not been published, they concluded that in the face of disasters such as COVID-19, even if the masks might not be significantly effective, as an option, people could use it before the evidence is available.27 Another unpublished meta-analysis on face masks in community settings suggested that face masks significantly reduce the risk of SARS-CoV-2 infection.28
The WHO started recommending wearing masks as part of a comprehensive approach to reducing the spread of SARS-CoV-2 in June 2020.29 This is consistent with the recommendations made by the Chinese health department at the beginning of the epidemic.30 In our results, the use of face masks reduced the risk of COVID-19 infection by 70% for health care workers. Only one study on the general population included in this study, and the adjusted ORs were also statistically significant. Besides, a cohort study in Beijing found that the use of masks in index patients was independently associated with a reduction in the risk of household infection.31 Investigation of the outbreak on USS Theodore Roosevelt found that low infection risk was related to self-reports of face coverings and wearing masks.32 This evidence suggests the protective effect of masks on the general population.
The United States Centers for Disease Control and Prevention specifies that the mask recommendation should not include medical masks.33 Because these masks should be reserved for healthcare workers. Regarding the types of masks, both N95 masks and general masks have been found effective in this study. This is consistent with the conclusions of previous studies. The Cochrane system review of Jefferson et al. showed that both N95 and surgical masks can effectively prevent the spread of respiratory viruses.7 And Long et al. indicated a protective effect of N95 respirators against laboratory-confirmed bacterial colonization (RR = 0.58, 95% CI 0.43-0.78).8 However, the currently available evidence has not yet confirmed the difference in protective effectiveness between N95 masks and medical-surgical masks,34 although when tested in the laboratory, it was found that N95 respirators were generally more effective than surgical masks and have better facial sealing characteristics.7 , 35 As face seal is critical for the N95 respirator to provide its protective effect at maximal capacity, improperly donning and doffing, or adjusting of the N95 respirator could lead to inadvertent contamination and air leak around the edge of N95 respirator, thus negating the potential protective benefit.7 , 35
This investigation also had several limitations. First, all the included studies were case-control studies and lacked adequately designed and high-quality randomized controlled studies. This may reduce the overall strength of the results. Second, because more research is currently focused on the treatment and pathology of COVID-19, the total sample size of studies on the effectiveness of PPE is still relatively small. We will continue to focus on the progress of relevant population-based studies. Third, the available studies that provided data for some subgroup analyses were limited, thus the statistical power was relatively low and the results should be interpreted with caution. Fourth, this study performed a meta-analysis on the adjusted data to calculate the corresponding results, however, the included original studies did not make the same adjustments for possible confounding factors, such as gender, age, vaccination, hand hygiene, and cultural difference, and thus, the heterogeneity of the final results may be affected. However, we conducted a sensitivity analysis using unadjusted raw data and the results did not change the conclusion, indicating that was generally robust.
CONCLUSION
This meta-analysis aims to provide comprehensive evidence to identify the risk of SARS-CoV-2 infection associated with mask-wearing. This could help healthcare workers, public health professionals, and policymakers to identify risk factors and develop strategies to reduce COVID-19 infection. The results show that the mask has a significant protective effect against COVID-19. However, more evidence is still needed to better define the protective effect of the mask on the wider population, and more large practical trials are needed to evaluate the efficacy of the mask on the face to prevent transmission of SARS-CoV-2.
Author Contributions
Mingming Liang &Yanni Li: Data curation, Writing, Original draft preparation, Software. Liang Gao: Data curation, Conceptualization, Methodology. John Patrick Uy: Data curation and Writing- Reviewing. Mubashir Ayaz Ahmed: Data curation, Visualization. Ce Cheng: Data curation, Visualization. Qin Zhou: Data curation, Visualization. Chenyu Sun: Supervision, Writing- Reviewing and Editing.
Footnotes
All authors read and approved the final manuscript.
Conflicts of interest: None to report.
Funding: This work has not received any funding.
Reference
- 1.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet (London, England) 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sommerstein R, Fux CA, Vuichard-Gysin D, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect control. 2020;9:100. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:1583–1591. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Respirator trusted-source information. 2018. Available at: https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/respsource1quest1.html. Accessed October 7, 2020.
- 5.Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asadi S, Cappa CD, Barreda S, et al. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci Rep. 2020;10:15665. doi: 10.1038/s41598-020-72798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jefferson T, Del Mar C, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ (Clin Res Ed) 2009;339:b3675. doi: 10.1136/bmj.b3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang M, Gao L, Cheng C, et al. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;36 doi: 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2009 The Ottawa Hopital. 2009. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed October 1, 2020
- 10.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trial. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Deeks JJ, Higgins JP, Altman DG, Group obotCSM. Chapter 10: analysing data and undertaking meta-analyses. Cochrane Handbook. Cochrane Training. 2020. Available at: https://training.cochrane.org/handbook/current/chapter-10#section-10-10-4-1. Accessed December 7, 2020
- 13.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 14.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res Ed) 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, Tong X, Wang J, et al. High SARS-CoV-2 antibody prevalence among healthcare workers exposed to COVID-19 patients. J Infect. 2020;81:420–426. doi: 10.1016/j.jinf.2020.05.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doung-ngern P, Suphanchaimat R, Panjangampatthana A, et al. Case-control study of use of personal protective measures and risk for severe acute respiratory syndrome coronavirus 2 infection, Thailand. Emerg Infect Dis J. 2020;26:2607–2616. doi: 10.3201/eid2611.203003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo X, Wang J, Hu D, et al. Survey of COVID-19 disease among orthopaedic surgeons in Wuhan, People's Republic of China. J Bone Joint Surg Am Volume. 2020;102:847–854. doi: 10.2106/JBJS.20.00417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heinzerling A, Stuckey MJ, Scheuer T, et al. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient - Solano County, California, February 2020. MMWR Morb Mortal Weekly Rep. 2020;69:472–476. doi: 10.15585/mmwr.mm6915e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khalil MM, Alam MM, Arefin MK, et al. Role of personal protective measures in prevention of COVID-19 spread among physicians in Bangladesh: a multicenter cross-sectional comparative study. SN Compr Clin Med. 2020:1–7. doi: 10.1007/s42399-020-00471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X, Pan Z, Cheng Z. Association between 2019-nCoV transmission and N95 respirator use. J Hosp Infect. 2020;105:104–105. doi: 10.1016/j.jhin.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. Available at: http://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020. Accessed September 15, 2020.
- 22.Stadnytskyi V, Bax CE, Bax A, Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc Natl Acad Sci USA. 2020;117:11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prather KA, Marr LC, Schooley RT, McDiarmid MA, Wilson ME, Milton DK. Airborne transmission of SARS-CoV-2. Science (New York, NY) 2020;370:303–304. doi: 10.1126/science.abf0521. [DOI] [PubMed] [Google Scholar]
- 24.Meyerowitz EA, Richterman A, Gandhi RT, Sax PE. Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Annal Inter Med. 2021;174:69–79. doi: 10.7326/M20-5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leung NHL, Chu DKW, Shiu EYC, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7:413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang H, Chen MB, Cui WY, Xu HL, Zheng QH. The efficacy of masks for influenza-like illness in the community: a protocol for systematic review and meta-analysis. Medicine. 2020;99:e20525. doi: 10.1097/MD.0000000000020525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rohde D, Ahern S, Clyne B, et al. Effectiveness of face masks worn in community settings at reducing the transmission of SARS-CoV-2: a rapid review [version 1; peer review: 1 approved with reservations] HRB Open Res. 2020;3:76. [Google Scholar]
- 29.WHO. Advice on the use of masks in the context of COVID-19. 2020. World Health Organization. Available at:https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak. Accessed June 20, 2020
- 30.Public Protection Guidelines for Pneumonia in Novel Coronavirus Infections. National Health Commission of the People's Republic of China. 2020. Available at:http://www.nhc.gov.cn/xcs/fkdt/202001/bc661e49b5bc487dba182f5c49ac445b.shtml. Accessed October 5, 2020
- 31.Wang Y, Tian H, Zhang L, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Global Health. 2020;5 doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Payne DC, Smith-Jeffcoat SE, Nowak G, et al. SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy Service Members - USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Weekly Rep. 2020;69:714–721. doi: 10.15585/mmwr.mm6923e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.How to Select, Wear, and Clean Your Mask. Centers for Disease Control and Prevention. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed October 6, 2020.
- 34.Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188:567–574. doi: 10.1503/cmaj.150835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rebmann T, Carrico R, Wang J. Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am J Infect Control. 2013;41:1218–1223. doi: 10.1016/j.ajic.2013.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]