Abstract
Background
The COVID-19 pandemic has caused a severe shortage of personal protective equipment (PPE), especially N95 respirators. Efficient, effective and economically feasible methods for large-scale PPE decontamination are urgently needed.
Aims
(1) to develop protocols for effectively decontaminating PPE using vaporized hydrogen peroxide (VHP); (2) to develop novel approaches that decrease set-up and take-down time while also increasing decontamination capacity; (3) to test decontamination efficiency for N95 respirators heavily contaminated by make-up or moisturizers.
Methods
We converted a decommissioned Biosafety Level 3 laboratory into a facility that could be used to decontaminate N95 respirators. N95 respirators were hung on metal racks, stacked in piles, placed in paper bags or covered with make-up or moisturizer. A VHP® VICTORY™ unit from STERIS was used to inject VHP into the facility. Biological and chemical indicators were used to validate the decontamination process. Findings: N95 respirators individually hung on metal racks were successfully decontaminated using VHP. N95 respirators were also successfully decontaminated when placed in closed paper bags or if stacked in piles of up to six. Stacking reduced the time needed to arrange N95 respirators for decontamination by approximately two-thirds while almost tripling facility capacity. Make-up and moisturizer creams did not interfere with the decontamination process.
Conclusions
Respirator stacking can reduce the hands-on time and increase decontamination capacity. When personalization is needed, respirators can be decontaminated in labelled paper bags. Make up or moisturizers do not appear to interfere with VHP decontamination.
Keywords: COVID-19, Decontamination, Vaporized hydrogen peroxide, N95 respirators
Introduction
SARS-CoV-2, the virus responsible for the COVID-19 pandemic, has infected almost 17 million people and caused more than 680,000 deaths worldwide through July 2020 [1]. Healthcare workers (HCWs) can be exposed to high viral loads of SARS-CoV-2 by inhaling droplets or aerosolized viral particles originating from patients under their care [2]. SARS-CoV-2 can survive in aerosols for more than 3 h and the virus can be efficiently transmitted in this form [3,4]. In China, more than 3000 HCWs were infected during the COVID-19 pandemic, and more than 10,600 workers were infected in Italy [5,6]. Shortages of personal protective equipment (PPE) can increase the risk of infection [2,7] and there is an increasing need to expand the manufacturing capability of PPE and to improve the supply chain [8]. Decontamination and reuse of PPE provides another means of increasing PPE availability. Several studies have validated the use of vaporized hydrogen peroxide (VHP) to decontaminate N95 respirators of bacteria, mycobacteria, viruses and, importantly, SARS-CoV-2 [9,10]. An advantage of using VHP as a decontaminant is that it is degraded into oxygen and water eliminating concerns of toxic byproducts.
Here, we provide a detailed protocol for using VHP to effectively decontaminate N95 respirators and demonstrate that this protocol is effective even with N95 respirators that are heavily covered with make-up and moisturizers as might occur during day to day activities. Further, we describe and validate simple but novel modifications to this approach that can substantially increase the number of N95 respirators that can be decontaminated in a typical facility while simultaneously improving workflow and dramatically saving time and personnel efforts.
Methods
Operation design
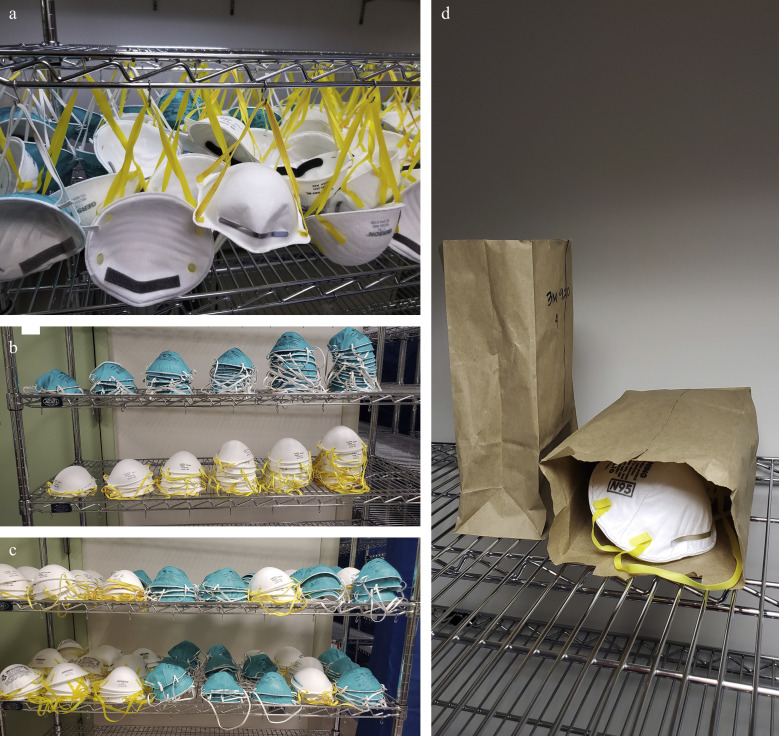
The Medical Science Building (MSB) located in the Newark campus of Rutgers University, holds a decommissioned Biosafety Level Three (BSL3) facility with a dedicated exhaust system making it possible to isolate and regulate airflow in this facility. This facility was also designed to maintain each room under negative pressure, in accordance with BSL3 design standards. These features enabled us to convert this facility into one that can be easily used to decontaminate N95 respirators. The facility has a 2400-ft3 common room and three 1200-ft3 modules. The common room was repurposed for N95 respirator decontamination and the three modules were partially sealed to contain VHP leakage. N95 respirators were hung on stainless racks using 50 metal hooks per shelf with five shelves per rack (Figure 1 a). The hooks were secured to the racks using pliers. In other experiments N95 respirators were positioned in piles (Figure 1b, c) or inside paper bags (Figure 1d). To optimize exposure to VHP, N95 respirators were hung such that they did not touch each other. Seventeen metal racks were located along the walls of the common room leaving space available for additional racks if needed. Based on this design, the capacity for this operation was 4250 N95 respirators per run using only the common room and the total capacity could be increased to 7250 N95 respirators per run if racks were also located in the three modules.
Figure 1.
N95 respirator placement for decontamination of mobile racks. (a) N95 respirators hung on the metal racks. (b) N95 respirator piles. Left to right stacks of two, four, six, eight, 10 and 12 N95 respirators. (c) Configuration of an entire rack of N95 respirators arranged in piles. (d) N95 respirators individually packaged in paper bags.
Decontamination protocol
SARS-CoV-2 can survive prolonged periods on solid surfaces, and it is eliminated from cardboard after 24 h [4]. As a result, multiple groups have recommended letting disposable N95 respirators ‘rest’ for at least 24 h between uses [11]. All N95 respirators received from the University Hospital (UH, Newark, NJ, USA) and used with COVID-19 patients were kept in sealed boxes in a secure area for at least 48 h before being hung for decontamination. Personnel wore PPE consisting of disposable Tyvek with booties and hoods, cover shoes, double gloves, aprons, P100 respirators and safety glasses to enter the facility and hang N95 respirators. It took a single individual an average of 30 min to hang 250 N95 respirators on one of our decontamination racks.
N95 respirators were then decontaminated with VHP using a VHP® VICTORY™ unit (Steris Life Sciences, Mentor, OH, USA) filled with a 35% aqueous hydrogen peroxide solution (Vaprox@). The VICTORY™ unit uses heat to vaporize hydrogen peroxide while maintaining the concentration below the dew point to keep hydrogen peroxide in a gaseous state thereby avoiding condensation. The concentration of VHP in the room was monitored using a VHP TS1000 Tri-Scale Sensor. If needed, a VHP AR12000 Aerator could be used to remove VHP from the room. The VICTORY™ unit was remotely controlled by a computer using SmartPhase™ software technology that automatically adjusted VHP injection rates based on room temperature, relative humidity, and VHP concentration. The programme automatically calculated bioburden reduction and VHP saturation in real time to maintain the concentration of VHP close to the setting point and to maintain the vapour state, respectfully.
Four fans were positioned in different areas of the common room to ensure a uniform distribution of VHP. Because VHP is more dense than air, fans were oriented to blow air towards the ceiling to facilitate the dispersion of VHP in the higher regions. The locations of the fans were marked on the ground using masking tape to ensure that they maintained positions during each decontamination run.
Decontamination was performed in four phases: conditioning, gassing, gassing-dwell and aeration. Based on the temperature, humidity and volume of the facility, the condition and gassing phases lasted approximately 90 min. During these phases, VHP was injected at a rate between 5 and 40 g/min to keep a target concentration of 400 ppm. The actual concentration varied between 400 and 800 ppm. The concentration of VHP was remotely monitored using the VNC Viewer software on a portable computer. The dwelling phase was maintained for 3 h with no additional VHP injected during this time. Supply and exhaust fans were switched back on at the end of the dwelling phase to facilitate the removal of the VHP. The aeration phase was kept overnight for approximately 15–18 h. The following morning, the residual concentration of VHP in the facility was measured using a Dräger x-Am 5100 (Dräger, Telford, PA, USA) to ensure that the VHP concentration was below the safe level of 1 ppm.
Five validation runs were conducted on approximately 1250 N95 respirators of different models. A rack with 250 control N95 respirators was decontaminated with every cycle to determine the effect of multiple sterilization cycles on the integrity of the N95 respirators. Biological indicators (BIs) (Spordex® VHP Biological Indicator Discs, Steris Life Sciences, Mentor, OH, USA) and chemical indicators (CIs) (Steraffin® VHP Type 4 Process Indicator, Steris Life Sciences, Mentor, OH, USA) were positioned in different parts of the room. Some indicators were also placed within closed control N95 respirators to validate that all areas were exposed to the correct concentration of VHP. After decontamination, CIs were inspected visually to observe whether they had changed from violet to yellow indicating that VHP had successfully contacted the area. BIs containing Geobacillus stearothermophilus spores that are commonly used to verify the successful decontamination of sterilization cycles [12,13], were aseptically transferred into Tryptic Soy Broth and incubated for 7 days at 37°C. Results, growth or no growth, were read at 24 h and 7 days post-inoculation. Positive and negative controls were included in every run to represent BI viability and media sterility. Decontamination was confirmed (pass) when both the CIs turned yellow indicating VHP exposure and the BI was negative for growth. Decontamination was not confirmed (fail) if either the CI did not turn the requisite yellow color or the BI was positive for growth.
N95 respirators
Respirator models 3M 9210, 3M 1870, 3M 1870+, 3M 1860S, and 3M 1860 (3M, St. Paul, MN; Cardinal Health, Dublin, OH, USA; Gerson, Middleboro, MA, USA); Cardinal Health S and M/L (Cardinal Health, Dublin, OH, USA), Gerson 2130 and Gerson 1730 (Gerson, Middleboro, MA, USA); Halyard Fluidshield 46727 and 46827 (O&M Halyard, Inc., Alpharetta, GA, USA) were tested in this study. These are the models most frequently used by HCWs at UH.
Quality control
At the end of each decontamination cycle, the PortaCount Pro+ Respirator Fit Tester Model 8038 was used to quantitatively define functional filtration integrity of the N95 respirators. Structural integrity was also evaluated via visual inspection of N95 respirators [14]. N95 respirators in the control rack underwent 12 decontamination cycles and were inspected after each run to determine whether there was loss in respirator integrity; the results of the respirator integrity checks are described in a separate study [14].
Improving workflow using N95 respirator piles
Trials were conducted to identify ways to increase the number of N95 respirators that could be decontaminated at the same time in our facility by replacing the tedious N95 respirator hanging process with a faster method. For this purpose, five N95 models (Table I ) were piled in stacks of four, six, eight, 10 and 12 units (Figure 1b). BIs and CIs were inserted into the middle of each pile to determine which pile configuration remained consistent with full N95 respirator decontamination.
Table I.
Decontamination results when N95 respirators were placed in piles of various sizes
| Respirator model | No. of respirators per pile | No. of replicates | No. of experiments | BIs and CIs results |
|---|---|---|---|---|
| Gerson 1730 (TC-84A-0160) | 4 | 3 | 4 | Pass |
| 6 | 3 | 4 | Pass | |
| 8 | 1 | 1 | Pass | |
| 10 | 1 | 1 | Pass | |
| 3M 1860S (TC-84A-0006) | 4 | 3 | 4 | Pass |
| 6 | 3 | 4 | Pass | |
| 8 | 1 | 1 | Pass | |
| 10 | 1 | 1 | BI and CI failed | |
| 12 | 1 | 1 | BI and CI failed | |
| 3M 8210 Plus | 4 | 3 | 4 | Pass |
| 6 | 3 | 3 | Pass | |
| Truline A501780 | 4 | 3 | 4 | Pass |
| 6 | 3 | 4 | Pass | |
| 8 | 1 | 1 | Pass | |
| 10 | 1 | 1 | Pass | |
| Cardinal Health N95A-S | 4 | 3 | 4 | Pass |
| 6 | 3 | 4 | Pass | |
| 8 | 1 | 2 | Pass | |
| 10 | 1 | 2 | Pass | |
| 12 | 1 | 2 | Pass |
Improving workflow by decontaminating N95 respirators in paper bags
HCWs at UH collected their N95 respirators in paper bags. Each bag was labelled with the user's name and contained either one or two N95 respirators. When the N95 respirators were received at the decontamination site, they were removed from the bag and hung on metal racks. This made it difficult to return N95 respirators to their original owners. Decontaminating N95 respirators without removing them from the paper bags could improve workflow and simplify the process needed to return N95 respirators to their original users. To test the safety of this procedure modification, a sample of five N95 respirators (Halyard Fluidshield 46727/46827) were put inside five different paper bags (Figure 1d), the N95 respirators were closed with tape to mimic a worst-case scenario where an N95 respirator was completely folded, and the bag was closed (in a normal operation the bags would be left open to facilitate the dispersion of VHP). BIs and CIs were inserted inside closed N95 respirators within the paper bags. The trial was repeated in five different decontamination runs.
Effect of make-up and moisturizer creams on decontamination efficacy
Several N95 respirators received from UH for decontamination had extensive traces of make-up or moisturizer creams. To determine whether a layer of make-up or moisturizer cream could interfere with the decontamination process, the inside part of N95 respirators (Halyard Fluidshield 46727/46827) that were received from the hospital and that were previously sterilized with VHP, was completely covered with make-up (Maybelline Fit Me Matte + Poreless Foundation, L'Oreal, New York, NY, USA), lipstick (Maybelline Lipstick, L'Oreal, New York, NY, USA), or moisturizer cream (Oil Free Moisturizer, Beauty 360, CVS Woonsocket, RI, USA) or a combination of make-up and moisturizer cream, BIs and CIs were placed inside the N95 respirator, and the N95 respirator was then folded and closed using tape. Halyard Fluidshield (model 46727/46827) N95 respirators were selected for this study because they can be folded. The trial was repeated in five different decontamination runs. The respirators used in these trials were not contaminated with SARS-CoV-2.
Results
Facility decontamination
An example of the decontamination cycle is reported in Supplementary Figure S2. On average, it took 90 min for VHP concentrations to reach a level reported to reduce micro-organisms by 25-logs based on calculations from the SmartPhase™ software. The concentration of VHP fell below 1 ppm approximately 5–6 h after turning on supply and exhaust fans. After the decontamination cycle, all the CIs turned yellow indicating optimal exposure to VHP, and there was no growth in the BIs 7 days post-inoculation. These results validated the successful decontamination of the facility. Additionally, CIs located inside control N95 respirators turned yellow and all BIs were negative for growth after 7 days post-inoculation, indicating that all surfaces of the N95 respirators were decontaminated even when folded.
Improving workflow using N95 respirator piles
One to four piles containing stacks of four, six, eight, 10 or 12 N95 respirators per pile were decontaminated for each of five N95 respirator models (Table I). The results of the BIs and CIs that had been inserted into the middle of the piles were used to determine whether effective decontamination had occurred. Our results showed that all N95 respirator models were decontaminated (pass, CIs turned yellow and no growth observed for the BIs) when stacked in piles of eight or fewer. However, the 3M 1860S (TC-84A-0006) N95 respirators were not decontaminated (failed, CIs did not turn yellow and growth was observed for the BIs) when piled in stacks of 10 or 12. All other N95 respirator models were decontaminated even when piled in stacks of 10 or 12. Four additional decontamination experiments were then performed on piles of four and six N95 respirators using all five N95 respirator models. In these follow up experiments, both four and six N95 respirator piles and all five models were decontaminated according to both the BI and CI indicators.
On each shelf we were able to place 24 piles of six N95 respirators (Figure 1c), for a total of 720 units per rack. When we hung N95 respirators, we were able to place 50 units per shelf, for a total of 250 per rack. In our operation we used 17 racks. Based on this design, we would have been able to increase our decontamination capacity from 4250 to 12,240 units per run when N95 respirators were arranged in piles instead of hanging them.
Placing the N95 respirators in piles also saved time in the setting up and taking down process. It took approximately 8 min to fill a rack with piles of N95 respirators, compared with 30 min when they were hung. Based on our operation design, it took in total 2 h and 20 min to arrange the N95 respirators in the 17 racks compared with 8 h and 30 min when they were hung. It took a similar time to remove the N95 respirators from the shelves after the decontamination.
N95 respirators in paper bags
Three replicates of N95 respirators folded up inside paper bags were tested in five separate experiments. BIs and CIs inserted in folded and closed N95 respirators inside the closed paper bags were used to test for decontamination. Our results showed effective decontamination for all N95 respirators in all experiments (Table II ).
Table II.
Decontamination results when N95 respirators were covered with make-up and moisturize cream or placed inside paper bags
| Respirator model | Condition | No. of replicates | No. of experiments | BIs and CIs results |
|---|---|---|---|---|
| Halyard Fluidshield 46727/46827 | Respirator covered in moisturizer cream | 3 | 5 | Pass |
| Respirator covered in foundation | 3 | 5 | Pass | |
| Respirator covered in moisturizer cream and foundation | 3 | 5 | Pass | |
| Halyard Fluidshield 46727/46827 | Inside brown paper bag | 3 | 5 | Pass |
Make-up and moisturizer creams
Halyard Fluidshield (model 46727/46827) N95 respirators were used to assess whether make-up and/or moisturizer creams interfere with the ability of VHP to decontaminate. BIs and CIs placed inside the N95 respirators were used to test for decontamination. Neither make-up nor moisturizer cream, nor a combination of both interfered with the decontamination procedure, across five separate experiments (Table II).
Discussion
We have described how to decontaminate thousands of N95 respirators using a relatively small 2400-ft3 facility. The entire decontamination process, from hanging the N95 respirators to the end of the sterilization cycle, took an entire day using a conventiona l mask-hanging protocol. We hung N95 respirators as the first task of the morning and then started the sterilization cycle later in the morning. The aeration cycle to remove VHP from the decontamination facility was then started in the late afternoon, and we went inside the facility the following morning when the VHP concentration was close to 0 ppm. Towards the end of the project, we hung N95 respirators the day before running a decontamination cycle to facilitate the process. Because the N95 respirators were kept in a BSL3 facility that is under negative pressure and locked, there was no risk of exposure to people outside the facility. When we ran decontamination cycles daily, we observed that the concentration of VHP would not fall below 1 ppm on the following day. It is possible that the walls, ceiling and floors of the facility became saturated with VHP when the decontamination cycle was run daily because the situation did not change even when there were less than 100 N95 respirators in the facility. Thus, we recommend every other day sterilization in facilities where this problem occurs. Some HCWs wear make-up or use moisturizer creams that can leave traces on N95 respirators, even ones destined for decontamination and reuse. Here we demonstrated that make-up or moisturizer creams are unlikely to interfere with the decontamination process when VHP is used. Our study describes a more efficient way to perform the decontamination process. We have also confirmed that most but not all models of N95 respirators will continue to fit and function properly for at least six decontamination cycles [14]. This has also been confirmed by others using a single N95 respirator model [15]. The integrity of N95 respirators must be maintained following decontamination to prevent distribution of inadequate PPE from respirator reuse programmes. We observed a downward trend in the functional integrity of Halyard Fluidshield N95 respirators throughout eight VHP decontamination cycles [14]. These data bring to light a potential liability of decontamination and reuse programmes and warrant further study.
Two of the goals of our study were to find ways to simplify the process of preparing N95 respirators for decontamination and to increase the overall number of N95 respirators that could be decontaminated in a single day. We tested the possibility of piling N95 respirators on top of each other in small stacks instead of hanging them. In these trials, we tested respirators from several brands to determine whether this process could be valid for different N95 respirator models. For one model, piles of 10 or 12 N95 respirators were not always completely decontaminated. However, we observed in repeated tests that all respirator models could be decontaminated in piles of four, six or eight. Based on these results, it seems likely that N95 respirators can be consistently decontaminated in pile sizes of up to six units, but each facility should validate this process.
Piling N95 respirators will speed up the preparation process and significantly increase the capacity of a decontamination facility. It took 30 min for a single individual to hang 250 N95 respirators on one rack. In contrast, it took 8 min to pile the same number of N95 respirators on a rack. This means that it would take 8.5 h for a single individual to hang 4250 N95 respirators compared with 2.5 h if N95 respirators were piled as described. Furthermore, piles take up substantially less space than hung N95 respirators. It follows that using a six-stack piling strategy would increase the capacity of a facility such as ours from 4250 to 12240 units. Piling N95 respirators would also enable all hooks to be eliminated from the decontamination racks. Hooks can tear the PPE of personnel hanging respirators; thus, eliminating hooks would improve the overall safety of the procedure.
We also looked at ways to improve the sorting process of N95 respirators after decontamination. Our experience is that HCWs prefer to receive their own originally worn N95 respirators put in paper bags marked with their name. For this reason, we decontaminated N95 respirators kept in paper bags, but we replicated the worst-possible scenario sealing the bags and inserting CIs and BIs inside N95 respirators that were closed. We found that it is possible to decontaminate N95 respirators under the conditions tested. Leaving N95 respirators in paper bags would also speed up and facilitate the sorting of N95 respirators after the decontamination process and will not significantly decrease the capacity of the facility. We estimated that we could hang 50 N95 respirators per shelf or put up to 20 paper bags containing one or two N95 respirator per shelf.
In this project, we were able to design an inexpensive reproducible operation for the decontamination of N95 respirators using VHP. Some advantages of this operation were that it required a small facility and that the N95 respirator capacity could be easily increased by our modified procedures. We also reported possible ways to speed up the process of preparing N95 respirators for decontamination by arranging them in piles of four or six instead on hanging. Finally, we validated the potential to keep N95 respirators as they were received, in paper bags, during the decontamination process thus reducing handling time and allowing the return of N95 respirators to their original user.
Acknowledgements
The authors would like to thank Drs. Mark Einstein, Debra Chew, Ms. Safia Amatullah, Ms. Jo Ellen Harris and Mr. Lee Clark for coordinating the N95 respirator decontamination programme between UH and Rutgers and coordinating delivery and pickup of N95 respirators.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhin.2020.12.006.
Conflict of interest statement
D.A. receives license fees and research support from Cepheid, a company which develops and sells rapid clinical assays to detect SARS-CoV-2. All other authors have no conflicts of interest to disclose.
Funding sources
This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (grant no. T32AI125185). Decontamination costs and respirators used in the decontamination studies were paid for or supplied by UH, Newark.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Map of the facility used for decontamination of N95 respirators. Yellow rectangles represent the locations of metal racks, blue arrows represent the location and direction of fan air flow and the blue rectangle indicates the location of the VHP Victory unit. The red numbers indicate the locations of BIs and CIs in the room and the relative position: “H” = located in the highest portion of the wall, “M” = located in the middle level of the wall, “L” = located in the lower portion of the wall toward the floor.
Example of a decontamination cycle. In the graph is reported the concentration of VHP as a function of time and the Log Biological Kill.
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagesh S., Chakraborty S. Saving the frontline health workforce amidst the COVID-19 crisis: Challenges and recommendations. J Glob Health. 2020;10 doi: 10.7189/jogh-10-010345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herron J.B.T., Hay-David A.G.C., Gilliam A.D., Brennan P.A. Personal protective equipment and COVID 19- a risk to healthcare staff? Br J Oral Maxillofac Surg. 2020;58:500–502. doi: 10.1016/j.bjoms.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Sullivan E.D. PPE guidance for COVID-19: be honest about resource shortages. BMJ. 2020;369:m1507. doi: 10.1136/bmj.m1507. [DOI] [PubMed] [Google Scholar]
- 8.Whitworth J. COVID-19: a fast evolving pandemic. Trans R Soc Trop Med Hyg. 2020;114:241–248. doi: 10.1093/trstmh/traa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibáñez-Cervantes G., Bravata-Alcántara J.C., Nájera-Cortés A.S., Meneses-Cruz S., Delgado-Balbuena L., Cruz-Cruz C. Disinfection of N95 masks artificially contaminated with SARS-CoV-2 and ESKAPE bacteria using hydrogen peroxide plasma: Impact on the reutilization of disposable devices. Am J Infect Control. 2020;48:1037–1041. doi: 10.1016/j.ajic.2020.06.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal S.M., Chander Y., Yezli S., Otter J.A. Evaluating the virucidal efficacy of hydrogen peroxide vapour. J Hosp Infect. 2014;86:255–259. doi: 10.1016/j.jhin.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Procedure Guidance for N95 and Facemask Reuse. Health ND; 2020. [Google Scholar]
- 12.Lemieux P., Sieber R., Osborne A., Woodard A. Destruction of spores on building decontamination residue in a commercial autoclave. Appl Environ Microbiol. 2006;72:7687–7693. doi: 10.1128/AEM.02563-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Batelle . 2016. Final report for the bioquell hydrogen peroxide vapor (HPV) decontamination for reuse of N95 respirators.https://www.fda.gov/media/136386/download Available at: [last accessed 10/30/2020] [Google Scholar]
- 14.Levine C., Grady C., Block T., Hurley H., Russo R., Peixoto B. Use, reuse or discard: quantitatively defined variance in N95 respirator integrity following vaporized hydrogen peroxide decontamination during the COVID-19 pandemic. J Hosp Infect. 2020;16(107):50–56. doi: 10.1016/j.jhin.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng V.C., Wong S.-C., Kwan G.S., Hui W.-T., Yuen K.-Y. Disinfection of N95 respirators by ionized hydrogen peroxide during pandemic coronavirus disease 2019 (COVID-19) due to SARS-CoV-2. J Hosp Infect. 2020;105:358–359. doi: 10.1016/j.jhin.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Map of the facility used for decontamination of N95 respirators. Yellow rectangles represent the locations of metal racks, blue arrows represent the location and direction of fan air flow and the blue rectangle indicates the location of the VHP Victory unit. The red numbers indicate the locations of BIs and CIs in the room and the relative position: “H” = located in the highest portion of the wall, “M” = located in the middle level of the wall, “L” = located in the lower portion of the wall toward the floor.
Example of a decontamination cycle. In the graph is reported the concentration of VHP as a function of time and the Log Biological Kill.